This randomized clinical trial assesses the effectiveness of support, collaboration, and competition within a behaviorally designed gamification intervention to increase physical activity among overweight and obese adults.
Key Points
Question
What is the best way to incorporate social incentives within a behaviorally designed gamification intervention to increase physical activity among overweight and obese adults?
Findings
In this randomized clinical trial of 602 overweight and obese adults from 40 states across the United States, gamification interventions with support, collaboration, and competition significantly increased physical activity compared with the control group during the 24-week intervention. The competition arm had the greatest increase in physical activity from baseline during the intervention; during the 12-week follow-up, physical activity was lower in all arms, but remained significantly greater in the competition arm than in the control arm.
Meaning
Small changes to the design of gamification can lead to important differences in effectiveness.
Abstract
Importance
Gamification, the use of game design elements in nongame contexts, is increasingly being used in workplace wellness programs and digital health applications. However, the best way to design social incentives in gamification interventions has not been well examined.
Objective
To assess the effectiveness of support, collaboration, and competition within a behaviorally designed gamification intervention to increase physical activity among overweight and obese adults.
Design, Setting, and Participants
This 36-week randomized clinical trial with a 24-week intervention and 12-week follow-up assessed 602 adults from 40 states with body mass indexes (calculated as weight in kilograms divided by height in meters squared) of 25 or higher from February 12, 2018, to March 17, 2019.
Interventions
Participants used a wearable device to track daily steps, established a baseline, selected a step goal increase, were randomly assigned to a control (n = 151) or to 1 of 3 gamification interventions (support [n = 151], collaboration [n = 150], and competition [n = 150]), and were remotely monitored. The control group received feedback from the wearable device but no other interventions for 36 weeks. The gamification arms were entered into a 24-week game designed using insights from behavioral economics with points and levels for achieving step goals. No gamification interventions occurred during follow-up.
Main Outcomes and Measures
The primary outcome was change in mean daily steps from baseline through the 24-week intervention period.
Results
A total of 602 participants (mean [SD] age, 39 [10] years; mean [SD] body mass index, 30 [5]; 427 [70.9%] male) were included in the study. Compared with controls, participants had a significantly greater increase in mean daily steps from baseline during the intervention in the competition arm (adjusted difference, 920; 95% CI, 513-1328; P < .001), support arm (adjusted difference, 689; 95% CI, 267-977; P < .001), and collaboration arm (adjusted difference, 637; 95% CI, 258-1017; P = .001). During follow-up, physical activity remained significantly greater in the competition arm than in the control arm (adjusted difference, 569; 95% CI, 142-996; P = .009) but was not significantly greater in the support (adjusted difference, 428; 95% CI, 19-837; P = .04) and collaboration (adjusted difference, 126; 95% CI, −248 to 468; P = .49) arms than in the control arm.
Conclusions and Relevance
All 3 gamification interventions significantly increased physical activity during the 24-week intervention, and competition was the most effective. Physical activity was lower in all arms during follow-up and only remained significantly greater in the competition arm than in the control arm.
Trial Registration
ClinicalTrials.gov identifier: NCT03311230
Introduction
In 2018, the US Department of Health and Human Services released the second edition of the Physical Activity Guidelines for Americans.1 Despite expanding evidence of the many health benefits associated with physical activity, nearly 80% of US adults are insufficiently active. The guidelines recommended that some physical activity is better than none, with increased benefits from more moderate and vigorous exercise.1 The guidelines also noted the increasing body of evidence indicating that even small increases or light-intensity physical activity can lead to health benefits, particularly for more sedentary individuals.1,2,3,4,5
Gamification is the use of game design elements, such as points and levels in nongame contexts, and is increasingly being used to promote healthy behaviors.6,7,8 For example, prior work from members of our group9,10 found evidence that gamification has been offered through workplace wellness programs across the United States and that nearly two-thirds of the most popular health and fitness mobile applications incorporate elements of gamification. However, most workplace wellness programs and digital health applications have not appropriately leveraged principles from theories of health behavior,6,8,10,11 which could be a major reason why recent evaluations suggest there has been little effect from them on health behaviors.12,13
A previous randomized clinical trial from members of our group14 demonstrated that behavioral economic principles could be embedded within a gamification intervention to significantly increase physical activity among families. However, this trial used a shorter intervention of 3 months, was conducted at a single site, and tested only 1 form of social incentive among family members.
In this study, our objective was to use a randomized clinical trial to test the effectiveness of gamification interventions that leverage insights from behavioral economics to enhance supportive, competitive, or collaborative social incentives to increase physical activity among overweight and obese adults. We partnered with a large consulting firm to test a scalable approach that enrolled individuals from across the United States and remotely monitored physical activity levels for 9 months with wearable devices and an automated technology platform.15
Methods
Study Design
Social incentives to Encourage Physical Activity and Understand Predictors (STEP UP) was a randomized clinical trial conducted from February 12, 2018, to March 17, 2019, consisting of a 2-week run-in period, a 24-week intervention period, and a 12-week follow-up period. Details of the study design and protocol have been published previously.16 The trial protocol (Supplement 1) was approved by the University of Pennsylvania Institutional Review Board. Data were not deidentified. The study was conducted using Way to Health,15 a research technology platform at the University of Pennsylvania used previously for remote monitoring and physical activity interventions.14,17,18,19,20,21 Participants used the study website to create an account, provide informed consent online, and complete baseline and validated survey assessments. Each participant selected whether to receive regular study communications by email, text message, or both. Eligible participants were mailed a wrist-worn wearable device (Withings Activité Steel), which lasts approximately 6 months without charging, along with a replacement battery. Participants connected their devices to the Way to Health platform for remote data collection and used them to track daily step counts. Prior work has demonstrated these types of devices are accurate for tracking step counts22 and have been used successfully in prior work.9,14,17All participants received $25 for enrolling in the trial, $50 for completing the 24-week intervention and surveys, and $50 for completing the 12-week follow-up and surveys.
