Abstract
Background
Although there is growing theoretical and empirical support for the proposition that media exposure to conflicting health information negatively influences public understanding and behavior, few studies have causally linked exposure to conflict with undesirable outcomes. Such outcomes might be particularly likely in the context of mammography, given widespread media attention to conflicting recommendations about the age at and frequency with which average-risk women should be screened for breast cancer.
Purpose
The current study tests whether exposure to conflicting information about mammography negatively influences women’s affective and cognitive responses and examines whether effects vary by socioeconomic position.
Methods
We conducted an online survey experiment in 2016 with a population-based sample of U.S. women aged 35–55 (N = 1,474). Participants were randomly assigned to one of four conditions that differed in the level of conflict about mammography presented in a news story (no, low, medium, or high conflict), stratifying by poverty level.
Results
Greater exposure to conflict increased women’s negative emotional responses to the story they read, their confusion about and backlash toward cancer prevention recommendations and research, and their ambivalence about mammography and other types of cancer screening, though ambivalence leveled off at high levels of exposure. There was little evidence that effects varied across socioeconomic position.
Conclusions
Findings add to the growing evidence base documenting undesirable outcomes of exposure to conflicting health information. Future research should examine whether the negative affective and cognitive responses observed translate into behavior, which could have implications for both health campaigns and patient-provider communication.
Keywords: Conflicting health information, Mammography, Population-based survey experiment, Socioeconomic position, Health communication
Women exposed to greater conflicting information about mammography reported negative emotional reactions, confusion about and backlash toward cancer prevention recommendations and research, and ambivalence about mammography and other types of cancer screening.
Introduction
For more than two decades, there has been substantial expert disagreement about the use of mammography to screen for breast cancer. This discord has accelerated in recent years, as professional organizations—including the U.S. Preventive Services Task Force (USPSTF), American Cancer Society (ACS), American College of Radiology (ACR), and American College of Obstetricians and Gynecologists (ACOG)—have issued conflicting recommendations about the age at and frequency with which average-risk women should be screened. In January 2016, the USPSTF reaffirmed its 2009 position [1] and recommended that women begin biennial routine screening at age 50 [2]. In contrast, ACS, which had long supported annual routine screening beginning at age 40, updated its guidelines in October 2015, recommending annual routine screening beginning at age 45 and biennial screening once a woman turns 55 [3]. ACOG recommends that women in their 40s have the option to initiate screening [4], whereas ACR continues to endorse routine annual screening beginning at age 40 [5].
Disagreement over mammography is not confined to professional circles, as new recommendations garner widespread media attention [6–10]. With each new recommendation, and each new study on breast cancer screening and mortality, journalists often invoke a conflict and controversy frame, reminding the public about expert disagreement over recommendations or how prior findings conflict with the latest research [9, 10]. For example, Young Lin and Rosenkrantz [11] found that controversy over screening was a theme in almost 30% of a convenience sample of online news stories about mammography over a 9-year-period. Given the breadth and intensity of this media coverage, it is not surprising that one-third to one-half of general U.S. population women perceive conflict and controversy over mammography [8, 12–14]. Yet awareness may not be distributed evenly across the population, as qualitative analyses suggest that awareness of mammography conflict and controversy may be lower among women from historically underserved populations [15, 16]; such unfamiliarity could influence how these women respond to such information when they ultimately encounter it.
Does awareness of mammography conflict and controversy produce undesirable affective, cognitive, and/or behavioral outcomes? Research suggests that such outcomes are plausible. For example, women have reported being confused about mammography recommendations, as documented in several survey [8, 14, 17] and focus group [15] studies. In addition, health services researchers, interested in whether mammography conflict and controversy has negatively influenced women’s screening behaviors, examined screening patterns following the USPSTF’s 2009 recommendation announcement. They found either no changes [18, 19] or small reductions in screening rates [20], if only initially [21]. Importantly, none of these studies directly addressed the role of media exposure in producing such outcomes. Only one study attempted to do so by randomly assigning women to read a news story that was either favorable or unfavorable toward the USPSTF 2009 recommendation change [22]. Researchers found no effects by condition, although overall women did report negative attitudes toward the recommendation change. However, participants were not actually exposed to conflicting or controversial information, as they read only a favorable or an unfavorable story. The goal of the current study is to test systematically whether exposure to conflicting information about mammography negatively influences women’s affective and cognitive responses. To accomplish this goal, we embedded an experimental design in a population-based survey of U.S. women aged 35–55, using a single news story as the basis for experimental stimuli in which the level of conflict—operationalized through reference to conflicting recommendations and the amount of conflict-laden language used to describe them—varied across conditions.
Effects of Exposure to Conflicting Health Information
Conflicting health information can be conceptualized as “two or more health-related propositions [statements or assertions about a health issue] that are logically inconsistent with one another” ([23], p. 1175). In the context of mammography, these are messages that provide competing propositions (initiate routine screening at age 40 vs. 45 vs. 50) about a particular behavior (mammography) resulting in a particular health outcome (breast cancer prevention) [24]. Given the conflicting or logically inconsistent recommendations, a woman who encounters this information must, in conversations with her provider, choose which recommendation to follow. Importantly, such informational conflict is often characterized by conflict-laden language that evokes controversy. A recent content analysis of news media coverage of mammography screening recommendations by the USPSTF and ACS found that coverage was often controversial in tone, with journalists explicitly highlighting expert debate and disagreement for the audience [10].
There is reason to expect effects of exposure to conflicting information about mammography, as a growing body of research has documented undesirable outcomes of media exposure to conflicting health information across a range of topics, including nutrition [25–27], the HPV vaccine [28], vaccines and autism [29], and dioxin regulation [30]. Studies to date have focused primarily on two cognitive responses: (i) confusion, or perceived ambiguity or uncertainty about the health topic in question [25, 29, 30] or health research in general [27]; and (ii) backlash, or negative beliefs or attitudes toward the health topic in question [25, 26] or health research in general [27]. Several studies have predicted such effects based on decision theory’s concept of ambiguity. Specifically, Ellsberg [31] posited that one important condition under which ambiguity may be high is “where there is conflicting opinion and evidence [emphasis in original]” (p. 659). Thus, exposure to conflicting information could give rise to perceived ambiguity—a state of uncertainty that is uncomfortable for many people. This discomfort, known as “ambiguity aversion,” can manifest itself in negative beliefs toward the subject of ambiguity [32, 33]. For instance, when people perceive ambiguity about nutrition recommendations and research (“nutrition confusion”), they become pessimistic and express negative beliefs toward such recommendations and research (“nutrition backlash”) [25, 34]. Similar cognitive responses have been observed in the context of cancer prevention recommendations more generally [32, 33].
Another potential cognitive response to conflicting health information is attitudinal ambivalence, whereby people hold both positive and negative evaluations of a given object at the same time [35–37]. Subjective ambivalence is “a psychological state of conflict associated with an attitude object,” and it is a function of one’s positive and negative thoughts or feelings toward that object ([37], p. 432). To the extent that exposure to conflicting information about mammography elicits both positive and negative thoughts, we might expect to observe greater ambivalence toward the object in question (mammography). For example, a woman might hear that screening can lead to early detection, which could generate positive thoughts, but also that it can increase the risk of harms such as false positives, which could generate negative thoughts. Although there is some evidence that exposure to conflict can produce ambivalence toward the health topic in question [26], this possibility has received little empirical attention.
