This randomized clinical trial examines the effects of virtual reality education before chest radiography on anxiety and distress during the procedure among pediatric patients.
Key Points
Question
What is the effect of virtual reality education for pediatric patients on anxiety during chest radiography?
Findings
In this randomized clinical trial with 99 children, children assigned to receive virtual reality education before chest radiography had significantly lower anxiety and distress scores during the procedure compared with those assigned to a control group.
Meaning
Virtual reality education effectively relieves the distress of the radiography experience among pediatric patients.
Abstract
Importance
Pediatric patients often encounter anxiety and distress in hospital settings, and virtual reality education, providing a vivid, immersive, and realistic experience, has been introduced to mitigate these anxiety responses.
Objective
To evaluate whether virtual reality education for pediatric patients before chest radiography could reduce anxiety and distress in children and improve the radiographic process.
Design, Setting, and Participants
This prospective randomized clinical trial was conducted in a tertiary academic hospital in Seongnam, Republic of Korea. Participants (n = 112) were children aged 4 to 8 years who underwent chest radiography between July 20, 2018, and September 11, 2018. Analysis was performed from October 2, 2018, to April 23, 2019.
Interventions
Children were randomized to simple verbal instruction (control group) or 3-minute virtual reality education explaining the process of chest radiography in detail and leading to appropriate cooperation (virtual reality group).
Main Outcomes and Measures
The primary outcome was anxiety and distress among pediatric patients based on behavioral observations using the amended version of the Observational Scale of Behavioral Distress scale for radiology procedures (total score of 30, with a score <5 indicating less distressed and a score ≥5 indicating more distressed). Secondary outcomes were the need of parental presence, parental satisfaction score, procedure time, number of repeated images, and process difficulty score.
Results
Of 99 children included in the final analysis, 50 (50.5%) were allocated to the control group (mean [SD] age, 5.6 [1.2] years; 26 boys [52.0%]) and 49 (49.5%) to the virtual reality group (mean [SD] age, 5.8 [1.3] years; 32 boys [65.3%]). The mean (SD) score for anxiety and distress (2.0 [3.7] vs 5.0 [6.1]; mean difference, 3.0 [95% CI, 1.0-5.0]; P = .004), need for parental presence (8 cases with parents present [16.3%] vs 18 cases with parents present [36.0%]), and mean (SD) procedure time (55.1 [21.6] seconds vs 75.0 [42.0] seconds) were lower in the virtual reality group than in the control group. The mean (SD) score for parental satisfaction (9.4 [1.4] vs 8.6 [2.0]) was higher in the virtual reality group than in the control group.
Conclusions and Relevance
Virtual reality education before chest radiography improved the radiography experience among pediatric patients by reducing anxiety, distress, and procedure time while increasing parents’ satisfaction.
Trial Registration
UMIN Clinical Trials Registry: UMIN000030663
Introduction
Pediatric patients often experience fear and anxiety in unfamiliar hospital settings and during procedures. In radiology settings, the unfamiliar radiology room and large radiology machines may be intimidating to pediatric patients, resulting in anxiety and distress.1 Distress among pediatric patients in radiology settings may lead to stress behaviors, such as crying, moving, and flailing, which result in delay or cancellation of the radiographic process.2 The stressful nature of radiographic procedures for pediatric patients also may result in long-term effects, such as posttraumatic stress syndrome or avoidance of health care.1
Several methods, including sedation and distraction, have been attempted to reduce stress levels among pediatric patients at radiology departments.3,4 Sedation of pediatric patients may be associated with increased procedure and recovery times after the procedure.4 Moreover, sedation administration may be associated with increased risk of cardiovascular and respiratory complications, such as desaturation.5 Positive environmental distractions, such as physical environmental distractions, including artwork and gardens, have been provided in pediatric radiology settings; these interventions reduced stress and improved the outcome in pediatric patients undergoing radiographic examinations.3
Recently, virtual reality (VR) systems have been introduced in patient education to minimize anxiety and improve outcome.6,7 Previous investigations with VR experience or gamification about the preoperative process demonstrated a significant reduction of preoperative anxiety in pediatric patients.8 Virtual reality systems with 360° video can deliver information via a consistent, vivid, and immersive experience to pediatric patients without physical and financial limitations. High immersion and vivid experience are the main characteristics provided by VR technology, which can be used to educate pediatric patients.7 Thus, it was hypothesized that VR education about the radiographic process before the imaging procedure could reduce anxiety and distress in pediatric patients. This study was designed to evaluate the effects of VR education about chest radiography on anxiety and distress among pediatric patients and on the efficiency of the radiographic procedure.
