Abstract
OBJECTIVES
In this study, our aim was to explore how coronary artery bypass grafting affects quality of life, and how this varies with age, particularly with patients at risk of deterioration.
METHODS
In a retrospective, multicentre cohort study, patients with isolated coronary artery bypass grafting and electively operated between January 2011 and January 2015 with pre- and postoperative quality-of-life data were included. Patients were classified into 3 age groups: <65, 65–79 and ≥80 years. Quality of life was measured up to 1-year follow-up using the Short Form-12 or the Short Form-36 health survey. A multivariable, linear regression analysis, with an adjustment for confounders, was used to evaluate the association between age and quality of life.
RESULTS
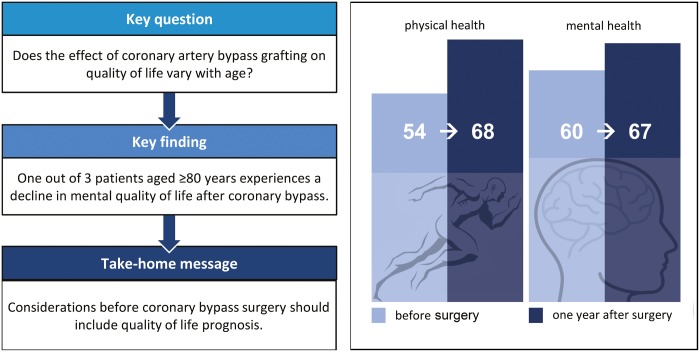
A total of 2606 patients were included in this study. Upon one-year of follow-up, the mean physical health of patients increased from 54 at baseline to 68, and mental health increased from 60 to 67. We observed decreased mental health in 20% of patients aged <65 years, 20% of patients aged 65–79 years and 29% of patients aged ≥80 years (P = 0.039). In this study, age was not associated with a lower physical or mental component score (P = 0.054 and P = 0.13, respectively). Independent risk factors for a decrease in quality of life consist of a better physical and mental score at baseline (P < 0.001) and a reduced left ventricular function (P < 0.001).
CONCLUSIONS
Most patients experience a relevant increase in physical and mental quality of life, but a proportion of patients aged ≥80 years undergo significant deterioration in mental health.
Keywords: Cardiac surgery, Coronary artery bypass grafting, Quality of life
INTRODUCTION
During the past decades, in Western countries, increasing life expectancy has resulted in a greater number of elderly people. Between 2011 and 2040, the Dutch population of 75 years and older is expected to double from 1.2 million to 2.6 million [1, 2]. As a result, during the next 30 years the number of patients with heart disease will increase by ∼55% [2], as will the number of older patients who might benefit from cardiac surgery. Meanwhile, continued advances in operative techniques, myocardial protection and perioperative care have led to a steady decline in operative mortality [3], thus further augmenting the number of elderly patients with a history of cardiac surgery.
Before making an informed decision as to whether to operate, one must weigh the potential advantages and disadvantages for each individual patient. The main reason to offer cardiac surgery is to improve survival and quality of life (QoL) [4]. The assessment of outcome measures has shifted from a physician’s perspective towards the patient’s perspective, and QoL is of critical importance for decision-making [5]. So far, findings on benefits in terms of QoL have been contradictory. Some studies report improvements in QoL [6, 7], whereas other studies allude to deterioration [8, 9]. Two review articles [9, 10] on QoL after coronary artery bypass grafting (CABG) have argued the need for more well-designed studies with a large number of patients, including preoperative and long-term postoperative quality-of-life data and information on patients lost to follow-up, to establish the generalizability of the results.
In this multicentre study, we evaluate in a large cohort of patients the influence of CABG on 1-year QoL and its variation with age. We also explore whether it is possible to identify characteristics of subgroups marked by deterioration in QoL.
MATERIALS AND METHODS
We conducted an observational, retrospective multicentre cohort study. The study was approved by the institutional review board of the Catharina Hospital Eindhoven (no. 2014-20), and conducted in agreement with the principles of the Helsinki declaration. The study is reported according to the REporting of studies Conducted using Observational Routinely collected health Data (RECORD) guidelines [11] (Supplementary Material Section S1 checklist).
Eligibility criteria
We included all adult patients who had undergone elective CABG and were operated between 1 January 2011 and 1 January 2015, and for whom preoperative and 1-year follow-up QoL data were available. Patients were operated in one of the 3 participating centres in the Netherlands: Isala Zwolle, Catharina Hospital Eindhoven or St. Antonius Hospital, Nieuwegein. We classified patients into 3 age groups: younger than 65 years, between 65 and 79 years and 80 years or older. We retrieved baseline demographic and clinical characteristics from the Netherlands Heart Registry (formerly Meetbaar Beter), a nationwide initiative of cardiac surgeons and cardiologists to improve the quality and transparency of care for patients with heart disease. All participating centres systematically collected patient-oriented and clinically relevant outcome measures [12]. We obtained mortality data from the regional municipal administration registration.
