Abstract
Patient: Male, 24
Final Diagnosis: Bee sting conjunctival injury
Symptoms: Eye pain • red eye
Medication: —
Clinical Procedure: Ablation of the bee sting
Specialty: Ophthalmology
Objective:
Unusual clinical course
Background:
Ocular bee stings have been rarely described in the literature, and their management is controversial. A case of conjunctival bee sting with retention of the stinger for 48 hours is presented with a review of the literature on the complications and management of ocular bee sting injury.
Case Report:
A 22-year-old beekeeper presented to the Emergency Department with mild symptoms from a conjunctival bee sting that he had received 48 hours previously. The stinger was removed in the Emergency Department, and topical antibiotic and anti-inflammatory treatment with corticosteroid were given. There were no complications in this case. However, review of the literature has shown that although the outcome from ocular bee stings can be mild, as in this case, ocular bee stings can result in severe visual symptoms that require amniotic membrane transplant (AMT). Management commonly includes removal of the stinger and both topical and systemic treatment with corticosteroids. The main complications include cataracts, inflammation of the anterior chamber, optic neuropathies, and changes in ocular pressure.
Conclusions:
Ocular bee stings have been rarely described in the literature, and the management remains controversial. As this case has shown, removal of the stinger and the use of topical treatment with antibiotics and corticosteroids can prevent potentially serious complications that may affect vision. Early and regular follow-up with ocular imaging may be required when symptoms persist.
MeSH Keywords: Adaptation, Ocular; Bees; Case Reports; Conjunctiva; Cornea
Background
Bee stings commonly occur and can lead to complications, the most serious of which is systemic anaphylaxis to bee venom [1]. Although rare, ocular bee stings can result in significant complications, including the spread of venom and its components, particularly when the sting is not removed quickly. Although cases of ocular bee stings have been described in the literature, there have only been five previously published reports of conjunctival bee stings [2–6], and only one with conjunctival bee sting with retention of the stinger [6]. The management ocular bee sting remains controversial, and there are no established clinical recommendations for treatment of these lesions.
A case of conjunctival bee sting with retention of the stinger for 48 hours is presented with a review of the literature on the complications and management of ocular bee sting injury.
Case Report
A 22-year-old professional beekeeper attended our ophthalmic Emergency Department after being stung in the right eye 48 hours previously. Given the profession of the patient and the remaining bee abdomen still attached to the stinger, this injury was presumed to be from a bee sting. However, no additional studies were undertaken to identify that the stinger was due to a bee. The bee sting resulted in a red and very painful eye with photophobia and the sensation of a conjunctival foreign body.
On clinical examination, the patient’s visual acuity was normal (20/20) without any optical correction. On examination of the right eye, the bee stinger was seen to have penetrated the right conjunctiva at the periphery of the cornea at the 6 o’clock position and at 2 mm from the limbus. The stinger pointed towards the limbus and did not injure the sclera, but was associated with significant conjunctival hyperemia. The use of fluorescein eye drops (Fluorescéine sodique Faure 0.5%) showed a small conjunctival defect with retention of fluorescein in a small subconjunctival pocket surrounding the stinger (Figure 1).
Figure 1.

A 22-year-old beekeeper with a conjunctival bee sting injury of the right eye at Day 0 on hospital admission showing the stinger under the conjunctiva.
The cornea was not injured, the anterior chamber was not inflamed, and there was no sign of infection or intraocular inflammation. Intraocular pressure was normal.
The stinger was immediately removed with forceps (Visitec Forceps, Abingdon, Oxon, UK) under a slit lamp, after instillation of 1% tetracaine (Laboratoires Théa, Clermont-Ferrand, France). The stinger was completely removed.
No stitches were needed on the conjunctiva. Topical treatment of an antibiotic combined with corticosteroids for use four times daily for 30 days included dexamethasone 0.1% and tobramycin 0.3% eye drops (Novartis Pharma, Rueil-Malmaison, France) to prevent inflammation and the immune response to bee venom. The patient was not hospitalized but attended daily follow-up visits following removal of the stinger, and then every two days, eight days, 15 days, and then at one month. At Day 2 of follow-up, no complications were found, and all symptoms had disappeared. At one week after removal of the conjunctival bee stinger, the conjunctiva of the right eye appeared normal (Figure 2).