It is conceivable that, when faced with conflicting information, women might experience ambivalence not only toward mammography but toward cancer screening more generally. This expectation is informed by growing evidence for carryover or spillover effects, whereby exposure to conflict in one health domain (e.g., mammography) carries over to other health domains (e.g., other types of cancer screening). Carryover effects are believed to operate through excitation transfer [25, 34]: Negative affect resulting from one emotion-arousing situation can trigger an enhanced reaction to another emotion-arousing situation [38]. If people are routinely exposed to conflicting information about mammography, the negative affect and cognitions resulting from each exposure (in the form of confusion and backlash) could build over time via repeated activation [39] and, in turn, affect responses to subsequent unrelated health messages or recommendations for behaviors about which there is little conflict (e.g., colorectal cancer screening).
Implicit in discussions of carryover effects is the expectation that media exposure to conflicting health information can produce negative emotional reactions. These potential affective responses have not been studied directly, but Nabi’s emotion-as-frame model [40, 41] provides additional theoretical rationale to expect such effects. The emotion-as-frame model suggests that when messages evoke discrete emotions, such as fear, anger, and hope, these guide cognitive efforts and attention which, in turn, influence risk perceptions, attitudes, and behaviors. In the context of media coverage of health issues, news stories that present topics in terms of threat would likely evoke fear among the public, stories that present topics as offering new solutions to existing health problems would likely evoke hope, and so forth [42]. It is therefore conceivable that news stories that present health topics in terms of conflict and controversy may evoke anger (e.g., frustration, annoyance) or distress among the public. Qualitative studies indicate that when people perceive a health issue to be marked by conflict and controversy, it can be met with frustration, annoyance, and distress [15, 43], but experimental tests of these relations are lacking.
Differential Effects of Exposure to Conflict: The Role of Socioeconomic Position
There is some evidence that awareness of mammography conflict and controversy may be lower among women from underserved populations [15, 16]—perhaps because this information fails to reach these women, or because it reaches them but they do not find it relevant or do not interpret it as conflicting or controversial. What is not known is whether exposure to mammography conflict and controversy differentially affects women from underserved populations, including those of lower socioeconomic position. Although numerous social determinants are recognized for their influence on health outcomes, the current study focuses on socioeconomic position because it is often considered the “fundamental cause” of health inequalities: Unequal distribution of prestige, power, resources, and knowledge can translate into disparities in medical treatment, environmental exposures, and other forms of inequality [44].
On the one hand, the effects of exposure to conflict could be stronger among populations of lower socioeconomic position. This possibility is consistent with a communication inequalities perspective, which recognizes differences in social groups’ abilities to access, attend to, process, retain, and act on information [45]. Viswanath and Emmons [46] posited that individuals of lower socioeconomic position may have greater difficulty “sorting through complex health messages [and] more difficulty reconciling conflicting messages” (p. S245), which could produce outcomes including frustration and confusion about cancer prevention research and recommendations [45]. On the other hand, it is possible that populations of lower socioeconomic position might be less responsive to exposure to conflict. Framing effects research has shown that the media can invite audiences to interpret information in particular ways, often consistent with their preexisting perceptions of a given issue [47, 48]. To the extent that women of lower socioeconomic position have distinct preexisting perceptions of mammography—perhaps because they are less aware of mammography conflict and controversy—they might respond to information about mammography differently than women of higher socioeconomic position [46]. If this is the case, then having less prior awareness could be protective: A woman who is minimally aware of mammography conflict and controversy might respond only to the conflict presented in the message, and thus her affective and cognitive responses would not be further affected by any prior exposure or knowledge. Ultimately, the existing literature does not enable a clear prediction about whether women of lower socioeconomic position will be more or less susceptible to conflicting messages.
The Current Study
The goal of the current study is to test experimentally whether media exposure to conflicting information about mammography negatively influences women’s affective and cognitive responses—specifically, negative emotional reactions, mammogram-specific cognitive responses (e.g., ambivalence about mammography), and more general cancer prevention- and screening-related cognitive responses (e.g., confusion about cancer prevention recommendations and research, backlash toward such recommendations and research, and ambivalence about other types of cancer screening). This study advances the existing literature on the effects of exposure to conflicting health information by using a single news story as the basis for the experimental stimuli, editing the story so that only the level of conflict varies across randomized conditions. In contrast, most experimental studies to date have operationalized exposure to conflict by randomly assigning participants to two different news stories or messages. For example, in some studies, participants were exposed either to two news stories that are consistent with one another on a given issue (i.e., convergent stories: no conflict exists) or to two news stories that are inconsistent with each other (i.e., divergent stories: conflict exists) [30, 49]. In other research, participants were exposed either to a one-sided message (positive or negative only: no conflict exists) or a two-sided message (both positive and negative: conflict exists) [27, 50]. We build on this prior work by operationalizing exposure to conflict as variation in the level of conflict present in a single news story, where the level of conflict is reflected both in the reference to conflicting recommendations and the amount of conflict-laden language used to describe them. This operationalization—which explicitly highlights conflict using a single news story—may ultimately be more powerful from a message effects perspective, as it does not rely on the audience noticing and recalling two or more stories and inferring conflict. Moreover, these explicit mentions have been documented in media coverage of health topics including nutrition and mammography [24].
Guided by Nabi’s emotion-as-frame model [40–42], as well as qualitative evidence of negative emotional reactions to conflicting messages [15, 43], we hypothesize a linear dose–response effect of exposure to conflict on negative affective responses. We predict that greater exposure to conflict will increase participants’ frustration, annoyance, and distress in response to the news story they read. We also ask whether increasing exposure to conflict will influence women’s mammogram-specific ambivalence, which has received limited attention [26] despite a clear theoretical rationale for expecting such effects [37]. In addition, we assess whether exposure to conflict will influence more general cancer prevention- and screening-related cognitive responses. First, given empirical evidence of negative cognitive responses [25–27, 29, 30] consistent with decision theory’s concept of ambiguity [31], we hypothesize a dose–response effect of exposure to conflict on confusion about and backlash toward cancer prevention recommendations and research, whereby increasing exposure will produce greater confusion and backlash. Second, given our interest in potential carryover effects [25, 34], we assess whether exposure to conflict will influence ambivalence toward other types of cancer screening. Looking across all outcome variables, we ask whether the effects of exposure to conflict vary by socioeconomic position. Because women of lower socioeconomic position could be more or less susceptible to such information [46], we examine its effect on each of the outcomes of interest.
Method
Participants and Procedure
We conducted an online survey experiment in 2016 with a population-based sample of U.S. women aged 35–55 (N = 1,474). We sampled women in this age range to maximize relevance of mammography conflict and controversy, as a key debate is whether women should begin screening in their 40s or 50s. The survey experiment was administered by GfK, a survey research firm that maintains a probability-based panel of ~55,000 U.S. adults aged 18 and older (KnowledgePanel). Population-based survey experiments allow researchers to make stronger causal claims than survey data alone, enable more time- and cost-effective data collection than laboratory experiments, and strengthen generalizability through their use of nationally representative samples [51]. Given a priori interests in assessing differential effects by socioeconomic position, we oversampled women living at or below 100% of the federal poverty level (n = 744); in 2016, the poverty threshold for a family of four with two children under age 18 was a household income of $24,339 [52]. The overall survey experiment completion rate among eligible panelists randomly selected to participate was 51.3%. The University of Minnesota Institutional Review Board approved this study.
