Abstract
OBJECTIVES
Decellularized pulmonary homografts (DPH) have shown excellent results for pulmonary valve replacement. However, controlled multicentre studies are lacking to date.
METHODS
Prospective European multicentre trial evaluating DPH for pulmonary valve replacement. Matched comparison of DPH to bovine jugular vein (BJV) conduits and cryopreserved homografts (CH) considering patient age, type of heart defect and previous procedures.
RESULTS
In total, 121 patients (59 female) were prospectively enrolled (August 2014–December 2016), age 21.3 ± 14.4 years, DPH diameter 24.4 ± 2.8 mm. No adverse events occurred with respect to surgical handling; there were 2 early deaths (30 + 59 years) due to myocardial failure after multi-valve procedures and no late mortality (1.7% mortality). After a mean follow-up of 2.2 ± 0.6 years, the primary efficacy end points mean peak gradient (16.1 ± 12.1 mmHg) and regurgitation (mean 0.25 ± 0.48, grade 0–3) were excellent. One reoperation was required for recurrent subvalvular stenosis caused by a pericardial patch and 1 balloon dilatation was performed on a previously stented LPA. 100% follow-up for DPH patients operated before or outside the trial (n = 114) included in the ESPOIR Registry, age 16.6 ± 10.4 years, diameter 24.1 ± 4.2 mm, follow-up 5.1 ± 3.0 years. The combined DPH cohort, n = 235, comprising both Trial and Registry data showed significantly better freedom from explantation (DPH 96.7 ± 2.1%, CH 84.4 ± 3.2%, P = 0.029 and BJV 82.7 ± 3.2%, P = 0.012) and less structural valve degeneration at 10 years when matched to CH, n = 235 and BJV, n = 235 (DPH 61.4 ± 6.6%, CH 39.9 ± 4.4%, n.s., BJV 47.5 ± 4.5%, P = 0.029).
CONCLUSIONS: Initial results of the prospective multicentre ESPOIR Trial showed DPH to be safe and efficient. Current DPH results including Registry data were superior to BJV and CH.
Trial registration clinicaltrials.gov identifier: NCT 02035540.
Keywords: Heart valve disease, Tissue engineering, Decellularization, Allografts
INTRODUCTION
Surgical replacement of the pulmonary valve remains the first-line procedure for valve replacement despite the rapid progress made in transcatheter pulmonary valve implantation in the right ventricular outflow tract [1]. This is highlighted by an implantation rate of only 58% of patients presenting for such a procedure in a recent retrospective multicentre trial in the USA including 3% of patients requiring urgent surgery for stent embolization [2]. Surgical implants, however, are far from ideal given the limited durability for biological valve prostheses, in particular for young patients, and the constraints of mechanical valves. As an alternative, tissue engineering methods have been used to construct artificial, cell-seeded or non-seeded heart valve prostheses, which, however, have not been successfully translated to clinical application thus far. In contrast, decellularized human heart valves have shown promising early to midterm results when used for pulmonary valve replacement (PVR) in congenital heart disease (CHD). Several groups using different decellularization protocols have described superior results using decellularized pulmonary homografts (DPH) compared with standard cryopreserved homografts (CH) [3], and bovine jugular vein (BJV) conduits [4].
However, there has been a degree of scepticism about the use of DPH with respect to the shorter follow-up periods for cell-free allografts and the lack of prospective controlled trials [5–7]. For example, in a recent propensity-matched analysis of 130 adult DPH and 130 CH patients undergoing the Ross procedure, da Costa and co-workers found comparable results in both groups over a period of up to 8 years with only slightly lower right ventricular outflow tract gradients in the DPH group [8, 9]. On the other hand, the da Costa’s group also showed excellent results in a retrospective analysis of the use of their established proprietary decellularization protocol in paediatric patients. Freedom from reintervention at 10 years for children below 12 years of age was a remarkable 91% [10].
The aim of this study is to (i) present early data from the first European-wide prospective trial on DPH for PVR and (ii) to summarize the current results for this specific DPH type in a matched direct comparison with CH and BJV.
MATERIALS AND METHODS
Study setting
The ESPOIR Trial received funding from the European Union’s Seventh Framework Programme under Grant Agreement No. 278453. The funding covered homograft procurement, processing and data collection. Corlife oHG, a Hannover Medical School spin-off company, which provided the decellularization service for the homografts, was the sponsor of the study according to Good Clinical Practice requirements.