Figure 2.

A 22-year-old beekeeper with a conjunctival bee sting injury of the right eye at Day 7 following removal of the stinger shows good healing of the conjunctiva.
Discussion
During a bee sting, the stinger passes through the tissue structures and attaches like a harpoon, preventing its removal. The bee is forced to lose its stinger and part of its abdomen, which results in the death of the bee (Figures 1, 2). The stinger contains a pocket of venom released from the abdomen of the bee, which is propelled by contraction for about 30 to 60 seconds, including after the bee releases the stinger (Figure 3–5) [7]. In some cases, including the present case, the withdrawal of the stinger, and topical treatment with steroidal anti-inflammatory agents and antibiotics is sufficient to treat the bee sting. In more severe cases, surgical treatment may be necessary, including penetrating keratoplasty or Descemet stripping automated endothelial keratoplasty (DSAEK).
Figure 3.
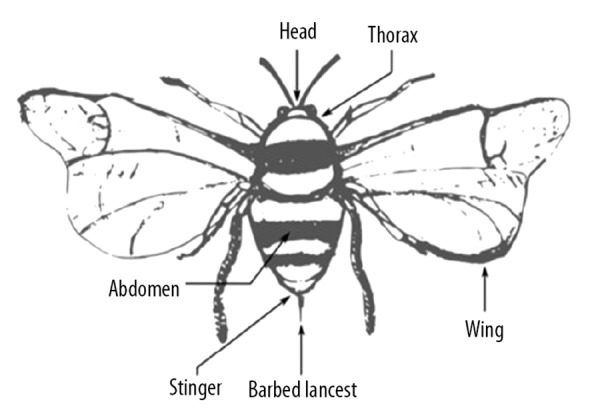
Simplified anatomy of the bee, showing the dorsal view. Artwork by first author, Axelle Semler-Collery.
Figure 4.
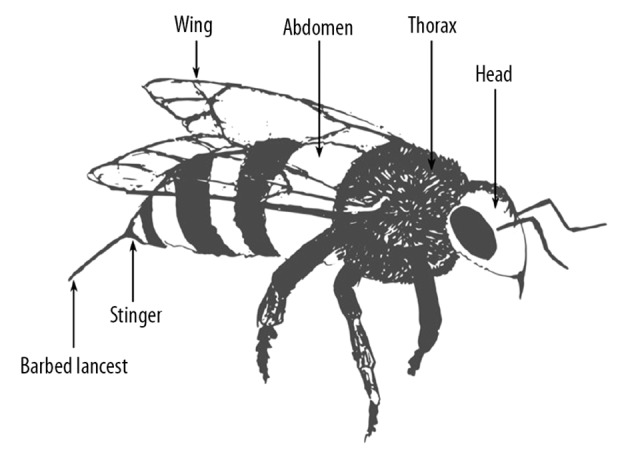
Simplified anatomy of the bee, showing the side view. Artwork by first author, Axelle Semler-Collery.
Figure 5.
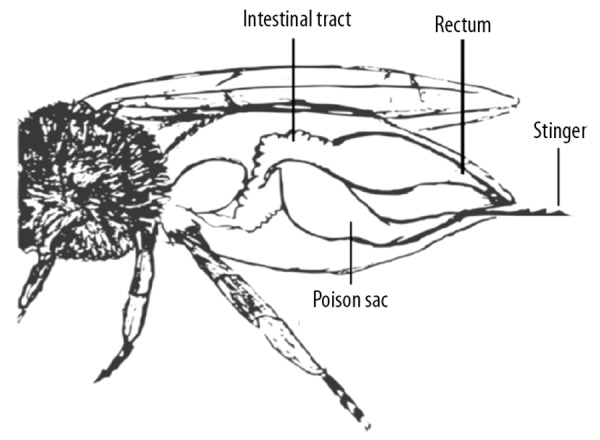
Simplified anatomy of the bee, showing the abdominal anatomy. Artwork by first author, Axelle Semler-Collery.
