Abstract
Introduction:
Long-acting reversible contraceptives (LARC), specifically implants and intrauterine devices (IUDs), are highly effective, low maintenance forms of birth control. Practice guidelines from the American College of Obstetricians and Gynecologists, American Academy of Family Physicians, and American Academy of Pediatrics recommend that LARC be considered first-line birth control for most women; however, uptake remains low. In this study, we sought to understand practices and barriers to provision of LARC in routine and immediate postpartum settings as they differ between specialties.
Methods:
We surveyed 3,000 Wisconsin physicians and advanced-practice providers in obstetrics-gynecology/women’s health (Ob-gyn), family medicine, pediatrics, and midwifery to assess practices and barriers (56.5% response rate). This analysis is comprised of contraceptive care providers (n=992); statistical significance was tested using chi-square and 2-sample proportions tests.
Results:
More providers working Ob-gyn (94.3%) and midwifery (78.7%) were skilled providers of LARC methods than those in family medicine (42.5%) and pediatrics (6.6%) (P < .0001). Lack of insertion skill was the most-cited barrier to routine provision among family medicine (31.1%) and pediatric (72.1%) providers. Among prenatal/delivery providers, over 50% across all specialties reported lack of device availability on-site as a barrier to immediate postpartum LARC provision; organizational practices also were commonly reported barriers.
Conclusions:
Gaps in routine and immediate postpartum LARC practice were strongly related to specialty, and providers’ experience heightened barriers to immediate postpartum compared to routine insertion. Skills training targeting family medicine and pediatric providers would enable broader access to LARC. Organizational barriers to immediate postpartum LARC provision impact many providers.
INTRODUCTION
Reducing unintended pregnancy is a national public health priority. Planned and safely spaced pregnancies result in fewer preterm births,1 higher educational and professional attainment for women and girls,2 lower abortion rates,2 and lower rates of maternal mortality.3 Similar to national estimates, in 2010, 46% of pregnancies in Wisconsin were unintended at an estimated cost of $313.5 million.4
Long-acting reversible contraceptives (LARC), including intrauterine devices (IUD) and hormonal subdermal implants, are the most effective and lowest-maintenance forms of reversible birth control currently available.5 Both patients and clinicians view these devices as highly acceptable contraceptive options,6,7 and practice guidelines from leading physician groups8–10 recommend that LARC be considered first-line birth control for most women; however, uptake remains low. High initial costs may be a barrier for some patients. A statewide initiative in Colorado that provided free contraceptives, including IUDs and implants, led to significant reductions in unintended teen pregnancies and abortions and dramatic cost savings to the health care system and social services.2,11
Strategies to increase access to LARC are essential. Prior studies identified knowledge gaps regarding patient eligibility for LARC12,13 as well as practice differences at the provider level.13,14 Known barriers to LARC provision include provider training2,12,15 and inability to perform same-day insertion,16 which together limit overall use. However, it is unclear how contraceptive care differs across specialties and among midlevel providers. For example, there is some evidence that advanced practice providers (APP) are less likely than physicians to insert LARC devices.17 Given that APPs comprise a large portion of the women’s health workforce, especially in underserved areas, it is important to understand their provision of contraceptives.
The immediate postpartum (IPP) period is an opportune time to provide these long-acting methods, increasing long-term cost effectiveness11 and eliminating the need for a follow-up visit.18 When compared to those using other reversible methods, women receiving LARC in the immediate postpartum period are more likely to have optimally spaced subsequent pregnancies.19
The purpose of this study was to understand contraceptive practices and barriers related to LARC methods in both the routine and immediate postpartum settings among physician and midlevel providers across practice specialties in Wisconsin.
METHODS
Setting and Design
We conducted a mailed survey of physicians, nurse practitioners, and midwives holding active licenses in Wisconsin in 2014. The study was reviewed by the University of Wisconsin-Madison Institutional Review Board and deemed exempt.
We obtained from the state’s Department of Safety and Professional Services a list of providers with an active license to practice medicine or surgery who listed their specialty as obstetrics and gynecology (ob-gyn), family medicine, or pediatrics; APPs if they had an active license and listed their specialty as midwifery, ob-gyn/women’s health, family medicine, or pediatrics. Physician assistants were not included. We included all providers who had a mailing address in Wisconsin or within 50 miles of the Wisconsin border (n = 7,750). ArcGIS 10.2 was used to geocode mailing addresses, and straight-line buffers were used to identify addresses meeting our 50-mile criteria.
The University of Wisconsin Survey Center (UWSC) mailed the survey to all ob-gyn (n = 1,002) and midwifery (n = 323) providers and sampled 21% in family medicine (n = 1,000) and 47% in pediatrics (n = 675) to achieve a total sample of 3,000. We sampled all ob-gyns and midwives given their high likelihood of providing services to women of reproductive age (13–44 years) and sampled providers in family medicine and pediatrics to ensure sufficient sample size for comparison across specialties. We used SAS 9.4 (SAS Institute Inc., Cary, NC) to select family medicine and pediatric providers via simple random sampling. In consultation with the UWSC, we developed an 8-page, written, self-administered survey. We adapted some questions from prior surveys,20,21 piloted the survey, and modified questions based on iterative feedback. UWSC employed Dillman’s Total Design Method22 utilizing a 4-contact data collection design between September and October 2015. Initial mailing included a cover letter, survey, self-addressed stamped envelope, and $5 cash incentive. All providers received a postcard reminder 6 days later. Follow-up mailings occurred 4 and 7 weeks from the first mailing.
