Short abstract
The preconceptional presence of microbiota in the female and male reproductive organs suggests that fertilization is taking place in a nonsterile environment and contributes to reproductive success. The concept of embryonic development in a sterile uterus has also been challenged with recent reports of the existence of a microbiome of the placenta, amniotic fluid and the fetal gut in normal, uncomplicated pregnancies. The maternal origins of the microbiota colonising the fetus and its surroundings are unknown as are the mechanisms of maternal-to-fetal transfer. In this review, we aim to highlight the preconception male and female microbiome, the maternal vaginal and gut microbiome during pregnancy and the fetal microbiome, including their possible roles in reproduction, and maternal and neonatal pregnancy outcome.
Keywords: Microbiome, maternal–fetal medicine, embryo, placenta, pregnancy, periconception
Introduction
The presence of microbes during pregnancy has for decades been associated with inflammation, disease and adverse pregnancy outcomes, such as preterm birth.1 However, this was under the long prevailing assumption that the human body, including the uterus and placenta were sterile sites. Recent evidence, however, demonstrates a unique set of microbiota in the vagina,2 uterine cavity3 and placenta4 in healthy pregnant women, which challenges this old adage that the embryo and fetus develop in a sterile environment.
The microbiota of the human body include bacteria, viruses, fungi, yeast and archaea. The term microbiome refers to the total genomic content of these microorganisms, but has nowadays become interchangeable with the term microbiota. Most of the microbiome research has focussed on the human gastro-intestinal tract hosting most of the microbiota across the body sites.5 It is known that the local gut microbiome is involved in the digestion of foods, synthesis of vitamins, host metabolism, defense against pathogens, and immune responses, such as suppressing inflammatory responses and promoting immunological tolerance via the innate immune system.6,7 The host-microbiome relationship can be beneficial, symbiotic and well-balanced, whereas a disruption in the local balance or composition of the microbiome can result in an unhealthy state of dysbiosis, which is among others associated with inflammation and disease (reviewed in Knight et al.8).
The Human Microbiome Project2,9 revealed the presence of a microbiome in different human anatomical niches, such as gut, oral cavity, skin and vagina. Besides a diversity in the residing commensal microbes (alpha-diversity) at each site within each individual, there is also a difference between individuals in diversity in the microbial composition at each site (beta-diversity).2 These differences are influenced by diet (Table 1), host genetics, body mass, early microbial exposure and antibiotics (reviewed in Turnbaugh et al.8). For a few years, it has been known that also the endometrium,3 placenta,4 amniotic fluid,10 seminal fluid11 and fetal gut12 have their own diverse and unique set of microbiota.
Table 1.
Exposures or conditions that affect the human maternal microbiome during the preconception period and pregnancy.
| Exposure/condition | Timing | Affected microbiome |
|---|---|---|
| Maternal diet19,94 | Preconception | Gut |
| Antibiotics95 | Preconception | Gut |
| BMI42,86,96,97 | Preconception | Gut, meconium (vaginal delivery) |
| Overweight / obesity96,98,99 | Preconception | Gut |
| Diabetes mellitus100 | Preconception | Meconium |
| Pregnancy34,35,37,40,41 | Pregnancy | Gut, vagina |
| Maternal diet19,101 | Pregnancy | Gut, placenta, meconium |
| Probiotics101,102 | Pregnancy | Placenta, meconium, Vagina |
| Overweight/obesity42,45,46 | Pregnancy | Gut |
| Gestational diabetes100,103 | Gut, placenta, meconium | |
| Gestational weight gain19,42,45,96 | Pregnancy | Gut, placenta |
| Chorioamnionitis4,66,104 | Pregnancy | Placenta, amniotic fluid |
The amount of biomass (the number of microbiota of a tissue or a sample) is a continuous matter of controversy and debate. It is almost impossible to prevent contamination of a sample with DNA present in the air13 or laboratory reagents.14,15 Because of the high number of microbiota of various microbiome niches, the impact of contamination will be limited. However, in samples with a low biomass, such as seminal fluid,11 placenta,4 amniotic fluid10,16 and meconium,17 the possibility exists that the contaminating DNA will dominate the result of the microbiome analysis.15 The challenge in interpreting microbiome research data is to approach contradicting results with this in mind.
In the present review, we aim to give an overview of the literature about the preconceptional and pregnancy microbiome at different sites and its impact on reproduction, fetal development and pregnancy outcome, with a focus on bacteria.
Preconception
The preconception period is important for pregnancy outcome, since preconception conditions (Table 1), such as diet and lifestyles have significant impact on reproductive success (reviewed in Steegers-Theunissen et al.18) and influence the composition of the gut microbiome during pregnancy.19 Also, at the core of successful conception and subsequent pregnancy lies the preconception maturation of female and male gametes. Therefore, it could be assumed that the microbiome during the preconception period contributes to pregnancy outcome. Herewith in line are the recent reports showing that the microbiome of the follicular fluid20,21 and endometrium are associated with implantation success.22 In the next paragraphs, we describe the preconceptional microbiome of follicular fluid, semen, uterus and vagina.
Microbiome of follicular fluid
Oocyte maturation occurs within the environment of the follicular fluid of the developing follicle. Pelzer et al.20,21 showed that the human follicular fluid in women undergoing IVF cycles is not sterile, but colonized with microbiota. To discriminate between procedure-related contamination and in vivo colonisation, the follicular fluids were classified as either contaminated when the detected microbiota in follicular fluid were also detectable in the vagina during transvaginal oocyte retrieval and colonized when the microbiota were only present within the follicular fluid. The most prevalent microbiota detected in colonized follicular fluids were Lactobacillus spp. (L. crispatus, L. gasseri, Actinomyces spp. and Propionibacterium spp.). It has been suggested that the follicular fluid microbiome influences the outcome of IVF treatment, since the presence of Lactobacillus spp. is associated with better embryo quality leading to significantly higher rates of embryo transfer and pregnancy.21 The antimicrobial properties of lactic acid, the major acid metabolite produced by Lactobacillus spp., can protect against adverse microbiota during oocyte maturation.23 Interestingly, the follicular fluid of the left compared to the right ovary contains significantly more microbiota, perhaps due to the asymmetrical vascularisation of the gonads,21 pointing towards distribution of microbiota via the blood stream.
