Key Points
Question
Are positive childhood experiences (PCEs) associated with adult depression and/or poor mental health (D/PMH) and adult-reported social and emotional support (ARSES) independent from adverse childhood experiences (ACEs)?
Findings
In this cross-sectional study, adults reporting higher PCEs had lower odds of D/PMH and greater ARSES after accounting for ACEs. The associations of PCEs with D/PMH also remained stable when controlling for ARSES.
Meaning
Positive childhood experiences demonstrate a dose-response association with adult D/PMH and ARSES after adjustment for ACEs; assessing and proactively promoting PCEs may reduce adult mental and relational health problems, even in the concurrent presence of ACEs.
Abstract
Importance
Associations between adverse childhood experiences (ACEs) and risks for adult depression, poor mental health, and insufficient social and emotional support have been documented. Less is known about how positive childhood experiences (PCEs) co-occur with and may modulate the effect of ACEs on adult mental and relational health.
Objective
To evaluate associations between adult-reported PCEs and (1) adult depression and/or poor mental health (D/PMH) and (2) adult-reported social and emotional support (ARSES) across ACEs exposure levels.
Design, Setting, and Participants
Data were from the cross-sectional 2015 Wisconsin Behavioral Risk Factor Survey, a random digit-dial telephone survey of noninstitutionalized Wisconsin adults 18 years and older (n = 6188). Data were weighted to be representative of the entire population of Wisconsin adults in 2015. Data were analyzed between September 2016 and January 2019.
Main Outcomes and Measures
The definition of D/PMH includes adults with a depression diagnosis (ever) and/or 14 or more poor mental health days in the past month. The definition of PCEs includes 7 positive interpersonal experiences with family, friends, and in school/the community. Standard Behavioral Risk Factor Survey ACEs and ARSES variables were used.
Results
In the 2015 Wisconsin Behavioral Risk Factor Survey sample of adults (50.7% women; 84.9% white), the adjusted odds of D/PMH were 72% lower (OR, 0.28; 95% CI, 0.21-0.39) for adults reporting 6 to 7 vs 0 to 2 PCEs (12.6% vs 48.2%). Odds were 50% lower (OR, 0.50; 95% CI, 0.36-0.69) for those reporting 3 to 5 vs 0 to 2 PCEs (25.1% vs 48.2%). Associations were similar in magnitude for adults reporting 1, 2 to 3, or 4 to 8 ACEs. The adjusted odds that adults reported “always” on the ARSES variable were 3.53 times (95% CI, 2.60-4.80) greater for adults with 6 to 7 vs 0 to 2 PCEs. Associations for 3 to 5 PCEs were not significant. The PCE associations with D/PMH remained stable across each ACEs exposure level when controlling for ARSES.
Conclusions and Relevance
Positive childhood experiences show dose-response associations with D/PMH and ARSES after accounting for exposure to ACEs. The proactive promotion of PCEs for children may reduce risk for adult D/PMH and promote adult relational health. Joint assessment of PCEs and ACEs may better target needs and interventions and enable a focus on building strengths to promote well-being. Findings support prioritizing possibilities to foster safe, stable nurturing relationships for children that consider the health outcomes of positive experiences.
This study evaluates associations between adult-reported positive childhood experiences and adult depression and/or poor mental health as well as reported social and emotional support across adverse childhood experience exposures levels.
Introduction
Research demonstrates that both positive and adverse experiences shape brain development and health across the life span.1,2,3,4,5. Understanding human development requires a model that incorporates both risks (factors that decrease the likelihood of successful development) and opportunities (factors that increase the likelihood of successful development). On the positive side, successful child development depends on secure attachment during the first years of life.6,7 As the child grows, exposure to spoken language8 and having the presence of safe, stable, nurturing relationships and environments are important factors for optimal development.9,10 On the other hand, children with adverse childhood experiences (ACEs) are at risk for observable changes in brain anatomy,11 gene expression,12,13 and delays in social, emotional, physical, and cognitive development lasting into adulthood.3,4,5,14,15,16,17
According to standardized measures, an estimated 61.5% of adults18 and 48% of children19 in the United States have been exposed to ACEs, with more than one-third of these having multiple exposures.18,19 The wide-ranging negative associations between exposure to multiple ACEs and diminished adult and child health are well documented.14,19,20,21,22 Most notable is the especially strong evidence linking ACEs with adult mental health problems including depression.22,23,24,25,26,27,28 A robust literature also exists regarding the effect of ACEs on adult relational health (often assessed by whether adults report that they get the social and emotional support they need) and how diminished adult social and emotional support contributes to poorer adult physical and mental health.29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56
Beyond the extensive and growing body of research dealing with lifelong correlates of adversity, many prior studies identify resiliency factors and adaptive skills and interventions associated with improved child development and child and adult health outcomes.2,3,16,17,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55 For example, the Search Institute developed a list of “40 Developmental Assets” and demonstrated associations between the number of assets and both positive and negative outcomes.52 A national population-based study53 on child flourishing and resilience shows strong associations with levels of family resilience and parent-child connection for children with exposures to greater ACEs, poverty, and chronic conditions. Similar studies, such as those assessing the US Centers for Disease Control and Prevention (CDC)’s “safe, stable, and nurturing relationships” model, show similar findings.55
Despite these advances, standardized measures and the prevalence of positive childhood experiences (PCEs) at the population level for adults or children are still unknown. Yet prior studies, using data from small or nonrepresentative samples, have explored interactions between PCEs and ACEs.25,41,56 For example, 1 study,41 conducted by Kaiser Permanente and CDC investigators, analyzed a cohort of 4648 women. They found that adult reports of specific positive family experiences in childhood (including closeness, support, loyalty, protection, love, importance, and responsiveness to health needs) were associated with lower rates of adolescent pregnancy across all ACEs exposure levels.41 The protective effects of reported interpersonal PCEs against mental health problems in adulthood have also been found among pregnant women25 and young adults56 exposed to ACEs. Despite these findings, few subsequent studies on ACEs have simultaneously evaluated PCEs.
Collectively, prior studies on child development point to the importance of research focusing on PCEs, especially those associated with parent-child attachment, positive parenting (eg, parental warmth, responsiveness, and support), family health, and positive relationships with friends, in school, and in the community. Knowledge of whether retrospectively reported PCEs co-occur with ACEs and how PCEs interact with ACEs to effect adult mental and relational health is needed to inform the nation’s growing focus on addressing early life and social determinants of healthy development and lifelong health.
This study used data from the 2015 Wisconsin Behavioral Risk Factor Survey (WI BRFS), a representative, population-based survey,57 to assess the prevalence of PCEs in an adult sample and evaluate hypothesized associations with adult mental and relational health across 4 ACEs exposure levels. This study builds on a 2017 Health Outcomes of Positive Experiences report58 featuring bivariate findings from the 2015 WI BRFS associating individual PCEs with negative adult health outcomes. Here, we construct a PCEs cumulative score measure and use multivariable regression methods to assess the magnitude and significance of associations between this PCEs score and (1) adult depression and/or poor mental health (D/PMH) and (2) adults’ reported social and emotional support (ARSES). Separate assessment of associations was conducted for each of 4 ACEs exposure levels.