Our primary variable of interest was skilled insertion of the 3 LARC devices: levonorgestrel IUD (LNG-IUD), copper IUD (Cu-IUD), and hormonal implant. Providers who reported both personally inserting LARC and being “very” or “extremely” confident in insertion of a specific LARC method were classified as “skilled [device] inserters.” Providers reporting that they “very often” refer patients to other clinicians for LARC insertion and/or “never” prescribe that LARC device were removed from the skilled inserters group for that device. This logic check thus excluded providers who were not inserting LARC regularly. If they were skilled inserters of any of the 3 devices, providers were considered skilled inserters of “any LARC.”
Our secondary outcomes included provider report of same-day LARC insertion, frequency of LARC counseling, knowledge of medical eligibility guidelines, and provider- and systems-level barriers. Knowledge of guidelines was measured by asking respondents to assess the accuracy of commonly perceived contraindications, including teenage patients (ages 13–19), nulliparous, nonmonogamous, postabortion, immediately postpartum or postplacental, breastfeeding, or history of ectopic pregnancy.8,11
Provider-level barriers assessed included lack of skill in insertion, lack of familiarity with insurance policies, cost of the device, challenges with reimbursement, and personal or religious beliefs. Systems-level barriers for both routine and IPP LARC included low patient interest, lack of eligible patients, lack of time available for counseling, and devices not available on site. Barriers unique to IPP LARC included group practice call schedule rotation, coordination of LARC services with delivery facility, delivery facility prohibition, and organizational policies related to IPP LARC.
Statistical Analysis
Most survey items used 5-point Likert-type response scales. Because exploratory analyses showed bimodally distributed data for the majority of items, we created dichotomous variables by collapsing responses (“Not at All/Never/None,” “A Little/Rarely/Very Few,” and “Somewhat/Sometimes/Some” = −1; “Very/Often/Quite a Bit/Many,” and “Extremely/Very Often/A Great Deal/Most” = +1).
Given the large between-specialty differences in LARC provision, we stratified results by specialty. For relevant analyses, we also stratified within-specialty results by provider type comparing physicians and midwives. We used the National Center for Health Statistics classification system23 to classify respondents as urban or rural, based on the county in which they indicated seeing the most patients.
We used chi-square tests and 2-sample tests of proportions to compare outcomes by provider specialty and considered P-values <. 05 to be significant. All analyses were conducted using Stata SE software (version 14.1, StataCorp, College Station, Texas).
RESULTS
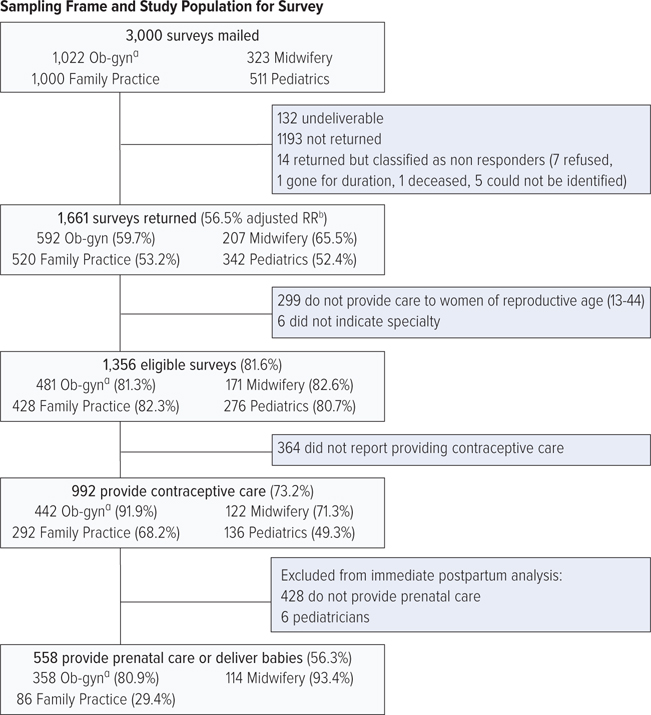
Of 3,000 mailed surveys, 1,661 surveys were returned and identifiable for an overall adjusted response rate of 56.5% (Figure 1). In this analysis, we include those who reported that they currently provide contraceptive services and indicated their specialty (n = 992, 59.7%). Contraceptive providers included 442 working in ob-gyn, 122 in midwifery, 292 in family medicine, and 136 in pediatrics. For the analyses of practice related to IPP contraception, we include the 56.3% (n = 558) of contraceptive providers who also reported providing prenatal care and/or delivering babies within the past 12 months. Eighty-one percent (n = 358) of those working in ob-gyn, 93.4% (n = 114) in midwifery, and 29.4% (n = 86) in family medicine met this criterion. The small number working in pediatrics (n = 6) were excluded from the IPP analyses. Table 1 provides a description of survey respondents by practice area.
