Abstract
The health benefits of physical activity (PA) are acknowledged and promoted by the scientific community, especially within primary care. However, there is little evidence that such promotion is provided in any consistent or comprehensive format. Brief interventions (i.e. discussion, negotiation or encouragement) and exercise referral schemes (i.e. patients being formally referred to a PA professional) are the two dominant approaches within primary care. These cost-effective interventions can generate positive changes in health outcomes and PA levels in inactive patients who are at increased risk for non-communicable diseases. Their success relies on the acceptability and efficiency of primary care professionals to deliver PA counselling. To this end, appropriate training and financial support are crucial. Similarly, human resourcing and synergy between the different stakeholders must be addressed. To obtain maximum adherence, specific populations should be targeted and interventions adapted to their needs. Key enablers include motivational interviewing, social support and multi-disciplinary approaches. Leadership and lines of accountability must be clearly delineated to ensure the success of the initiatives promoting PA in primary care. The synergic and multisectoral action of several stakeholders, especially healthcare professionals, will help overcome physical inactivity in a sustainable way.
Keywords: physical activity, evidence-based health promotion, non-communicable diseases, primary care
INTRODUCTION
Physical inactivity is considered by the World Health Organization (WHO) as one of the leading risk factors for non-communicable diseases (NCDs) (World Health Organization, 2013). It is responsible for causing more than five million deaths worldwide each year, including 6% of the burden of disease from coronary heart disease, 7% of type 2 diabetes, 10% of breast cancer and 10% of colon cancer (Lee et al., 2012) with a global healthcare cost estimated at 53.8 billion US dollars (Ding et al., 2016). Conversely, physical activity (PA) helps to reduce the rate of NCDs (Pedersen and Saltin, 2015) but also stress, anxiety and depression, and improves mental wellbeing (Sallis et al., 2016, Stranges et al., 2014, World Health Organization, 2015a). Moreover, PA is associated with other healthy behaviours, including better eating patterns, abstention from smoking, and sleep hygiene (Pate et al., 1996, Stranges et al., 2008).
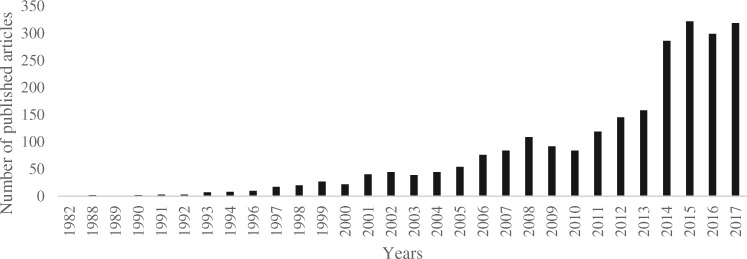
Considering the health benefits of PA, its promotion has increasingly been recognized as a priority for public health, supported by many countries through the development of policies and interventions (Bull et al., 2015, Kahlmeier et al., 2014). In 2013, the WHO published the ‘Global Action Plan for the Prevention and Control of Non-communicable Diseases 2013–20’ (World Health Organization, 2013), underlining the importance of PA in the prevention and management of NCDs. The importance of the contribution by the health sector, particularly in primary care, is becoming increasingly recognized. The ‘Physical activity strategy for the WHO European Region 2016–25’ recommends that ‘Member States should work towards making the promotion of physical activity by health professionals the norm’ and that ‘early identification, counselling and referral at the primary care level should be integrated into standard practice and should respond to the different needs of patients’ (World Health Organization, 2015b). Moreover, the Toronto Charter for Physical Activity recommends that PA and NCDs prevention should be integrated into primary healthcare systems (Global Advocacy for Physical Activity the Advocacy Council of the International Society for Physical and Health, 2012). Recently, there have been calls in leading medical journals to implement PA counselling in primary care as a preventive medicine measure (AuYoung et al., 2016, Berra et al., 2015, Das and Horton, 2016, Estabrooks et al., 2003, Heath et al., 2012, Khan et al., 2011, Williams, 2011). The number of articles concerning PA within primary care has doubled between 2012 and 2014 (Figure 1), illustrating the growing interest amongst researchers and funding bodies.
Fig. 1:
Number of PubMed-referenced articles published between 1982 and 2017 concerning ‘physical activity’ and ‘primary care’.
Several approaches to promote PA to patients in healthcare settings have shown small but positive effects (Hillsdon et al., 2005, Orrow et al., 2012, Sanchez et al., 2015). Does sustainable and efficient implementation of PA counselling within primary care, however, remain a Utopian quest? Several factors contribute to its success or failure: promotional approaches, healthcare professionals’ involvement and skills, patients’ awareness and engagement, characteristics of the PA programmes, costs and political support. The aim of this contribution is to present and critically discuss these factors using selected examples.
APPROACHES OF PA PROMOTION WITHIN PRIMARY CARE
Brief interventions
A brief intervention involves discussion, negotiation or encouragement, other support or follow-up (National Institute for Health and Care Excellence, 2013), often taking no more than a few minutes for basic advice. It may also involve a referral for further interventions, directing people to other options, or more intensive support. Brief interventions can be delivered by any trained healthcare professional (e.g. nurses, primary care physicians, pharmacists, physiotherapists, etc.). PA levels increase in participants who received brief interventions in primary care (Elley et al., 2003, Lamming et al., 2017, National Institute for Health and Care Excellence, 2013, Pears et al., 2016, Pears et al., 2015), as compared with usual care [effect size: 0.17; 95% confidence interval (CI): 0.06–0.28] (Campbell et al., 2012). The evidence is limited, however, regarding long-term impact, effectiveness, feasibility and acceptability, and on the impact of tailoring advice, types of providers, provider training and setting (Lamming et al., 2017).
