Abstract
Intestinal strictures are common complications of Crohn's disease (CD). Endoscopic balloon dilatation (EBD) constitutes an alternative therapy to surgery, but associated factors of procedure success are inconclusive. Therefore, we aimed to evaluate the EBD success rate and its associated factors in CD patients.
This is a retrospective cohort study of consecutive EBDs that were conducted between 2006 and 2014 among patients with CD with lower gastrointestinal tract strictures. Patients’ and stricture characteristics, short term procedure success and related complications at 1 week follow-up, and long-term clinical endpoints were documented.
A total of 138 dilatations were performed on 64 CD patients. The overall dilatation success rate was 84.8%, with no difference between primary or anastomotic strictures, or between first or recurrent dilatation procedures. Long strictures (≥4 cm) were negatively associated with successful EBDs, but not with perforations. A multivariate analysis adjusting for age, sex, smoking, and disease duration revealed that a maximal dilatation diameter of ≥15 mm was positively associated with a successful EBD, while an inflamed stricture was negatively associated with procedure success. Strictures which were both long and inflamed were associated with the lowest EBD success rates compared with other strictures. Only 32.8% of patients required surgery during the follow-up period. Long-term prevention of surgery was negatively associated with stricture length and with a successful EBD.
EBD is highly successful in treating intestinal strictures and in prevention of surgery in CD patients. Although EBD of long strictures is safe, it will not prevent surgery in the majority of cases.
Keywords: Crohn's disease, endoscopic balloon dilatation, intestinal strictures
1. Introduction
The prevalence of Crohn's disease (CD) is 0.5% in the Western world population.[1] The disease may have a fibrostenotic component, which can result in intestinal strictures that are associated with hospitalizations and surgery. A luminal stricture is prevalent in about 11% of patients with CD, and up to 35% of these patients will have developed a stricture at 10 years from diagnosis.[2] Primary strictures are considered to be a result of tissue remodeling, mostly following recovery from inflammation. Secondary strictures appear at the surgical anastomosis, and up to 70% of patients will require an additional operation for the new stricture during the course of their life.[3]
The approach to CD-associated strictures is individually tailored according to the degree of fibrosis and inflammation.[4] Anti-inflammatory agents can have some clinical efficacy in reducing the inflammatory component of the stricture, but anti-fibrotic medications are currently unavailable.[2] Consequently, endoscopic or surgical interventions are the cornerstone of treatment for strictures, especially when the fibrotic component is significant.[4] Studies have shown that CD patients with a stricture that is fibrotic, symptomatic, straight (i.e., without angulation), shorter than 4 cm, and without associated fistula, abscess, or malignancy, are expected to gain a symptomatic relief and a delay or elimination of the need for surgery after an endoscopic balloon dilatation (EBD).[4] Surgical therapy, including resection or stricturoplasty, is effective but it is an invasive procedure, and may be associated with major complications.[5,6]
Previous studies examining EBD success rates have yielded high success. A meta-analysis by Navaneethan et al[7] included 24 studies with varying endoscopic protocols for treating 1,571 EBD procedures among 1,163 CD patients. The average success rate was 89%, and the rate of major complications (e.g., perforation, bleeding that required blood transfusion, abscess, fistula, or sepsis) was 4%, of which 3% were perforations. In Israel, a single study by Greener et al[8] included 72 cases of EBD procedures among 39 CD patients, reported a technical success rate of 82% and a major complications rate of 7.6%. The main complications of EBD are perforation and bleeding, and the relatively rare ones are sepsis, abscess, fistula formations, and those related to sedation. No associated mortality has been reported.[4,5,8]
The aims of the present study were to evaluate the success rate of EBD procedures of lower gastrointestinal (GI) strictures in patients with CD, to analyze the risk factors for EBD complications and need for future surgery in a single tertiary center in Israel.
2. Methods
A retrospective cohort study, among consecutive CD patients who underwent EBD procedures for lower GI tract strictures, at the Department of Gastroenterology and Liver Diseases of the Tel Aviv Medical Center between 2006 and 2014. Patients with anal canal strictures were excluded. Also, patients were excluded if medical records were incomplete including at least 1-week follow-up after the EBD procedure.
This study was approved by the local institutional review board.
2.1. EBD endoscopic protocol
A stricture was defined as the lack of passage of an 11.5-mm diameter endoscope. EBDs were performed mostly during colonoscopy under conscious sedation in an ambulatory setting. The EBD procedures were wire-guided, with graded balloon insufflation. Pre-EBD imaging enabled the evaluation of stricture length using computed tomography (CT), but this evaluation was not mandatory prior to EBD performance. Strictures were dilated to a diameter that enabled the transverse of the endoscope or to a larger diameter according to the endoscopist's judgment. Fluoroscopy was optional for technically difficult dilatations, such as in suspected angulated or long strictures. The patients were observed and monitored for at least 2 hours following the procedure, after which they were discharged unless a complication was suspected.
