Abstract
Maternal smoking during pregnancy is associated with both reduced birth weight and adverse neurobehavioral outcomes. The aim of this study was to investigate longitudinal associations between maternal smoking during pregnancy and childhood behavioral outcomes and to determine the role of birth weight in mediating such associations. The study included 489 mother-child pairs. Prenatal exposures were assessed via maternal interviews conducted on average one year after delivery and child behavior assessments were completed at 5–12 years using the Child Behavior Checklist (CBCL) and Teacher Report Form (TRF). Maternal smoking during pregnancy was associated with externalizing and total behavior problems according to both mother and teacher-report. Maternal smoking was also associated with the following percent increases in scores 41% (CBCL) and 44% (TRF) for aggressive behavior and 65% (CBCL) and 47% (TRF) for attention problems. Associations with behavior problems were attenuated or no longer observed for mothers that quit smoking in early pregnancy. The proportion of the total effect of maternal smoking on behavioral outcomes explained by differences in birth weight was small and ranged from 6.6% for externalizing behavior on the CBCL to 20.1% for rule-breaking behavior on the CBCL. Maternal smoking during pregnancy was associated with increases in externalizing and total behavior problems. Our results suggest that birth weight differences explain only a small proportion of the magnitude of association between maternal smoking during pregnancy and selected behavioral outcomes.
Keywords: smoking, pregnancy, behavioral problems, externalizing behavior, birth weight
Introduction
Maternal smoking during pregnancy has been associated with adverse neurobehavioral outcomes in offspring, particularly externalizing behavior problems. Studies have reported increased risks of conduct problems, oppositional defiant disorder, aggressive behavior, and attention deficit hyperactivity disorder among toddlers and children prenatally exposed to cigarette smoke.1–7 Studies extending into adolescence and adulthood have also observed increased risks of these same types of behavior problems.8–10
Maternal smoking during pregnancy has more immediate effects on neonatal outcomes, including reduced fetal growth and low birth weight (LBW). Infants born to mothers who smoke during pregnancy are on average 150–250 grams smaller compared to infants of non-smokers.11, 12 In a study of term live born infants, 23.4% of LBW infants (<2500g) were exposed to maternal smoking during pregnancy compared to 10.9% of their normal birth weight counterparts.13 Reduced birth weight is also associated with neurobehavioral outcomes, independent of prenatal smoking exposure, with effects observed across a spectrum of birth weights below 3500g.14 For example, very low birth weight (VLBW) infants (≤1500 g) have an approximate 3-fold increased risk for ADHD relative to children with normal birth weight.15–18
LBW has been proposed as one potential etiologic pathway that mediates the effect of in-utero exposure to tobacco smoke on neurobehavioral development.19 Given that maternal smoking is associated with reduced birth weight and that reduced birth weight is associated with impaired neurobehavioral development, it is plausible that the observed associations between maternal smoking and childhood behavior problems operate through a pathway involving birth weight. While some studies have attempted to address the role of birth weight in the association between maternal smoking and ADHD,1, 20 there has been less focus on other behavioral outcomes. The aim of this study is to investigate the association between maternal smoking during pregnancy and several measures of childhood behavior problems, according to mother and teacher-report, and to determine the role of birth weight in mediating such observed associations.
Method
A cohort study of childhood neurodevelopment was conducted among children born between 1996 through 2002 whose mothers had previously participated in a case-control study aimed at investigating risk factors for a specific birth defect, hemifacial microsomia (HFM). Cases, <36 months old, were identified from craniofacial centers in 26 cities in the United States and Canada and age-matched controls were selected from the pediatrician offices of the cases or offices within the same zip code. Participant mothers were re-contacted when their child reached an age of 5–6 years old. A series of tests were administered when children were ages 5 to 12 years to collect data on several measures of neurodevelopment. The present analysis was restricted to singleton control children, or those without a structural birth defect. This study was approved by the Institutional Review Board at Boston University and was completed in compliance with HIPAA standards.
Outcome measures
The Child Behavior Checklist (CBCL) and the Teacher Report Form (TRF) were used to measure behavioral adaptation based on maternal and teacher-report, respectively. These instruments are easy to administer and are widely used in psychiatric research. Item content is similar between tests and allows for a systematic comparison of child behavior. Both measures provide summary composite scales of internalizing behavior problems (e.g. shy, withdrawn), externalizing behavior problems (e.g. hyperactive, disruptive), and total behavior problems. The reliability and validity of these measures is excellent.21 T-scores are calculated for these three broadband scales on each test with a mean of 50 and standard deviation of 10. In addition to the three broadband scales, eight syndrome scales are constructed by summing scores for items reflecting problems or complaints in the following areas: aggressive behavior, anxious/depressed, attention problems, rule-breaking behavior, withdrawn/depressed, somatic complaints, social problems, and thought problems. The present analysis is restricted to children with both a completed CBCL and TRF to facilitate comparison of mother-reported and teacher-reported behavior problems. Of the 884 controls included in the initial case-control study, 839 controls were from sites that received IRB approval to contact participants for follow-up. After excluding 13 non-singleton infants,560 had either a completed CBCL or TRF, with 489 having completed both forms. In this sample, the correlation coefficients for mother and teacher reported scores on the syndrome scales ranged from 0.09 for somatic complaints to 0.39 for attention problems.
Maternal smoking
Data on maternal smoking were collected through a structured interview conducted at the time of recruitment into the initial case-control study when the child was <36 months old. Mothers were asked about average number of cigarettes smoked per day prior to pregnancy, any change in average number of cigarettes smoked per day after they became pregnant, and when the change occurred. We categorized women as non-smokers if they reported not smoking at the time of their last menstrual period (LMP) or at any point afterwards. Women that smoked during the time frame from their LMP but quit by the end of the third lunar month of pregnancy were categorized as quitters. Lastly, women that smoked after the third lunar month of pregnancy were categorized as smokers.