Exercise referral schemes
Generally, an ‘exercise referral’ involves patients being formally referred by health professionals to a third party, often an exercise professional. Several programmes around the world currently test/use variations of exercise referral/prescription (see examples in Table 1), typically modified prescription forms issued by a physician or other licensed health professionals that record baseline clinical, physiological and personal data and prescribe PA. Interventions vary widely in terms of what is done within and outside of the healthcare system, and whether PA is promoted individually or in groups.
Table 1:
Examples of initiatives providing a prescription form
| Initiative name | Country/nation |
|---|---|
| Exercise is Medicine® Australia | Australia |
| Sport sur ordonnance | Belgium |
| Exercise is Medicine® Canada | Canada |
| Motion på recept | Denmark |
| Physical Activity Prescription | Finland |
| Sport sur ordonnance | France |
| Rezept für Bewegung | Germany |
| Green Prescription | New Zealand |
| Healthwise | Northern Ireland |
| Grønn recep | Norway |
| Exercise is Medicine® Poland | Poland |
| Diabetes em Movimento | Portugal |
| Qatar National Physical Activity Guidelines | Qatar |
| Exercise is Medicine® Singapore | Singapore |
| Caminem programe | Spain |
| Fysisk Aktivitet på Recept, FaR® | Sweden |
| Physical Activity Promotion in Primary Care | Switzerland |
| Care Sport Connectors | The Netherlands |
| Exercise is Medicine® | United States of America |
| Let's Get Moving | United Kingdom |
| National Exercise Referral Scheme | Wales |
Consultation between the physician or other licensed healthcare staff and the patient, and written PA prescription were common factors amongst the various approaches within the Scandinavian region (Kallings, 2011). The ‘Beweegkuur’ intervention in the Netherlands aimed to steer patients’ toward more autonomy for lifestyle improvements (Berendsen et al., 2015, Rutten et al., 2014). Beweegkuur increased light and moderate PA by 2.1 h/week (95% CI: 1.0–3.2) and improved mobility, mood, pain, blood pressure, blood sugar and weight loss (Schutte et al., 2015). Three systematic reviews show that, compared with usual care, exercise referral schemes had a small effect in increasing the proportion of individuals achieving 90–150 min of at least moderate intensity activity per week (relative risk range: 1.12–1.20, 95% CI range: 1.03–1.35) (Campbell et al., 2015, Pavey et al., 2011, Williams et al., 2007). Whilst studies suggest exercise referral schemes may improve compliance with PA recommendations compared with brief interventions (Gallegos-Carrillo et al., 2017) and the rate of adherence to PA following PA prescription (effect size: 0.17, 95% CI: 0.09–0.24) (Arsenijevic and Groot, 2017), gaps in the evidence still exist (Pakravan and Jones, 2014). The lack of evidence of effectiveness may be linked to large variations in schemes including characteristics of the PA sessions (e.g. time, cost, location etc.) (Morgan et al., 2016). Given the limited evidence, NICE in the UK recommends restricting exercise referral schemes to sedentary high-risk patients (National Institute for Health and Care Excellence, 2014).
Exercise referral schemes with connectors
Although some primary care physicians and other members of the primary care team are keen to promote PA in clinic (Helmink et al., 2012, Pears et al., 2015), they often avoid referring for differing reasons (please see subsection below). An emerging type of intervention, involving ‘Care Sport Connectors’ (healthcare or community-based exercise professional) who connects primary care and the sport and recreation sector, is being tested in the Netherlands (Leenaars et al., 2016b). Patients are referred to these ‘connectors’ who help them be more physically active, by explaining the benefits and normalizing PA as a behaviour rather than a therapy. They guide patients towards local PA opportunities in the patients’ locality, often at a time suited to them. This approach reduces the burden on pressurized health services. Professionals involved in this intervention ascribed three roles to the connector: broker, referral and facilitator (Leenaars et al., 2016a, 2016b). To be effective a connector should be identified with appropriately trained, resourced and dedicated professional support, and the intervention aligned to condition management pathways. The often overlooked ‘added value’ is that knowledge and skills accrued can be applied to the general population as well.
HEALTHCARE PROFESSIONALS’ PERSPECTIVES
Primary care practitioners are well placed to help address the problems of physical inactivity (Hoffmann et al., 2016, Thornton et al., 2016). They have greater access to the population as a whole than any other single health professional (Gates, 2016, McNally, 2015), frequent engagement with those most in need of PA advice (McNally, 2015), and are a trusted source of lifestyle advice and information (Weiler et al., 2012a). Primary care professionals (e.g. physicians, nurses, physiotherapists, etc.) can evaluate patients’ PA behaviour using the 5As framework (assess, advise, agree, assist, arrange) (Estabrooks et al., 2003): assess patients’ PA level, physical abilities, readiness to change and beliefs and knowledge; advise on health risks, the benefit of change and appropriate dose of PA; agree upon an action plan with achievable goals; assist patients in identifying and addressing barriers; finally, arrange follow-up with reminders to monitor progress. Assessing the amount of moderate PA per week could quickly become a standard of care in clinical practice by asking two simple questions (Sallis, 2017):
‘On average, how many days per week do you engage in moderate or greater intensity PA (like a brisk walk)?’
‘On average, how many minutes do you engage in this PA in those days?’
To achieve the minimal WHO recommendations for cardiorespiratory endurance exercise, the product of the two responses should be equal to or higher than 150 min/week (equal to or higher than 75 min/week for vigorous PA only). If the patient does not meet these recommendations, he/she should be advised to engage adequately in PA according to his/her capability. Specific recommendations according to types of chronic disease have been published by Pedersen and Saltin (2015).