Figure 1.
Survey Flow Diagram
Abbreviations: Ob-gyn, obstetrics and gynecology; RR, risk ratio.
a Practicing in obstetrics and gynecology.
b Adjusted for the proportion of the unknown eligibility who are eligible.
Table 1.
Selected Personal and Practice Characteristics of Wisconsin Contraceptive Providers, by Specialty
| ob-gyna (n=442) | Midwifery (n=122) | Family Medicine (n-292) | Pediatrics (n=136) | P-valueb | |
|---|---|---|---|---|---|
| Provider level | |||||
| Physician | 343 (77.6%) | 0 (0.0%) | 187 (64.0%) | 117 (86.0%) | <.0001 |
| Advanced practice provider | 99 (22.4%) | 122 (100.0%) | 105 (36.0%) | 19 (14.0%) | |
| Sex | |||||
| Female | 312 (70.6%) | 120 (98.4%) | 202 (69.2%) | 120 (88.2%) | <.0001 |
| Race/ethnicity | |||||
| Hispanic | 13 (2.9%) | 4 (3.3%) | 6 (2.1%) | 3 (2.2%) | .11 |
| Non-Hispanic white | 375 (84.8%) | 110 (90.2%) | 261 (89.4%) | 112 (82.4%) | |
| Non-Hispanic black | 11 (2.5%) | 0 (0.0%) | 3 (1.0%) | 0 (0.0%) | |
| Non-Hispanic otherc | 33 (7.4%) | 7 (5.7%) | 15 (5.1%) | 17 (12.5%) | |
| Earned license | |||||
| 1994 or earlier | 168 (38.0%) | 18 (14.8%) | 70 (24.0%) | 36 (26.5%) | <.0001 |
| 1995–2004 | 126 (28.5%) | 41 (33.6%) | 81 (27.7%) | 44 (32.3%) | |
| 2005 or later | 148 (33.5%) | 63 (51.6%) | 141 (48.3%) | 56 (41.2%) | |
| Practice settingd | |||||
| Group/solo practice | 297 (67.2%) | 59 (48.4%) | 183 (62.7%) | 81 (59.6%) | .002 |
| Hospital | 122 (27.6%) | 36 (29.5%) | 32 (11.0%) | 22 (16.2%) | <.0001 |
| Academic | 74 (16.7%) | 19 (15.6%) | 42 (14.4%) | 31 (22.8%) | .18 |
| Othere | 89 (20.1%) | 55 (45.1%) | 83 (28.4%) | 29 (21.3%) | <.0001 |
| % Medicaid patients | |||||
| Up to half | 245 (55.4%) | 34 (27.9%) | 185 (63.4%) | 73 (53.7%) | <.0001 |
| Half or more | 194 (43.9%) | 88 (72.1%) | 107 (36.6%) | 62 (45.6%) | |
| Urban/rural statusf | |||||
| Large metro | 156 (35.3%) | 42 (34.4%) | 79 (27.1%) | 57 (41.9%) | .004 |
| Small metro | 203 (45.9%) | 57 (46.7%) | 122 (41.8%) | 55 (40.4%) | |
| Micropolitan or rural | 77 (17.4%) | 20 (16.4%) | 85 (29.1%) | 22 (16.2%) |
Not all columns add up to 100%, due to missing values.
Abbreviations: ob-gyn, obstetrician-gynecologists.; APP, advanced practice providers.
Ob-gyn, obstetrician-gynecologists and advanced practice providers in ob-gyn or women’s health.
From chi-square test of homogeneity.
Includes Non-Hispanic Asian, Non-Hispanic American Indian/Alaska Native, Non-Hispanic Hawaiian/Pacific Islander, and Non-Hispanic “other.”
Percentages do not add up to 100% because this was a “check all that apply” item.
Includes Planned Parenthood, other family planning clinics, health maintenance organizations/managed care, Federally Qualified Health Centers, and “other.”
Only accounts for the first of up to 2 counties listed (n = 167 listed a second county of practice).
