ABSTRACT
Hypernatremia affects up to 9% of critically ill patients upon hospital admission, especially in elderly patients with thirst impairment. However, hypernatremia is not entirely explained by fluid imbalance. Recent studies suggest that sodium is an important enhancer of the immune system, raising the question of whether inflammatory states such as sepsis may contribute to hypernatremia. Although sepsis patients with hypernatremia face a greater mortality rate, there is a lack of studies examining a potential association between hypernatremia and sepsis. Motivated by the frequent concurrence of hypernatremia and sepsis observed at an eastern Pennsylvanian community hospital, the current study was conducted to evaluate whether hypernatremia on admission may serve as a potential surrogate marker for sepsis. The medical records of 153 patients with hypernatremia on admission (serum sodium > 145mEq/L) were retrospectively analyzed. The mean age of patients was 81.1. Sepsis was observed in 77.1% of patients, of which 86.2% had dementia. This study demonstrated a positive correlation between hypernatremia on admission and the presence of sepsis. We suggest that the existence of hypernatremia should prompt clinicians to further investigate for sources of infection, especially in the elderly and patients with dementia.
KEYWORDS: Hypernatremia, sodium, sepsis, dementia
1. Introduction
Sodium concentration is the major determinant of the extracellular fluid volume in the body, and it is normally maintained within a narrow physiologic range despite large variations in daily sodium and water intake. Hypernatremia – defined as serum sodium greater than 145mEq/L – is a condition that is commonly observed in patients upon hospital admission, affecting up to 9% of critically ill patients in some hospitals [1–5]. Higher levels of sodium can be associated with a wide range of clinical features which are generally the result of neurological dysfunction due to brain cell shrinkage. Some of these major features include confusion or seizures [6]. Moreover, the mortality rate of patients with hypernatremia is significantly higher than that of patients not affected by this condition [1–5].
Multiple etiologies exist for the development of hypernatremia, but most cases are directly correlated to a decreased or difficult access to water. One major cause, thirst impairment, is frequently seen in patients with dementia, older adults, or intubated patients [7]. In a normal physiological state, hypernatremia generates intense sensation of thirst to protect the body against neurological injury. This normal response may be impaired in elderly or demented patients due to disrupted function of the hypothalamus and impairment of the thirst reflex – which may be absent in up to two thirds of elderly patients with hypernatremia – this results in a reduced ability to replace water losses [8,9]. In fact, an increased incidence of hypernatremia has been reported in nursing home patients above age 85 with severe mobility impairment and the inability to feed themselves [10,11]. To make matters worse, elderly and demented patients often have a restricted access to water. They are either unable to ask for water given their underlying condition, or due to iatrogenic reasons, they do not receive adequate fluid replenishment following hypotonic water depletion [9,12,13].
Recent evidence shows that serum sodium levels may not be completely explained by fluid balance or sodium intake [14]. Some studies suggest that sodium is intimately tied to the immune system, thus raising the question of whether inflammatory states such as sepsis can play a role in the development of hypernatremia [15]. Although sepsis patients with hypernatremia face a greater mortality rate, there is currently a lack of studies examining the exact relationship between hypernatremia and sepsis [16]. If hypernatremia is positively correlated with sepsis, using sodium concentration as a potential laboratorial marker for sepsis could facilitate timely diagnosis and improve the prognosis of hypernatremic septic patients, especially in elderly patients where classic signs of infection are often absent [17]. Motivated by the frequent coincidence of hypernatremia and sepsis observed at Easton Hospital, an eastern Pennsylvanian community hospital, the current study was conducted to evaluate whether hypernatremia on admission may serve as a potential surrogate marker for sepsis.
2. Methods
The study was conducted at Easton Hospital, an eastern Pennsylvania community hospital. Medical records from 2008 through 2010 were reviewed. All patients with serum sodium levels greater than 145mmol/l on admission were included into the study. A diagnosis of sepsis on the admission or discharge note was used to include patients into the cohort. Any two of the following criteria were used to meet the definition of sepsis: temperature greater than 38.5°C or less than 35°C, heat rate greater than 90 beats per minute, respiratory rate greater than 20 breaths per minute, white blood cell count greater than 12,000 or less than 4,000, and evidence of infection by culture or visual inspection. Other data collected for analysis included age, gender, leukocyte count on admission, and presence of dementia.
The study was submitted, reviewed and approved by the local Institutional Review Board.