2.2. Data collection
Data on patient and stricture characteristics were collected retrospectively from patient's medical records. All data were extracted per protocol by a single physician in a uniform manner, and was later validated by a blinded inflammatory bowel disease (IBD) specialized gastroenterologist.
Patient and disease characteristics were documented and included demographics, body weight and smoking status, disease onset, location, and medications used. Stricture type was defined as primary or secondary (anastamotic).
Stricture length was documented in centimeters according to imaging or endoscopic reports, while long strictures were defined as those of ≥4 cm length. Strictures were characterized according to macroscopic features as fibrotic, inflamed, ulcerated, angulated, or of fistular proximity. Inflamed strictures were defined endoscopically if features of inflammation such as ulcers or significant erythema were documented by the endoscopist. A fibrotic stricture was defined endoscopically if the mucosa did not have any inflammation features or through imaging if there was a pre-stenotic dilatation. A stricture could have been defined as both inflamed and fibrotic. Location of the stricture was defined according to the primary stricture.
The extent of dilatation was calculated as the difference between the maximal and minimal balloon inflation per endoscopic session.
EBD history, EBD urgency, and procedure parameters such as initial and maximal dilatation diameter were documented.
2.3. Short-term success of the EBD procedure
A successful EBD was defined by the ability to pass an 11.5 mm wide endoscope through the stricture after the dilatation and the absence of any documented complications during a 1-week follow up. EBD associated complications were defined as: perforations, which were treated surgically or conservatively, minor or major bleeding, hospitalization within 1 week following the procedure.
2.4. Long-term success of the EBD procedure
Medical records of patients included in the analysis were reviewed until 2019. Long-term clinical endpoints were documented as either: diagnosis of GI malignancy; documentation of stircturoplasty or stricture resection surgery; or loss to follow-up. Time to each event was calculated from the first documented EBD procedure documented.
2.5. Statistical analysis
Analysis of the distribution of the study sample's characteristics included continuous variables that were presented as means ± standard deviation (SD), and categorical variables as proportions. Univariate analysis was used for the comparison of variable distribution between the study groups. The Pearson chi-squared test was used to test the difference in the distribution of categorical variables between groups. The independent samples T test or the Mann-Whitney test was used to test the difference in the distribution of continuous variables between groups. The data were analyzed by binary logistic regression, controlling for potential confounders, in search of reliable predictive factors for efficacy and safety of the EBD procedure. Multivariate analysis adjusted for age and sex as universal confounders, and for smoking and disease duration which are established risk factors for CD complications.
Sensitivity analysis comparing first and second EBD's success rate were performed to account for this potential confounder.
The Kaplan–Meier method was used to estimate the probability of surgery free survival among CD patients after their first EBD procedure. The log-rank test was used to test the difference in overall surgery-free survival distributions between the study groups. Cox regression analysis was used to estimate the proportional hazard ratio for surgery during follow-up.
The analysis was carried out using SPSS version 22.0 for Windows (SPSS Inc., Chicago, IL). A P value <.05 was considered statistically significant.
3. Results
3.1. Study population characteristics
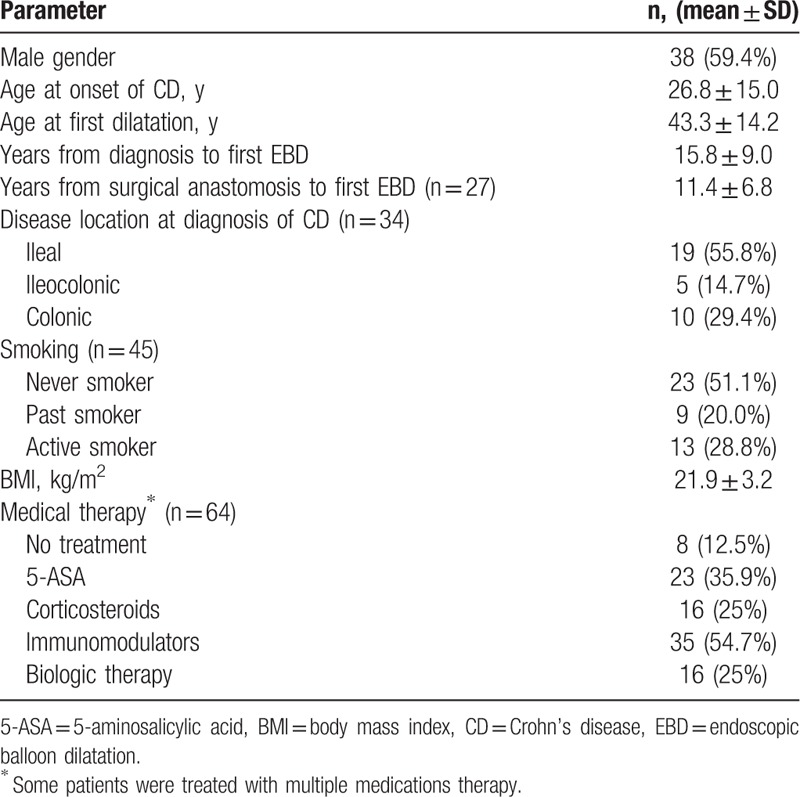
Sixty-four patients with CD were included in the analysis. In most patients, first dilatation was performed due to obstructive symptoms and further dilatations were performed in case of symptoms recurrence or recurrence of a stricture in follow-up endoscopies. EBD was performed only once in 34 of them, and between 2 and 8 times in the remaining 30 patients. At the time of the first EBD, the mean age of the entire cohort was 43.3 ± 14.2 years (range, 23–80), 59.4% were men and the mean body mass index (BMI) was 21.9 ± 3.2. Only 12.5% of patients had not been treated with any medication, while 25% were treated with corticosteroids. The demographics and clinical characteristics of the study population are listed in Table 1. Among patients who underwent more than one EBD, the mean time from the preceding EBD was 0.7 ± 1.2 years.