LARC Provision
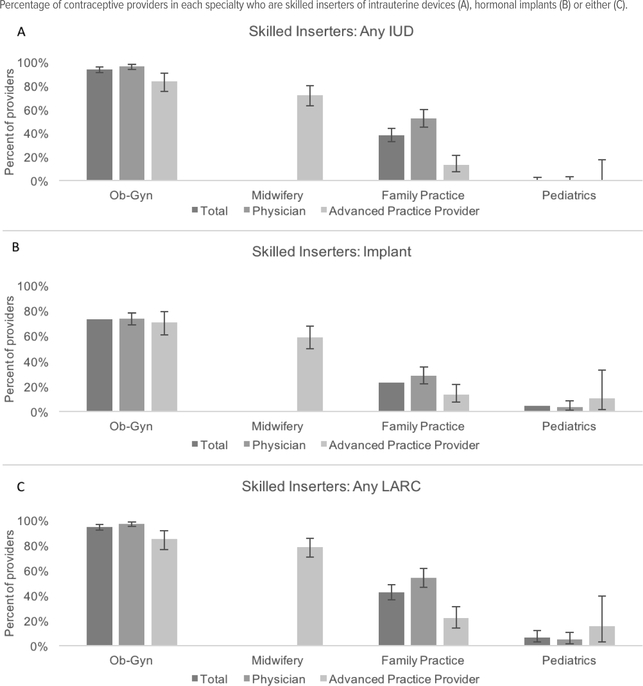
Figure 2 shows the percentages of contraceptive providers identified as skilled in insertion by device and by provider type. Overall, 94.3% of providers in ob-gyn, 78.7% in midwifery, 42.5% in family medicine, and 6.6% in pediatrics are skilled inserters of at least one device. A greater proportion of physicians than APPs working in ob-gyn and family medicine were skilled at insertion of each (P < .0001). There were no significant differences by provider sex (P = .12), years since clinical training (P = .37), or urban-rural practice location (P = .12). Only 30.0% of pediatric providers who have been trained in LARC insertion report currently inserting a device, while the majority of providers in the other specialties do (P < .001).
Figure 2.
Proportion of Contraceptive Providers Surveyed, by and Within Specialty, Who Are Skilled Inserters of 1 or More LARC Methods
Providers who reported both personally inserting LARC and being “very” or “extremely” confident in insertion of a specific LARC method were classified as “skilled [device] inserters.”
Error bars represent 95% confidence intervals.
Abbreviations: IUD=Intrauterine device. LARC=Long-acting reversible contraceptives.
More providers working in ob-gyn are skilled in the insertion of IUDs compared to implants (P < .0001); a greater proportion of those working in ob-gyn compared to midwifery are skilled IUD inserters (P < .0001). Thirty-eight percent of those working in family medicine and none in pediatrics were skilled IUD inserters and, similarly, were less likely to be skilled implant inserters when compared to those in ob-gyn (P < .0001).
There are marked differences by specialty in counseling practice. Ninety-eight percent in ob-gyn, 91.8% in midwifery, 82.5% in family medicine, and 53.7% in pediatrics reported that they discuss the LNG-IUD “often” or “very often” (all pairwise differences < .05). Similarly, more in ob-gyn (83.7%) and midwifery (82.0%) reported that they discuss the implant “often” or “very often,” compared to those in family medicine (66.1%) and pediatrics (54.4%, all pairwise differences < .05). A greater proportion of providers in ob-gyn (73.5%) and midwifery (79.5%) reported that they discuss the Cu-IUD “often” or “very often” compared to those in family medicine (57.2%) and pediatrics (13.2%, all pairwise differences < .05).
When asked about providing same-day LARC insertion, responses vary by specialty: 74.7% in ob-gyn, 52.5% in midwifery, 29.1% in family medicine, and 14.0% in pediatrics (all pairwise differences P < .001) make same-day insertion available to their patients. Of providers who do not currently insert either IUDs or implants, 85.2% reported that they refer their patients to other clinicians “often” or “very often,” with no differences by specialty (P = .51).
Eligibility Guideline Knowledge
We assessed knowledge of current patient eligibility guidelines by asking respondents to indicate whether selected patient characteristics were contraindications for LARC devices. As shown in Table 2, across specialties, one of the most common perceived contraindications was the immediate postpartum period, reported by 16.8% of those working in ob-gyn, 28.2% in midwifery, 36.5% in family medicine, and 38.3% in pediatrics. Many working in family medicine (33.7%), pediatrics (39.2%), and midwifery (35.9%) considered a history of ectopic pregnancy to be a contraindication, compared to 11.3% in ob-gyn. More than a quarter of providers in pediatrics (26.7%) saw women in the postabortion period as contraindicated for LARC, and about a third of providers in family practice (30.5%) saw teens as contraindicated.
Table 2.
Perceived Contraindications for Any LARC Among Wisconsin Providers Who Report Providing Contraceptive Carea
| Ob-gyn (n = 435) |
Midwifery (n = 117) |
Family Medicine (n = 282) |
Pediatrics (n = 120) |
P-valueb | |
|---|---|---|---|---|---|
| For teens or adolescents ages 13–19 | 12.0% | 9.0% | 30.5% | 20.8% | <.0001 |
| For nulliparous patients | 5.3% | 3.4% | 12.8% | 9.2% | .007 |
| For nonmonogamous patients | 13.3% | 10.3% | 20.2% | 10.0% | .016 |
| Following an abortion | 3.7% | 5.1% | 18.4% | 26.7% | <.0001 |
| While breastfeeding | 3.2% | 7.7% | 24.8% | 17.5% | <.0001 |
| For patients with a history of ectopic pregnancy | 11.3% | 35.9% | 33.7% | 39.2% | <.0001 |
| Immediately postpartum/postplacental | 16.8% | 28.2% | 36.5% | 38.3% | <.0001 |
Abbreviations: LARC, Long-acting reversible contraceptive; Ob-gyn, includes obstetrician gynecologists and advanced practice providers working in Ob-gyn or women’s health.