Microbiome of semen
Up until now, the microbiome of the interieur milieus during spermatogenesis, such as that of the testis or epididymis, have not been reported. However, the microbiome of the ejaculate has been analysed and most likely represents the presence of microbiota from all contributing sites of the male reproductive tract, including epididymis, seminal vesicles, prostate, bulbourethral glands and urethra. It revealed that semen contains the strictly anaerobic Prevotella and high proportions of facultative anaerobic bacteria of which the most abundant bacteria are Lactobacillus, Pseudomonas, Gardnerella, Finegoldia, Corynebacterium and Staphylococcus.11,24 Based on the microbiome composition of the semen samples analysed so far, different seminal types can be identified, dominated by either Lactobacillus, Pseudomonas or Prevotella.11,24 However, it is still unknown whether the microbiome of semen is associated with male fertility or semen quality, although Weng et al.24 found a positive association of a Lactobacillus dominated microbiome with semen quality. The latter could be explained by the high levels of lactic acid synthetized by Lactobaccilus, which could protect against the negative influence of Gram-negative bacteria during spermatogenesis.23,24
The seminal microbiome has a lower biomass, but a higher diversity of the microbiome compared to the vaginal microbiome (see below) and induces a significant change in the vaginal microbiome after intercourse.25 As the seminal fluid and its microbiome get into contact with the endometrial fluid, a similar change in the endometrial microbiome could also occur. Hypothetically, an endometrial microbiome change and mixing of the endometrial and seminal fluid can influence the maternal–embryonic interaction during implantation and placentation. Supportive of this hypothesis, are experiments in rodent models that show an essential role for seminal fluid in enabling successful embryo implantation and optimal placental development (reviewed in Robertson and Sharkey26).
The uterine/endometrial microbiome
Verstraelen et al.3 showed in a group of women (n = 19) with a variety of reproductive conditions by endometrial biopsies that the uterine microbiome mainly seems to consist of three bacterial phyla, in particular Proteobacteria, Firmicutes and Bacteroidetes, with Bacteroidetes being the most dominant phylum in the majority of the women included.3 Importantly, species diversity and richness of the endometrium were significantly higher than that in the adjacent vaginal compartiment (see below). The endometrium is suggested to be colonized with both vaginal and gut microbiota, since microbiota associated with the gastrointestinal tract, such as Bacteroidetes (Bacteroidetes xylanisolvens, Bacteroidetes thetaiotaomicron, Bacteroidetes fragilis) and Proteobacteria, as well as microbiota associated with the vaginal microbiome, such as Lactobacillus iners, L. crispatus and Prevotella amnii, were all identified in the endometrial samples.3
A different microbiome was found in endometrial fluid aspirates, with the most abundant genera being Lactobacillus, Gardnerella, Bifidobacterium, Streptococcus and Prevotella.22 Importantly, a Lactobacillus-dominated microbiome of the aspirates was associated with higher chance of live birth, whereas the presence of other bacteria, especially for Gardnerella or Streptococcus genera, seemed to be correlated with implantation failure or early pregnancy loss.22
Microbiome of vagina
The non-gravid vaginal microbiome is complex and in most women dominated by four Lactobacillus spp., i.e. L. crispatus, L. iners, L. jensenii or L. gasseri.27–29 Some women show a vaginal microbiome less dominated by Lactobacillus spp. and have more strict anaerobes.27–29 Ethnicity is of influence on the vaginal microbiome, since several studies showed that healthy, non-pregnant women from European descent have a Lactobacillus-dominated vaginal microbiome, whereas healthy non-pregnant African-American and Hispanic women have a non-Lactobacillus-dominated microbiome.28–30 In addition, the vaginal microbiome is dynamic and seems to be affected by the menstrual cycle, the dominant microbiota and sexual activity.27
The diversity of the non-pregnant vaginal microflora may be important for pregnancy outcome, since at the time of embryo transfer, the vaginal microflora seems to be an important factor in the success of the IVF-embryo transfer procedure: A vaginal microbiome composed solely of Lactobacillus (L. crispatus, L. iners, L. jensenii, L. gasseri or other Lactobacillus species) at the moment of menses before embryo transfer is associated with a successful outcome of the IVF-ET procedure.31
In summary, recent research has repeatedly demonstrated the existence of a microbiome in the male and female reproductive organs and changed the perception of sterile fertilization. The increasing evidence that the presence of microbiota in the female reproductive tract plays a role during the process of implantation, indicates that residing microbiota of the male and female reproductive tract around the conception could influence, both beneficially or detrimentally, local immune responses and direct the process of embryo implantation and subsequent placental development and function.
Pregnancy
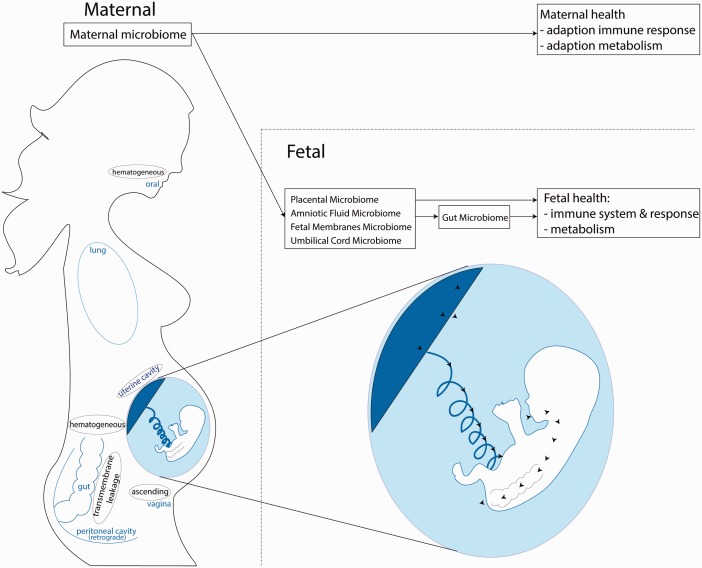
Around fertilization and during pregnancy, the maternal body undergoes a series of physiological adaptions to prepare for support, protect and nurture the embryo and fetus.32,33 Besides anatomical, biochemical and immunological adaptions, the residing microbiome in the maternal body undergoes changes in parallel (Table 1). We are only beginning to understand which roles the maternal and paternal microbiota are playing during pregnancy. In line with the current knowledge about the interactive roles of the gut microbiome, not only dysbiosis in the gut, but also dysbiosis in the endometrium, vagina and placenta during pregnancy, could potentially lead to inflammation or disease. These changes may increase risk of adverse pregnancy outcomes, such as miscarriage and preterm birth. In the next paragraphs, we describe the pregnancy microbiome at different locations (Figure 1).
Figure 1.
Overview of the maternal and fetal microbiome during pregnancy, health effects and maternal–fetal microbiome axes.
Maternal microbiome
Microbiome of the vagina
After implantation, the dynamics and stability of the vaginal microbial community change during the course of pregnancy (Tables 1 and 2). During the first trimester, a dominance of genus Lactobacillus in the vaginal microbiome of Caucasian women is observed.34–37
Table 2.
