Abstract
Objective: To analyze the long‐term effect of double‐strut bone graft for osteonecrosis of the femoral head (ONFH).
Methods: A total of 366 adult patients with ONFH in 466 hips underwent double‐strut bone graft from March 1988 to January 1999. Of them, 186 patients with 206 hips and an average age of 32.2 years (range, 20–60 years) were followed up for more than five years, up to January 2006. Based on the Association Research Circulation Osseous (ARCO) classification, there were 36 hips in stage IIB, and 30, 40, 40, 32 and 28 in stage IIC, IIIA, IIIB, IIIC and IV, respectively. The functional results of affected hips were evaluated by the hundred forked method.
Results: Hip pain in all patients disappeared or alleviated greatly after the operation. The height of the femoral head improved to various extents, and the range of motion of the hip joint increased. The patients were followed up for 5–16 years, (average 10.5 years). The total scores increased significantly postoperatively (P < 0.01). The rate of excellent and good results was 83.3%, 80.0%, 75.0%, 65.0%, 40.6% and 28.6% in stage IIB, IIC, IIIA, IIIB, IIIC and IV, respectively (63.6% for the whole group).
Conclusion: The long–term effect of double‐strut bone graft for ONFH is satisfactory in relation to staging of ONFH. Favorable results can be expected in young ONFH patients in stage IIB, IIC, and IIIA, IIIB.
Keywords: Bone transplantation, Femur head necrosis, Treatment outcome
Introduction
Osteonecrosis of the femoral head (ONFH), a common orthopaedic disease, mostly affects young and middle‐aged people. About 80% of the involved femoral heads will collapse in one to four years, resulting in dysfunction of the affected joint. Eventually, most of the patients are destined to have artificial hip joint replacement 1 . In order to change the natural history of ONFH and preserve the necrotic femoral head, a double‐strut bone graft technique has been employed in our department for 366 adult patients with ONFH in 466 hips since March 1988. Of them, 186 patients with 206 hips have been followed up for more than 5 years to evaluate the long‐term outcomes of this head‐preserving technique.
Methods and materials
Of the 186 patients with 206 hips, there were 116 men and 70 women, with a mean age of 32.2 years ranging from 20 to 60 years. The etiological classification was steroid‐induced ONFH in 60 patients with 68 hips, alcohol‐induced ONFH in 86 patients with 96 hips, both steroid and alcohol‐induced ONFH in 30 patients with 32 hips, and traumatic ONFH in 10 patients with 10 hips. Based on the Association Research Circulation Osseous (ARCO) classification, there were 36 hips in stage IIB, and 30, 40, 40, 32 and 28 in stage IIC, IIIA, IIIB, IIIC and IV, respectively. Age distribution was as follows: 80 hips (38.8%) in the third decade, 70 (34.0%) in the forth, 36 (17.5%) in the fifth and 20 (9.7%) in the sixth. Ninety of the involved hips were on the left and 116 on the right.
Operative technique and postoperative management
The patient was placed in the lateral decubitus position, and the Moore approach adopted. A technique of double‐strut bone graft described previously was utilized: after exposure of the femoral head, a fenestration, 14 mm × 14 mm in size, was made at the posterior wall of the neck below the head. The necrotic bone was thoroughly removed, and then bone grafting performed. First, some marrow pieces were crushed and pressed under the cartilage of the femoral head, and then match‐sized iliac strips were planted around the periphery inside the femoral head. The double‐strut bone graft, consisting of one iliac bone strut, 10 mm × 10 mm × (25–35) mm, and another bone strut pedicle with femoral quadratus, 14 mm × 14 mm × (30–50) mm, was finally implanted in the big passage at the center of the head. The double‐strut bone graft was propped up and supported under cartilage at the proximal side, inserted into the fenestration and blocked by itself at the distal side 2 . For the first three weeks after surgery, the patient was subjected to bed rest in a supine position, and the operated leg was restricted in an abduction position, then the patient was allowed to sit and exercise in bed. Timing of weight‐bearing ambulation was determined by the integration status of the bone graft within the femoral head.