Based on our expectations regarding a dose–response effect of increasing exposure to conflict, participants—stratified by poverty level—were randomly assigned to one of four conditions that differed in the level of conflict about mammography presented in a news story (no, low, medium, or high conflict). Stimuli were based on a real news story—published and/or syndicated in national, regional, and online news media outlets in 2014—that reported the results of a research study questioning the value of routine mammography screening. The low conflict condition most closely resembles the real news story on which the stimuli were based. Consistent with recommendations for identifying messages for experimental research [53], this story was identified through a content analysis of media coverage of mammography screening recommendations [10]. Participants in the no conflict condition did not view a news story because, given the inherent conflict and controversy around mammography, we could not ensure that all indicators of conflict would be removed; the mere mention of mammography could cue conflict for some participants.
Across low, medium, and high conflict conditions, news story stimuli varied only in the level of conflict presented. Level of conflict was operationalized through reference to conflicting recommendations and the amount of conflict-laden language used to describe them. Medium and high conflict news stories were edited to underscore conflict about mammography screening recommendations by including phrases such as “conflicting recommendations” and “contradictory guidelines,” as well as conflict-laden language that evokes controversy by referring to “[spurring] heated debate” and “scientists’ ongoing disagreement about the benefits of breast cancer screening” (see Supplementary Appendix for news story stimuli). The increasing conflict levels were substantiated by a Linguistic Inquiry and Word Count (LIWC) analysis of the news story stimuli [54]. We expected to observe a shift in the balance of positively and negatively valenced words as conflict increased. Consistent with expectations, the LIWC analysis showed that the low conflict story was characterized by largely positively valenced words (positive = 1.47, negative = 0.00), the medium conflict story was characterized by both positively and negatively valenced words (positive = 1.12, negative = 1.12), and the high conflict story was characterized by more negatively than positively valenced words (positive = 1.01, negative = 2.36). Story length was similar across news story conditions (low = 200 words; medium = 265 words; high = 293 words), as was story format. Before the study launch, news story stimuli were pretested with a sample of 150 women aged 35–55 recruited from a national opt-in Qualtrics panel; results showed no statistically significant differences across conditions in perceptions of story accuracy, objectivity, and readability (all ps > .10).
All participants answered baseline questions about their clinical history (e.g., mammography history, breast cancer history), followed by several individual difference variables not analyzed here (e.g., general trust in institutions, understanding of scientific research). Participants in the no conflict condition answered the baseline questions directly followed by the post-test outcome questions. Participants in the low, medium, and high conflict conditions answered the baseline questions, next read their assigned news story, answered questions about the story they read, and last answered all other post-test outcome questions.
Measures
Baseline measures
To assess mammography history, we adapted a measure from the National Cancer Institute’s Health Information National Trends Survey (HINTS): “When did you have your most recent mammogram to check for breast cancer?” Response options included “1 year ago or less,” “more than 1 year ago, but within the past 2 years,” “more than 2 years ago, but within the past 3 years,” “more than 3 years ago, but within the past 5 years,” “more than 5 years ago,” “I have never had a mammogram,” and “I do not know.” For ordinary least squares (OLS) regression analyses, categories were collapsed into 1 (never had a mammogram; included do not know), 2 (had a mammogram more than 1 year ago), and 3 (had a mammogram in the past year). Breast cancer history was assessed by asking, “Have you ever had breast cancer?” Responses options included “yes,” “no,” and “I do not know,” which were collapsed into 1 (yes) and 2 (no; included do not know). GfK provided sociodemographic data about participants, including poverty level (living at or below vs. above 100% of the federal poverty level), education, race/ethnicity, and age.
We did not assess confusion, backlash, or ambivalence at baseline because the current study was conducted at a single time point, and assessing such cognitions immediately before experimental exposure could have activated women’s thinking about the topic and influenced subsequent responses.
Post-test measures
To assess affective responses to exposure to conflict, we adapted measures of emotional responses previously used by Nabi and colleagues [42, 55]. After reading their randomly assigned news story, participants in the low, medium, and high conflict conditions were asked to indicate the extent to which they felt five emotions about the article they read (interested, frustrated, alert, annoyed, distressed). The survey was programmed to fully randomize the order in which the five emotion items were presented to minimize potential order effects. Response options ranged from 1 (very slightly or not at all) to 5 (extremely). Because our a priori interests were in negative emotional responses, we analyzed three of these discrete emotions (frustrated: M = 2.44, standard deviation [SD] = 1.24; annoyed: M = 2.26, SD = 1.25; and distressed: M = 2.25, SD = 1.15) as separate outcomes; the three items were not so strongly correlated so as to suggest they were capturing identical emotional responses (Spearman’s ρ = .61–.72, p = .000; Table 1). Participants in the no conflict condition did not receive these questions.
Table 1.
Bivariate correlations among outcome variables and prior mammogram history
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| 1. Frustration | 1.00 | |||||||
| 2. Annoyance | .72*** | 1.00 | ||||||
| 3. Distress | .67*** | .61*** | 1.00 | |||||
| 4. Confusion | .20*** | .21*** | .17*** | 1.00 | ||||
| 5. Backlash | .04 | .12*** | .00 | .53*** | 1.00 | |||
| 6. Ambivalence (mammography) | .02 | .06 | .06 | .16*** | .14*** | 1.00 | ||
| 7. Ambivalence (other cancer screening) | .03 | .07* | .05 | .18*** | .19*** | .57*** | 1.00 | |
| 8. Prior mammogram history | .13*** | .09* | .11*** | −.01 | −.08** | −.26*** | −.18*** | 1.00 |
Pearson’s r or Spearman’s ρ, depending on level of measurement.
*p < .05; **p < .01; ***p < .001.
We asked all participants about one mammogram-specific cognitive response to exposure to conflict: ambivalence about mammography, which was assessed with a measure previously used by Han and colleagues [56]. Participants indicated whether they agreed or disagreed with the following statement: “I have mixed feelings about getting a mammogram.” Response options ranged from 1 (strongly disagree) to 5 (strongly agree) (M = 2.55, SD = 1.20).
We also assessed three more general cancer prevention- and screening-related cognitive responses: (i) confusion about cancer prevention recommendations and research; (ii) backlash toward such recommendations and research; and (iii) ambivalence about other types of cancer screening. The confusion and backlash measures were adapted from those previously used in the nutrition context [25, 34]. Prior research has demonstrated that these measures reflect distinct constructs [34], which is consistent with the moderate correlation between measures observed in the current study (r = .53, p = .000; Table 1).
To assess confusion, we asked participants to give us their opinion on each of the following statements: “It is not clear to me how best to avoid cancer,” “I find cancer recommendations to be confusing,” “Cancer research findings make sense to me,” “I know what I should be doing to avoid cancer,” “I find cancer research studies hard to follow,” and “I understand scientists’ recommendations about how to avoid cancer.” All six items were randomly presented to minimize potential order effects. Response options ranged from 1 (strongly disagree) to 5 (strongly agree). The third, fourth, and sixth items were reverse-coded so that a higher score signified greater confusion. Items were averaged to create a confusion scale (range = 1–5; M = 2.91, SD = .64), which demonstrated good internal consistency (Cronbach’s α = .76).