Dynamics of local microbiomes preconceptionally and during pregnancy.
| Location | Timing | Dynamics | |
|---|---|---|---|
| Maternal-preconception | |||
| Ovary20,21 | Preconception | Unknown | |
| Uterine/endometrium22 | Preconception | Stable | |
| Vagina27,34,40 | Preconception | Highly dynamic | |
| Gut2,41,42 | Preconception | Stable – diet dependent | |
| Maternal-pregnancy | |||
| Vagina34,39,40 | Pregnancy | Increased stability with each trimester | |
| Gut41,42 | Pregnancy | Dynamic – trimester dependent, increase microbial load | |
| Oral105 | Pregnancy | Dynamic – trimester dependent, increase microbial load | |
| Fetal | |||
| Placenta4 | Pregnancy | Unknown | |
| Amniotic fluid10 | Pregnancy | Unknown | |
| Fetal membrane10 | Pregnancy | Unknown | |
| Umbilical cord64 | Pregnancy | Unknown | |
As pregnancy progresses beyond the first trimester, lesser diversity and richness combined with an increased stability are seen.34–39 Also, various species of Lactobacillus, such as L. iners, L. crispatus, L. jensenii and L. johnsonii, are enriched in pregnancy.34 With continuation of pregnancy, in some women, a shift from one Lactobacillus-dominated to another Lactobacillus-dominated composition occurs,40 whereas in other women, a specific increase in Lactobacillus is accompanied by a decrease in anaerobic microbiota.37 While the vaginal microbiome varies during the course of pregnancy, around term, the vaginal microbiome seems to return to a non-pregnant composition.34
Women with a relatively stable vaginal microbiome throughout pregnancy, in terms of richness and diversity, seem to deliver more often at term, whereas women with a decrease of richness and diversity of the vaginal microbiome early in pregnancy seem to be at risk of preterm birth.35,36,39 So far there are no indications that the composition of the vaginal microbiome before pregnancy predicts the dynamics during pregnancy and pregnancy outcome.39
Microbiome of the gastrointestinal tract
During the first trimester of pregnancy, the maternal gut microbiome is comparable to the microbiome in the preconceptional period.41 However, with progression of the pregnancy, the total number of microbiota increases (Table 1), paralleled by an overall increase in Proteobacteria and Actinobacteria.41,42 It has also been shown that levels of Faecalibacterium are decreased during the third trimester of pregnancy.41 Whereas within the gut of individual women the general diversity and richness decrease (alpha diversity), between women the diversity increases (beta diversity).41 Another study, however, showed no changes in the gut microbiota during pregnancy or upon delivery,35 indicating that more research is needed into the maternal microbiome during pregnancy.
Animal research showed that germ-free mice transplanted with third trimester stool microbiota of pregnant women as compared to germ-free animals treated with first trimester stool microbiota of pregnant women had reduced glucose tolerance and more weight gain.41 These effects suggest that the maternal gut microbiome has an active role in the metabolic changes observed during pregnancy. In view of the effect of the gut microbiota on immune responses,6,7 changes in the maternal gut microbiota during pregnancy could also have an impact on the maternal immune system. Adaptations of the maternal immune response during pregnancy are necessary to accept and prevent rejection of the semi-allogenic fetal tissues, while simultaneously maintaining its defence mechanism against microbes to ensure maternal and fetal survival during the same period (reviewed in Mor et al.43).
Also during pregnancy,44 the maternal gut microbiome is strongly influenced by dietary patterns.19 A recent study showed that the maternal diet in mice during the periconception period and during pregnancy led to significant changes in the gut microbiome and metabolic pathways throughout pregnancy. In addition, obesity during pregnancy is associated with a different maternal gut microbiome composition (Table 1),42,45,46 characterized by increased Bacteriodes and Staphylococcus.42
Changes in the gut microbial composition between the first and third trimester are suggested to be involved in supporting the changing metabolic and immunological needs of the maternal body. However, there are indications that microbiota are also important for fetal growth and development, since as described below, transfer of microbiota from the mother to the fetus takes place.
Embryonic and fetal microbiome
After reaching the uterine cavity, the blastocyst hatches so that the trophectoderm, the outer extra-embryonic layer, is able to invade the maternal endometrium and reach the local microbiome. The three embryonic cell lines, the epiblast, trophectoderm and hypoblast, will give rise to the different embryonic and extra-embryonic tissues. Epiblast and trophectoderm chorion most likely contribute to the chorion,47 whereas the epiblast will give rise to the embryo proper and the amnion.47 Around 17–20 weeks of gestation, the inner amniotic membrane will fuse with the outer chorion to form the double-layered chorioamniotic membrane.48 In order to form the placenta, cells of the trophectoderm will invade the maternal spiral arties to remodel them. Initially, these cells accumulate in the lumen to form trophoblast plugs49 blocking maternal blood flow to the placenta until the end of the first trimester, when they disintegrate.50
Many pregnancy complications, such as preeclampsia, fetal growth restriction and abruption placentae, but also preterm birth, premature rupture of membranes and late spontaneous abortion are associated with disorders of deep placentation.51 Suboptimal invasion of the endometrium and aberrant spiral artery remodelling will result in placental insufficiency,52,53 which will often lead to (iatrogenic) preterm birth because of fetal distress caused by either inadequate placental attachment and uteroplacental ischemia or premature placental detachment. As such, these pregnancy complications often find their origin during embryonic implantation.52
Implantation is accompanied by an interactive immunological dialogue between local cytokines, chemokines, the maternal immune system and the developing embryo. More recently, Mor et al.43 have hypothesized a role for the local microbiome in this interactive immunological dialogue. Although unknown so far, it is feasible that also the seminal and endometrial microbiome may play a role in the process of implantation and placentation.
In the following paragraph, we will give a summary of the microbiome of the fetus and its environment (Figure 1).
Microbiome of the placenta
Stout et al.54 used high magnification imaging in combination with the use of histologic tissue staining and observed intracellular microorganisms in the basal plates of 27% of both preterm and term placentas. More importantly, the apparent evidence of the presence of microbiota was found without any histological or pathological signs of infection. Parnell et al.55 found significant differences between the microbiome of the basal plate and the placental villi. Proteobacteria, Actinobacteria, Bacteroidetes, Cyanobacteria, Firmicutes, and Spirochaetes were detected in the basal plate, whereas the placental villi harboured Acidobacteria, Actinobacteria, Firmicutes, Proteobacteria, and Spirochaetes. This may be related to different susceptibility of the different spatial compartments of the placenta to infection and specific pathogens.56–59
The combination of 16S rDNA and whole-genome shotgun metagenomic techniques showed that the placenta exhibits its own unique microbiome, with a low abundance but a metabolically rich microbiome. The placental microbiome largely consists of nonpathogenic commensal microbiota from the phyla of Firmicutes, Tenericutes, Proteobacteria, Bacteroidetes, and Fusobacteria4 and mostly resembles that of the oral cavity4 and the deep endometrium of non-pregnant women3 rather that of the adjacent vaginal microbiome.2 This is in contrast to another study which failed to identify a distinct placental microbiome and ascribed the detected bacteria of the placenta samples to bacterial contamination of the environment or the reagents used.60
Although, the presence of commensal, symbiotic placental microbiota seems increasingly valid, the presence of pathological microbes or a potential local dysbiosis can lead to adverse pregnancy outcomes. A different microbiome, as compared with normal pregnancy outcome, has been detected in placentas of pregnancies complicated by preterm birth.61 The microbiota found in the preterm placenta were similar to those commonly residing in the vagina (Prevotella bivia, Lactobacillus spp., Peptostreptococcus magnus, or Gardnerella vaginalis). In placentas of other pregnancy complications such as preeclampsia or fetal growth restriction (FGR), the microbiota Bacillus cereus, Listeria monocytogenes, Salmonella, Escherichia, Klebsiella pneumoniae, Actinobacillus actinomycetemcomitans, Fusobacterium nucleatum ssp., Porphyromonas gingivalis and Prevotella intermedia have been cultured or sequenced.61–63
Since fetal viability, growth and development are completely dependent on optimal placental function, the recent finding of a placental microbiome in healthy pregnancy may implicate a role for the bacteria in normal fetal growth and development.
