Editor: In 2014, the Joint United Nations Program on HIV/AIDS (UNAIDS) and partners announced the 90-90-90 treatment targets to end the AIDS epidemic by 2030. The targets are diagnosis of 90% of people with HIV infection, provision of antiretroviral therapy (ART) to 90% of people diagnosed with HIV infection, and viral suppression of HIV replication among 90% of those provided with ART by 2020. Achieving those targets would equate to 73% of all HIV-infected persons achieving viral suppression.
In the United States, there were an estimated 38,500 new HIV infections in 2015.1 Of those diagnosed with HIV infection, men who have sex with men (MSM), black men, Hispanic/Latino men, Native Hawaiians and Pacific Islanders, and American Indian/Alaska Natives were disproportionately burdened by HIV infection (Fig. 1). Although many states are close to achieving the HIV testing target set forth by UNAIDS, nearly all states need to increase ART and viral suppression among those diagnosed with HIV infection. To reach UNAIDS 90-90-90 targets, new interventions are needed to prevent HIV infection and engage at-risk communities with health care providers.
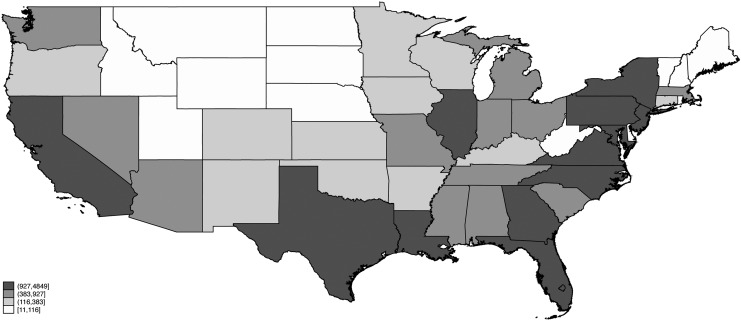
FIG. 1.
New HIV infections in the United States of America by state, 2015.
Historically, poor health care engagement has been observed among minority MSM. That phenomenon has been attributed to many factors such as uninsured or underinsured status; health care access; and psychosocial, social, and geographic determinants of health.2 A survey of black MSM found many participants experienced stigma from health care providers due to race and sexual orientation, with nearly half of the participants reporting mistrust of medical establishments. Among both HIV-infected and uninfected participants, those who reported greater stigma had longer gaps in time since their last medical examinations. To increase health care engagement, Internet-based tools have been shown to be acceptable, feasible, and generate impact.3 Digital innovations with Internet-based tools not only had positive effects on clinic attendance rates, risk reduction, and self-care, but they also increased ART adherence. Because of this, the Centers for Disease Control and Prevention have made digital tools and new technologies a priority to reach young MSM of all races.4 mHealth innovations (short message service and phone calls) were also effective in improving clinic attendance, ART adherence, and reduced time from testing to treatment.
In addition to carrying a higher burden of HIV infection, minority MSM also are underprescribed pre-exposure prophylaxis (PrEP) for HIV infection.5 Akin to digital innovations used for HIV infection, telehealth-based approaches have been shown to be effective in increasing PrEP access among young MSM, while reducing barriers to care, such as stigma, cost, and medical distrust. Increasing access to PrEP could not only prevent HIV infection acquisition, but also act as a gateway to primary care, which may have benefits for behavioral health, mental health, and prevention and treatment of other diseases. To end the HIV epidemic, it is not only necessary to expand the use of digital innovations to increase testing and treatment among those with HIV infection, but also prevent new infections from occurring with increased use of PrEP for HIV infection.
Author Information
Dr. Jeffrey D. Klausner was the United States Centers for Disease Control and Prevention branch chief for HIV and TB, South Africa, 2009–2011. Since then, he worked to identify innovative ways to increase testing and treatment among underserved populations. In addition, he is now studying tools to increase pre-exposure prophylaxis for HIV infection use among health care adverse populations.
Acknowledgments
N.K. is supported by the Fogarty International Center of the National Institutes of Health (NIH) under award number D43TW009343 and the University of California Global Health Institute (UCGHI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or UCGHI.
Authors' Contributions
N.K. reviewed the literature and created the figure. N.K. and J.D.K. drafted the article.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
Time for article preparation was supported, in part, by NIH/FIC D43TW009343 (Fogarty International Center of the NIH and the University of California Global Health Institute Training Program), NIH P30MH058107 (The Center for HIV Identification, Prevention, and Treatment Services), and NIH/NIAID AI028697 (UCLA Center for AIDS Research). No funding bodies had any role in study design, data collection and analysis, decision to publish, or preparation of the article.
References
- 1. Centers of Disease Control and Prevention: Estimated HIV Incidence and Prevalence in the United States 2010–2015 Vol. 23. Centers for Disease Control and Prevention, Atlanta, GA, 2018. [Google Scholar]
- 2. Eaton LA, Driffin DD, Kegler C, et al. : The role of stigma and medical mistrust in the routine health care engagement of black men who have sex with men. Am J Public Health 2015;105:e75–e82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Daher J, Vijh R, Linthwaite B, et al. : Do digital innovations for HIV and sexually transmitted infections work? Results from a systematic review (1996–2017). BMJ Open 2017;7:e017604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Centers of Disease Control and Prevention: HIV Prevention Progress Report, 2019. Centers of Disease Control and Prevention, Atlanta, GA, 2019 [Google Scholar]
- 5. Goldstein RH, Streed CG, Jr., Cahill SR: Being PrEPared—Preexposure prophylaxis and HIV disparities. N Engl J Med 2018;379:1293–1295 [DOI] [PubMed] [Google Scholar]