Follow‐up and outcome evaluation
During the first six months after surgery, the patients were assessed every month, every two months in the second six months, every three months in the next twelve months, and every six months thereafter. Patients were then followed up yearly until five years after the surgery. If patients complained of any discomfort, an additional assessment was always performed.
During the first postoperative year, the patients were required to visit the clinic, when they were interviewed, or responded to a questionnaire. Clinical and radiographic evaluations were performed at each follow‐up.
A 100‐point rating score system, consisting of a 60‐point clinical part and a 40‐point radiographic part, was used. The clinical part includes 25 points for pain, 18 points for function, and 17 points for range of motion (ROM) of the joint. The outcome was rated as excellent (≥90 points), good (75–89 points), fair (60–74 points), and poor (<60 points).
Statistical analysis
Data were analyzed with SPSS 11.0 (SPSS, Chiago, IL, USA). The Student's t‐test was performed for paired data and the χ2 test for inter‐stage comparison. The level of significance was set at P < 0.05, except for inter‐stage comparisons for which it was set at 0.003.
Results
Hip pain disappeared or alleviated greatly after the operation in all patients. The height of the femoral head improved to various extents. For the collapsed femoral heads of stage IIIC and IV, the postoperative height increased slightly or not at all, however, the ROM of the hip joints improved. The clinical outcomes remained satisfactory by two years after operation, with excellent and good rates of 95.2%. Five years after surgery, surgical outcomes worsened in a few patients. Thereafter, all patients experienced some deterioration, which varied according to stage. The most significant decrease was observed in stages IIIC and IV; followed by stages IIIA and IIIB; and the results in stages IIB and IIC remained the best with the least deterioration (Fig. 1).
Figure 1.
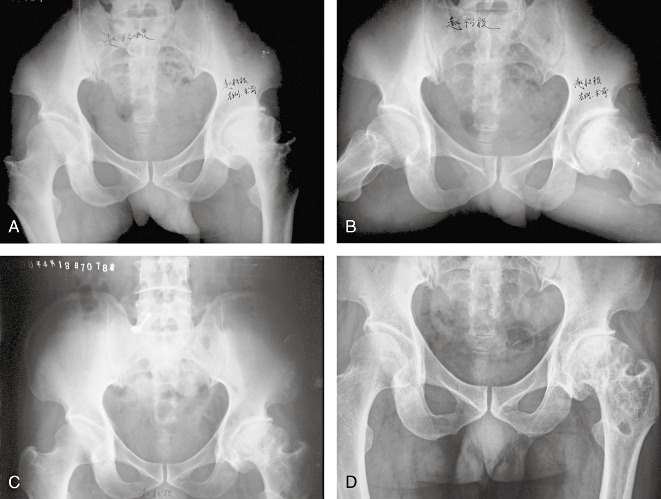
A 44‐year‐old male patient suffered from traumatic osteonecrosis of left femoral head (ARCO, stage III‐C) as shown: (a) and (b) preoperative X‐rays; (c) 5 years after operation; (d) 11 years after operation, showing maintenance of the height of the femoral head.
Outcome evaluation (1, 2, 3)
Table 1.