Baseline characteristics
Baseline demographic data included age, sex, body mass index (BMI), logistic European System for Cardiac Operative Risk Evaluation (log EuroSCORE I) and perioperative data, including the use of cardiopulmonary bypass and the number of grafts. We also collected data on previous cardiac surgery and comorbidities such as diabetes mellitus (oral therapy or insulin-dependent diabetes) [13], pulmonary disease (prolonged use of steroids or other lung medication) [14], arterial vascular disease (peripheral or abdominal vascular pathology or operation due to arterial vascular disease) [14], renal disease (a reduced renal function prior to surgery with an estimated glomerular filtration rate <60 ml/min/1.73 m2) [15] and ventricular function (left ventricular ejection fraction: good >50%, moderate 30–50% or poor <30%) [16]. The log EuroSCORE I is a widely used risk stratification system, which estimates the mortality risk for individual adult cardiac surgery patients [17].
Outcome measures
The primary outcome was QoL, which was assessed using the Short Form Health Survey-36 (SF-36; version 2) or the Short Form Health Survey-12 (SF-12; version 2). The SF-36 is a validated and widely used questionnaire for the assessment of QoL. The questionnaire consists of 8 domains: vitality, physical functioning, bodily pain, general health perceptions, physical role functioning, emotional role functioning, social role functioning and mental health [18]. The SF-12 is a shortened version of the SF-36 questionnaire, developed to limit the survey length [19]. Two summarized scores can be calculated from both instruments: a physical component summary (PCS) and a mental component summary (MCS). A higher score indicates a better QoL; a score of zero is equivalent to maximum disability and a score of 100 is equivalent to no disability [18]. The Isala and Catharina Hospitals used the SF-36 questionnaire, and the St. Antonius Hospital used the SF-12 questionnaire. Because the same domain and summary scores are calculated with a standard syntax file, and because in patients with coronary disease the sensitivity and responsiveness to change measured by both questionnaires seem similar [19], all data were merged into 1 database.
We assessed QoL at baseline (up to 2 months before surgery) and 10–14 months after surgery. For inclusion, at least 50% of the questions of each domain had to be filled in when using the SF-36 and 100% when using the SF-12. For each patient we calculated an increase, decrease or no change in QoL at 1 year after surgery compared to baseline. The minimal clinically important difference (MCID) was set at 5 points: an increased QoL was defined by an increase in the component score >5 points, a decrease was defined by a decrease in score >5 points, and no change in QoL was defined by a ≤ 5 point decrease or increase in score [20]. We defined as responders patients who completed both the preoperative and follow-up questionnaires. Non-responders were patients who completed only the preoperative questionnaire. We compared demographics, comorbidity, surgical data and preoperative QoL between the responders and non-responders to evaluate the generalizability.
Secondary outcomes were postoperative complications including surgical re-exploration [13], deep sternal wound infection [21], renal failure within 30 days after surgery [14] and stroke within 72 h after surgery [22]. Coronary reintervention and myocardial infarction were measured up to 1 year after surgery [13]. Definitions of complications are included in the Supplementary Material Section S1 checklist.
Analyses
Characteristics of patients are presented as proportions (with percentages) for dichotomous variables. Differences in dichotomous variables between the age groups were tested using the χ2 test or the Fisher’s exact test. The analysis of variance was used, with multiple comparison (Bonferroni correction) for analyses of age groups. Differences between summary scores at baseline and at 1-year follow-up were tested using a paired t-test. On the basis of a recent study concerning MCID in SF-36 scores, sensitivity analyses were conducted using an MCID of 4 points [23]. The linear regression analysis was used to evaluate the impact of age (independent variable) on the difference in QoL (dependent variable). Univariable analyses were used to identify possible deteriorating subgroups based on comorbidities at baseline; age was always included as the independent variable in the model, because this was our variable of interest. All variables with P < 0.1 in the univariable analyses were included in the multivariable model. All analyses were tested 2-sided, and variables with P-values of <0.05 were considered statistically significant. All data were analysed using SPSS version 23.0 (IBM Corp. Released 2015. IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY).
RESULTS
A total of 8643 patients underwent an elective CABG procedure in the 3 participating centres. Of them, both the preoperative and the postoperative quality-of-life assessments were completed (responders) in 2606 patients (30%).