Table 1.
Population characteristics at the time of first dilatation (n = 64).
3.2. EBD procedure characteristics
Our analysis included 138 dilatations performed in 117 endoscopic procedures. EBDs were performed during colonoscopy (92.8%) or balloon enteroscopy (7.2%). Prior to EBD, stricture length was assessed through CT for 82 strictures (59.4%). Fluoroscopy was performed for 23 strictures (16.7%), while for the remaining strictures, length was estimated by the endoscopist. In 72.5% of cases one stricture was dilated per procedure, and in 18.8% of cases 2 strictures were dilated.
Strictures were dilated to a maximal diameter according to the endoscopist's judgment (Table 2). The mean increase in dilatation diameter during a single session was 3.7 ± 1.9 mm (range, 1–14 mm).
Table 2.
EBD procedure characteristics (n = 138).
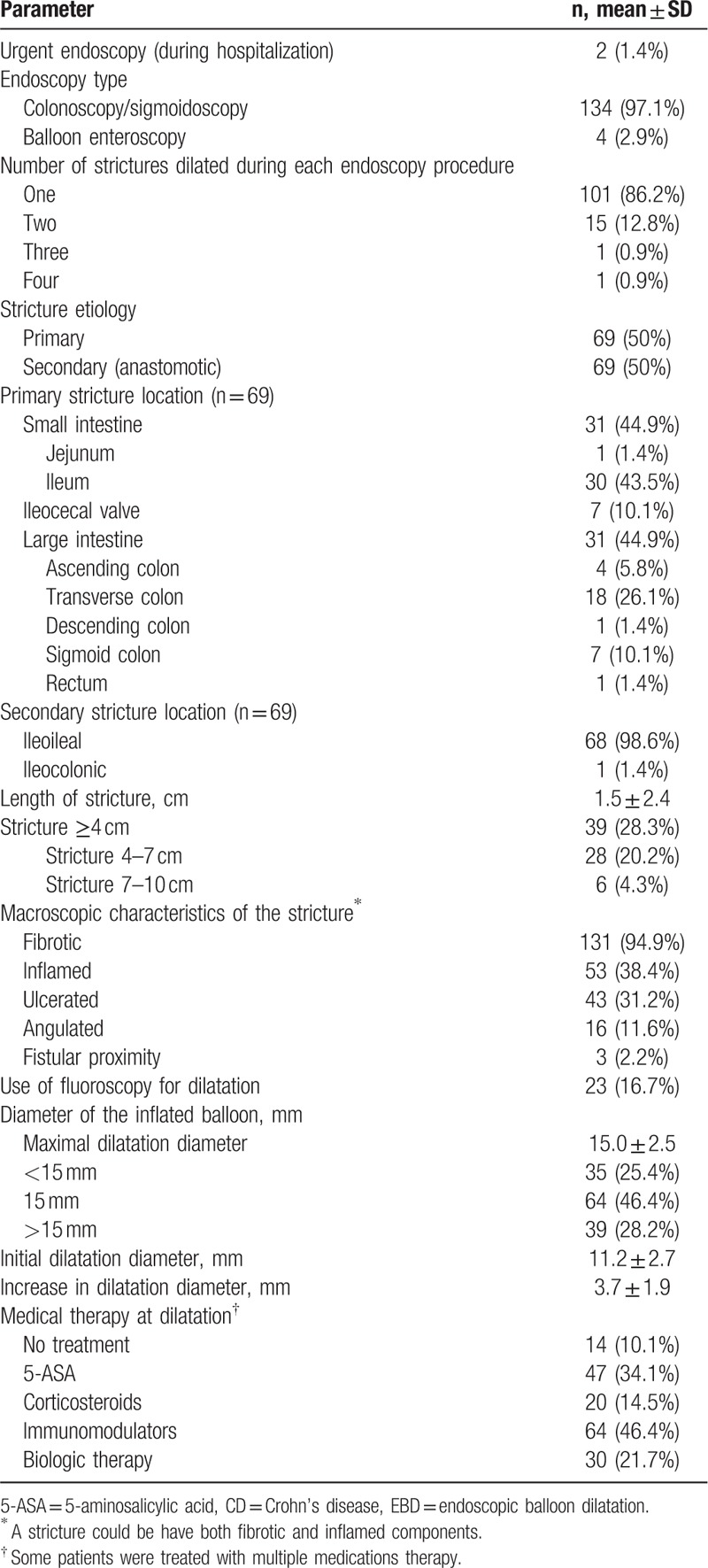
One-half of strictures were anastomotic strictures, which were mostly ileoileal. EBDs of primary strictures were equally distributed between the large and small intestines, mainly in the transverse colon and the ileum, respectively (Table 2).
