This study determines whether infrared video assessment of spontaneous retinal venous pulsation is associated with intracranial pressure and is a valid tool to indicate the presence or absence of raised intracranial pressure in patients without papilledema.
Key Points
Question
Is infrared video assessment of spontaneous venous pulsation useful for identifying patients with elevated intracranial pressure?
Findings
In this study that included 105 patients, there was a statistically significant association between the grading of spontaneous venous pulsation (assessed through infrared videos) and simultaneous intracranial pressure in patients without papilledema.
Meaning
Infrared video assessments of spontaneous venous pulsation can be used as a noninvasive method of assessment of intracranial pressure and have the potential to help determine which patients need invasive intracranial pressure monitoring.
Abstract
Importance
A convenient and reliable method for noninvasive intracranial pressure assessments is desirable to reduce the need for invasive procedures (eg, intracranial pressure monitoring and lumbar punctures) and allow clinicians to identify and treat patients with intracranial hypertension in a timely manner.
Objective
To determine whether infrared video assessment of spontaneous retinal venous pulsation is associated with intracranial pressure and is a valid tool to indicate the presence or absence of raised intracranial pressure in patients without papilledema.
Design, Setting, and Participants
A single-center prospective study was conducted at a tertiary referral center between January 2017 and May 2018. Patients consecutively admitted for clinically indicated elective 24-hour invasive intracranial pressure monitoring had ophthalmic review including infrared video recording of their spontaneous venous pulsation. Two neuro-ophthalmologists, who were masked to the intracranial pressure monitoring results, independently graded the spontaneous venous pulsation (grade 0 to 3). Analysis began in June 2018.
Main Outcomes and Measures
The association between simultaneously recorded intracranial pressure and spontaneous venous pulsation (binary variable: present/absent) assessed through retinal infrared video recordings was evaluated using a multiple linear regression model.
Results
Of 105 patients, the mean (SD) age was 39 (14) years, and 79 (75%) were women. The mean (SD) simultaneous intracranial pressure was 1 (5) mm Hg for 91 patients (86.7%) with spontaneous venous pulsations and 13 (14) mm Hg for 14 patients (13.3%) without spontaneous venous pulsations. A multiple linear regression model adjusted for 7 potential confounders confirmed a statistically significant association between intracranial pressure and spontaneous venous pulsation (β = −9.1; 95% CI, −13.7 to −4.6; P < .001; adjusted R2 = 0.42).
Conclusions and Relevance
The absence of spontaneous venous pulsation on retinal infrared video recordings is significantly associated with higher levels of intracranial pressure and should raise the suspicion of intracranial hypertension.
Introduction
Spontaneous retinal venous pulsation (SVP) is the rhythmic constriction and redilation of the retinal veins near the optic disc, synchronized to the cardiac cycle. It occurs owing to the pressure gradient between the retinal veins within the eye and the lower pressure in the retrobulbar portion of the central retinal vein, the latter being determined by the pressure of the cerebrospinal fluid (CSF).1,2,3,4 Spontaneous retinal venous pulsation tends to disappear when the CSF pressure is high owing to loss of the physiological pressure gradient and distention of the retinal veins. The validity of the absence of SVP as a predictive marker of raised intracranial pressure (ICP) has been investigated but never confirmed in vivo.
Spontaneous retinal venous pulsation has been reported to be absent in 7% to 23% of healthy individuals when assessed with direct ophthalmoscopy.5,6,7,8 Our group has reported that motion-stabilized infrared (IR) video, recorded using the Heidelberg Spectralis optical coherence tomography (OCT) system (Heidelberg Engineering) is highly sensitive in detecting spontaneous venous pulsation, being able to show SVP in 99% of healthy individuals.9 This implies that in those healthy patients where SVP is not observable via direct ophthalmoscopy, SVP is likely to be present but difficult to visualize owing to its small amplitude. This diagnostic study investigated the association between SVP and ICP using the previously described SVP assessment technique.9
Methods
This study has been approved by the South West (Central Bristol) Human Research Ethics Committee. Written informed consent was waived, although verbal consent was obtained from all patients. Data were collected from January 2017 to May 2018 and analyzed beginning in June 2018.
Consecutive patients admitted at the National Hospital for Neurology and Neurosurgery for elective 24-hour ICP monitoring were prospectively identified. Children (younger than 18 years) and patients with ocular comorbidity that could interfere with the validity of the data (eg, central retinal vein occlusion, ocular media opacity, glaucoma) were excluded.
Intracranial pressure monitoring was performed following an established local protocol.10,11 The indication for ICP monitoring included patients with symptoms suggestive of intracranial hypertension, shunt malfunction, or other CSF dynamics disorders (eg, abnormal intracranial compliance, normal pressure hydrocephalus, low CSF pressure/volume syndromes) but in whom the ICP status was unclear based on their examination findings (eg, papilledema) and other noninvasive investigations (eg, imaging). In our institution, the final decision to perform ICP monitoring is taken by a multidisciplinary team that includes neurosurgeons, neurologists, and neuroradiologists.