Providers who answered zero LARC barriers (n = 38) were excluded from this analysis.
Chi-square test of difference by specialty.
Provider and Systems Barriers
As shown in Table 3, barriers differed by specialty and were most commonly reported by those working outside of ob-gyn practice settings. Lack of skill with insertion was cited most frequently by providers in pediatric settings (72.1%), followed by those in family medicine (31.1%) and midwifery (10.9%, all pairwise comparisons P < .0001). Challenges with reimbursement were cited by 10.7% in pediatrics; more in midwifery (16.0%) than in family medicine (8.7%) reported this barrier (P = .03). Fourteen percent of providers in midwifery, 10.8% in family medicine, and 10.7% in pediatrics reported that cost of devices was a barrier (P = .002). Lack of familiarity with insurance policies was cited by 17.2% of providers in pediatrics but by fewer than 10% of providers in other specialties. Personal or religious beliefs was cited by fewer than 5% in all specialties. Five percent or fewer of ob-gyn providers indicated that any provider-level barrier affected their LARC provision.
Table 3.
Barriers Affecting Routine LARC Provision “Quite a Bit” or “a Great Deal,” Among Wisconsin Providers Who Report Providing Contraceptive Carea
| Ob-gyn (n = 438) |
Midwifery (n = 119) |
Family Medicine (n = 277) |
Pediatrics (n = 122) |
P-valueb | |
|---|---|---|---|---|---|
| Lack of skill in insertion | 1.8% | 10.9% | 31.1% | 72.1% | <.0001 |
| Lack of familiarity with | 2.5% | 7.6% | 9.4% | 17.2% | <.0001 |
| insurance policies | |||||
| Cost of device | 5.0% | 14.3% | 10.8% | 10.7% | .002 |
| Challenges with reimbursement | 4.1% | 16.0% | 8.7% | 10.7% | <.0001 |
| Personal or religious beliefs | 0.7% | 3.4% | 2.5% | 3.3% | .08 |
| Low patient interest | 5.3% | 10.1% | 13.4% | 27.1% | <.0001 |
| Lack of eligible patients | 3.4% | 1.7% | 7.9% | 12.3% | <.0001 |
| Lack of time for counseling | 0.9% | 0.8% | 2.2% | 9.0% | <.0001 |
| Lack of time for procedure | 0.9% | 0.8% | 4.3% | 13.9% | <.0001 |
| Devices not available on-site | 4.8% | 17.7% | 12.3% | 29.5% | <.0001 |
| Separate visit required for insertion | 3.0% | 10.1% | 9.8% | 21.3% | <.0001 |
Abbreviations: LARC, Long-acting reversible contraceptive; Ob-gyn, includes obstetrician-gynecologists and advanced practice providers working in Ob-gyn or women’s health.
Providers who answered zero LARC barriers (n = 36) were excluded from this analysis.
Chi-square test of difference by specialty.
The lack of availability of devices on-site was reported by more providers in pediatrics (29.5%) than in midwifery (17.7%) or family medicine (12.3%; P < .05). Lack of patient interest was cited most frequently by providers in pediatrics (27.1%), followed by those in family medicine (13.4%) and midwifery (10.1%, P < .001). Several barriers were reported infrequently by providers in family medicine and midwifery, but commonly by those in pediatrics, including lack of eligible patients (12.3%), lack of time for procedure (13.9%), and requirement of a separate visit for insertion (21.3%). Lack of time for counseling was reported by 10% or fewer of all providers in each specialty area. Again, fewer than 5% of providers in ob-gyn settings indicated that any systems-level barrier affected LARC provision.
More than 80% of respondents indicated resources for patient education, and about half or more indicated provider education on counseling and an algorithm for counseling would help them counsel patients about LARC methods. Sixty-six percent of providers indicated that in-person continuing medical education would help enable their practice, but only 34.9% responded that having a nonphysician educator present in clinic would be helpful. Fewer in ob-gyn (34.0% and 20.7%, respectively) indicated that either of these resources would help them counsel about LARC (P < .001).
Unique IPP LARC Issues
A majority (95%) of prenatal/delivery providers reported that they discuss postpartum contraception during pregnancy or at delivery; only 12.4% reported specifically discussing IPP LARC, a proportion that did not differ by specialty (P = 0.29). Nine percent of prenatal/delivery providers reported discussing the LNG-IUD as a form of IPP contraception with “many” or “most” patients; 6.1% the Cu-IUD; and 11.1% the implant, with no differences by specialty for any device.