Clinical score comparison between pre‐operation and follow‐up
| Stage | Hips | Pain | Function | ROM | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre‐operation | Follow‐up | t value | Pre‐operation | Follow‐up | t value | Pre‐operation | Follow‐up | t value | ||
| IIB | 36 | 9.86 ± 4.55 | 24.17 ± 1.89 | 17.34 | 11.23 ± 2.76 | 15.50 ± 1.65 | 7.57 | 10.25 ± 1.36 | 14.69 ± 1.31 | 14.72 |
| IIC | 30 | 7.00 ± 5.19 | 22.33 ± 2.86 | 13.66 | 9.63 ± 1.84 | 15.07 ± 2.16 | 11.65 | 9.03 ± 0.85 | 14.07 ± 1.26 | 19.67 |
| IIIA | 40 | 6.75 ± 5.13 | 21.63 ± 3.08 | 15.85 | 8.38 ± 1.55 | 14.40 ± 2.34 | 14.67 | 8.78 ± 0.86 | 14.10 ± 1.06 | 25.36 |
| IIIB | 40 | 6.63 ± 4.99 | 21.13 ± 3.30 | 13.73 | 7.98 ± 1.23 | 12.35 ± 1.98 | 11.51 | 8.65 ± 1.00 | 13.35 ± 1.58 | 19.11 |
| IIIC | 32 | 6.56 ± 4.82 | 20.00 ± 3.59 | 12.64 | 7.53 ± 1.16 | 11.63 ± 2.42 | 8.17 | 8.28 ± 0.68 | 12.15 ± 1.39 | 12.62 |
| IV | 28 | 5.18 ± 5.35 | 19.11 ± 3.86 | 10.97 | 6.21 ± 1.20 | 10.89 ± 2.53 | 8.63 | 7.50 ± 1.23 | 10.86 ± 2.01 | 7.79 |
Data expressed as mean ± SD. The differences in scores of each index between pre and post operation were compared by t test by stage and were statistically significant (P < 0.01). ROM, range of movement.
Table 2.
Radiographic and overall points between pre‐operation and follow‐up
| Stage | Hips | Radiographs | Total points | ||||
|---|---|---|---|---|---|---|---|
| Pre‐operation | Follow‐up | t value | Pre‐operation | Follow‐up | t value | ||
| IIB | 36 | 30 | 34.31 ± 4.95 | 5.22 | 61.39 ± 4.98 | 88.67 ± 6.39 | 18.01 |
| IIC | 30 | 30 | 32.17 ± 3.39 | 3.50 | 55.67 ± 5.94 | 83.63 ± 4.69 | 20.44 |
| IIIA | 40 | 20 | 30.75 ± 2.13 | 31.87 | 43.90 ± 5.36 | 80.88 ± 3.92 | 35.68 |
| IIIB | 40 | 20 | 27.63 ± 3.39 | 14.21 | 43.25 ± 4.95 | 74.45 ± 5.92 | 24.07 |
| IIIC | 32 | 20 | 24.22 ± 4.60 | 5.19 | 42.06 ± 6.03 | 68.00 ± 6.09 | 18.80 |
| IV | 28 | 10 | 16.96 ± 8.64 | 4.26 | 28.89 ± 4.73 | 57.82 ± 13.14 | 10.59 |
Data expressed as mean ± SD. The differences in scores of each index between pre and post operation were compared by t test by stage and were statistically significant (P < 0.01).
Table 3.
Long‐term follow up results (hips)
| Stage | Hips | Excellent | Good | Fair | Poor | Excellent/Good rate (%) |
|---|---|---|---|---|---|---|
| IIB | 36 | 16 | 14 | 3 | 3 | 83.3 |
| IIC | 30 | 12 | 12 | 3 | 3 | 80.0 |
| IIIA | 40 | 11 | 19 | 7 | 3 | 75.0 |
| IIIB | 40 | 9 | 17 | 8 | 6 | 65.0 |
| IIIC | 32 | 2 | 11 | 9 | 10 | 40.6 |
| IV | 28 | 1 | 7 | 8 | 12 | 28.6 |
| Total | 206 | 51 | 80 | 38 | 37 | 63.6 |
Statistical difference was treated by analysis of variance, χ2 = 33.954, P = 0.0001.
Clinical evaluation (occupying 60% of the 100‐point scoring system) 3
Pain (25 points). Two years post surgery, no recurrence of pain was noted. By the fifth postoperative year, most patients with stage IIB to IIIB lesions (132/146 hips, 90.4% of the total) still suffered no pain. However, mild pain occurred in one third of the patients with stage IIIC and IV lesions. During the period from 5 to 16 years after surgery, pain recurred in 6 of the 66 (9.1%) stage IIB and IIC patients, in 10 of the 80 (12.5%) stage IIIA and IIIB patients, and in 15 of the 60 (25%) stage IIIC and IV patients, respectively.