Statistical analysis
Distributions of maternal characteristics were calculated according to maternal smoking status; smoker, quitter, or non-smoker. Unadjusted and adjusted linear regression models were used to calculate mean differences (MD) and 95% confidence intervals (CI) for internalizing, externalizing, and total behavior problems on the CBCL and TRF tests using non-smokers as the reference group. Assumptions of linear regression models, including normality, linear relationship, and homoscedasticity, were tested. Variables considered as potential confounders were maternal race/ethnicity (non-Hispanic white, other), maternal age (≤25, 26–34, ≥35), maternal education (≤12 years, 13–15 years, ≥16 years), marital status (married/cohabitating, single/divorced/separated), family income (<35,000, 35,000–64,999, ≥65,000), periconceptional multivitamin use (yes/no), defined as the one month prior to and after the LMP, and prenatal alcohol use (yes/no). Data on these variables were collected in the initial case-control interview by maternal self-report. Data on birth weight and gestational age were collected. Using means and standard deviations published from a United States birth reference, birth weight z-scores standardized by gestational age and sex were calculated.22
Negative binomial regression models were used to model the scores for the CBCL and TRF syndrome scales. These models account for overdispersion of data and their use in statistical analyses of these scales is recommended over the use of T scores in order to retain the variation of the scores, which are truncated when converted to T scores.21 Computationally, the negative binomial regression model provides the incidence rate ratio (IRR) which can be interpreted as the percent increase or decrease in score for exposed compared to unexposed, independent of other covariates.
Sensitivity analyses
Because there are some data suggesting a threshold effect of maternal smoking and behavior problems,3, 10 we performed an analysis which restricted smokers and quitters to those reporting ≥10 cigarettes/day. We also examined the impact of childhood exposure to environmental tobacco smoke (ETS). Information on exposure to ETS during childhood was obtained on a subset of participants through a supplemental questionnaire mailed to the parents during the follow-up study. Lastly, to assess the impact of non-participation, models from the primary analysis were weighted using the inverse probability of participation weights (IPW). Briefly, IPW are weights that are assigned to the available data to restore the representativeness of the original sample. The weights were determined from fitting a logistic regression model in which participation was predicted using the following measured covariates, maternal race, education, age, marital status, income, pre-pregnancy BMI, parity, alcohol use, multivitamin use, smoking, infant gestational age, low birth weight, and infant sex. All analyses were performed using SAS Software Version 9.3.
Mediation analysis
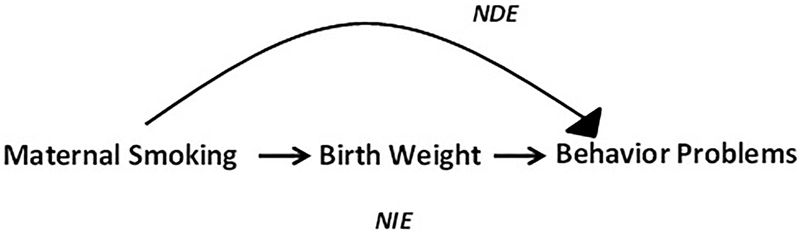
Based on evidence of associations between maternal smoking and birth weight, and between birth weight and behavior problems, birth weight can be considered as a potential causal intermediate. A causal mediation analysis framework was employed to estimate the total effect (TE) of maternal smoking on behavior problems and partition it into the natural direct effect (NDE) and the natural indirect effect (NIE)(Figure 1).23 The proportion of the association mediated (PM) by birth weight was also calculated. For T-score outcomes using a linear regression model the PM was calculated as NIE/TE and for raw score outcomes using a negative binomial regression model the PM was calculated as ((NDEx(NIE-1))÷(NDExNIE-1)). The proportion mediated can provide insight into the role of different pathways by indicating how much of the effect of the exposure on the outcome is due to the effect of the exposure on the intermediate. Birth weight was only considered as a potential mediator between smoking and childhood behavior for outcomes with which it demonstrated (i) one point change in the outcome measure for linear models (β>1.0 or β < −1.0), or (ii) a 10% change in the ratio measure for negative binomial models (β>0.095 or β<−0.10), after adjustment for smoking. Standardized birth weight was modeled as a continuous variable in the mediation analyses. Interaction between maternal smoking and birth weight on behavior problems was also considered.
Figure 1.
Maternal Smoking and Childhood Behavior: Natural Direct Effect (NDE) and Natural Indirect Effect (NIE) Mediated through Birth Weight.
Several assumptions are required by the mediation analysis, including no unmeasured confounding of relationships between (i) exposure-outcome; (ii) mediator-outcome, and (iii) exposure-mediator and (iv) no effect of exposure that confounds the mediator-outcome relationship. We performed a bias analysis to assess the potential impact of an unmeasured confounder of the mediator and outcome on the results of the mediation analysis using the CBCL aggressive outcome as an example. We simulated a binary confounder, U, 1,000 times under a scenario of moderate confounding and a scenario of strong confounding using a random binomial distribution. U was simulated to have the following properties in each dataset, a baseline probability of 15%, a decreased probability of 10% with each unit increase in standardized birth weight and an increased probability of 5% in the moderate confounding scenario and 10% in the strong confounding scenario. The mediation analysis was subsequently performed on each of the 1,000 datasets, adjusting for U, and the range of results for the indirect and direct effects under both the moderate confounding and strong confounding scenario were plotted.
Results
In our study, 16.1% of mothers (n=79) reported smoking during pregnancy. Among mothers that reported smoking at any point during pregnancy, approximately 44% quit in early pregnancy, defined as the first through third lunar month of pregnancy, while the remaining 56% (n=44) smoked into (n=6) or throughout late pregnancy (n=38). Compared to non-smokers, women who smoked into late pregnancy were more likely to be white, non-Hispanic, single, and have ≤ 12 years of education. They were also less likely to use multivitamins in the periconceptional period and were more likely to drink during pregnancy. (Table 1)
Table 1.