More prenatal/delivery providers in ob-gyn (81.4%) correctly indicated that the IPP period is not a contraindication to using any LARC, compared to those in family medicine (68.6%) and midwifery (68.8%, P < .01). A greater proportion of prenatal/delivery providers in ob-gyn (96.6%) compared to midwifery (89.0%) and family medicine (81.4%) appropriately stated that these devices are not contraindicated while breastfeeding (P < .01).
Table 4 compares barriers reported by prenatal/delivery providers to routine versus IPP provision of LARC. Prenatal/delivery providers generally reported heightened barriers to providing IPP compared to routine LARC. In all 3 specialty groups, a significantly greater proportion reported lack of skill in IPP insertion (all P < .0001), devices not available onsite in the IPP period (all P < .0001), and lack of familiarity with IPP vs routine insurance policies (all P < .01). A significantly greater proportion of those working in ob-gyn reported issues regarding cost of devices, challenges with reimbursement, lack of eligible patients, and lack of time for counseling in the IPP period compared to in-routine practice (all P < .0001). Lack of skill with IPP insertion was a commonly cited barrier among those in family medicine (35.9%) and midwifery (34.2%). Over 20% of providers in midwifery reported barriers to IPP LARC related to low patient interest, lack of familiarity with insurance, cost of device, challenges with reimbursement, and policies in the group organization or practice related to LARC.
Table 4.
Comparison of Barriers Affecting Routine and Immediate Postpartum LARC Provision “Quite a Bit” or “a Great Deal” Among Wisconsin Providers Who Report Providing Both Contraceptive Care and Prenatal Care or Obstetrical Deliverya
| Ob-gyn (n=358) | Family Medicine (n=86) | Midwifery (n=111) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Routine | IPP | P-valueb | Routine | IPP | P-valueb | Routine | IPP | P-valueb | |
| Barriers impacting both routine and IPP LARC | |||||||||
| Lack of skill in insertion | 0.8% | 13.8% | <.0001 | 8.1% | 35.9% | <.0001 | 11.7% | 34.2% | <.0001 |
| Lack of familiarity with insurance policies | 1.7% | 10.6% | <.0001 | 3.5% | 16.7% | <.0001 | 7.2% | 22.5% | .001 |
| Cost of device | 3.4% | 8.5% | <.0001 | 5.8% | 7.7% | .63 | 14.4% | 20.7% | .13 |
| Challenges with reimbursement | 3.1% | 16.3% | <.0001 | 8.1% | 9.0% | .85 | 16.2% | 22.5% | .24 |
| Personal or religious beliefs | 0.6% | 0.9% | .62 | 2.3% | 1.3% | .62 | 3.6% | 6.3% | .35 |
| Low patient interest | 3.9% | 28.7% | <.0001 | 11.6% | 16.7% | .35 | 10.8% | 36.0% | <.0001 |
| Lack of eligible patients | 2.0% | 9.4% | <.0001 | 3.5% | 5.1% | .60 | 1.8% | 6.3% | .09 |
| Lack of time for counseling | 0.6% | 5.9% | <.0001 | 1.2% | 5.1% | .14 | .9% | 2.7% | .31 |
| Devices not available on-site | 3.4% | 52.5% | <.0001 | 7.0% | 50.0% | <.0001 | 18.0% | 59.5% | <.0001 |
| Barriers unique to IPP LARC | |||||||||
| Group practice call schedule rotation | N/A | 16.4% | N/A | N/A | 3.9% | N/A | N/A | 13.5% | N/A |
| Coordination of LARC services with delivery facility | N/A | 37.8% | N/A | N/A | 34.6% | N/A | N/A | 46.0% | N/A |
| Delivery facility prohibition of LARC | N/A | 31.4% | N/A | N/A | 35.9% | N/A | N/A | 27.0% | N/A |
| Policies in my organization or practice related to immediate postpartum LARC | N/A | 23.8% | N/A | N/A | 24.4% | N/A | N/A | 30.6% | N/A |
Abbreviations: IPP, immediate postpartum; LARC, long-acting reversible contraceptive; N/A, Not applicable.
Providers who answered zero LARC barriers (n = 3) were excluded from routine columns; providers who answered zero IPP LARC barriers (n = 28) were excluded from IPP columns.
Chi-square test of difference by LARC insertion period.
DISCUSSION
In this statewide survey of contraceptive providers in Wisconsin, we found significant differences between and within provider specialty groups, with providers in ob-gyn and midwifery practices more likely to be skilled at the insertion of IUDs and implants, when compared to providers in family medicine and pediatrics. We identified similar variation by specialty in counseling practices, same-day provision, and knowledge of eligibility guidelines.
In the routine setting, few working in ob-gyn practices indicated barriers to providing these methods. However, those in family medicine and pediatrics frequently reported a lack of skill and absence of devices on-site. These heightened barriers may be a reflection of scope of practice differences, with pediatric and family practice providers seeing a smaller volume of reproductive health issues compared to those in ob-gyn or midwifery.