Healthcare professionals’ views
Despite increasing advocacy by many organizations, initiatives or private companies [e.g. WHO, International Society for Physical Activity and Health (ISPAH), African Physical Activity Network (AFPAN), Asia Pacific Physical Activity Network (APPAN), Health Enhancing Physical Activity (HEPA) Europe Network, Exercise is Medicine®, ExerciseWorks!, etc.] to enhance PA counselling in primary healthcare, still two thirds of patients are not advised by physicians regarding PA (Barnes and Schoenborn, 2012). Many reasons are cited, including lack of time, lack of adherence and competing priorities (Leenaars et al., 2015), and lack of knowledge to provide PA advice (Din et al., 2015, Hebert et al., 2012, Lobelo et al., 2008). Healthcare professionals’ own PA experiences may present another obstacle, as those who themselves are not active may not prescribe PA, believing it to be hypocritical (Din et al., 2015). Other primary care physicians believe that patients are not interested in being coached, are not motivated, do not have time or have family commitments which can be barriers to adoption of PA (Bull et al., 1997). Whilst improvements in physical health may be the primary outcome of an intervention, there are a range of additional outcomes equally important in identifying the impact of a programme, including quality of life, mental health, social inclusion, mobility, confidence, self-image and self-esteem, and costs and consequences for both the individual and for services. Professional acceptance and widespread implementation is more likely if the intervention is accompanied by a formative evaluation, and consideration should be given to a wide range of parameters. Even if the lack of PA counselling might be considered medical ‘neglect’ (Weiler et al., 2012b), solutions to incite healthcare professionals to implement it within their practice should be encouraged, including financial incentives.
Training for healthcare professionals
Effective PA promotion in healthcare settings relies on professionals having the appropriate level of knowledge and skills to assess, counsel and support their patients. In most cases these are lacking (Dacey et al., 2014, Dunlop and Murray, 2013, Potemkina and Boytsov, 2014, Scott et al., 2017, Weiler et al., 2012a). Recent surveys undertaken by the HEPA Europe network (Ward, 2015b) and others (Dacey et al., 2014, Dunlop and Murray, 2013, Weiler et al., 2012a) have highlighted the very limited medical curriculum time that is dedicated to PA and health, so it is not surprising that doctors often do not feel sufficiently equipped to provide support or information to their patients. Tomorrow's doctors want more teaching and training on PA for health (Bull et al., 1997, Osborne et al., 2017, Scott et al., 2017). The ‘Physical activity strategy for the WHO European Region 2016–25’ encourages governments to work with healthcare providers (and their representatives) and institutions to develop and implement courses on the health benefits of PA with a special focus to the provision of advice to patients (World Health Organization, 2015b). Training in PA counselling has been developed, tested or implemented within the medical curriculum offered by institutions in the UK, USA, UAE, Bahrain, Thailand, Australia, Switzerland, and 12 Latin American countries (Arciniegas Calle et al., 2016, Dacey et al., 2014, Gates, 2015, Martin et al., 2014, Scott et al., 2016, Stoutenberg et al., 2015, Strong et al., 2017). In the Latin American countries, >4000 healthcare professionals were trained between 2011 and 2014 with a one-day ‘Exercise is Medicine®’ course (Arciniegas Calle et al., 2016). Training for healthcare professionals is also at the core of the half-day Physical Activity Promotion in Primary Care (PAPRICA) initiative in Switzerland (Martin et al., 2014) that offers doctors knowledge, skills and teaching aids to motivate their patients to move regularly. The duration of such training may be too short to fully develop the skills to prescribe PA. However, it serves to raise awareness of the importance of PA promotion. Public Health England published online a set of BMJ Learning resources to support healthcare professionals integrating PA into the prevention and treatment of NCDs (Bird, 2014). More than 3500 physicians trained at least partially within the first six months of publication (Varney and Fenton, 2015). Public Health England also worked with ExerciseWorks! to develop and evaluate a set of undergraduate teaching resources for UK medical schools to train current or future healthcare professionals (Gates, 2016, Varney and Fenton, 2015). In Australia, most medical schools include PA training in their medical curriculum (Strong et al., 2017) with the focus largely on cardiorespiratory endurance exercise recommendations. Healthcare professionals may also access, both in scientific and grey literature, general and specific recommendations concerning PA counselling and prescription (Gates, 2016, Gates et al., 2017, Pedersen and Saltin, 2015, Stoutenberg et al., 2015, Thornton, 2017, Thornton et al., 2016). A range of supporting resources are available online for healthcare professionals (and patients) in several countries, including websites with comprehensive materials such as factsheets concerning diseases and PA, for example, Australia (www.exerciseismedicine.com.au, last accessed 29 May 2018), Luxembourg (www.sport-sante.lu, last accessed 29 May 2018) and Sweden (www.fyss.se, last accessed 29 May 2018). Physicians are the primary care professionals who predominantly advise patients, but other healthcare professionals, such as physiotherapists, nurses or pharmacists, are also able to counsel patients to be more active (Buchholz and Purath, 2007, Kunstler et al., 2018, Lamarche and Vallance, 2013, Richards and Cai, 2016). However, they too are in need of training in PA-related counselling (Bakhshi et al., 2015). In France, specific academic training for connectors and adapted PA teachers is done in the faculties of sport sciences. Educating healthcare professionals could also help tackle the low PA levels of healthcare professionals themselves.