All patients received an ophthalmology examination during the ICP monitoring period. This included slitlamp biomicroscopy (with Frisen grading of papilledema and clinical assessment of SVP) and measurement of intraocular pressure by applanation tonometry. The retina and optic disc were then examined using the Spectralis OCT system (Heidelberg Engineering). Mean thickness of the retinal nerve fiber layer in a 1.7-mm circle around each disc and an objective measurement of the cup-disc diameter ratio were calculated. Ten-second IR videos of the patients’ optic discs were recorded. The whole ophthalmology examination was performed with the patient in sitting position. Simultaneous ICP was defined as the mean ICP (in mm Hg) measured over the same minute as the IR video recordings of SVP.
The IR video recordings were subsequently assessed independently by 2 neuro-ophthalmologists (F.D.B. and J.A.M.) masked to the ICP results. For each eye, SVP was graded using the system first proposed by Hedges3: 0, SVP absent; 1, up to 33% change in vessel diameter; 2, 33% to 66% change; or 3, more than 66% change. Patients with no observable SVP (grade 0) in both eyes, when assessed by both examiners, were considered to have absent SVP for the purposes of analysis.
The association between ICP and SVP (present or absent) was assessed using a multiple linear regression model. A P value of .05 was the statistical significance threshold. The following covariates were included: age, sex, presence of a CSF shunt, intraocular pressure, mean arterial pressure, retinal nerve fiber layer thickness, and cup-disc diameter ratio. To assess the predictive value of the absence of SVP, a receiver operating characteristics curve was built, and the area under the curve calculated. Stata, version 15.0 (StataCorp) was used for the statistical analysis.
Results
Overall, 105 consecutive patients fulfilled the selection criteria. The mean (SD) age was 39 (14) years (range, 18-78), and 79 (75%) were women. The clinical indications for ICP monitoring and the assessment results are summarized in Table 1 and Table 2. Overall, 91 patients (86.7%) had no evidence of disc swelling on either clinical examination or OCT, while 14 (13.3%) had subtle disc elevation but no clinically definite papilledema.
Table 1. Clinical Indications for 24-Hour ICP Monitoring.
| Indication | Patients, No. (%) | Simultaneous ICP, Mean (SD), mm Hg |
|---|---|---|
| Suspected CSF dynamics disorder causing headachea | 41 (39) | 3 (8) |
| Suspected CSF shunt malfunction | 34 (32) | 2 (11) |
| Known hydrocephalus with suspected raised ICP | 15 (14) | 1 (5) |
| Known Chiari malformation with suspected raised ICP | 13 (13) | 2 (5) |
| Suspected normal pressure hydrocephalus | 2 (2) | −2 (3) |
Abbreviations: CSF, cerebrospinal fluid; ICP, intracranial pressure.
For example, idiopathic intracranial hypertension and spontaneous intracranial hypotension.
Table 2. Patients’ Intracranial Pressure and Clinical Characteristicsa.
| Characteristic | SVP | P value | |
|---|---|---|---|
| Absent | Present | ||
| Patients, No. (%) | 14 (13) | 91 (87) | NA |
| Simultaneous ICP, mean (SD) [range], mm Hgb | 13 (14) [−12 to 36] | 1 (5) [−17 to 14] | <.001 |
| Simultaneous pulse amplitude, mean (SD)c | 10 (5) | 5 (2) | <.001 |
| 24-h ICP, mean (SD) [range], mm Hg | 16 (11) [−5 to 30] | 4 (5) [−11 to 24] | <.001 |
| 24-h Pulse amplitude, mean (SD), mm Hg | 9 (4) | 5 (2) | <.001 |
| Night ICP (supine), mean (SD) [range], mm Hg | 21 (8) [1 to 31] | 8 (5) [−5 to 25] | <.001 |
| MAP, mean (SD), mm Hg | 89 (13) | 92 (9) | .28 |
| IOP, mean (SD), mm Hg | 16 (3) | 15 (3) | .25 |
Abbreviations: ICP, intracranial pressure; IOP, intraocular pressure; MAP, mean arterial pressure; NA, not applicable; SVP, spontaneous venous pulsation.
1 mm Hg = 1.36 cm H2O.
Simultaneous ICP is the mean ICP (in mm Hg) over the same minute as the infrared video recording.
Simultaneous pulse amplitude is the mean ICP pulse amplitude (in mm Hg) over the same minute as the infrared video recording.