More providers in our sample were skilled in placement of IUDs than implants, consistent with results from a study of rural family medicine and internal medicine physicians.14 Similar to results from another study, family medicine and pediatric providers were less likely to recommend, provide, and feel comfortable inserting IUDs than those working in ob-gyn practices.13 A greater proportion of physicians than APPs are skilled at inserting any LARC, similar to findings in a 2008 survey of family planning providers.17 With the growing reliance on APPs for women’s preventive care including contraceptive counseling, LARC training specific for APPs is needed.
We found that providers face important systems-level barriers to routine LARC provision, including devices not being available onsite. Tyler et al (2012) showed that providers without IUDs onsite had increased odds of misconceptions about IUD safety, suggesting that knowledge deficits may accompany systems barriers, both of which have tangible consequences for LARC provision.12 In the present study, few in ob-gyn indicated substantial barriers, implying that LARC provision is strongly influenced by the clinical context. For example, the frequency with which providers insert LARC may influence barriers such as reimbursement or navigating insurance; however, this is an area for further research.
Despite indicating knowledge about immediate postpartum insertion, providers discuss IPP LARC fairly infrequently. This is important because contraceptive discussions with a prenatal provider increase the likelihood of postpartum LARC use.24 Known challenges associated with IPP LARC use, such as high IUD expulsion rates, could limit the enthusiasm of some providers.11 Providers reported more barriers to the insertion in the postpartum period, including unique barriers such as facility policies. These findings support the importance of strategies developed by the “Learning Community” of the Association of State and Territorial Health Officials, which implemented policies in birthing facilities that sought to address several of the barriers identified in our study, including training, reimbursement, stocking, and supply.25
This study is limited in that it measures self-reported practices and not actual practice. Some questions (ie, insertion, same-day insertion) assessed LARC provision as a whole rather than by device, but in fact these practices may differ between IUDs and implants. Similarly, the survey does not specifically ask providers about their IPP LARC insertion practices, instead asking only if providers discuss IPP LARC as a contraceptive option. While we have a strong response rate, practices among nonrespondents may differ from those who did respond to the survey. Further, without knowing the reach of each specialty in their provision of contraception across the state, we cannot fully estimate the impact of these differences in practice on access at the population level.
Our findings suggest that strategies to support contraceptive recommendations from American College of Obstetricians and Gynecologists, American Academy of Family Physicians, and American Academy of Pediatrics should address both provider skill gaps as well as systems-related barriers in both the routine and obstetrical settings. In light of the myriad complex barriers to contraceptive access, addressing providers’ challenges at the healthcare system level may be a feasible strategy for intervention. Education through continuing medical education could improve provider understanding of contraindications and guide discussions about LARC. Our study suggests that increasing training, especially among APPs and pediatric and family medicine providers, as well as revising health systems policies, are critical steps to improving women’s broad access to these essential health services.
Funding/Support:
This work was supported, in part, by funding from the Wisconsin Department of Health Services and the University of Wisconsin School of Medicine and Public Health from the Wisconsin Partnership Program and the Herman and Gwendolyn Shapiro Foundation.
Financial Disclosures: None declared.
REFERENCES
- 1.Rodriguez MI, Chang R, Thiel de Bocanegra H. The impact of postpartum contraception on reducing preterm birth: findings from California. Am J Obstet Gynecol. 2015;213(5):703.e1–703.e6. doi: 10.1016/j.ajog.2015.07.033. [DOI] [PubMed] [Google Scholar]
- 2.Ricketts S, Klingler G, Schwalberg R. Game change in Colorado: widespread use of long-acting reversible contraceptives and rapid decline in births among young, low-income women. Perspect Sex Reprod Health. 2014;46(3):125–132. doi: 10.1363/46e1714. [DOI] [PubMed] [Google Scholar]
- 3.Tsui AO, McDonald-Mosley R, Burke AE. Family planning and the burden of unintended pregnancies. Epidemiol Rev. 2010;32(1):152–174. doi: 10.1093/epirev/mxq012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sonfield A, Kost K. Public costs from unintended pregnancies and the role of public insurance programs in paying for pregnancy-related care: national and state estimates for 2010. Guttmacher Institute; https://www.guttmacher.org/pubs/public-costs-of-UP-2010.pdf. Published February 2015. Accessed December 1, 2016. [Google Scholar]
