Abstract
Background:
The demographic profile and clinical manifestations of mood disorder subtypes can differ across regions; however, there is a lack of studies from Saudi Arabia on the sociodemographic characteristics of adult Saudi patients with mood disorder subtypes.
Objective:
The study aims to explore the sociodemographic profile of adult Saudi patients with different types of mood disorders.
Methods:
This retrospective study analyzed the data of all adult Saudi patients (aged ≥18 years) who were diagnosed with a mood disorder and attended the psychiatric outpatient clinic at King Fahd Hospital of the University (KFHU), Al Khobar, Saudi Arabia, between 1982 and 2011. Patients with psychiatric comorbidity were not included in the analyses. Major depressive disorder (depression), bipolar disorder, adjustment disorder and dysthymia were the four subtypes of mood disorder identified in the sample, and all eligible patients were categorized accordingly.
Results:
A total of 340 patients were included in this study. Slightly less than half (42.4%) the study population were aged 18–30 years. Further, 58% of the patients were females, 67.6% were married and 58.8% were unemployed. Depression was the most common mood disorder (~73%). Of the patients with bipolar disorder (n = 38), more than half were male and aged 18–30 years (~58% each); these percentages were higher than that observed in other subtypes.
Conclusion:
This study found that among patients at KFHU, depression is the most common mood disorder and that most patients are females. In contrast, bipolar disorder is more common among males. Further in-depth studies in a larger sample size may provide better patient profiling, which can be used for developing effective screening programs.
Keywords: Adjustment disorder, bipolar disorder, depression, dysthymia, mood disorder, Saudi Arabia
INTRODUCTION
Mood disorder, also known as mood affective disorder, is a group of conditions characterized by disturbance in a person's mood, ranging from elevated (mania or hypomania) to depressed moods (major depression).[1] In fact, mood disturbances may also oscillate between mania and depression, such as in bipolar disorder.[2] Other subtypes include dysthymia (milder form of major depression), cyclothymiacs (milder form of bipolar disorder) and adjustment disorder (abnormal reaction to a life stressor).[2] Mood disorder is the most common psychiatric illness in clinical and community settings, and it has a well-established impact on the quality of life and functioning of affected patients.[2,3,4] Of all mental illnesses, depression is responsible for >40% of disability-adjusted life years (DALYs).[5]
Mood disorder subtypes may differ in their demographic attributes and clinical presentation. In turn, this can affect responses to treatment, and thus requires tailored treatments.[6,7] Several studies have reported on the clinical features of mood disorder subtypes.[6] However, only few have focused on profiling the demographic features for these disorders, and in those studies, the main focus was only on bipolar and major depressive disorders.[8,9,10] In addition, there have been several inconsistencies between the findings of these studies. Some studies found that prevalence of bipolar disorder was higher among single and divorced patients than married patients, whereas other studies found the opposite.[11,12] Similarly, while most studies suggest that educational level does not have a significant influence on the prevalence of bipolar disorder, a few studies have found high prevalence of bipolar disorder among those with low education levels.[12] Similar inconsistencies were also noted in relation to age and gender among different subtypes of mood disorders.[13]
Cultural variations in expressing emotions may also impact patients’ symptomatology.[14] Studies have suggested that the demographic profile of patients with mood disorders may vary considerably between Eastern and Western countries because of cultural differences.[15] While studies on Western populations have found that bipolar disorder is associated with younger age and low educational level,[16] studies on Eastern populations did not support these findings.[17] However, there are very limited studies on Eastern communities and usually confined to a specific age group from a country, such as those conducted by Ghanbari Jolfaei et al. and Uddin et al., with the latter only including patients with bipolar disorder.[15,18,19] Furthermore, the studies had small sample sizes.
Saudi Arabia is a Middle Eastern country with a unique culture and demographic that differs from that of the Western and other Asian communities.[16,17] Consequently, it is necessary to study the demographic attributes of mood disorders’ subtypes within the Saudi population; however, only a limited number of such studies have been conducted.[20] In fact, most studies that focused on demographic features related to different types of mental illnesses in Saudi Arabia are old and of inadequate quality.[20] Therefore, newer, in-depth, quality studies are required to investigate the demographic attributes of mood disorders’ subtypes in the Saudi population.