The average maximal dilation diameter was 15.0 ± 2.5 mm (range, 10–20 mm). Thirty-nine (28.3%) strictures were longer than ≥4 cm, in which the mean maximal dilatation diameter was 15.0 ± 2.2 mm. Main characteristics of all 138 dilatations are presented in Table 2.
3.3. Short-term success and complications rates of EBD
The success rate of EBD procedures was 84.7% (117/138) and it did not differ between primary strictures and anastomotic strictures (85.5% vs. 84.1%, respectively P = .404). There were 7 procedure-related complications (6 perforations [4.3%] and 1 major bleeding [0.7%]), and 14 cases of technical failure (10.1%). Five of the perforations were treated surgically, and 1 was treated conservatively. The major bleeding was treated with infusions of packed red blood cells. All 7 patients with complications were hospitalized during the week following the dilatation. No other hospitalizations were documented and there was no mortality.
3.4. Association between patient and stricture characteristics and short-term EBD success and complications
Successful EBD procedures were characterized by lower rates of the following: corticosteroid therapy, stricture inflammation, large intestinal location, stricture length >4 cm, higher rates of fibrosis, and stricture dilatation of ≥15 mm (Table 3). Strictures longer than 4 cm were positively associated with failed procedures, but not with EBD-associated bleeding (2.0% vs. 0.0%, among patients with long vs. short strictures respectively, P = .176), EBD-associated perforation, (4.1% vs. 4.5% among patients with long vs. short strictures respectively, P = .743), and post EBD hospitalization (6.1% vs. 4.5% among patients with long vs. short strictures respectively, P = .677). Thus, long strictures were associated with technical failure of the procedure, but not with worse clinical outcomes. The majority of these long strictures were primary and not anastomotic strictures (67.3% vs. 40.4%, respectively, P = .002).
Table 3.
Factors associated with EBD success, complications, and long-term stricture surgery over time.
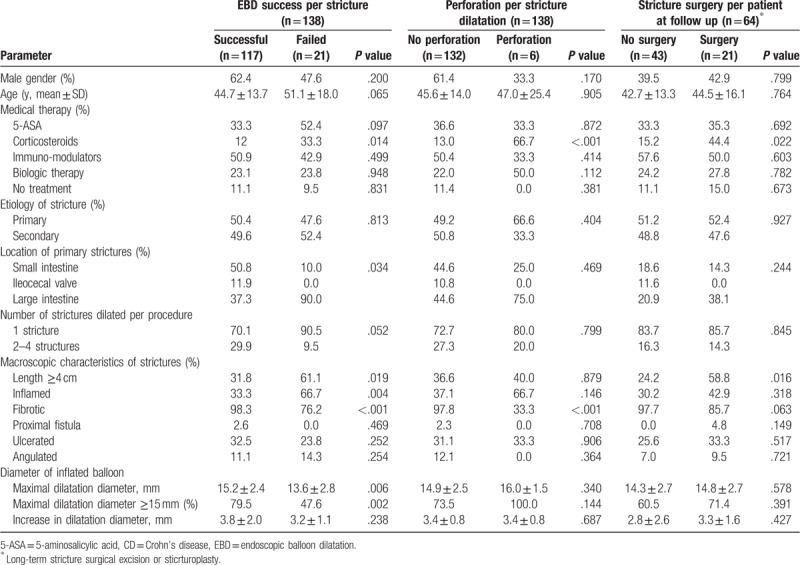
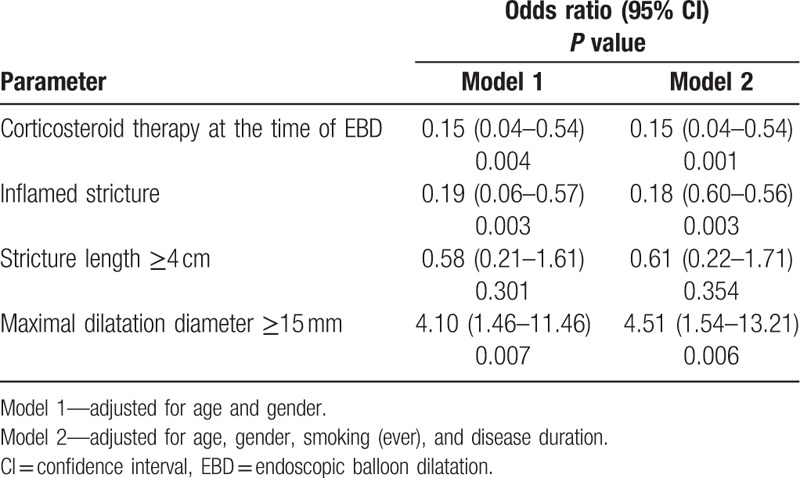
Dilatation diameter increase of each stricture was not associated with EBD success or perforation rate (Table 3). Multivariate analysis adjusted for age, sex, smoking, and disease duration showed that a successful EBD was positively associated with each increase in 1 mm of dilatation diameter (odds ratio [OR] = 1.29, 95% confidence interval [CI], 1.04–1.61, P = .021). A maximal dilatation diameter of ≥15 mm was positively associated with a successful EBD procedure (OR = 4.51, 95% CI 1.54–13.21, P = .006). Factors that were negatively associated with EBD success included an inflamed stricture and systemic corticosteroid therapy at the time of the procedure (Table 4).