Review of the literature has identified 35 previous publications that have included 56 reported cases of ocular bee stings. However, only five previous publications of conjunctival bee stings have been reported [2–6], and only one previous report has been of conjunctival bee sting with retention of the stinger [6]. This review has allowed an evaluation of the different clinical presentations and complications of ocular bee stings and their management. The majority of previously published cases involved corneal bee stings (51 cases), and there were five cases of conjunctival bee stings (9%) [2–6]. Six publications described cases of periocular bee stings [8,9] and palpebral bee stings [10–13], and in two publications, ocular complications were described that included blepharochalasis and optic neuropathy [8,9].
Four previously published reports described allergic and inflammatory complications associated with the release of the components of bee venom, including the polypeptides melittin and apamin, and the enzymes hyaluronidase and phospholipase A2 [14–17]. Melittin is believed to be involved in the development of cataract by denaturing protein and has an affinity for cell membranes [18–22]. Histology of the cornea following bee sting injury has shown the presence of crystals that may contain melittin with associated fibrosis and inflammation [23]. Apamin can cause optic neuropathy due to its neurotoxic properties [6,20,21,24]. Variability of symptoms have been described, depending on the differences in the composition of bee venom and the quantity of bee venom injected [20,25,26].
The possible complications in cases of conjunctival or corneal bee stings are listed in Table 1. In more than 70% of previous publications, there was conjunctival hyperemia associated with conjunctival edema on initial examination, which indicated a local inflammatory reaction due to the components of bee venom [17]. In 60% of cases, there was a visible corneal stromal inflammation around the bee sting site, and in 40% of cases, there was associated edema of the eyelid. There were five main complications identified that had an impact on vision, including inflammation of the anterior chamber, cataracts, ocular pressure abnormalities, cellular alterations of the corneal endothelium, and optic neuropathies. Tables 2 and 3 list the complications and the treatments used in either conjunctival or corneal bee stings.
Table 1.
Reported clinical symptoms following conjunctival or corneal bee sting.
| Clinical symptoms following conjunctival or corneal bee sting | |
|---|---|
| Keratitis | Raised intraocular pressure |
| Kerato-uveitis | Bullous keratopathy |
| Corneal edema | Choroidal detachment |
| Cataracts | Choroidal atrophy |
| Iris atrophy | Macular striae |
| Endothelial cell loss | Vitreous infiltration |
| Optic neuropathy | Staphyloma |
| Hyphema | Dermatochalasis |
| Hypopion | Muscular paralysis |
| Toxic endophthalmitis | |
Table 2.
| Author | Case | Sex | Age | Visual acuity before treatment | Visual acuity after treatment | Removal | Complications | Topical treatment | Systemic treatment | Surgical treatment | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Uveitis | Cataract | IOP | Endothelial changes | Optic neuropathy | ||||||||||
| Isawumi et al. [2] | 1 | M | 62 | 20/20 | 20/20 | Yes | No | No | No | No | No | Yes | Yes | No |
| Szeghy et al. [5] | 1 | M | 22 | 20/1000 | 20/32 | Yes | Yes | Yes | No | No | No | Yes | No | No |
| Rishi et al. [4] | 1 | M | 19 | 20/60 | 20/20 | Yes | Yes | No | Yes | No | No | Yes | Yes | No |
| Lin et al. [6] | 1 | M | 43 | 20/30 | 20/30 | Yes | No | No | No | No | No | Yes | No | No |
| Choi et al. [3] | 1 | M | 46 | LP | 20/20 | Yes | Yes | No | No | No | Yes | Yes | Yes | No |
IOP – increased intraocular pressure.
Table 3.
Treatment of conjunctival and corneal bee stings, from previously reported cases.
| Characteristic | Average (range) | % |
|---|---|---|
| Age (years) | 31 (3–70) | |
|
| ||
| Gender | ||
| Male | 81.82% | |
| Female | 18.18% | |
|
| ||
| Stinger removed | 79.55% | |
|
| ||
| Complications presented | ||
| Uveitis | 59.09% | |
| Cataract | 34.09% | |
| Raised intraocular pressure (IOP) | 18.18% | |
| Endothelium alteration | 29.55% | |
| Optic neuropathy | 2.27% | |
| Worse symptoms following stinger removal | 31.82% | |
| Received topical treatment | 88.64% | |
| Received systemic treatment | 52.27% | |
| Required additional surgical treatment | 27.27% | |
There is controversy regarding the removal of the bee stinger in the management of ocular been stings, as early complications have been highlighted following removal. Manipulation of the stinger retained in the cornea can cause severe inflammatory reactions from the release of toxins, causing new complications [25–28], or by preventing complete healing of the lesions [29]. The surgical removal of the stinger may be complicated and can result in additional corneal scarring after removal [30]. These complications can cause reduced visual acuity by altering the transparency of the cornea, depending on the initial location of the stinger, which may be either central or paracentral [27]. Retention of the bee stinger combined with appropriate treatment has been described by some authors where the distal portion of the stinger is left in place, especially when local complications or inflammation were present [21,24,25,31].