Microbiome of fetal membranes, umbilical cord and amniotic fluid
Already in 2005, the presence of several different microbial DNA was reported in the amniotic membranes of term healthy pregnancies of women in or outside labour.63 More recently, the composition of the microbiota in the fetal membranes was shown to consist of Actinobacteria, Bacteroidetes, Firmicutes, Proteobacteria, Spirochaetes. Although, most of these microbiota were also detectable in the basal plate and placental villi of the placenta attached, the ratio of the different microbiota and total composition of the microbiome was significantly different between basal plate and placental villi.55
In 2005, Jimenez et al.64 reported the identification of bacteria in umbilical cord blood from term neonates born via elective caesarean section. The microbiota identified were Enterococcus faecium, Propionibacterium acnes, Staphylococcus epidermidis, and Streptococcus sanguinis, which are regarded as commensals in healthy neonates.64
In healthy pregnant women, bacteria were found not only in the placenta and umbilical cord blood, but also in the amniotic fluid. A recent, elegant study comparing the microbiome of different maternal and fetal samples collected during elective term caesarean section showed that the microbiota in amniotic fluid were similar to the placental microbiota.10 The most prevalent phylum, Proteobacteria, showed low abundance, low richness and low diversity, but with high consistency across different individuals. Other phyla detected were Enterobacter, and Escherichia/Shigella, Propionibacterium, Lactobacillus, Streptococcus and Staphylococcus. Importantly, besides microbial DNA, also viable microbiota were detected.10 In addition, in amniotic fluid aspirated from healthy women between a gestational age of 16 until 20 weeks and who delivered at term, Ureaplasma spp. was detected.65
Although the reported bacterial findings seem not to be related to adverse pregnancy outcome, different compositions of the microbiome of the amniotic fluid are associated with chorioamnionitis (Table 1) and could even be used for prediction of preterm birth.66
The developing fetus is not only immersed in amniotic fluid, but the swallowing and exchange of amniotic fluid are indispensable for proper development of the fetal lung and gastrointestinal tract.16,67 Around term, the fetus will swallow around 1000 ml amniotic fluid per day including the microbiota.68 The presence of amniotic bacteria may thus aid in bacterial colonisation of the fetal gut. Indeed, continuous fetal amniotic fluid ingestion could then lead to colonization of the fetal gut69 (see also below).
Microbiome of the fetal gut
In line with the observations that the amniotic fluid contains bacteria, also the meconium as product of the fetal gut is not sterile.10,12,17 The presence of Streptococcus, Enterobacteriaceae, such as Enterobacter and Escherichia, Propionibacterium, Lactobacillus, Bacillales has been reported; however, the dominant microbiota in meconium samples seems to differ between studies.10,17 Although the meconium microbiome has a unique microbial composition, it shows significant resemblance with both the microbiota of the amniotic fluid10,17 and the placenta.10 These data suggest, in contrast to the general belief, that colonization of the gut already occurs during pregnancy.
It thus seems increasingly evident that the fetal compartment, including the placenta and membranes, are not sterile, but colonised during pregnancy. The fetal gut may be colonised via the placenta and amniotic fluid, since the meconium microbiome resembles the microbiome of the placenta and amniotic fluid. The function of the fetal microbiome is unknown; however, considering the effect of the adult microbiome on immune responses and metabolism, it may be speculated that the fetal microbiome is important for maturation of the fetal immune response as well as for optimal setting of the fetal metabolism (Figure 1).
The maternal–fetal microbiota axes
The mechanisms by which microbiota transfer from the mother to the fetus are still unclear. However, it is not unthinkable that the routes for seeding of maternal microbiota to the fetal environment are the same as the suggested potential routes of intrauterine infection (Figure 1).70 Although they could potentially contribute, iatrogenic routes such as chorionic villus sampling, amniocentesis or blunt external trauma, are not plausible as standard.
The systemic blood circulation
The most obvious and effective route would be spreading via the systemic blood circulation. During pregnancy, the cardiac output directed toward the uterine arteries increases from 3.5% at the beginning of pregnancy to 12% around term.71 The combined effect of all maternal pregnancy adaptions leads to an increased uteroplacental blood flow of 20–50 ml/min to 450–800 ml/min at term in singleton pregnancies,72 which may contribute to delivering diverse microorganisms to the fetal–maternal interface.
Direct evidence for a haematogenous maternal gut-fetal route comes from animal studies showing that oral intake of genetically labeled Enterococcus Fecium by pregnant mice could be traced back in the amniotic fluid64 and meconium,73 whereas it could not be detected in non-inoculated pregnant mice.64,73 Maternal dendritic cells and leukocytes are suggested as trafficking cells for bacterial uptake by placenta.74 Dendritic cells can cross the paracellular space of the intestinal epithelium to directly ingest bacteria from the intestinal lumen. However, dendritic cells are relatively ineffective at killing internalized organisms, and bacteria can by way of dendritic cells hematogeneously spread to other locations, such as the placenta75 and be transferred to the fetus via the paracellular pathway of the placental barrier76 into the amniotic fluid or the fetal blood circulation via the umbilical cord.
The similarity of composition of the placental microbiome to the microbiome of oral cavity4 and the longstanding association between periodontal disease and adverse pregnancy outcome supports the hematogenous shedding of periodontitis-associated bacteria (reviewed in Cobb et al.77).
The peritoneal cavity
While all abdominal organs are enclosed in the subperitoneal cavity by the peritoneum, the fallopian fimbriated ends are structures that open into the peritoneal cavity.78 This makes retrograde spreading of microbiota present in the peritoneal cavity fluid to the fetal compartments another possible route of transfer of bacteria from the mother to the fetus.