The study was registered under ClinicalTrials.gov NCT 02035540 and received the European Network of Centres for Pharmacoepidemiology and Pharmacovigilance (ENCePP®) seal as a Post Authorization Safety Study (PASS) under Reference No. 5064. It was also registered with the German authorities under Ref. Number NIS242 (www.espoir-clinicaltrial.eu). Approval was given by all local ethics committees before the start of the study and informed consent was obtained appropriately from all participants or parents.
Indication for PVR according to the current clinical guidelines was the key inclusion criterion without age limits; patients with active endocarditis were not included. Surgical procedures were performed according to locally established standard procedures under the cardiopulmonary bypass.
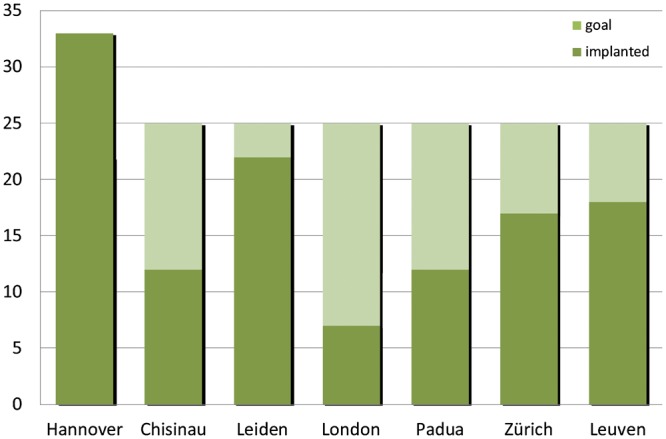
Homograft procurement and processing
Homografts were procured in line with current European Directives via 4 different tissue banks (European Homograft Bank, Dr R. Jashari; German Society for Tissue Transplantation - DGFG, M. Börgel; Heart Valve Bank Beverwijk, A. van den Bogaerdt; Fondazione Banca dei Tesutti di Treviso, Dr A. Paolin) and shipped to Hannover for processing at Corlife (www.corlife.eu). Processing comprised ∼30 different steps using a detergent-based approach as previously described [11]. A microbiological assessment was performed at the time of the incoming inspection, and during and after processing with a final 14-day quarantine. Each homograft was assessed histologically before and after processing, and the DNA content was measured before and after processing prior to final release. Reference samples of all homografts were stored in accordance with the European-wide Paul Ehrlich Institute authorization (www.pei.de, ESPOIR PV PEI.G.11634.01.1) for at least 1 year.
Statistical analysis
Summaries of the numeric data are given as means and standard deviation (SD). The Mann–Whitney U-test for non-paired samples was used for data with skew distribution. Time-related events, such as freedom from explantation and endocarditis, were evaluated according to the Kaplan–Meier test, including numbers at risk at 0, 5 and 10 years, and freedom-from-event rates at 0, 5 and 10 years, with their respective 95% confidence limits.
The proportion of explanted and dysfunctional grafts over time was calculated for all 3 valve grafts as described [4]. A peak echocardiographic gradient of ≥50 mmHg and regurgitation grade ≥ moderate was defined as dysfunctional.
Patients for matching were chosen from the updated RVOT Conduit Registry [12] and each DPH patient was matched to a BJV and CH patient. Matching was performed on the basis of the patient’s age at implantation, diagnosis, the number of previous operations and the number of previous PVR. Of all patient data sets analysed, 61% (429/705) were derived from the 7 centres participating in the ESPOIR study, the remaining were derived from 7 additional centres participating in the RVOT Registry. The propensity score matching showed excellent comparability of the 2 homograft groups, BJV patients were less comparable because of the upper size limit of 22 mm of BJV.
Pulmonary valve annulus measurements were converted as described [4] and z-value developments were calculated for DPH and BJV, as CH measurements were unfortunately limited.
SPSS 23 (IBM Corporation, Somer, NY) was used for the analyses. No correction was performed for multiple testing. All the statistical tests were 2-sided and a P-value of ≤0.05 was considered statistically significant.