Function (18 points). During the first two postoperative years, functional outcomes were significantly improved with slight or no limping and unlimited walking. By the fifth postoperative year, most patients with stage IIB to IIIB (132/146 hips, 90.4%) had achieved unlimited walking without limping, while some patients endured slight limping. One third of the patients with stage IIIC and IV limped slightly, but could walk more than 1000 m without a walking aid. During the period from 5 to 16 years after surgery, slight limping recurred in 12 of the 66 (18.2%) patients with stage IIB and IIC and in 18 of the 80 (22.5%) patients with stage IIIA and IIIB. Furthermore, 30% of the patients with stage IIIC and IV suffered from moderate to severe limping with severely abnormal gait and walking distance less than 500 m or limited to indoor ambulation, and required a walking cane or single crutch.
ROM (17 points). During the first two postoperative years, ROM was improved in all patients, however, the ‘4’ test (sitting with legs crossed) was positive. By the fifth postoperative year, patients with stage IIA and IIB attained a ROM of minimal flexion of 90°, abduction of 15 to 30°, and internal and external rotation of 5 to 15° or more. Patients with IIIA and IIIB also attained a ROM of more than 60° of flexion, 15° of abduction and 5° of rotation. Nevertheless, most patients with stage IIIC and IV had a limited abduction of less than 15°. During the period from 5 to 16 years after surgery, a slight decrease in ROM was found in patients with stage IIB to IIIB; and severe limitation of ROM happened in 30% of the patients with stage IIIC and IV, who had difficulties with abduction and external rotation.
Radiographic evaluation (40 points).
Stage IIB and IIC were referred to as stage II, and stage IIIA, IIIB and IIIC as stage III. If one stage increment (deterioration) in radiography was noted postoperatively, 10 points were subtracted on postoperative assessment. If one stage decrement (improvement) was noted, 10 points were added. At the second year after surgery, the immediate postoperative increase in femoral head height was maintained with a good concentric relationship with the acetabulum. By the fifth postoperative year, most femoral heads in stage IIB and IIC showed good bone quality with femoral head height maintained; 20% of femoral heads in stage IIIA and IIIB showed decrease in femoral head height; moreover, one third of the femoral heads in stage IIIC and IV experienced recurrent collapse with significant decrease in height. During the period from 5 to 16 years after surgery, collapse of the femoral head recurred in 12 of the 66 (18.2%) patients with stage IIB and IIC, in 24 of the 80 (30%) patients with stage IIIA and IIIB, in 19 of the 32 (59.4%) patients with stage IIIC, and in 20 of the 28 (71.4%) patients with stage IV.
A total of 186 patients with 206 hips were followed up for more than 5 years (average 10.5 years ranging from 5 to 16 years). In summary, the rate of excellent and good results was 83.3% in stage IIB, 80.0% in stage IIC, 75.0% in stage IIIA, 65.0% in stage IIIB, 40.6% in stage IIIC and 28.6% in stage IV, respectively (Table 3). The overall rate for excellent and good results was 63.6%, and there was a statistically significant difference among the different stages (χ2 = 33.954,P < 0.0001). The excellent and good rate for stage IIB, IIC and IIIA was statistically different from stage IIIC and IV. The values of χ2 and P for each stage were IIB (χ2 = 13.292, P = 0.0001; χ2 = 19.521, P = 0.0001), IIC (χ2 = 9.976, P = 0.002; χ2 = 15.488, P = 0.0001), IIIA (χ2 = 8.733, P = 0.003; χ2 = 14.401, P = 0.0001). Statistical difference between stage IIIB and IV was also found (χ2 = 8.74, P = 0.003), but no statistical difference between stage IIIC and IV was found (χ2 = 0.954, P = 0.329).