Increased intestinal permeability due to a change in microbiome or inflammation41 could result in gut bacterial leakage into the peritoneal cavity.79 Inflammatory cells are known to spread across the one cell-layer peritoneum into the peritoneal cavity.78 However, whether the inflammatory state and shift in gut microbiome during pregnancy leads to increased gut permeability and transfer of the gut microbiome into the peritoneal cavity is unknown; however, the ability of dendritic cells to cross the intestinal lumen74 suggests it is possible.
The lower reproductive tract
Ascending maternal vaginal microbiota could also be a potential source of microbiome of the fetal compartment,80 since DNA from vaginal microbes has been found in amniotic fluid.81 The fetal membranes are thought to form a barrier to ascending microorganisms, which is supported by the fact that after prolonged (premature) rupture of the membranes, intrauterine infection and preterm labour often occur.82 Since the fusion of the fetal membranes to form a barrier does not occur until 17–20 weeks of gestation,48 the uterine cavity could still be accessible for ascending vaginal microbiota, hereby potentially contributing to the early placental and fetal microbiome.
Uterine cavity
The presence of a local residing uterine and endometrial microbiota3,22,83 indicates that during pregnancy, a local microbiome may also be present. Since with implantation the fetal and maternal compartment come into close contact, it is feasible that the uterine and endometrial microbiome, and perhaps even the seminal microbiome, could contribute to the initial placental microbiome.
The main source of the microbiome of the fetal compartment during pregnancy has to be maternal, however, despite different theoretical routes of spreading, it is unknown which, what and how the maternal microbiome contributes to the microbiome of the fetal compartments.
Birth
Despite microbial colonization of the fetal compartments, including the fetal gut, the main maternal source of the postnatal microbiome of the newborn immediately after birth is probably provided during birth. Depending on the birth mode, vaginal delivery versus caesarean section, the neonate has to respectively pass through the vagina or the abdominal skin. The mechanistic process of being born exposes the newborn to commensal bacteria colonizing the vagina, perineum and skin, subsequently resulting in neonatal gut and skin colonization.
Vaginal delivery leads to colonization of neonatal gut with microbes resembling the maternal vaginal microbiota, such as Lactobacillus, Prevotella and Bifidobacterium.84,85 On the other hand, neonates delivered by caesarean section showed an intestinal absence of vaginal microbes, e.g. Bifidobacterium,84 but the presence of microbes resembling the microbial communities of the maternal skin, such as Staphylococcus, Corynebacterium, and Propionibacterium spp.85
Conclusion
The physiological state of pregnancy demands a significant adaptation of the maternal body, including changes in the residing microbial compositions and establishing a placental and fetal microbiome. In addition, during the preconception period, the composition of the male and female microbiome may also interfere with reproductive success. However, it is still difficult to determine which microbial composition is detrimental and optimal for the host or what the exact function of the microbiome at each location is.
The changes in the maternal microbiome seem to support maternal health, since it affects maternal metabolism,41 while also influencing maternal immune responses. On the other hand, changes in the maternal microbiome could also be important for colonisation of the fetus, most likely necessary for the development of fetal immune responses and for inducing the metabolic settings (Figure 1).86,87 It is therefore essential to understand the routes of microbial seeding and how the fetal microbiome is established.
The potentially important role of the maternal and fetal microbiome in maternal, fetal and neonatal health prompts the question of antibiotic use during pregnancy. Antibiotic treatment is associated with disruption of the microbiome88,89 and with a large number of health problems, such as metabolic and immunological diseases.88 Recent studies have shown that prenatal antibiotic use is associated with an increased risk of childhood asthma90 and childhood obesity.91 There are speculations that this is due to the effect of prenatal antibiotics on the maternal and fetal microbiome, resulting in dysbiosis, with detrimental effects on health. In line with the DOHaD theory,92 cautious use of antibiotics should therefore be indicated, since the effect of in utero exposure on the establishment of the fetal microbiome and postnatal development and health in later life is unknown, while it is known that the desired effect of preventing adverse pregnancy outcome is minimal.70
In order to put the roles of the microbiome in maternal and fetal physiology and pathology in perspective, the next steps in microbiome research should also include the interactive effects of other microorganisms present, such as bacteria, viruses, fungi, yeast and archaea. Racicot et al.93 showed that the cervix of pregnant mice is more susceptible to viral infection as compared to the cervix of non-pregnant mice. More importantly, a viral infection of the cervix during pregnancy reduces the protection against ascending vaginal bacteria. Besides, expanding the range of microbiota, combining microbiome research with whole genome sequencing, metagenomics and metabolomics are essential to interpret the potential effects of the microbiome on maternal metabolism and epigenetics.
For the microbiome research focussing on the period of pregnancy, we would like to propose to include the periconception period. Not only do the results of the endometrial22 and vaginal microbiome39 suggest an interactive role around and during pregnancy, effective lifestyle interventions during the preconception period increase not only pregnancy chances, but also health in maternal postpartum and neonatal life.18
This knowledge could lead to the development of pregnancy or periconceptional novel dietary interventions, such as treatment with pre- or probiotics, to prevent or correct certain dysbiotic states. Preconceptional or early pregnancy microbiome data could be future biomarkers to determine obstetrical and fetal health. The ultimate goal would be, if necessary, to postpone a pregnancy to correct a suboptimal and dysbiotic maternal (and paternal) microbiome composition to optimally prepare a couple for a future healthy pregnancy and child.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Guarantor
SS.
Contributorship
SS: Concept, design, manuscript preparation, manuscript editing and manuscript review. RST and MF: Manuscript editing and manuscript review.