RESULTS
Initial results within the prospective ESPOIR Trial cohort
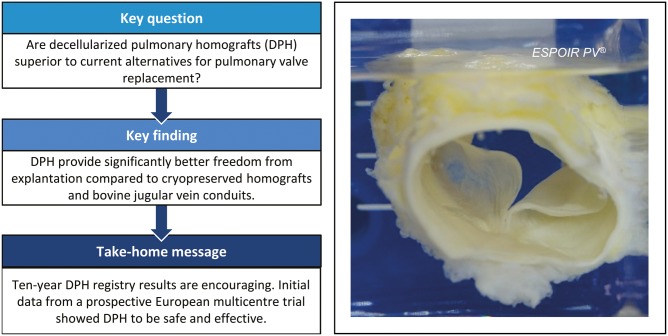
In total, 121 patients were prospectively enrolled in the ESPOIR Trial between August 2014 and December 2016 at 7 centres in Europe. The rates of patient inclusion at the respective centres are outlined below in Fig. 1.
Figure 1:
Patient inclusion within the prospective multicentre ESPOIR Trial by centre.
The mean age of patients was 21.3 years (standard deviation 14.4) and the mean implanted DPH diameter was 24.4 mm (SD 2.8). The procedural success rate was 100% and there were no intraoperative adverse events related to the valve implantation. Two early deaths occurred, both in grown-up congenital heart disease patients (30 and 59 years) due to postoperative myocardial failure after multi-valve procedures. There has been no late mortality so far, resulting in an overall mortality rate of 1.7%.
After a mean of 2.2 years (SD 0.6), the primary efficacy end points were excellent, with a mean peak gradient of 16.1 mmHg (SD 12.1) and a mean regurgitation grade of 0.25 (SD 0.48, grade 0–3).
One DPH was explanted after 23 months due to technical reasons during reoperation for recurrent subvalvular stenosis caused by a pericardial patch. The valve itself, however, showed no signs of degeneration. In addition, 1 balloon dilatation procedure was performed on a previously stented LPA. All other procedures and subsequent follow-up have been uneventful to date, leading to an overall freedom from explantation and a reintervention rate of 98.3%.
Characteristics of the ESPOIR Registry patients
Since January 2005, 114 additional patients received a DPH prior to or outside of the ESPOIR Trial cohort. 100% follow-up has been implemented for these patients using the same protocol as the ESPOIR Trial, and these patients have been included in the ESPOIR Registry. The mean age of the ESPOIR Registry patients is lower than the age of the patients within the trial cohort with a mean of 16.6 years (SD 10.4). The mean DPH had a diameter of 24.1 mm (SD 4.2) and the mean follow-up period is considerably longer at 6.0 years (SD 3.5).
Table 1 provides details for the ESPOIR Trial and the ESPOIR Registry patients with respect to underlying cardiac malformations and previous cardiac operations. Table 1 also provides details of the matched pairs of patients who received either a CH or a BJV conduit.
Table 1:
Patient characteristics for the ESPOIR Trial and the ESPOIR Registry cohort, and the respective matched CH and BJV cohorts
| The ESPOIR Trial cohort and matched pairs |
The ESPOIR Registry cohort and matched pairs |
|||||
|---|---|---|---|---|---|---|
| DPH | CH | BJV | DPH | CH | BJV | |
| Implantation period | 2014–2016 | 1988–2015 | 2000–2016 | 2005–2018 | 1985–2014 | 1999–2012 |
| Diagnoses (%) | ||||||
| TOF | 44 | 35 | 54 | 48 | 49 | 68 |
| Ross | 21 | 41 | 10 | 11 | 21 | 7 |
| PI/PS | 14 | 6 | 10 | 17 | 5 | 5 |
| PA | 10 | 9 | 11 | 13 | 8 | 6 |
| DORV | 5 | 1 | 7 | 4 | 8 | 6 |
| TAC | 4 | 4 | 6 | 4 | 4 | 4 |
| TGA | 1 | 3 | 2 | 3 | 4 | 2 |
| Other | 1 | 1 | 0 | 0 | 1 | 2 |
| Total (n) | 121 | 121 | 121 | 114 | 114 | 114 |
| Age at implantation (years), mean (SD) | 21.4 (14.4) | 21.2 (14.6) | 17.6 (11.6) | 16.6 (10.4) | 16.5 (10.6) | 15.6 (9.2) |
| Follow-up (years), mean (SD) | 2.2 (0.6) | 5.2 (4.4) | 4.1 (3.7) | 6.0 (3.5) | 5.1 (5.1) | 4.4 (3.3) |
| Total follow-up (years) | 93 | 781 | 715 | 578 | 862 | 738 |
| Sex (male), n (%) | 61 (50) | 71 (59) | 66 (55) | 75 (66%) | 72 (63) | 54 (47) |
| Number of previous operations | ||||||
| 0 | 11 | 28 | 8 | 17 | 21 | 11 |
| 1 | 62 | 51 | 75 | 60 | 53 | 65 |
| 2 | 32 | 29 | 24 | 24 | 33 | 27 |
| >2 | 16 | 13 | 14 | 13 | 7 | 11 |
| Conduit diameter (mm), mean (SD) | 24.4 (2.8) | 24.2 (2.8) | 20.6 (2.3) | 24.1 (4.2) | 23.5 (3.6) | 20.1 (2.9) |
| 12–19 | 6 | 6 | 25 | 15 | 13 | 30 |
| 20–23 | 37 | 47 | 96 | 34 | 37 | 82 |
| 24–29 | 78 | 68 | 0 | 65 | 64 | 2 |
BJV: bovine jugular vein; CH: cryopreserved homograft; DPH: decellularized pulmonary homografts; SD: standard deviation.
