Abstract
The private healthcare sector in low- and middle-income countries is increasingly seen as of public health importance, with widespread interest in improving private provider engagement. However, there is relatively little literature providing an in-depth understanding of the operation of private providers. We conducted a mixed methods analysis of the nature of competition faced by private delivery providers in Uttar Pradesh, India, where maternal mortality remains very high. We mapped health facilities in five contrasting districts, surveyed private facilities providing deliveries and conducted in-depth interviews with facility staff, allied providers (e.g. ambulance drivers, pathology laboratories) and other key informants. Over 3800 private facilities were mapped, of which 8% reported providing deliveries, mostly clustered in cities and larger towns. 89% of delivery facilities provided C-sections, but over half were not registered. Facilities were generally small, and the majority were independently owned, mostly by medical doctors and, to a lesser extent, AYUSH (non-biomedical) providers and others without formal qualifications. Recent growth in facility numbers had led to intense competition, particularly among mid-level facilities where customers were more price sensitive. In all facilities, nearly all payment was out-of-pocket, with very low-insurance coverage. Non-price competition was a key feature of the market and included location (preferably on highways or close to government facilities), medical infrastructure, hotel features, staff qualifications and reputation, and marketing. There was heavy reliance on visiting consultants such as obstetricians, surgeons and anaesthetists, and payment of hefty commission payments to agents who brought clients to the facility, for both new patients and those transferring from public facilities. Building on these insights, strategies for private sector engagement could include a foundation of universal facility registration, adaptation of accreditation schemes to lower-level facilities, improved third-party payment mechanisms and strategic purchasing, and enhanced patient information on facility availability, costs and quality.
Keywords: Private sector, private providers, delivery care, maternal health, economics, competition, India, Uttar Pradesh, public–private engagement
Introduction
In low- and middle-income countries (LMICs) the public health importance of the private healthcare sector is increasingly noted, given its current role in provision, and potential role in Universal Health Coverage (Mcpake and Hanson, 2016). Though there is considerable cross-country heterogeneity, the private sector often accounts for over 25% of curative care and sometimes over 50% (Mackintosh et al., 2016), and on average 40% of maternal healthcare (Campbell et al., 2016a). There is widespread interest in improving strategies for private provider engagement, e.g. through enhanced regulation, government purchasing, quality improvement networks or social accountability (Montagu et al., 2016), and a gradually growing literature documenting private sector market share, clientele and quality, and evaluating private sector interventions (Montagu and Goodman, 2016; Morgan et al., 2016). However, there is relatively little in-depth assessment of the operation of LMIC private providers, the incentives they face and the competitive strategies they employ (Bautista, 1995; Bennett, 1996; Kamat and Nichter, 1998; Nakamba et al., 2002; Goodman, 2004; Jeffery and Jeffery, 2008; George and Iyer, 2013; Gautham et al., 2014; Tsevelvaanchig et al., 2017). An enhanced understanding of the nature of competition in these markets can assist policy and programme decision-makers in anticipating the challenges associated with private sector functioning and in designing strategies for engaging with private providers that are appropriate and incentive-compatible.
In this article, we focus on private provision of delivery care. A key strategy to reduce maternal mortality has been increased skilled birth attendance, primarily through delivery at health facilities (Campbell et al., 2006). However, facility deliveries do not improve outcomes if quality of care is poor, so it is essential that maternity facilities have the required infrastructure, skilled staff, and emergency obstetric capacity and/or functioning referral mechanisms (Goldenberg and Mcclure, 2017). In practice, there are major concerns about the quality of delivery care in both public and private facilities (Sharma et al., 2015; Campbell et al., 2016b).
The private sector dominates healthcare delivery in India (Mackintosh et al., 2016), and while private facility use is lower for delivery than for curative care, it is still substantial and increasing. The percentage of deliveries occurring in facilities increased from 39% to 79% between 2005–06 and 2015–16 (Indian Institute for Population Studies, 2016). Much of this increase reflects increased public facility use, attributed to the Janani Suraksha Yojana (JSY) financial incentive scheme for community health workers (termed ASHAs) and women (Lim et al., 2010), together with free public ambulance services (Babiarz et al., 2016). However, private sector deliveries also increased, now accounting for over a quarter of births (20.7% in rural and 42.5% in urban India) (Indian Institute for Population Studies, 2016). Several studies have documented the availability and structural quality of private emergency obstetric services in India (Mony et al., 2013; Jayanna et al., 2014; Sabde et al., 2014; Salazar et al., 2016), but no studies were identified on the competitive environment and strategies of these providers.
This study aims to address this gap, by providing an analysis of the nature of competition faced by private delivery providers in Uttar Pradesh, particularly exploring the roles of price and non-price competition, and the implications for accessibility and quality. We draw on both quantitative and qualitative methods, in order to combine a detailed description of the market structure and provider characteristics with in-depth analysis of competitive strategies and exploration of commercially and legally sensitive topics.
Methods
Study setting
With a population of over 220 million, Uttar Pradesh is India’s most populous state (Government of Uttar Pradesh, 2015), with 29% of the population below the poverty line compared with the all India average of 22% (Government of India, 2011–12). Although predominantly rural (77%), eight of its cities contain over 1 million people (Government of India, 2011). Delivery outcomes are poor, with a maternal mortality rate of 201 per 100 000 births compared with the Indian average of 130 (Government of India, 2018), and an infant mortality rate of 64 per 1000 compared with the Indian average of 41 (Indian Institute for Population Studies, 2016).
We selected three contrasting study sites, providing variation in socio-economic status, proximity to large cities and religious orientation: (1) two zones of Kanpur City (KC) (which comprises the major portion of Kanpur Nagar district), one a relatively high-income zone and one lower income; (2) the contiguous mostly rural districts of Kannauj and Kanpur Dehat (KKD); and (3) the contiguous districts of Bareilly and Rampur (BR), which have a relatively large Muslim population. In 2012, use of private facilities for delivery ranged from 10% of births in Kanpur Dehat, to 15% in Kannauj, 23% in Bareilly and 27% in both Kanpur City and Rampur (Government of India, 2014), and has likely risen further since.
Public delivery facilities include Primary Health Centres which should perform normal deliveries, Community Health Centres which should perform C-sections (though in practice <20% may have this capacity (International Institute for Population Sciences, 2010), and district or higher level hospitals which should provide comprehensive emergency obstetric care. Private providers include allopathic (western medical) practitioners, and practitioners of alternative medicine systems collectively termed AYUSH (Ayurveda, Unani, Siddha, Homeopathy), who often also practice allopathic medicine. Unqualified and non-degree providers, termed Rural Medical Practitioners (RMPs) or ‘informal providers’ are also common outpatient providers, and some have small inpatient facilities (George and Iyer, 2013; Gautham et al., 2014).
Conceptualizing competition
Markets vary from the most competitive (with many sellers of similar products sold at a common price with minimal profits), to the other extreme of few sellers with considerable discretion over price. Most healthcare markets fall somewhere between these extremes in the realm of imperfect or monopolistic competition, which takes place between a substantial number of providers whose services are good but not perfect substitutes for each other (Dranove and Satterthwaite, 2000). However, there is considerable variation in the nature and intensity of competition within such healthcare markets, depending e.g. on the price sensitivity of consumers, their ability to observe quality, the degree of product differentiation/market segmentation, barriers to entering the market, and local levels of market concentration (Clarke, 1985; Scherer and Ross, 1990; Jacobs, 1997). These market characteristics affect the way providers compete, both in terms of price and non-price factors, and these variations in competition in turn can have substantial implications for the performance of such markets in terms of accessibility and quality of care. We use this competition ‘lens’ to understand the market for delivery care, investigating (1) the market structure in terms of the number and types of facilities and their characteristics, (2) the intensity and nature of price competition and (3) non-price competition strategies such as product differentiation and promotion.