Methods
Study
The protocol of this prospective randomized clinical trial (Supplement 1) was approved by the institutional review board of Seoul National University Bundang Hospital. Written informed consent was obtained from all parents or guardians, and children aged 7 years or older signed additional agreements directly after receiving detailed instructions with their parents or guardians. This study was conducted at the Seoul National University Bundang Hospital between July 20, 2018, and September 11, 2018. Analysis was performed from October 2, 2018, to April 23, 2019.
Patients
A total of 100 children with American Society of Anesthesiology physical status of I or II who were aged 4 to 8 years and undergoing chest radiography were enrolled in this study. Children with a history of prematurity or congenital disease, hearing impairment, cognitive deficits or cognitive and intellectual developmental disabilities, history of epilepsy or seizure taking psychoactive medications, history of epilepsy or seizure, and prior experience of chest radiography during the past 1 year were excluded from the study.
Randomization and Intervention
The children were randomized to the control or VR group via a computer-generated randomization code (Random Allocation Software, version 1.0; Isfahan University of Medical Sciences) by an independent researcher who was only responsible for patient assignment 10 minutes before chest radiography. An opaque envelope containing sequential numbers was transferred to another researcher, and the intervention was performed in a separated area 5 minutes before entering the radiography room. The blinded researcher observed the child and evaluated the Observational Scale of Behavioral Distress (OSBD) scale (described below) in the radiography room during the chest radiography process. The child and parents or guardians were not blinded to the intervention, whereas the evaluator and the radiology technologist were blinded to the assignment.
For pediatric patients in the control group, chest radiography was performed with usual simple verbal instructions for chest radiography. Children in the VR group received a 3-minute VR educational presentation regarding the radiologic process with a head-mounted VR display.
Virtual Reality Experience of the Radiography Room
The VR experience was provided as a 360°, 3-dimensional virtual environment that introduced and explained the process of chest radiography. All equipment and machines of the radiography room were measured, and 3-dimensional rendering was performed with graphic work. The script of the VR video on the radiographic process was written by radiology technologists and anesthesiologists (J.-W.P., S.-H.H) from Seoul National University Bundang Hospital and was revised by the pediatric psychiatrist (H.-J.Y.). The 3-minute video was produced in collaboration with a VR producing company (JSC Games, Seoul, Republic of Korea). Chatan and Ace, famous animation characters of the animated film “Hello Carbot” (ChoiRock Contents Factory, Seoul, Republic of Korea), explained the process of chest radiography in detail (Figure 1A), encouraging children to cooperate appropriately. Permission to use these animation characters had been obtained (licensing agreement with ChoiRock Contents Factory). In the VR video, pediatric patients experienced the process of chest radiography with Chatan and Ace. They were asked to enter and experience a radiography room. Children learned how to position themselves in front of a radiography machine (Figure 1B) and were encouraged to take a deep breath and to cooperate appropriately without anxiety. A head-mounted VR display, Oculus Go (Oculus VR), was used to participate in the VR video (Figure 1C).
Figure 1. Virtual Reality (VR) Experience of the Radiography Room.
Outcome Measurement
Children’s stress and anxiety during the radiography process was measured with the amended version of an OSBD scale for radiographic procedures by a blinded single evaluator to exclude any possible interrater bias.9,10,11 The OSBD was originally developed for use with children requiring bone marrow aspiration9 and has been widely used to assess various children's procedural pain and distress, with good interrater reliability.10 The OSBD scale included 11 operationally defined behaviors indicative of distress, including crying, clinging, fear, restraint, and screaming.9 The total score of the OSBD scale was 30, and the OSBD scores were dichotomized at 5 and stratified into 2 categories (more distressed and less distressed) for the purpose of the analysis. Less distressed was defined as an OSBD score of less than 5 on the basis of a previous study that used the amended OSBD score.11
The radiology technologist asked the child before the entrance to the radiography room whether the child wanted to be with his or her parent during the radiographic process. Parental presence was also decided during the process of chest radiography whenever the child wanted parental presence. The incidence of parental presence was counted. Parents’ or guardians’ satisfaction scores about the overall process of chest radiography using a numerical rating scale (0, very dissatisfied; 10, very satisfied) were also recorded.
The time for the radiographic procedure (time from entering the radiography room to the production of a chest radiographic image) and the number of repeated procedures were recorded by a blinded single evaluator. After the chest radiograph was obtained, the radiology technologist scored the level of difficulty of the chest radiographic imaging for each child using a numerical rating scale (0, very difficult; 10, very easy).