Outcome comparison of all decellularized pulmonary homograft recipients (ESPOIR Trial and Registry patients) with matched cryopreserved homograft and bovine jugular vein conduit patients
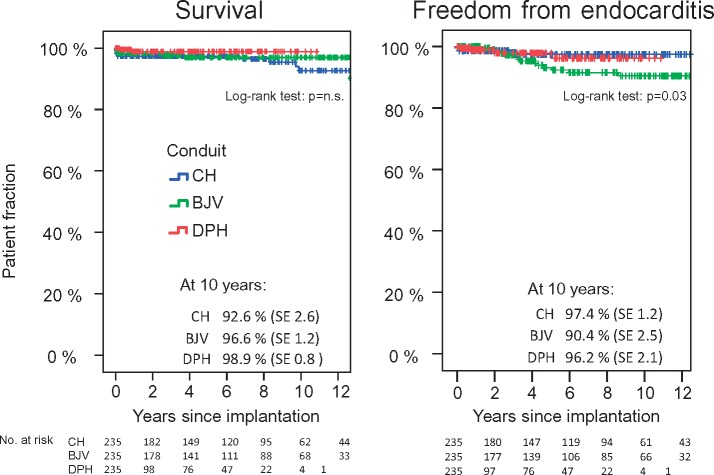
As the follow-up period for the ESPOIR Trial patients was relatively short, we opted to pool data from the ESPOIR Trial and the ESPOIR Registry to provide a complete overview of our current DPH results. The following analyses are, therefore, based on 235 DPH patients compared with 235 CH and 235 BJV matched patients. There was no difference in the survival rates for the 3 groups after 10 years. The rate of freedom from endocarditis was significantly lower for BJV patients (P = 0.033), as shown in Fig. 2.
Figure 2:
Survival and freedom from endocarditis for DPH, CH and BJV cohorts. Detailed comparisons including log-rank test results are provided within Table 2. BJV: bovine jugular vein; CH: cryopreserved homografts; DPH: decellularized pulmonary homografts.
Patients were also compared on the basis of the immediate implantation results and the potential influence of suboptimal implantation results on the long-term outcome. In contrast to CH and BJV, DPH showed no aggravation of an immediate postoperative stenosis or immediate pulmonary regurgitation (Fig. 3A and B). Z-values of DPH remained normal within the observation period regardless of whether they were over-, norm- or undersized at implantation. Only DPH and BJV are displayed here, as the information available for CH was incomplete (Fig. 3C).