Data collection and analysis
We followed a sequential and explanatory mixed methods design (Creswell et al., 2003), starting with a quantitative phase followed by a qualitative phase with some overlap between the two phases. The quantitative phase was designed to obtain the broad characteristics of the market and private facilities and provide a sampling frame that would allow us to purposively sample private facilities for the in-depth interviews (IDIs) in the qualitative phase. The qualitative phase was designed to explore the competitive strategies and business practices in the delivery care market. Data analysis followed an iterative process with, e.g. the market segmentation themes suggested in the qualitative interviews used for categorizing the facilities in the survey dataset. Qualitative data were also used to triangulate with quantitative data on pricing, staff and referrals, besides providing an in-depth understanding of private provider conduct.
Quantitative phase
A key challenge was the lack of a complete sampling frame of private facilities, due to incomplete government registration. We therefore began by systematically mapping all public and private facilities in our study sites, recording whether they appeared to provide deliveries. We defined ‘facilities’ as providers of clinical services operating from a fixed location, including public, for-profit and charitable/trust entities, and all systems of medicine. The mapping was conducted in February to April 2016, by walking or driving down every street and alley, verifying the location of facilities listed on government registers and the internet and identifying others. In Kanpur City, the mapping was conducted throughout the two selected zones; in the other sites, we mapped the district and block towns only, as the vast majority of facilities were reported to be in these peri-urban centres.
We used the mapping data to identify all private facilities conducting deliveries, and conducted a survey of all of these in March to May 2016. We visited all 410 recorded as providing deliveries during the mapping and completed surveys for 262. Of the 148 not interviewed, 7 were not found or vacant, 1 was involved in data collection for another study and 27 refused. A much higher number (113) were deemed ineligible because they said they did not provide deliveries. When contacted by senior research staff, most said they provided maternal healthcare but did not conduct deliveries on site. However, it is likely that a few denied providing deliveries to avoid our survey, or because they were concerned about regulatory violations. The true refusal rate may therefore be higher than the 9.3% of facilities reporting providing delivery care.
The private facility survey covered facility characteristics, infrastructure, type of staff, services provided, availability of equipment and medicines, cases seen, referral practices, links with allied service providers, participation in programmes/associations, and prices charged for delivery. Where possible the clinician in charge of delivery services (often the owner or medical superintendent) was interviewed. Where this person was very busy, some sections of the questionnaire (on infrastructure and business practices) were answered by a manager, but we made every effort to ask the questions related to clinical care of a staff member responsible for deliveries. The survey was piloted on facilities outside the study sites. Analysis was conducted in Stata 14.0. As we aimed to include all delivery facilities, rather than taking a sample, confidence intervals are not presented.
Qualitative phase
From April to October 2016, semi-structured IDIs were conducted with:
Private delivery facility owners/managers (n = 34), purposively selected from the surveyed facilities to provide variation in terms of number of beds and deliveries, staffing, whether they performed C-sections, rural/urban location, owner’s religion, private-for-profit v. charitable status, time in operation and prices charged for deliveries. We aimed to interview the person most involved with the management of the maternal health services business.
Allied providers who interacted with private delivery facilities (n = 46), such as ambulance drivers/owners, visiting consultants, staff from medical stores, diagnostic centres and blood banks, smaller-scale rural private clinics, ASHAs and Dais (traditional birth attendants). These were identified through suggestions provided by facility staff during the survey and IDIs, visiting local diagnostic centres and medical stores, and snowballing from allied providers interviewed.
Stakeholders at the State and District/Ward level (n = 12), from Government health services, professional associations and NGOs who were engaged with private sector policies and programmes.
IDIs were conducted in Hindi or English by senior team members, lasting 1 to 3 h. Considering the legal and commercial sensitivity of the information, we took care to reassure respondents about maintaining confidentiality, and for some questions, asked about their perceptions of other providers’ behaviours rather their own. Audio recordings were permitted for 18 IDIs and 7 stakeholder interviews, with detailed notes taken for the others. The note-takers translated the Hindi transcripts and detailed notes into English; these were reviewed by two senior research team members to ensure translation accuracy. Data were analysed using the framework approach (Ritchie et al., 2013). Translated transcripts and detailed notes were read by two team members to develop a coding structure reflecting both the literature on competition (deductive approach) and issues arising from the data (inductive approach). Data were coded using NVivo, and commonly occurring themes and sub-themes were identified.
Ethical approval was obtained from the Institutional Review Boards of LSHTM and Centre for Media Studies (CMS-IRB), New Delhi. Informed oral consent was obtained from all interviewees.
Results
Market structure
In total 3976 healthcare facilities were mapped, of which 96% were private-for-profit, 1% not-for-profit and 3% public (Supplementary Table S1). Most private facilities were outpatient clinics run by doctors or AYUSH practitioners. Only around 9% of all facilities provided deliveries (n = 368), of which 80% were private-for-profit, 1% private not-for-profit and 19% government.
We developed a typology of private delivery facilities, based primarily on the IDIs. The respondents had various ways of grouping facilities, but the most prominent was by sophistication of delivery services:
They (facilities) can be divided into small with only normal deliveries, second which do normal and C sections…nursing homes which can take some complicated cases, and bigger hospitals which provide specialized care to complicated cases (High-level facility 3, KC).
We thus grouped private facilities into three broad categories: high-level facilities with intensive care units (ICU); mid-level facilities which conducted C-sections but had no ICU; and low-level facilities which only conducted normal deliveries. This categorization is not perfect as the standard of intensive care varies widely and some facilities may fear admitting to performing C-sections. However, the typology was useful for understanding the commonalities and heterogeneity within the market. It also corresponded with reported socio-economic status of clientele, with high-level facilities said to serve the wealthy upper and upper-middle class (described by one high-level facility respondent as the ‘stinking rich’), mid-level facilities serving middle-income clients (described as those with an income of INR 15 000-20 000/USD 233-310 per month), and low-level facilities serving the lower-middle classes. While a couple of low-level private facilities were staffed by Dais, in general they were said to conduct very few deliveries these days, reflecting the role of JSY in encouraging poorer women to use public facilities. JSY and free government ambulances were also said to have attracted many patients away from other low- and mid-level facilities, but not to have affected demand for high-level facilities.