Condition of bone graft fusion
The current study showed that the bone grafts healed quickly in patients aged less than 30 years, taking a mean time of 3.2 months (range, 2.9–3.5 months). For patients between 30 and 49 years the average bone graft fusion time was 3.8 months (range, 3.4–4.1 months) and for the 40–49 year age group 4.5 months (range, 3.9–5.1 months). A longer time was needed for bone graft fusion in patients between 50 and 60 years, in whom the mean time was 5.5 months (range, 4.4–6.4 months).
Discussion
Treatment of ONFH
Treatment of ONFH should be individualized based on the patient's age, size and site of necrosis, and risk of collapse 4 . Optimal outcome can only be achieved by a good understanding of treatment principles, and choosing proper treatment methods for each stage. The treatment principles of ARCO are as follows: (i) stages 0 to IIA should be treated by core decompression; (ii) for stages IIB to IIIB osteotomy or bone grafting is indicated; and (iii) in stage IIIC or more, advanced artificial hip joint replacement should be considered 5 .
ONFH frequently occurs in young people, so head‐preserving options should be considered first. Ueo et al. analyzed mechanical changes in the necrotic femoral head using a finite element model, and found that stress concentration around the necrotic bone would lead to fracture inside the head 6 . Stress concentration not only affects the local biomechanics, but also prevents repair of necrotic tissue. Femoral head collapse, which results in malfunction of the hip joint, occurs during the repair stage of necrosis. Therefore, how to maintain the mechanically supporting force of the subchondral bone in the weight‐bearing area becomes one of the key questions in preventiion and repair of femoral head collapse during the repair stage of necrosis. Many nonvascularized and vascularized bone‐grafting techniques have been applied 2 , 3 , 7 , 8 , 9 , 10 .
All bone grafting techniques have two characteristics: one is that osteogenic factors, which the graft bone carries, as well as the rich blood supply, can promote fusion of the graft bone; the other is that the strength provided by the bone graft increases the local mechanical strength inside the femoral head and prevents its collapse. Vascularized or free fibular graft provides excellent supporting strength 7 , 8 , however, fibular autografts are unsatisfactory because they require an additional incision. In addition, fibular grafts must be fixed with screws, and vascular anastomosis as a difficult and demanding technique after which vascular contraction may occur 8 , 10 . So, an alternative is to obtain a vascularized bone graft from near the femoral head (e.g. from the ilium or trochanter).
The double‐strut bone grafting technique with a posterior approach allows complete removal of the necrotic bone resulting in complete decompression. Moreover, the massive bone graft carries plenty of osteogenic factors and a rich blood supply, which accelerate the fusion process. With its powerful supporting strength, a double‐strut bone graft can restore the height and natural biomechanics of the head and prevent its collapse. It has been shown in animal experiments that the postoperative natural mechanics of the femoral head can revert to normal. Also, because this technique does not damage the normal structure of the femoral neck and head, another treatment can be chosen if it fails 2 .
Long‐term outcome of double‐strut bone graft
In recent years, it has been reported that there is a close correlation between the prognosis of ONFH and the degree of necrosis 11 . There are many methods to identify the extent of necrosis in ONFH. For example, it can be calculated by measuring the angle, or be assessed by radiograph, quantitative computed tomography and magnetic resonance imaging (MRI) 12 , 13 . Lafforgue et al. calculated the angle formed by the lines from the center of the femoral head to the two margins of the necrotic segment in the coronal plane on MRI, and considered that an angle of more than 75° indicated a poor prognosis, but an angle of less than 45° was associated with a better outcome 13 . Beltran et al. classified the size of the necrotic area as measured on MRI as stage A (no necrosis), B (<25%), C (25‐50%) and D (>50%) 14 . They found that the outcome of core decompression became worse with increasing stage.