Figure 3:
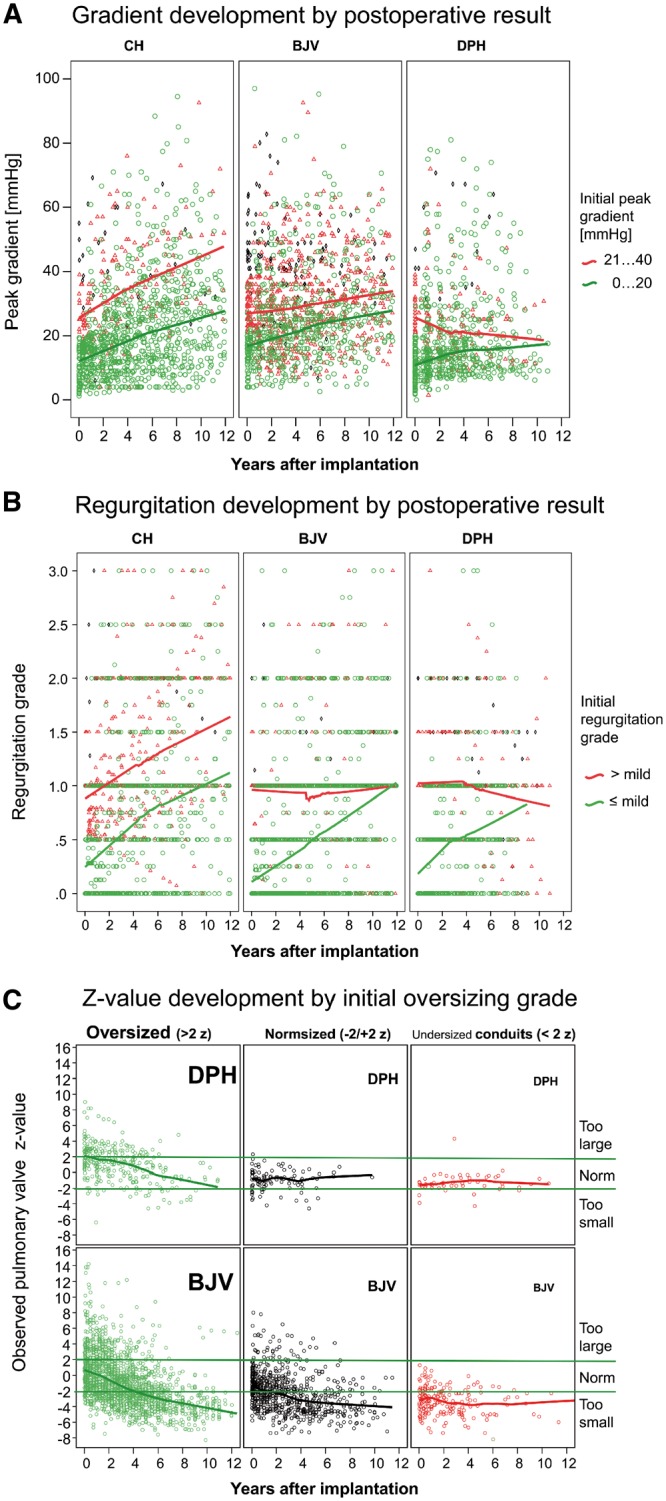
(A) Echocardiographic peak gradient over time for DPH, CH and BJV differentiated by the residual immediate implantation result (below or above 20 mmHg). (B) Regurgitation grade over time differentiated by immediate postoperative valve competence (below or above mild regurgitation). (C) Z-value development over time for DPH and BJV differentiated by the initial z-score at implantation (oversized >2z, normsized −2/+2z or undersized <−2z). BJV: bovine jugular vein conduits; CH: cryopreserved conventional homografts; DPH: decellularized pulmonary homografts.
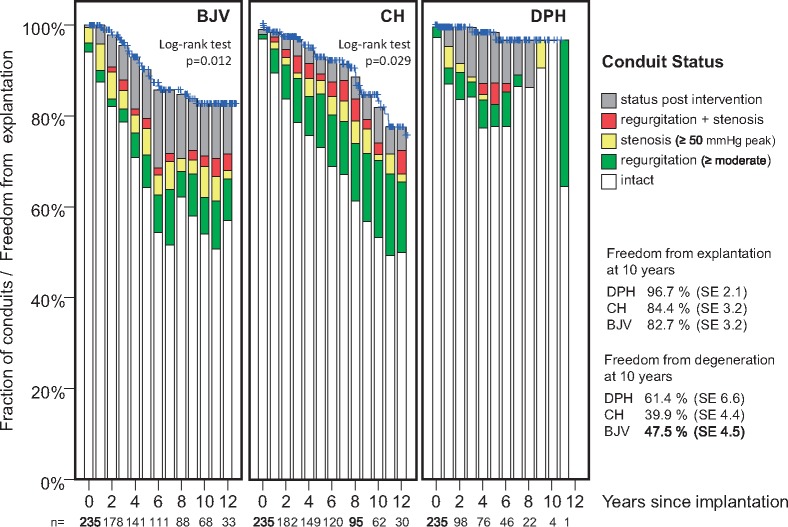
Figure 4 gives an overview of freedom from explantation and the current functional status of the remaining conduits within each of the 3 matched groups. DPH showed significantly better rates of freedom from explantation and degeneration than CH (P = 0.029) and BJV (P = 0.012) at 10-year follow-up.
