Abstract
Objective
To examine (a) changes in parental involvement across early emerging adulthood, (b) whether yearly fluctuations in parental involvement were associated with adherence and glycated hemoglobin (HbA1c) over time, and (c) whether higher involvement was more beneficial for those with poorer executive function (EF).
Methods
A total of 228 high school seniors (M age = 17.76) with type 1 diabetes reported on mothers’ and fathers’ acceptance, knowledge of diabetes activities, disclosure to mothers and fathers regarding diabetes, and adherence at four yearly time points. At baseline, participants completed performance-based measures of EF. HbA1c was collected from assay kits.
Results
Growth curve models revealed significant declines in disclosure to fathers and mothers’ and fathers’ knowledge of diabetes activities; no changes were found in mothers’ or fathers’ acceptance nor disclosure to mothers. Multilevel models indicated significant between-person effects for nearly all aspects of parental involvement with more acceptance, knowledge, and disclosure associated with better HbA1c and adherence. Within-person effects for disclosure to fathers, and mothers’ and fathers’ knowledge indicated that in years when emerging adults perceived higher amounts of these types of involvement (compared with their own average), HbA1c was lower. Within-person effects were found for acceptance to mothers, disclosure to mothers and fathers, and mothers’ diabetes knowledge for adherence. Disclosure to fathers and mothers’ knowledge of diabetes activities were especially beneficial for HbA1c for those with poorer EF performance.
Conclusions
Parental involvement in diabetes management remains important during the high-risk time of emerging adulthood, especially for those with poorer EF.
Keywords: diabetes, family functioning, longitudinal research, neuropsychology, parents
Introduction
Emerging adulthood (ages 18–25) is thought to be an especially high-risk period for diabetes management (Weissberg-Benchell, Wolpert, & Anderson, 2007), due to numerous transitions and changing relationships with parents. Emerging adults experience many transitions such as beginning college, moving in and out of the parental home (Seiffge-Krenke, 2006), and becoming more responsible for their own care (Hanna, Weaver, Stump, Guthrie, & Oruche, 2014). Some emerging adults may find this greater responsibility for diabetes care cognitively demanding, as it involves planning to achieve diabetes goals (e.g., initiating blood glucose checks) in the face of competing interests.
Emerging adults may experience challenges in diabetes management as parental involvement in type 1 diabetes (T1D) continues to decline across adolescence (King, Berg, Butner, Butler, & Wiebe, 2014), with little known about what facets of parental involvement decline longitudinally across emerging adulthood. Three facets of parental involvement have been identified as consistently important across adolescence (Berg, Butner et al., 2017): (a) the warmth and acceptance of high-quality parent–child relationships, (b) how much adolescents disclose to parents about their diabetes management, and (c) the knowledge parents have about their child’s diabetes activities (often referred to as a facet of parental monitoring). Across adolescence, declines are seen in parental knowledge as well as in the warm and accepting quality of the relationship (King et al., 2014). No information is available regarding changes in adolescent disclosure about diabetes management over time. Maintenance in these aspects of parental involvement during adolescence are associated with better diabetes management (Helgeson et al., 2014; King et al., 2014). Research is only beginning to reveal that parental involvement may decline further across emerging adulthood, with individuals reporting that parents are less involved in problem-solving around diabetes after they graduate from high school (Majumder, Cogen, & Monaghan, 2017) and that parents are less responsible for diabetes tasks after high school (Hanna et al., 2014).
Though parental involvement might decrease across emerging adulthood (Lindell & Campione-Barr, 2017), a growing number of studies show that early emerging adults still benefit from parental involvement in their diabetes care. Both cross-sectional (Goethals et al., 2017; Helgeson et al., 2014) and longitudinal research (Luyckx & Seiffge-Krenke, 2009) suggests that higher quality relationships with parents are related to better diabetes management in emerging adults. In a cross-sectional study, Helgeson et al. (2018) found that emerging adults who reported parents were more knowledgeable about their diabetes had lower glycated hemoglobin (HbA1c). One way in which emerging adults may keep parents in the know about their diabetes is through disclosure of diabetes-related information (Osborn, Berg, Hughes., Pham, & Wiebe, 2013). On a daily basis, on days when late adolescents voluntarily disclosed diabetes information to their mothers (but not to their fathers) they showed better adherence and fewer self-regulation failures surrounding blood glucose checking (Berg, Queen et al., 2017). These results suggest both between- and within-person differences in parental involvement are associated with diabetes outcomes. Thus, in the present study, we examined both between-person differences in the accepting quality of parent–child relationships, parental knowledge, and disclosure to parents across early emerging adulthood as well as yearly within-person fluctuations in parental involvement to understand how aspects of parental involvement were associated with diabetes management.