Characteristics of the patients
Table 1 presents all baseline, operative and postoperative characteristics of the study population. The proportion of women increases with age (P < 0.001). A greater proportion of patients aged 65–79 years suffered from diabetes, pulmonary and/or arterial vascular disease. Patients aged ≥80 years more frequently had reduced left ventricular function (P = 0.010) and renal disease prior to surgery (P < 0.001). During hospitalization, the incidence of stroke was higher in patients aged 65–79 years (P = 0.040). We observed no significant differences between the 3 age groups concerning any of the other postoperative complications.
Table 1:
Baseline, operative and postoperative characteristics of patients with CABG
| <65 years (n = 1073) | 65–79 years (n = 1380) | ≥80 years (n = 153) | P-value | |
|---|---|---|---|---|
| Baseline characteristics | ||||
| Sex (female) | 136 (13) | 283 (21) | 56 (37) | <0.001 |
| BMIa (kg/m2) | 0.035 | |||
| <25 | 158 (23) | 252 (27) | 33 (34) | |
| 25–30 | 353 (51) | 454 (49) | 48 (50) | |
| >30 | 180 (26) | 214 (23) | 15 (16) | |
| Log EuroSCOREb I (%) | <0.001 | |||
| <10 | 1065 (99) | 1299 (94) | 121 (79) | |
| 10–20 | 4 (0.4) | 68 (4.9) | 25 (16) | |
| >20 | 0 (0.0) | 13 (0.9) | 7 (4.6) | |
| Diabetes mellitus | 202 (19) | 340 (25) | 35 (23) | 0.003 |
| Pulmonary disease | 70 (6.5) | 138 (10) | 12 (7.8) | 0.009 |
| Arterial vascular disease | 74 (6.9) | 183 (13) | 17 (11) | <0.001 |
| Renal disease (ml/min/1.73 m2) | <0.001 | |||
| eGFR ≥60 | 985 (92) | 1081 (78) | 84 (55) | |
| eGFR 30–59 | 84 (7.8) | 283 (21) | 67 (44) | |
| eGFR <30 | 4 (0.4) | 16 (1.2) | 2 (1.3) | |
| LVEFc (%) | 0.010 | |||
| >50 | 871 (81) | 1058 (77) | 110 (72) | |
| 30–50 | 173 (16) | 263 (19) | 39 (26) | |
| <30 | 29 (2.7) | 55 (4.0) | 4 (2.6) | |
| Previous cardiac surgery | 16 (1.5) | 28 (2.0) | 2 (1.3) | 0.55 |
| Operative characteristics | ||||
| Use of 1 arterial graft | 438 (41) | 861 (62) | 109 (71) | <0.001 |
| Use of 2 or more arterial grafts | 594 (55) | 469 (34) | 41 (27) | |
| Use of ECCa | 653 (94) | 860 (93) | 93 (97) | 0.24 |
| Postoperative characteristics | ||||
| Deep sternal wound infection | 5 (0.5) | 7 (0.5) | 2 (1.3) | 0.33 |
| Stroke | 0 (0.0) | 7 (0.5) | 0 (0.0) | 0.040 |
| Renal failure | 2 (0.2) | 2 (0.1) | 0 (0.0) | 1.00 |
| Surgical re-exploration | 24 (2.2) | 45 (3.3) | 3 (2.0) | 0.25 |
| Myocardial infarctiond | 26 (2.5) | 22 (1.6) | 3 (2.0) | 0.34 |
| Coronary reinterventione | 31 (2.9) | 45 (3.3) | 2 (1.4) | 0.41 |
Values are presented as n (%).
BMI is unknown for 899 patients and the use of ECC is unknown for 884 patients; data are available from two of the participating hospitals.
Log EuroSCORE I, data missing for 4 patients.
LVEF, data missing for 4 patients.
Myocardial infarction, data missing for 34 patients.
Coronary reintervention, data missing for 29 patients.
BMI: body mass index; CABG: coronary artery bypass grafting; ECC: extracorporeal circulation; eGFR: estimated glomerular filtration rate; LVEF: left ventricular ejection fraction.