Methods
Population and Data
Data were from the cross-sectional 2015 WI BRFS, a representative, telephone survey of noninstitutionalized Wisconsin adults 18 years and older who speak English or Spanish (n = 6188).57 The WI BRFS response rate was 45.0% (weighted American Association of Public Opinion Research median, 47.2%). The cooperation rate was 64.9% (weighted American Association of Public Opinion Research median, 68.0%). The 2015 WI BRFS core and state-added items data sets were linked. Institutional review board (IRB) approval was not required because data are based on a survey conducted by a public agency and do not include personal health information. Respondent oral consent methods and construction of race/ethnicity variables used standard CDC BRFS approved methods.
There were 18.1% to 21.1% missing cases for state-added ARSES, ACEs, and PCEs items. “Don’t know/refused” responses to these questions were 0.2% to 0.9%. A 10% missing value rate for the WI BRFS state-added items is expected and is attributed to the administration of the core WI BRFS survey by another state to Wisconsin residents who have out-of-state cellular phones. In these cases, the WI BRFS state-added items were not available to be administered.59 The remainder of missing cases were nearly all owing to respondent dropoffs prior to administering the ARSES, ACEs, and PCEs questions after administration of the core WI BRFS. Differences in D/PMH prevalence rates between respondents and missing cases were not notable. See eTable 1 in the Supplement for additional details.
Key Measures
Positive Childhood Experiences Score
The PCEs score included 7 items asking respondents to report how often or how much as a child they: (1) felt able to talk to their family about feelings; (2) felt their family stood by them during difficult times; (3) enjoyed participating in community traditions; (4) felt a sense of belonging in high school (not including those who did not attend school or were home schooled); (5) felt supported by friends; (6) had at least 2 nonparent adults who took genuine interest in them; and (7) felt safe and protected by an adult in their home. The PCEs score items were adapted from 4 subscales included in the Child and Youth Resilience Measure–28 60: (1) 4 items from the Psychological, Caregiving subscale (see PCEs items 1, 2, 7, and 6 listed previously); (2) 1 from the Education subscale (PCEs item 4); (3) 1 from the Culture subscale (PCEs item 3), and (4) 1 from the Peer Support subscale (PCEs item 5). Items were designed in the Child and Youth Resilience Measure–28 for cultural sensitivity, and their validity was supported by associations with improved resilience.61 Psychometric analyses confirmed use of a PCEs cumulative score. See eTable 2 in the Supplement for details.
Adverse Childhood Experiences
We used data from the standardized ACEs survey items defined by the CDC.62,63 The ACEs measure included 11 ACEs items assessing recollections of childhood experiences of physical or emotional abuse or neglect, sexual abuse, and household dysfunctions such as substance abuse, parental incarceration, and divorce. As recommended by the CDC, items were coded using cumulative score groupings of 0, 1, 2 to 3, or 4 to 8 ACEs. Subjective reports of experiences in childhood are the intended construct for assessment of both PCEs and ACEs and not whether what is reported would be validated using objective assessments.64
Adult-Reported Social and Emotional Support
Adult-reported social and emotional support is assessed using a standardized single item, “How often do you get the social and emotional support you need?” Response choices were “always,” “usually,” “sometimes,” “rarely,” or “never.” Based on previous research and analysis of this ARSES variable, this study separately evaluated “always” and “usually” responses and created a combined “sometimes/rarely/never” response category.45,47,48
Depression/Poor Mental Health
The D/PMH category was constructed using (1) the single item on depression asking whether a physician or other health professional “ever told you that you have a depressive disorder, including depression, major depression, dysthymia, or minor depression?”; and (2) a score of 14 or higher on the single item validated as an indicator of current poor mental health59,60,65,66 that asked, “Now thinking about your mental health, which includes stress, depression, and problems with emotions, for how many days during the past 30 days was your mental health not good?” Adults reporting either or both of these outcomes were included in the D/PMH variable.
Other Covariates
Demographic covariates included age (18-34 years, 35-54 years, 55-64 years, and 65 years or older), race/ethnicity (nonwhite or white/non-Hispanic), and annual income (less than $25 000, $25 000-$49 999, $50 000-$74 999, and $75 000 or more). Sample size and statistical power analysis findings required combining race/ethnicity subgroups into 2 categories for purposes of statistical analysis.
Analytic Methods
Prevalence rates for all variables were computed, and bivariate associations between individual PCE items and PCEs cumulative score groups and all other variables were evaluated using χ2 tests. Iterative and recursive analyses confirmed independent variable construction and focused on confirmation of assumptions on the linearity and comparability of associations with study outcomes when ordinal (count) or cumulative score groupings of PCEs and ACEs were used. Cumulative score groups of 0 to 2, 3 to 5, and 6 to 7 PCEs and 0, 1, 2 to 3, and 4 to 8 ACEs were also selected to ensure adequate statistical power to detect meaningful associations. Such score groups also simplify reporting of results by narrowing the number of comparative groups requiring reporting. Interaction variables crossing PCEs by ACEs and PCEs by ARSES were also analyzed for each study outcome and supported decisions to assess PCEs, ACEs, and ARSES as independent (vs interacting) variables in regression models.
As noted, multivariable logistic regression analyses evaluated 2 association pathways between PCEs items and cumulative score groups and 2 outcome variables: (1) meeting criteria for D/PMH and (2) reports of “always” on ARSES. Regression models were adjusted for age, sex, race/ethnicity, income, and ACEs. Separate models were evaluated for each ACEs exposure level (0, 1, 2-3, and 4-8) to examine stability of associations across ACEs exposure levels. We further assessed the stability of associations between D/PMH and PCEs when ARSES were or were not controlled for in regression models. This was done to further understand more nuanced association pathways between PCEs and ARSES and their individual or interacting association with D/MPH. Additional sensitivity analyses of PCEs associations when ACEs were or were not included in models were also conducted. The survey data were weighted to be representative of the Wisconsin population. We used SPSS Complex Samples, version 24 (IBM Corporation) for data analysis.67 A P value of .05 or less was used to determine statistical significance.