A previously published case described by Gilboa et al. showed that a stinger left in place for many years could be inert and not cause any complication, with a description of a stinger retained for 28 years. Among the eight cases from the literature where stingers were left in place [20,24–26,32,33], four of the cases had complications of ocular inflammation [20,24,32], and three cases had cataracts [20,33]. In one case, it was not possible to determine whether increased inflammation was due to the attempted withdrawal of the stinger or persistence of a portion of the stinger in a patient without other types of treatment [32].
Some authors have recommended the withdrawal of the bee stinger [6,32–35]. However, on review of previously published studies, treatment included the withdrawal of the stinger and topical treatment with steroidal anti-inflammatory drugs combined with topical and systemic antibiotics, and some authors have described surgical removal techniques. For example, Chauhan et al. [35] recommended the use of an ophthalmic endoilluminator during the procedure. A detailed examination is always necessary before removal of the bee stinger, including eyelid eversion, especially when the stinger is not found at the site of the lesion [36]. The introduction of systemic treatment with corticosteroids is also widely recommended and seems to prevent complications or increase their resolution [3,13,32,34,37–39]. On review of the previously reported cases, there were 43 stinger removals, 17 cases of clinical exacerbation following the withdrawal of the stinger (approximately 40% of cases), with only one patient who did not follow the prescribed postoperative medical instructions [40]. Analysis of the 17 cases that had worse symptoms following the withdrawal of the stinger, 59% of the cases did not receive systemic corticosteroid treatment (Table 3).
Gudiseva et al. [37] described the largest number of previously reported cases of ocular bee stings, in which six out of 11 patients, including five patients treated with systemic corticosteroids, did not have any symptoms following the withdrawal of the bee stinger. However, five patients who only received topical treatment developed complications, including cataracts, increased intraocular pressure, and uveitis [37]. These findings support the use of combined systemic and topical treatment, rather than the use of topical treatment alone [37]. In some reports, surgical treatment was sometimes required during follow-up, including the use of phacoemulsification [41,42], external trabeculectomy [24,37], penetrating keratoplasty [6,23,37,41], or Descemet stripping automated endothelial keratoplasty (DSAEK) [43]. Several case reports showed a favorable outcome following washing of the anterior chamber with balanced salt solution (BSS) combined with the surgical removal of the stinger [17,34,38,41,44].
Following further analysis of the published cases of conjunctival bee stings [2–6], four of these five cases did not show stinger retention, as described in the present case. The only previously published case that described a conjunctival lesion with persistent stinger did not describe the method of removal of the bee stinger [6]. However, this previous case report was similar to the present case, with an isolated lesion without associated deep ocular inflammation, treated with topical eye drops, and with a good short-term outcome [6]. In this case, slit lamp removal and treatment with topical antibiotic eye drops and corticosteroids showed satisfactory results on patient follow-up. In the five previously published cases of conjunctival bee stings, complications were described following conjunctival suturing, in two out of five cases, which should encourage vigilant follow-up of these patients. In one of these two cases, optic neuropathy [3] was described only a few hours after the bee sting. In the second case, the conjunctival lesion was complicated by extensive uveitis with iris atrophy, pupillary siderosis, and secondary cataract [5].
Additional examinations in cases of ocular bee sting include the use of optical coherence tomography (OCT) of the anterior chamber [32,33], which makes it possible to identify and time the surgical removal of the bee stinger by determining the extent of the lesion and its localization. OCT can also be useful postoperatively in evaluating the total resection of the stinger. The use of confocal microscopy can make it possible to visualize the presence of corneal residues, which may be responsible for the persistence of local inflammation [31,45]. Finally, the use of specular microscopy of the corneal endothelium [22,35,46,47] appears to be an important examination method for use in patient follow-up for patients who have alterations of the corneal endothelium, in particular for the evaluation of endothelial cell loss, which can be important in the context of corneal bee stings [22,24,28,35,38].