References
- 1.Romero R, Espinoza J, Goncalves LF, et al. The role of inflammation and infection in preterm birth. Semin Reprod Med 2007; 25: 21–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Human Microbiome Project Consortium. Structure, function and diversity of the healthy human microbiome. Nature 2012; 486: 207–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Verstraelen H, Vilchez-Vargas R, Desimpel F, et al. Characterisation of the human uterine microbiome in non-pregnant women through deep sequencing of the V1-2 region of the 16S rRNA gene. PeerJ 2016; 4: e1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aagaard K, Ma J, Antony KM, et al. The placenta harbors a unique microbiome. Sci Transl Med 2014; 6: 237ra65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Falony G, Joossens M, Vieira-Silva S, et al. Population-level analysis of gut microbiome variation. Science 2016; 352: 560–564. [DOI] [PubMed] [Google Scholar]
- 6.Flint HJ, Scott KP, Louis P, et al. The role of the gut microbiota in nutrition and health. Nat Rev Gastroenterol Hepatol 2012; 9: 577–589. [DOI] [PubMed] [Google Scholar]
- 7.Maranduba CM, De Castro SB, de Souza GT, et al. Intestinal microbiota as modulators of the immune system and neuroimmune system: impact on the host health and homeostasis. J Immunol Res 2015; 2015: 931574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Knight R, Callewaert C, Marotz C, et al. The microbiome and human biology. Annu Rev Genomics Hum Genet 2017; 18: 65–86. [DOI] [PubMed] [Google Scholar]
- 9.Turnbaugh PJ, Ley RE, Hamady M, et al. The human microbiome project. Nature 2007; 449: 804–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Collado MC, Rautava S, Aakko J, et al. Human gut colonisation may be initiated in utero by distinct microbial communities in the placenta and amniotic fluid. Sci Rep 2016; 6: 23129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hou D, Zhou X, Zhong X, et al. Microbiota of the seminal fluid from healthy and infertile men. Fertil Steril 2013; 100: 1261–1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gosalbes MJ, Llop S, Valles Y, et al. Meconium microbiota types dominated by lactic acid or enteric bacteria are differentially associated with maternal eczema and respiratory problems in infants. Clin Exp Allergy 2013; 43: 198–211. [DOI] [PubMed] [Google Scholar]
- 13.Moissl-Eichinger C, Auerbach AK, Probst AJ, et al. Quo vadis? Microbial profiling revealed strong effects of cleanroom maintenance and routes of contamination in indoor environments. Sci Rep 2015; 5: 9156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grahn N, Olofsson M, Ellnebo-Svedlund K, et al. Identification of mixed bacterial DNA contamination in broad-range PCR amplification of 16S rDNA V1 and V3 variable regions by pyrosequencing of cloned amplicons. FEMS Microbiol Lett 2003; 219: 87–91. [DOI] [PubMed] [Google Scholar]
- 15.Salter SJ, Cox MJ, Turek EM, et al. Reagent and laboratory contamination can critically impact sequence-based microbiome analyses. BMC Biol 2014; 12: 87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dasgupta S, Arya S, Choudhary S, et al. Amniotic fluid: source of trophic factors for the developing intestine. World J Gastrointest Pathophysiol 2016; 7: 38–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ardissone AN, de la Cruz DM, Davis-Richardson AG, et al. Meconium microbiome analysis identifies bacteria correlated with premature birth. PLoS One 2014; 9: e90784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Steegers-Theunissen RP, Twigt J, Pestinger V, et al. The periconceptional period, reproduction and long-term health of offspring: the importance of one-carbon metabolism. Hum Reprod Update 2013; 19: 640–655. [DOI] [PubMed] [Google Scholar]
- 19.Gohir W, Whelan FJ, Surette MG, et al. Pregnancy-related changes in the maternal gut microbiota are dependent upon the mother's periconceptional diet. Gut Microbes 2015; 6: 310–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pelzer ES, Allan JA, Cunningham K, et al. Microbial colonization of follicular fluid: alterations in cytokine expression and adverse assisted reproduction technology outcomes. Hum Reprod 2011; 26: 1799–1812. [DOI] [PubMed] [Google Scholar]
- 21.Pelzer ES, Allan JA, Waterhouse MA, et al. Microorganisms within human follicular fluid: effects on IVF. PLoS One 2013; 8: e59062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moreno I, Codoner FM, Vilella F, et al. Evidence that the endometrial microbiota has an effect on implantation success or failure. Am J Obstet Gynecol 2016; 215: 684–703. [DOI] [PubMed] [Google Scholar]
- 23.Tachedjian G, Aldunate M, Bradshaw CS, et al. The role of lactic acid production by probiotic Lactobacillus species in vaginal health. Res Microbiol 2017; 168: 782–792. [DOI] [PubMed] [Google Scholar]
- 24.Weng SL, Chiu CM, Lin FM, et al. Bacterial communities in semen from men of infertile couples: metagenomic sequencing reveals relationships of seminal microbiota to semen quality. PLoS One 2014; 9: e110152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mandar R, Punab M, Borovkova N, et al. Complementary seminovaginal microbiome in couples. Res Microbiol 2015; 166: 440–447. [DOI] [PubMed] [Google Scholar]
- 26.Robertson SA, Sharkey DJ. Seminal fluid and fertility in women. Fertil Steril 2016; 106: 511–519. [DOI] [PubMed] [Google Scholar]
- 27.Gajer P, Brotman RM, Bai G, et al. Temporal dynamics of the human vaginal microbiota. Sci Transl Med 2012; 4: 132ra52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ravel J, Gajer P, Abdo Z, et al. Vaginal microbiome of reproductive-age women. Proc Natl Acad Sci U S A 2011; 108(Suppl 1): 4680–4687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhou X, Brown CJ, Abdo Z, et al. Differences in the composition of vaginal microbial communities found in healthy Caucasian and black women. ISME J 2007; 1: 121–133. [DOI] [PubMed] [Google Scholar]
- 30.Fettweis JM, Brooks JP, Serrano MG, et al. Differences in vaginal microbiome in African American women versus women of European ancestry. Microbiology 2014; 160: 2272–2282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hyman RW, Herndon CN, Jiang H, et al. The dynamics of the vaginal microbiome during infertility therapy with in vitro fertilization-embryo transfer. J Assist Reprod Genet 2012; 29: 105–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Feldt-Rasmussen U, Mathiesen ER. Endocrine disorders in pregnancy: physiological and hormonal aspects of pregnancy. Best Pract Res Clin Endocrinol Metab 2011; 25: 875–884. [DOI] [PubMed] [Google Scholar]
- 33.Newbern D, Freemark M. Placental hormones and the control of maternal metabolism and fetal growth. Curr Opin Endocrinol Diabetes Obes 2011; 18: 409–416. [DOI] [PubMed] [Google Scholar]