Spontaneous retinal venous pulsation was initially assessed by slitlamp examination and recorded as absent in 52 patients (49.5%) (bilateral SVP grade 0), present in 51 patients (48.6%) (SVP grade ≥1 in at least 1 eye), and difficult to assess in 2 patients (0.02%). When SVP was assessed using motion-stabilized IR video recordings, only 14 patients (13.3%) had absent SVP (grade 0 bilaterally), and the remaining 91 patients (86.7%) had SVP (at least grade 1 SVP in at least 1 eye). The 2 independent observers agreed on the presence or absence of SVP in 200 eyes (95.2%) and the interrater reliability was 0.82 (Cohen κ). In the 5 cases in which the observers disagreed, the discrepancy was only due to a single SVP grade.
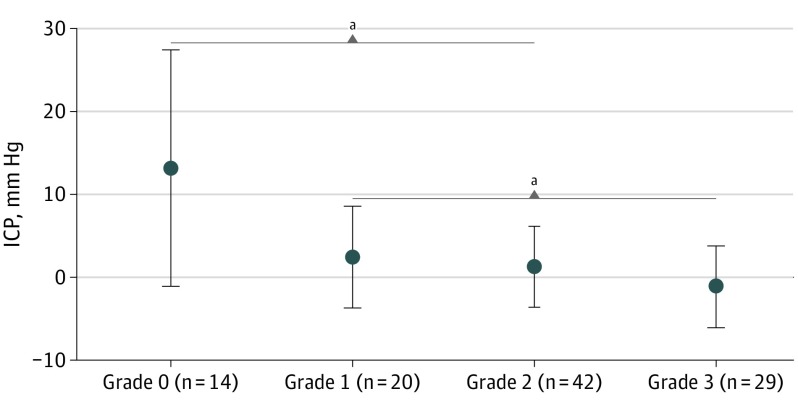
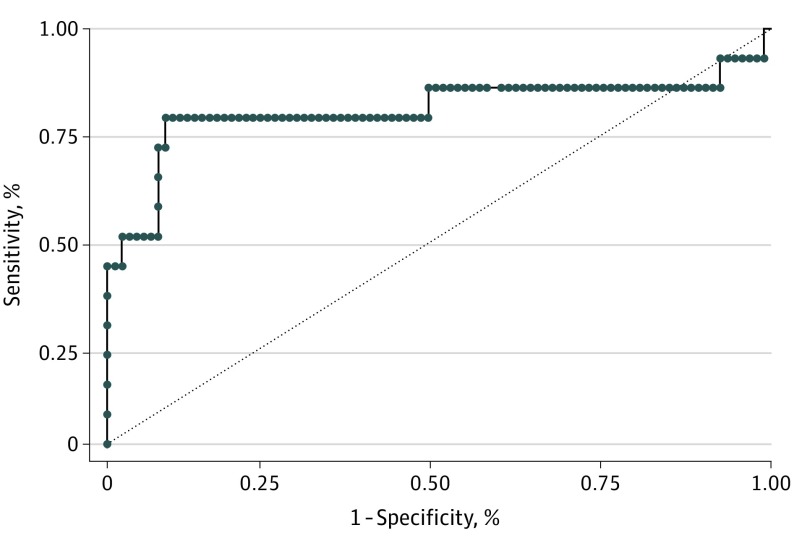
Simultaneous ICP measurements by SVP grade are displayed in Figure 1. The mean simultaneous ICP was significantly higher in the group of patients with absent SVP (95% CI, −16.3 to −8.4; P < .001). An unadjusted linear regression demonstrated a significant association between simultaneous ICP and SVP group (β = −12.4; 95% CI, −16.4 to −8.3; P < .001; R2 = 0.26). The validity of this association was also confirmed after adjusting for the 7 confounders (β = −9.1; 95% CI, −13.7 to −4.6; P < .001; R2 = 0.42). The receiver operating characteristics analysis showed an area under the curve of 0.80 (SE, 0.09; 95% CI, 0.62-0.69) (Figure 2).
Figure 1. Mean (SD) Simultaneous Intracranial Pressure (ICP) Measurements by Spontaneous Venous Pulsation Grade.
aUnpaired t test, P < .001; 95% CI, −16.3 to −8.4.
Figure 2. Receiver Operating Characteristics Curve Plotting the Predictive Value of Spontaneous Venous Pulsation in Determining Intracranial Pressure.
Area under the receiver operating characteristic curve = 0.8046.
Discussion
The debate about the validity and usefulness of the relationship between SVP and ICP is longstanding.5,12,13,14 A large study conducted by Wong and White13 evaluated SVP and ICP in 106 patients undergoing lumbar punctures and concluded that SVP is not a reliable predictor of ICP. A significant limitation of their study is that CSF pressure and SVP were assessed in different body positions (lateral decubitus and sitting), not taking into account the physiological ICP changes that occur with posture.15 Our study overcomes this issue through the simultaneous assessment of ICP and SVP in sitting position, and the results confirm that under these conditions there is a significant association between ICP and SVP.