3. Results
During the selected time frame for the study, 153 patients met the inclusion criteria into the study. Table 1 describes the patient characteristics and incidence of hypernatremia by severity – which was divided according to sodium levels in mild hypernatremia (145–149 mEq/L), moderate hypernatremia (150–159 mEq/L), and severe hypernatremia (≥ 160 mEq/L). The mean age was 81.1. Among the 153 patients with hypernatremia, 118 (77.1%) presented with sepsis on admission, 77 (50.3%) were male, and 132 (86.2%) had the diagnosis of dementia. Of the 118 patients who had sepsis, 84.6% had dementia. Dementia was also present in 91.4% of patients without sepsis. The proportion of patients with dementia increased as the hypernatremia became more severe (mild: 76.2%, moderate: 83%, and severe: 97.7%, p = 0.031). Overall, most patients had moderate hypernatremia (150–159 mEq/L) or severe hypernatremia (≥160 mEq/L), but when comparing the proportion of patients with sepsis within each subcategory of hypernatremia (mild, moderate, severe), there was no significant difference between the number of patients who had sepsis and those who did not (p = 0.63). There was also no significant difference in the incidence of sepsis between the three subcategories of hypernatremia (mild, moderate, severe) (p = 0.63). The incidence of each type of infection is detailed in Figure 1.
Table 1.
Patient characteristics and comorbidity by hypernatremia and sepsis.
| Total |
Sepsis at Admission |
Hypernatremia |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Patients (N = 153) |
Yes (n = 118) |
No (n = 35) |
P value* | Mild (n = 21) |
Moderate (n = 89) |
Severe (n = 43) |
P value* | ||
| Sex | Male | 50.3 | 51.7 | 45.7 | .53 | 42.9 | 56.2 | 41.9 | .23 |
| Female | 49.7 | 48.3 | 54.3 | 57.1 | 43.7 | 58.1 | |||
| Mean Age | 81.1 | 80.7 | 82.5 | .36 | 82.4 | 80.3 | 82.2 | .49 | |
| Sepsis at | Yes | 77.1 | – | – | – | 71.4 | 79.8 | 74.4 | .63 |
| Admission | No | 22.9 | 28.6 | 20.2 | 25.6 | ||||
| Hypernatremia | Mild | 13.7 | 12.7 | 17.1 | |||||
| Moderate | 58.2 | 60.2 | 51.4 | .63 | – | – | – | – | |
| Severe | 28.1 | 27.1 | 31.4 | ||||||
| Dementia | 86.2 | 84.6 | 91.4 | .31 | 76.2 | 83.0 | 97.7 | .026 | |
* From χ2 tests, except for mean age which employed an ANOVA
Figure 1.
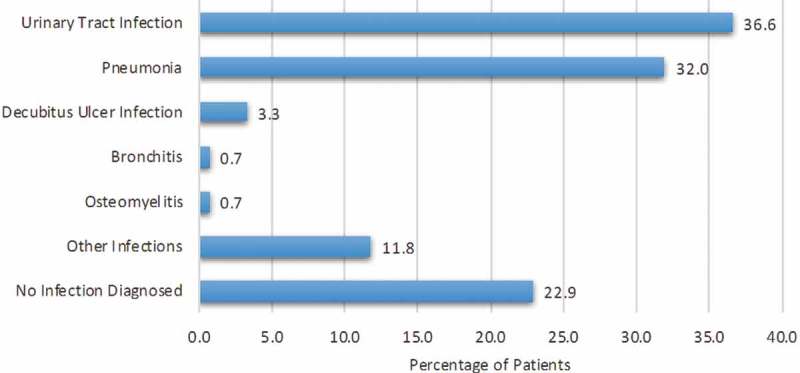
Types of infections.
4. Discussion
The aim of this study was to examine the incidence of sepsis in patients hospitalized with hypernatremia. The results demonstrate a remarkably positive association between hypernatremia on admission and sepsis. The patients in this study population are elderly (mean age: 81.1), with most individuals (86.2%) also suffering from dementia. Elderly patients are at higher risk of developing hypernatremia due to many causes: impaired renal function, decreased thirst reflex, and cognitive decline [9–13]. A diagnosis of dementia is very relevant because these patients either have an impaired thirst mechanism or are unable to ask for water given their underlying neuropsychiatric condition [18]. In fact, this study found a statistically significant increase in the percentage of hypernatremic patients with dementia as the hypernatremia became more severe. This finding is consistent with previous research [18,19]. Hypernatremia by itself can cause altered mental status, which in turn can further limit the ability of these individuals to access free water. Concerns about aspiration risk in patients with altered mental status may also cause caregivers to withhold water, further worsening the hypernatremia. Recent evidence, however, has also shown that hypernatremia in ill patients is not completely explained by sodium intake or fluid balance [14]. In this study, there was a subset of hypernatremic patients who had sepsis but did not have dementia, which might suggest that an underlying infection may play a role in the development of hypernatremia.