- 34.Aagaard K, Riehle K, Ma J, et al. A metagenomic approach to characterization of the vaginal microbiome signature in pregnancy. PLoS One 2012; 7: e36466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.DiGiulio DB, Callahan BJ, McMurdie PJ, et al. Temporal and spatial variation of the human microbiota during pregnancy. Proc Natl Acad Sci U S A 2015; 112: 11060–11065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hyman RW, Fukushima M, Jiang H, et al. Diversity of the vaginal microbiome correlates with preterm birth. Reprod Sci 2014; 21: 32–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Romero R, Hassan SS, Gajer P, et al. The vaginal microbiota of pregnant women who subsequently have spontaneous preterm labor and delivery and those with a normal delivery at term. Microbiome 2014; 2: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Walther-Antonio MR, Jeraldo P, Berg Miller ME, et al. Pregnancy's stronghold on the vaginal microbiome. PLoS One. 2014; 9: e98514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stout MJ, Zhou Y, Wylie KM, et al. Early pregnancy vaginal microbiome trends and preterm birth. Am J Obstet Gynecol 2017; 217: 356 e1–356. e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Romero R, Hassan SS, Gajer P, et al. The composition and stability of the vaginal microbiota of normal pregnant women is different from that of non-pregnant women. Microbiome 2014; 2: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Koren O, Goodrich JK, Cullender TC, et al. Host remodeling of the gut microbiome and metabolic changes during pregnancy. Cell 2012; 150: 470–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Collado MC, Isolauri E, Laitinen K, et al. Distinct composition of gut microbiota during pregnancy in overweight and normal-weight women. Am J Clin Nutr 2008; 88: 894–899. [DOI] [PubMed] [Google Scholar]
- 43.Mor G, Aldo P, Alvero AB. The unique immunological and microbial aspects of pregnancy. Nat Rev Immunol 2017; 17: 469–482. [DOI] [PubMed] [Google Scholar]
- 44.Wu GD, Chen J, Hoffmann C, et al. Linking long-term dietary patterns with gut microbial enterotypes. Science 2011; 334: 105–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Antony KM, Ma J, Mitchell KB, et al. The preterm placental microbiome varies in association with excess maternal gestational weight gain. Am J Obstet Gynecol 2015; 212: 653.e1–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gomez-Arango LF, Barrett HL, McIntyre HD, et al. Contributions of the maternal oral and gut microbiome to placental microbial colonization in overweight and obese pregnant women. Sci Rep 2017; 7: 2860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dobreva MP, Pereira PN, Deprest J, et al. On the origin of amniotic stem cells: of mice and men. Int J Dev Biol 2010; 54: 761–777. [DOI] [PubMed] [Google Scholar]
- 48.Ilancheran S, Moodley Y, Manuelpillai U. Human fetal membranes: a source of stem cells for tissue regeneration and repair? Placenta 2009; 30: 2–10. [DOI] [PubMed] [Google Scholar]
- 49.Huppertz B, Weiss G, Moser G. Trophoblast invasion and oxygenation of the placenta: measurements versus presumptions. J Reprod Immunol 2014; 101-102: 74–79. [DOI] [PubMed] [Google Scholar]
- 50.Jauniaux E, Watson AL, Hempstock J, et al. Onset of maternal arterial blood flow and placental oxidative stress. A possible factor in human early pregnancy failure. Am J Pathol 2000; 157: 2111–2122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Brosens I, Pijnenborg R, Vercruysse L, et al. The “Great Obstetrical Syndromes” are associated with disorders of deep placentation. Am J Obstet Gynecol 2011; 204: 193–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Roberts JM. Pathophysiology of ischemic placental disease. Semin Perinatol 2014; 38: 139–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Steegers EA, von Dadelszen P, Duvekot JJ, et al. Pre-eclampsia. Lancet 2010; 376: 631–644. [DOI] [PubMed] [Google Scholar]
- 54.Stout MJ, Conlon B, Landeau M, et al. Identification of intracellular bacteria in the basal plate of the human placenta in term and preterm gestations. Am J Obstet Gynecol 2013; 208: 226.e1–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Parnell LA, Briggs CM, Cao B, et al. Microbial communities in placentas from term normal pregnancy exhibit spatially variable profiles. Sci Rep 2017; 7: 11200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Aagaard KM, Lahon A, Suter MA, et al. Primary human placental trophoblasts are permissive for Zika virus (ZIKV) replication. Sci Rep 2017; 7: 41389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cao B, Mysorekar IU. Intracellular bacteria in placental basal plate localize to extravillous trophoblasts. Placenta 2014; 35: 139–142. [DOI] [PubMed] [Google Scholar]
- 58.Miner JJ, Cao B, Govero J, et al. Zika virus infection during pregnancy in mice causes placental damage and fetal demise. Cell 2016; 165: 1081–1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Robbins JR, Skrzypczynska KM, Zeldovich VB, et al. Placental syncytiotrophoblast constitutes a major barrier to vertical transmission of Listeria monocytogenes. PLoS Pathog 2010; 6: e1000732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lauder AP, Roche AM, Sherrill-Mix S, et al. Comparison of placenta samples with contamination controls does not provide evidence for a distinct placenta microbiota. Microbiome 2016; 4: 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.McElrath TF, Hecht JL, Dammann O, et al. Pregnancy disorders that lead to delivery before the 28th week of gestation: an epidemiologic approach to classification. Am J Epidemiol 2008; 168: 980–989 00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Leviton A, Allred EN, Kuban KC, et al. Microbiologic and histologic characteristics of the extremely preterm infant's placenta predict white matter damage and later cerebral palsy. The ELGAN study. Pediatr Res 2010; 67: 95–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Steel JH, Malatos S, Kennea N, et al. Bacteria and inflammatory cells in fetal membranes do not always cause preterm labor. Pediatr Res 2005; 57: 404–411. [DOI] [PubMed] [Google Scholar]
- 64.Jimenez E, Fernandez L, Marin ML, et al. Isolation of commensal bacteria from umbilical cord blood of healthy neonates born by cesarean section. Curr Microbiol 2005; 51: 270–274. [DOI] [PubMed] [Google Scholar]
- 65.Rodriguez N, Fernandez C, Zamora Y, et al. Detection of Ureaplasma urealyticum and Ureaplasma parvum in amniotic fluid: association with pregnancy outcomes. J Matern Fetal Neonatal Med 2011; 24: 47–50. [DOI] [PubMed] [Google Scholar]
- 66.Urushiyama D, Suda W, Ohnishi E, et al. Microbiome profile of the amniotic fluid as a predictive biomarker of perinatal outcome. Sci Rep 2017; 7: 12171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Greenough A. Factors adversely affecting lung growth. Paediatr Respir Rev 2000; 1: 314–320. [DOI] [PubMed] [Google Scholar]
- 68.Brace RA. Physiology of amniotic fluid volume regulation. Clin Obstet Gynecol 1997; 40: 280–289. [DOI] [PubMed] [Google Scholar]
- 69.Underwood MA, Gilbert WM, Sherman MP. Amniotic fluid: not just fetal urine anymore. J Perinatol 2005; 25: 341–348. [DOI] [PubMed] [Google Scholar]