Statistical Analysis
Power analysis was performed using G*Power software, version 3.1.2 (Heinrich Heine University). A previous study reported that the incidence of stress and anxiety during the radiographic process was 53% in children based on the amended OSBD.11 A relative reduction of 50% of the incidence of stress and anxiety during the radiographic process was considered to be clinically significant with respect to the effect of VR education. A sample size of 50 children per group was determined using a power of 0.8, significance level of .05, and 10% dropout rate. SPSS, version 21.0 (SPSS Inc) was used for all statistical analyses. Baseline characteristics were compared between groups. Continuous data are presented as means (SDs), and categorical variables are shown as number (percentage). An independent t test was used to analyze continuous variables, and a χ2 test or Fisher exact test was used to analyze categorical variables. A full analysis set was used for data analysis. All of the reported P values were 2-sided, and P < .05 was considered to indicate statistical significance.
Results
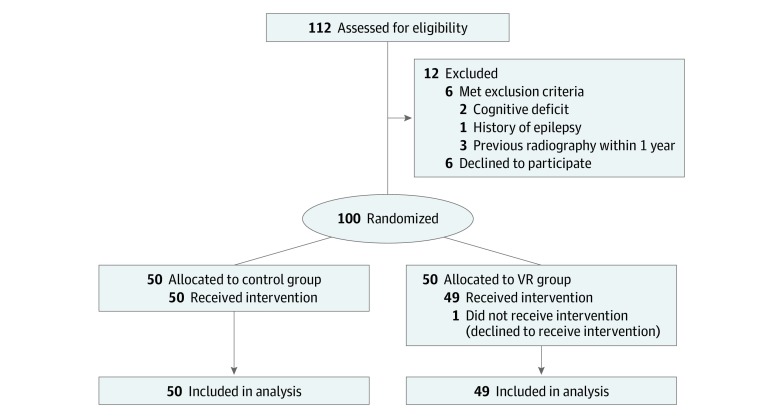
Of the 112 children assessed on the day of chest radiography, 12 patients were excluded (6 children declined to participate, and 6 children did not meet the inclusion criteria). A total of 100 children participated in this study, 50 of whom were randomly assigned to the control group and 50 to the VR group. Among them, 1 child in the VR group refused to participate during the intervention on the day of chest radiography owing to a scheduling conflict; thus, data for 99 children were included in the final analysis (Figure 2).
Figure 2. CONSORT Flow Diagram.
VR indicates virtual reality education.
Baseline characteristics were similar between the groups. The mean (SD) age of the children was 5.6 (1.2) years in the control group and 5.8 (1.3) years in the VR group. The number of boys was 26 (52.0%) in the control group and 32 (65.3%) in the VR group. Mean (SD) weight (19.7 [5.9] kg in the control group; 22.1 [8.0] kg in the VR group) and height (106.5 [17.1] cm in the control group; 110.4 [17.6] cm in the VR group) were comparable between the 2 groups. Reasons for chest radiography were respiratory and/or cardiovascular symptoms (21 in the control group; 19 in the VR group) or preoperative workup (29 in the control group; 30 in the VR group).
The number of less distressed children (OSBD score, <5) was significantly higher in the VR group (38 [77.6%]) than in the control group (26 [52.0%]), and the degree of stress and anxiety measured with the amended version of the OSBD scale was significantly lower in the VR group than in the control group (mean [SD] OSBD score, 2.0 [3.7] vs 5.0 [6.1]; mean difference, 3.0 [95% CI, 1.0 to 5.0]) (Table).
Table. Analysis of Primary and Seconday Outcomes.
| Outcome | Control Group (n = 50) | Virtual Reality Group (n = 49) | Mean Difference (95% CI) | Risk Ratio (95% CI) | P Value |
|---|---|---|---|---|---|
| Primary Outcomes | |||||
| OSBD category, No. (%)a | |||||
| More distressed | 24 (48.0) | 11 (22.4) | NA | 0.3 (0.1 to 0.7) | .008 |
| Less distressed | 26 (52.0) | 38 (77.6) | NA | ||
| OSBD score, mean (SD) | 5.0 (6.1) | 2.0 (3.7) | 3.0 (1.0 to 5.0) | NA | .004 |
| Secondary Outcomes | |||||
| Parental presence, No. (%) | 18 (36.0) | 8 (16.3) | NA | 0.3 (0.1 to 0.9) | NA |
| Parental satisfaction score, mean (SD) | 8.6 (2.0) | 9.4 (1.4) | −0.8 (−1.5 to −0.1) | NA | NA |
| Time for radiography procedure, mean (SD), s | 75.0 (42.0) | 55.1 (21.6) | 19.9 (6.6 to 33.3) | NA | NA |
| Repeated procedure, No. (%) | 8 (16.0) | 4 (8.2) | NA | 0.5 (0.1 to 1.7) | NA |
| Process difficulty score, mean (SD) | 8.7 (1.8) | 9.2 (1.4) | −0.5 (−1.2 to 0.2) | NA | NA |
Abbreviations: NA, not applicable; OSBD, Observational Scale of Behavioral Distress.