The presence of an underlying infection or systemic inflammatory response syndrome (SIRS) can increase the body’s free water requirement, contributing to a significant free water deficit and subsequent hypernatremia. In a study of rat models with experimental sepsis, alterations in the hypothalamic pituitary axis, including elevated aldosterone and corticosterone levels, were reported [20]. Notably, sodium was the only major electrolyte to be elevated in these animal models. These hormonal alterations in response to sepsis may be further contributing factors in the development of hypernatremia.
It is known that dysnatremias are a significant risk factor for mortality in critically ill patients [21]. Both hyponatremia and hypernatremia were significantly associated with death among pneumonia patients. The effect of hypernatremia on mortality in particular may be more pronounced than hyponatremia. Several retrospective studies have shown a mortality rate range of 30% to 48% for patients with hypernatremia levels > 150 mEq/l [22].
Conversely, recent evidence also suggests that sodium is a significant promoter of immune function. This may provide an explanation for the frequency of sepsis among patients hospitalized with hypernatremia. Sodium acts by enhancing the function of macrophages and T-lymphocytes [23]. In fact, a hypernatremic environment may serve as an immunological defense mechanism in inflammatory states such as infection [15]. During skin infections, the concentration of sodium in the skin increases. In humans and mice the sodium accumulation that occurs during cutaneous bacterial infections endogenously boosts antimicrobial capacity by promoting phagosomal acidification and oxidative burst. Salt-induced enhancement of leukocyte function is not only confined to macrophages of the innate immune system, but also enhances T cells, which form an essential part of the antigen-specific adaptive immune system and whose function is known to be governed by various microenvironmental factors. A study that evaluated the effects of skin sodium concentration on macrophages demonstrated that the activation of macrophages in the presence of high sodium chloride concentrations modified epigenetic markers and enhanced mitogen-activated protein kinase dependent nuclear factor of activated T cells. This high-salt response resulted in elevated nitric oxide production and improved the immunity to intracellular pathogens such as Leishmania major. Furthermore, the effect of sodium on the immune system was replicated on the kidneys. Electrolyte concentrations found in the medullary environment of the kidney impact the immunobiology of the renal mononuclear cell network and augment the production of enzymes that are linked to anti-inflammatory phenotypes of mononuclear phagocytes [24].
Despite the association between elevated sodium levels in particular organs and an increase in immune response, classic signs of infection may be absent in the elderly due to an aging immune system [25]. In this context, it is not clear if the hypernatremia observed in our population can be attributed to an attempt to fight an infectious process, an impaired thirst mechanism, or possibly a combination of both factors. Regardless, our findings suggest that individuals with an underlying infection may initially present as hypernatremic patients. Most patients presented with moderate (150–159 mEq/L) or severe (>160 mEq/L) hypernatremia, but there was no significant difference in the incidence of sepsis between the subcategories of hypernatremia (mild, moderate, severe). Therefore, clinicians may be warranted in pursuing further investigation for a possible source of infection in patients who present with any level of hypernatremia, especially in elderly patients.
One limitation of this study is a lack of a comparison group. The presence of a comparison group could establish a baseline to determine the incidence of sepsis in patients without hypernatremia. Subsequent studies of the data could clarify the nature of the relationship between hypernatremia on admission to a higher incidence of sepsis. Adding a comparison group would be beneficial to assess the statistical significance of the study findings. Another potential limitation of this study is the retrospective design. Given intrinsic design limitations of this chart review study, we cannot make conclusions about cause and effect correlations. The observation of our data points that an association between sepsis and hypernatremia exists, however we cannot clarify the exact nature of this association. On that note, it is hoped that this study findings will prompt future research, ideally in prospective format, that could seek to establish whether the presence of hypernatremia is significantly related to sepsis and what is the exact nature of such association.