From the review of the literature and the cumulative experience from previously reported cases of ocular bee stings, some lessons can be learned regarding the optimal initial management. The affected eye can be rinsed with a sterile normal saline solution and treated with topical anti-inflammatory eye drops and antibiotics. An ophthalmological evaluation is necessary to correctly visualize the lesion under a slit lamp and remove the stinger, if it is accessible. If the stinger is inserted too deeply, surgical intervention may be necessary to extract it. Also, careful follow-up is required to re-evaluate the affected eye and to ensure that healing has occurred and that there are no complications that may impair vision in the patient with a previous ocular bee sting, including conjunctival bee sting.
Conclusions
Ocular bee sting injuries are rare but can have serious complications that include cataracts, uveitis, raised intraocular pressure, and optic neuropathies. A thorough examination of the eye is required to identify and remove the bee sting and may require the use of additional methods of examination, including confocal microscopy, optical coherence tomography (OCT) of the anterior chamber, and specular microscopy of the corneal endothelium. Although there are no treatment guidelines, management includes the withdrawal of the stinger and the use of topical anti-inflammatory eye drops and antibiotics combined with systemic corticosteroid treatment. Careful and frequent follow-up is required to ensure that there are no complications in the first few weeks following initial treatment and to ensure that vision in the affected eye is preserved.
Footnotes
Conflict of interest
None.
References:
- 1.Mingomataj EÇ. Unusual reactions to hymenoptera stings: What should we keep in mind? Clin Rev Allergy Immunol. 2014;1:91–99. doi: 10.1007/s12016-014-8434-y. [DOI] [PubMed] [Google Scholar]
- 2.Isawumi MA, Hassan M. Honeybee sting of the sclera: Ocular features, treatment, outcome and presumed pathogenesis. Pan Afr Med J. 2014;17:30. doi: 10.11604/pamj.2014.17.30.3297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Choi MY, Cho SH. Optic neuritis after bee sting. Korean J Ophthalmol. 2000;14:49–52. doi: 10.3341/kjo.2000.14.1.49. [DOI] [PubMed] [Google Scholar]
- 4.Rishi E, Rishi P. Intraocular inflammation in a case of bee sting injury. GMS Ophthalmol Cases. 2018;8 doi: 10.3205/oc000084. Doc02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Szeghy G, Pápai IC, Vas Z. [To note the eye injury caused by bee sting] Ophthalmologica. 1963;146:74–82. doi: 10.1159/000304500. [in German] [DOI] [PubMed] [Google Scholar]
- 6.Lin PH, Wang NK, Hwang YS, et al. Bee sting of the cornea and conjunctiva: Management and outcomes. Cornea. 2011;30:392–94. doi: 10.1097/ICO.0b013e3181f234a6. [DOI] [PubMed] [Google Scholar]
- 7.Winston ML. The biology of the honey bee. USA: Harvard University Press; 1991. [Google Scholar]
- 8.Berríos RR, Serrano LA. Bilateral optic neuritis after a bee sting. Am J Ophthalmol. 1994;117:677–78. doi: 10.1016/s0002-9394(14)70084-4. [DOI] [PubMed] [Google Scholar]
- 9.Finney JL, Peterson HD. Blepharochalasis after a bee sting. Plast Reconstr Surg. 1984;73:830–32. doi: 10.1097/00006534-198405000-00021. [DOI] [PubMed] [Google Scholar]
- 10.Wiwatwongwana D. Eyelid bee sting with late migration onto the cornea after primary removal: The mystery of the bee stinger. Arch Ophthalmol. 2012;130:392. doi: 10.1001/archopthalmol.2011.1796. [DOI] [PubMed] [Google Scholar]