More distressed was indicated by a score of 5 or higher; less distressed, less than 5.
The need for parental presence was lower (8 [16.3%] in the VR group; 18 [36.0%] in the control group) and the mean (SD) parental satisfaction scores (9.4 [1.4] in the VR group; 8.6 [2.0] in the control group) were higher in the VR group than in the control group (Table). The mean (SD) procedure time for chest radiography was shorter in the VR group (55.1 [21.6] seconds) than in the control group (75.0 [42.0] seconds). The number of repeated chest radiographic procedures (4 [8.2%] in the VR group; 8 [16.0%] in the control group) and the mean (SD) difficulty score (9.2 [1.4] in the VR group; 8.7 [1.8] in the control group) measured by a radiologic technologist were comparable between the 2 groups (Table).
Discussion
This is the first clinical trial, to our knowledge, to show the outcome of using VR technology to educate pediatric patients scheduled for chest radiography with respect to measuring their anxiety and stress levels. The findings of this randomized clinical trial suggest that preprocedural VR education reduces anxiety and stress levels in children, which in turn reduces the time required for the overall chest radiographic procedure. In addition, parental satisfaction regarding the overall process of chest radiography was increased after VR education for chest radiography.
Pediatric patients often experience fear and anxiety in a variety of health care settings, including examinations, procedures, and operations, because of the strange, sterile environment.1 Severe distress may lead to physiologic and psychological responses in pediatric patients, causing delays and difficulty in performing the procedure. In the current study, distress and anxiety in pediatric patients were evaluated with the amended version of the OSBD scale for radiographic procedures, which is a behavioral assessment tool.9 The scores on the OSBD scale were classified into 2 categories (more distressed and less distressed) for the purpose of this analysis. Less distressed was defined as an OSBD score of less than 5, and a higher proportion of children with a VR education were in this category compared with the control group. These effects of reduced anxiety may be attributed to familiarity and exposure to the strange environment through VR education, a finding consistent with previous investigations in pediatric patients undergoing surgery.6
Parents are often required to accompany their child during the radiographic process because of the child’s anxiety, but the presence of the parents may lead to unnecessary radiographic environmental exposure. The need for parental presence was lower in the VR group, and the satisfaction score of the parents in this group was higher than in the control group. Through reducing anxiety in children and parents, immersive and vivid VR education before a radiographic procedure was effectively able to increase parental satisfaction and reduce unnecessary exposure to the radiographic environment for parents.
Radiology technologists could be often distracted by stressful pediatric patients, reducing their focus. Radiographic procedure time was approximately 20 seconds less in the VR group than in the control group. This result may be attributed to higher compliance in the VR group than in the control group during the procedure despite the comparable difficulty score between the 2 groups. The radiographic procedure time and number of repeated images taken were associated with efficiency and radiation exposure in children and the radiology technologist. The number of repeated procedures in the control group (16%) was twice that in the VR group (8%).
This study included children aged 4 to 8 years. At 4 years of age, children are able to discriminate between reality and fantasy and to play with objects in a symbolic way.12 Therefore, it was assumed that they could understand that the VR contents were not real and that the VR contents were symbolic materials replacing imaginary play in the real world. In addition, anxiety and fear about body damage is evident in preschool ages because their capacities of imagination expanded markedly,12 and therefore, psychological preparation for medical procedures is needed especially for this age.
Data from 1 child in the VR group were excluded from the analysis. After the written consent and randomization, the parent of the child refused to participate in the study owing to her personal schedule, and chest radiography was performed for the child without any intervention. In the present study, a total of 10 minutes was spent on randomization and intervention before chest radiography. In the clinical setting, 10 minutes of preparation including 3 minutes of the intervention may be considered to be long to manage at times.