Participants
Recruitment occurred from October 30, 2017, to July 11, 2018, in partnership with Deloitte Consulting, which sent email invitations to all their employees in the United States (approximately 26 000 people). Participants were eligible for the trial if they were 18 years or older, able to read and provide informed consent to participate, had a self-reported body mass index (BMI) (calculated as weight in kilograms divided by height in meters squared) of 25 or higher, and owned a smartphone or tablet compatible with the wearable device. Participants were excluded if they had a condition that made participation unfeasible (eg, inability to provide informed consent, illiteracy, or inability to speak, read, and write English), they had a condition that made participation unsafe (eg, pregnancy or being told by a physician not to exercise), they were already enrolled in another study that targeted physical activity, or they would be unable to complete the 36-week trial because of another medical condition or other reason.
Baseline Step Count
After the wearable device was set up and connected to the study, the participant was asked to get used to wearing the device for several weeks. During this run-in period, a baseline step count was estimated using the second week of data—a method used in previous work.14,17 Data from the first week were ignored to diminish the potential upward bias of the estimate from higher activity during initial device use. To prevent potential mismeasurement, we ignored any daily values less than 1000 steps because evidence indicates that these values are unlikely to represent capture of actual activity during the whole day.23,24 If less than 4 days of data were available during the second week (n = 13), the participant was contacted to inquire about any device issues and the run-in period was extended until at least 4 days of data were captured.
Goal Setting
Each participant was informed of his or her baseline step count and then asked to choose a step goal increase that was 33%, 40%, or 50% higher than the baseline (each goal rounded up to the next hundred), or the participant could select another goal as long as it was at least 1500 steps greater than baseline. These options were based on prior work.14 An important difference from the prior study14 was that participants could change their goal at any time as long as it was within these options.
Randomization
After establishing a baseline and selecting a step goal increase, participants were randomized electronically by stratifying on participant baseline step count (<5000 steps per day, 5001-7500 steps per day, or >7500 steps per day) and using block sizes of 4 groups with 3 participants per group. Participants were randomized in groups of 3 because of the design of the collaborative and competitive gamification interventions. All investigators, statisticians, and data analysts were blinded to arm assignments until the study and analysis were completed.
Interventions
Participants randomized to the control arm (n = 151) were asked to use the wearable device and strive for their daily step goal for 36 weeks. They received regular feedback from the wearable device and its smartphone application but no other interventions.
Participants in the intervention arms (support [n = 151], collaboration [n = 150], and competition [n = 150]) were entered into a game with points and levels that was run automatically (participants did not have to actively play the game, just strive for step goals) and provided a daily notification of their progress. The design was based on prior work14 that incorporated principles from behavioral economics but also included several changes to improve participant experience.
First, participants in the gamification arms signed a precommitment pledge to strive to achieve their step goal during the 36-week study. Precommitment has been demonstrated to motivate behavior change.25,26 In prior work,14 step goal targets began immediately, which was challenging for some participants. Therefore, in this trial, participants had a ramp-up period during the first 4 weeks in which daily step goal targets increased by 25% per week from baseline to the goal. Participants were asked to strive for this step goal for the rest of the trial but could change the goal at any point as long as it was within the original options provided to them.
Second, every Monday the participant received 70 points (10 for each day of the week). If the participant did not achieve their step goal on the prior day, they lost 10 points from their balance. This design leverages prospect theory,27 which has demonstrated that loss framing is more effective at motivating behavior change than gain framing.19,27
Third, at the end of each week, participants could move up or down levels (from lowest to highest: blue, bronze, silver, gold, or platinum). This design creates achievable goal gradients (the notion that the next-highest level was attainable), a sense of social status, and progression through the game. We made 3 important changes from the prior study.14 We used 5 levels instead of 4 to allow for more progression in a longer trial. Participants needed 40 points to advance a level (rather than 50 in the previous study14) to allow for more forgiveness. Instead of beginning in the bottom level, participants were started in silver so they would feel the loss of dropping to bronze if they did not achieve enough points in the first week.
Fourth, we leveraged the fresh start effect, which is the tendency for aspirational behavior around temporal landmarks, such as the beginning of the year, month, or week.28 Similar to the prior trial,14 participants started each week with a fresh set of 70 points. A new component was added to help reengage participants who were struggling to meet their goals at weeks 8 and 16 (defined as being in the blue or bronze levels of the game). These participants were sent an email that stated that they would get a fresh start by being reset to the silver level and offered the opportunity to readjust their goals among the initial options.
Fifth, the game varied based on the social incentive arm, described as follows. In the support arm, participants were asked to identify a family member or friend who would be a support sponsor and be emailed a weekly report on the participant’s performance in the game, including points and level. This sponsor was sent a message at the start of the study to do their best to support the participant in their progress during the study.
In the collaboration arm, participants were placed into a team of 3 total participants. These participants typically did not know each other before the study but were introduced to each other by email. Each day, 1 of the members of the group was randomly selected to represent his or her team for that day and that information was shared with the entire group. If the selected participant met his or her step goal on the previous day, the team kept their points. If he or she did not meet the goal, then the entire team lost 10 points. In this design, each person is accountable to the others on the team, which may induce a collaborative effort to meet their daily goals. The entire team moved up a level only if the team had at least 40 points by the end of the week.