To the best of the author's knowledge, in Saudi Arabia, to date, only one major study has assessed the demographic characteristics of patients with depression but not of other subtypes.[21] Therefore, the aim of the current study was to determine the sociodemographic characteristics of adult Saudi patients with different mood disorder subtypes, which would guide future interventional studies.
METHODS
This retrospective study analyzed the data of all adult Saudi patients diagnosed with a mood disorder and who attended the psychiatric outpatient clinic at King Fahd Hospital of the University (KFHU), Al Khobar, Saudi Arabia, between 1982 and 2011. KFHU is the only teaching hospital of the city and one of the largest Government hospitals in the Eastern Province of Saudi Arabia, and thus receives a substantial proportion of Saudi psychiatric patients from the area with varied demographic characteristics. Therefore, the sample size of this study is representative of the surrounding area's Saudi population. The study was approved by the Institutional Review Board of Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia (Ref no.: IRB-2018-01-206). Patient consent was not deemed necessary for this study as the data were completely anonymized.
Inclusion criteria included diagnosis of mood disorder based on the Structured Clinical Interview for the International Statistical Classification of Diseases - 10th revision (ICD-10). Patients were excluded if they were non-Saudi, <18 years of age, had inconclusive diagnosis or a psychiatric comorbidity. Major depressive disorder (depression), bipolar disorder, adjustment disorder and dysthymia were the four subtypes of mood disorder identified in the sample, and all eligible patients were categorized accordingly.
Data were analyzed using SPSS version 23 (IBM SPSS, Chicago, IL, USA). Descriptive statistics in the form of bar graphs were used to compare the sociodemographic characteristics of patients with mood disorder subtypes.
RESULTS
Overall sample characteristics
A total of 354 patients’ data were analyzed, of which 340 patients met the inclusion criteria. The patients included were aged 18–90 years (mean ± standard deviation = 32 ± 0.4 years), with most being aged 18–30 years (42.4%). Further, 58% of the patients were females, 67.6% were married and 58.8% were unemployed [Table 1]. Most of the unemployed patients were females (n = 164; 82%), of which the majority were housewives (n = 145; 88.4%). In contrast, of the 142 males included in the study, only 36 (25.4%) were unemployed. The employed males worked in a range of jobs, mainly nonmanagerial. In terms of the mood disorders, depression was the most common (n = 248), followed by bipolar disorder (n = 38), adjustment disorder (n = 31) and dysthymia (n = 23) [Figure 1].
Table 1.
Demographic characteristics of the sample (n = 340)
| Variables | Frequency (%) |
|---|---|
| Gender | |
| Male | 142 (42) |
| Female | 198 (58) |
| Age (years) | |
| 18-30 | 144 (42.4) |
| 31-40 | 92 (27.1) |
| 41-50 | 63 (18.5) |
| 51-60 | 20 (5.9) |
| 61-70 | 16 (4.7) |
| 71-80 | 3 (0.9) |
| 81-90 | 2 (0.6) |
| Occupation | |
| Employed | 90 (26.5) |
| Unemployed | 200 (58.8) |
| Student | 50 (14.7) |
| Marital status | |
| Single | 95 (27.9) |
| Married | 230 (67.6) |
| Divorced | 13 (3.8) |
| Widow | 2 (0.59) |
Figure 1.