PATIENTS’ PERSPECTIVES
Whilst most patients know that PA confers health benefits, only 18% of UK adults knew the current PA guidelines in 2013 (Knox et al., 2013), and this varied according to gender, age, and disadvantaged population groups. Only one-third of patients reported they received PA counselling by their physicians (AuYoung et al., 2016, Barnes and Schoenborn, 2012), whilst other research has found limited evidence of consistent or comprehensive support (Joelsson et al., 2017, Shuval et al., 2017).
SUCCESSFUL FACTORS OF PA PROGRAMMES
After brief counselling or referral, adherence and retention can be problematic. PA should be tailored to the individuals’ health and social needs and interests, varying from personal home-based exercises to community-based activities. Involvement of other attendees and family is seen as an important facilitator of adherence, as is ‘making exercise a habit’. Barriers to attendance include limited activity options, inconvenient timing of sessions, their cost and location (Morgan et al., 2016). An intimidating gym atmosphere, dislike of the music and TV and a lack of confidence in operating gym equipment were also frequently reported. Patients should receive support beyond the end of the intervention and their needs and preferences should be considered. It is important that professionals adjust a protocol to address local circumstances, with a clearly agreed-upon and understood delivery framework. Access to a recreational centre, although important, is not sufficient on its own to increase PA. For example, regular programmes delivered in community recreational centres may not be effective for people with sedentary lifestyles and obesity (Arsenijevic and Groot, 2017).
COST MISCONCEPTIONS
The cost related to PA counselling is often claimed by decision makers as a major barrier to its development in primary care. However, evidence showing cost-effectiveness of the PA interventions is growing. To be considered cost-effective, a treatment cost should be lower than $100 000 per quality-adjusted life-year (QALY) gained (Neumann et al., 2014). Compared with usual care, the cost-utility of brief interventions promoting PA was <$19 000 per QALY gained (Vijay et al., 2016). Exercise referral schemes varied from <$16 000 to >$130 000 per QALY gained (Campbell et al., 2015, Murphy et al., 2012). This can be further enhanced if the patients contribute to the cost of the PA sessions. For example, one 16-week programme to increase PA resulted in a base-case incremental cost-effectiveness ratio of $15 578 per QALY, falling to $12 539 if participants were to contribute $2.50 per session (Murphy et al., 2012). Nevertheless, the cost paid by patients should not be too high to deter participation, especially among disadvantaged population subgroups. There is sufficient evidence of the cost-effectiveness to justify the international recommendations of significant investment (e.g. reimbursement of the PA programmes) from national health systems or health insurance companies (World Health Organization, 2015b).
POLICY DECISIONS
International bodies regularly provide recommendations and encourage governments to increase support for PA promotion. The ‘Physical activity strategy for the WHO European Region 2016–25’ recommends that PA promotion for health should be endorsed and led at the head-of-government level in collaboration with the health sector (i.e. national ministries of health) (World Health Organization, 2015b). The state governments, however, do not systematically follow the international recommendations (Bull et al., 2015), which are often even not translated in the local language. The transition to a newly elected government has the potential to change a nation’s level of support for WHO and other internationally developed policies and recommendations, as in the Netherlands where a new government decided to stop supporting an intervention aiming to increase promotion of PA in primary care (Berendsen et al., 2015). Similarly a program promoting PA in Vanuatu was stopped at an early stage due to the loss of support from the Ministry of Health (Siefken et al., 2014). In contrast, a first step was made in France with an article on PA prescription for people with long-term conditions (Article 144) in the Law No 2016-41 dated 26 January 2016 for the modernization of the French healthcare system; it will be interesting to follow the evolution of this policy.
SYNERGIZE PA PROMOTION IN PRIMARY CARE
In light of the global pandemic of inactivity, far too many people still remain sedentary despite many initiatives aimed at tackling the problem. Multiple stakeholders are investing much energy trying to promote PA with insufficient coordination. This induces duplication, resulting in wasted resources and a diluted impact. This paradigm must change into an approach based on synergy of all the relevant stakeholders (e.g. government, civil society, private sector, non-governmental organizations, sport bodies, etc.) (Ward, 2015a, World Health Organization, 2004). Synergy should be implemented at all levels of PA promotion: international, national, local, etc. Synergy within the primary care teams should be encouraged. All synergies should result in a community of practice, sharing interest or passion in promoting PA (Gates et al., 2017). By sharing knowledge and experience, problems will be solved more easily and the standards of the interventions improved. This knowledge sharing will unify the multi-professional team, promote ownership and induce sustainable practice change (Gates et al., 2017). To that end, leaders should be identified to coordinate the synergy. Strategies to promote PA within the healthcare system should build on the lessons learned from other large scale health promotion initiatives including tobacco control or immunization programmes (Bull and Bauman, 2011, Henderson, 1998). These programmes include implementation within existing health service structures, involvement of the community, encouragement of research initiatives and strong public communication elements (Bull and Bauman, 2011). The most popular media and interactive workshops could be targeted to promote PA (Lion et al., 2017). Nevertheless, these actions alone are insufficient for population change, and require contributions from other sectors (Bull and Bauman, 2011).
CONCLUSION
Healthcare professionals, especially primary care practitioners, see large numbers of patients during their careers. This has enormous potential for advocating participation in regular PA. Therefore, scaled-up interventions to promote PA within primary healthcare to tackle NCDs are increasing worldwide. However, these interventions are still facing the classical barriers: education of healthcare professionals and patients, financial support and community engagement. An integrated approach, addressing these barriers should be supported, promoted and implemented by national and local governments in synergy with key strategic stakeholders.
Only through the concerted action of healthcare professions and relevant stakeholders can we hope to overcome one of the greatest threats, not just to the enduring health of each nation’s population, but to the sustainability of our combined medical systems.