Characteristics of Women by Smoking Status During Pregnancy, 1996–2002
| Prenatal Smoking (n=44) | Periconceptional Smoking (Quitters) (n=35) | Non-Smokers (n=410) | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Maternal Race/Ethnicity | ||||||
| White, non-Hispanic | 42 | 95.5 | 28 | 80.0 | 298 | 72.7 |
| Other | 2 | 4.5 | 7 | 20.0 | 112 | 27.3 |
| Maternal Age at Conception | ||||||
| ≤25 | 13 | 29.5 | 17 | 48.6 | 91 | 22.2 |
| 26–34 | 22 | 50.0 | 15 | 42.9 | 248 | 60.5 |
| ≥35 | 9 | 20.5 | 3 | 8.6 | 71 | 17.3 |
| Maternal Education | ||||||
| ≤12 years | 23 | 52.3 | 17 | 48.6 | 104 | 25.4 |
| 13–15 years | 13 | 29.5 | 8 | 22.9 | 97 | 23.7 |
| ≥16 years | 8 | 18.2 | 10 | 28.6 | 208 | 50.7 |
| Missing | 0 | 0.0 | 0 | 0.0 | 1 | 0.2 |
| Marital Status | ||||||
| Married/Cohabitating | 33 | 75.0 | 29 | 82.9 | 373 | 91.0 |
| Single/Divorced/Separated | 11 | 25.0 | 6 | 17.1 | 37 | 9.0 |
| Family Income | ||||||
| <35,000 | 16 | 36.4 | 14 | 40.0 | 113 | 27.6 |
| 35,000–64,999 | 20 | 45.5 | 10 | 28.6 | 127 | 31.0 |
| >65,000 | 6 | 13.6 | 9 | 25.7 | 151 | 36.8 |
| Missing | 2 | 4.5 | 2 | 5.7 | 19 | 4.6 |
| Prepregnancy BMI | ||||||
| <18.5 | 3 | 6.8 | 2 | 5.7 | 10 | 2.4 |
| 18.5–24.9 | 25 | 56.8 | 20 | 57.1 | 258 | 62.9 |
| 25–29.9 | 12 | 27.3 | 9 | 25.7 | 80 | 19.5 |
| ≥30 | 4 | 9.1 | 4 | 11.4 | 55 | 13.4 |
| Missing | 0 | 0.0 | 0 | 0.0 | 7 | 1.7 |
| Prenatal Alcohol Drinking | 9 | 20.5 | 4 | 11.4 | 41 | 10.0 |
| Multivitamin Use (+/− 1 Month LMP) | 8 | 18.2 | 9 | 25.7 | 147 | 35.9 |
| Gestational Age | ||||||
| <37 | 5 | 11.4 | 3 | 8.6 | 24 | 5.9 |
| ≥37 | 39 | 88.6 | 32 | 91.4 | 385 | 93.9 |
| Infant Sex - Male | 17 | 38.6 | 12 | 34.3 | 212 | 51.7 |
| Mean | SD | Mean | SD | Mean | SD | |
| Birth Weight z-score | −0.10 | 1.18 | 0.33 | 0.90 | 0.12 | 0.99 |
Maternal smoking during pregnancy was associated with higher average scores, indicating worse behavior, for broadband scales of externalizing and total behavior problems on the CBCL (MD:3.45; CI:0.23,6.66 and MD:5.07; CI:1.65,8.49, respectively) and on the TRF (MD:3.47; CI:0.74,6.20 and MD:3.64; CI:0.52,6.76, respectively). Compared to children of non-smokers, children whose mothers quit smoking in early pregnancy had similar mean scores for externalizing and total behavior problems on the CBCL and TRF. (Table 2)
Table 2.
Adjusted Mean Differences and 95% Confidence Intervals for Smoking and Behavior Problems, CBCL and TRF Broadband Scales, T-Scores
| Smokers (n=44) | Quitters (n=35) | Non-Smokers (n=410) | |||
|---|---|---|---|---|---|
| Outcomes | Mean (SD) | MDa (95% CI) | Mean (SD) | MDa (95% CI) | Mean (SD) |
| Child Behavior Checklist | |||||
| Internalizing | 49.6 (10.7) | 2.06 (−1.17, 5.30) | 46.9 (9.9) | −1.69 (−5.15, 1.76) | 48.4 (9.6) |
| Externalizing | 50.5 (10.3) | 3.45 (0.23, 6.66) | 48.3 (8.9) | 0.85 (−2.59, 4.28) | 47.3 (9.7) |
| Total | 51.5 (9.8) | 5.07 (1.65, 8.49) | 47.3 (10.3) | 0.21 (−3.45, 3.87) | 46.9 (10.4) |
| Teacher Report Form | |||||
| Internalizing | 49.6 (9.0) | 1.10 (−1.81, 4.02) | 46.4 (8.9) | −1.97 (−5.08, 1.14) | 48.2 (8.8) |
| Externalizing | 52.2 (8.7) | 3.47 (0.74, 6.20) | 49.4 (9.4) | 0.84 (−2.07, 3.75) | 48.2 (8.2) |
| Total | 52.3 (9.2) | 3.64 (0.52, 6.76) | 48.3 (9.8) | −0.26 (−3.59, 3.07) | 48.0 (9.5) |
Adjusted for maternal race, education, age, marital status, prenatal alcohol use, and periconceptional multivitamin use
Negative binomial regression models for the syndrome scales are presented in Table 3. The largest increases in scores associated with maternal smoking during pregnancy were observed for CBCL syndrome scales of attention problems, social problems, and thought problems with increases of 65%, 63%, and 47%, respectively. According to teacher-report, point estimates were largest for syndromes scales of attention (RR:1.47; CI:0.91,2.37) and rule-breaking (RR:1.69; CI: 0.90, 3.17), but all confidence intervals included the null value. In general, associations with behavioral outcomes were attenuated for children of quitters.