Quality of life
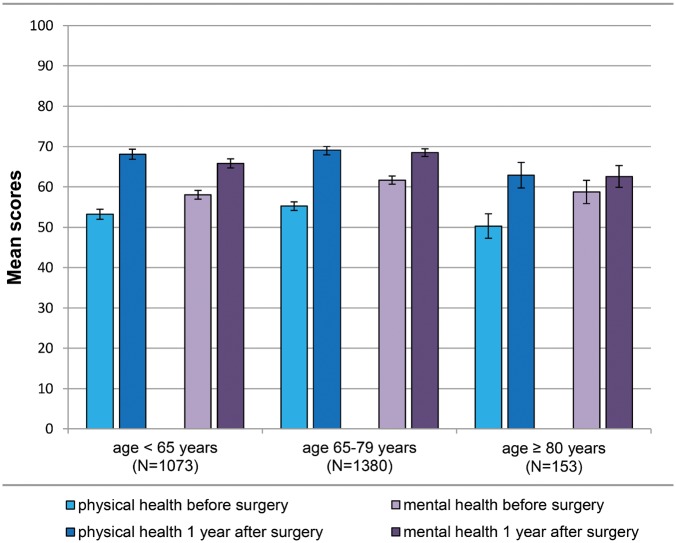
Mean MCS and PCS scores at baseline and at 1-year follow-up are presented in bar charts per age group (Fig. 1). All subscale scores are provided in the Supplementary Material, Section S3. Differences in QoL between baseline and 1 year after surgery are presented in Fig. 2A and B. We observed a decrease in physical health 1 year after CABG (>5 points) in 15% of patients younger than 65 years, in 15% of patients between 65 and 79 years and in 16% of patients ≥80 years (P = 0.92; Fig. 2A). We registered a decrease in mental health 1 year after CABG (>5 points) in 20% of patients aged <65 years, in 20% of patients aged 65–79 years and in 29% of patients aged ≥80 years (P = 0.039) (Fig. 2B). Sensitivity analyses (using an MCID of 4 points) of differences in QoL revealed similar proportions of decreased physical and mental health components (Supplementary Material, Section S4A and B).
Figure 1:
Quality-of-life data of patients with coronary artery bypass grafting according to age categories. Mean scores of the physical and the mental health component scores (with 95% confidence intervals) of patients with coronary artery bypass grafting before and 1 year after surgery for each age category.
Figure 2:
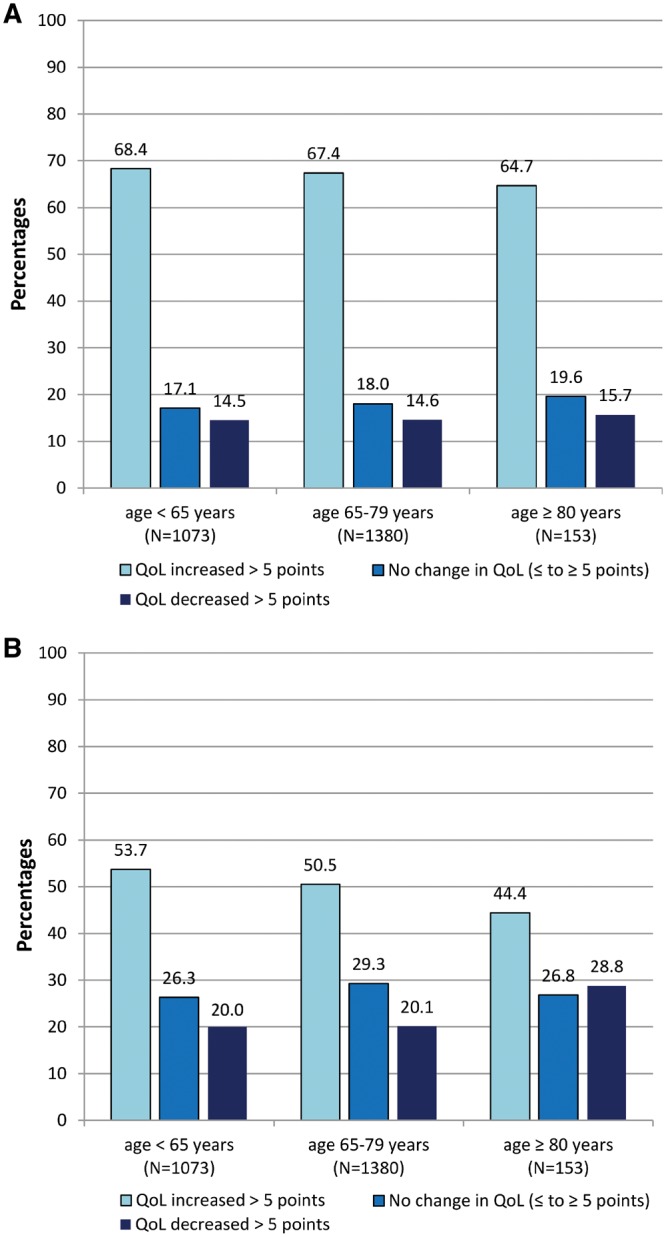
(A) Difference in QoL of patients with coronary artery bypass grafting: physical component score. Differences between baseline and 1-year follow-up per age group, in the quality of life physical component score; cut-off value 5 points. (B) Difference in quality of life of patients with coronary artery bypass grafting: the mental component score. Differences between baseline and 1-year follow-up per age group, in the quality of life mental component score; cut-off value 5 points. QoL: quality of life.