Figure 4:
Freedom from explantation and functional conduit status for DPH, CH and BJV cohorts. Log-rank test results for freedom of explantation are shown, detailed comparisons are provided within Table 2. BJV: bovine jugular vein conduits; CH: cryopreserved conventional homografts; DPH: decellularized pulmonary homografts.
Table 2 summarizes the specific results for each conduit type at 5 and 10 years.
Table 2:
Freedom from diverse adverse outcomes for DPH, CH and BJV cohorts
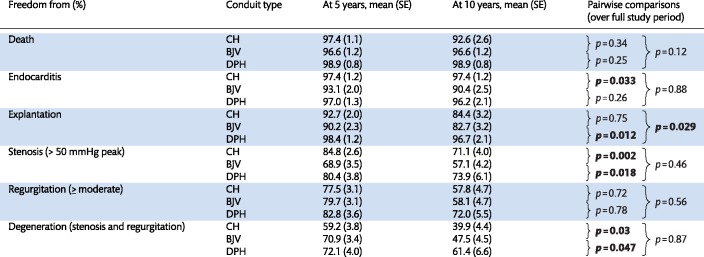
|
BJV: bovine jugular vein; CH: cryopreserved homograft; DPH: decellularized pulmonary homografts; SE: standard error.
DISCUSSION
The ESPOIR Trial was set up as a prospective, observational and non-randomized trial design. While many will argue for a randomized design as the gold standard, there are a number of reasons, which speak against the use of a randomized approach in this context. These include (i) the paucity of available homografts, (ii) the vast amount of existing data on CHs and BJVs for PVR in the literature [13] and (iii) patients’ and parents’ preference for decellularized homografts based on the very promising early data available on DPH. In addition, our experience with obtaining the ethics approval in several centres across Europe for a study involving children indicates that this study would have not been approved by the majority of the ethics committees at the participating centres, if a randomized design had been chosen.
This study adds important information to current knowledge on the clinical application of decellularized valves, as the ESPOIR Trial is the first prospective multicentre trial to evaluate cell-free homografts, whereas all other reports on this new therapeutic option have been either retrospective in character, or based on the experience of a single centre [1, 2, 7]. Early data from the ESPOIR Trial are in line with the expected mortality rates for PVR in CHD patients [13, 14]. The procedural success rate was 100% and no unexpected severe adverse events, such as graft rupture or late dehiscence, were observed, proving DPH to be safe in a multicentre setting. So far the short-term follow-up of up to 3 years has revealed excellent haemodynamics across DPH conduits. Only 1 DPH had to be explanted for technical reasons due to a patch-related subvalvular stenosis, which developed 2 years postoperatively.
Although our initial data are promising, the long-term follow-up of these patients is absolutely needed to draw definitive conclusions about the use of DPH. These long-term data will then need to show equal or superior performance to the excellent clinical results reported for conventional CHs [15, 16].
To maximize our current evidence basis on DPH for this current analysis, we pooled the data from patients operated within the ESPOIR prospective trial together with the data from patients operated prior to the trial and the small number of DPH patients who could not be enrolled in the study. A key factor in this analysis is that the follow-up rate for all of these patients is 100%. A comparison with matched data from more than 700 patients undergoing PVR, either with a cell-free homograft, a conventional homograft or a BJV conduit, showed statistically significant better results for cell-free homografts at 10 years for freedom from any reintervention and for structural valve degeneration.
Postoperative residual stenosis and more than mild immediate postoperative regurgitation have been identified as risk factors for reduced homograft durability in PVR [17]. In our analysis of matched patients with these postoperative risk factors, DPH patients did not show such increased gradients or regurgitation in contrast to CH and BJV, which may suggest some form of regenerative capacity for DPH.
Earlier analogous analyses of DPH results have been criticized because of the difference in mean follow-up times [4, 6]; this difference can be attributed to the relative novelty of DPH as a therapeutic option and will be balanced over time as experience and observation times with DPH increase. In this analysis, for example, the patients from the ESPOIR Registry had a slightly longer mean follow-up than that of the matched CH and BJV patients.
Owing to the low number of infants and toddlers included in this analysis, it is difficult to determine the value of DPH as an option for valve replacement for this age group. PVR in neonates and infants is rare, because of the limited availability of donated homografts with the required small diameters. Potentially, partial PVR using 1 DPH cusp may provide an option for this age group, but this requires an investigation in a further prospective study. Meanwhile, alternative options such as individually created PTFE conduits are currently being evaluated for very young patients requiring PVR [18].