Table 3.
Adjusted Rate Ratios and 95% Confidence Intervals for Smoking and Behavior Problems on CBCL and TRF Syndrome Scales, Raw Scores
| Smokers (n=44) | Quitters (n=35) | Non-Smokers (n=410) | |||
|---|---|---|---|---|---|
| Mean (SD) | RRa (95% CI) | Mean (SD) | RRa (95% CI) | Mean (SD) | |
| Child Behavior Checklist | |||||
| Aggressive Behavior | 5.1 (4.7) | 1.41 (0.97, 2.06) | 3.6 (4.5) | 0.98 (0.64, 1.50) | 3.6 (4.2) |
| Anxious/Depressed | 3.4 (4.1) | 1.36 (0.98, 1.90) | 2.2 (2.3) | 0.81 (0.56, 1.19) | 2.7 (2.7) |
| Attention Problems | 4.3 (4.0) | 1.65 (1.11, 2.45) | 2.7 (3.6) | 1.05 (0.67, 1.65) | 2.6 (3.2) |
| Rule-Breaking Behavior | 1.7 (1.6) | 1.28 (0.85, 1.92) | 1.5 (1.9) | 1.16 (0.75, 1.81) | 1.3 (1.7) |
| Social Problem | 2.9 (3.2) | 1.63 (1.14, 2.33) | 2.1 (2.6) | 1.14 (0.76,1.70) | 1.7 (2.0) |
| Somatic Complaints | 1.5 (1.6) | 1.27 (0.80, 2.01) | 1.3 (2.2) | 1.05 (0.64, 1.73) | 1.3 (1.8) |
| Thought Problems | 2.2 (2.1) | 1.47 (1.00, 2.15) | 1.3 (1.4) | 0.88 (0.57, 1.37) | 1.6 (2.1) |
| Withdrawn/Depressed | 0.8 (1.1) | 0.92 (0.54, 1.56) | 0.8 (1.2) | 0.92 (0.52, 1.61) | 0.8 (1.3) |
| Teacher Report Form | |||||
| Aggressive Behavior | 3.0 (4.1) | 1.44 (0.67, 3.06) | 2.1 (4.1) | 1.09 (0.47, 2.51) | 1.9 (4.5) |
| Anxious/Depressed | 2.5 (3.2) | 1.21 (0.77, 1.89) | 1.6 (2.3) | 0.82 (0.50, 1.37) | 2.1 (2.9) |
| Attention Problems | 11.2 (10.2) | 1.47 (0.91, 2.37) | 7.0 (8.6) | 0.96 (0.57, 1.63) | 7.6 (9.7) |
| Rule-Breaking Behavior | 1.4 (1.8) | 1.69 (0.90, 3.17) | 1.0 (1.7) | 1.20 (0.59, 2.44) | 0.8 (1.8) |
| Social Problem | 1.6 (1.8) | 1.27 (0.76, 2.11) | 1.1 (1.7) | 0.92 (0.51, 1.65) | 1.1 (1.9) |
| Somatic Complaints | 0.6 (1.5) | 1.27 (0.51, 3.14) | 0.4 (0.8) | 1.02 (0.40, 2.62) | 0.4 (1.1) |
| Thought Problems | 0.7 (1.3) | 1.31 (0.63, 2.74) | 0.2 (0.6) | 0.43 (0.16, 1.15) | 0.6 (1.4) |
| Withdrawn/Depressed | 1.0 (1.7) | 1.06 (0.58, 1.91) | 0.8 (1.7) | 0.85 (0.43, 1.67) | 0.9 (1.5) |
Adjusted for maternal race, education, age, marital status, prenatal alcohol use, and periconceptional multivitamin use
Results from the IPW analysis and the analysis restricted to heavy smokers (≥10 cigarettes/day) are presented in Table 4. The associations between smoking during pregnancy and behavioral measures were attenuated after accounting for differences in participation, most notably for teacher-reported outcomes, which changed from 3.64 (0.52, 6.76) for total behavior problems in the primary analysis to 2.59 (−0.58, 5.76) in the IPW analysis. Results from the sensitivity analysis restricted to heavy smokers demonstrated slight increases in the mean differences of externalizing and total behavior problem scores for smokers compared to non-smokers. Among those with complete information on prenatal and childhood smoke exposure, 43% of children exposed prenatally were also exposed in childhood while 5% of children of non-smokers were exposed to ETS in childhood (n=8). Due to a small number of children with discordant prenatal and postnatal exposures, we were unable to disentangle the separate effects of prenatal and postnatal exposure to cigarette smoke on behavior problems.
Table 4.