- 5.Trussell J, Henry N, Hassan F, Prezioso A, Law A, Filonenko A. Burden of unintended pregnancy in the United States: potential savings with increased use of long-acting reversible contraception. Contraception. 2013;87(2):154–161. doi: 10.1016/j.contraception.2012.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Secura GM, Allsworth JE, Madden T, Mullersman JL, Peipert JF. The Contraceptive CHOICE Project: reducing barriers to long-acting reversible contraception. Am J Obstet Gynecol. 2010;203(2):115.e1–115.e7. doi: 10.1016/j.ajog.2010.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harper CC, Henderson JT, Raine TR, et al. Evidence-based IUD practice: family physicians and obstetrician-gynecologists. Fam Med. 2012;44(9):637–645. [PMC free article] [PubMed] [Google Scholar]
- 8.ACOG Committee Opinion No. 450: Increasing use of contraceptive implants and intrauterine devices to reduce unintended pregnancy. Obstet Gynecol. 2009;114(6):1434–1438. doi: 10.1097/AOG.0b013e3181c6f965. [DOI] [PubMed] [Google Scholar]
- 9.Randel A Guidelines for the use of long-acting reversible contraceptives. Am Fam Physician. 2012;85(4):403–404. [PubMed] [Google Scholar]
- 10.Ott MA, Sucato GS; Committee on Adolescence. Contraception for adolescents. Pediatrics. 2014;134(4):e1257–e1281. doi: 10.1542/peds.2014-2300. [DOI] [PubMed] [Google Scholar]
- 11.Goldthwaite LM, Shaw KA. Immediate postpartum provision of long-acting reversible contraception: Curr Opin Obstet Gynecol. 2015;27(6):460–464. doi: 10.1097/GCO.0000000000000224. [DOI] [PubMed] [Google Scholar]
- 12.Tyler CP, Whiteman MK, Zapata LB, Curtis KM, Hillis SD, Marchbanks PA. Health care provider attitudes and practices related to intrauterine devices for nulliparous women. Obstet Gynecol. 2012;119(4):762–771. doi: 10.1097/AOG.0b013e31824aca39. [DOI] [PubMed] [Google Scholar]
- 13.Harper CC, Stratton L, Raine TR, et al. Counseling and provision of long-acting reversible contraception in the US: national survey of nurse practitioners. Prev Med. 2013;57(6):883–888. doi: 10.1016/j.ypmed.2013.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lunde B, Smith P, Grewal M, Kumaraswami T, Cowett A, Harwood B. Long acting contraception provision by rural primary care physicians. J Womens Health. 2014;23(6):519–524. doi: 10.1089/jwh.2013.4286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rubin SE, Fletcher J, Stein T, Segall-Gutierrez P, Gold M. Determinants of intrauterine contraception provision among US family physicians: a national survey of knowledge, attitudes and practice. Contraception. 2011;83(5):472–478. doi: 10.1016/j.contraception.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 16.Biggs MA, Arons A, Turner R, Brindis CD. Same-day LARC insertion attitudes and practices. Contraception. 2013;88(5):629–635. doi: 10.1016/j.contraception.2013.05.012. [DOI] [PubMed] [Google Scholar]
- 17.Harper CC, Blum M, de Bocanegra HT, et al. Challenges in translating evidence to practice: the provision of intrauterine contraception. Obstet Gynecol. 2008;111(6):1359–1369. doi: 10.1097/AOG.0b013e318173fd83. [DOI] [PubMed] [Google Scholar]
- 18.Zerden ML, Tang JH, Stuart GS, Norton DR, Verbiest SB, Brody S. Barriers to receiving long-acting reversible contraception in the postpartum period. Womens Health Issues. 2015;25(6):616–621. doi: 10.1016/j.whi.2015.06.004. [DOI] [PubMed] [Google Scholar]
- 19.Thiel de Bocanegra H, Chang R, Howell M, Darney P. Interpregnancy intervals: impact of postpartum contraceptive effectiveness and coverage. Am J Obstet Gynecol. 2014;210(4):311.e1–311.e8. doi: 10.1016/j.ajog.2013.12.020. [DOI] [PubMed] [Google Scholar]
- 20.Biggs MA, Harper CC, Malvin J, Brindis CD. Factors influencing the provision of long-acting reversible contraception in California. Obstet Gynecol. 2014;123(3):593–602. doi: 10.1097/AOG.0000000000000137. [DOI] [PubMed] [Google Scholar]
- 21.Frost Jennifer J, Gold RB, Frohwirth L, Blades N. Variation in service delivery practices among clinics providing publicly funded family planning services in 2010. Guttmacher Institute; https://www.guttmacher.org/sites/default/files/report_pdf/clinic-survey-2010.pdf. Published May 2012. Accessed September 18, 2018. [Google Scholar]
- 22.Hoddinott S, Bass M. The Dillman Total Design Survey Method. Can Fam Physician. 1986;32:2366–2368. [PMC free article] [PubMed] [Google Scholar]
- 23.Ingram DD, Franco SJ. 2013 NCHS Urban-Rural Classification Scheme for Counties. Vital Health Stat 2 2014;(166):1–73. [PubMed] [Google Scholar]
- 24.Starr KA, Martins SL, Watson S, Gilliam ML. Postpartum contraception use by urban/rural status: an analysis of the Michigan Pregnancy Risk Assessment Monitoring System data. Womens Health Issues. 2015;25(6):622–627. doi: 10.1016/j.whi.2015.06.014. [DOI] [PubMed] [Google Scholar]
- 25.Rankin KM, Kroelinger CD, DeSisto CL, et al. Application of implementation science methodology to immediate postpartum long-acting reversible contraception policy roll-out across states. 2016;20(Suppl 1):173–179. doi: 10.1007/s10995-016-2002-4. [DOI] [PMC free article] [PubMed] [Google Scholar]