Parental involvement may be especially beneficial for emerging adults whose executive function (EF) capacity is lower relative to peers, as they may be at highest risk for disruptions in diabetes management (Suchy et al., 2016). A growing literature indicates that EF is associated with adherence and HbA1c (see Duke & Harris, 2014) with longitudinal changes in parent’s perceptions of some aspects of EF associated with changes in adherence (Miller et al., 2013). In our previous work with the present sample, performance measures of EF were predictive of changes in HbA1c (while controlling for intelligence), but not adherence, over time (Berg et al., 2018). The more widely used self-report measure of EF (i.e., the BRIEF) was not associated with changes in HbA1c nor adherence. The type of planning, problem-solving, and consistent behavioral execution of tasks required for maintaining low HbA1c (measured by performance measures of EF) may be difficult for emerging adults to manage independently. Warm and accepting parental involvement may provide the context where greater daily involvement may be possible for emerging adults with lower EF. Further, parents’ greater knowledge of diabetes activities may be especially beneficial as it may buffer emerging adults’ EF weaknesses by monitoring adherence behaviors, offering reminders as needed, and encouraging activities that are consistent with and discouraging activities that are inconsistent with lower HbA1c.
The present study examined longitudinal changes in the warm and accepting quality of the mother and father-emerging adulthood relationship, disclosure to mothers and fathers, and mothers’ and fathers’ knowledge of diabetes activities. We also assessed whether yearly fluctuations in these aspects of parental involvement were associated with adherence and HbA1c over four yearly assessments, and whether higher parental involvement was more beneficial for adherence and HbA1c for emerging adults experiencing poorer EF. We expected that parental knowledge of diabetes activities would decline across time, continuing the prior declines demonstrated in the literature across adolescence (King et al., 2014); however, we expected maintenance of acceptance across time (Lindell & Campione-Barr, 2017). We did not have specific predictions about disclosure. We predicted that greater between- and within-person differences in parental involvement would be associated with better adherence and lower HbA1c, and that this relationship would be especially beneficial for early emerging adults with poorer EF abilities.
Methods
Participants
High school seniors with T1D were recruited for a longitudinal multisite study investigating the transition to early emerging adulthood from outpatient pediatric endocrinology clinics during clinic visits or by phone in two southwestern U.S. cities. Individuals were eligible if they had been diagnosed with T1D for at least 1 year (M time since diagnosis = 7.35 years, SD =3.88), used English as their primary language, were in their final year of high school, lived with a parent or parent figure at baseline (68.4% lived with both biological parents, 27.1% with one biological parent; 4.5% with adoptive parents or grandparents), would be able to have regular contact with parents over the subsequent 3 years, and had no condition that would prohibit study completion. Of the qualifying 507 individuals approached, 301 (59%) agreed to participate, of which 247 (49%) enrolled in the study (see Berg, Queen et al., 2017). At baseline, 236 participants had survey data and valid cognitive data. At baseline, 62% were female, 43% reported using an insulin pump, average HbA1c was 8.27 (SD = 1.62), 75.2% identified as non-Hispanic white, 14.2% as Hispanic, and 4.8% as African American.
Participants were followed every year (Time 2 N = 216, Time 3 N = 211, Time 4 N = 179), with the most common reason for withdrawal (19 total) that participants were too busy. Eight participants reported that they did not have a father figure to report on at any time point. To maintain consistent samples across mother and father analyses, these participants were dropped from analyses [thus the analyses include 228 participants (mean age = 17.76, SD = 0.39) at baseline].
Procedure
The study had IRB approval, with parents providing written consent and teens written consent or assent (later consented after they turned 18) at enrollment. EF and intelligence (IQ) were assessed in the laboratory and an online survey measured parental involvement and adherence. Participants were paid $50 for the first two and $75 for the last two assessments. At each time point, teens reported illness and demographic variables including whether they used an insulin pump (i.e., pump status) and whom they were living with. As extreme hyper- and hypoglycemia can affect cognitive performance (Desrocher & Rovet, 2004), blood glucose was checked prior to completing cognitive tests. If blood glucose was outside the range of 75 to 400 mg/dl, steps were taken to normalize blood glucose; cognitive testing was rescheduled for one participant who could not bring blood glucose in range. Blood glucose levels in the cognitive testing session were unrelated to EF and IQ (r values < .13, all p-values > .11).