In the competition arm, participants were placed into a group of 3 total participants. These participants typically did not know each other before the study but were introduced to each other by email. At the end of each week, the participants received an email with a leaderboard that ranked them on their cumulative points in the study thus far and displayed their level. This feedback may have helped induce participants to compete for the top spot in their group.
Outcome Measures
The primary outcome was change in daily steps from baseline through the intervention period (weeks 5-24, which excludes the 4-week ramp-up phase). Secondary outcomes included the proportion of participant-days that step goals were achieved during the intervention and follow-up periods and change in daily steps from baseline to the follow-up period.
Statistical Analysis
A priori power calculations used a 2-phased testing procedure, which has an overall familywise error rate that is controlled at 0.05.29 In the first phase, the 3 intervention arms were compared with the control arm. We estimated that a sample of 600 participants (150 per arm) would provide at least 80% power to detect an 800-step difference between each intervention arm and the control arm. This approach assumed that the control group had mean daily steps of 6000, an SD of 2000 steps, a 10% dropout rate, and a conservative Bonferroni adjustment of the type I error rate with a 2-sided α of .017. In the second phase, only intervention arms that were significantly different from the control arm were compared with each other using a conservative Bonferroni adjustment of the type I error rate with a 2-sided α of .017 to adjust for up to 3 comparisons.
All randomly assigned participants were included in the intention-to-treat analysis. For each patient on each day of the study (participant-day level), the number of steps achieved was obtained as a continuous variable. These data were dichotomized at the participant-day level to create a binary variable that indicated whether each participant achieved his or her step goal, and this variable was used to estimate the proportion of participant-days that step goals were achieved.
Data are missing for any day that the participant did not use the wearable device or did not upload data. During the intervention period, missing step data rates ranged from 19% to 29% (eTable 1 in Supplement 2), which is similar to previous physical activity interventions.14,17,18,19,20,21 For the prespecified main analysis, we used multiple imputation for step values that were missing or for values less than 1000 steps per day. This method has been used in prior work14,17,18,19,20,21 and in this study because evidence indicates that daily step values less than 1000 may not represent full data capture.23,24 Five imputations were conducted using the mice package in R, version 3.4.0 (R Foundation for Statistical Computing), which allows for participant random effects with this data structure.30 The following determinants of missing data were included: study arm, week of study, calendar month, baseline step count, age, sex, race/ethnicity, educational level, marital status, annual household income, self-reported health, prior use of a smartphone or wearable device to track step counts, level of experience with wireless technology to track activity, regular travel to another city for work, and BMI. Results were combined using Rubin’s standard rules.31 This imputation approach has been used in prior work.14,17 Sensitivity analyses were conducted using collected data without multiple imputation, both with and without step values less than 1000.
Unadjusted analyses estimated mean daily steps for each month of the study by arm. Similar to prior work,14,17 adjusted analyses used PROC GLIMMIX in SAS, version 9.4 (SAS Institute Inc) to fit generalized mixed-effects models with a random intercept, to adjust for participant random effects, and to account for the repeated measures of daily step counts. In the main adjusted model, we included baseline step count and fixed effects for calendar month and study arm. To test the robustness of our findings, we fit a fully adjusted model that also included age, sex, race/ethnicity, marital status, annual household income, and BMI (calculated from self-reported height and weight). For change in steps, we assumed a normal distribution and obtained difference in steps between arms for the intervention and follow-up periods using the least squared means command. To estimate the adjusted difference in the proportion of participant-days that step goals were achieved between arms, we used the bootstrap method, resampling participants from within each arm 500 times. Determinants of success or failure in the interventions will be reported in the future.
Results
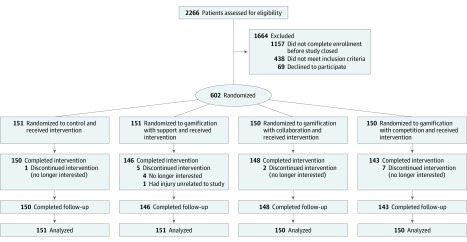
In this trial, 602 participants (mean [SD] age, 39 [10] years; mean [SD] BMI, 30 [5]; 427 [70.9%] male) from 40 states in the United States were randomized (Figure 1). Distribution of participants by US census region was similar across arms (eTable 2 in Supplement 2). Baseline participant characteristics were well balanced across the study arms (Table 1). Mean (SD) baseline daily steps were 6086 (2631) in the control arm, 6297 (2571) in the gamification with support arm, 6120 (2583) in the gamification with collaboration arm, and 6313 (2812) in the gamification with competition arm (P = .88). A total of 587 participants (97.5%) completed the entire 36-week study. No adverse events related to the interventions were reported during the entire trial.
Figure 1. CONSORT Diagram.
Participants in all arms used a wearable device to track daily step counts, established a baseline, and selected a step goal increase. Participants in the control arm received regular feedback from the wearable device and its smartphone application but no other interventions. Participants in the gamification arms were entered into the intervention that ran automatically during the first 24 weeks and then had no interventions during the 12-week follow-up period.