The important aspects of the ARCO classification are extent of the necrotic area and of collapse. A better long‐term outcome was shown in our study, which did not include patients with stage I and IIA lesions. The rate of excellent and good results was 83.3% in stage IIB, 80.0% in stage IIC, 75.0% in stage IIIA, 65.0% in stage IIIB, 40.6% in stage IIIC and 28.6% in stage IV, respectively. On the whole, we can conclude that stage II lesions had an excellent outcome (81.8%), and early stage III (stage IIIA and IIIB) an adequate one (70%). However, stage IIIC and IV showed poor results (35%) due to the large necrotic area and severity of collapse. As time went by postoperatively, the clinical outcome became worse for all stages. The current study shows that the long‐term outcome of double‐strut bone grafting is related to necrotic extent, presence of collapse and degree of ONFH. That is to say, the prognosis of ONFH is related to the stage of ARCO and the time since surgery. This is consistent with results reported by other authors.
Wang et al. reported a series of 683 hips with ONFH treated by vascularized fibular bone graft, which showed that excellent and good rates for stages I, II, III, and IV were 100.0%, 96.2%, 34.2% and 10.0% respectively, with an average 6 year follow‐up (range, 1–19 years) 7 . The excellent and good rate was 86.7% for the whole group, with stages III and IV combined being 25.5%. In a review of 60 ONFH cases (68 hips) treated by vascularized free fibular bone graft with a mean 18 years (range, 15–22 years) of follow‐up, Judet and Gilbert reported a total excellent and good rate of 52%, with stages II and III being 52% 15 . Thus, it has been shown that the effectiveness of vascularized fibular bone grafting is related to the stage of ONFH. Therefore, this bone‐grafting technique is especially indicated for patients with stage II and early stage III ONFH. It can avoid or delay the need for artificial hip replacement significantly, and is especially indicated for the young patients 2 , 7 .
Poor long‐term clinical outcome in advanced stages of ONFH
Non‐traumatic osteonecrosis is a systemic disease, of which ONFH is a local manifestation. Once necrotic bone has formed, it is difficult to prevent progression of ONFH. So far, preservation of the head has been the basic treatment principle. However, all current bone‐grafting techniques have their pros and cons. A good clinical outcome can be obtained in the early to mid follow‐up period, but the results deteriorate on long‐term follow‐up. The earlier the stage, the better the outcome is. Long‐term follow up shows that poor results are found mostly in stages IIIC and IV. In our early report of 27 hips with stage III and IV ONFH patients, the excellent and good rate was 96.3% by an average of 3.2 years follow up (range, 2–7 years) 2 . In this study, with a mean of 10.5 years (range, 5–16 years) follow up, the excellent and good rate was 55% (77/140) for stage III and IV lesions. The reasons we have considered for these poor outcomes are as follows: (i) the staging according to ARCO: in ARCO stage IIIC cases, the necrotic area or crescent sign can involve far more than 30% of the total head and reach 80% or more. Moreover, femoral head collapse can reach 10 mm or more and develop a conical shape. Although no such classification has been reported, such cases should be separately classified as a ‘severe type of stage IIIC’ in our opinion. The degeneration of the head cartilage and deformation of head profile that is observed in these cases means that satisfactory results can not be achieved by any head‐preserving method 7 ; (ii) increasing amount of daily activities after recovery; (iii) in some cases' recurrence is associated with the reappearance of inducing factors: for example, patients with alcohol‐induced ONFH resume drinking heavily; or patients with steroid‐related ONFH have to use steroids again because of illness. Undoubtedly, alcohol and steroids affect the quality and quantity of bone; and (iv) age is a important factor. Generally, patients over 50 years of age take more than five months to heal. Furthermore, osteoporosis could be a factor in making bone weak. Therefore, for patients with the same stage of ONFH, the elderly have a poorer postoperative result. Judet and Gilbert have pointed out that, in their reported series, better results (80%) were achieved in patients aged under 40 years 15 . Therefore, we can draw the conclusion that for patients over 55 years of age with stage IIIC or more, artificial hip replacement should be recommended 16 .