ACKNOWLEDGEMENTS
Dr A.L., Prof. A.V. and Mr M.W. are the representatives of their respective institutions within the HEPA Europe (European network for the promotion of health-enhancing PA) which works for ‘Better health and wellbeing in the WHO European region through more physical activity for all people’. All authors are grateful to the members of the HEPA Europe working group ‘HEPA promotion in health care settings’ led by Mr M.W. and Ms Eszter Füzéki. This working group aims to promote healthcare related HEPA activities across the WHO European Region. Main activities include identifying common concerns, sharing information on development and research, promoting good practice, informing policy and strategy and advocating for evidence-based interventions.
The opinions and the data communicated in this article are those from the authors and do not necessarily reflect the views of the HEPA Europe network.
FUNDING
This contribution is part of the Sport-Santé project which has received financial support from the Œvre Nationale de Secours Grande–Duchesse Charlotte and the ministère de l'Enseignement supérieur et de la Recherche.
REFERENCES
- Arciniegas Calle M. C., Lobelo F., Jimenez M. A., Paez D. C., Cortes S., de Lima A.. et al. , (2016) One-day workshop-based training improves physical activity prescription knowledge in Latin American physicians: a pre-test post-test study. BMC Public Health 16, 1224.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arsenijevic J., Groot W. (2017) Physical activity on prescription schemes (PARS): do programme characteristics influence effectiveness? Results of a systematic review and meta-analyses. BMJ Open 7, e012156.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- AuYoung M., Linke S. E., Pagoto S., Buman M. P., Craft L. L., Richardson C. R.. et al. , (2016) Integrating physical activity in primary care practice. American Journal of Medicine 129, 1022–1029. [DOI] [PubMed] [Google Scholar]
- Bakhshi S., Sun F., Murrells T., While A. (2015) Nurses' health behaviours and physical activity-related health-promotion practices. British Journal of Community Nursing 20, 289–296. [DOI] [PubMed] [Google Scholar]
- Barnes P. M., Schoenborn C. A. (2012) Trends in adults receiving a recommendation for exercise or other physical activity from a physician or other health professional. NCHS Data Brief 2012, 1–8. [PubMed] [Google Scholar]
- Berendsen B. A., Kremers S. P., Savelberg H. H., Schaper N. C., Hendriks M. R. (2015) The implementation and sustainability of a combined lifestyle intervention in primary care: mixed method process evaluation. BMC Family Practice 16, 37.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berra K., Rippe J., Manson J. E. (2015) Making physical activity counseling a priority in clinical practice: the time for action is now. JAMA 314, 2617–2618. [DOI] [PubMed] [Google Scholar]
- Bird W. (2014) Physical Activity in the Treatment of Long Term Conditions. http://learning.bmj.com/learning/course-intro/physical-activity.html?courseId=10051913 (last accessed 21 November 2017).
- Buchholz S. W., Purath J. (2007) Physical activity and physical fitness counseling patterns of adult nurse practitioners. Journal of the American Association of Nurse Practitioners 19, 86–92. [DOI] [PubMed] [Google Scholar]
- Bull F., Milton K., Kahlmeier S., Arlotti A., Jurican A. B., Belander O.. et al. , (2015) Turning the tide: national policy approaches to increasing physical activity in seven European countries. British Journal of Sports Medicine 49, 749–756. [DOI] [PubMed] [Google Scholar]
- Bull F. C., Bauman A. E. (2011) Physical inactivity: the “Cinderella” risk factor for noncommunicable disease prevention. Journal of Health Communication 16, 13–26. [DOI] [PubMed] [Google Scholar]
- Bull F. C., Schipper E. C., Jamrozik K., Blanksby B. A. (1997) How can and do Australian doctors promote physical activity? Preventive Medicine 26, 866–873. [DOI] [PubMed] [Google Scholar]
- Campbell F., Blank L., Messina J., Day M., Buckley Woods H., Payne N., Goyder E., Armitage C. (2012) Physical Activity: Brief Advice for Adults in Primary Care (National Institute for Health and Clinical Excellence Public Health Intervention Guidance). NICE Centre for Public Health Excellence, Sheffield. [Google Scholar]
- Campbell F., Holmes M., Everson-Hock E., Davis S., Buckley Woods H., Anokye N.. et al. , (2015) A systematic review and economic evaluation of exercise referral schemes in primary care: a short report. Health Technology Assessment 19, 1–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dacey M. L., Kennedy M. A., Polak R., Phillips E. M. (2014) Physical activity counseling in medical school education: a systematic review. Medical Education Online 19, 24325.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das P., Horton R. (2016) Physical activity-time to take it seriously and regularly. Lancet 388, 1254–1255. [DOI] [PubMed] [Google Scholar]
- Din N. U., Moore G. F., Murphy S., Wilkinson C., Williams N. H. (2015) Health professionals' perspectives on exercise referral and physical activity promotion in primary care: findings from a process evaluation of the National Exercise Referral Scheme in Wales. Health Education Journal 74, 743–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding D., Lawson K. D., Kolbe-Alexander T. L., Finkelstein E. A., Katzmarzyk P. T., van Mechelen W.. et al. and Lancet Physical Activity Series 2 Executive Committee, (2016) The economic burden of physical inactivity: a global analysis of major non-communicable diseases. Lancet 388, 1311–1324. [DOI] [PubMed] [Google Scholar]