Table 4.
Patient and stricture characteristics associated with EBD success.
The highest success rate for the EBD procedure was observed within the group of patients with strictures that were neither long (≥4 cm) nor inflamed. Strictures which were either long or inflamed were associated with lower success rates, and strictures which were both long and inflamed showed the lowest success rate (Fig. 1A). Inflamed strictures (both long and short ones) were negatively associated with a successful EBD procedure in a multivariate analysis adjusted for age, sex, smoking, disease duration, and maximal dilatation diameter (Fig. 1B).
Figure 1.
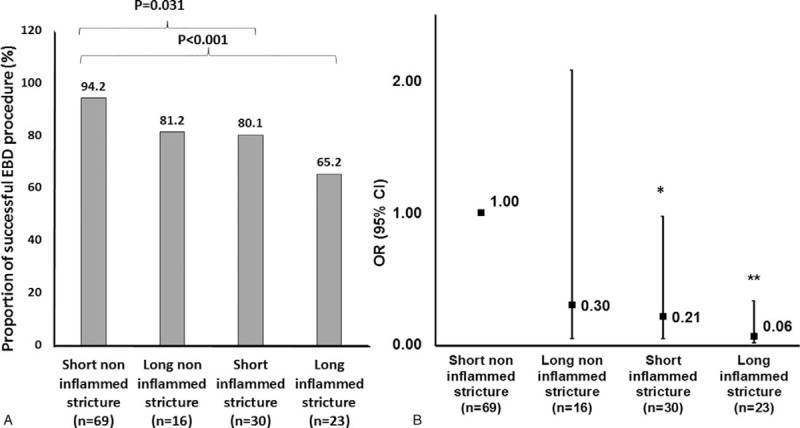
Success rate of the EBD procedure (A) and adjusted associations with successful EBD (B) among subtypes of strictures. Legend: ∗P < .05, ∗∗P < .001. Short strictures ≤4 cm, long strictures ≥4 cm. Odds ratios are adjusted to age, sex, smoking, duration of disease, and a maximal dilatation diameter of ≥15 mm. EBD = endoscopic balloon dilatation.
When the first 64 EBDs were compared with the 74 repeat EBDs, the success rate of the former was lower than that of the latter, however the difference was not statistically significant (79.7% vs. 89.2%, respectively, P = .246). Adjusted to age, sex, and maximal dilatation diameter, the first-time dilatation was negatively associated with a successful procedure, although this finding was also not statistically significant (OR = 0.48, 95% CI, 0.18–1.23, P = .127).
3.5. Stricture fibrosis has a protective association with post-EBD perforation
A post-EBD perforation was the most prevalent complication in our study. Post-EBD perforation procedures were characterized by higher rates of steroid therapy and lower rates of a fibrotic stricture (Table 3). Systemic corticosteroids therapy was positively associated with post-EBD perforation, while a fibrotic stricture was negatively associated with that complication (multivariate analysis, adjusted to age, and sex, OR = 14.34, 95% CI 2.20–93.20, P = .005 and OR = 0.013; 95% CI, 0.002–0.109; P < .001, respectively).
3.6. Long-term success and complications rates of EBD
The mean follow-up for long-term complications after the first dilatation was 3.3 ± 3.1 years (range, 0–12 years).
No GI malignancies were detected throughout the follow-up period. Eleven patients (17.1%) underwent bowel resection surgery and 10 patients (15.6%) were lost to follow-up within the first year of follow-up. Ten (15.6%) additional patients underwent surgery within the following 1 to 9 years of follow-up, reaching a total of 32.8% of patients that required surgery during the follow-up period.