To assess backlash, we asked participants to give us their opinion on each of the following statements: “I am tired of hearing about what I should or should not do to avoid cancer,” “Scientific research provides good guidance about how to avoid cancer,” “The evidence about how to avoid cancer is growing,” “Scientists really do not know how you should avoid cancer,” and “I pay attention to new research on cancer.” Again, all five items were randomly presented. Response options ranged from 1 (strongly disagree) to 5 (strongly agree). The second, third, and fifth items were reverse-coded so that a higher score signified greater backlash. Items were averaged to create a backlash scale (range = 1–5; M = 2.80, SD = .56), although evidence of internal consistency was limited (Cronbach’s α = .60; see Discussion section).
To assess ambivalence toward other types of screening, we adapted a measure used by Han and colleagues [56]. Participants indicated whether they agreed or disagreed with the following statement: “I have mixed feelings about getting checked (or screened) for other types of cancer.” Response options again ranged from 1 (strongly disagree) to 5 (strongly agree) (M = 2.52, SD = 1.11).
After answering all outcome questions, participants in the low, medium, and high conflict conditions were asked two questions designed to serve as manipulation checks. They were asked to “think back to the news story that you read earlier. How much conflicting information did you notice in the article you read?” Using a sliding scale, participants responded from 0 (none) to 100 (a lot) (M = 56.03, SD = 24.86). Participants also were asked “How much debate, disagreement, or controversy did you notice in the article you read?” Again, they used a sliding scale to indicate their response from 0 (none) to 100 (a lot) (M = 55.54, SD = 23.29). If we observed greater recognition of conflict and controversy as the level of conflict increased across conditions, then we would interpret this pattern as evidence of successful experimental manipulation.
Analytic Approach
First, we performed descriptive analyses for baseline and outcome measures to understand data distribution. We then calculated bivariate correlations to estimate associations among outcome variables (Pearson’s r or Spearman’s ρ, depending on level of measurement); for each outcome variable, we also calculated means by experimental condition. Next, to estimate whether exposure to increasing levels of conflict had effects on the outcome variables of interest, we estimated OLS regression models. Because we hypothesized dose–response effects of exposure to conflict, we performed trend analyses, calculating linear and quadratic contrasts [57]. For the affective response models, low conflict exposure was the reference category in OLS regression models; for the cognitive response models, the no conflict condition was the reference category. For the negative emotional response and ambivalence models, results were consistent when estimated with ordered logit regression. Given the stratification design, we specified regression models with interaction terms by condition and poverty level to test whether exposure to conflict had a differential effect on women of higher versus lower socioeconomic position. Interaction contrasts were calculated to assess whether effects of exposure varied by poverty level. All analyses were conducted using Stata 15 (StataCorp, College Station, TX).
Finally, we assessed correlations between prior mammography history and outcome variables to determine its appropriateness as a covariate. Previous research has shown that prior experience with mammography is a strong predictor of women’s responses to messages about breast cancer screening [58, 59]. Table 1 shows that, in our sample, mammography history was significantly associated with all outcome variables except confusion, and the directions of associations are consistent with expectations based on previous research. Therefore, all multivariable models adjusted for prior mammogram history. We did not restrict our analyses to women over age 40 because even though no professional organizations recommend routine mammograms for average-risk women under age 40, screening is widely recommended for younger women at higher risk of breast cancer (e.g., based on genetic or family history). In our sample, 14.1% of women aged 35–39 reported having had a mammogram in the past year, and 19.6% reported having had a mammogram more than 1 year ago.
Results
Participant Characteristics
Roughly one-third (35.5%) of participants were aged 50–55 years, 20.4% were 45–49, 21.8% were 40–44, and 22.4% were 35–39. Half of the sample was of lower socioeconomic position by design, with 50.7% living at or below 100% of the federal poverty level. Just more than 10% of participants had less than a high school degree, 25.8% had completed high school, 31.9% had some college education, and 31.6% had a Bachelor’s degree or higher. Over half (58.2%) of the sample was non-Hispanic White, 12.2% participants were non-Hispanic Black, 23.4% were Hispanic/Latino, and 6.2% self-identified as members of one or more other non-Hispanic racial group. Just more than one-quarter (26.8%) reported never having had a mammogram, 28.6% reported having had a mammogram more than one year ago, and 44.4% reported having had a mammogram in the past year. Only 2.9% reported having a personal history of breast cancer.
Randomization to condition was successful, as there were no significant differences across conditions in age, poverty level (by design), education, race/ethnicity, prior mammogram history, or breast cancer history (all ps > .10).
Manipulation Check
Consistent with expectations, participants reported noticing more conflicting information as the level of conflict increased across news story conditions (low: M = 50.12, 95% confidence interval [CI] = 47.50 to 52.71; medium: M = 57.08, 95% CI = 54.43 to 59.73; high: M = 60.79, 95% CI = 58.23 to 63.36). Similarly, participants noticed more debate, disagreement, and controversy as the level of conflict increased across conditions (low: M = 49.34, 95% CI = 46.90 to 51.79; medium: M = 57.55, 95% CI = 55.06 to 60.04; high: M = 59.70, 95% CI = 57.29 to 62.11).
Effects of Exposure to Conflict on Affective and Cognitive Responses
Mean affective and cognitive responses by experimental condition are reported in Table 2. As predicted, exposure to conflict increased participants’ negative emotional responses to the article they read. Linear contrast analyses show a significant linear trend: As exposure to conflict increased, participants reported greater frustration [linear contrast coefficient = .21, 95% CI = 0.14 to 0.29; F(1, 1,004) = 31.21, p = .000], annoyance [linear contrast coefficient = .22, 95% CI = 0.15 to 0.30; F(1, 1,004) = 34.28, p = .000], and distress [linear contrast coefficient = .09, 95% CI = 0.02 to 0.16; F(1, 1,003) = 7.06, p = .008] about the news story they read. Interaction contrast analyses indicate that effects did not vary by poverty level: frustrated [interaction contrast coefficient = −.13, 95% CI = −0.29 to 0.02; F(1, 1,004) = 3.06, p = .080]; annoyed [interaction contrast coefficient = −.05, 95% CI = −0.21 to 0.10; F(1, 1,004) = 0.49, p = .485]; and distressed [interaction contrast coefficient = −.10, 95% CI = −0.24 to 0.04; F(1, 1,003) = 2.04, p = .153].
Table 2.
Mean affective and cognitive responses by experimental condition
| Affective (negative emotional) responses | Cognitive responses | ||||||
|---|---|---|---|---|---|---|---|
| Exposure to conflict condition | Frustration | Annoyance | Distress | Confusion | Backlash | Ambivalence (mammography) | Ambivalence (other cancer screening) |
| No conflicta | – | – | – | 2.82 (.62) | 2.74 (.55) | 2.37 (1.16) | 2.46 (1.08) |
| Low conflict | 2.17 (1.22) | 2.01 (1.18) | 2.13 (1.16) | 2.89 (.67) | 2.82 (.56) | 2.67 (1.19) | 2.60 (1.13) |
| Medium conflict | 2.48 (1.22) | 2.21 (1.22) | 2.26 (1.14) | 2.95 (.62) | 2.81 (.56) | 2.66 (1.20) | 2.55 (1.12) |
| High conflict | 2.69 (1.23) | 2.55 (1.28) | 2.36 (1.14) | 2.98 (.63) | 2.86 (.57) | 2.56 (1.23) | 2.48 (1.12) |
Standard deviations are provided in parentheses. For all outcome variables, range = 1–5.
aParticipants in the no conflict condition did not receive affective response items.