- Dunlop M., Murray A. D. (2013) Major limitations in knowledge of physical activity guidelines among UK medical students revealed: implications for the undergraduate medical curriculum. British Journal of Sports Medicine 47, 718–720. [DOI] [PubMed] [Google Scholar]
- Elley C. R., Kerse N., Arroll B., Robinson E. (2003) Effectiveness of counselling patients on physical activity in general practice: cluster randomised controlled trial. BMJ 326, 793.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estabrooks P. A., Glasgow R. E., Dzewaltowski D. A. (2003) Physical activity promotion through primary care. JAMA 289, 2913–2916. [DOI] [PubMed] [Google Scholar]
- Gallegos-Carrillo K., Garcia-Pena C., Salmeron J., Salgado-de-Snyder N., Lobelo F. (2017) Brief counseling and exercise referral scheme: a pragmatic trial in Mexico. American Journal of Preventive Medicine 52, 249–259. [DOI] [PubMed] [Google Scholar]
- Gates A. B. (2015) Training tomorrow's doctors, in exercise medicine, for tomorrow's patients. British Journal of Sports Medicine 49, 207–208. [DOI] [PubMed] [Google Scholar]
- Gates A. B. (2016) Making every contact count for physical activity–for tomorrow's patients: the launch of the interdisciplinary, undergraduate, resources on exercise medicine and health in the U.K. British Journal of Sports Medicine 50, 322–323. [DOI] [PubMed] [Google Scholar]
- Gates A. B., Kerry R., Moffatt F., Ritchie I. K., Meakins A., Thornton J. S.. et al. , (2017) Movement for movement: exercise as everybody's business? British Journal of Sports Medicine 51, 767–768. [DOI] [PubMed] [Google Scholar]
- Global Advocacy for Physical Activity the Advocacy Council of the International Society for Physical and Health. (2012) NCD prevention: investments [corrected] that work for physical activity. British Journal of Sports Medicine 46, 709–712. [DOI] [PubMed] [Google Scholar]
- Heath G. W., Parra D. C., Sarmiento O. L., Andersen L. B., Owen N., Goenka S., Lancet Physical Activity Series Working, G. et al. , (2012) Evidence-based intervention in physical activity: lessons from around the world. Lancet 380, 272–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hebert E. T., Caughy M. O., Shuval K. (2012) Primary care providers' perceptions of physical activity counselling in a clinical setting: a systematic review. British Journal of Sports Medicine 46, 625–631. [DOI] [PubMed] [Google Scholar]
- Helmink J. H., Kremers S. P., van Boekel L. C., van Brussel-Visser F. N., de Vries N. K. (2012) Factors determining the motivation of primary health care professionals to implement and continue the ‘Beweegkuur’ lifestyle intervention programme. Journal of Evaluation in Clinical Practice 18, 682–688. [DOI] [PubMed] [Google Scholar]
- Henderson D. A. (1998) Eradication: lessons from the past. Bulletin of the World Health Organization 76(Suppl. 2), 17–21. [PMC free article] [PubMed] [Google Scholar]
- Hillsdon M., Foster C., Thorogood M. (2005) Interventions for promoting physical activity. Cochrane Database of Systematic Reviews 1, CD003180 [DOI] [PMC free article] [PubMed]
- Hoffmann T. C., Maher C. G., Briffa T., Sherrington C., Bennell K., Alison J.. et al. , (2016) Prescribing exercise interventions for patients with chronic conditions. Canadian Medical Association Journal 188, 510–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joelsson M., Bernhardsson S., Larsson M. E. (2017) Patients with chronic pain may need extra support when prescribed physical activity in primary care: a qualitative study. Scandinavian Journal of Primary Health Care 35, 64–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahlmeier S., Popp C., Martin B. W., Backovic-Jurican A., Banzer W., Berggren F.. et al. , (2014) A systematic overview of institutions and bodies active in physical activity promotion in Europe. Swiss Sports & Exercise Medicine 62, 13–18. [Google Scholar]
- Kallings L. (2011) Physical Activity on Prescription in the Nordic Region: Experiences and Recommendations. Helsedirekektoratet, Uppsala. [Google Scholar]
- Khan K. M., Weiler R., Blair S. N. (2011) Prescribing exercise in primary care. BMJ 343, d4141.. [DOI] [PubMed] [Google Scholar]
- Knox E. C., Esliger D. W., Biddle S. J., Sherar L. B. (2013) Lack of knowledge of physical activity guidelines: can physical activity promotion campaigns do better? BMJ Open 3, e003633.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunstler B. E., Cook J. L., Freene N., Finch C. F., Kemp J. L., O'Halloran P. D.. et al. (2018) Physiotherapist-led physical activity interventions are efficacious at increasing physical activity levels: a systematic review and meta-analysis. Clinical Journal of Sport Medicine 28, 304–315. [DOI] [PubMed] [Google Scholar]
- Lamarche K., Vallance J. (2013) Prescription for physical activity a survey of Canadian nurse practitioners. Canadian Nurse 109, 22–26. [PubMed] [Google Scholar]
- Lamming L., Pears S., Mason D., Morton K., Bijker M., Sutton S.. et al. , (2017) What do we know about brief interventions for physical activity that could be delivered in primary care consultations? A systematic review of reviews. Preventive Medicine 99, 152–163. [DOI] [PubMed] [Google Scholar]
- Lee I. M., Shiroma E. J., Lobelo F., Puska P., Blair S. N., Katzmarzyk P. T.Lancet Physical Activity Series Working, Group. (2012) Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet 380, 219–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leenaars K. E., Florisson A. M., Smit E., Wagemakers A., Molleman G. R., Koelen M. A. (2016a) The connection between the primary care and the physical activity sector: professionals' perceptions. BMC Public Health 16, 1001.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leenaars K. E., Smit E., Wagemakers A., Molleman G. R., Koelen M. A. (2015) Facilitators and barriers in the collaboration between the primary care and the sport sector in order to promote physical activity: a systematic literature review. Preventive Medicine 81, 460–478. [DOI] [PubMed] [Google Scholar]