In older children, adolescents and young adults, however, DPH appears to be the best currently available therapeutic option for PVR. A growing number of patients require multi-valve procedures, e.g. as a follow-up to Truncus arteriosus or after Ross procedures. In selected cases, we have performed a double semilunar valve replacement using cell-free pulmonary and aortic valves with excellent early to midterm results [19]. Long-term results for these approaches are currently pending, for example the results for a prospective study on aortic valve replacement (ARISE), which ended patient inclusion in summer 2018 [20].
Limitations
As outlined above, there are a number of limitations to this study, including the 1-armed study design and the restrictions inherent in the matching process caused by low numbers and high variance in congenital heart defects. The shorter overall follow-up times available for DPH patients are the biggest limitation and definitive conclusions obviously will need longer follow-up. In addition, only retrospectively collected data were available for BJV and CH, which though is more likely to underestimate valve degeneration and other adverse events in these 2 cohorts in comparison with the prospective follow-up for DPH patients. Clinical outcomes are also likely to vary depending on the decellularization protocol; therefore, the results from this study are not necessarily directly transferable to other proprietary protocols.
CONCLUSION
The initial results of the prospective European ESPOIR Trial over a period of up to 3 years proved DPH to be safe and efficient in a multicentre setting with excellent short-term haemodynamics. Continued follow-up over a period of at least 10–20 years is planned. Our analysis of more than 700 patients following PVR has shown DPH performance to be superior to other widely used options, such as BJV conduits (Contegra®) and standard CHs, in cohorts matched for age, type of congenital heart defect and the number of previous procedures.
ACKNOWLEDGEMENTS
The authors specifically thank the participating tissue banks and their respective executive teams for their support in implementing this study. The authors are extremely grateful to the following individuals and their organizations for contributing to the RVOT Registry: M.S., M.H., B.M., J.V.P., G.S., M.P., E. Sandica, Ch. Sebening, N. Doll, R. Cesnjevar, A.C., R. Goerg, T. Loukanov, W. Hemmer, A. Rüffer and E. Cheptanaru. The authors also thank Nina McGuinness for editorial assistance.
Funding
This study was supported by a grant from the European Union’s Seventh Framework Programme for Research, Technological Development and Demonstration [Grant Agreement No. 278453].
Conflict of interest: Axel Haverich holds shares in Corlife oHG, the company providing the service of processing decellularized allografts used in this study. Ramadan Jashari is the Director of the European Homograft Bank. All other authors declare that there are no conflicts of interest.
Footnotes
Presented at the 32nd Annual Meeting of the European Association for Cardio-Thoracic Surgery, Milan, Italy, 18–20 October 2018.
REFERENCES
- 1. Morgan GJ. Pulmonary regurgitation- is the future percutaneous or surgical? Front Pediatr 2018;6:184.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Martin MH, Meadows J, McElhinney DB, Goldstein BH, Bergersen L, Qureshi AM. et al. Safety and feasibility of melody transcatheter pulmonary valve replacement in the native right ventricular outflow tract: a Multicenter Pediatric Heart Network Scholar Study. JACC Cardiovasc Interv 2018;11:1642–50. [DOI] [PubMed] [Google Scholar]
- 3. Bibevski S, Ruzmetov M, Fortuna RS, Turrentine MW, Brown JW, Ohye RG.. Performance of synergraft decellularized pulmonary allografts compared with standard cryopreserved allografts: results from multiinstitutional data. Ann Thorac Surg 2017;103:869–74. [DOI] [PubMed] [Google Scholar]