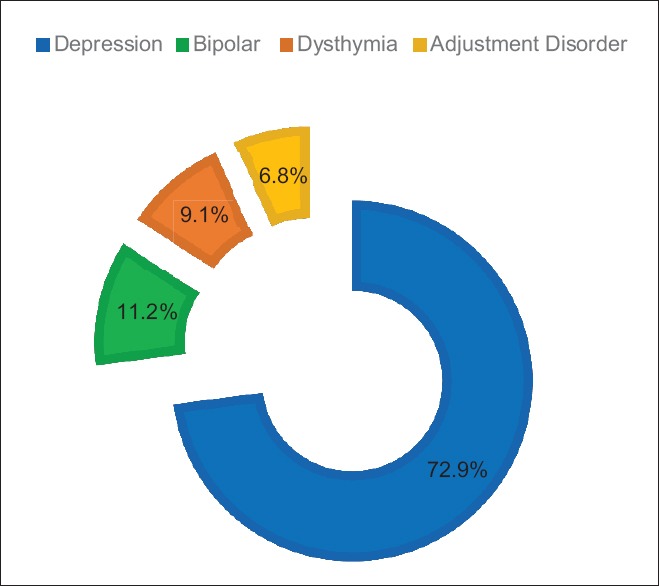
Distribution of mood disorder in the sample (n = 340)
Mood disorder and demographic variables
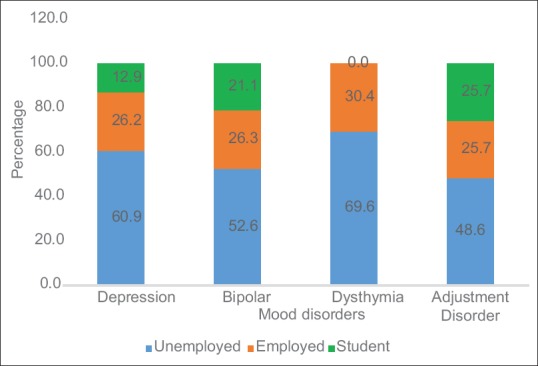
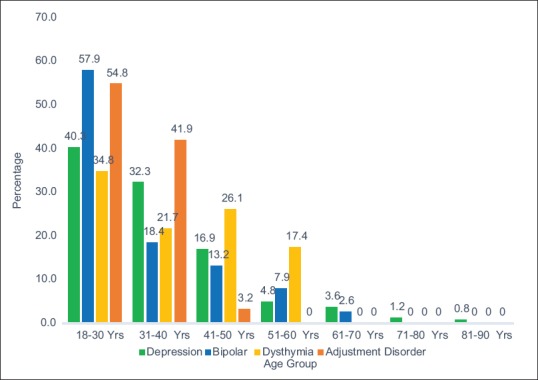
Depression was the most common among females and those who were married and unemployed, a trend that was also observed in all other subtypes. In bipolar disorder, the youngest age group (18–30 years) had a significantly high representation (57.9%) compared with the rest of the study cohort (χ2 = 4.8; P = 0.03). Unlike other subtypes, significantly more males than females had bipolar disorder (57.8%; P < 0.05) [Figures 2 and 3]. The age range of depression was 18–90 years, with no preponderance toward any age group.
Figure 2.
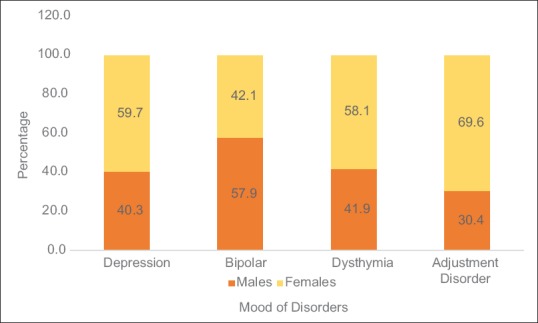
Employment status among subtypes of mood disorder
Figure 3.
Representation of age groups among the subtypes of mood disorder
In the total study population, 78.3% of the married and 69.9% of unemployed patients had dysthymia. However, occupation or marital status was not significantly different from the rest of the sample (χ2 = 0.94, P = 0.33; χ2 = 1.27, P = 0.26), respectively. Similar to the results in depression, dysthymia and the total sample, the majority of patients with adjustment disorder were unemployed females. In addition, 97% of the adjustment disorder patients were aged <40 years, of which those aged <30 years accounted for more than half (55%) [Figure 4].
Figure 4.
Gender distribution among the subtypes of mood disorder
DISCUSSION
The demographic profile and clinical manifestations of mood disorder subtypes can differ across regions, which can affect treatment responses.[6,7] In Saudi Arabia, only few studies have reported on the sociodemographic characteristics of adult Saudi patients for different mood disorder subtypes, and have focussed mainly on depression.[20] To fill this gap in the literature, the current study reports the sociodemographic characteristics of adult Saudi patients with depression, bipolar disorder, adjustment disorder and dysthymia attending a teaching hospital in Saudi Arabia.
Among the four subtypes of mood disorders assessed in this study, major depressive disorder was the most common (73%), and it also included a wider range of age groups, which is in line with the global scenario.[20,22] These findings are unsurprising given that depression is expected to become a leading cause of disease burden by 2030,[23] accounting for 40.5% of DALYs caused by mental and substance use disorders.[24] This also possibly explains the higher percentage of unemployment among the current study's sample.