Adjusted Mean Differences and 95% Confidence Intervals for Smoking and Behavior Problems, Broadband Scales, Sensitivity Analyses
| Primary Analysis | Inverse Probability Weighted | Restriction to Heavy Smokers | ||||
|---|---|---|---|---|---|---|
| Smokers (n=44) | Quitters (n=35) | Smokers (n=44) | Quitters (n=35) | Smokers (n=41) | Quitters (n=16) | |
| Outcomes | MDa (95% CI) | MDa (95% CI) | MDa (95% CI) | MDa (95% CI) | MDa (95% CI) | MDa (95% CI) |
| Child Behavior Checklist | ||||||
| Internalizing | 2.06 (−1.17, 5.30) | −1.69 (−5.15, 1.76) | 2.02 (−1.22, 5.26) | −1.58 (−4.95, 1.79) | 1.62 (−1.71, 4.94) | −0.40 (−5.35, 4.54) |
| Externalizing | 3.45 (0.23, 6.66) | 0.85 (−2.59, 4.28) | 3.15 (−0.11, 6.42) | 0.99 (−2.40, 4.39) | 4.11 (0.82, 7.41) | 1.31 (−3.59, 6.21) |
| Total | 5.07 (1.65, 8.49) | 0.21 (−3.45, 3.87) | 4.69 (1.19, 8.18) | 0.47 (−3.16, 4.11) | 5.20 (1.69, 8.70) | 0.27 (−4.95, 5.49) |
| Teacher Report Form | ||||||
| Internalizing | 1.10 (−1.81, 4.02) | −1.97 (−5.08, 1.14) | 0.02 (−2.94, 2.97) | −2.41 (−5.48, 0.67) | 0.50 (−2.48, 3.48) | −1.69 (−6.13, 2.74) |
| Externalizing | 3.47 (0.74, 6.20) | 0.84 (−2.07, 3.75) | 2.66 (−0.13, 5.46) | 0.89 (−2.01, 3.79) | 3.68 (0.92, 6.45) | −1.22 (−5.33, 2.90) |
| Total | 3.64 (0.52, 6.76) | −0.26 (−3.59, 3.07) | 2.59 (−0.58, 5.76) | −0.64 (−3.93, 2.66) | 3.78 (0.57, 7.00) | −2.51 (−7.29, 2.27) |
Adjusted for maternal race, education, age, marital status, prenatal alcohol use, and periconceptional multivitamin use
Reference group for all analyses is non-smokers
Mediation analysis
Birth weight was inversely associated with externalizing and total behavior problems on both the CBCL and TRF. Syndrome scale outcomes on the CBCL were also inversely associated with birth weight, except anxiety, somatic problems and withdrawn/depressed. Associations between birth weight and TRF outcomes were fewer, thereby limiting the number of teacher-reported outcomes eligible for the mediation analysis.
The NIE for all of the outcomes analyzed was small, ranging from 0.32 to 0.36 for the linear outcomes and 1.03 to 1.05 for the count outcomes. The proportion of the observed association mediated through birth weight ranged from 6.6% to 20.1%. Where numbers were sufficient to allow for comparisons, mediated proportions were similar for mother-reported outcomes and teacher-reported outcomes.(Table 5)
Table 5.
Mediation Analysis of Smoking and Behavior Problems by Standardized Birth Weight Z-Scorea
| Birth Weight Z-Score β (SE) | Natural Direct Effect | Natural Indirect Effect | Total Effect | Proportion Mediated | |
|---|---|---|---|---|---|
| Child Behavior Checklist | |||||
| Internalizing | −0.77 (−1.63, 0.10) | -- | -- | -- | |
| Externalizing | −1.54 (−2.39, −0.68) | 2.84 (0.88, 4.80) | 0.36 (−1.60, 2.32) | 3.20 (1.24, 5.16) | 11.3 |
| Total | −1.38 (−2.29, −0.47) | 4.55 (1.20, 7.90) | 0.32 (−0.15, 0.78) | 4.86 (1.50, 8.23) | 6.6 |
| Syndrome Scales | |||||
| Aggressive Behavior | −0.21 (−0.31, −0.10) | 1.36 (0.95, 1.97) | 1.05 (0.98, 1.13) | 1.44 (0.99, 2.08) | 15.9 |
| Anxious/Depressed | −0.11 (−0.21, −0.02) | 1.37 (0.99, 1.90) | 1.03 (0.99, 1.07) | 1.41 (1.01, 1.96) | 10.0 |
| Attention Problems | −0.16 (−0.27, −0.04) | 1.59 (1.08, 2.35) | 1.04 (0.98, 1.11) | 1.66 (1.12, 2.45) | 9.7 |
| Rule-Breaking Behavior | −0.17 (−0.28, −0.05) | 1.18 (0.80, 1.76) | 1.04 (0.98, 1.10) | 1.23 (0.83, 1.83) | 20.1 |
| Social Problem | −0.16 (−0.27, −0.06) | 1.53 (1.08, 2.18) | 1.03 (0.98, 1.09) | 1.58 (1.11, 2.26) | 8.0 |
| Somatic Complaints | −0.04 (−0.16, 0.09) | -- | -- | -- | |
| Thought Problems | −0.10 (−0.20, 0.02) | 1.44 (0.99, 2.10) | 1.03 (0.98, 1.07) | 1.48 (1.01, 2.15) | 8.9 |
| Withdrawn/Depressed | −0.04 (−0.18, 0.11) | -- | -- | -- | |
| Teacher Report Form | |||||
| Internalizing | −0.17 (−0.95, 0.62) | -- | -- | -- | |
| Externalizing | −0.70 (−1.43, 0.04) | -- | -- | -- | |
| Total | −0.81 (−1.65, 0.04) | -- | -- | -- | |
| Syndrome Scales | |||||
| Aggressive Behavior | −0.19 (−0.40, 0.02) | 1.44 (0.68, 3.06) | 1.05 (0.97, 1.13) | 1.50 (0.70, 3.22) | 14.1 |
| Anxious/Depressed | −0.02 (−0.14, 0.11) | -- | -- | -- | |
| Attention Problems | −0.08 (−0.21, 0.04) | -- | -- | -- | |
| Rule-Breaking Behavior | −0.07 (−0.24, 0.11) | -- | -- | -- | |
| Social Problem | −0.09 (−0.24, 0.05) | 1.27 (0.76, 2.10) | 1.03 (0.98, 1.08) | 1.30 (0.79, 2.16) | 12.4 |
| Somatic Complaints | 0.01 (−0.23, 0.24) | -- | -- | -- | |
| Thought Problems | −0.02 (−0.23, 0.19) | -- | -- | -- | |
| Withdrawn/Depressed | −0.04 (−0.19, 0.12) | -- | -- | -- | |
Adjusted for maternal race, education, age, marital status, prenatal alcohol use, and periconceptional multivitamin use
The results of the mediation analysis with the adjustment of a simulated mediator-outcome confounder are presented in the Supplementary Materials. After 1,000 simulations, the direct effect between maternal smoking and the aggressive syndrome scale on the CBCL that was most frequently observed after adjustment for a strong confounder was larger than the observed, 1.44 compared to 1.36, and ranged from 1.16 to 1.68. Upon adjustment for a moderate confounder, the direct effect ranged from 1.24 to 1.57, with a value of 1.37 most frequently observed. The indirect effect was similar to the observed of 1.05 in all scenarios (Supplemental Figures).