Table 1. Characteristics of the 602 Study Participantsa.
| Characteristic | Control (n = 151) | Gamification With Support (n = 151) | Gamification With Collaboration (n = 150) | Gamification With Competition (n = 150) | P Value |
|---|---|---|---|---|---|
| Sociodemographics | |||||
| Age, mean (SD), y | 38.5 (10.9) | 39.4 (10.1) | 38.3 (10.0) | 38.7 (10.0) | .70 |
| Male sex | 97 (64.2) | 110 (72.8) | 107 (71.3) | 113 (75.3) | .17 |
| Race/ethnicity | |||||
| White non-Hispanic | 72 (47.7) | 72 (47.7) | 81 (54.0) | 80 (53.3) | .74 |
| Black non-Hispanic | 10 (6.6) | 9 (6.0) | 5 (3.3) | 8 (5.3) | |
| Asian non-Hispanic | 49 (32.5) | 57 (37.7) | 48 (32.0) | 52 (34.7) | |
| Hispanic | 10 (6.6) | 7 (4.6) | 7 (4.7) | 3 (2.0) | |
| Other | 10 (6.6) | 6 (4.0) | 9 (6.0) | 7 (4.7) | |
| Educational level | |||||
| High school graduate | 1 (0.7) | 0 (0.0) | 1 (0.7) | 1 (0.7) | .86 |
| Some college or specialized training | 8 (5.3) | 5 (3.3) | 4 (2.7) | 6 (4.0) | |
| College graduate | 142 (94.0) | 146 (96.7) | 145 (96.7) | 143 (95.3) | |
| Marital status | |||||
| Single | 43 (28.5) | 31 (20.5) | 39 (26.0) | 38 (25.3) | .59 |
| Married | 102 (67.5) | 113 (74.8) | 102 (68.0) | 101 (67.3) | |
| Other | 6 (4.0) | 7 (4.6) | 9 (6.0) | 11 (7.3) | |
| Annual household income, $ | |||||
| <50 000 | 1 (0.7) | 1 (0.7) | 2 (1.3) | 1 (0.7) | .82 |
| 50 000-100 000 | 33 (21.9) | 29 (19.2) | 26 (17.3) | 36 (24.0) | |
| >100 000 | 117 (77.5) | 121 (80.1) | 122 (81.3) | 113 (75.3) | |
| Self-reported measures | |||||
| Health status | |||||
| Excellent | 6 (4.0) | 8 (5.3) | 5 (3.3) | 11 (7.3) | .16 |
| Very good | 43 (28.5) | 54 (35.8) | 46 (30.7) | 55 (36.7) | |
| Good | 84 (55.6) | 63 (41.7) | 69 (46) | 66 (44.0) | |
| Fair | 16 (10.6) | 22 (14.6) | 28 (18.7) | 18 (12.0) | |
| Poor | 2 (1.3) | 4 (2.6) | 2 (1.3) | 0 (0.0) | |
| Prior wearable device use | 89 (58.9) | 100 (66.2) | 94 (62.7) | 101 (67.3) | .42 |
| BMI, mean (SD) | 29.5 (4.1) | 29.2 (4.8) | 30.1 (5.7) | 29.7 (4.9) | .35 |
| Diabetes | 10 (6.6) | 4 (2.6) | 11 (7.3) | 5 (3.3) | .40 |
| Hyperlipidemia | 27 (17.9) | 22 (14.6) | 29 (19.3) | 27 (18) | .26 |
| Hypertension | 23 (15.2) | 16 (10.6) | 20 (13.3) | 17 (11.3) | .79 |
| Smoking actively | 5 (3.3) | 5 (3.3) | 7 (4.7) | 5 (3.3) | .90 |
| Physical activity measures | |||||
| Baseline daily steps, mean (SD) | 6086 (2631) | 6297 (2571) | 6120 (2583) | 6313 (2812) | .88 |
| Step goal selection | |||||
| 33% Increase from baseline | 64 (42.4) | 56 (37.1) | 56 (37.3) | 60 (40.0) | .33 |
| 40% Increase from baseline | 19 (12.6) | 14 (9.3) | 24 (16.0) | 20 (13.3) | |
| 50% Increase from baseline | 19 (12.6) | 31 (20.5) | 32 (21.3) | 22 (14.7) | |
| Custom goal at least 1500 steps greater than baseline | 49 (32.5) | 50 (33.1) | 38 (25.3) | 48 (32) | |
| Step goal increase from baseline, mean (SD) | 2144 (1160) | 2243 (923) | 2200 (980) | 2210 (1529) | .60 |
Abbreviation: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared).
Data are presented as number (percentage) of participants unless otherwise indicated.