Technical success of an EBD procedure was negatively associated with surgery. Only 25.5% of patients undergoing successful EBDs required surgery compared with 61.5% of patients with an unsuccessful EBD, P = 0.013. The mean surgery-free survival duration among patients with an unsuccessful EBD was shorter than that of a successful EBD (4.4 ± 1.6 vs. 8.1 ± 0.8 years, log rank χ2 = 7.4, P = .006) (Fig. 2B). Adjusting for age, sex, smoking, disease duration, and maximal dilatation diameter, a successful EBD was associated with lower hazard of surgery within the follow-up period (hazard ratio [HR] = 0.29, 95% CI 0.10–0.85, P = .024).
Figure 2.
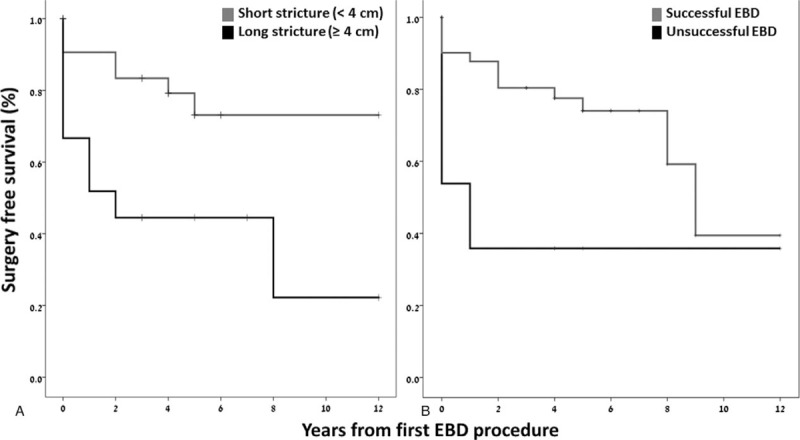
The mean surgery-free survival distribution according to stricture length (A) and EBD success (B). Legend: (A) Log rank χ2 = 6.4, P = .011. (B) Log rank χ2 = 7.4, P = .006. EBD = endoscopic balloon dilatation.
A long stricture (≥4 cm) was positively associated with surgery compared with short strictures (55.6% vs. 21.9%, P = .016). The mean surgery-free survival duration among patients with a long stricture was shorter than that of patients with short strictures (4.7 ± 1.3 vs. 9.3 ± 0.8 years, log rank χ2 = 6.4, P = .011) (Fig. 2A). Adjusting for age, sex, smoking, disease duration, and maximal dilatation diameter, a short stricture was associated with lower hazard of surgery within the follow-up period (HR = 0.31, 95% CI 0.10–0.99, P = .048). Inflamed strictures were less likely to be associated with surgery compared with non-inflamed strictures (28.6% vs. 40.9%, P = .318). There was no difference in mean surgery-free survival distribution between patients with an inflamed stricture compared with a non-inflamed stricture (5.5 ± 0.8 vs. 7.9 ± 0.9 years, log rank χ2 = 0.7, P = .402).
No other stricture characteristics were associated with surgery at follow-up (Table 3).
4. Discussion
This retrospective study aimed to evaluate the association between patient and disease characteristics and the success of EBD procedures among CD patients. Short-term EBD success rates were high, and were negatively associated with corticosteroid therapy, and with strictures’ length and inflammation, but were positively associated with a dilatation diameter of ≥15 mm. Long-term, surgery free survival was positively associated with strictures shorter of 4 cm and with technically successful EBDs.
The EBD procedure appears to be an appealing alternative to invasive surgical interventions and their associated complications. The performance of EBDs is still considered unstandardized, mainly because previous studies differ in study designs, EBD techniques, types of dilated strictures, the outcome measures used, and follow-up periods.[9]
We examined 138 EBD procedures of lower GI tract strictures of 64 consecutive CD patients treated during a period of 9 years in a tertiary medical center in Israel. The success rate of these EBD procedures was 84%, and the long-term prevention of surgery following EBD was 67.2%. These findings in agreement with success rates,[6,10,11] and surgery free survival[12–14] reported by others. Two recent meta-analyses reported an 89% technical success rate of EBD procedures among CD patients.[7,15] Our slightly lower success rates may be explained by the relatively sizable proportion (28.3%) of our patients who underwent EBD for the dilation of long strictures (≥4 cm). Long strictures have been associated with a lower EBD success rate,[3] and some studies excluded them from analysis,[10] considering greater stricture length as being an indication for surgical treatment.[6] In our cohort, the success rate of dilatation of long strictures was lower compared with short strictures, however, complication rate was not increased. Thus, a long stricture is associated with an increased rate of technical procedural failure but most probably not with a potential perforation. Therefore we may conclude that the EBD approach may offer a reasonably safe alternative to surgery. However, long-term prevention of surgery was negatively associated with stricture length, with higher hazard of surgery and shorter surgery-free survival documented among patients with long strictures. Our results are in agreement with previous reports of stricture length of ≤5 cm being associated with a surgery-free outcome, while every 1 cm increase of stricture length increased the hazard of need for surgery by 8% (P = .008).[15] Interestingly, prevention of surgery was also associated with a successful EBD among CD patients. Taken together, these results may imply that long strictures, and possibly inflamed strictures, are associated with EBD failure, and thereby determinants of surgery at follow-up.