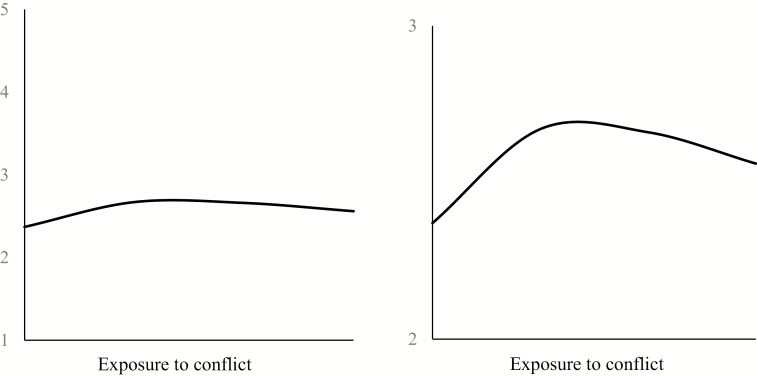
In answer to our research question about whether exposure to conflict influences mammogram-specific ambivalence, results indicate that this exposure increased ambivalence—but only to a point. Specifically, there was evidence of a significant quadratic trend: At lower levels of exposure to conflict, participants reported greater ambivalence about mammography, but at high levels of conflict, ambivalence was attenuated [quadratic contrast coefficient = −.10, 95% CI = −0.16 to −0.05; F(1, 1,447) = 11.89, p = .001; Fig. 1]. There was also evidence of a significant, though weaker, linear trend [linear contrast coefficient = .07, 95% CI = 0.01 to 0.13; F(1, 1,447) = 5.85, p = .016]. Interaction contrast analysis indicates that neither the quadratic nor linear effect varied by poverty level [interaction quadratic contrast coefficient = .04, 95% CI = −0.08 to 0.16; F(1, 1,447) = 0.50, p = .479; interaction linear contrast coefficient = −.04, 95% CI = −0.16 to 0.07; F(1, 1,447) = 0.55, p = .459].
Fig. 1.
Quadratic exposure effect on ambivalence about mammography [quadratic contrast coefficient = −.10, 95% CI = −0.16 to −0.05; F(1, 1,447) = 11.89, p = .001]. Findings are graphed for the full ambivalence scale (left panel) and, for illustrative purposes, a selection of the scale where the quadratic effect resided (right panel).
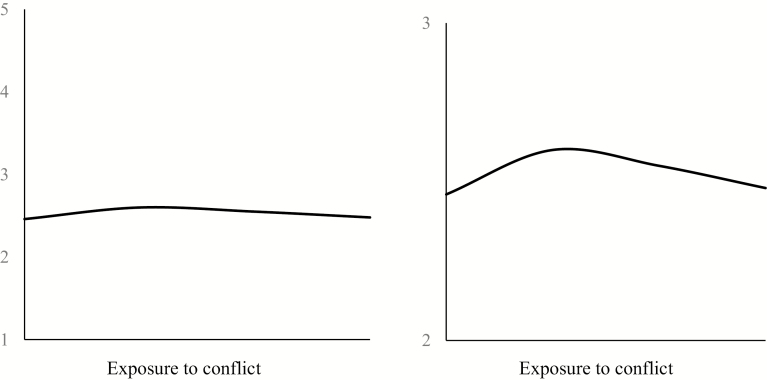
We then tested whether exposure to conflict produced three more general cancer prevention- and screening-related cognitions: confusion, backlash, and ambivalence about other types of cancer screening. Consistent with our hypotheses, there was evidence of a significant linear trend for confusion and backlash: As exposure to conflict increased, participants reported greater confusion about [linear contrast coefficient = .06, 95% CI = 0.03 to 0.09; F(1, 1,445) = 13.79, p = .000] and backlash toward [linear contrast coefficient = .04, 95% CI = 0.01 to 0.07; F(1, 1,441) = 7.30, p = .007] cancer prevention recommendations and research. Interaction contrast analyses indicate that effects did not vary by poverty level: confusion [interaction contrast coefficient = .03, 95% CI = −0.03 to 0.10; F(1, 1,445) = 0.92, p = .339] and backlash [interaction contrast coefficient = .04, 95% CI = −0.01 to 0.10; F(1, 1,441) = 2.43, p = .119]. As for ambivalence about other types of cancer screening, there was evidence of a curvilinear trend, similar to that observed for mammogram-specific ambivalence [quadratic contrast coefficient = −.06, 95% CI = −0.11 to −0.00; F(1, 1,450) = 3.95, p = .047; Fig. 2], though again the effect of exposure to conflict did not vary by poverty level [interaction contrast coefficient = −.03, 95% CI = −0.14 to 0.08; F(1, 1,450) = 0.31, p = .579]. There was no evidence of a significant linear trend [linear contrast coefficient = .01, 95% CI = −0.05 to 0.06; F(1, 1,450) = 0.06, p = .809].
Fig. 2.
Quadratic exposure effect on ambivalence about other types of cancer screening [quadratic contrast coefficient = −.06, 95% CI = −0.11 to −0.00; F(1, 1,450) = 3.95, p = .047]. Findings are graphed for the full ambivalence scale (left panel) and, for illustrative purposes, a selection of the scale where the quadratic effect resided (right panel).
Discussion
The current study addresses several gaps in the literature. First, although there is growing theoretical and empirical support for the proposition that media exposure to conflicting health information negatively influences public understanding and behavior, there are few studies causally linking exposure to conflicting information with undesirable outcomes [25–27, 29, 30]. Second, in the context of mammography in particular, there is concern that conflicting recommendations about the age at and frequency with which women should be screened may be producing several cognitive (e.g., confusion about screening) and behavioral (e.g., less screening adherence) effects, but to date there has been little research directly investigating the role of media exposure in producing such effects [9]. We therefore conducted an online survey experiment with a population-based sample of U.S. women aged 35–55 to test whether media exposure to conflicting information about mammography negatively influenced women’s affective and cognitive reactions. Results showed that greater exposure to conflict increased women’s negative emotional responses to the article they read (i.e., frustration, annoyance, distress). Exposure to conflict also increased women’s mammogram-specific ambivalence, though this leveled off at high levels of exposure, and produced three more general cancer prevention- and screening-related cognitive responses: (i) confusion about cancer prevention recommendations and research; (ii) backlash toward such recommendations and research; and (iii) ambivalence about other types of cancer screening (which again leveled off at high levels of exposure). Across outcome variables, there was little evidence that effects varied along socioeconomic lines—which our robust experimental design, with its stratification by poverty level, was well equipped to test.
The effects on women’s negative emotional reactions is consistent with predictions based on Nabi’s emotion-as-frame model [40–42], as well as with qualitative research that has documented negative emotional responses to conflict and controversy about topics including mammography [15] and nutrition (e.g., fish consumption) [43]. To our knowledge, this is the first study to provide experimental tests of these relations. This study is also one of the first [26] to assess whether exposure to conflict produces attitudinal ambivalence toward the object in question (here, mammography) [35–37]. We found evidence of a quadratic trend: Mammogram-specific ambivalence was highest among those in the low and medium exposure conditions. It could be that those who were exposed to high levels of conflict were less ambivalent about mammography because they were already leaning toward a decision against screening, and thus did not experience mixed feelings; future research should consider this possibility.