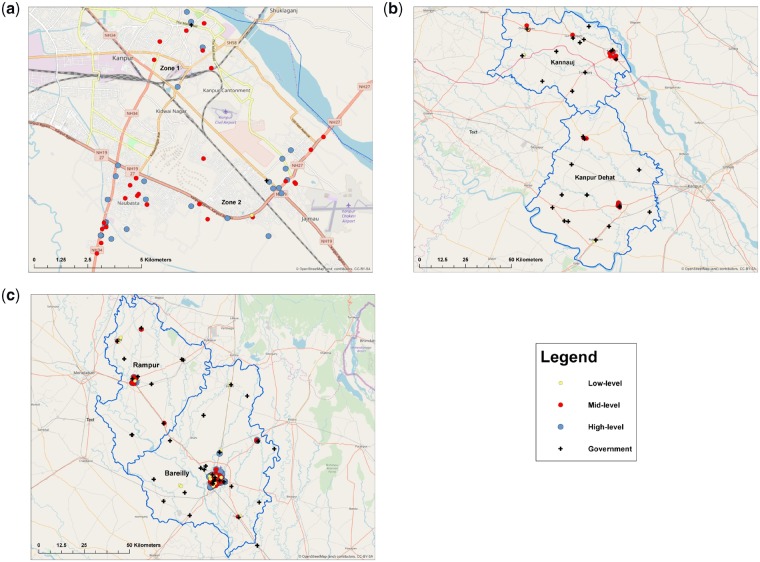
Figure 1a–c shows the location of private delivery facilities by category (and also government facilities) in each study site. Private facilities were heavily concentrated in the urban areas of Kanpur city, Bareilly city and Rampur town, where they massively out-numbered government facilities (e.g. 65:2 in the Kanpur city Zones). Outside these major urban areas, private and government delivery facilities were more similar in number (e.g. 1.5:1 in Kannauj and Kanpur Dehat). Most private facilities were mid-level (43%) or high level (46%), meaning that 89% provided C-sections. Only 11% were low level, mainly located in Kannauj, Bareilly and Rampur.
Figure 1.
(a) Kanpur City Zones 1 and 2 (n = 1 low-level, 26 mid-level, 27 high level, 2 government). (b) Kanauj and Kanpur Dehat districts (n = 6 low-level, 17 mid-level, 3 high-level, 31 government). (c) Bareilly and Rampur districts (n = 22 low-level, 70 mid-level, 90 high-level, 38 government).
There was evidence of substantial recent entry in to the market: while almost half the private facilities had been in operation for over a decade (Table 1), around a fifth of high-level facilities and a third of mid- and low-facilities had opened within the past 5 years:
Table 1.
Characteristics of private delivery facilities, by type
| Low level | Mid-level | High level | Total | |
|---|---|---|---|---|
| (N = 29) | (N = 113) | (N = 120) | (N = 262) | |
| Ownership type (%) | ||||
| Individual | 86.2 | 70.8 | 71.7 | 72.9 |
| Partnership | 13.8 | 23.9 | 22.5 | 22.1 |
| Company (Private Ltd or Public Ltd) | 0 | 0 | 5.0 | 2.3 |
| Faith-based or other not-for-profit | 0 | 5.3 | 0.8 | 2.7 |
| Owner lives at facility (%) | 62.1 | 36.4 | 39.2 | 40.5 |
| At least one female owner (%) | 55.2 | 33.9 | 30.0 | 34.5 |
| Medical qualification of owner(s)a (%) | ||||
| Medical doctor | 34.4 | 72.8 | 78.4 | 70.3 |
| AYUSH (BAMS, BUMS, BHMS) | 44.8 | 13.6 | 12.5 | 16.6 |
| Otherb | 10.3 | 9.1 | 4.2 | 7.0 |
| None | 13.8 | 6.4 | 8.3 | 8.1 |
| Infrastructure and equipment (%) | ||||
| Mains electricity connection | 96.6 | 100 | 100 | 99.6 |
| Back-up electricity source | 92.3 | 97.3 | 99.2 | 97.6 |
| Wired phone line or mobile phone | 86.2 | 92.9 | 99.2 | 95.0 |
| Internet connection | 44.8 | 67.0 | 90.8 | 75.5 |
| Ambulance | 0 | 0.9 | 11.9 | 5.8 |
| Pick-up van | 0 | 20.4 | 28.8 | 21.9 |
| Operating theatre | 24.1 | 94.7 | 99.2 | 88.9 |
| ICUc | 0 | 0 | 100 | 45.8 |
| Pathology | 20.7 | 33.6 | 64.2 | 46.2 |
| Ultrasound | 7.1 | 39.6 | 65.0 | 47.9 |
| Blood bank | 0 | 4.6 | 5.0 | 4.3 |
| In-house medical store | 51.7 | 67.6 | 92.5 | 77.3 |
| Government registration (%) | 8.0 | 50.5 | 53.1 | 47.2 |
| Network participation (%) | ||||
| Federation of OBGYN Societies of India (FOGSI) | 3.7 | 13.0 | 34.8 | 22.0 |
| Member of maternal health social franchise | 0 | 1.8 | 7.6 | 4.3 |
| Delivery-related training within last 2 years | 0 | 4.5 | 2.5 | 3.1 |
| Bed and room numbers, median (IQR) | ||||
| Number of inpatient beds | 5 (2, 8) | 10 (10, 18) | 20 (13.5, 39.5) | 15 (10, 24) |
| Number of private rooms | 0 (0, 2) | 3 (2, 4) | 4.5 (3, 8) | 4 (2, 6) |
| Delivery numbers per month, median (IQR) | ||||
| All deliveries | 4 (2, 6) | 13 (7, 24) | 18 (11, 30) | 14 (7, 25) |
| Normal deliveries | 4 (2, 6) | 10 (4, 20) | 12 (7, 20) | 10 (5, 20) |
| C-sections | 3 (2, 7) | 5 (3, 8) | 4 (3, 8) | |
| Years in operation, median (IQR) | 6 (4, 13) | 8 (3, 14) | 10 (6, 16) | 9 (4, 15) |
Sums to >100% as there may be more than one owner.
Includes Auxiliary Nurse Midwife, Bachelor of Electro Homeopathy & Surgery/BEMS, a range of diploma degrees, and unspecified qualifications.
We defined high-level facilities as those with an ICU.
Source: Private delivery facility survey.
When we started in 1993 there were only a few hospitals. Now there are 16-17 within a radius of 5 kms (High-level facility 3, KC).
However, respondents also noted that some rural areas remained very under-served, with limited capacity to manage birth complications in either the Government or private sector.
Ownership of private delivery facilities was overwhelmingly by individuals or partnerships (mainly husband and wife) (Table 1). Commercial chains were almost entirely absent from the market, with only 6% of owners having more than one facility, most commonly two. Most were owned by medical doctors (70%) with MBBS or MD degrees, though 17% of owners had AYUSH qualifications, and 15% had unrecognized diplomas and certificates in nursing or AYUSH or no health qualifications. Among the 76 facilities not owned by medical doctors, 75% reported employing at least one doctor on staff, though it is likely that some reported visiting consultants as staff members out of regulatory concerns.
Over half the facilities were not on the registration list held by the Chief Medical Officer, with registration particularly low among low-level facilities (8%). Only 22% reported being a member of the national obstetrics and gynaecology association (FOGSI), with this most common among high-level facilities. Membership of maternal health social franchise networks was very rare (4%), very few had received any recent delivery-related training (3%), and only three or four high-level hospitals were accredited with national bodies, with accreditation reported to be out of reach for most of the market.
Most facilities were relatively small, with a median of 15 beds. Nearly all low-level facilities had 10 or fewer beds, but 30% of high-level facilities had over 30, and 6% (seven facilities) had over 100. Private rooms were offered at 89% of facilities, with a median of four rooms; however, less than half of low-level facilities had private rooms. Availability of other infrastructure and equipment is shown in Table 1.