Results
Population Characteristics and Prevalence of Study Outcomes by PCEs
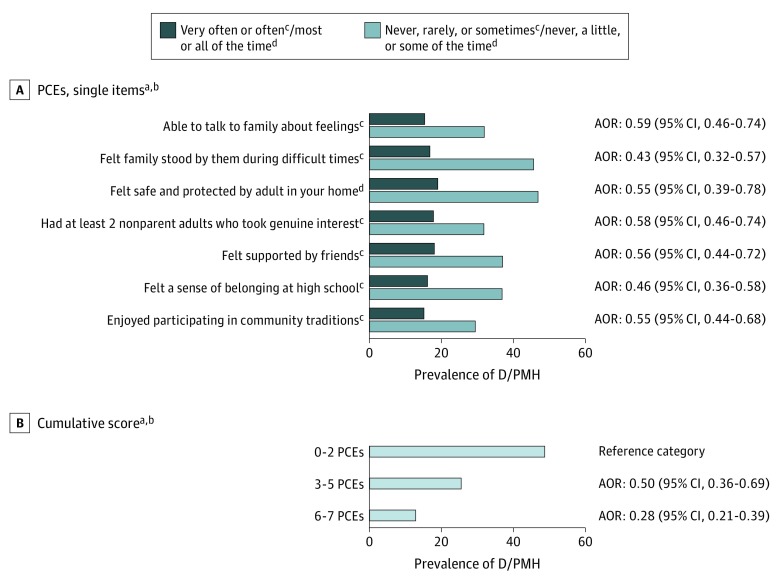
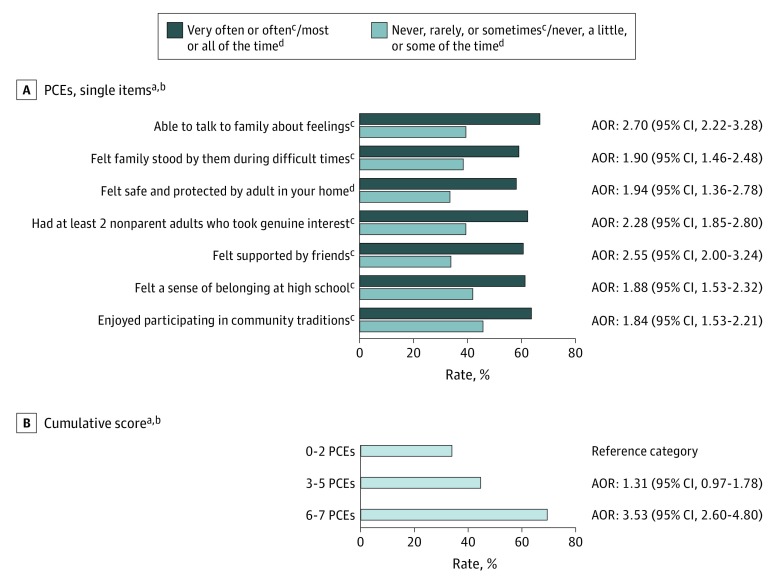
Demographic characteristics for the 2015 WI BRFS mirrored the state population: 50.7% women and 84.9% white. About half (52.3%) reported 6 to 7 PCEs, more than half (56.7%) reported ACEs, 21.2% met D/PMH criteria, and more than half (55.1%) reported “always” to getting the social and emotional support they needed (ARSES). Nonwhite, younger, and lower-income adults reported fewer levels of PCEs (Table 1). Compared with those reporting 6 to 7 PCEs, adults reporting 0 to 2 PCEs had nearly 4 times higher prevalence of D/PMH (48.2% vs 12.6%) and were half as likely to report “always” to getting the social and emotional support they needed (33.0% vs 67.9%) (Table 2). Similar variations in prevalence were observed when each of the 7 PCEs items were separately evaluated for each study outcome (Figures 1 and 2 and eTable 5 in the Supplement). As hypothesized and shown in these Figures, stronger associations emerged for cumulative PCEs scores.
Table 1. Study Population Characteristics and Prevalence of PCEs by D/PMH, ACEs, ARSES, and Demographic Characteristics.
| Population Characteristics (n = Unweighted Sample Size) | Statewide Population Prevalence Estimates | Prevalence of PCEs (n = 4926)a | P Value (Test of Independence) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 0-2 PCEs | 3-5 PCEs | 6-7 PCEs | |||||||
| Unweighted No. | Weighted % | Unweighted No. | Weighted % | Unweighted No. | Weighted % | Unweighted No. | Weighted % | ||
| All respondents | 6188 | 100 | 635 | 13.2 | 1606 | 34.5 | 2685 | 52.3 | NA |
| D/PMH (n = 6187) | |||||||||
| Yes | 1289 | 21.2 | 294 | 29.4 | 402 | 40.1 | 347 | 30.5 | <.001 |
| No | 4898 | 78.8 | 341 | 8.7 | 1204 | 33.0 | 2338 | 58.3 | |
| ACEs exposure levels (n = 4974)a,b | |||||||||
| 0 ACEs | 2275 | 43.3 | 106 | 4.9 | 567 | 27.3 | 1568 | 67.8 | <.001 |
| 1 ACE | 1142 | 23.0 | 100 | 8.3 | 406 | 38.6 | 625 | 53.1 | |
| 2-3 ACEs | 967 | 19.9 | 174 | 18.5 | 400 | 42.1 | 390 | 39.5 | |
| 4-8 ACEs | 590 | 13.7 | 255 | 39.4 | 232 | 39.4 | 100 | 21.2 | |
| ARSES (n = 5021)a | |||||||||
| Always | 2707 | 55.1 | 195 | 7.9 | 687 | 27.3 | 1743 | 64.8 | <.001 |
| Usually | 1337 | 25.8 | 171 | 12.9 | 507 | 41.9 | 635 | 45.2 | |
| Sometimes, rarely, or never | 977 | 19.1 | 263 | 28.7 | 393 | 44.7 | 284 | 26.6 | |
| Age (n = 6127), y | |||||||||
| 18-34 | 977 | 28.8 | 98 | 13.0 | 267 | 37.9 | 350 | 49.2 | .03 |
| 35-54 | 1737 | 33.0 | 201 | 15.6 | 407 | 31.9 | 748 | 52.5 | |
| 55-64 | 1426 | 17.6 | 169 | 12.6 | 389 | 36.0 | 613 | 51.4 | |
| 65 or older | 1987 | 20.5 | 163 | 10.4 | 532 | 33.1 | 954 | 56.5 | |
| Sex (n = 6188) | |||||||||
| Male | 2720 | 49.3 | 248 | 11.9 | 763 | 36.3 | 1133 | 51.7 | .09 |
| Female | 3468 | 50.7 | 387 | 14.3 | 843 | 32.8 | 1552 | 52.9 | |
| Race/ethnicity (n = 6129) | |||||||||
| Nonwhite | 757 | 15.1 | 107 | 17.0 | 208 | 44.7 | 233 | 38.3 | <.001 |
| White, non-Hispanic | 5372 | 84.9 | 521 | 12.6 | 1385 | 33.1 | 2433 | 54.3 | |
| Income level (n = 5461),c $ | |||||||||
| <24 999 | 1331 | 22.5 | 219 | 22.0 | 387 | 38.3 | 437 | 39.6 | <.001 |
| 25 000-49 999 | 1511 | 27.8 | 168 | 14.9 | 431 | 36.9 | 631 | 48.3 | |
| 50 000-74 999 | 1010 | 18.9 | 83 | 9.7 | 288 | 39.1 | 465 | 51.3 | |
| 75 000 or more | 1609 | 30.7 | 105 | 8.2 | 334 | 25.9 | 888 | 66.0 | |
Abbreviations: ACEs, adverse childhood experiences; ARSES, adult-reported social and emotional support; D/PMH, depression and/or poor mental health; NA, not applicable; PCEs, positive childhood experiences; WI BRFS, Wisconsin Behavioral Risk Factor Survey.
A 10% missing value rate is expected and attributed to core WI BRFS survey administration to out-of-state cellular phone holders who never received the WI BRFS state added items.59 The remainder were nearly all owing to respondent dropoffs prior to administering the ARSES, ACEs, and PCEs questions, which were administered after the end of the core WI BRFS. No notable differences in prevalence of D/PMH were found between respondents and cases missing ARSES, ACEs, or PCEs data. See eTable 1 in the Supplement.
The ACEs cumulative scores were created placing adults into categories of 0, 1, 2 to 3, or 4 to 8 ACEs based on their responses to the 11 ACEs items. Three sexual abuse items were combined into a single item, and alcohol and substance abuse items were presented as a single ACEs item.
Income missing values rate was 11.7%.