Limitations
There are some limitations to be considered. First, this study was performed with chest radiography, a painless and noninvasive diagnostic procedure, because this is the most common procedure in pediatric radiology. More investigations with VR education are needed with pediatric patients undergoing computed tomography or magnetic resonance imaging, which frequently require sedation. Second, instead of a standard education video, VR education was used for the current study because the main characteristics offered by the VR technology are the high immersion and real-time interaction.7 The addition of another intervention group, with a standard video that features the same character as in the VR content, could investigate the effect of VR on anxiety during chest radiography. Third, the VR content of the current study was produced with a male character in Korean. However, gender-specific or gender-neutral contents in multiple languages using dubbing would be needed to apply this VR intervention to children in clinical settings because gender role is sensitive at preschool age13 and it is difficult to manage the procedural anxiety across different languages. Fourth, parents were not blinded to the intervention, and therefore, it is possible that parents’ and guardians’ satisfaction scores may have social desirability bias.
Conclusions
The immersive and vivid VR education before chest radiography was effective in improving anxiety in children, parental satisfaction, and procedure time in pediatric patients. The result of this study may be widely applied and extended to research with a broader patient population. Further studies with VR education are needed with pediatric patients undergoing computed tomography or magnetic resonance imaging, which frequently require sedation, to better understand the efficacy of the intervention in reducing anxiety and distress in pediatric radiology.
Trial Protocol
Data Sharing Statement
References
- 1.Alexander M. Managing patient stress in pediatric radiology. Radiol Technol. 2012;83(6):549-560. [PubMed] [Google Scholar]
- 2.Tyson ME, Bohl DD, Blickman JG. A randomized controlled trial: child life services in pediatric imaging. Pediatr Radiol. 2014;44(11):1426-1432. doi: 10.1007/s00247-014-3005-1 [DOI] [PubMed] [Google Scholar]
- 3.Quan X, Joseph A, Nanda U, et al. Improving pediatric radiography patient stress, mood, and parental satisfaction through positive environmental distractions: a randomized control trial. J Pediatr Nurs. 2016;31(1):e11-e22. doi: 10.1016/j.pedn.2015.08.004 [DOI] [PubMed] [Google Scholar]
- 4.Etzel-Hardman D, Kapsin K, Jones S, Churilla H. Sedation reduction in a pediatric radiology department. J Healthc Qual. 2009;31(4):34-39. doi: 10.1111/j.1945-1474.2009.00035.x [DOI] [PubMed] [Google Scholar]
- 5.Sanborn PA, Michna E, Zurakowski D, et al. Adverse cardiovascular and respiratory events during sedation of pediatric patients for imaging examinations. Radiology. 2005;237(1):288-294. doi: 10.1148/radiol.2371041415 [DOI] [PubMed] [Google Scholar]
- 6.Ryu JH, Park SJ, Park JW, et al. Randomized clinical trial of immersive virtual reality tour of the operating theatre in children before anaesthesia. Br J Surg. 2017;104(12):1628-1633. doi: 10.1002/bjs.10684 [DOI] [PubMed] [Google Scholar]
- 7.Willaert WI, Aggarwal R, Van Herzeele I, Cheshire NJ, Vermassen FE. Recent advancements in medical simulation: patient-specific virtual reality simulation. World J Surg. 2012;36(7):1703-1712. doi: 10.1007/s00268-012-1489-0 [DOI] [PubMed] [Google Scholar]
- 8.Ryu JH, Park JW, Nahm FS, et al. The effect of gamification through a virtual reality on preoperative anxiety in pediatric patients undergoing general anesthesia: a prospective, randomized, and controlled trial. J Clin Med. 2018;7(9):E284. doi: 10.3390/jcm7090284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blount RL, Loiselle KA. Behavioural assessment of pediatric pain. Pain Res Manag. 2009;14(1):47-52. doi: 10.1155/2009/348184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tucker CL, Slifer KJ, Dahlquist LM. Reliability and validity of the brief behavioral distress scale: a measure of children’s distress during invasive medical procedures. J Pediatr Psychol. 2001;26(8):513-523. doi: 10.1093/jpepsy/26.8.513 [DOI] [PubMed] [Google Scholar]
- 11.Bradford R. Short communication: the importance of psychosocial factors in understanding child distress during routine X-ray procedures. J Child Psychol Psychiatry. 1990;31(6):973-982. doi: 10.1111/j.1469-7610.1990.tb00838.x [DOI] [PubMed] [Google Scholar]
- 12.Martin A, Volkmar FR, Lewis M. Lewis’s Child and Adolescent Psychiatry: A Comprehensive Textbook. Baltimore, MD: Lippincott Williams & Wilkins; 2007. [Google Scholar]
- 13.Cherney ID, London K. Gender-linked differences in the toys, television shows, computer games, and outdoor activities of 5-to 13-year-old children. Sex Roles. 2006;54(9-10):717-726. doi: 10.1007/s11199-006-9037-8 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
Data Sharing Statement