- 11.Zambrano-Infantino RC, Piñieríia-Gonsálvez JF, Montaño C, Rodríguez C. Optic neuritis after a bee sting. Invest Clin. 2013;54:180–85. [PubMed] [Google Scholar]
- 12.Chaurasia S, Muralidhar R. Retained bee stinger in the tarsal plate. Int Ophthalmol. 2011;31:111–12. doi: 10.1007/s10792-011-9418-z. [DOI] [PubMed] [Google Scholar]
- 13.Maltzman JS, Lee AG, Miller NR. Optic neuropathy occurring after bee and wasp sting. Ophthalmology. 2000;107:193–95. doi: 10.1016/s0161-6420(99)00020-2. [DOI] [PubMed] [Google Scholar]
- 14.Chen CJ, Richardson CD. Bee sting-induced ocular changes. Ann Ophthalmol. 1986;18:285–86. [PubMed] [Google Scholar]
- 15.Sobotka AK, Franklin RM, Adkinson FJ, et al. Allergy to insect stings. J Allergy Clin. Immunol. 1976;57:29–40. doi: 10.1016/0091-6749(76)90076-2. [DOI] [PubMed] [Google Scholar]
- 16.Çaça I, Ari S, Ülü K, Ayata A. Bee sting of the cornea: A case study and review of the literature. Ann Ophthalmol. 2006;38:77–80. doi: 10.1385/ao:38:1:77. [DOI] [PubMed] [Google Scholar]
- 17.Yildirim N, Erol N, Basmak H. Bee sting of the cornea: A case report. Cornea. 1998;17:333–34. doi: 10.1097/00003226-199805000-00015. [DOI] [PubMed] [Google Scholar]
- 18.King TP, Spangfort MD. Structure and biology of stinging insect venom allergens. Int Arch Allergy Immunol. 2000;123:99–106. doi: 10.1159/000024440. [DOI] [PubMed] [Google Scholar]
- 19.Ghosh SK, Chattopadhyay D, Sen AC, Chakrabarti B. Melittin-induced conformational changes in human lens protein. Curr Eye Res. 1991;10:1065–68. doi: 10.3109/02713689109020345. [DOI] [PubMed] [Google Scholar]
- 20.Limaiem R, Chaabouni A, El Maazi A, et al. [Ocular lesions by bee sting. About a case] Journal Français d’Ophtalmologie. 2009;32:277–79. doi: 10.1016/j.jfo.2009.01.007. [in French] [DOI] [PubMed] [Google Scholar]
- 21.Smith DG, Roberge RJ. Corneal bee sting with retained stinger. J Emerg Med. 2001;20:125–28. doi: 10.1016/s0736-4679(00)00298-5. [DOI] [PubMed] [Google Scholar]
- 22.Gürlü VP, Erda N. Corneal bee sting-induced endothelial changes. Cornea. 2006;25:981–83. doi: 10.1097/01.ico.0000226364.57172.72. [DOI] [PubMed] [Google Scholar]
- 23.Nassif KF, Hyndiuk RA, Hatchell DL, et al. Bee sting to the cornea: A clinical and microscopic evaluation. Cornea. 1982;1(4):325–30. [Google Scholar]
- 24.Teoh SC, Lee JJ, Fam HB. Corneal honeybee sting. Can J Ophthalmol. 2005;40:469–71. doi: 10.1016/S0008-4182(05)80008-0. [DOI] [PubMed] [Google Scholar]
- 25.Gilboa M, Gdal-On M, Zonis S. Bee and wasp stings of the eye. Retained intralenticular wasp sting: A case report. Br J Ophthalmol. 1977;61:662–64. doi: 10.1136/bjo.61.10.662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arcieri ES, França ET, de Oliveria HB, et al. Ocular lesions arising after stings by hymenopteran insects. Cornea. 2002;21:328–30. doi: 10.1097/00003226-200204000-00019. [DOI] [PubMed] [Google Scholar]
- 27.Ang MJ, Kadir SZ, Fadzillah AJ, Zunaina E. A case series of bee sting keratopathy with different outcomes in Malaysia. Cureus. 2017;9(2):e1035. doi: 10.7759/cureus.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chuah G, Law E, Chan WK, Ang CL. Case reports and mini review of bee stings of the cornea. Singapore Med J. 1996;37:389–91. [PubMed] [Google Scholar]
- 29.Jain V, Shome D, Natarajan S. Corneal bee sting misdiagnosed as viral keratitis. Cornea. 2007;26:1277–78. doi: 10.1097/ICO.0b013e31814b8bae. [DOI] [PubMed] [Google Scholar]