Discussion
Maternal smoking during pregnancy was associated with several types of childhood behavior problems, including externalizing and total behavior problems. Scales for attention problems were also associated with maternal smoking during pregnancy. Social problems according to mother-report and rule-breaking behavior according to teacher-report were higher among children of smokers. These associations were attenuated or eliminated for mothers who quit by the third lunar month of pregnancy. In general, internalizing behavior problems were not associated with smoking exposure. These results are in agreement with previous studies in which associations have been observed between maternal smoking and externalizing problems, but not internalizing problems such as withdrawn, depressed, and anxious behavior.2, 4
The results of the mediation analysis indicated that a small proportion of the associations between maternal smoking and several types of behavior problems was explained by an indirect effect through birth weight. Although the percent mediated ranged from 4.5% for teacher-reported total behavior problems to 20% for mother-reported rule-breaking syndrome scale, the indirect effects were quite small and corresponding confidence intervals included the null value. The potential for mediation by birth weight with ADHD was addressed by Nigg et. al20 who concluded that low birth weight did not mediate the association due to minimal change in the effect estimate when included in the regression model. This was true for both mother-reported outcomes obtained from the DISC instrument and teacher-reported outcomes from the TRF.20 The present analysis improves on this through the quantification of both direct and indirect effects and by utilizing a continuous and standardized measure of birth weight; this allowed for analysis of the entire spectrum of birth weight. Furthermore, we performed a bias analysis to simulate and adjust for the presence of a confounder of the birth weight and behavioral outcome relationship, using the CBCL aggressive syndrome scale as an example, which did not materially alter our findings.
In a study of maternal smoking during pregnancy and academic performance among grade school children of both smokers and non-smokers,24 increases in birth weight, even within the clinically normal range, were associated with improved reading and math scores. Similarly our results suggest that improvements in birth weight may result in a reduction, albeit a small reduction, of the magnitude of association between maternal smoking during pregnancy and selected behavioral measures. Birth weight was more strongly associated with most mother-reported behavior problems than with teacher-reported behavior problems, thereby limiting the number of mediation analyses on teacher-reported outcomes. Stronger correlations of birth weight with parent-reported behavior on the CBCL than with teacher-reported outcomes on the teacher’s checklist of psychopathology, an instrument comparable to the TRF, have previously been noted.25 While the reason for stronger associations between birth weight and mother-reported outcomes is not clear, it is possible that mothers of low birth weight children over-report behavioral problems relative to mothers of children with normal birth weight. Despite a limited number of analyses of birth weight and teacher-reported outcomes, results between mother and teacher-reported outcomes were similar where comparison allowed.
One mechanism through which maternal smoking may affect the neurodevelopment of offspring is through fetal brain nicotine receptors that alter cell differentiation and proliferation causing deficits in the creation of cells upon nicotine exposure.26 The mechanism through which birth weight affects neurobehavioral development may involve the disruption of cortical development. Cortical development is inversely related to birth weight and regional cortical volumes have been associated with some measures of poorer neurodevelopment.27 Other proposed mechanisms include nutritional deprivation28 and maternal illnesses that may alter fetal brain development through immune activation.29 In addition to prenatal cigarette smoke exposure and birth weight, childhood environmental tobacco smoke (ETS) exposure has also been associated with behavioral problems in some,30 but not all studies.31 Due to a small number of children with discordant prenatal and postnatal exposures, we were unable to disentangle the separate effects of prenatal and postnatal exposure to cigarette smoke.
Strengths of this study include the availability of data on behavior problems obtained from two separate sources, which included the CBCL and the TRF. Overall the associations between maternal smoking during pregnancy and child behavior problems were of similar magnitude for both sets of reporters. Associations with attention and social problem syndrome scales were slightly larger for mother-report than teacher-report, while associations with rule-breaking syndrome scale were slightly larger for teacher-report than mother-report. A previously conducted study utilizing the CBCL and TRF similarly demonstrated that teachers reported fewer attention problems and more externalizing behavior problems than mothers.32 Contrary to our findings, a study using a 10 item child behavior questionnaire observed parents’ rating of externalizing behavior were higher when compared to teachers’ ratings, but this difference may be explained by the utilization of a different instrument.2
Our study contributes to the existing literature regarding timing of prenatal exposure to cigarette smoke, a component that has been a limitation of previous studies on the topic.2 Results indicated that scores on behavioral measures were similar among children of non-smokers and children of women that quit smoking early in pregnancy, suggesting that the effect of cigarette smoke on behavioral outcomes may be either a result of an accumulation of exposure or most detrimental later in pregnancy. Other studies have observed a decrease in risk of selected behavioral outcomes with quitting or decreasing levels of smoking, yet small associations remain, with one study reporting a reduction in child aggressive behavior associated with a decrease in smoking during pregnancy6 and another reporting smaller associations for child hyperactivity among mothers that quit smoking by the 8th week of pregnancy than among mothers that did not.5 Rantakallio et al. reported little difference in the prevalence of delinquency among adolescent male children of mothers who stopped smoking during pregnancy and mothers that smoked throughout pregnancy, although the time at which mothers stopped smoking was not indicated.9 A study of maternal smoking and neurodevelopment among adolescent mothers reported that significant associations with CBCL outcomes of total behavior problems, externalizing behavior, delinquency and aggression were observed for first trimester exposure. Second and third trimester data were not presented because they did not achieve statistical significance, but it is possible that the parameter estimates were still elevated.10 Mothers who quit smoking in early pregnancy, defined by the third lunar month or approximately 10 weeks post-conception, smoked fewer cigarettes per day than mothers who did not quit, therefore making it difficult to determine if the association between maternal smoking and behavior problems is driven by intensity or duration. The results of a sensitivity analysis restricting to mothers who reported smoking at least 10 cigarettes per day were similar indicating that even among heavy smokers the risk of behavior problems was greatly reduced if women stopped smoking in early pregnancy.