Daily Step Counts
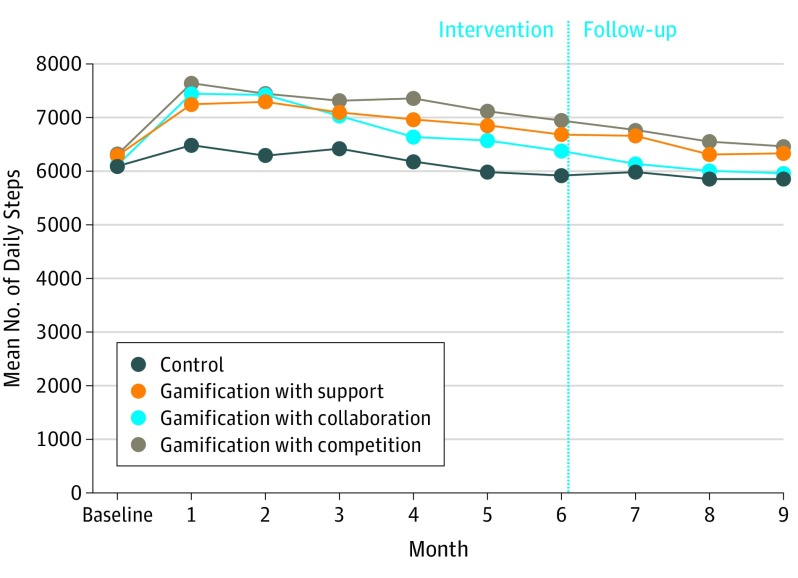
The unadjusted mean daily steps by month and study arm are depicted in Figure 2. The gamification with competition arm had the highest physical activity levels during the entire trial and had 1166 steps per day more than the control arm in month 1, 1022 steps per day more in month 6 (last intervention month), and 609 steps per day more in month 9 (end of follow-up). The gamification with support arm had 771 steps per day more than the control arm in month 1, remained steady with 760 steps per day more than the control arm in month 6, and declined to 476 steps per day more than the control arm in month 9. The gamification with collaboration arm had 979 steps per day more than the control arm in month 1, declined to 460 steps per day more than the control arm in month 6, and declined to 95 steps per day more than the control arm in month 9. Mean steps per day for the overall intervention and follow-up periods are depicted by arm in Table 2. Participants with lower baseline steps (<5000 steps per day or 5001-7500 steps per day) had greater increases in daily step counts than participants with higher baseline steps (eTable 3 in Supplement 2).
Figure 2. Unadjusted Mean Daily Steps by Month and Study Arm.
The mean daily steps for each arm by month using imputed data are shown. The vertical line separates the intervention period from the follow-up period.
Table 2. Adjusted Differences in Daily Steps Among the Study Arms.
| Variable | Control | Gamification With Support | Gamification With Collaboration | Gamification With Competition |
|---|---|---|---|---|
| Steps per day at baseline, mean (SD) | 6086 (2631) | 6297 (2571) | 6120 (2583) | 6313 (2812) |
| Steps per day in the main intervention period, mean (SD)a | 6162 (2142) | 6975 (2403) | 6814 (2197) | 7237 (2934) |
| Main adjusted modelb | ||||
| Difference compared with control and adjusted for baseline (95% CI) | NA | 689 (267 to 977) | 637 (258 to 1017) | 920 (513 to 1328) |
| P value | NA | <.001 | .001 | <.001 |
| Fully adjusted modelc | ||||
| Difference compared with control and adjusted for baseline (95% CI) | NA | 710 (316 to 1104) | 645 (262 to 1027) | 936 (516 to 1356) |
| P value | NA | <.001 | .001 | <.001 |
| Follow-up period | ||||
| Steps per day, mean (SD) | 5899 (2128) | 6432 (2320) | 6038 (1640) | 6592 (2685) |
| Main adjusted modelb | ||||
| Difference compared with control and adjusted for baseline (95% CI) | NA | 428 (19 to 837) | 126 (−235 to 488) | 569 (142 to 996) |
| P value | NA | .04 | .49 | .009 |
| Fully adjusted modelc | ||||
| Difference compared with control and adjusted for baseline (95% CI) | NA | 482 (71 to 893) | 110 (−248 to 468) | 553 (116 to 990) |
| P value | NA | .02 | .55 | .01 |
Abbreviation: NA, not applicable.
The main intervention period included weeks 5 to 24 and excluded the ramp-up phase. The follow-up period included weeks 25 to 36.
The main adjusted model adjusted for baseline step count and repeated measures and had fixed effects for calendar month and study arm.
The fully adjusted model also adjusted for age, sex, race/ethnicity, marital status, annual household income, and body mass index.
In the main adjusted model, compared with controls, participants had a significantly greater increase in mean daily steps from baseline in the competition arm (adjusted difference from control, 920; 95% CI, 513-1328; P < .001), support arm (adjusted difference from control, 689; 95% CI, 267-977; P < .001), and collaboration arm (adjusted difference from control, 637; 95% CI, 258-1017; P = .001) (Table 2). No significant differences were found among the gamification arms during the intervention period (eTable 4 in Supplement 2). During follow-up, physical activity in the competition arm remained significantly greater than that in the control arm (adjusted difference from control, 569; 95% CI, 142-996; P = .009) but was not significantly greater in the support (adjusted difference from control, 428; 95% CI, 19-837; P = .04) and collaboration (adjusted difference from control, 126; 95% CI, −248 to 468; P = .49) arms than the control arm. Results were similar in the fully adjusted model (Table 2) and in sensitivity analyses that used collected data without multiple imputation (eTable 5 and eTable 6 in Supplement 2).
Proportion of Participant-Days Goal Achieved
The unadjusted proportion of participant-days that step goals were achieved was 0.25 in the control arm, 0.36 in the gamification with support arm, 0.36 in the gamification with collaboration arm, and 0.41 in the gamification with competition arm. These levels were lower in the follow-up period at 0.23 in the control arm, 0.28 in the gamification with support arm, 0.26 in the gamification with collaboration arm, and 0.30 in the gamification with competition arm (Table 3).