The typical number of private facility deliveries reported per month was low, with a median of 10 normal deliveries and four C-sections (in contrast some public facilities were said to conduct over 200). It is possible that facilities under-reported these figures, perhaps out of concern that the information might be relayed to tax authorities, but they likely give a picture of the general scale of operation. Both high- and mid-level facilities accounted for substantial shares of private deliveries (Figure 2), though high-level facilities were much less common in the more rural districts of Kanpur Dehat and Kannauj. While low-level facilities made up 11% of facilities they only accounted for 3.5% of private deliveries (Figure 2). To give a rough indication of market concentration in each district, we calculated the share of reported private sector deliveries accounted for by the five facilities with the highest utilization. The top five facilities were responsible for over half of private deliveries in Kanpur Dehat (84%), Kannauj (70%) and Rampur (54%), compared with 33% in Kanpur City, and only 10% in Bareilly.
Figure 2.
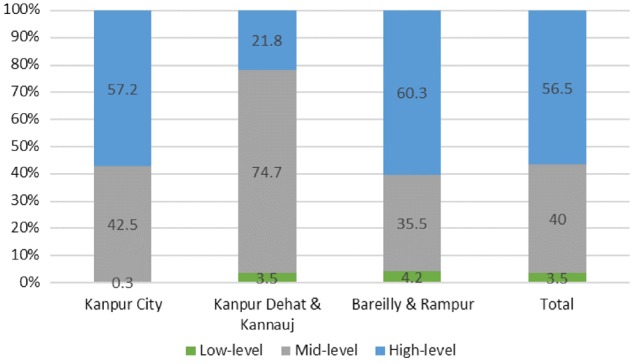
Share of private deliveries by facility type and study site.
Pricing
Private sector deliveries were usually priced as all-inclusive ‘packages’ including clinical care, hotel aspects, medicines and tests. There were different package rates for normal and caesarean deliveries, and for general wards and private rooms. Rates could also be higher for patients with likely complications, e.g. due to hypertension.
Based on survey responses, a normal delivery was on average USD 67 (INR 4500) in a general ward and USD 97 (INR 6500) in a private room, and a C-section USD 165 (INR 11 000) and USD 202 (INR 13 500), respectively (Table 2). Survey respondents reported relatively minor differences across facility categories, with the median price of a normal delivery only USD 15 higher in a high-level than a low-level facility. However, during IDIs much higher upper-ranges were given for high-level facilities, up to USD 373 (INR 25 000) for normal deliveries and USD 1492 (INR 100 000) for C-sections, perhaps indicating that prices reported under survey conditions may be biased downwards, particularly for higher-end facilities.
Table 2.
Midpoint of price rangea for deliveries in private facilities [USD, median (IQR)]
| Low-level | Mid-level | High-level | Total | |
|---|---|---|---|---|
| (N = 29) | (N = 113) | (N = 120) | (N = 262) | |
| Normal deliveries | ||||
| General ward | 52 | 56 | 67 | 67 |
| (52, 67) | (49, 67) | (52, 82) | (52, 82) | |
| Private rooms | 90b | 82 | 105 | 97 |
| (67, 135) | (67, 105) | (82, 127) | (82, 120) | |
| C-Section deliveries | ||||
| General ward | 165 | 165 | 165 | |
| (135, 187) | (165, 202) | (135, 262) | ||
| Private rooms | 202 | 217 | 202 | |
| (165, 236) | (202, 258) | (195, 247) |
Survey respondents were asked the typical price range for delivery, and the midpoint of these ranges was calculated. Based on the median of these midpoints.
Less than half of private primary facilities had private rooms (n = 11).
Source: Private delivery facility survey.
Most respondents from all facility categories spoke about the need to conform to local market rates to remain competitive, with a few actively surveying competitors’ prices. One facility’s low rates could have a major effect on the market:
Because of X Hospital (a mid-level private facility), no one can change the rates. They charge minimum for the delivery cases. X hospital has ruined the market of entire Kannauj (Mid-level facility 13, KKD).
Within a facility the package rate could vary across patients by a few thousand rupees (USD 15–30) but a couple of facilities reported higher variations (INR 7000-10 000/USD 105–150). Patients were said to demand discounts, based on their financial constraints or in some cases political connections. Smaller hospitals in the city outskirts and in rural block towns seemed to face particularly strong pressure, with a few reporting that patients and relatives could create a ‘nuisance’ when their request was turned down, though several facilities said they did adjust their prices to patients’ paying capacity. Due to these flexible rates, it was also common to avoid giving bills to patients:
If you make a bill then you will not be able to justify about the charges, like you charged 13000 from Rekha Devi for general ward and so why did you charge 15000 from Shyama Devi. It demands an explanation. How did you calculate? So you can be caught in an audit (financial comparison). So if there is no bill, then there is no audit (Mid-level facility 15, KKD).
The vast majority of patients paid in cash. Around a fifth of mid- and high-level facilities were enrolled in the government health insurance scheme for poorer groups, Rashtriya Swasthya Beema Yojana (RSBY) (http://www.rsby.gov.in/how_works.html). However, many facilities no longer participated due to low reimbursement rates, burdensome paperwork, and difficulties obtaining payments, including requests for bribes. Only a few, mainly high-end facilities, were empanelled in other public (8%) or private (4%) insurance schemes, termed TPAs (Third-Party Administrators). Some higher-end facilities were empanelled with as many as 20 schemes, but even in these facilities over 90% of clients were uninsured and paid out-of-pocket. Respondents at a few mid-level facilities expressed interest in TPA affiliation, but faced obstacles reaching the standards demanded, e.g. for ‘private rooms, air conditioners in the rooms and television’. Low-level facilities were not even aware of the insurance schemes.
Non-price competition
The IDIs revealed five key dimensions of non-price competition between private facilities: location, medical infrastructure, hotel features, staffing and marketing including commission payments.
Location
Location was considered vital in influencing demand. Mid-level facilities often located on main roads leading into large towns (Figure 1a):
This being a by-pass road, patients come here directly with ease, majority of those are from rural areas who cannot afford costly hospitals in the central part of the city (Medical store 1, BR).
It also made sense for facilities to locate in clusters, benefiting from the area’s reputation for healthcare provision. Mid-level facilities outside major towns tended to cluster close to government facilities (Figure 1b, c); C-sections were rarely available in these government facilities, so patients with complications were referred to higher level government hospitals in the nearest major town. However, patients were often reluctant to travel that far, and instead preferred (or were encouraged by ASHAs or other agents) to approach nearby private facilities.
….the government is focusing on delivery services and patient is going there free of cost as 108 (free ambulance) is there to carry the patient to the hospital. When the patient gets referred, he lands in the market. So, in the market, there is other also besides me. So it is better opportunity to work here rather than anywhere else (Mid-level facility 15, KKD).
Medical infrastructure
Variations in medical infrastructure were a key aspect of non-price competition, such as operating theatres, ICUs and neo-natal ICUs (NICUs):
Nowadays pregnant women visit hospitals during pregnancy and they are well informed if there is going to be any complication during delivery. So they prefer a hospital where there is facility of surgery and blood. We also recommend same to such cases (High-level facility 4, BR).
These days the system of NICU is running a lot. So some people go more because they will get NICU facility… if they think there is some trouble with the child (Ambulance driver 1, KC).
Perhaps most important was the capacity for C-sections, provided by 89% of private facilities (Table 1), particularly as this allowed facilities to compete with the government sector. Survey data indicated that on average close to 30% of private deliveries were C-sections (Table 1), though for 2% (six facilities) this was 75% or more. Respondents attributed high C-section rates to client preferences, together with a high-risk case-mix often attributed to receiving referrals from other facilities, and less often to economic incentives:
We get mainly high risk cases. So most of our deliveries are C-secs. Also because SES (socio-economic status) are high, people also want a planned surgery…. Because they don’t want to experience pain in normal delivery and simply say do surgery to avoid those kind of problems (High-level facility 3, KC).