Association between age and quality of life
Table 2 shows the results of the regression analysis. Higher age was not significantly associated with a difference in QoL after 1-year follow-up (PCS P = 0.054 and MCS P = 0.13; respectively). Differences in QoL between men and women were also not significant. The multivariable regression analysis identified baseline PCS (P < 0.001), pulmonary disease (P < 0.001), a reduced left ventricular function (P < 0.001 for 30–50%) and renal disease (P < 0.001) as independent risk factors of a decreased physical QoL 1 year after surgery. The baseline MCS (P < 0.001) and a reduced left ventricular function (P < 0.001 for 30–50% ejection fraction) were identified as independent risk factors for decreased mental QoL 1 year after surgery. R2 is 0.25 for the multivariable PCS model and 0.24 for the multivariable MCS model, meaning that ∼25% variation in the dependent variable, i.e. change in QoL, can be explained by the independent variables included in the multivariable models.
Table 2:
Association between age and difference in quality of life in patients with CABG
| Univariable analysis (single component age adjusted) | Multivariable analysis (adjusted for all variables listed) | |||||
|---|---|---|---|---|---|---|
| Physical component score | Physical component score | |||||
| Beta | 95% CI | P-value | Beta | 95% CI | P-value | |
| Age (years) | −0.82 | −0.16 to 0.00 | 0.054 | −0.04 | −0.11 to 0.03 | 0.28 |
| Baseline PCS | −0.46 | −0.49 to −0.42 | <0.001 | −0.47 | −0.51 to −0.44 | <0.001 |
| Pulmonary disease | −4.04 | −6.75 to −1.32 | 0.004 | −7.27 | −9.65 to −4.89 | <0.001 |
| LVEF | ||||||
| EF 30–50% | −2.80 | −4.77 to −0.83 | 0.005 | −3.23 | −4.94 to −1.51 | <0.001 |
| EF <30% | −0.63 | −4.82 to 3.57 | 0.77 | −1.44 | −5.10 to 2.22 | 0.44 |
| Renal disease | −0.03 | −0.04 to −0.01 | 0.002 | −0.03 | −0.04 to −0.01 | <0.001 |
| Previous cardiac surgery | 9.89 | 4.16 to 15.61 | 0.001 | 0.99 | −4.04 to 6.03 | 0.69 |
| Mental component score | Mental component score | |||||
| Beta | 95% CI | P-value | Beta | 95% CI | P-value | |
| Age (years) | −0.06 | −0.13 to 0.02 | 0.13 | 0.01 | −0.05 to 0.08 | 0.67 |
| Baseline MCS | −0.45 | −0.49 to −0.42 | <0.001 | −0.46 | −0.49 to −0.43 | <0.001 |
| Sex | 3.09 | 1.33 to 4.84 | 0.001 | −1.17 | −2.72 to 0.38 | 0.14 |
| LVEF | ||||||
| EF 30–50% | −3.54 | −5.27 to −1.80 | <0.001 | −3.70 | −5.22 to −2.19 | <0.001 |
| EF <30% | −1.49 | −5.20 to 2.22 | 0.43 | −2.18 | −5.38 to 1.02 | 0.18 |
| Previous cardiac surgery | 5.08 | −0.00 to 10.17 | 0.050 | −0.02 | −4.43 to 4.38 | 0.99 |
Adjusted univariable and multivariable association between age and difference in the physical or the mental component score.
Beta: unstandardized regression coefficient; CABG: coronary artery bypass grafting; CI: confidence interval; LVEF: left ventricular ejection fraction; MCS: mental component summary; PCS: physical component summary.
Responders and non-responders
Non-responders (n = 1644) provided baseline data on QoL but no follow-up data. Baseline characteristics, operative characteristics and postoperative complications of responders and non-responders are listed in Table 3.