Table 2. Prevalence and Adjusted Odds Ratios of Adult D/PMH and Reports of “Always” on the ARSES Item by PCEs and Other Regression Model Variables.
| Population Characteristics (Raw Sample Size) | Prevalence of D/PMH | P Value | Adjusted Odds Ratio (95% CI) for Meeting D/PMH Criteria | Prevalence of “Always” on ARSES Item | P Value | Adjusted Odds Ratio (95% CI) for Reports of “Always” on ARSES Itema | ||
|---|---|---|---|---|---|---|---|---|
| Unweighted No. | Weighted % | Unweighted No. | Weighted % | |||||
| All Respondents | 1289 | 21.2 | NA | NA | 2707 | 55.1 | NA | NA |
| Positive childhood experiences (PCEs) (n = 4926)a,b,c | ||||||||
| 0-2 PCEs reported | 294 | 48.2 | <.001 | 1 [Reference] | 195 | 33.0 | <.001 | 1 [Reference] |
| 3-5 PCEs reported | 402 | 25.1 | 0.50 (0.36-0.69) | 687 | 43.6 | 1.31 (0.97-1.78) | ||
| 6-7 PCEs reported | 347 | 12.6 | 0.28 (0.21-0.39) | 1743 | 67.9 | 3.53 (2.60-4.80) | ||
| Adverse childhood experiences (ACEs) (n = 4974)a | ||||||||
| No ACEs reported | 252 | 11.9 | <.001 | 1 [Reference] | 1394 | 62.4 | <.001 | 1.22 (0.88-1.69) |
| 1 ACE reported | 215 | 20.2 | 1.62 (1.18-2.21) | 596 | 53.9 | 0.93 (0.67-1.30) | ||
| 2-3 ACEs reported | 294 | 29.2 | 2.40 (1.77-3.24) | 439 | 47.6 | 0.90 (0.64-1.27) | ||
| 4-8 ACEs reported |
285 | 42.4 | 3.10 (2.20-4.37) | 226 | 44.2 | 1 [Reference] | ||
| Age (n = 6127), y | ||||||||
| 18-34 | 215 | 21.0 | .01 | 1.09 (0.78-1.53) | 408 | 56.8 | .44 | 1.09 (0.84-1.42) |
| 35-54 | 406 | 22.6 | 1.51 (1.10-2.06) | 766 | 54.9 | 0.97 (0.76-1.23) | ||
| 55-64 | 331 | 24.2 | 1.64 (1.20-2.24) | 600 | 52.1 | 0.88 (0.69-1.13) | ||
| 65 or older | 332 | 16.9 | 1 [Reference] | 911 | 55.8 | 1 [Reference] | ||
| Sex (n = 6188) | ||||||||
| Male | 444 | 16.9 | <.001 | 0.59 (0.47-0.74) | 1189 | 55.3 | .80 | 0.97 (0.81-1.17) |
| Female | 845 | 25.5 | 1 [Reference] | 1518 | 54.8 | 1 [Reference] | ||
| Race/ethnicity (n = 6129) | ||||||||
| Nonwhite | 203 | 23.8 | <.25 | 0.98 (0.67-1.42) | 294 | 53.5 | .64 | 1.19 (0.84-1.70) |
| White, non-Hispanic | 1078 | 20.9 | 1 [Reference] | 2391 | 55.2 | 1 [Reference] | ||
| Income level (n = 5461),d $ | ||||||||
| <24 999 | 454 | 33.3 | <.001 | 2.91 (2.11-4.02) | 465 | 47.8 | <.001 | 0.67 (0.51-0.88) |
| 25 000-49 999 | 340 | 22.6 | 1.76 (1.29-2.41) | 667 | 53.4 | 0.81 (0.64-1.03) | ||
| 50 000-74 999 | 172 | 18.4 | 1.43 (1.02-2.01) | 458 | 54.3 | 0.81 (0.62-1.05) | ||
| 75 000 or more | 205 | 13.1 | 1 [Reference] | 857 | 62.3 | 1 [Reference] | ||
Abbreviations: ACEs, adverse childhood experiences; ARSES, adult-reported social and emotional support; D/PMH, depression and/or poor mental health; NA, not applicable; PCEs, positive childhood experiences; WI BRFS, Wisconsin Behavioral Risk Factor Survey.
A 10% missing value rate is expected and attributed to core WI BRFS 5 survey administration to out-of-state cellular phone holders who never received the WI BRFS state added items.59 The remainder were nearly all owing to respondent dropoffs prior to administering the ARSES, ACEs, and PCEs questions, which were administered after the end of the core WI BRFS. No notable differences in prevalence of D/PMH were found between respondents and cases missing ARSES, ACEs, or PCEs data. See eTable 1 in the Supplement.
Without adjustment for ACEs, PCEs associations with D/PMH were 0.19 (95% CI, 0.14-0.25) and 0.40 (95% CI, 0.30-0.54) for adults reporting 6 to 7 and 3 to 5 PCEs vs 0 to 2 PCEs, respectively.
Without adjustment for ACEs, PCEs associations with “always” on the ARSES variable were 3.83 (95% CI, 2.89-5.06) and 1.35 (95% CI, 1.01-1.81) for adults reporting 6 to 7 and 3 to 5 PCEs vs 0 to 2 PCEs, respectively.
Income missing values rate is 11.7%. Income was not imputed for the WI BRFS by the Wisconsin Department of Health Services so federal poverty level could not be calculated.
Figure 1. Prevalence of Depression and/or Poor Mental Health Among Adults by Positive Childhood Experiences (PCEs) Single Items and Cumulative Scores .
See eTable 5 in the Supplement for percentages of depression and/or poor mental health and adult-reported social and emotional support across PCEs items and scores.
aSource: authors’ analysis of the 2015 Wisconsin Behavioral Risk Factor Survey.
bAdjusted odds ratios (AORs) shown are adjusted for age, sex, race/ethnicity, income, and adverse childhood experiences.
cNever, rarely, or sometimes is the reference category.
dNever, a little, or some of the time is the reference category.
Figure 2. Prevalence of Adult Reporting Always Receiving Needed Social Emotional Support by Positive Childhood Experiences (PCEs) Single Items and Cumulative Scores .
See eTable 5 in the Supplement for percentages of depression and/or poor mental health and adult-reported social and emotional support across PCEs items and scores.
aSource: authors’ analysis of the 2015 Wisconsin Behavioral Risk Factor Survey.
bAdjusted odds ratios (AORs) shown are adjusted for age, sex, race/ethnicity, income, and adverse childhood experiences.
cNever, rarely, or sometimes is the reference category.
dNever, a little, or some of the time is the reference category.
The lowest adult D/PMH prevalences were observed for respondents reporting both 6 to 7 PCEs and either no ACEs (10.5%) or “always” on the ARSES variable (8.5%). Highest D/PMH prevalences were for those reporting 0 to 2 PCEs and either 4 to 8 ACEs (59.7%) or “sometimes/ rarely/never” on the ARSES variable (61.7%). Yet, even among those reporting always getting needed social and emotional support, a subset reported 0 to 2 PCEs, and this group had 4 times greater prevalence of D/PMH compared with those reporting 6 to 7 PCEs (33.8% vs 8.5%). Likewise, 21.2% of those with 4 to 8 ACEs and 26.6% of those reporting “sometime/rarely/never” to the ARSES item nonetheless also reported 6 to 7 PCEs. (Table 1, Table 3, and eTable 3 in the Supplement).