References
- 1. Li Z. Establishment of osteonecrosis and joint reconstruction center in Sino‐Japan friendship Hospital (Chin). Zhonguo Guzhongliu Gubing, 2004, 3: back cover. [Google Scholar]
- 2. Wang Y, Zhang C, Wang L, et al. Double strut bone grafting for the treatment of advanced femoral head necrosis (Chin). Zhonghua Gu Ke Za Zhi, 1995, 15: 584–587. [Google Scholar]
- 3. Wang Y, Zhu S. The treatment and outcome evaluation methods for adult femoral head necrosis (Chin). Med J Chin People's Liberation Army, 1998, 23: 77–78. [Google Scholar]
- 4. Li Z, Zhang N, Shi Z, et al. Prediction of collapse and selection of head‐preserving methods for the osteonecrosis of femoral head (Chin). Zhonghua Gu Ke Za Zhi, 2003, 23: 193–196. [Google Scholar]
- 5. Cui Q, Wang Y. Femoral head necrosis In: Luo X, Qiu G, eds. Artificial Hip Joint, 1st edn. Peking: Peking Union Medical College Publication, 2003; 275–279. [Google Scholar]
- 6. Ueo T, Tsutsumi S, Yamamuro T, et al. Biomechanical aspects of the development of aseptic necrosis of the femoral head. Arch Orthop Trauma Surg, 1985, 104: 145–149. [DOI] [PubMed] [Google Scholar]
- 7. Wang K, Tong Z, Wang C, et al. Free vascularized fibular bone grafting for the treatment of femoral head necrosis (Chin). Zhonghua Xian Wei Wai Ke Za Zhi, 2000, 23: 254–256. [Google Scholar]
- 8. Urbaniak JR, Coogan PG, Gunneson EH, et al. Treatment of the femoral head with free vascularized fibula grafting. J Bone Joint Surg Am, 1995, 77: 681–694. [DOI] [PubMed] [Google Scholar]
- 9. Eisenschenk A, Lautenbach M, Schwetlick G, et al. Treatment of femoral head necrosis with vascularized iliac crest transplants. Clin Orthop Relat Res, 2001, 386: 100–105. [DOI] [PubMed] [Google Scholar]
- 10. Berend KR, Gunneson EE, Urbaniak JR. Free vascularized fibular grafting for the treatment of postcollapse osteonecrosis of the femoral head. J Bone Joint Surg Am, 2003, 85: 987–993. [DOI] [PubMed] [Google Scholar]
- 11. Liu H, Wang Y, Han S, et al. Biomechanical study of double strut bone grafting for the treatment of femoral head necrosis (Chin). J Tradit Chin Orthop Tramatol, 2004, 16: 3–5. [Google Scholar]
- 12. Steinberg ME, Bands RE, Parry S, et al. Does lesion size affect the outcome in avascular necrosis? Clin Orthop Relat Res, 1999, 367: 262–271. [PubMed] [Google Scholar]
- 13. Lafforgue P, Dahan E, Chagnaud C, et al. Early‐stage avascular necrosis of the femoral head: MR imaging for prognosis in 31 cases with at least 2 years of follow‐up. Radiology, 1993, 187: 199–204. [DOI] [PubMed] [Google Scholar]
- 14. Beltran J, Knight CT, Zuelzer WA, et al. Core decompression for avascular necrosis of the femoral head: correlation between long‐term results and preoperative MR staging. Radiology, 1990, 175: 533–536. [DOI] [PubMed] [Google Scholar]
- 15. Judet H, Gilbert A. Long‐term results of free vascularized fibular grafting for femoral head necrosis. Clin Orthop Relat Res, 2001, 386: 114–119. [DOI] [PubMed] [Google Scholar]
- 16. Mont MA, Jones LC, Hungerford DS. Nontraumatic osteonecrosis of the femoral head: ten years later. J Bone Joint Surg Am, 2006, 88: 1117–1132. [DOI] [PubMed] [Google Scholar]