We also observed effects on more general cancer prevention- and screening-related cognitive responses. First, the effects on women’s confusion and backlash are consistent with previous research—which has found similar results in the context of nutrition [25–27], vaccines and autism [29], and dioxin regulation [30]. Taken together, these findings are in line with theorizing on how conflicting information exposure can trigger perceived ambiguity and, in turn, negative interpretations of that ambiguity [25, 32–34]. Moreover, the fact that exposure to conflict influenced more general cancer cognitions could signal the potential for carryover effects, as these cognitions could, in turn, affect responses to subsequent unrelated health messages or recommendations for behaviors about which there is little conflict (e.g., colorectal cancer screening). Second, we observed effects on ambivalence about other types of cancer screening, similar to the curvilinear trend observed for mammogram-specific ambivalence. This result provides additional evidence in support of carryover effects in the context of cancer screening, though these effects were modest compared with those that have been observed in studies of cumulative exposure to conflict [25, 34]. Ultimately, carryover effects are worth exploring in future work, given growing theoretical and empirical attention to this phenomenon in diverse content domains [60, 61].
Across outcomes, effects of exposure to conflict did not vary by poverty level. There are several potential explanations for these null findings. First, the existing literature did not enable a clear prediction about whether women of lower socioeconomic position would be more or less susceptible to conflicting messages: A communication inequalities perspective suggested that effects could be stronger among women of lower socioeconomic position, since they might struggle to reconcile conflicting messages, whereas a framing effects perspective suggested that effects could be stronger among women of higher socioeconomic position [46], given that they may have had greater prior exposure to mammography conflict and controversy. Conceivably, both possibilities were true and thus canceled each other out. In the present study, we could not test whether initial awareness of mammography conflict and controversy was lower among women of lower socioeconomic position, as we did not ask women about their awareness before our conflict manipulation; doing so immediately before experimental exposure could have activated women’s thinking about the topic and influenced subsequent responses. Second, lower income women who choose to participate in GfK’s KnowledgePanel might differ systematically from lower income women who choose not to participate—for example, they might be more engaged or informed about health issues, and thus might be similar to higher income GfK panelists. Last, perhaps responses to conflicting health information are driven primarily by educational attainment or research literacy, rather than socioeconomic position. Post hoc analyses show that poverty level was significantly associated but not redundant with both of these variables (Spearman’s ρeducation= .31, p = .000; Spearman’s ρresearch literacy= .14, p = .000); stratifying by these specific variables could be worthwhile in future research on the potential differential effects of exposure to conflict.
Study results should be considered in light of several observations. First, observed effects were small yet meaningful. We were able to show effects after participants were exposed only to a brief experimental manipulation. As importantly, communication effects are often small [62, 63], and on a population level can translate into substantial public health impact [64]. Second, conducting this experiment with population-based data—which included an oversample of women living at or below 100% of the federal poverty level—increased the study’s internal and external validity, but it also constrained survey length due to cost. Although the study was strengthened by basing message stimuli on a real news story identified in content analysis research [10], a future study with a national opt-in sample might assess whether similar effects are observed across multiple message exposures about distinct health topics, which would avoid case-category confound [65] while accurately reflecting real-world exposure to conflicting health information. A subsequent experimental study might also benefit from a longitudinal design, which would enable a baseline (Time 1) assessment of potential moderators and cofounders—such as prior awareness of mammography conflict and controversy and perceptions of confusion, backlash, and/or ambivalence—before a Time 2 experimental exposure to conflict. Through the use of random assignment to conditions, we assume that the observed findings were not due to variations in previously held awareness or beliefs, but we cannot empirically confirm this with the data at hand. Third, our multi-item backlash scale demonstrated lower internal consistency than has been observed in prior research. This could be because the cancer prevention-related items, which were adapted from the nutrition context [25, 34], were less content-specific, and thus might have been more difficult for participants to answer. Fourth, it is conceivable that negative emotional reactions mediated the effects of exposure to conflict on cognitive responses; this possibility cannot be rigorously tested in this study, given simultaneous measurement of outcome variables, but should be tested in subsequent work. Fifth, although the overall pattern of means observed in our manipulation check suggested successful experimental manipulation, there was some overlap between the medium and high conflict condition confidence intervals. Future research should prioritize creating even greater variation in conflict across conditions, while minimizing differences in story length, which in our study ranged from 200 to 293 words. Last, our operationalization of the level of conflict present in a single news story reflects both the reference to conflicting recommendations and the amount of conflict-laden language used to describe them. Although this operationalization is an ecologically valid representation of news media coverage of mammography [10], researchers should consider disentangling conflict and controversy—for example, by studying how women might be influenced by the extent of conflicting scientific evidence on the effectiveness of mammography for different age groups, absent conflict-laden language.
The current study adds to the growing evidence base documenting undesirable outcomes of media exposure to conflicting health information. Future research should examine whether the negative affective and cognitive responses observed here translate into behavioral effects, which could have implications for both health campaigns and patient–provider communication. On the one hand, such responses could undermine campaigns or interventions designed to encourage not only mammography but also other health behaviors. For example, women with greater exposure to conflicting information about mammography may not only be more confused by and more doubtful of cancer prevention recommendations and research, but these cognitions could, in turn, produce less adherence to health recommendations more generally—including those about which there is little conflict (e.g., colorectal cancer screening, skin cancer prevention). We found some evidence of potential carryover effects in this study, but future studies should specifically test whether exposure to conflict does in fact reduce receptivity to health messages and adherence to health recommendations. Ultimately, campaigns and interventions occur in the context of a broader information environment, which is increasingly characterized by conflicting and often controversial health information [23]. It therefore may be important to take this broader environment into account when designing interventions, such as by developing health messages that acknowledge existing conflicting information with the goal of “inoculating” or protecting against its influence [66].
On the other hand, there may be situations where exposure to conflict is motivating. For example, the negative affective and cognitive responses observed in this study could prompt patients to talk with their health care providers about cancer screening decision making. In the case of mammography, ambivalence toward screening, particularly among women in their 40s, might be a reasonable cognitive response, given ongoing expert disagreement about the age at and frequency with which women should be screened. Here, interventions with providers may be important, such as decision aids that help them to discuss the potential harms and benefits of screening with patients [67], with the added benefit of improving patient understanding of and ability to negotiate conflicting health recommendations. Such efforts—which may be particularly important for underserved populations—could promote informed decision making around screening, as recommended by professional organizations like USPSTF and ACS [2, 3], and ensure high value care.
Supplementary Material
Acknowledgments
The authors thank Cabral Bigman, Lauren Feldman, Erika Franklin Fowler, Seth Goldman, Sarah Gollust, and K. (Vish) Viswanath for their helpful feedback during earlier stages of this research. This work was supported by a Building Interdisciplinary Research Careers in Women’s Health Grant (2 K12-HD055887) from the Eunice Kennedy Shriver National Institutes of Child Health and Human Development, the Office of Research on Women’s Health, and the National Institute on Aging, administered by the University of Minnesota Women’s Health Research Program. Additional support was provided by a grant from the National Cancer Institute (1R21CA218054-01A1) and a Grant-in-Aid of Research, Artistry and Scholarship from the Office of the Vice President for Research at the University of Minnesota. This content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Compliance with Ethical Standards
Authors’ Statement of Conflict of Interest and Adherence to Ethical Standards The authors declare that they have no conflicts of interest.
Primary Data The authors had full control of all primary data.
Authors’ Contributions RHN designed the study and led data collection, with input from MCY and AJR. All authors contributed to data analysis and interpretation. RHN led manuscript writing, with MCY and AJR providing critical revisions. All authors read and approved the final version of the manuscript.