- Leenaars K. E., Smit E., Wagemakers A., Molleman G. R, Koelen M. A. (2016b) The role of the care sport connector in the Netherlands. Health Promotion International, December 23, 2016, doi: 10.1093/heapro/daw097. [DOI] [PubMed]
- Lion A., Thornton J. S., Vaillant M., Pertuy J., Besenius E., Hardy C.. et al. , (2017) Effect of promotional initiatives on visits to a dedicated website for physical activity and non-communicable disease in Luxembourg: an event study. Frontiers in Public Health 5, 114.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lobelo F., Duperly J., Frank E. (2008) Physical activity habits of doctors and medical students influence their counselling practices. British Journal of Sports Medicine 43, 89–92. [DOI] [PubMed] [Google Scholar]
- Martin B. W., Padlina O., Martin-Diener E., Bize R., Cornuz J., Kahlmeier S. (2014) Physical activity promotion in the health care setting in Switzerland. Swiss Sports & Exercise Medicine 62, 19–22. [Google Scholar]
- McNally S. (2015) Exercise: The Miracle Cure and the Role of the Doctor in Promoting It. Academy of Medical Royal Colleges, London. [Google Scholar]
- Morgan F., Battersby A., Weightman A. L., Searchfield L., Turley R., Morgan H.. et al. , (2016) Adherence to exercise referral schemes by participants – what do providers and commissioners need to know? A systematic review of barriers and facilitators. BMC Public Health 16, 227.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy S. M., Edwards R. T., Williams N., Raisanen L., Moore G., Linck P.. et al. , (2012) An evaluation of the effectiveness and cost effectiveness of the National Exercise Referral Scheme in Wales, UK: a randomised controlled trial of a public health policy initiative. Journal of Epidemiology and Community Health 66, 745–753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence (2013) Physical Activity: Brief Advice for Adults in Primary Care: NICE Public Health Guidance 44. National Institute for Health and Care Excellence, London. [Google Scholar]
- National Institute for Health and Care Excellence (2014) Exercise Referral Schemes to Promote Physical Activity - NICE Public Health Guidance 54. National Institute for Health and Care Excellence, London. [Google Scholar]
- Neumann P. J., Cohen J. T., Weinstein M. C. (2014) Updating cost-effectiveness – the curious resilience of the $50, 000-per-QALY threshold. New England Journal of Medicine 371, 796–797. [DOI] [PubMed] [Google Scholar]
- Orrow G., Kinmonth A. L., Sanderson S., Sutton S. (2012) Effectiveness of physical activity promotion based in primary care: systematic review and meta-analysis of randomised controlled trials. BMJ 344, e1389.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osborne S. A., Adams J. M., Fawkner S., Kelly P., Murray A. D., Oliver C. W. (2017) Tomorrow's doctors want more teaching and training on physical activity for health. British Journal of Sports Medicine 51, 624–625. [DOI] [PubMed] [Google Scholar]
- Pakravan A, Jones A. (2014) Exercise Referral Schemes in Primary Care: Where does Sport and Exercise Medicine stand? BJSM Blog. http://blogs.bmj.com/bjsm/2014/03/16/exercise-referral-schemes-in-primary-care-where-does-sport-and-exercise-medicine-stand/ (last accessed 29 May 2018).
- Pate R. R., Heath G. W., Dowda M., Trost S. G. (1996) Associations between physical activity and other health behaviors in a representative sample of US adolescents. American Journal of Public Health 86, 1577–1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pavey T. G., Taylor A. H., Fox K. R., Hillsdon M., Anokye N., Campbell J. L.. et al. , (2011) Effect of exercise referral schemes in primary care on physical activity and improving health outcomes: systematic review and meta-analysis. BMJ 343, d6462.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pears S., Bijker M., Morton K., Vasconcelos J., Parker R. A., Westgate K.. et al. , (2016) A randomised controlled trial of three very brief interventions for physical activity in primary care. BMC Public Health 16, 1033.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pears S., Morton K., Bijker M., Sutton S., Hardeman W., Team V. B. I. P. (2015) Development and feasibility study of very brief interventions for physical activity in primary care. BMC Public Health 15, 333.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen B. K., Saltin B. (2015) Exercise as medicine – evidence for prescribing exercise as therapy in 26 different chronic diseases. Scandinavian Journal of Medicine & Science in Sports 25(Suppl. 3), 1–72. [DOI] [PubMed] [Google Scholar]
- Potemkina R., Boytsov S. (2014) Exercise in medicine in Russia. Swiss Sports & Exercise Medicine 62, 35–37. [Google Scholar]
- Richards E. A., Cai Y. (2016) Integrative review of nurse-delivered physical activity interventions in primary care. Western Journal of Nursing Research 38, 484–507. [DOI] [PubMed] [Google Scholar]
- Rutten G. M., Meis J. J., Hendriks M. R., Hamers F. J., Veenhof C., Kremers S. P. (2014) The contribution of lifestyle coaching of overweight patients in primary care to more autonomous motivation for physical activity and healthy dietary behaviour: results of a longitudinal study. International Journal of Behavioral Nutrition and Physical Activity 11, 86.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallis J. F., Bull F., Guthold R., Heath G. W., Inoue S., Kelly P. Lancet Physical Activity Series 2 Executive, C. et al. , (2016) Progress in physical activity over the Olympic quadrennium. Lancet 388, 1325–1336. [DOI] [PubMed] [Google Scholar]