A limitation of our study was the small sample size. The results of the mediation analysis are based on 44 mothers that reported smoking during pregnancy. Another limitation is the possibility of unmeasured confounding of maternal smoking and behavior problems in offspring, specifically by parental behaviors and genetic risk factors.33 Researchers have demonstrated that the association between maternal smoking during pregnancy and behavior problems, specifically ADHD and conduct problems, in offspring can largely be accounted for by parental behaviors and genetic components that are related to maternal smoking and are risk factors for these behavioral outcomes.34, 35 The ability for such factors to potentially confound the association with behavioral outcomes other than conduct disorder and hyperactivity and attention problems is less clear. The presence of an unmeasured confounder that is associated with maternal smoking and an increase in behavioral problems would have caused our estimates to be overstatements of the true association. We evaluated possible mediation by birth weight, but were unable to evaluate other potential mediators, for example, offspring intelligence.36 Misclassification of the exposure is another potential limitation. Data on smoking during pregnancy was based on maternal self-report and retrospectively collected and may be underreported. The prevalence of any prenatal smoking in our study was 16.2%, which is similar to national estimates corresponding to this time period. Lastly, participation bias is possible since our study included 60% of all eligible participants. Results from the IPW analysis showed an attenuation of overall results after accounting for differences between participants and non-participants.
In conclusion, we report associations between maternal smoking during pregnancy and several scales of behavior problems according to both mother and teacher-report. Furthermore, we explain that only a minimal proportion of these associations can be explained by the difference in birth weight distributions between smokers and non-smokers, although our results are based on a small number of mothers that smoked during pregnancy. Future studies are needed to understand the role of birth outcomes and additionally to identify other intermediates that may be targeted by interventions.
Supplementary Material
Financial Support
This work was supported by the National Institutes of Health [R01 DE11939].
Footnotes
Conflicts of Interest
None
Ethical Standards
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national guidelines on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008, and has been approved by the Boston University Institutional Review Board.
REFERENCES
- 1.Thapar A, Fowler T, Rice F, et al. Maternal smoking during pregnancy and attention deficit hyperactivity disorder symptoms in offspring. Am J Psychiatry. 2003;160(11):1985–1989. [DOI] [PubMed] [Google Scholar]
- 2.Batstra L, Hadders-Algra M, Neeleman J. Effect of antenatal exposure to maternal smoking on behavioural problems and academic achievement in childhood: prospective evidence from a Dutch birth cohort. Early Hum Dev. 2003;75(1–2):21–33. [DOI] [PubMed] [Google Scholar]
- 3.Stene-Larsen K, Borge AI, Vollrath ME. Maternal smoking in pregnancy and externalizing behavior in 18-month-old children: results from a population-based prospective study. J Am Acad Child Adolesc Psychiatry. 2009;48(3):283–289. [DOI] [PubMed] [Google Scholar]
- 4.Orlebeke JF, Knol DL, Verhulst FC. Child behavior problems increased by maternal smoking during pregnancy. Arch Environ Health. 1999;54(1):15–19. [DOI] [PubMed] [Google Scholar]
- 5.Kotimaa AJ, Moilanen I, Taanila A, et al. Maternal smoking and hyperactivity in 8-year-old children. J Am Acad Child Adolesc Psychiatry. 2003;42(7):826–33. [DOI] [PubMed] [Google Scholar]
- 6.Brook DW, Zhang C, Rosenberg G, et al. Maternal cigarette smoking during pregnancy and child aggressive behavior. Am J Addict. 2006;15(6):450–456. [DOI] [PubMed] [Google Scholar]
- 7.Braun JM, Froehlich TE, Daniels JL, et al. Association of environmental toxicants and conduct disorder in U.S. children: NHANES 2001–2004. Environ Health Perspect. 2008;116(7):956–962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Paradis AD, Fitzmaurice GM, Koenen KC, et al. Maternal smoking during pregnancy and criminal offending among adult offspring. J Epidemiol Community Health. 2011;65(12):1145–1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rantakallio P, Laara E, Isohanni M, et al. Maternal smoking during pregnancy and delinquency of the offspring: an association without causation? Int J Epidemiol. 1992;21(6):1106–1113. [DOI] [PubMed] [Google Scholar]
- 10.Cornelius MD, De Genna NM, Leech SL, et al. Effects of prenatal cigarette smoke exposure on neurobehavioral outcomes in 10-year-old children of adolescent mothers. Neurotoxicol Teratol. 2011;33(1):137–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Steyn K, de Wet T, Saloojee Y, et al. The influence of maternal cigarette smoking, snuff use and passive smoking on pregnancy outcomes: the Birth To Ten Study. Paediatr Perinat Epidemiol. 2006;20(2):90–99. [DOI] [PubMed] [Google Scholar]