In case of Caesar, profit of hospital is more since patient stay is more, ranging from 5 to 7 days… (High-level facility 12, KC).
In-house services were also said to give facilities a competitive edge, particularly pathology, diagnostic imaging (especially ultrasound) and a medical store:
Yes, we have our ambulance, diagnostic services and a medical store. In fact profit is less if these are done from outside. Here they get each and every service under one roof like a shopping mall (High-level facility 9, BR).
Hotel features
Hotel features such as furnishings, private rooms and customer service were also central in attracting patients. Many high-level private facilities offered luxury hotel-like accommodation that included a variety of differently priced private rooms, some with air-conditioning, television and en-suite bathrooms. Even mid- and low-level facilities increasingly offered basic private rooms. These features attracted patients from other private facilities, and from government facilities where hotel aspects were known to be poor.
Staff qualification and reputation
Staff with higher qualifications and good reputations provided a distinct competitive edge:
Irrespective of how many glasses (plate glass building façade) you have put in the hospital…glass and story (number of floors) do not matter. Qualification, education and facilities matter (Mid-level facility 1, KC).
Reputation was built both on technical skills and compassion, familiarity and trust gained over many years, almost establishing clinicians as a brand:
Like while buying ‘surf’ powder—people ask give us Nirma (Indian clothes detergent brand)—they do not say surf or detergent powder. Similarly, in this area, Dr. XY’s name sells like Nirma brand (Mid-level facility 10, KC).
Most important is that Sir [Dr. XX] himself see all the patients. When he goes on rounds in the ward more than half of the patient gets cured just by seeing him. They feel that doctor himself is coming to ask about their condition (Private Facility Public Relations Officer (PRO) 1, KKD).
Reflecting women’s preferences, most obstetricians were female, and female staff were also valued in low-level facilities without medical doctors. While most facilities claimed to have a medical doctor on staff and many an obstetrician, in practice nearly all mid- and high-level facilities relied heavily on visiting consultants for delivery care, with a median 5 and 7 consultants, respectively, particularly obstetricians, anaesthetists and surgeons, who in turn were affiliated with several hospitals:
We will be in touch with 3-4 anaesthesiologists (visiting consultants). They also have 4-5 hospitals they go to. So if one is not available then we call another (Professional association representative 1 and hospital owner, BR).
Basically you have to increase the acquaintance with doctors so that they give work. Right now I only have 4 hospitals. All these hospitals are maternity only. Or else surgical/general (Consultant 1, BR).
One high-level facility providing advanced multi-specialty care worked with over 90 consultants:
Other hospitals have many visiting consultants…… There is one person there whose only work is to phone and call consultants and maintain their accounts (Mid-level facility 8, KC).
These consultants operated on three different business models (Box 1). In some cases consultants (and facility owners) reportedly also held government posts, though such ‘dual practice’ was officially outlawed.
Key Messages
The private healthcare sector is an important provider of maternity care in low- and middle-income countries but there is relatively little literature providing an in-depth understanding of the operation of these providers.
Delivery facilities in Uttar Pradesh formed part of a rapidly expanding and heterogeneous market, segmented by complexity of care and socio-economic status of clientele; most facilities were small and independently owned, generally clustered in cities and larger towns and over half were not registered.
To address strong competition from both the public sector and other private providers, facilities employed a range of price and non-price strategies; key elements of non-price competition included location, medical infrastructure, hotel features, staff qualification and reputation, and marketing.
Concerns include lack of care for complex deliveries in less urban areas, limited affordability of private facilities, a lack of appropriate medical professionals and qualified nurses on staff leading to heavy reliance on visiting consultants, and high commission payments to agents who brought clients to the facility, for both new patients and those transferring from public facilities.
Two thirds of low-level facilities also used visiting consultants, but usually just one, generally for emergencies. In the more remote areas with only low-level facilities, there was a critical shortage of doctors, and patients were usually served by AYUSH providers, nurses or unqualified staff. We also heard of low-level facilities providing surgical care without qualified medicks:
In X Hospital, Dr. Y, who is not qualified at all does the surgery himself, even gives anaesthesia himself and thus saves money there also (Mid-level facility 13, KKD).
Respondents noted the challenges of attracting doctors outside larger cities, given the lack of infrastructure and economic opportunities:
This is a very interior area sir. This is one of the cheapest regions sir, and here doctor, MBBS doctor, isn’t there amongst us in the private. The condition is not good here. There are no amenities or facilities here. Big doctors are not able to get through their expenses here so will they sit here? (RMP 1, KKD).
In both rural and urban areas, there were also major challenges attracting other types of qualified staff, particularly nurses with legitimate degrees and diplomas.
Box 1 Business models for visiting consultants
Respondents outlined three business models for consultants, though they could co-exist in one facility:
Model 1—Consultants visit a facility regularly to conduct outpatient clinics, being paid a fixed amount every month, or per patient.
Model 2—Consultants are ‘on-call’, visiting a range of facilities when required, receiving a fixed fee for service (e.g. USD 30 for an anaesthetist), or an agreed percent (e.g. 30–50% of the client’s total bill). Facilities have a number of consultants on their books, to ensure they can find one when needed. Some consultants may also run their own hospitals or clinics.
Model 3—Higher-end obstetricians have their own outpatient practices where they enrol women for antenatal care, but contract with one or more high-level facilities, where they effectively rent services for their patients’ deliveries (i.e. ward, operating theatre, nursing staff and medicine costs). The consultant bills the patient directly, or in some cases the patient pays the hospital and doctor separately.
Marketing and commission payments
Most private facilities put considerable effort into promotion and marketing. While some well-established facilities could rely on reputation and word-of-mouth, newer facilities in particular used a range of marketing strategies, with one mid-level facility noting ‘one has to struggle to attract the patients’.
Mass print media such as hoardings and newspaper advertisements were sometimes used, but said to be costly and were not encouraged by the Medical Council of India. A more popular approach was ‘health camps’, particularly for mid- and low-level facilities. Camps were held close to rural communities or at the facility, with clinicians providing free services and medicines for certain conditions, occasionally including maternal health. The camps were partly seen as a charitable act, but also attracted patients to the facility:
…. at [the camp] we give medicines free of cost for 1-2 days. So what happens with that is that the patient gets impressed there, and then that patient comes till here……. If we see 100 patients there, then 10 patients come to us within the next week. And those patients we give special response to, who come through the camp—30% off (Mid-level facility 1, KC).
Several large- and medium-sized facilities employed full-time marketing agents, termed ‘PROs’ (public relations officers), whose job was to increase patient business. They travelled around 50–100 villages, spreading information about their hospital’s services and networking with local agents including Dais, ASHAs, ambulance drivers and RMPs to draw in patients. A few PROs were well-networked with health staff in in order to attract (informal) referrals:
Sometimes in case of emergency or for better care, they (ASHAs) directly bring cases to our hospitals. We provide them incentives which ranges from R 1500 to 2500–3000 depending upon the situation. I also establish contacts with the ASHAs to know the status of pregnant women in their areas … mobilizing ASHAs to come directly to our hospital (PRO 2, KKD).