Ethical Approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent Informed consent was obtained from all individual participants included in the study.
References
- 1. Calonge N, Petitti DB, DeWitt TG, et al. Screening for breast cancer: US preventive services task force recommendation statement. Ann Intern Med. 2009;151:716–726. [DOI] [PubMed] [Google Scholar]
- 2. Siu AL; U.S. Preventive Services Task Force Screening for breast cancer: U.S. preventive services task force recommendation statement. Ann Intern Med. 2016;164:279–296. [DOI] [PubMed] [Google Scholar]
- 3. Oeffinger KC, Fontham ET, Etzioni R, et al. ; American Cancer Society Breast cancer screening for women at average risk: 2015 guideline update from the American Cancer Society. JAMA. 2015;314:1599–1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. American College of Obstetricians and Gynecologists. Breast cancer risk assessment and screening in average-risk women. ACOG Practice Bulletin: Clinial management guidelines for obstetrician–gynecologists 2017. Available at www.acog.org Accessibility verified May 16, 2018.
- 5. American College of Radiology. ACR and SBI: Draft USPSTF breast cancer screening recommendations would cost thousands of lives and could eliminate mammography insurance coverage for millions of women 2015. Available at www.prnewswire.com Accessibility verified May 16, 2018.
- 6. Schwartz LM, Woloshin S. News media coverage of screening mammography for women in their 40s and tamoxifen for primary prevention of breast cancer. JAMA. 2002;287:3136–3142. [DOI] [PubMed] [Google Scholar]
- 7. Holmes-Rovner M, Charles S. The mammography screening controversy: Who and what is heard in the press? Patient Educ Couns. 2003;51:75–81. [DOI] [PubMed] [Google Scholar]
- 8. Squiers LB, Holden DJ, Dolina SE, Kim AE, Bann CM, Renaud JM. The public’s response to the U.S. preventive services task force’s 2009 recommendations on mammography screening. Am J Prev Med. 2011;40:497–504. [DOI] [PubMed] [Google Scholar]
- 9. Nagler RH, Fowler EF, Gollust SE. Covering controversy: What are the implications for women’s health? Womens Health Issues. 2015;25:318–321. [DOI] [PubMed] [Google Scholar]
- 10. Nagler RH, Fowler EF, Marino NM, Mentzer KM, Gollust SE. The evolution of mammography controversy in the news media: A content analysis of four publicized screening recommendations, 2009 to 2016. Womens Health Issues. 2019;29:87–95. doi: 10.1016/j.whi.2018.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Young Lin LL, Rosenkrantz AB. The U.S. online news coverage of mammography based on a google news search. Acad Radiol. 2017;24:1612–1615. [DOI] [PubMed] [Google Scholar]
- 12. Taplin SH, Urban N, Taylor VM, Savarino J. Conflicting national recommendations and the use of screening mammography: Does the physician’s recommendation matter? J Am Board Fam Pract. 1997;10:88–95. [PubMed] [Google Scholar]
- 13. Meissner HI, Rimer BK, Davis WW, Eisner EJ, Siegler IC. Another round in the mammography controversy. J Womens Health (Larchmt). 2003;12:261–276. [DOI] [PubMed] [Google Scholar]
- 14. Kiviniemi MT, Hay JL. Awareness of the 2009 US preventive services task force recommended changes in mammography screening guidelines, accuracy of awareness, sources of knowledge about recommendations, and attitudes about updated screening guidelines in women ages 40–49 and 50+. BMC Public Health. 2012;12:899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Allen JD, Bluethmann SM, Sheets M, et al. Women’s responses to changes in U.S. Preventive Task Force’s mammography screening guidelines: Results of focus groups with ethnically diverse women. BMC Public Health. 2013;13:1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Nagler RH, Lueck JA, Gray LS. Awareness of and reactions to mammography controversy among immigrant women. Health Expect. 2017;20:638–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Allen SV, Solberg Nes L, Marnach ML, et al. Patient understanding of the revised USPSTF screening mammogram guidelines: Need for development of patient decision aids. BMC Womens Health. 2012;12:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Block LD, Jarlenski MP, Wu AW, Bennett WL. Mammography use among women ages 40–49 after the 2009 U.S. preventive services task force recommendation. J Gen Intern Med. 2013;28:1447–1453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Pace LE, He Y, Keating NL. Trends in mammography screening rates after publication of the 2009 US Preventive Services Task Force recommendations. Cancer. 2013;119:2518–2523. [DOI] [PubMed] [Google Scholar]
- 20. Wharam JF, Landon B, Zhang F, Xu X, Soumerai S, Ross-Degnan D. Mammography rates 3 years after the 2009 US Preventive Services Task Force guidelines changes. J Clin Oncol. 2015;33:1067–1074. [DOI] [PubMed] [Google Scholar]
- 21. Wang AT, Fan JQ, Van Houten HK, et al. Impact of the 2009 US Preventive Services Task Force guidelines on screening mammography rates on women in their 40s. PLoS One. 2014;9:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Davidson AS, Liao X, Magee D. Attitudes of women in their forties toward the 2009 USPSTF mammogram guidelines: A randomized trial on the effects of media exposure. Am J Obstet Gynecol. 2011;205:7. [DOI] [PubMed] [Google Scholar]
- 23. Carpenter DM, Geryk LL, Chen AT, Nagler RH, Dieckmann NF, Han PK. Conflicting health information: A critical research need. Health Expect. 2016;19:1173–1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Nagler RH, LoRusso SM. Conflicting information and message competition in health and risk messaging. In: Parrott R, ed. Encyclopedia of Health and Risk Message Design and Processing. New York: Oxford University Press; 2018:353–372. [Google Scholar]
- 25. Lee CJ, Nagler RH, Wang N. Source-specific exposure to contradictory nutrition information: Documenting prevalence and effects on adverse cognitive and behavioral outcomes. Health Commun. 2018;33:453–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chang C. Men’s and women’s responses to two-sided health news coverage: A moderated mediation model. J Health Commun. 2013;18:1326–1344. [DOI] [PubMed] [Google Scholar]
- 27. Chang C. Motivated processing: How people perceive news covering novel or contradictory health research findings. Sci Commun. 2015;37:602–634. [Google Scholar]
- 28. Nan X, Daily K. Biased assimilation and need for closure: Examining the effects of mixed blogs on vaccine-related beliefs. J Health Commun. 2015;20:462–471. [DOI] [PubMed] [Google Scholar]
- 29. Dixon GN, Clarke CE. Heightening uncertainty around certain science: Media coverage, false balance, and the autism-vaccine controversy. Sci Commun. 2012;35:358–382. [Google Scholar]
- 30. Jensen JD, Hurley RJ. Conflicting stories about public scientific controversies: Effects of news convergence and divergence on scientists’ credibility. Public Underst Sci. 2012;21:689–704. [DOI] [PubMed] [Google Scholar]
- 31. Ellsberg D. Risk, ambiguity, and the savage axioms. Q J Econ. 1961; 75:643–669. [Google Scholar]
- 32. Han PK, Moser RP, Klein WM. Perceived ambiguity about cancer prevention recommendations: Associations with cancer-related perceptions and behaviours in a US population survey. Health Expect. 2007;10:321–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Han PK, Kobrin SC, Klein WM, Davis WW, Stefanek M, Taplin SH. Perceived ambiguity about screening mammography recommendations: Association with future mammography uptake and perceptions. Cancer Epidemiol Biomarkers Prev. 2007;16:458–466. [DOI] [PubMed] [Google Scholar]