Table 3. Prevalence of D/PMH and Reports of “Always” on the ARSES Item by PCEs Scores for Each of 4 Adverse Childhood Experiences ACEs Exposure Levels (0, 1, 2-3, or 4-8).
| Categories by ACEs and PCEs | Meets D/PMH Criteriaa | Reports of “Always” to Getting Needed Social and Emotional Support (ARSES) | ||||
|---|---|---|---|---|---|---|
| Unweighted No. | Weighted % | Adjusted Odds Ratiob (95% CI) | Unweighted No. | Weighted % | Adjusted Odds Ratiob (95% CI) | |
| No ACEs reported | ||||||
| 0-2 PCEs | 17 | 12.1 | 1 [Reference] | 35 | 34.6 | 1 [Reference] |
| 3-5 PCEs | 86 | 15.8 | 1.15 (0.51-2.62) | 266 | 47.3 | 1.58 (0.84-2.95) |
| 6-7 PCEs | 148 | 10.5 | 0.88 (0.42-1.87) | 1072 | 70.5 | 4.18 (2.31-7.55) |
| 1 ACE reported | ||||||
| 0-2 PCEs | 35 | 45.7 | 1 [Reference] | 38 | 30.9 | 1 [Reference] |
| 3-5 PCEs | 85 | 24.2 | 0.38 (0.17-0.83) | 161 | 39.5 | 1.33 (0.68-2.62) |
| 6-7 PCEs | 94 | 13.4 | 0.21 (0.10-0.46) | 390 | 67.6 | 4.93 (2.54-9.58) |
| 2-3 ACEs reported | ||||||
| 0-2 PCEs | 87 | 53.3 | 1 [Reference] | 47 | 30.3 | 1 [Reference] |
| 3-5 PCEs | 131 | 31.4 | 0.47 (0.26-0.84) | 167 | 43.9 | 1.65 (0.90-3.02) |
| 6-7 PCEs | 76 | 16.0 | 0.18 (0.10-0.34) | 223 | 59.2 | 2.80 (1.53-5.13) |
| 4-8 ACEs reported | ||||||
| 0-2 PCEs | 155 | 59.7 | 1 [Reference] | 75 | 35.1 | 1 [Reference] |
| 3-5 PCEs | 100 | 36.9 | 0.49 (0.28-0.84) | 93 | 41.7 | 1.19 (0.69-2.03) |
| 6-7 PCEs | 29 | 20.7 | 0.23 (0.11-0.46) | 56 | 65.6 | 3.37 (1.66-6.84) |
Abbreviations: ACEs, adverse childhood experiences; ARSES, adult-reported social and emotional support; D/PMH, depression and/or poor mental health; PCEs, positive childhood experiences.
Prevalence of D/PMH varied across levels of ACEs within each PCEs cumulative score category (0-2, 3-5, and 6-7) at P < .01.
Adjusted odds ratios adjusted for age, sex, race/ethnicity, and income.
Association Pathway 1: PCEs and D/PMH
After controlling for ACEs, the adjusted odds of D/PMH were 72% lower (odds ratio [OR], 0.28; 95% CI, 0.21-0.39) for adults with the highest vs lowest PCEs scores (12.6% vs 48.2%). Odds were 50% lower (OR, 0.50; 95% CI, 0.36-0.69) for those reporting intermediate PCEs scores of 3 to 5 (25.1% vs 48.2%) (Table 2). Associations were similar in magnitude for adults reporting 1, 2 to 3, or 4 to 8 ACEs (Table 3).
Association Pathway 2: PCEs and ARSES
The adjusted odds of “always” reports on the ARSES item were 3.53 times (95% CI, 2.60-4.80) greater for adults with the highest vs lowest PCEs scores. Adjusted odds of reports of “always” on the ARSES variable were not significant for adults with intermediate PCEs of 3 to 5 (adjusted OR, 1.31; 95% CI, 0.97-1.78) (Table 2). Findings were similar across all ACEs exposure level subgroups (Table 3). Because PCEs and ARSES were strongly associated as hypothesized, we further examined whether each variable demonstrated an independent association with D/PMH and whether associations of PCEs with D/PMH remained stable when ARSES was included in regression models. Results showed that PCEs associations with D/PMH remained significant and changed only modestly when ARSES was included. Associations between ARSES and D/PMH also remained stable when PCEs were or were not included. See eTable 4 in the Supplement for details.
Discussion
This study examined the prevalence of adult reports of both PCEs and ACEs in a statewide sample and found that PCEs both co-occur with and operate independently from ACEs in their associations with the adult health outcomes evaluated here. Findings also confirm the hypotheses that PCEs may exert their association with D/PMH through their association with ARSES. However, PCEs maintained an association with D/PMH independent from ARSES. Findings are both consistent with prior research showing that relational experiences in childhood are associated with adult social and relational skills and health3,15,56,68 and also point to enduring effects of PCEs on D/PMH separate from their influence on adult ARSES.
While PCEs associations with D/PMH were substantial and similar for adults reporting ACEs, associations were not statistically significant for those reporting no ACEs. Insignificant findings may be owing to low sample sizes for respondents with no ACEs and fewer PCEs. Results still raise questions for further exploration. We hypothesize that PCEs may have a greater influence in promoting positive health, such as getting needed social and emotional support or flourishing as an adult. In turn, these positive health attributes may reduce the burden of illness even if the illness is not eliminated. This is consistent with prior research demonstrating a dual continuum of health whereby flourishing is found to be present for many adults despite concurrent mental health conditions.69
Limitations
First, this study is cross-sectional and cannot confirm causal effects. Second, the 2015 Wisconsin adult population is less diverse than the United States as a whole. Third, PCEs focused on the domain of positive emotional experiences in interpersonal relationships. Other types of positive experiences, (eg, safe and supportive environments, nature or spiritual experiences, participation in activities, or accomplishment) require further study, highlighting the need to develop and test additional measures of PCEs. Fourth, we were not able to directly examine bias in reporting of PCEs among adults with depression, although studies show an absence of such biases for reports of ACEs.64,70 Finally, the WI BRFS did not assess overall well-being or flourishing.69 As such, we were not able to assess whether PCEs affect positive adult health outcomes as hypothesized. Sample size limitations may have resulted in false-negative findings in some cases.
Conclusions
Overall, study results demonstrate that PCEs show a dose-response association with adult mental and relational health, analogous to the cumulative effects of multiple ACEs. Findings suggest that PCEs may have lifelong consequences for mental and relational health despite co-occurring adversities such as ACEs. In this way, they support application of the World Health Organization’s definition of health emphasizing that health is more than the absence of disease or adversity.71 The World Health Organization’s positive construct of health is aligned with the proactive promotion of positive experiences in childhood because they are foundational to optimal childhood development and adult flourishing. Including PCEs as well as positive health outcomes measures in routinely collected public health surveillance systems, such as the National Survey of Children’s Health and state Behavioral Risk Factor Surveillance Surveys, may advance knowledge and allow the nation to track progress in promoting flourishing despite adversity or illness among children and adults in the United States.