- 4. Sarikouch S, Horke A, Tudorache I, Beerbaum P, Westhoff-Bleck M, Boethig D. et al. Decellularized fresh homografts for pulmonary valve replacement: a decade of clinical experience. Eur J Cardiothorac Surg 2016;50:281–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Alexander ME. Finding the next good thing. J Thorac Cardiovasc Surg 2017;153:1555–6. [DOI] [PubMed] [Google Scholar]
- 6. D’Udekem Y. Decellularized homografts: in fashion or really superior? Eur J Cardiothorac Surg 2016;50:291.. [DOI] [PubMed] [Google Scholar]
- 7. Helder MR, Kouchoukos NT, Zehr K, Dearani JA, Maleszewski JJ, Leduc C. et al. Late durability of decellularized allografts for aortic valve replacement: a word of caution. J Thorac Cardiovasc Surg 2016;152:1197–9. [DOI] [PubMed] [Google Scholar]
- 8. Etnel JRG, Suss PH, Schnorr GM, Veloso M, Colatusso DF, Balbi Filho EM. et al. Fresh decellularized versus standard cryopreserved pulmonary allografts for right ventricular outflow tract reconstruction during the Ross procedure: a propensity-matched study. Eur J Cardiothorac Surg 2018;54:434–40. [DOI] [PubMed] [Google Scholar]
- 9. da Costa FDA, Etnel JRG, Charitos EI, Sievers HH, Stierle U, Fornazari D. et al. Decellularized versus standard pulmonary allografts in the ross procedure: propensity-matched analysis. Ann Thorac Surg 2018;105:1205–13. [DOI] [PubMed] [Google Scholar]
- 10. da Costa FDA, Etnel JRG, Torres R, Balbi Filho EM, Torres R, Calixto A. et al. Decellularized allografts for right ventricular outflow tract reconstruction in children. World J Pediatr Congenit Heart Surg 2017;8:605–12. [DOI] [PubMed] [Google Scholar]
- 11. Cebotari S, Tudorache I, Ciubotaru A, Boethig D, Sarikouch S, Goerler A. et al. Use of fresh decellularized allografts for pulmonary valve replacement may reduce the reoperation rate in children and young adults: early report. Circulation 2011;124:S115–23. [DOI] [PubMed] [Google Scholar]
- 12. Sandica E, Boethig D, Blanz U, Goerg R, Haas NA, Laser KT. et al. Bovine jugular veins versus homografts in the pulmonary position: an analysis across two centers and 711 patients-conventional comparisons and time status graphs as a new approach. Thorac Cardiovasc Surg 2016;64:25–35. [DOI] [PubMed] [Google Scholar]
- 13. Ferraz Cavalcanti PE, Sa MP, Santos CA, Esmeraldo IM, de Escobar RR, de Menezes AM. et al. Pulmonary valve replacement after operative repair of tetralogy of Fallot: meta-analysis and meta-regression of 3,118 patients from 48 studies. J Am Coll Cardiol 2013;62:2227–43. [DOI] [PubMed] [Google Scholar]
- 14. Khanna AD, Hill KD, Pasquali SK, Wallace AS, Masoudi FA, Jacobs ML. et al. Benchmark outcomes for pulmonary valve replacement using the Society of Thoracic Surgeons Databases. Ann Thorac Surg 2015;100:138–45; discussion 145–6. [DOI] [PubMed] [Google Scholar]
- 15. Meijer FMM, Kies P, Jongbloed MRM, Hazekamp MG, Koolbergen DR, Blom NA. et al. Excellent durability of homografts in pulmonary position analysed in a predefined adult group with tetralogy of Fallot. Interact CardioVasc Thorac Surg 2019;28:279–83. [DOI] [PubMed] [Google Scholar]
- 16. Romeo JLR, Mokhles MM, van de Woestijne P, de Jong P, van den Bosch A, van Beynum IM. et al. Long-term clinical outcome and echocardiographic function of homografts in the right ventricular outflow tract. Eur J Cardiothorac Surg 2019;55:518--26. [DOI] [PubMed] [Google Scholar]
- 17. Bokma JP, Winter MM, Oosterhof T, Vliegen HW, van Dijk AP, Hazekamp MG. et al. Individualised prediction of pulmonary homograft durability in tetralogy of Fallot. Heart 2015;101:1717–23. [DOI] [PubMed] [Google Scholar]
- 18. Mercer CW, West SC, Sharma MS, Yoshida M, Morell VO.. Polytetrafluoroethylene conduits versus homografts for right ventricular outflow tract reconstruction in infants and young children: an institutional experience. J Thorac Cardiovasc Surg 2018;155:2082–91.e1. [DOI] [PubMed] [Google Scholar]
- 19. Bobylev D, Sarikouch S, Tudorache I, Cvitkovic T, Soylen B, Boethig D. et al. Double semilunar valve replacement in complex congenital heart disease using decellularized homografts. Interact CardioVasc Thorac Surg 2019;28:151–7. [DOI] [PubMed] [Google Scholar]
- 20. www.arise-clinicaltrial.eu (18 February 2019, date last accessed).