- 34. Nagler RH. Adverse outcomes associated with media exposure to contradictory nutrition messages. J Health Commun. 2014;19:24–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Thompson MM, Zanna MP, Griffin DW. Let’s not be indifferent about (attitudinal) ambivalence. In: Petty RE, Krosnick JA, eds. Attitude Strength: Antecedents and Consequences. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc; 1995:361–386. [Google Scholar]
- 36. Jonas K, Diehl M, Brömer P. Effects of attitudinal ambivalence on information processing and attitude-intention consistency. J Exp Soc Psychol. 1997;33:190–210. [Google Scholar]
- 37. Priester JR, Petty RE. The gradual threshold model of ambivalence: Relating the positive and negative bases of attitudes to subjective ambivalence. J Pers Soc Psychol. 1996;71:431–449. [DOI] [PubMed] [Google Scholar]
- 38. Zillmann D. Transfer of excitation in emotional behavior. In: Petty RE, Cacioppo JT, eds. Social Psychophysiology: A Sourcebook. New York: Guilford Press; 1983:215–240. [Google Scholar]
- 39. Roskos-Ewoldsen DR, Roskos-Ewoldsen B, Dillman Carpentier F. Media priming: An updated synthesis. In: Bryant J, Oliver MB, eds. Media Effects: Advances in Theory and Research. New York: Taylor & Francis; 2009:74–93. [Google Scholar]
- 40. Nabi RL. Exploring the framing effects of emotion: Do discrete emotions differentially influence information accessibility, information seeking, and policy preference? Commun Res. 2003;30:224–247. [Google Scholar]
- 41. Nabi RL. Emotion and persuasion: A social cognitive perspective. In: Roskos-Ewoldsen DR, Monahan J, eds. Social Cognition and Persuasion: Theories and Methods. Mahwah, NJ: Lawrence Erlbaum Associates; 2007:377–398. [Google Scholar]
- 42. Nabi RL, Prestin A. Unrealistic hope and unnecessary fear: Exploring how sensationalistic news stories influence health behavior motivation. Health Commun. 2016;31:1115–1126. [DOI] [PubMed] [Google Scholar]
- 43. Vardeman JE, Aldoory L. A qualitative study of how women make meaning of contradictory media messages about the risks of eating fish. Health Commun. 2008;23:282–291. [DOI] [PubMed] [Google Scholar]
- 44. Phelan JC, Link BG, Diez-Roux A, Kawachi I, Levin B. “Fundamental causes” of social inequalities in mortality: A test of the theory. J Health Soc Behav. 2004;45:265–285. [DOI] [PubMed] [Google Scholar]
- 45. Viswanath K, Nagler RH, Bigman-Galimore CA, McCauley MP, Jung M, Ramanadhan S. The communications revolution and health inequalities in the 21st century: Implications for cancer control. Cancer Epidemiol Biomarkers Prev. 2012;21:1701–1708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Viswanath K, Emmons KM. Message effects and social determinants of health: Its application to cancer disparities. J Commun. 2006;56:S238–S264. [Google Scholar]
- 47. Scheufele DA. Framing as a theory of media effects. J Commun. 1999;49:103–122. [Google Scholar]
- 48. Entman RM. Framing: Toward clarification of a fractured paradigm. J Commun. 1993;43:51–58. [Google Scholar]
- 49. Kobayashi K. Effects of conflicting scientific arguments on belief change: Argument evaluation and expert consensus perception as mediators. J Appl Soc Psychol. 2018, 48:177–187. [Google Scholar]
- 50. Tan ASL, Lee CJ, Nagler RH, Bigman CA. To vape or not to vape? Effects of exposure to conflicting news headlines on beliefs about harms and benefits of electronic cigarette use: Results from a randomized controlled experiment. Prev Med. 2017;105:97–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Mutz DC. Population-Based Survey Experiments. Princeton, New Jersey: Princeton University Press, 2011. [Google Scholar]
- 52. U.S. Census Bureau. Poverty thresholds by size of family and number of children.2016. Available at https://www.census.gov/data/tables/time-series/demo/income-poverty/historical-poverty-thresholds.html. Accessibility verified November 14, 2018.
- 53. Slater MD, Peter J, Valkenburg PM. Message variability and heterogeneity: A core challenge for communication research. In: Cohen EL, ed. Communication Yearbook 39. New York: Routledge; 2015:1–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Tausczik YR, Pennebaker JW. The psychological meaning of words: LIWC and computerized text analysis methods. J Lang Soc Psychol. 2009;29:24–54. [Google Scholar]
- 55. Nabi RL, Stitt CR, Halford J, Finnerty KL. Emotional and cognitive predictors of the enjoyment of reality-based and fictional television programming: An elaboration of the uses and gratifications perspective. Media Psychol. 2006;8:421–447. [Google Scholar]
- 56. Han PK, Williams AE, Haskins A, et al. Individual differences in aversion to ambiguity regarding medical tests and treatments: Association with cancer screening cognitions. Cancer Epidemiol Biomarkers Prev. 2014;23:2916–2923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Keppel G, Wickens TD.. Design and Analysis: A Researcher’s Handbook. 4th ed. Upper Saddle River, NJ: Pearson Prentice Hall; 2004. [Google Scholar]
- 58. Yu J, Nagler RH, Fowler EF, Kerlikowske K, Gollust SE. Women’s awareness and perceived importance of the harms and benefits of mammography screening: Results from a 2016 national survey. JAMA Intern Med. 2017;177:1381–1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Nagler RH, Franklin Fowler E, Gollust SE. Women’s awareness of and responses to messages about breast cancer overdiagnosis and overtreatment: Results from a 2016 National Survey. Med Care. 2017;55:879–885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Hopkins DJ, Mummolo J. Assessing the breadth of framing effects. Quart J Polit Sci. 2017;12:37–57. [Google Scholar]
- 61. Ophir Y, Jamieson KH. Intentions to use a novel Zika vaccine: The effects of misbeliefs about the MMR vaccine and perceptions about Zika. J Public Health. 2018. doi: 10.1093/pubmed/fdy042 (e-pub ahead of print). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Snyder LB, Hamilton MA, Mitchell EW, Kiwanuka-Tondo J, Fleming-Milici F, Proctor D. A meta-analysis of the effect of mediated health communication campaigns on behavior change in the United States. J Health Commun. 2004;9(suppl 1):71–96. [DOI] [PubMed] [Google Scholar]
- 63. Valkenburg PM, Peter J. Five challenges for the future of media-effects research. Int J Commun. 2013;7:197–215. [Google Scholar]
- 64. Cappella J, Hornik R. The importance of communication science in addressing core problems in public health. In: Buzzanell PM, Carbaugh D, eds. Distinctive Qualities in Communication Research. New York: Routledge; 2009:73–86. [Google Scholar]
- 65. Jackson S. Message Effects Research: Principles of Design and Analysis. New York: Guilford; 1992. [Google Scholar]
- 66. Niederdeppe J, Gollust SE, Barry CL. Inoculation in competitive framing: Examining message effects on policy preferences. Public Opin Q. 2014;78:634–655. [Google Scholar]
- 67. Hersch J, Barratt A, Jansen J, et al. Use of a decision aid including information on overdetection to support informed choice about breast cancer screening: A randomised controlled trial. Lancet. 2015;385:1642–1652. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.