One interviewee even reported this leading to PROs fighting over patients outside a public hospital:
There was news recently that in xx hospital, people from private sector were roaming. They were picking-up the patients. So what happened was that a patient was approached from two hospitals and they got engaged in a fight on the issue that the patient will go to their respective hospitals. Means there were two dogs for a single chapatti [Indian bread]! (Mid-level facility 15, KKD).
Payment of commission to agents for bringing new clients or referrals was a very common feature of the market. IDI respondents described the importance of commission payments or ‘cuts’, particularly for private ambulance drivers, ASHAs and RMPs.
When they (ambulances) pick up a patient they call the (hospital) management first that sir I’m getting a patient. What is it for? For this…and tell me sir how much will you give me, what will you give me? Then they say that okay sir, I’ll just let you know (High-level facility 5, KC).
While some in-kind gifts were given, such as sweets or sarees for ASHAs, financial commission payments were standard and large—often 20–30% of the full patient fee.
There is one X hospital in this area, they get many delivery cases. ASHA sends patients in large numbers to that hospital. Everyone’s commission is set in advance. Every third month (quarterly) there is party in ABC hotel for them (organized by X Hospital). They arrange all sort of entertainment activities for the invitees. They spend lakhs of rupees on a single day. These ASHAs also get gifts—sweets and clothes (Medical store 1, BR).
To facilitate commission claims, one facility noted registration numbers of ambulances bringing patients so they could be paid afterwards:
Some people are honest in their work. Like X hospital, they make a slip in the name of driver who drops the patients. What they do is on a bill of Rs. 1 lakh they give Rs. 30,000 to private drivers very honestly. They have installed CCTV and they note down the ambulance driver vehicle number and name at the time when driver reaches the hospital for dropping the patients (Ambulance driver 2, BR).
Commission was also paid to diagnostic providers and sometimes medical stores, who in turn paid private facilities and government doctors for referring patients to them, reportedly ranging from 30% to 70% of the patient fee. Diagnostic providers sometimes also paid other allied providers for referrals:
We appointed a boy who used to stick pamphlets on the clinic of those doctors who are ‘Jholachhap’ (unqualified/informally trained) and those doctors used to send their patients to us with a slip so that they can claim commission afterwards. If a patient is known to the local RMPs, we give them concession (Diagnostic provider 1, BR).
In contrast, some facilities said they never gave commissions, and others that they had given up this practice due to its large and increasing costs, with one doctor claiming that unaffordable commissions had led him to close his rural delivery practice. A few agents like ASHAs and RMPs said they had rejected overtures made by private facilities:
They had invited me few times, they asked me—Doctor Saab [sir] please come for lunch. But I never went (RMP 2, BR).
Discussion
This study is the first to explore the market structure and competitive strategies of private delivery providers in India. It revealed a rapidly expanding and heterogeneous market, segmented by complexity of care and clientele socio-economic status. The market generally conformed to the characteristics of monopolistic competition, with private facilities reportedly facing strong competition from both the public sector and other private providers, though there were areas of relatively high concentration in urban areas and for some market segments. Providers were likely to be relatively sensitive to profit incentives given that most facilities were owned by individual or partnerships (implying little separation between ownership and management), and the very low numbers of non-profit organizations. Barriers to entry into the market appeared relatively low for a healthcare market, reflecting poor regulatory enforcement and the small scale of most facilities, as indicated by high recent entry. However, some barriers still existed in terms of the reputation of well-established providers, and poor availability of qualified staff and consultants outside the cities. Price competition was reportedly quite intense competition, reflecting the price sensitivity of clients in a context of very low-insurance coverage and generally low socio-economic status. However, non-price competition was a key feature of the market, with providers seeking to maintain and increase market share by product differentiation on aspects of care observable to patients such as medical infrastructure, hotel features and staff reputation. However, the potential for clients to judge clinical quality of delivery care either before or after delivery is likely to have been very low, leading many providers to rely heavily on marketing and commission payments to attract patients.
A key challenge for the study was the initial identification of delivery facilities. We conducted an intensive mapping exercise to address this, but it is likely that those most hidden or least willing to acknowledge conducting deliveries would be lower-level facilities. There may also have been a few rural facilities outside block centres which our mapping did not cover. This could have somewhat biased upwards our estimates of qualifications and infrastructure though IDIs and informal conversations indicated that nearly all facilities were captured. Data collection covered issues that were sensitive from commercial, ethical and regulatory perspectives. We found considerable indications of this in triangulating between the survey data and IDIs, and across IDI respondents. For example, IDIs indicated higher prices and less qualified staff than survey data. While some respondents were clearly cautious about discussing topics such as facility registration, dual practice and commission payments, others discussed these issues openly, indicating that they were considered normal.
The study covered five diverse districts but cannot be considered representative of Uttar Pradesh state; in particular, we did not include the poorest districts where private deliveries are least common (Government of India, 2014). Even greater care is needed in considering the applicability of the findings to other Indian states. Uttar Pradesh has the second lowest State Domestic Product (GDP) (Government of India, 2018–19) in India, and one would expect wealthier states to have a more developed private market, facilities with better infrastructure and staffing, higher insurance coverage, and greater entry of hospital chains (Mony et al., 2013). Caution is also needed in extrapolating these findings to markets for other healthcare services. Given that 85% of study facilities also provided general inpatient care, there are likely to be many similarities between delivery care and other inpatient services in terms of market segmentation by sophistication of services, price packages (which are elastic and negotiable), low-insurance coverage and out-of-pocket payments (often without bills), commissions for referrals, and heavy reliance on visiting consultants. However, our facility mapping indicated that markets for outpatient services are very different, reflecting the >10-fold higher number of facilities. Further research on competition is therefore warranted both in settings with different income levels and for different health services.
Turning to the implications for accessibility, delivery facilities were highly clustered, leading to a crowded marketplace in urban and peri-urban centres, with intense competition, particularly among mid-level facilities. Outside these more urban areas, geographical accessibility was much lower, especially for C-section and intensive care, and staff were less qualified. One might expect government facilities to fill this gap, but in practice rural public C-section provision was very limited, meaning that many women travelled substantial distances for delivery care—either electively or in an emergency.
In terms of financial accessibility, typical prices reported in the survey ranged from USD 50 to 120 for normal deliveries, and USD 130–250 for C-sections, with IDIs indicating that prices may have been higher in practice; these facilities would be unaffordable to a large share of the population. Even for middle-income clients, the economic burden was potentially high, especially for C-sections, given the very low private insurance coverage.
We did not assess clinical quality, but others have documented major concerns with the quality of private and public sector care for delivery and more generally (Das et al., 2012; Sharma et al., 2017). Quality concerns identified in this study included lack of qualified medics and nurses on staff, and heavy reliance on visiting consultants. This allowed costly specialist resources to be spread across many clustered facilities, but using consultants rather than full-time staff may affect timeliness and continuity of care, maintenance of quality standards, and supervision of junior staff, with consultants likely to be under substantial time pressure. Reliance on busy consultants, especially obstetricians covering several facilities, could also be one reason for high C-section rates in private facilities, reflecting the desire to plan the timing of delivery (Peel et al., 2018). One reason for relying on consultants was the highly fragmented nature of the markets, with most facilities performing very few deliveries (median of 14 per month). Even though specialist staff such as surgeons and anaesthetists might also have had a role in other procedures, low delivery numbers would have reduced the capacity of facilities to pay full-time specialist staff. More generally, it has been noted that provision of high-quality maternity care requires a relatively high caseload, so that clinicians regularly see key complications, and therefore maintain skills in managing these (Kruk et al., 2016). The degree to which these benefits are reaped by busy consultants covering many hospitals is unclear.