Even as society continues to address remediable causes of childhood adversities such as ACEs, attention should be given to the creation of those positive experiences that both reflect and generate resilience within children, families, and communities. Success will depend on full engagement of families and communities and changes in the health care, education, and social services systems serving children and families. A joint inventory of ACEs and PCEs, such as the positive experiences assessed here, may improve efforts to assess needs, target interventions, and engage individuals in addressing the adversities they face by leveraging existing assets and strengths.72 Initiatives to conduct broad ACEs screening, such as those ensuing in California’s Medicaid program, may benefit from integrated assessments including PCEs.73
Recommendations and practice guidelines included in the National Bright Futures Guidelines for Health Supervision of Infants, Children, and Adolescents74 and the CDC’s Essentials for Childhood initiative9 encourage policies and initiatives to help child-serving professionals and programs to adopt effective approaches to promote the type of PCEs evaluated in this study. The Health Outcomes of Positive Experiences framework48 and the Prioritizing Possibilities national agenda for promoting child health and addressing ACEs75 each seek to advance existing and emerging evidence-based approaches44,45,47,48,50,54,76,77 that promote a positive construct of health in clinical, public health, and human services settings. This study adds to the growing evidence that childhood experiences have profound and lifelong effects. Results hold promise for national, state, and community efforts to achieve positive child and adult health and well-being by promoting the largely untapped potential to promote positive experiences and flourishing despite adversity.53,78
eTable 1. Prevalence of Depression/Poor Mental Health (D/PMH) and Demographic Characteristics Among Adults With or Without Missing Values for Positive Childhood Experiences (PCEs), Adult Reported Social and Emotional Support (ARSES) and Adverse Childhood Experiences (ACEs) WI BRFS State Added Items
eTable 2. Summary of Findings From Psychometric Analysesa Conducted on Positive Childhood Experiences (PCEs) Seven Item Measure
eTable 3. Prevalence of Adult Depression and/or Poor Mental Health (D/PMH) by Adult Reported Social and Emotional Support (ARSES) and Positive Childhood Experiences (PCEs)
eTable 4. Adjusted Odds Ratios of Adult Depression and/or Poor Mental Health (D/PMH) by Adult Reported Social and Emotional Support (ARSES) and Positive Childhood Experiences (PCEs) Under Alternative Model Configurations
eTable 5. Prevalence of Depression and/or Poor Mental Health (D/PMH) and Adult Reporting "Always" Receiving Needed Social Emotional Support (ARSES), By Positive Childhood Experiences (PCEs) Cumulative Scores and Single Items
References
- 1.Lamb ME, Lerner RM. Handbook of Child Psychology and Developmental Science: Socioemotional Processes. Vol 3 7th ed Hoboken, NJ: John Wiley & Sons Inc; 2015. [Google Scholar]
- 2.Masten AS, Barnes AJ. Resilience in children: developmental perspectives. Children (Basel). 2018;5(7):. doi: 10.3390/children5070098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Raby KL, Roisman GI, Fraley RC, Simpson JA. The enduring predictive significance of early maternal sensitivity: social and academic competence through age 32 years. Child Dev. 2015;86(3):695-. doi: 10.1111/cdev.12325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hoppen TH, Chalder T. Childhood adversity as a transdiagnostic risk factor for affective disorders in adulthood: a systematic review focusing on biopsychosocial moderating and mediating variables. Clin Psychol Rev. 2018;65:81-151. doi: 10.1016/j.cpr.2018.08.002 [DOI] [PubMed] [Google Scholar]
- 5.Shonkoff JP, Garner AS; Committee on Psychosocial Aspects of Child and Family Health; Committee on Early Childhood, Adoption, and Dependent Care; Section on Developmental and Behavioral Pediatrics . The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129(1):e232-e246. doi: 10.1542/peds.2011-2663 [DOI] [PubMed] [Google Scholar]
- 6.Ainsworth MD, Blehar MC, Waters E, Wall S. Patterns of Attachment: a Psychological Study of the Strange Situation. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc; 1978. [Google Scholar]
- 7.Rees C. Childhood attachment. Br J Gen Pract. 2007;57(544):920-922. doi: 10.3399/096016407782317955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thiebaut de Schotten M, Cohen L, Amemiya E, Braga LW, Dehaene S. Learning to read improves the structure of the arcuate fasciculus. Cereb Cortex. 2014;24(4):989-995. doi: 10.1093/cercor/bhs383 [DOI] [PubMed] [Google Scholar]
- 9.US Centers for Disease Control and Prevention National Center for Injury Prevention and Control Essentials for childhood: steps to create safe, stable, nurturing relationships and environment. 2014. https://www.cdc.gov/violenceprevention/pdf/essentials-for-childhood-framework508.pdf. Accessed February 5, 2019.
- 10.Sege RD, Harper Browne C. Responding to ACEs with HOPE: health outcomes from positive experiences. Acad Pediatr. 2017;17(7S):S79-S85. doi: 10.1016/j.acap.2017.03.007 [DOI] [PubMed] [Google Scholar]
- 11.McEwen BS, Bowles NP, Gray JD, et al. Mechanisms of stress in the brain. Nat Neurosci. 2015;18(10):1353-1363. doi: 10.1038/nn.4086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Essex MJ, Boyce WT, Hertzman C, et al. Epigenetic vestiges of early developmental adversity: childhood stress exposure and DNA methylation in adolescence. Child Dev. 2013;84(1):58-75. doi: 10.1111/j.1467-8624.2011.01641.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boyce WT. Epigenomics and the unheralded convergence of the biological and social sciences. Agency for Healthcare Research and Quality, Rockville, MD. https://www.ahrq.gov/sites/default/files/publications/files/population-health.pdf. Accessed October 2, 2019.
- 14.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) study. Am J Prev Med. 1998;14(4):245-258. doi: 10.1016/S0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- 15.Jones DE, Greenberg M, Crowley M. Early social-emotional functioning and public health: the relationship between kindergarten social competence and future wellness. Am J Public Health. 2015;105(11):2283-2290. doi: 10.2105/AJPH.2015.302630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Slopen N, Chen Y, Priest N, Albert MA, Williams DR. Emotional and instrumental support during childhood and biological dysregulation in midlife. Prev Med. 2016;84:90-96. doi: 10.1016/j.ypmed.2015.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen Y, Kubzansky LD, VanderWeele TJ. Parental warmth and flourishing in mid-life. Soc Sci Med. 2019;220:65-72. doi: 10.1016/j.socscimed.2018.10.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Merrick MT, Ford DC, Ports KA, Guinn AS. Prevalence of adverse childhood experiences from the 2011-2014 behavioral risk factor surveillance system in 23 states. JAMA Pediatr. 2018;172(11):1038-1044. doi: 10.1001/jamapediatrics.2018.2537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bethell CD, Newacheck P, Hawes E, Halfon N. Adverse childhood experiences: assessing the impact on health and school engagement and the mitigating role of resilience. Health Aff (Millwood). 2014;33(12):2106-2115. doi: 10.1377/hlthaff.2014.0914 [DOI] [PubMed] [Google Scholar]
- 20.US Centers for Disease Control and Prevention ACEs study: violence prevention. https://www.cdc.gov/violenceprevention/acestudy/. Published April 1, 2016. Accessed October 6, 2018.