Table 3. Adjusted Differences in the Proportion of Participant-Days That Step Goals Were Achieved.
| Variable | Control | Gamification With Support | Gamification With Collaboration | Gamification With Competition |
|---|---|---|---|---|
| Main Intervention Perioda | ||||
| Proportion of participant-days that step goal was achieved | 0.25 | 0.36 | 0.36 | 0.41 |
| Main adjusted modelb | ||||
| Difference relative to control (95% CI) | NA | 0.11 (0.10-0.13) | 0.11 (0.09-0.12) | 0.16 (0.14-0.18) |
| P value | NA | <.001 | <.001 | <.001 |
| Fully adjusted modelc | ||||
| Difference relative to control (95% CI) | NA | 0.11 (0.10-0.13) | 0.11 (0.09-0.12) | 0.16 (0.14-0.18) |
| P value | NA | <.001 | <.001 | <.001 |
| Follow-up Period | ||||
| Proportion of participant-days that step goal was achieved | 0.23 | 0.28 | 0.26 | 0.30 |
| Main adjusted modelb | ||||
| Difference relative to control (95% CI) | NA | 0.04 (0.03-0.06) | 0.03 (0.01-0.04) | 0.07 (0.06-0.09) |
| P value | NA | .04 | .10 | <.001 |
| Fully adjusted modelc | ||||
| Difference relative to control (95% CI) | NA | 0.04 (0.03-0.06) | 0.03 (0.01-0.04) | 0.07 (0.06-0.09) |
| P value | NA | .04 | .08 | .001 |
Abbreviation: NA, not applicable.
The main intervention period included weeks 5 to 24 and excluded the ramp-up phase. The follow-up period included weeks 25 to 36.
The main adjusted model adjusted for baseline step count and repeated measures and had fixed effects for calendar month and study arm.
The fully adjusted model also adjusted for age, sex, race/ethnicity, marital status, annual household income, and body mass index.
In the main adjusted model, compared with controls, participants had a significantly greater proportion of participant-days that step goals were achieved in the competition (adjusted difference from control, 0.16; 95% CI, 0.14-0.18; P < .001), support (adjusted difference from control, 0.11; 95% CI, 0.10-0.13; P < .001), and collaboration (adjusted difference from control, 0.11; 95% CI, 0.09-0.12; P < .001) arms. No significant differences were found among the gamification arms during the intervention period (eTable 7 in Supplement 2). In the follow-up period, participant-days that step goals were achieved were significantly different from control in only the competition arm (adjusted difference from control, 0.07; 95% CI, 0.06-0.09; P < .001). Results were similar in the fully adjusted model (Table 3) and in sensitivity analyses that used collected data without multiple imputation (eTable 8 and eTable 9 in Supplement 2).
Discussion
In this trial of overweight and obese adults across the United States, we found that gamification interventions with support, collaboration, and competition each significantly increased physical activity compared with the control group during the 24-week study period. Gamification with competition resulted in the greatest increases in physical activity and was the only intervention for which physical activity remained significantly greater than that for the control group during the 12-week follow-up period.
Our findings reveal several important insights that could be used to help improve future intervention design. First, a key aspect of our study design was incorporating principles from behavioral economics, such as precommitment, loss aversion, goal gradients, and the fresh start effect. To our knowledge, this was 1 of the first national evaluations of a behaviorally designed gamification intervention. Because gamification is often used within workplace wellness programs and digital health applications,6,7,8,9,10 incorporating these behavioral insights could improve intervention design to affect a broader population.
Second, most previous gamification interventions have been of shorter duration of 12 weeks or less.6,8,14,32 During our 24-week intervention, physical activity levels declined slowly in all arms; however, differences between the gamification with competition arm and the control arm were mostly steady (1166 steps per day more in month 1 and 1022 steps per day more in month 6). Gamification with support had a smaller magnitude difference but similar pattern of physical activity, whereas physical activity in the gamification with collaboration arm declined compared with control over time.
Third, our findings suggest that the effect of different social incentives may vary based on the social connection among participants. A prior randomized clinical trial14 found that gamification with collaboration led to significant increases in physical activity of 953 steps per day within families. Another trial33 found that a similar collaborative intervention among 2-person teams led to greater weight loss if the team members lived together than if they lived separately (10 vs 6 lb). However, in the STEP UP trial, participants did not previously know each other, and the collaboration intervention arm had the smallest increase in physical activity among the gamification arms. A study by Zhang and colleagues34 compared support with competition in a 4-week randomized clinical trial among college students in which their identities were kept anonymous. They also found that competition led to a greater effect on physical activity. This finding suggests that competition may be more effective than collaboration when participants do not have any preexisting social connections.
This study has several strengths, including its incorporation of insights from behavioral economics, scalable approach with remote monitoring through use of an automated technology platform and wearable devices, participation from adults in 40 states, longer duration compared with previous gamification interventions, and potential consequences given the already widespread use of gamification for promoting healthy behaviors. Of note, the interventions did not rely on participants previously knowing each other, which makes it a more scalable approach in some settings.
As indicated in the 2018 Physical Activity Guidelines, even small increases in physical activity can lead to health benefits.1 A recent study35 among older women found that higher daily step counts were associated with lower premature mortality in a dose-dependent relationship up until 7500 steps per day. The gamification interventions in this trial resulted in physical activity increases of approximately 600 to 900 steps per day during the 24-week period; however, step increases were higher among participants with a baseline of less than 7500 steps per day. Nonetheless, further work is needed to understand the clinical effect of these changes. Future research could evaluate the interventions for a longer duration, test approaches to better improve the sustainability of the interventions during follow-up, and consider investigating ways to match the most optimal social incentive design to each participant.