- 70.Goldenberg RL, Culhane JF, Iams JD, et al. Epidemiology and causes of preterm birth. Lancet 2008; 371: 75–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Thaler I, Manor D, Itskovitz J, et al. Changes in uterine blood flow during human pregnancy. Am J Obstet Gynecol 1990; 162: 121–125. [DOI] [PubMed] [Google Scholar]
- 72.Assali NS, Rauramo L, Peltonen T. Measurement of uterine blood flow and uterine metabolism. VIII. Uterine and fetal blood flow and oxygen consumption in early human pregnancy. Am J Obstet Gynecol 1960; 79: 86–98. [DOI] [PubMed] [Google Scholar]
- 73.Jimenez E, Marin ML, Martin R, et al. Is meconium from healthy newborns actually sterile? Res Microbiol 2008; 159: 187–193. [DOI] [PubMed] [Google Scholar]
- 74.Perez PF, Dore J, Leclerc M, et al. Bacterial imprinting of the neonatal immune system: lessons from maternal cells? Pediatrics 2007; 119: e724–e732. [DOI] [PubMed] [Google Scholar]
- 75.Donnet-Hughes A, Perez PF, Dore J, et al. Potential role of the intestinal microbiota of the mother in neonatal immune education. Proc Nutr Soc 2010; 69: 407–415. [DOI] [PubMed] [Google Scholar]
- 76.Uhlig HH, Powrie F. Dendritic cells and the intestinal bacterial flora: a role for localized mucosal immune responses. J Clin Invest 2003; 112: 648–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Cobb CM, Kelly PJ, Williams KB, et al. The oral microbiome and adverse pregnancy outcomes. Int J Womens Health 2017; 9: 551–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Pannu HK, Oliphant M. The subperitoneal space and peritoneal cavity: basic concepts. Abdom Imaging 2015; 40: 2710–2722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Emani R, Alam C, Pekkala S, et al. Peritoneal cavity is a route for gut-derived microbial signals to promote autoimmunity in non-obese diabetic mice. Scand J Immunol 2015; 81: 102–109. [DOI] [PubMed] [Google Scholar]
- 80.Kim MJ, Romero R, Gervasi MT, et al. Widespread microbial invasion of the chorioamniotic membranes is a consequence and not a cause of intra-amniotic infection. Lab Invest 2009; 89: 924–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.DiGiulio DB. Diversity of microbes in amniotic fluid. Semin Fetal Neonatal Med 2012; 17: 2–11. [DOI] [PubMed] [Google Scholar]
- 82.Romero R, Quintero R, Oyarzun E, et al. Intraamniotic infection and the onset of labor in preterm premature rupture of the membranes. Am J Obstet Gynecol 1988; 159: 661–666. [DOI] [PubMed] [Google Scholar]
- 83.Andrews WW, Goldenberg RL, Hauth JC, et al. Endometrial microbial colonization and plasma cell endometritis after spontaneous or indicated preterm versus term delivery. Am J Obstet Gynecol 2005; 193: 739–745. [DOI] [PubMed] [Google Scholar]
- 84.Biasucci G, Rubini M, Riboni S, et al. Mode of delivery affects the bacterial community in the newborn gut. Early Hum Dev 2010; 86: 13–15. [DOI] [PubMed] [Google Scholar]
- 85.Dominguez-Bello MG, Costello EK, Contreras M, et al. Delivery mode shapes the acquisition and structure of the initial microbiota across multiple body habitats in newborns. Proc Natl Acad Sci U S A 2010; 107: 11971–11975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Gomez de Aguero M, Ganal-Vonarburg SC, Fuhrer T, et al. The maternal microbiota drives early postnatal innate immune development. Science 2016; 351: 1296–1302. [DOI] [PubMed] [Google Scholar]
- 87.Wen L, Ley RE, Volchkov PY, et al. Innate immunity and intestinal microbiota in the development of Type 1 diabetes. Nature 2008; 455: 1109–1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Langdon A, Crook N, Dantas G. The effects of antibiotics on the microbiome throughout development and alternative approaches for therapeutic modulation. Genome Med 2016; 8: 39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Guarner F, Malagelada JR. Gut flora in health and disease. Lancet 2003; 361: 512–519. [DOI] [PubMed] [Google Scholar]
- 90.Stensballe LG, Simonsen J, Jensen SM, et al. Use of antibiotics during pregnancy increases the risk of asthma in early childhood. J Pediatr 2013; 162: 832–838.e3. [DOI] [PubMed] [Google Scholar]
- 91.Mueller NT, Whyatt R, Hoepner L, et al. Prenatal exposure to antibiotics, cesarean section and risk of childhood obesity. Int J Obes 2015; 39: 665–670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Barker DJ. The fetal and infant origins of adult disease. BMJ 1990; 301: 1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Racicot K, Cardenas I, Wunsche V, et al. Viral infection of the pregnant cervix predisposes to ascending bacterial infection. J Immunol 2013; 191: 934–941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Del Chierico F, Vernocchi P, Dallapiccola B and Putignani L. Mediterranean diet and health: food effects on gut microbiota and disease control. Int J Mol Sci 2014; 15: 11678–11699. [DOI] [PMC free article] [PubMed]
- 95.Bartosch S, Fite A, Macfarlane GT and McMurdo ME. Characterization of bacterial communities in feces from healthy elderly volunteers and hospitalized elderly patients by using real-time PCR and effects of antibiotic treatment on the fecal microbiota. Appl Environ Microbiol 2004; 70: 3575–3581. [DOI] [PMC free article] [PubMed]
- 96.Santacruz A, Collado MC, Garcia-Valdes L, et al. Gut microbiota composition is associated with body weight, weight gain and biochemical parameters in pregnant women. Br J Nutr 2010; 104: 83–92. [DOI] [PubMed]
- 97.Mueller NT, Shin H, Pizoni A, et al. Birth mode-dependent association between pre-pregnancy maternal weight status and the neonatal intestinal microbiome. Sci Rep 2016; 6: 23133. [DOI] [PMC free article] [PubMed]
- 98.Blaut M. Gut microbiota and energy balance: role in obesity. Proc Nutr Soc 2015; 74: 227–234. [DOI] [PubMed]
- 99.Turnbaugh PJ, Hamady M, Yatsunenko T, et al. A core gut microbiome in obese and lean twins. Nature 2009; 457: 480–484. [DOI] [PMC free article] [PubMed]
- 100.Hu J, Nomura Y, Bashir A, et al. Diversified microbiota of meconium is affected by maternal diabetes status. PLoS One 2013; 8: e78257. [DOI] [PMC free article] [PubMed]
- 101.Rautava S, Collado MC, Salminen S and Isolauri E. Probiotics modulate host-microbe interaction in the placenta and fetal gut: a randomized, double-blind, placebo-controlled trial. Neonatology 2012; 102: 178–184. [DOI] [PubMed]
- 102.Vitali B, Cruciani F, Baldassarre ME, et al. Dietary supplementation with probiotics during late pregnancy: outcome on vaginal microbiota and cytokine secretion. BMC Microbiol 2012; 12: 236. [DOI] [PMC free article] [PubMed]
- 103.Bassols J, Serino M, Carreras-Badosa G, et al. Gestational diabetes is associated with changes in placental microbiota and microbiome. Pediatr Res 2016; 80: 777–784. [DOI] [PubMed]
- 104.Prince AL, Ma J, Kannan PS, et al. The placental membrane microbiome is altered among subjects with spontaneous preterm birth with and without chorioamnionitis. Am J Obstet Gynecol 2016; 214: 627 e1–e16. [DOI] [PMC free article] [PubMed]
- 105.Fujiwara N, Tsuruda K, Iwamoto Y, et al. Significant increase of oral bacteria in the early pregnancy period in Japanese women. J Investig Clin Dent 2017; 8. [DOI] [PubMed]