Another key concern was the referral policy in government facilities unable to cater for delivery complications, which left high-risk women at the mercy of private facilities and agents with a strong financial stake in their referral location. This hampered continuity of care at this key stage, and could lead to poor choices of private facilities, and/or substantial financial burdens to women who had planned a free government delivery. More generally, commission payments for bringing patients to facilities were common and high, a widespread phenomenon in India, despite being outlawed by the Medical Council of India Code of Ethics (Medical Council of India, 2002; Krishnan, 2014). These payments may have pushed up prices, and potentially compromised quality of care, if agents took patients where their commission was highest, rather than where they thought quality was best. Facilities that saw their clientele as price sensitive, may also have compromised the quality of their care in order to keep prices low in the face of hefty commissions.
These findings highlight several potential areas of intervention. First, considering that less than half the delivery facilities were registered, a key foundation would be universal registration, facilitating assurance of minimum standards and targeting of quality improvement initiatives. Despite the official adoption of the Clinical Establishments Act in Uttar Pradesh mandating this, the Act is yet to be implemented, reflecting major political challenges in increasing regulation in the medical sector, and the contested roles of AYUSH providers.
Secondly, there is a major lack of quality improvement strategies, with almost no delivery-related training for private providers, and very limited coverage of broader strategies. While existing accreditation schemes were out of reach of all but the highest-end facilities, such schemes could play an important role in quality improvement and quality signalling if linked with insurance empanelment, and adapted to the context of mid-level facilities (Montagu and Goodman, 2016). The National Accreditation Board for Hospitals (NABH) and Healthcare Providers (2016) has introduced a step-wise system beginning with a pre-accreditation Entry level certificate which represents important progress. However, the fragmented nature of the market implies that engaging in facility-by-facility quality improvement is a substantial challenge, unless there is greater consolidation of the market and/or careful targeting of facilities. Consolidation might be encouraged through more effective regulation, incentivising facilities to merge in order to meet staffing and infrastructure requirements, or through third-party payers prioritizing larger facilities or facility networks for empanelment. However, concern has been expressed about overpricing and malpractices in corporatized Indian hospitals (Rao, 2018), and such strategies could further reduce access and affordability, especially for the least served populations. An alternative could be to target facilities for quality improvement initiatives based on their local market share, with our analysis showing that the busiest facilities were responsible for a relatively high share of the private delivery market in most of the areas studied.
Turning to demand-side strategies, improving patient information could reduce the need for commission-earning agents, and improve quality of care, e.g. through independently verified facility report cards, or mobile/online information and review platforms. Demand could also be influenced by expansion of subsidized third-party payment mechanisms within the private sector, combined with strategic purchasing of more complex care, as proposed under the recently announced ‘National Health Protection Scheme’ of Ayushman Bharat (Chatterjee, 2018). However, the widespread bureaucratic challenges which discouraged private facilities from participating in RSBY and JSY would need to be addressed (Yadav et al., 2017). Specific contracting mechanisms could also be considered to subsidize emergency referrals from primary level government facilities to appropriate private providers in areas where higher level government services are not available within a reasonable distance.
Finally, providers are heavily affected by competition, and for most private providers the government sector remained a key competitor. This implies that an appropriately financed and good quality public sector is likely to be one of the most important influences on not only public but also private sector performance.
Ethical approval
Ethical approval was obtained from the Institutional Review Boards of the London School of Hygiene and Tropical Medicine, UK, and the Centre for Media Studies (CMS-IRB) in New Delhi, India. Informed oral consent was obtained from all interviewees.
Supplementary Material
Acknowledgements
We are grateful to all our study subjects for participating in this study, and to the National Health Mission of Uttar Pradesh for their support.
Funding
This research was supported by funding from MSD, through its MSD for Mothers programme. MSD for Mothers is an initiative of Merck & Co., Inc., Kenilworth, NJ, USA. MSD had no role in the design, collection, analysis and interpretation of data, in writing the manuscript, or in decisions to submit for publication. The content of the manuscript is solely the responsibility of the authors and does not represent the official views of MSD.
Conflict of interest statement. None declared.
References
- Government of India. 2018–19. State Domestic Product and Other Aggregates GOI, New Delhi, India: Ministry of Statistics and Programme Implementation. http://mospi.nic.in/data, accessed 24 June 2019.
- National Accreditation Board for Hospital (NABH) and Healthcare Providers. 2016. Introduction to Pre-Accreditation Entry Level Certification Standards New Delhi: NABH, Quality Council of India, http://www.nabh.co/Hospital-EntryLevel.aspx, accessed 19 June 2018.
- Babiarz KS, Mahadevan SV, Divi N, Miller G.. 2016. Ambulance service associated with reduced probabilities of neonatal and infant mortality in two Indian states. Health Affairs (Millwood) 35: 1774–82. [DOI] [PubMed] [Google Scholar]
- Bautista 1995. Markets in Health Care: An Analysis of Demand, Supply and the Market Structure of Health Care in the Philippines. London: London School of Hygiene & Tropical Medicine. [Google Scholar]
- Bennett S. 1996. Imperfect Information and Hospital Competition in Developing Countries: A Bangkok Case Study. London: London School of Economics and Political Science, University of London. [Google Scholar]
- Campbell OM, Benova L, Macleod D. et al. 2016a. Family planning, antenatal and delivery care: cross-sectional survey evidence on levels of coverage and inequalities by public and private sector in 57 low- and middle-income countries. Tropical Medicine & International Health 21: 486–503. [DOI] [PubMed] [Google Scholar]
- Campbell OM, Calvert C, Testa A. et al. 2016b. The scale, scope, coverage, and capability of childbirth care. Lancet (London, England) 388: 2193–208. [DOI] [PubMed] [Google Scholar]
- Campbell OM, Graham WJ; Lancet Maternal Survival Series Steering Group. 2006. Strategies for reducing maternal mortality: getting on with what works. Lancet 368: 1284–99. [DOI] [PubMed] [Google Scholar]
- Chatterjee P. 2018. National Health Protection Scheme revealed in India. Lancet (London, England) 391: 523–4. [DOI] [PubMed] [Google Scholar]
- Clarke R. 1985. Industrial Economics. Malden, Massachusetts: Blackwell Publishers Inc. [Google Scholar]
- Creswell JW, Plano Clark VL, Gutmann ML, Hanson WE.. 2003. Advanced mixed methods research designs In: Tashakkori A, Teddlie C (eds). Handbook of Mixed Methods in Social and Behavioral Research. Thousand Oaks, CA: Sage, 209–40. [Google Scholar]
- Das J, Holla A, Das V, Mohanan M, Tabak D, Chan B.. 2012. In urban and rural India, a standardized patient study showed low levels of provider training and huge quality gaps. Health Affairs (Millwood) 31: 2774–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dranove D, Satterthwaite M.. 2000. The industrial organization of health care markets In: Culyer A, Newhouse J (eds). Handbook of Health Economics. Amsterdam, The Netherlands: Elsevier Science, 1093–139. [Google Scholar]
- Gautham M, Shyamprasad KM, Singh R, Zachariah A, Singh R, Bloom G.. 2014. Informal rural healthcare providers in North and South India. Health Policy Planning 29(Suppl 1): i20–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George A, Iyer A.. 2013. Unfree markets: socially embedded informal health providers in northern Karnataka, India. Social Science & Medicine (1982) 96: 297–304. [DOI] [PubMed] [Google Scholar]
- Goldenberg RL, Mcclure EM.. 2017. Improving birth outcomes in low- and middle-income countries. The New England Journal of Medicine 377: 2387–8. [DOI] [PubMed] [Google Scholar]
- Goodman C. 2004. An Economic Analysis of the Retail Market for Fever and Malaria Treatment in Rural Tanzania. London: London School of Hygiene and Tropical Medicine, University of London. [Google Scholar]
- Government of India. 2011. List of Cities with Their Population: Census of India http://www.censusindia.gov.in/towns/up_towns.pdf, accessed 15 April 2019.