Table 3:
Baseline, operative and postoperative characteristics of responding and non-responding patients with CABG
| Responders (n = 2606) | Non-responders (n = 1644) | P-value | |
|---|---|---|---|
| Baseline characteristics | |||
| Sex (female) | 475 (18) | 374 (23) | <0.001 |
| Age, mean (SD) | 66 (9.0) | 65.7 (10.2) | 0.34 |
| BMIa (kg/m2) | 0.042 | ||
| <25 | 443 (26) | 214 (25) | |
| 25–30 | 855 (50) | 410 (47) | |
| >30 | 409 (24) | 249 (29) | |
| Log EuroSCOREb I (%) | 0.024 | ||
| <10 | 2485 (96) | 1538 (94) | |
| 10–20 | 97 (3.7) | 80 (4.9) | |
| >20 | 20 (0.8) | 23 (1.4) | |
| Diabetes mellitusc | 577 (22) | 455 (28) | <0.001 |
| Pulmonary diseasec | 220 (8.4) | 164 (10) | 0.089 |
| Arterial vascular diseasec | 274 (11) | 222 (14) | 0.003 |
| Renal diseasec (ml/min/1.73 m2) | <0.001 | ||
| eGFR ≥60 | 2150 (83) | 1257 (77) | |
| eGFR 30–59 | 434 (17) | 359 (22) | |
| eGFR <30 | 22 (0.8) | 27 (1.6) | |
| LVEFd (%) | 0.31 | ||
| >50 | 2039 (78) | 1261 (77) | |
| 30–50 | 475 (18) | 310 (19) | |
| <30 | 88 (3.4) | 69 (4.2) | |
| Previous cardiac surgery | 46 (1.8) | 37 (2.3) | 0.27 |
| QoL score baseline PCS, mean (SD) | 54.1 (20.4) | 53.6 (21.9) | 0.42 |
| QoL score baseline MCS, mean (SD) | 60.0 (18.6) | 57.8 (20.6) | 0.001 |
| Operative characteristics | |||
| Use of 1 arterial graft | 1408 (54) | 981 (60) | <0.001 |
| Use of 2 or more arterial grafts | 1104 (42) | 593 (36) | |
| Use of ECCa | 1606 (93) | 803 (90) | 0.005 |
| Postoperative characteristics | |||
| Deep sternal wound infection | 14 (0.5) | 11 (0.7) | 0.58 |
| Stroke | 7 (0.3) | 14 (0.9) | 0.008 |
| Renal failure | 4 (0.2) | 11 (0.7) | 0.006 |
| Surgical re-exploration | 72 (2.8) | 63 (3.8) | 0.053 |
| Myocardial infarctione | 51 (2.0) | 25 (1.7) | 0.49 |
| Coronary reinterventionf | 78 (3.0) | 53 (3.6) | 0.35 |
All numbers are presented with percentages, unless otherwise indicated.
BMI and the use of ECC data available from two of the participating hospitals.
Log EuroSCORE 1 for 13 patients is unknown.
Diabetes mellitus, pulmonary disease, arterial vascular disease and renal disease is unknown for 2 patients.
LVEF for 22 patients is unknown.
Myocardial infarction for 458 patients is unknown.
Coronary reintervention for 451 patients is unknown.
BMI: body mass index; CABG: coronary artery bypass grafting; ECC: extracorporeal circulation; LVEF: left ventricular ejection fraction; MCS: mental component summary; PCS: physical component summary; QoL: quality of life; SD: standard deviation.
In the non-responder group, 37 patients (2.3%) died within <120 days, and a total of 75 patients (4.6%) died during the first year. Significant differences between the groups were BMI (P = 0.042), diabetes (P < 0.001), arterial vascular disease (P = 0.003) and renal disease (P < 0.001). Also, the incidence of postoperative complications, such as stroke (P = 0.008) and renal failure (P = 0.006), was higher among the non-responders. Between both groups baseline PCS measurements were similar (P = 0.42), but we found statistically significant differences in baseline MCS (P = 0.001).
DISCUSSION
One year after CABG the quality of life of patients usually increases rather than decreases. The potential beneficial effects of CABG hold true especially for the physical component score of QoL. We observed less favourable effects of CABG on the mental component score. Age as a continuous variable was not significantly associated with a difference in QoL after 1 year of follow-up. Nevertheless, 1 out of 3 patients aged ≥80 years reported a decline in mental QoL.
Several factors might explain why some patients report a decline in QoL. The results of this study show that baseline MCS and baseline PCS are both independent risk factors for a decreased QoL after CABG; in other words, patients with a higher QoL before surgery are more at risk of experiencing a decreased QoL after surgery. This finding, in statistics known as regression to the mean, is also observed in other studies [7, 24, 25], resulting in convincing evidence that a QoL assessment should be part of the preoperative examination, and expectations regarding QoL should also be discussed with the patient preoperatively. Another factor behind the decline in QoL in some patients could be side-effects of surgery, like a new comorbidity or reduced independence. Postoperative cognitive decline after CABG is reported with incidence rates varying between 30% and 60%, depending on cognitive tests, time of assessment and the patient population [26, 27]. Cognitive performance, QoL and the ability to perform daily activities reflect on patient-centred domains that are crucial to the patient’s retention of independence [26]. Furthermore, factors influencing QoL, like other health problems or loss of relatives, might have been experienced in these patients irrespective of cardiac surgery, and not at all been caused by the intervention.