Some of the overall characteristics of this study group reflect the general characteristics of Saudi Arabia's community. For example, half of the patients were aged <30 years, which is in line with a median age of 26.4 years for the general Saudi population.[25] In addition, the majority of patients in the current study were females, married and unemployed, which is similar to that found in depression-related studies from Saudi Arabia.[20]
The overall high rate of young individuals diagnosed with mood disorder is in agreement with other cohorts that examined patients’ age in population- and clinical-based samples and suggested that 50%–75% of mental illnesses begin around the age of 14–24 years.[26] This is possibly because people are vulnerable in their older adolescence to young adulthood, as they face physiological changes due to experiencing major transitions in life during this period.[26] Further, this age group is easily influenced by psychosocial factors, thereby making them vulnerable to substance abuse and, in turn, predisposing them to mental illnesses.[27]
The overall higher rate of unemployment in the study (42% unemployed) may reflect the well-established dysfunction and decreased productivity seen in relation to mental illness.[26] In addition, this high rate of unemployment is also representative of a large proportion of the females in the study being housewives, a common occurrence in Arab societies. Taking dysthymia as an example, the high percentage of females, who were mostly housewives, could be due to the mild but chronic nature of depression. This challenges the functional ability even more than other subtypes of mood disorder.
Several studies have highlighted an interrelatedness between mental illness and unemployment: while some have found mental illness to be a risk factor for unemployment, others have found unemployment to be a prospective risk factor for mental illness.[27] The latter studies presumed that employment plays a crucial role in an individual's mental well-being by providing financial independence and overall confidence, the lack of which may lead to mental illness. However, the current study is unable to validate these findings, as assessing these aspects was beyond its scope.
The current study cohort had a larger proportion of females than males. This is unsurprising because in mood disorders such as depression, several studies have shown a higher prevalence among women, and particularly young women.[15,20] In fact, some studies have found that the prevalence of depression is almost twice more common in young females than males (aged 14–24 years); nevertheless, this difference decreases with increase in age.[28] This mood disorder-related gender discrepancy[29] may be because females are more sensitive to adversities in their surroundings than males or due to hormonal changes (e.g., postpartum and postmenopausal), rendering females prone to mood disorders such as depression.
In our study, more males than females were diagnosed with bipolar disorder. According to a systematic review by Dell’Aglio et al.,[30] most similar studies did not find gender differences in terms of prevalence of bipolar disorder. Females tend to have a late onset of bipolar disorder compared with males;[31] our study predominantly had young females who could later develop bipolar disorder, and thus this study's gender prevalence findings can alter with time.
Adjustment disorder was most common in patients who had been divorced; this is unsurprising given that adjustment disorder is a long-lasting strong reaction to a life stressor, such as divorce or financial conflicts.
To the best of the author's knowledge, this is the first study from Saudi Arabia assessing the sociodemographic profile of patients with not only bipolar or depressive disorders but also other subtypes of mood disorders. In addition, the study only included patients who had been diagnosed based on ICD-10 criteria and excluded all cases with inconclusive diagnosis, thereby limiting the possibility of bias.
Limitations and Recommendations
As with other record-based cross-sectional studies, testing the homogeneity of data is not possible because of the study's retrospective design. In addition, only Saudi nationals were included in this study, thereby limiting generalizability of the findings. However, it should be noted that the data were collected from a Government teaching hospital, in which, due to regulations, non-Saudis working in only the public sector are eligible for care; therefore, excluding non-Saudis minimized bias.
The sample size of the current study, while small, is comparable with that of similar studies.[31,32] Further, although studied previously to some extent, assessing clinical characteristics such as ages at onset of illness and first hospitalization, number of episodes and suicidal risk in Saudi Arabia would provide a greater level of understanding a patient's profile and may assist in a more individualized clinical care.
The current study analyzed the data of all patients with mood disorders that met the inclusion criteria since KFHU opened in 1982 until the upgradation of mental health service initiated in 2011. The timeframe selected may be considered a limitation; for example, women's employment rates have massively increased in the very recent past, and thus this demographic data may have altered.