We did not detect any difference in the success rate between sexes, primary or secondary strictures, first or repeat EBDs, stricture ulcerations, or anatomy (straight or angulated). An earlier analysis of CD-associated upper GI strictures which were treated with serial EBD procedures also demonstrated no differences in short-term efficacy, safety, or long-term outcome between the first and any later dilation procedure in the same patient.[13]
EBD complications in our cohort included mostly perforations that required surgery. There was no mortality. In line with previous studies, perforations are the most common adverse event of stricture dilatations of CD patients,[6] while EBD-associated mortality has not been reported.[6,16–18]
A multivariate analysis revealed that a successful EBD was positively associated with each increase in 1 mm of dilatation diameter, and that a maximal dilatation diameter of ≥15 mm was strongly associated with a successful EBD procedure. In a recently published retrospective analysis of CD-related intestinal strictures of patients undergoing EBD, a maximal dilatation size of 16 to 18 mm exhibited a longer interval between subsequent dilations, but were not more protective against future surgery.[19] In contrast, a study by Gustavsson et al[6] demonstrated that stricture dilatation of 25 mm was associated with a higher complications rate compared with one of ≤20 mm. We assume that our study did not find similar correlation because none of the strictures in our institution were dilated for over 20 mm.
Stricture characteristics which were negatively associated with EBD success included inflammation and the use of corticosteroid therapy at the time of EBD. Corticosteroid therapy was also positively associated with post-EBD perforation, while a fibrotic non-inflamed stricture was negatively associated with it. We assume that corticosteroid therapy was given to treat inflammation at the stricture site, which was also found to be associated with EBD failure and perforation. Likewise, all post-EBD perforations occurred in areas of active inflammation in a study by Singh et al,[20] and those authors concluded that inflammatory strictures might be prone to post-EBD perforation unlike fibrotic strictures. This possibility was further supported by a critical review of the literature by Makkar and Bo,[21] who suggested that active inflammation is associated with a higher risk of perforation. Long and inflamed strictures were associated with lower success rates of the EBD procedure among our study population, while dilatation of short and non-inflamed strictures were highly successful (94%), indicating that such cases would be most suitable for this procedure.
There are several limitations to our study. Primarily, the data extracted from the patients’ medical records and analyzed retrospectively raise a potential information bias. This bias was minimized by meticulous data collection by a single observer, and blinded validation of the data by an IBD specialist gastroenterologist. Also, data were extracted in a uniform manner, from consecutive patients’ files so this potential bias was non-differential. In a small number of cases, there was no documentation of stricture length or inflammatory state. Finally, data were gathered from a single center, and EBDs were conducted in a hospital setting, therefore referral filter bias may exist, limiting external validity.
Strengths of this study include a long follow-up of a relatively large cohort, who were all treated and followed by the same experienced and dedicated endoscopists. Data were collected in a uniform manner and blindly validated. Potential confounders were controlled by multivariate adjustment.
In conclusion, the results of this study indicate that the short-term success rates of an EBD procedure for strictures associated with CD are high. A successful EBD was negatively associated with corticosteroid therapy, and with long and inflamed strictures, and positively associated with a maximum dilatation diameter of ≥15 mm. Interestingly, a long stricture was not associated with perforations, the most common complication of EBD procedures. Prevention of surgery was associated with a successful EBD, and a short stricture. This may imply that long strictures, are determinants of both EBD success and long term need of surgery. These findings may assist in clinical allocation of CD patients to undergo an EBD rather than invasive surgery for the dilation of strictures, while lowering the risks of an unsuccessful procedure.
Author contributions
Conceptualization: Erez Scapa, Nitsan Maharshak.
Data curation: Ophir Winder, Erez Scapa, Henit Yanai, Sophie Barnes, Nitsan Maharshak.
Formal analysis: Naomi Fliss-Isakov, Gilad Winder.
Methodology: Erez Scapa, Nitsan Maharshak.
Validation: Naomi Fliss-Isakov.
Writing – original draft: Ophir Winder, Naomi Fliss-Isakov.
Writing – review & editing: Naomi Fliss-Isakov, Roy Dekel, Iris Dotan, Nitsan Maharshak.
Footnotes
Abbreviations: BMI = body mass index, CD = Crohn's disease, CI = confidence interval, CT = computed tomography, EBD = endoscopic balloon dilatation, HR = hazard ratio, IBD = inflamatory bowel disease, OR = odds ratio, SD = standard deviation.
OW and NFI have contributed equally and are first authors.
The authors have no conflicts of interest to disclose.