- 12.Bernstein IM, Plociennik K, Stahle S, et al. Impact of maternal cigarette smoking on fetal growth and body composition. Am J Obstet Gynecol. 2000;183(4):883–886. [DOI] [PubMed] [Google Scholar]
- 13.Dietz PM, England LJ, Shapiro-Mendoza CK, et al. Infant morbidity and mortality attributable to prenatal smoking in the U.S. Am J Prev Med. 2010;39(1):45–52. [DOI] [PubMed] [Google Scholar]
- 14.Kelly YJ, Nazroo JY, McMunn A, et al. Birthweight and behavioural problems in children: a modifiable effect? Int J Epidemiol. 2001;30(1):88–94. [DOI] [PubMed] [Google Scholar]
- 15.Mick E, Biederman J, Prince J, et al. Impact of low birth weight on attention-deficit hyperactivity disorder. J Dev Behav Pediatr. 2002;23(1):16–22. [DOI] [PubMed] [Google Scholar]
- 16.Weisglas-Kuperus N, Koot HM, Baerts W, et al. Behaviour problems of very low-birthweight children. Dev Med Child Neurol. 1993;35(5):406–416. [PubMed] [Google Scholar]
- 17.Botting N, Powls A, Cooke RW, et al. Attention deficit hyperactivity disorders and other psychiatric outcomes in very low birthweight children at 12 years. J Child Psychol Psychiatry. 1997;38(8):931–941. [DOI] [PubMed] [Google Scholar]
- 18.Wadsby M, Nelson N, Ingemansson F, et al. Behaviour problems and cortisol levels in very-low-birth-weight children. Nord J Psychiatry. 2014;68(8):626–632. [DOI] [PubMed] [Google Scholar]
- 19.Herrmann M, King K, Weitzman M. Prenatal tobacco smoke and postnatal secondhand smoke exposure and child neurodevelopment. Curr Opin Pediatr. 2008;20(2):184–190. [DOI] [PubMed] [Google Scholar]
- 20.Nigg JT, Breslau N. Prenatal smoking exposure, low birth weight, and disruptive behavior disorders. J Am Acad Child Adolesc Psychiatry. 2007;46(3):362–369. [DOI] [PubMed] [Google Scholar]
- 21.Achenbach T, Rescorla L. Manual for the ASEBA School-Age Forms and Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, and Families; 2001. [Google Scholar]
- 22.Talge NM, Mudd LM, Sikorskii A, et al. United States Birth Weight Reference Corrected For Implausible Gestational Age Estimates. Pediatrics. 2014;133(5):844–853. [DOI] [PubMed] [Google Scholar]
- 23.Valeri L, Vanderweele TJ. Mediation analysis allowing for exposure-mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros. Psychol Methods. 2013;18(2):137–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Anthopolos R, Edwards SE, Miranda ML. Effects of maternal prenatal smoking and birth outcomes extending into the normal range on academic performance in fourth grade in North Carolina, USA. Paediatr Perinat Epidemiol. 2013;27(6):564–574. [DOI] [PubMed] [Google Scholar]
- 25.Buschgens CJ, Swinkels SH, van Aken MA, et al. Externalizing behaviors in preadolescents: familial risk to externalizing behaviors, prenatal and perinatal risks, and their interactions. Eur Child Adolesc Psychiatry. 2009;18(2):65–74. [DOI] [PubMed] [Google Scholar]
- 26.Slotkin TA. Fetal nicotine or cocaine exposure: which one is worse? J Pharmacol Exp Ther. 1998;285(3):931–945. [PubMed] [Google Scholar]
- 27.Peterson BS, Vohr B, Staib LH, et al. Regional brain volume abnormalities and long-term cognitive outcome in preterm infants. JAMA. 2000;284(15):1939–1947. [DOI] [PubMed] [Google Scholar]
- 28.Makrides M, Anderson A, Gibson RA, et al. Improving the neurodevelopmental outcomes of low-birthweight infants. Nestle Nutr Inst Workshop Ser. 2013;74:211–221. [DOI] [PubMed] [Google Scholar]
- 29.Smith SE, Li J, Garbett K, et al. Maternal immune activation alters fetal brain development through interleukin-6. J Neurosci. 2007;27(40):10695–10702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Eskenazi B, Trupin LS. Passive and active maternal smoking during pregnancy, as measured by serum cotinine, and postnatal smoke exposure. II. Effects on neurodevelopment at age 5 years. Am J Epidemiol. 1995;142(9 Suppl):S19–29. [DOI] [PubMed] [Google Scholar]
- 31.Fergusson DM, Horwood LJ, Lynskey MT. Maternal smoking before and after pregnancy: effects on behavioral outcomes in middle childhood. Pediatrics. 1993;92(6):815–822. [PubMed] [Google Scholar]
- 32.Breslau N, Chilcoat HD. Psychiatric sequelae of low birth weight at 11 years of age. Biol Psychiatry. 2000;47(11):1005–1011. [DOI] [PubMed] [Google Scholar]
- 33.Knopik VS. Maternal smoking during pregnancy and child outcomes: real or spurious effect? Dev Neuropsychol. 2009;34(1):1–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Maughan B, Taylor A, Caspi A, et al. Prenatal smoking and early childhood conduct problems: testing genetic and environmental explanations of the association. Arch Gen Psychiatry. 2004;61(8):836–843. [DOI] [PubMed] [Google Scholar]
- 35.Thapar A, Rice F, Hay D, et al. Prenatal smoking might not cause attention-deficit/hyperactivity disorder: evidence from a novel design. Biol Psychiatry. 2009;66(8):722–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rahu K, Rahu M, Pullmann H, et al. Effect of birth weight, maternal education and prenatal smoking on offspring intelligence at school age. Early Hum Dev. 2010;86(8):493–497. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.