Limitations
A limitation of our study is that the OCT systems are not portable and can only be used to examine patients in sitting position. This technique is thus limited in its applicability to patients with severe illness. Moreover, fundus video interpretation requires experienced assessors to identify SVP. Automated systems able to quantify SVP would reduce dependence on expert assessors, potentially facilitating its application in environments with limited access to experienced clinicians. Further limitations of this study are the small number of patients with absent SVP and the heterogeneity of the group.
Conclusions
These results confirm that there is a significant association between SVP and ICP, thereby support the utility of performing SVP assessments using OCT IR video recordings in patients with suspected abnormal CSF pressure. Further work is needed to develop a technique that could be used in bedbound patients and to automate the assessment of SVP.
References
- 1.Morgan WH, Hazelton ML, Yu DY. Retinal venous pulsation: expanding our understanding and use of this enigmatic phenomenon. Prog Retin Eye Res. 2016;55:82-107. doi: 10.1016/j.preteyeres.2016.06.003 [DOI] [PubMed] [Google Scholar]
- 2.Jacks AS, Miller NR. Spontaneous retinal venous pulsation: aetiology and significance. J Neurol Neurosurg Psychiatry. 2003;74(1):7-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hedges TR Jr, Baron EM, Hedges TR III, Sinclair SH. The retinal venous pulse: its relation to optic disc characteristics and choroidal pulse. Ophthalmology. 1994;101(3):542-547. doi: 10.1016/S0161-6420(94)31302-9 [DOI] [PubMed] [Google Scholar]
- 4.Levine DN, Bebie H. Phase and amplitude of spontaneous retinal vein pulsations: an extended constant inflow and variable outflow model. Microvasc Res. 2016;106:67-79. doi: 10.1016/j.mvr.2016.03.005 [DOI] [PubMed] [Google Scholar]
- 5.Levin BE. The clinical significance of spontaneous pulsations of the retinal vein. Arch Neurol. 1978;35(1):37-40. doi: 10.1001/archneur.1978.00500250041009 [DOI] [PubMed] [Google Scholar]
- 6.Lorentzen SE. Incidence of spontaneous venous pulsation in the retina. Acta Ophthalmol (Copenh). 1970;48(4):765-770. [PubMed] [Google Scholar]
- 7.Legler U, Jonas JB. Assessment of the spontaneous pulsations of the central retinal vein in daily ophthalmic practice. Clin Exp Ophthalmol. 2007;35(9):870-871. doi: 10.1111/j.1442-9071.2007.01641.x [DOI] [PubMed] [Google Scholar]
- 8.Harder B, Jonas JB. Frequency of spontaneous pulsations of the central retinal vein. Br J Ophthalmol. 2007;91(3):401-402. doi: 10.1136/bjo.2006.103341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McHugh JA, D’Antona L, Toma AK, Bremner F. Spontaneous venous pulsations detected with infrared videography. J Neuroophthalmol. In press. [DOI] [PubMed] [Google Scholar]
- 10.Chari A, Dasgupta D, Smedley A, et al. Intraparenchymal intracranial pressure monitoring for hydrocephalus and cerebrospinal fluid disorders. Acta Neurochir (Wien). 2017;159(10):1967-1978. doi: 10.1007/s00701-017-3281-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thompson SD, Coutts A, Craven CL, Toma AK, Thorne LW, Watkins LD. Elective ICP monitoring: how long is long enough? Acta Neurochir (Wien). 2017;159(3):485-490. doi: 10.1007/s00701-016-3074-z [DOI] [PubMed] [Google Scholar]
- 12.Walsh TJ, Garden JW, Gallagher B. Obliteration of retinal venous pulsations during elevation of cerebrospinal-fluid pressure. Am J Ophthalmol. 1969;67(6):954-956. doi: 10.1016/0002-9394(69)90094-4 [DOI] [PubMed] [Google Scholar]
- 13.Wong SH, White RP. The clinical validity of the spontaneous retinal venous pulsation. J Neuroophthalmol. 2013;33(1):17-20. doi: 10.1097/WNO.0b013e3182622207 [DOI] [PubMed] [Google Scholar]
- 14.Van Uitert RL, Eisenstadt ML. Venous pulsations not always indicative of normal intracranial pressure. Arch Neurol. 1978;35(8):550. doi: 10.1001/archneur.1978.00500320070022 [DOI] [PubMed] [Google Scholar]
- 15.Andresen M, Hadi A, Petersen LG, Juhler M. Effect of postural changes on ICP in healthy and ill subjects. Acta Neurochir (Wien). 2015;157(1):109-113. doi: 10.1007/s00701-014-2250-2 [DOI] [PubMed] [Google Scholar]