In our study population, we found significant differences in baseline characteristics; more patients aged 65–79 years suffered from diabetes, pulmonary disease and/or arterial vascular disease. Also, the incidence of postoperative stroke was significantly higher in this age group. These findings however, do not account for the lower postoperative physical or mental QoL observed in our patients aged ≥80 years; this suggests that QoL relates to much more than just the presence of symptoms of disease, comorbidities and complications of surgery. The Constitution of the World Health Organization (WHO) defined QoL as ‘individuals’ perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns’ [28]; in other words, QoL is influenced by various physical, mental, social and environmental factors. This probably explains why independent ‘medical’ variables account for only 25% of the variance of QoL in both of our regression models. Future studies to compare the QoL of patients after surgery with patients after less invasive treatments (e.g. medication or percutaneous interventions) would provide valuable knowledge about the real harms and benefits of surgery on elderly patients and the impact on their QoL.
To assess the generalizability of our results we compared data from the responding and non-responding patients with CABG, as recommended by Noyez et al. [10]. We included information on demographics, comorbidity and the cardiac risk of all patients who could possibly have been included and on the patients actually included. Compared to the responding patients the non-responders had a higher prevalence of several comorbidity risk factors. A recent study suggested that the so-called non-responders in studies evaluating QoL after cardiac surgery may be older, be at higher operative risk and have a lower preoperative QoL; these factors may result in a positive overestimation of change in QoL for the total population [29]. This also seems to apply to our study meaning that in the total population of –patients with CABG, the number of patients with decreased mental well-being might be higher. However, compared to the QoL data from an age-matched control group of Dutch inhabitants, data from our patients resulted in remarkably high PCS and MCS scores (mean PCS 54.1 vs 50.4 and mean MCS 60.0 vs 52.5 for responders vs the general population) [30].
Our multicentre study also has important limitations. First, the number of patients with total available QoL data is low (30%), and reasons for the lack of pre- and/or postoperative data remain unclear. All data were collected by e-mail or a written survey, which might have led to reporting bias. A more personal approach (e.g. follow-up by telephone or at the outpatient clinic) might have led to higher response rates. For the non-responders, we chose to include only patients with complete preoperative QoL information, because these are the only patients from whom we could expect 1-year QoL data. Second, we lack information on preoperative mental health, discharge destination, participation in a rehabilitation programme and other events influencing QoL upon 1-year follow-up (e.g. other health problems, dependency or loss of relatives). Third, we lack information on survival and QoL from patients who were not accepted for surgery.
The outcomes of our study show that although most patients experience an improved physical and mental quality of life, a relevant proportion of patients deteriorate in mental health. Because in vulnerable elderly patients a small decline can have important consequences for their daily lives, such as loss of independence, it is imperative to discuss this issue during preoperative counselling.
Conflict of interest: Massimo A. Mariani has received grants from Atricure Inc., Edwards Lifesciences and Abbot Inc. and has given training for Livanova and Getinge. All other authors declared no conflict of interest.
Supplementary Material
Footnotes
Presented at the 32nd Annual Meeting of the European Association for Cardio-Thoracic Surgery, Milan, Italy, 18–20 October 2018.
REFERENCES
- 1. de Jong A, Daalhuizen F.. De Nederlandse Bevolking in Beeld Verleden Heden Toekomst. Planbureau voor de Leefomgeving; 2014. www.pbl.nl (19 May 2018, date last accessed). [Google Scholar]
- 2. Vaartjes I, Dis I, Van Vissseren FLJ, Bots ML.. Hart- en vaatziekten in Nederland 2015. Centrum; 2015, 132 http://www.hartstichting.nl/9800/13341/15305/HVZ_in_Nederland_2010 (20 February 2018, date last accessed). [Google Scholar]
- 3. Huber CH, Goeber V, Berdat P, Carrel T, Eckstein F.. Benefits of cardiac surgery in octogenarians–a postoperative quality of life assessment. Eur J Cardiothorac Surg 2007;31:1099–105. [DOI] [PubMed] [Google Scholar]
- 4. Sousa-Uva M, Neumann F-J, Ahlsson A, Alfonso F, Banning AP, Benedetto U.. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur J Cardiothorac Surg 2019;55:4–90. [DOI] [PubMed] [Google Scholar]
- 5. Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck-Ytter Y, Schünemann HJ.. What is “quality of evidence” and why is it important to clinicians? BMJ 2008;336:995–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Baig K, Harling L, Papanikitas J, Attaran S, Ashrafian H, Casula R. et al. Does coronary artery bypass grafting improve quality of life in elderly patients? Interact CardioVasc Thorac Surg 2013;17:542–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Shan L, Saxena A, McMahon R, Newcomb A.. Coronary artery bypass graft surgery in the elderly: a review of postoperative quality of life. Circulation 2013;128:2333–43. [DOI] [PubMed] [Google Scholar]
- 8. Markou ALP, van der Windt A, van Swieten HA, Noyez L.. Changes in quality of life, physical activity, and symptomatic status one year after myocardial revascularization for stable angina. Eur J Cardiothorac Surg 2008;34:1009–15. [DOI] [PubMed] [Google Scholar]
- 9. Abah U, Dunne M, Cook A, Hoole S, Brayne C, Vale L. et al. Does quality of life improve in octogenarians following cardiac surgery? A systematic review. BMJ Open 2015;5:e006904.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Noyez L, De Jager MJ, Markou AL.. Quality of life after cardiac surgery: underresearched research. Interact CardioVasc Thorac Surg 2011;13:511–15. [DOI] [PubMed] [Google Scholar]
- 11. Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I. et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) Statement. PLoS Med 2015;12:e1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. van Veghel D, Marteijn M, de Mol B.. First results of a national initiative to enable quality improvement of cardiovascular care by transparently reporting on patient-relevant outcomes. Eur J Cardiothorac Surg 2016;49:1660–9. [DOI] [PubMed] [Google Scholar]
- 13.Stichting Meetbaar Beter. Meetbaar Beter Boek 2015. November 2. Math Made, D&B Communicatie en Drukkerij Snep; 2015, 1–172. www.meetbaarbeter.com (21 January 2018, date last accessed).