References
- [1].Freeman HJ. Natural history and long-term clinical course of Crohn's disease. World J Gastroenterol 2014;20:31–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Rieder F, Zimmermann EM, Remzi FH, et al. Crohn's disease complicated by strictures: a systematic review. Gut 2013;62:1072–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Olaison G, Smedh K, Sjödahl R. Natural course of Crohn's disease after ileocolic resection: endoscopically visualised ileal ulcers preceding symptoms. Gut 1992;33:331–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Paine E, Shen B. Endoscopic therapy in inflammatory bowel diseases (with videos). Gastrointest Endosc 2013;78:819–35. [DOI] [PubMed] [Google Scholar]
- [5].Ajlouni Y, Iser JH, Gibson PR. Endoscopic balloon dilatation of intestinal strictures in Crohn's disease: safe alternative to surgery. J Gastroenterol Hepatol 2007;22:486–90. [DOI] [PubMed] [Google Scholar]
- [6].Gustavsson A, Magnuson A, Blomberg B, et al. Endoscopic dilation is an efficacious and safe treatment of intestinal strictures in Crohn's disease. Aliment Pharmacol Ther 2012;36:151–8. [DOI] [PubMed] [Google Scholar]
- [7].Navaneethan U, Lourdusamy V, Njei B, et al. Endoscopic balloon dilation in the management of strictures in Crohn's disease: a systematic review and meta-analysis of non-randomized trials. Surg Endosc 2016;30:5434–43. [DOI] [PubMed] [Google Scholar]
- [8].Greener T, Shapiro R, Klang E, et al. Clinical outcomes of surgery versus endoscopic balloon dilation for stricturing Crohn's disease. Dis Colon Rectum 2015;58:1151–7. [DOI] [PubMed] [Google Scholar]
- [9].Arebi N, Hart AL, Thomas-Gibson S. A review of endoscopic balloon dilatation techniques for treating Crohn's strictures: time to standardise therapy. Expert Rev Gastroenterol Hepatol 2016;10:1101–7. [DOI] [PubMed] [Google Scholar]
- [10].Fumery M, Patel NS, Boland BS, et al. Efficacy and safety of endoscopic balloon dilatation of ileoanal pouch strictures. Inflamm Bowel Dis 2018;24:1316–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Lee HW, Park SJ, Jeon SR, et al. Long-term outcomes of endoscopic balloon dilation for benign strictures in patients with inflammatory bowel disease. Gut Liver 2018;12:530–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Baars JE, Theyventhiran R, Aepli P, et al. Double-balloon enteroscopy-assisted dilatation avoids surgery for small bowel strictures: a systematic review. World J Gastroenterol 2017;23:8073–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Singh A, Agrawal N, Kurada S, et al. Efficacy, safety, and long-term outcome of serial endoscopic balloon dilation for upper gastrointestinal Crohn's disease-associated Strictures-A Cohort Study. J Crohns Colitis 2017;11:1044–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Bossuyt P, Debeuckelaere C, Ferrante M, et al. Risk stratification for surgery in stricturing ileal Crohn's disease: The BACARDI risk model. J Crohns Colitis 2018;12:32–8. [DOI] [PubMed] [Google Scholar]
- [15].Bettenworth D, Gustavsson A, Atreja A, et al. A pooled analysis of efficacy, safety, and long-term outcome of endoscopic balloon dilation therapy for patients with stricturing Crohn's disease. Inflamm Bowel Dis 2017;23:133–42. [DOI] [PubMed] [Google Scholar]
- [16].Shivashankar R, Edakkanambeth Varayil J, Scott Harmsen W, et al. Outcomes of endoscopic therapy for luminal strictures in Crohn's disease. Inflamm Bowel Dis 2018;24:1575–81. [DOI] [PubMed] [Google Scholar]
- [17].Taida T, Nakagawa T, Ohta Y, et al. Long-term outcome of endoscopic Balloon dilatation for strictures in patients with Crohn's disease. Digestion 2018;98:26–32. [DOI] [PubMed] [Google Scholar]
- [18].Lan N, Stocchi L, Ashburn JH, et al. Outcomes of endoscopic balloon dilation vs surgical resection for primary ileocolic strictures in patients with Crohn's disease. Clin Gastroenterol Hepatol 2018;16:1260–7. [DOI] [PubMed] [Google Scholar]
- [19].Reutemann BA, Turkeltaub JA, Al-Hawary M, et al. Endoscopic balloon dilation size and avoidance of surgery in stricturing Crohn's disease. Inflamm Bowel Dis 2017;23:1803–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Singh VV, Draganov P, Valentine J. Efficacy and safety of endoscopic balloon dilation of symptomatic upper and lower gastrointestinal Crohn's disease strictures. J Clin Gastroenterol 2005;39:284–90. [DOI] [PubMed] [Google Scholar]
- [21].Makkar R, Bo S. Colonoscopic perforation in inflammatory bowel disease. Gastroenterol Hepatol (N Y) 2013;9:573–83. [PMC free article] [PubMed] [Google Scholar]