- 21.Burke NJ, Hellman JL, Scott BG, Weems CF, Carrion VG. The impact of adverse childhood experiences on an urban pediatric population. Child Abuse Negl. 2011;35(6):408-413. doi: 10.1016/j.chiabu.2011.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lehman BJ, Taylor SE, Kiefe CI, Seeman TE. Relationship of early life stress and psychological functioning to blood pressure in the CARDIA study. Health Psychol. 2009;28(3):338-346. doi: 10.1037/a0013785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, Anda RF. Adverse childhood experiences and the risk of depressive disorders in adulthood. J Affect Disord. 2004;82(2):217-225. doi: 10.1016/j.jad.2003.12.013 [DOI] [PubMed] [Google Scholar]
- 24.Hayashi Y, Okamoto Y, Takagaki K, et al. Direct and indirect influences of childhood abuse on depression symptoms in patients with major depressive disorder. BMC Psychiatry. 2015;15:244. doi: 10.1186/s12888-015-0636-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chung EK, Mathew L, Elo IT, Coyne JC, Culhane JF. Depressive symptoms in disadvantaged women receiving prenatal care: the influence of adverse and positive childhood experiences. Ambul Pediatr. 2008;8(2):109-116. doi: 10.1016/j.ambp.2007.12.003 [DOI] [PubMed] [Google Scholar]
- 26.Poole JC, Dobson KS, Pusch D. Childhood adversity and adult depression: the protective role of psychological resilience. Child Abuse Negl. 2017;64:89-100. doi: 10.1016/j.chiabu.2016.12.012 [DOI] [PubMed] [Google Scholar]
- 27.Copeland WE, Shanahan L, Hinesley J, et al. Association of childhood trauma exposure with adult psychiatric disorders and functional outcomes. JAMA Netw Open. 2018;1(7):e184493. doi: 10.1001/jamanetworkopen.2018.4493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Young-Wolff KC, Alabaster A, McCaw B, et al. Adverse childhood experiences and mental and behavioral health conditions during pregnancy: the role of resilience. J Womens Health (Larchmt). 2019;28(4):452-461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cohen S. Social relationships and health. Am Psychol. 2004;59(8):676-684. doi: 10.1037/0003-066X.59.8.676 [DOI] [PubMed] [Google Scholar]
- 30.Uchino BN. Social support and health: a review of physiological processes potentially underlying links to disease outcomes. J Behav Med. 2006;29(4):377-387. doi: 10.1007/s10865-006-9056-5 [DOI] [PubMed] [Google Scholar]
- 31.Shor E, Roelfs DJ, Yogev T. The strength of family ties: a meta-analysis and meta-regression of self-reported social support and mortality. Soc Networks. 2013;4(35):626-638. doi: 10.1016/j.socnet.2013.08.004 [DOI] [Google Scholar]
- 32.Schüssler-Fiorenza Rose SM, Eslinger JG, Zimmerman L, et al. Adverse childhood experiences, support, and the perception of ability to work in adults with disability. PLoS One. 2016;11(7):e0157726. doi: 10.1371/journal.pone.0157726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Reblin M, Uchino BN. Social and emotional support and its implication for health. Curr Opin Psychiatry. 2008;21(2):201-205. doi: 10.1097/YCO.0b013e3282f3ad89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Strine TW, Chapman DP, Balluz L, Mokdad AH. Health-related quality of life and health behaviors by social and emotional support: their relevance to psychiatry and medicine. Soc Psychiatry Psychiatr Epidemiol. 2008;43(2):151-159. doi: 10.1007/s00127-007-0277-x [DOI] [PubMed] [Google Scholar]
- 35.Brinker J, Cheruvu VK. Social and emotional support as a protective factor against current depression among individuals with adverse childhood experiences. Prev Med Rep. 2016;5:127-133. doi: 10.1016/j.pmedr.2016.11.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cheong EV, Sinnott C, Dahly D, Kearney PM. Adverse childhood experiences (ACEs) and later-life depression: perceived social support as a potential protective factor. BMJ Open. 2017;7(9):e013228. doi: 10.1136/bmjopen-2016-013228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grav S, Hellzèn O, Romild U, Stordal E. Association between social support and depression in the general population: the HUNT study, a cross-sectional survey. J Clin Nurs. 2012;21(1-2):111-120. doi: 10.1111/j.1365-2702.2011.03868.x [DOI] [PubMed] [Google Scholar]
- 38.Brody GH, Yu T, Beach SR. Resilience to adversity and the early origins of disease. Dev Psychopathol. 2016;28(4pt2):1347-1365. doi: 10.1017/S0954579416000894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Banyard V, Hamby S, Grych J. Health effects of adverse childhood events: identifying promising protective factors at the intersection of mental and physical well-being. Child Abuse Negl. 2017;65:88-98. doi: 10.1016/j.chiabu.2017.01.011 [DOI] [PubMed] [Google Scholar]
- 40.Biglan A, Van Ryzin MJ, Hawkins JD. Evolving a more nurturing society to prevent adverse childhood experiences. Acad Pediatr. 2017;17(7S):S150-S157. doi: 10.1016/j.acap.2017.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hillis SD, Anda RF, Dube SR, et al. The protective effect of family strengths in childhood against adolescent pregnancy and its long-term psychosocial consequences. Perm J. 2010;14(3):18-27. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2937841/. doi: 10.7812/TPP/10-028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Boyce T. The Orchid and the Dandelion. New York, NY: Knopf Publishing; 2019. [Google Scholar]
- 43.Cadet JL. Epigenetics of stress, addiction, and resilience: therapeutic implications. Mol Neurobiol. 2016;53(1):545-560. doi: 10.1007/s12035-014-9040-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Leslie LK, Mehus CJ, Hawkins JD, et al. Primary health care: potential home for family-focused preventive interventions. Am J Prev Med. 2016;51(4)(suppl 2):S106-S118. doi: 10.1016/j.amepre.2016.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rayce SB, Rasmussen IS, Klest SK, Patras J, Pontoppidan M. Effects of parenting interventions for at-risk parents with infants: a systematic review and meta-analyses. BMJ Open. 2017;7(12):e015707. doi: 10.1136/bmjopen-2016-015707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Southwick SM, Charney DS. The science of resilience: implications for the prevention and treatment of depression. Science. 2012;338(6103):79-82. doi: 10.1126/science.1222942 [DOI] [PubMed] [Google Scholar]
- 47.Traub F, Boynton-Jarrett R. Modifiable resilience factors to childhood adversity for clinical pediatric practice. Pediatrics. 2017;139(5):e20162569. doi: 10.1542/peds.2016-2569 [DOI] [PubMed] [Google Scholar]
- 48.National Scientific Council on the Developing Child Supportive relationships and active skill-building strengthen the foundations of resilience: working paper 13. http://www.developingchild.harvard.edu Published 2019. Accessed March 5, 2019.