5. Conclusion
Patients admitted with hypernatremia are significantly more likely to have sepsis as well. This is true in patients with dementia, mainly from nursing home settings, and also among nondemented patients. Signs of infection may be suppressed in the elderly due to an aging immune system. The classical presentation of infections – namely fever and high white count – is less frequent in the elderly compared to younger patients. Our study identifies hypernatremia as a potential surrogate marker of sepsis. Given the high mortality rate of sepsis patients with hypernatremia, we conclude that the presence of hypernatremia should spur the clinician to further investigate for a possible source of infection, especially in the elderly and nursing home populations with dementia. This could lead to prompt diagnosis, efficient work-up, and a potentially life-saving management plan.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1].Bagshaw SM, Townsend DR, Mcdermid RC.. Disorders of sodium and water balance in hospitalized patients. Can J Anaesth. 2009;56(2):151–167. [DOI] [PubMed] [Google Scholar]
- [2].Nur S, Khan Y, Nur S, et al. Hypernatremia: correction rate and hemodialysis. Case Rep Med. 2014;4 Article ID 736073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Reynolds RM, Padfield PL, Seckl J.. Disorders of sodium balance. BMJ. 2006;332(7543):702–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Kim SW. Hypernatemia: successful treatment. Electrolyte Blood Press. 2006;4(2):66–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Vedantam A, Robertson C, Gopinath S. Morbidity and mortality associated with hypernatremia in patients with severe traumatic brain injury. Neurosurg Focus. 2017;43(5):E2. [DOI] [PubMed] [Google Scholar]
- [6].Diringer M. Chapter 38 - Neurologic manifestations of major electrolyte abnormalities. Handb Clin Neurol. 2017;141:705–713. [DOI] [PubMed] [Google Scholar]
- [7].Braun MM, Barstow CH, Pyzocha NJ. Diagnosis and management of sodium disorders: hyponatremia and hypernatremia. Am Fam Physician. 2015;91(5):299–307. [PubMed] [Google Scholar]
- [8].Hoorn EJ, Betjes MG, Weigel J, et al. Hypernatraemia in critically ill patients: too little water and too much salt. Nephrol Dial Transplant. 2008;23(5):1562–1568. [DOI] [PubMed] [Google Scholar]
- [9].Molaschi M, Ponzetto M, Massaia M, et al. Dehydration in the elderly on admission to hospital. J Nutr Health Aging. 1997;1(3):156–160. [PubMed] [Google Scholar]
- [10].Macdonald NJ, McConnell KN, Stephen MR, et al. Hypernatraemic dehydration in patients in a large hospital for the mentally handicapped. BMJ. 1989;299(6713):1426–1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Lavizzo-Mourey R, Johnson J, Stolley P. Risk factors for dehydration among elderly nursing home residents. J Am Geriatr Soc. 1988;36(3):213–218. [DOI] [PubMed] [Google Scholar]
- [12].Chassagne P, Druesne L, Capet C, et al. Clinical presentation of hypernatremia in elderly patients: a case control study. J Am Geriatr Soc. 2006;54(8):1225–1230. [DOI] [PubMed] [Google Scholar]
- [13].Gross CR, Lindquist RD, Woolley AC, et al. Clinical indicators of dehydration severity in elderly patients. J Emerg Med. 1992;10(3):267–274. [DOI] [PubMed] [Google Scholar]
- [14].van IJzendoorn MC, Buter H, Kingma WP, et al. The development of intensive care unit acquired hypernatremia is not explained by sodium overload or water deficit: a retrospective cohort study on water balance and sodium handling. Crit Care Res Pract. 2016;6 Article ID 9571583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Quinn JW, Sewell K, Simmons DE. Recommendations for active correction of hypernatremia in volume-resuscitated shock or sepsis patients should be taken with a grain of salt: A systematic review. SAGE Open Med. 2018;6:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Ni HB, Hu XX, Huang XF, et al. Risk factors and outcomes in patients with hypernatremia and sepsis. Am J Med Sci. 2016;351(6):601–605. [DOI] [PubMed] [Google Scholar]
- [17].Nasa P, Juneja D, Singh O. Severe sepsis and septic shock in the elderly: an overview. World J Crit Care Med. 2012;1(1):23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Mahowald JM, Himmelstein DU. Hypernatremia in the elderly: relation to infection and mortality. J Am Geriatr Soc. 1981;29(4):177–180. [DOI] [PubMed] [Google Scholar]
- [19].Shah MK, Workeneh B, Taffet GE. Hypernatremia in the geriatric population. Clin Interv Aging. 2014;9:1987–1992. Published 2014 Nov 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Flierl MA, Rittirsch D, Weckbach S, et al. Disturbances of the hypothalamic-pituitary-adrenal axis and plasma electrolytes during experimental sepsis. Ann Intensive Care. 2011;1:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Lindner G, Funk GC. Hypernatremia in critically ill patients. J Crit Care. 2013;28:216.e11–216.e20. [DOI] [PubMed] [Google Scholar]
- [22].Sen S, Tran N, Chan B, et al. Sodium variability is associated with increased mortality in severe burn injury. Burns Trauma. 2017;5:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Schatz V, Neubert P, Schröder A, et al. Elementary immunology: na+ as a regulator of immunity. Pediatr Nephrol. 2016;32(2):201–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Jantsch J, Schatz V, Friedrich D, et al. Cutaneous Na+ storage strengthens the antimicrobial barrier function of the skin and boosts macrophage-driven host defense. Cell Metab. 2015;21(3):493–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].van Duin D. Diagnostic challenges and opportunities in older adults with infectious diseases. Clinl Infect Dis. 2012;54(7):973–978. [DOI] [PMC free article] [PubMed] [Google Scholar]