The author recommends more in-depth studies to ascertain the risk factors for mood disorder in the population of Saudi Arabia. Further studies with extended approach including information about patient's financial and social supports are important. In addition, although clinical characteristics such as age of patient at onset of illness and at first hospitalization, number of episodes and suicidal risk have previously been studied, these characteristics should be reassessed to provide a current understanding of patients’ profile. This, in turn, may assist in providing patients with a personalized care approach, and thus improve therapy.[33]
CONCLUSION
This study found that among patients at KFHU, Al Khobar, Saudi Arabia, depression is the most common mood disorder and that most patients are females. In contrast, bipolar disorder is more common among males. Further in-depth studies that focus on profiling patients with mental illnesses may assist in developing effective screening programs for mental disorders.
Ethical considerations
The study was approved by the Institutional Review Board (IRB) of Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia (Ref no.: IRB-2018-01-206). This study was conducted in accordance with the ethical principles of the Declaration of Helsinki, as revised in 2013. Requirement for patient consent was waived by the IRB because of the study design and the data being completely anonymized.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Peer review
This article was peer reviewed by two independent and anonymous reviewers
REFERENCES
- 1.Sadock BJ. Inevitable suicide: A new paradigm in psychiatry. J Psychiatr Pract. 2012;18:221–4. doi: 10.1097/01.pra.0000415080.51368.cf. [DOI] [PubMed] [Google Scholar]
- 2.Carlson NR, Heth CD. 4th Canadian Edition. Pearson Education Inc; 2007. Psychology the Science of Behaviour. [Google Scholar]
- 3.American Psychiatric Association. 5th ed. Washington DC: American Psychiatric Association; 2013. Diagnostic and Statistical Manual of Mental Disorders (DSM-5) [Google Scholar]
- 4.Rihmer Z. Prediction and prevention of suicide in bipolar disorders. Clin Neuropsychiatry. 2005;2:48–54. [Google Scholar]
- 5.Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, et al. Global burden of disease attributable to mental and substance use disorders: Findings from the Global Burden of Disease Study 2010. Lancet. 2013;382:1575–86. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- 6.Serretti A, Mandelli L, Lattuada E, Cusin C, Smeraldi E. Clinical and demographic features of mood disorder subtypes. Psychiatry Res. 2002;112:195–210. doi: 10.1016/s0165-1781(02)00227-5. [DOI] [PubMed] [Google Scholar]
- 7.Rouillon F. Epidemiology of bipolar disorders. Current studies. Encephale. 1997;23:7–11. [PubMed] [Google Scholar]
- 8.Leonpacher AK, Liebers D, Pirooznia M, Jancic D, MacKinnon DF, Mondimore FM, et al. Distinguishing bipolar from unipolar depression: The importance of clinical symptoms and illness features. Psychol Med. 2015;45:2437–46. doi: 10.1017/S0033291715000446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moreno C, Hasin DS, Arango C, Oquendo MA, Vieta E, Liu S, et al. Depression in bipolar disorder versus major depressive disorder: Results from the national epidemiologic survey on alcohol and related conditions. Bipolar Disord. 2012;14:271–82. doi: 10.1111/j.1399-5618.2012.01009.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rosenblat JD, McIntyre RS. Treatment of mixed features in bipolar disorder. CNS Spectr. 2017;22:141–6. doi: 10.1017/S1092852916000547. [DOI] [PubMed] [Google Scholar]
- 11.Lee S, Ng KL, Tsang A. A community survey of the twelve-month prevalence and correlates of bipolar spectrum disorder in Hong Kong. J Affect Disord. 2009;117:79–86. doi: 10.1016/j.jad.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 12.Negash A, Alem A, Kebede D, Deyessa N, Shibre T, Kullgren G. Prevalence and clinical characteristics of bipolar I disorder in Butajira, Ethiopia: A community-based study. J Affect Disord. 2005;87:193–201. doi: 10.1016/j.jad.2005.03.011. [DOI] [PubMed] [Google Scholar]