- 49.Shonkoff JP. Capitalizing on advances in science to reduce the health consequences of early childhood adversity. JAMA Pediatr. 2016;170(10):1003-1007. doi: 10.1001/jamapediatrics.2016.1559 [DOI] [PubMed] [Google Scholar]
- 50.Leitch L. Action steps using ACEs and trauma-informed care: a resilience model. Health Justice. 2017;5(1):5. doi: 10.1186/s40352-017-0050-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schaefer LM, Howell KH, Schwartz LE, Bottomley JS, Crossnine CB. A concurrent examination of protective factors associated with resilience and posttraumatic growth following childhood victimization. Child Abuse Negl. 2018;85:17-27. doi: 10.1016/j.chiabu.2018.08.019 [DOI] [PubMed] [Google Scholar]
- 52.Bleck J, DeBate R. Long-term association between developmental assets and health behaviors: an exploratory study. Health Educ Behav. 2016;43(5):543-551. doi: 10.1177/1090198115606915 [DOI] [PubMed] [Google Scholar]
- 53.Bethell CD, Gombojav N, Whitaker RC. Family resilience and connection promote flourishing among US children, even amid adversity. Health Aff (Millwood). 2019;38(5):729-737. doi: 10.1377/hlthaff.2018.05425 [DOI] [PubMed] [Google Scholar]
- 54.Marie-Mitchell A, Kostolansky R. A systematic review of trials to improve child outcomes associated with adverse childhood experiences. Am J Prev Med. 2019;56(5):756-764. doi: 10.1016/j.amepre.2018.11.030 [DOI] [PubMed] [Google Scholar]
- 55.Schofield TJ, Lee RD, Merrick MT. Safe, stable, nurturing relationships as a moderator of intergenerational continuity of child maltreatment: a meta-analysis. J Adolesc Health. 2013;53(4)(suppl):S32-S38. doi: 10.1016/j.jadohealth.2013.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kosterman R, Mason WA, Haggerty KP, Hawkins JD, Spoth R, Redmond C. Positive childhood experiences and positive adult functioning: prosocial continuity and the role of adolescent substance use. J Adolesc Health. 2011;49(2):180-186. doi: 10.1016/j.jadohealth.2010.11.244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wisconsin Department of Health Services/Centers for Disease Control and Prevention Behavioral Risk Factor Surveillance System Survey Data. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2015. [Google Scholar]
- 58.Sege R, Bethell C, Linkenbach J, Jones J, Klika B, Pecora PJ. Balancing Adverse Childhood Experiences With HOPE: New Insights Into the Role of Positive Experience on Child and Family Development. Boston, MA: The Medical Foundation; 2017. [Google Scholar]
- 59.Chowdhury P, Pierannunzi C, Garvin WS, Town M. Health behaviors and chronic conditions of movers: out-of-state interviews among cell phone respondents, BRFSS 2014. Surv Pract. 2018;11(2). doi: 10.29115/SP-2018-0010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Liebenberg L, Ungar M, LeBlanc JC. The CYRM-12: a brief measure of resilience. Can J Public Health. 2013;104(2):e131-e135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ungar M, Liebenberg L, Boothroyd R, et al. The study of youth resilience across cultures: lessons from a pilot study of measurement development. Res Hum Dev. 2008;5(3):166-180. doi: 10.1080/15427600802274019 [DOI] [Google Scholar]
- 62.National Center for Injury Prevention and Control BRFSS Adverse Childhood Experiences (ACE) module. https://www.cdc.gov/violenceprevention/acestudy/pdf/brfss_adverse_module.pdf. Accessed February 5, 2019.
- 63.Child Abuse & Neglect Prevention Board, Children’s Hospital of Wisconsin The influence of adverse childhood experiences on the health of Wisconsin citizens in adulthood (revised version). 2016. https://preventionboard.wi.gov/Documents/WisconsinACEBrief%282011-13%29WEB_9.16.pdf. Accessed October 11, 2018.
- 64.Rohner RP, Khaleque A, Cournoyer DE. Parental acceptance-rejection: theory, methods, cross-cultural evidence and implications. Ethos. 2005;33(3):299-334. doi: 10.1525/eth.2005.33.3.299 [DOI] [Google Scholar]
- 65.Moriarty DG, Zack MM, Kobau R. The Centers for Disease Control and Prevention’s Healthy Days Measures: population tracking of perceived physical and mental health over time. Health Qual Life Outcomes. 2003;1(37):37. doi: 10.1186/1477-7525-1-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Pierannunzi C, Hu SS, Balluz L. A systematic review of publications assessing reliability and validity of the Behavioral Risk Factor Surveillance System (BRFSS), 2004-2011. BMC Med Res Methodol. 2013;13(49):49. doi: 10.1186/1471-2288-13-49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Corp IBM. Released 2016. IBM SPSS Statistics and SPSS Complex Samples for Windows, Version 24.0. Armonk, NY: IBM Corp. [Google Scholar]
- 68.Schor EL. Why becoming a good parent begins in infancy: how relationship skills are developed throughout the life course. https://www.lpfch.org/publication/why-becoming-good-parent-begins-infancy-how-relationship-skills-are-developed-throughout. Published January 3, 2018. Accessed March 5, 2019.
- 69.Agenor C, Conner N, Aroian K. Flourishing: an evolutionary concept analysis. Issues Ment Health Nurs. 2017;38(11):915-923. doi: 10.1080/01612840.2017.1355945 [DOI] [PubMed] [Google Scholar]
- 70.Frampton NMA, Poole JC, Dobson KS, Pusch D. The effects of adult depression on the recollection of adverse childhood experiences. Child Abuse Negl. 2018;86:45-54. doi: 10.1016/j.chiabu.2018.09.006 [DOI] [PubMed] [Google Scholar]
- 71.Misselbrook D. W is for wellbeing and the WHO definition of health. Br J Gen Pract. 2014;64(628):582. doi: 10.3399/bjgp14X682381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Leitch L. Positive and Adverse Childhood Experiences Survey (PACES): threshold global works. https://www.thresholdglobalworks.com/portfolio-items/paces-survey/. Published March 2017. Accessed March 5, 2019.
- 73.California Pan Ethnic Health Network Governor Newsom’s budget makes important investments in health equity and prevention. https://cpehn.org/blog/201901/governor-newsom%E2%80%99s-budget-makes-important-investments-health-equity-and-prevention. Published January 11, 2019. Accessed March 5, 2019.
- 74.Hagan JF, Shaw JS, Duncan PM. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. Elk Grove Village, IL: Bright Futures/American Academy of Pediatrics; 2017. [Google Scholar]
- 75.Bethell CD, Solloway MR, Guinosso S, et al. Prioritizing possibilities for child and family health: an agenda to address adverse childhood experiences and foster the social and emotional roots of well-being in pediatrics. Acad Pediatr. 2017;17(7S):S36-S50. doi: 10.1016/j.acap.2017.06.002 [DOI] [PubMed] [Google Scholar]
- 76.Bloom SL. Advancing a national cradle-to-grave-to-cradle public health agenda. J Trauma Dissociation. 2016;17(4):383-396. doi: 10.1080/15299732.2016.1164025 [DOI] [PubMed] [Google Scholar]
- 77.Bethell C, Gombojav N, Solloway M, Wissow L. Adverse childhood experiences, resilience and mindfulness-based approaches: common denominator issues for children with emotional, mental, or behavioral problems. Child Adolesc Psychiatr Clin N Am. 2016;25(2):139-156. doi: 10.1016/j.chc.2015.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.VanderWeele TJ, McNeely E, Koh HK. Reimagining health-flourishing. JAMA. 2019;321(17):1667-1668. doi: 10.1001/jama.2019.3035 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Prevalence of Depression/Poor Mental Health (D/PMH) and Demographic Characteristics Among Adults With or Without Missing Values for Positive Childhood Experiences (PCEs), Adult Reported Social and Emotional Support (ARSES) and Adverse Childhood Experiences (ACEs) WI BRFS State Added Items
eTable 2. Summary of Findings From Psychometric Analysesa Conducted on Positive Childhood Experiences (PCEs) Seven Item Measure
eTable 3. Prevalence of Adult Depression and/or Poor Mental Health (D/PMH) by Adult Reported Social and Emotional Support (ARSES) and Positive Childhood Experiences (PCEs)
eTable 4. Adjusted Odds Ratios of Adult Depression and/or Poor Mental Health (D/PMH) by Adult Reported Social and Emotional Support (ARSES) and Positive Childhood Experiences (PCEs) Under Alternative Model Configurations
eTable 5. Prevalence of Depression and/or Poor Mental Health (D/PMH) and Adult Reporting "Always" Receiving Needed Social Emotional Support (ARSES), By Positive Childhood Experiences (PCEs) Cumulative Scores and Single Items