- Sallis R. E. (2017) Exercise in the treatment of chronic disease: an underfilled prescription. Current Sports Medicine Reports 16, 225–226. [DOI] [PubMed] [Google Scholar]
- Sanchez A., Bully P., Martinez C., Grandes G. (2015) Effectiveness of physical activity promotion interventions in primary care: a review of reviews. Preventive Medicine 76, S56–S67. [DOI] [PubMed] [Google Scholar]
- Schutte B. A., Haveman-Nies A., Preller L. (2015) One-year results of the BeweegKuur lifestyle intervention implemented in Dutch primary healthcare settings. BioMed Research International 2015, 1.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott H., Adams J., Osborne S., Jenkins E., Oliver C. W., Baker G.. et al. , (2017) Infographic: tomorrow's doctors want to learn more about physical activity for health. British Journal of Sports Medicine 51, 624.1–625. [DOI] [PubMed] [Google Scholar]
- Scott H., Fawkner S., Oliver C., Murray A. (2016) Why healthcare professionals should know a little about infographics. British Journal of Sports Medicine 50, 1104–1105. [DOI] [PubMed] [Google Scholar]
- Shuval K., Leonard T., Drope J., Katz D. L., Patel A. V., Maitin-Shepard M.. et al. , (2017) Physical activity counseling in primary care: insights from public health and behavioral economics. CA: Cancer Journal for Clinicians 67, 233–244. [DOI] [PubMed] [Google Scholar]
- Siefken K., Schofield G., Schulenkorf N. (2014) Inspiring Pacific women to realise sustainable lifestyle changes: an attempt to halt the spread of chronic diseases. In Schulenkorf N., Adair D. (eds), Global Sport-for-Development: Critical Perspectives, 1st edition, Chapter 12. London: Palgrave Macmillan, pp. 216–242. [Google Scholar]
- Stoutenberg M., Stasi S., Stamatakis E., Danek D., Dufour T., Trilk J. L.. et al. , (2015) Physical activity training in US medical schools: preparing future physicians to engage in primary prevention. Physician and Sports Medicine 43, 388–394. [DOI] [PubMed] [Google Scholar]
- Stranges S., Dorn J. M., Shipley M. J., Kandala N. B., Trevisan M., Miller M. A.. et al. , (2008) Correlates of short and long sleep duration: a cross-cultural comparison between the United Kingdom and the United States: the Whitehall II Study and the Western New York Health Study. American Journal of Epidemiology 168, 1353–1364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stranges S., Samaraweera P. C., Taggart F., Kandala N. B., Stewart-Brown S. (2014) Major health-related behaviours and mental well-being in the general population: the Health Survey for England. BMJ Open 4, e005878.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strong A., Stoutenberg M., Hobson-Powell A., Hargreaves M., Beeler H., Stamatakis E. (2017) An evaluation of physical activity training in Australian medical school curricula. Journal of Science and Medicine in Sport 20, 534–538. [DOI] [PubMed] [Google Scholar]
- Thornton J. S. (2017) Physical activity prescription and engaging the entire ‘community of practice’. British Journal of Sports Medicine, February 17, 2017, doi: 10.1136/bjsports-2016-097191. [DOI] [PubMed]
- Thornton J. S., Fremont P., Khan K., Poirier P., Fowles J., Wells G. D.. et al. , (2016) Physical activity prescription: a critical opportunity to address a modifiable risk factor for the prevention and management of chronic disease: a position statement by the Canadian Academy of Sport and Exercise Medicine. British Journal of Sports Medicine 50, 1109–1114. [DOI] [PubMed] [Google Scholar]
- Varney J, Fenton K. (2015) Moving Healthcare Professionals at Every Level. Public Health Matters. https://publichealthmatters.blog.gov.uk/2015/10/19/moving-healthcare-professionals-at-every-level-2/ (last accessed 21 November 2017).
- Vijay G. C., Wilson E. C., Suhrcke M., Hardeman W., Sutton S. V. B. I. Programme Team. (2016) Are brief interventions to increase physical activity cost-effective? A systematic review. British Journal of Sports Medicine 50, 408–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward M. (2015a) C=EM2: Yes, Physical Activity Promotion Really is Rocket Science, 6th HEPA Europe Conference, Istanbul, Turkey.
- Ward M. (2015b) A Survey of Physical Activity in Medical Curricula: A report of the HEPA in Health Care Settings HEPA Europe Working Group. HEPA Europe.
- Weiler R., Chew S., Coombs N., Hamer M., Stamatakis E. (2012a) Physical activity education in the undergraduate curricula of all UK medical schools: are tomorrow's doctors equipped to follow clinical guidelines? British Journal of Sports Medicine 46, 1024–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiler R., Feldschreiber P., Stamatakis E. (2012b) Medicolegal neglect? The case for physical activity promotion and exercise medicine. British Journal of Sports Medicine 46, 228–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams N. H. (2011) Promoting physical activity in primary care. BMJ 343, d6615.. [DOI] [PubMed] [Google Scholar]
- Williams N. H., Hendry M., France B., Lewis R., Wilkinson C. (2007) Effectiveness of exercise-referral schemes to promote physical activity in adults: systematic review. British Journal of General Practice 57, 979–986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2004) Global Strategy on Diet, Physical Activity and Health. World Health Organization, Geneva. [Google Scholar]
- World Health Organization (2013) Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020. World Health Organization, Geneva. [Google Scholar]
- World Health Organization (2015a) Factsheets on Health-Enhancing Physical Activity in the 28 European Union Member States of the WHO European Region. WHO Regional Office for Europe, Copenhagen.
- World Health Organization (2015b) Physical activity strategy for the WHO European Region 2016–2025. WHO Regional Office for Europe, Copenhagen.