- 30.Höllhumer R, Carmichael TR. Bee sting of the cornea: A running case report. Afr Vision Eye Health. 2015;74(1) Art. 288. [Google Scholar]
- 31.Yuen K, Lai J, Law R, Lam D. Confocal microscopy in bee sting corneal injury. Eye. 2003;17:845–47. doi: 10.1038/sj.eye.6700425. [DOI] [PubMed] [Google Scholar]
- 32.Rai RR, Gonzalez-Gonzalez LA, Papakostas TD, et al. Management of corneal bee sting injuries. Semin Ophthalmol. 2017;32:177–81. doi: 10.3109/08820538.2015.1045301. [DOI] [PubMed] [Google Scholar]
- 33.Sá A, Arruda S, Cohen MJ, Furtado JM. Presumed bee stinger retained intraocularly in the absence of inflammation. JAMA Ophthalmol. 2015;133:222. doi: 10.1001/jamaophthalmol.2014.4353. [DOI] [PubMed] [Google Scholar]
- 34.Hasanee K, Carlsson A, ten Hove MW. Corneal bee sting: Full-thickness penetration in a patient wearing a contact lens. Can J Ophthalmol. 2004;39:548–51. doi: 10.1016/s0008-4182(04)80148-0. [DOI] [PubMed] [Google Scholar]
- 35.Chauhan D. Corneal honey bee sting: Endoilluminator-assisted removal of retained stinger. Int Ophthalmol. 2012;32:285–88. doi: 10.1007/s10792-012-9553-1. [DOI] [PubMed] [Google Scholar]
- 36.Bhalerao S, Singh P, Rani P, Rathi V. The sting of a honey bee: An unusual subconjunctival foreign body. Indian J Ophthalmol. 2017;65:1226–28. doi: 10.4103/ijo.IJO_533_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gudiseva H, Uddaraju M, Pradhan S, et al. Ocular manifestations of isolated corneal bee sting injury, management strategies, and clinical outcomes. Indian J Ophthalmol. 2018;66(2):262–68. doi: 10.4103/ijo.IJO_600_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim JH, Kim M, Lee SJ, et al. Corneal bee sting controlled with early surgical intervention and systemic high-dose steroid therapy. Case Rep Ophthalmol Med. 2014;2014:140626. doi: 10.1155/2014/140626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fard AM, Pourafkari L, Nader ND. Cornea bee sting. QJM. 2015;108(11):911. doi: 10.1093/qjmed/hcv090. [DOI] [PubMed] [Google Scholar]
- 40.Glover LP. Bee sting of the cornea. Am J Ophthalmol. 1943;26:744. [Google Scholar]
- 41.Ahmed M, Lee CS, McMillan B, et al. Predicting visual function after an ocular bee sting. Int Ophthalmol. 2018 doi: 10.1007/s10792-018-0978-z. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 42.Pal N, Azad RV, Sharma YR, et al. Bee sting-induced ciliochoroidal detachment. Eye. 2005;19:1025–26. doi: 10.1038/sj.eye.6701720. [DOI] [PubMed] [Google Scholar]
- 43.Hammel N, Bahar I. Descemet-stripping automated endothelial keratoplasty after bee sting of the cornea. J Cataract Refract Surg. 2011;37(9):1726–28. doi: 10.1016/j.jcrs.2011.06.020. [DOI] [PubMed] [Google Scholar]
- 44.Vélez M, Mannis MJ, Ortega JG, Tobón CA. Corneal hymenoptera stings: A new therapeutic approach. Vis Pan-Am. 2012;11(4):117–19. [Google Scholar]
- 45.Razmjoo H, Abtahi MA, Roomizadeh P, et al. Management of corneal bee sting. Clin Ophthalmol. 2011;5:1697–700. doi: 10.2147/OPTH.S26919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Siddharthan K, Raghavan A, Revathi R. Clinical features and management of ocular lesions after stings by hymenopteran insects. Indian J Ophthalmol. 2014;62:248–51. doi: 10.4103/0301-4738.128637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tuft SJ, Crompton DO, Coster DJ. Insect sting in a cornea. Am J Ophthalmol. 1985;99:727–28. doi: 10.1016/s0002-9394(14)76051-9. [DOI] [PubMed] [Google Scholar]