Limitations
This study has several limitations. First, participants were employed by a large consulting firm, were college educated, and needed access to a smartphone or tablet, which may limit generalizability. These interventions should be tested in other populations and settings. Second, participant eligibility criteria were based on self-report. Third, we evaluated physical activity using step counts and did not have data on other measures of physical activity or health outcomes. Recent evidence and the new physical activity guidelines indicate that even small increases in low-intensity physical activity provide health benefits1,2,3,4,5; however, moderate to vigorous physical activity provides greater benefit and should be evaluated in future studies. Fourth, we did not capture information on communications or interactions among the participants in groups in competition or collaboration and thus are unable to further evaluate these mechanisms. Fifth, this study followed up participants through 36 weeks. Although this is longer than most previous gamification interventions, future studies should evaluate the longer-term sustainability.
Conclusions
In a remotely monitored trial of overweight and obese adults across the United States, the groups receiving gamification interventions with support, collaboration, and competition each had significantly increased physical activity compared with the control group during the 24-week study period. Gamification with competition was the most effective during the intervention and was the only intervention for which physical activity was significantly greater than that for the control during the 12-week follow-up period. Physical activity increases during follow-up were modest, and these approaches should be tested in other populations. Gamification is commonly used in workplace wellness programs and digital health interventions.6,7,8,9,10 The results of the STEP UP trial indicate that small changes to the design of gamification can lead to important differences in effectiveness.
Trial Protocol
eTable 1. Missing data rates by arm and study period
eTable 2. Distribution of participants by arm and US Census Region.
eTable 3. Unadjusted changes in daily step by arm and baseline step count.
eTable 4. Adjusted differences in daily steps between the gamification arms using multiple imputation
eTable 5. Adjusted differences in daily steps without multiple imputation
eTable 6. Adjusted differences in daily steps without multiple imputation and excluding step values <1000
eTable 7. Adjusted differences in the proportion of participant-days step goals were achieved between the gamification arms using multiple imputation
eTable 8. Adjusted differences in the proportion of participant-days step goals were achieved without multiple imputation
eTable 9. Adjusted differences in the proportion of participant-days step goals were achieved without multiple imputation and excluding step values <1000
Data Sharing Statement
References
- 1.Piercy KL, Troiano RP, Ballard RM, et al. The physical activity guidelines for Americans. JAMA. 2018;320(19):2020-2028. doi: 10.1001/jama.2018.14854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thompson PD, Eijsvogels TMH. New physical activity guidelines. JAMA. 2018;320(19):1983-1984. doi: 10.1001/jama.2018.16070 [DOI] [PubMed] [Google Scholar]
- 3.Giroir BP, Wright D. Physical activity guidelines for health and prosperity in the United States. JAMA. 2018;320(19):1971-1972. doi: 10.1001/jama.2018.16998 [DOI] [PubMed] [Google Scholar]
- 4.Spartano NL, Davis-Plourde KL, Himali JJ, et al. Association of accelerometer-measured light-intensity physical activity with brain volume: the Framingham Heart Study. JAMA Netw Open. 2019;2(4):e192745-e192745. doi: 10.1001/jamanetworkopen.2019.2745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.LaCroix AZ, Bellettiere J, Rillamas-Sun E, et al. ; Women’s Health Initiative (WHI) . Association of light physical activity measured by accelerometry and incidence of coronary heart disease and cardiovascular disease in older women. JAMA Netw Open. 2019;2(3):e190419-e190419. doi: 10.1001/jamanetworkopen.2019.0419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Edwards EA, Lumsden J, Rivas C, et al. Gamification for health promotion. BMJ Open. 2016;6(10):e012447. doi: 10.1136/bmjopen-2016-012447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kawachi I. It’s all in the game: the uses of gamification to motivate behavior change. JAMA Intern Med. 2017;177(11):1593-1594. doi: 10.1001/jamainternmed.2017.4798 [DOI] [PubMed] [Google Scholar]
- 8.Sardi L, Idri A, Fernández-Alemán JL. A systematic review of gamification in e-Health. J Biomed Inform. 2017;71:31-48. doi: 10.1016/j.jbi.2017.05.011 [DOI] [PubMed] [Google Scholar]
- 9.Patel MS, Foschini L, Kurtzman GW, et al. Using wearable devices and smartphones to track physical activity. Ann Intern Med. 2017;167(10):755-757. doi: 10.7326/M17-1495 [DOI] [PubMed] [Google Scholar]
- 10.Cotton V, Patel MS. Gamification use and design in popular health and fitness mobile applications. Am J Health Promot. 2019;33(3):448-451. doi: 10.1177/0890117118790394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Conroy DE, Yang CH, Maher JP. Behavior change techniques in top-ranked mobile apps for physical activity. Am J Prev Med. 2014;46(6):649-652. doi: 10.1016/j.amepre.2014.01.010 [DOI] [PubMed] [Google Scholar]