- Government of India. 2011–12. Number and Percentage of Population below the Poverty Line .New Delhi: Reserve Bank of India; https://rbidocs.rbi.org.in/rdocs/Publications/PDFs/162T_BST130913.pdf, accessed 15 April 2019. [Google Scholar]
- Government of India. 2014. Annual Health Survey 2012-13 Fact Sheet. New Delhi: Registrar General. [Google Scholar]
- Government of India. 2018. Special Bulletin on Maternal Mortality in India 2014–16 .New Delhi: Sample Registration System, Office of the Registrar General India, Ministry of Home Affairs. [Google Scholar]
- Government of Uttar Pradesh. 2015. Statistics of Uttar Pradesh, Lucknow: Uttar Pradesh Information Department.http://up.gov.in/upstateglance.aspx, accessed 15 April 2019.
- Indian Institute for Population Studies. 2016. National Family Health Survey (NFHS-4), India, 2015-16: Fact Sheet. Mumbai: IIPS. [Google Scholar]
- International Institute for Population Sciences. 2010. District Level Household and Facility Survey (DLHS-3), 2007-08: India. Mumbai: IIPS. [Google Scholar]
- Jacobs P. 1997. The Economics of Health and Medical Care .Gaithersburg, MD: Aspen. [Google Scholar]
- Jayanna K, Mony P B M R. et al. 2014. Assessment of facility readiness and provider preparedness for dealing with postpartum haemorrhage and pre-eclampsia/eclampsia in public and private health facilities of northern Karnataka, India: a cross-sectional study. BMC Pregnancy and Childbirth, 14: 304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeffery P, Jeffery R.. 2008. ‘Money itself discriminates’: obstetric emergencies in the time of liberalisation. Contributions to Indian Sociology 42: 59–91. [Google Scholar]
- Kamat VR, Nichter M.. 1998. Pharmacies, self-medication and pharmaceutical marketing in Bombay, India. Social Science & Medicine (1982) 47: 779–94. [DOI] [PubMed] [Google Scholar]
- Krishnan V. 2014. India turns spotlight on kickbacks for referrals. BMJ (Clinical Research ed.) 349: g5265.. [DOI] [PubMed] [Google Scholar]
- Kruk ME, Leslie HH, Verguet S. et al. 2016. Quality of basic maternal care functions in health facilities of five African countries: an analysis of national health system surveys. Lancet Global Health 4: e845–55. [DOI] [PubMed] [Google Scholar]
- Lim SS, Dandona L, Hoisington JA. et al. 2010. India’s Janani Suraksha Yojana, a conditional cash transfer programme to increase births in health facilities: an impact evaluation. The Lancet 375: 2009–23. [DOI] [PubMed] [Google Scholar]
- Mackintosh M, Channon A, Karan A. et al. 2016. What is the private sector? Understanding private provision in the health systems of low-income and middle-income countries. Lancet 388: 596–605. [DOI] [PubMed] [Google Scholar]
- Mcpake B, Hanson K.. 2016. Managing the public-private mix to achieve universal health coverage. Lancet 388: 622–30. [DOI] [PubMed] [Google Scholar]
- Medical Council of India 2002. Indian Medical Council (Professional Conduct, Etiquette and Ethics) Regulations (Published in Part III, Section 4 of the Gazette of India, Dated 6th April, 2002; Amended up to 8th October 2016). New Delhi: Medical Council of India. [Google Scholar]
- Montagu D, Goodman C.. 2016. Prohibit, constrain, encourage, or purchase: how should we engage with the private health-care sector? Lancet (London, England) 388: 613–21. [DOI] [PubMed] [Google Scholar]
- Montagu D, Goodman C, Berman P, Penn A, Visconti A.. 2016. Recent trends in working with the private sector to improve basic healthcare: a review of evidence and interventions. Health Policy and Planning 31: 1117–32. [DOI] [PubMed] [Google Scholar]
- Mony PK, Krishnamurthy J, Thomas A. et al. 2013. Availability and distribution of emergency obstetric care services in Karnataka State, South India: access and equity considerations. PLoS One 8: e64126.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan R, Ensor T, Waters H.. 2016. Performance of private sector health care: implications for universal health coverage. Lancet 388: 606–12. [DOI] [PubMed] [Google Scholar]
- Nakamba P, Hanson K, Mcpake B.. 2002. Markets for hospital services in Zambia. The International Journal of Health Planning and Management 17: 229–47. [DOI] [PubMed] [Google Scholar]
- Peel A, Bhartia A, Spicer N, Gautham M.. 2018. ‘ If I do 10-15 normal deliveries in a month I hardly ever sleep at home.’ A qualitative study of health providers’ reasons for high rates of caesarean deliveries in private sector maternity care in Delhi, India. BMC Pregnancy and Childbirth 18: 470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao S. 2018. Expert view: what can India do to stop hospitals from overcharging? Scroll.in, Mar 17. [Google Scholar]
- Ritchie J, Spencer L, William O.. 2013. Carrying out Qualitative Analysis. Ch 9 Qualitative Research Practice. London: Sage. [Google Scholar]
- Sabde Y, De Costa A, Diwan V.. 2014. A spatial analysis to study access to emergency obstetric transport services under the public private ‘Janani Express Yojana’ program in two districts of Madhya Pradesh, India. Reproductive Health 11: 57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salazar M, Vora K, De Costa A.. 2016. The dominance of the private sector in the provision of emergency obstetric care: studies from Gujarat, India. BMC Health Services Research 16: 225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scherer F, Ross D.. 1990. Industrial Market Structure and Economic Performance. Boston: Houghtin Mifflin Company. [Google Scholar]
- Sharma G, Mathai M, Dickson KE. et al. 2015. Quality care during labour and birth: a multi-country analysis of health system bottlenecks and potential solutions. BMC Pregnancy and Childbirth 15(Suppl 2): S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma G, Powell-Jackson T, Haldar K, Bradley J, Filippi V.. 2017. Quality of routine essential care during childbirth: clinical observations of uncomplicated births in Uttar Pradesh, India. Bulletin of the World Health Organization 95: 419–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsevelvaanchig U, Gouda H, Baker P, Hill PS.. 2017. Role of emerging private hospitals in a post-Soviet mixed health system: a mixed methods comparative study of private and public hospital inpatient care in Mongolia. Health Policy and Planning 32: 476–86. [DOI] [PubMed] [Google Scholar]
- Yadav V, Kumar S, Balasubramaniam S. et al. 2017. Facilitators and barriers to participation of private sector health facilities in government-led schemes for maternity services in India: a qualitative study. BMJ Open 7: e017092.. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.