- 14.Projectgroep BHN Registratieproject. Handboek BHN Registratieproject v4.01. Afdeling Klinische Informatiekunde, AMC Amsterdam; 2015, 1–180.
- 15. Stevens PE, Levin A.. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med 2013;158:825. [DOI] [PubMed] [Google Scholar]
- 16. Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L. et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 2015;16:233–71. [DOI] [PubMed] [Google Scholar]
- 17. Roques F, Michel P, Goldstone AR, Nashef SAM.. The logistic EuroSCORE. Eur Heart J 2003;24:881–2. [DOI] [PubMed] [Google Scholar]
- 18. Ware JEJ, Sherbourne CD.. The MOS 36-ltem short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992;30:473–83. [PubMed] [Google Scholar]
- 19. Müller-Nordhorn J, Roll S, Willich SN.. Comparison of the short form (SF)-12 health status instrument with the SF-36 in patients with coronary heart disease. Heart 2004;90:523–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stichting Meetbaar Beter. Meetbaar Beter Boek 2016. Math Made, D&B Communicatie en Drukkerij Snep; 2016, 1–174. www.meetbaarbeter.com.
- 21.Projectgroep BHN Registratieproject. BHN Registratieproject Handboek v4.0. Afdeling Klinische Informatiekunde, AMC Amsterdam; 2014, 1–189.
- 22. Sacco RL, Kasner SE, Broderick JP, Caplan LR, Connors JJ, Culebras A. et al. An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013;44:2064–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Badhiwala JH, Witiw CD, Nassiri F, Akbar MA, Jaja B, Wilson JR. et al. Minimum clinically important difference in SF-36 scores for use in degenerative cervical myelopathy. Spine 2018;43:E1260–6. [DOI] [PubMed] [Google Scholar]
- 24. Noyez L, Markou ALP, van Breugel FCF.. Quality of life one year after myocardial revascularization. Is preoperative quality of life important? Interact CardioVasc Thorac Surg 2006;5:115–20. [DOI] [PubMed] [Google Scholar]
- 25. Kurfirst V, Mokráček A, Krupauerová M, Canádyová J, Bulava A, Pešl L. et al. Health-related quality of life after cardiac surgery–the effects of age, preoperative conditions and postoperative complications. J Cardiothorac Surg 2014;9:46.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Selnes OA, Gottesman RF, Grega MA, Baumgartner WA, Zeger SL, Mckhann GM.. Cognitive and neurologic outcomes after coronary-artery bypass surgery. N Engl J Med 2012;366:250–7. [DOI] [PubMed] [Google Scholar]
- 27. Kok WF, van Harten AE, Koene BM, Mariani MA, Koerts J, Tucha O. et al. A pilot study of cerebral tissue oxygenation and postoperative cognitive dysfunction among patients undergoing coronary artery bypass grafting randomised to surgery with or without cardiopulmonary bypass. Anaesthesia 2014;69:613–22. [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization. Health Statistics and Information Systems. 2018. http://www.who.int/healthinfo/survey/whoqol-qualityoflife/en/ (21 January 2018, date last accessed).
- 29. Noyez L. Is quality of life post cardiac surgery overestimated? Health Qual Life Outcomes 2014;12:2–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Centraal Bureau voor de Statistiek. Gezondheid, aandoeningen, beperkingen; leeftijd en geslacht, 2010-2013. 2014. http://statline.cbs.nl (19 May 2018, date last accessed).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.