- 12.Song Z, Baicker K. Effect of a workplace wellness program on employee health and economic outcomes. JAMA. 2019;321(15):1491-1501. doi: 10.1001/jama.2019.3307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Romeo A, Edney S, Plotnikoff R, et al. Can smartphone apps increase physical activity?. J Med Internet Res. 2019;21(3):e12053. doi: 10.2196/12053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patel MS, Benjamin EJ, Volpp KG, et al. Effect of a game-based intervention designed to enhance social incentives to increase physical activity among families. JAMA Intern Med. 2017;177(11):1586-1593. doi: 10.1001/jamainternmed.2017.3458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Asch DA, Volpp KG. On the way to health. LDI Issue Brief. 2012;17(9):1-4. [PubMed] [Google Scholar]
- 16.Harrison JD, Jones JM, Small DS, et al. Social incentives to encourage physical activity and understand predictors (STEP UP). Contemp Clin Trials. 2019;80:55-60. doi: 10.1016/j.cct.2019.04.001 [DOI] [PubMed] [Google Scholar]
- 17.Chokshi NP, Adusumalli S, Small DS, et al. Loss-framed financial incentives and personalized goal-setting to increase physical activity among ischemic heart disease patients using wearable devices. J Am Heart Assoc. 2018;7(12):e009173. doi: 10.1161/JAHA.118.009173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patel MS, Asch DA, Rosin R, et al. Individual versus team-based financial incentives to increase physical activity. J Gen Intern Med. 2016;31(7):746-754. doi: 10.1007/s11606-016-3627-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Patel MS, Asch DA, Rosin R, et al. Framing financial incentives to increase physical activity among overweight and obese adults. Ann Intern Med. 2016;164(6):385-394. doi: 10.7326/M15-1635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Patel MS, Volpp KG, Rosin R, et al. A randomized trial of social comparison feedback and financial incentives to increase physical activity. Am J Health Promot. 2016;30(6):416-424. doi: 10.1177/0890117116658195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patel MS, Volpp KG, Rosin R, et al. A randomized, controlled trial of lottery-based financial incentives to increase physical activity among overweight and obese adults. Am J Health Promot. 2018;32(7):1568-1575. doi: 10.1177/0890117118758932 [DOI] [PubMed] [Google Scholar]
- 22.Case MA, Burwick HA, Volpp KG, Patel MS. Accuracy of smartphone applications and wearable devices for tracking physical activity data. JAMA. 2015;313(6):625-626. doi: 10.1001/jama.2014.17841 [DOI] [PubMed] [Google Scholar]
- 23.Bassett DR Jr, Wyatt HR, Thompson H, Peters JC, Hill JO. Pedometer-measured physical activity and health behaviors in U.S. adults. Med Sci Sports Exerc. 2010;42(10):1819-1825. doi: 10.1249/MSS.0b013e3181dc2e54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kang M, Rowe DA, Barreira TV, Robinson TS, Mahar MT. Individual information-centered approach for handling physical activity missing data. Res Q Exerc Sport. 2009;80(2):131-137. doi: 10.1080/02701367.2009.10599546 [DOI] [PubMed] [Google Scholar]
- 25.Ariely D, Wertenbroch K. Procrastination, deadlines, and performance. Psychol Sci. 2002;13(3):219-224. doi: 10.1111/1467-9280.00441 [DOI] [PubMed] [Google Scholar]
- 26.Rogers T, Milkman KL, Volpp KG. Commitment devices: using initiatives to change behavior. JAMA. 2014;311(20):2065-2066. doi: 10.1001/jama.2014.3485 [DOI] [PubMed] [Google Scholar]
- 27.Kahneman D, Tversky A. Prospect theory: an analysis of decision under risk. Econometrica. 1979;47(2):263. doi: 10.2307/1914185 [DOI] [Google Scholar]
- 28.Dai H, Milkman KL, Riis J. The fresh start effect: temporal landmarks motivate aspirational behavior. Manage Sci. 2014;60(10):2563-2582. doi: 10.1287/mnsc.2014.1901 [DOI] [Google Scholar]
- 29.Burman CF, Sonesson C, Guilbaud O. A recycling framework for the construction of Bonferroni-based multiple tests. Stat Med. 2009;28(5):739-761. doi: 10.1002/sim.3513 [DOI] [PubMed] [Google Scholar]
- 30.Young R, Johnson DR. Handling missing values in longitudinal panel data with multiple imputation. J Marriage Fam. 2015;77(1):277-294. doi: 10.1111/jomf.12144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York, NY: Wiley; 1987. doi: 10.1002/9780470316696 [DOI] [Google Scholar]
- 32.Brown M, O’Neill N, van Woerden H, Eslambolchilar P, Jones M, John A. Gamification and adherence to web-based mental health interventions. JMIR Ment Health. 2016;3(3):e39. doi: 10.2196/mental.5710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kurtzman GW, Day SC, Small DS, et al. Social incentives and gamification to promote weight loss. J Gen Intern Med. 2018;33(10):1669-1675. doi: 10.1007/s11606-018-4552-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhang J, Brackbill D, Yang S, Becker J, Herbert N, Centola D. Support or competition? how online social networks increase physical activity. Prev Med Rep. 2016;4:453-458. doi: 10.1016/j.pmedr.2016.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lee I-M, Shiroma EJ, Kamada M, Bassett DR, Matthews CE, Buring JE. Association of step volume and intensity with all-cause mortality in older women [published online May 29, 2019]. JAMA Intern Med. 2019. doi: 10.1001/jamainternmed.2019.0899 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
eTable 1. Missing data rates by arm and study period
eTable 2. Distribution of participants by arm and US Census Region.
eTable 3. Unadjusted changes in daily step by arm and baseline step count.
eTable 4. Adjusted differences in daily steps between the gamification arms using multiple imputation
eTable 5. Adjusted differences in daily steps without multiple imputation
eTable 6. Adjusted differences in daily steps without multiple imputation and excluding step values <1000
eTable 7. Adjusted differences in the proportion of participant-days step goals were achieved between the gamification arms using multiple imputation
eTable 8. Adjusted differences in the proportion of participant-days step goals were achieved without multiple imputation
eTable 9. Adjusted differences in the proportion of participant-days step goals were achieved without multiple imputation and excluding step values <1000
Data Sharing Statement