- 13.Chengappa KN, Kupfer DJ, Frank E, Houck PR, Grochocinski VJ, Cluss PA, et al. Relationship of birth cohort and early age at onset of illness in a bipolar disorder case registry. Am J Psychiatry. 2003;160:1636–42. doi: 10.1176/appi.ajp.160.9.1636. [DOI] [PubMed] [Google Scholar]
- 14.Chang M. Understanding Depression Across Cultures: A Social Identity Perspective. PhD Thesis. 2017 [Google Scholar]
- 15.Ghanbari Jolfaei A, Ghadamgahi P, Ahmadzad-Asl M, Shabani A. Demographic and diagnostic features of 3147 inpatients with mood disorders in Iran. Iran J Psychiatry Behav Sci. 2016;10:e2298. doi: 10.17795/ijpbs-2298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stewart WF, Ricci JA, Chee E, Hahn SR, Morganstein D. Cost of lost productive work time among US workers with depression. JAMA. 2003;289:3135–44. doi: 10.1001/jama.289.23.3135. [DOI] [PubMed] [Google Scholar]
- 17.Mohammadi MR, Ghanizadeh H, Noorbala AA, Davidian H, Malek Afzali AA, Naghavi HR. Prevalence of mood disorders in Iran. Iran J Psychiatry. 2006;1:59–64. [Google Scholar]
- 18.Bilaç Ö, Ercan ES, Uysal T, Aydın C. Prevalence of anxiety and mood disorders and demographic characteristics of elementary school students. Turk Psikiyatri Derg. 2014;25:171–80. [PubMed] [Google Scholar]
- 19.Uddin MM, Ahmed HU, Alam MT, Niessen LW, Shamsul DA. Conference: 16th Annual Conference of the International-Society-for-Bipolar-Disorders. 2014:122–3. [Google Scholar]
- 20.Alibrahim OA, Al-Sadat N, Elawad NA. Gender and risk of depression in Saudi Arabia, a systematic review and meta-analysis. J Public Health Afr. 2010;1:e7. doi: 10.4081/jphia.2010.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abumadini MS. Depressive disorders in psychiatric outpatient clinic attendees in Eastern Saudi Arabia. J Family Community Med. 2003;10:43–7. [PMC free article] [PubMed] [Google Scholar]
- 22.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62:617–27. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.World Health Organization. The Global Burden of Disease: 2004 Update. Geneva, Switzerland: WHO Press, World Health Organization; 2008. [Google Scholar]
- 24.Rozatkar AR, Gupta N. Global burden of psychiatric disorders: Has it increased? Indian J Soc Psychiatry. 2016;32:249–50. [Google Scholar]
- 25.Karlin NJ, Weil J, Felmban W. Aging in Saudi Arabia. Gerontol Geriatr Med. 2016;2:2333721415623911. doi: 10.1177/2333721415623911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martel A, Fuchs C. Preface transitional age youth and mental illness – Influences on young adult outcomes. Early Interv Psychiatry. 2017;11:393–400. [Google Scholar]
- 27.Lawental M, Surratt HL, Buttram ME, Kurtz SP. Serious mental illness among young adult women who use drugs in the club scene: Co-occurring biopsychosocial factors. Child Adolesc Psychiatr Clin N Am. 2017;26:13–7. doi: 10.1080/13548506.2017.1330545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pearson C, Janz T, Ali J. Mental and Substance Use Disorders in Canada. Health at a Glance. 2013 [Google Scholar]
- 29.Kendler KS, Gardner CO. Sex differences in the pathways to major depression: A study of opposite-sex twin pairs. Am J Psychiatry. 2014;171:426–35. doi: 10.1176/appi.ajp.2013.13101375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dell’Aglio JC, Jr, Basso LA, Argimon II, Arteche A. Systematic review of the prevalence of bipolar disorder and bipolar spectrum disorders in population-based studies. Trends Psychiatry Psychother. 2013;35:99–105. doi: 10.1590/s2237-60892013000200002. [DOI] [PubMed] [Google Scholar]
- 31.Arnold LM. Gender differences in bipolar disorder. Psychiatr Clin North Am. 2003;26:595–620. doi: 10.1016/s0193-953x(03)00036-4. [DOI] [PubMed] [Google Scholar]
- 32.Yaseen YA. Adjustment disorder: Prevalence, sociodemographic risk factors, and its subtypes in outpatient psychiatric clinic. Asian J Psychiatr. 2017;28:82–5. doi: 10.1016/j.ajp.2017.03.012. [DOI] [PubMed] [Google Scholar]
- 33.Brimblecombe N, Knapp M, Murguia S, Mbeah-Bankas H, Crane S, Harris A, et al. The role of youth mental health services in the treatment of young people with serious mental illness: 2-year outcomes and economic implications. Psychol Health Med. 2018;23:82–8. doi: 10.1111/eip.12261. [DOI] [PubMed] [Google Scholar]