Measures
Parental Involvement
Parental Relationship Quality. The five-item acceptance subscale from the Mother-Father-Peer (MFP) scale (Epstein, 1983) measured emerging adults’ perceptions of mothers’ and fathers’ communication of acceptance separately on a 1 (strongly disagree) to 5 (strongly agree) scale. Reliability in the present sample ranged from α = .81 to .87 for perceptions of acceptance from mothers and α =.81 to .90 for perceptions of fathers across the four time points.
Parental Knowledge. Emerging adults reported on parents’ knowledge of their diabetes activities via the six-item diabetes parental monitoring scale (Berg et al., 2008). Emerging adults reported separately how much their mothers and fathers “really” know about their diabetes care (e.g., blood sugar readings) on a 1 (doesn’t know) to 5 (knows everything) scale. Reliability in the present sample ranged from α = .94 to .95 for perceptions of mother and .94 to .96 for perceptions of father across the four time points.
Diabetes Disclosure. Emerging adults completed three diabetes disclosure items developed by Osborn et al. (2013) (e.g., “I spontaneously tell my [mother/father] about what is going on with my diabetes management”) on a 1 (strongly disagree) to 5 (strongly agree) scale. Separate ratings were obtained for mothers and fathers. Reliability ranged from α = .83 to .90 for perceptions of mother and .88 to .93 for perceptions of father across the four time points.
Executive Function
Performance-based EF was measured through four subtests of the Delis–Kaplan Executive Function System battery (Delis, Kaplan, & Kramer, 2001) at baseline, using widely recognized components of EF: Trail Making Test (Letter Number Sequencing Condition completion time), Color-Word Interference (Inhibition and Inhibition/Switching Condition completion times), Verbal Fluency (Letter and Category Conditions correct responses), and Design Fluency (correct responses for each of the three conditions). The mean of the eight norm-based age-corrected scaled scores (based on test manual; Delis et al., 2001) was computed to generate a single EF performance score. Cronbach’s alpha for this composite was .83.
Estimate of Intelligence
IQ was measured as a covariate to ascertain that the effect of EF could not be explained by intelligence. Individuals completed the Vocabulary subtest of the Wechsler Adult Intelligence Scale-Fourth Edition (Wechsler, 2008) as an estimate of crystallized IQ (Lezak, Howieson, Bigler, & Tranel, 2013); this sub-test correlates r = .91 to .92 with verbal IQ and .79 to .81 with Full Scale IQ in the present age group (Wechsler, 2008). Norm-based age-corrected scaled scores (Wechsler, 2008) were analyzed.
Diabetes Outcomes
Adherence
Emerging adults completed six (or seven if they were on a pump) items selected from the Self-Care Inventory (La Greca, Follansbee, & Skyler, 1990) to be those most recommended to measure adherence to diabetes tasks and to occur daily. Participants rated behaviors over the past month (1 = never did it to 5 = always did this as recommended without fail); average scores were analyzed (α ranged from .77 to 83 across the four time points).
Glycemic Control
HbA1c was obtained on the day of cognitive testing, and at later time points with HbA1c mail-in kits (processed by CoreMedica Laboratories, accredited by the College of American Pathologists; www.coremedica.net). This approach was chosen over obtaining HbA1c from medical records to ensure that HbA1c measures occurred on the day of cognitive testing, the same procedures were used across time points, and HbA1c could be obtained from those who were not under routine care. At baseline, the kit was completed after receiving instructions from an assistant who observed test completion. This measure was highly correlated with point-of-care HbA1c assays in medical records at baseline (r = .74, p < .001).
Analytic Plan
Missing data ranged for variables from a low of 0.8% to a high of 32%. To account for missing data, we generated 10 datasets through multiple imputation (MI) (Graham, 2009) estimating data for those missing a variable at a time point and for those who skipped a time point but remained in the study. MI was chosen over maximum likelihood (ML) estimation to be consistent with the systematic data approach in the larger study.
MI included variables beyond those in the present analyses across the four time points to ensure an adequate missing-at-random model and to account for the longitudinal nature of the data. Across all analyses, the lowest efficiency was 0.947, indicating that the 10 datasets adequately recovered the missing data.1
To examine changes in parental involvement across time, we estimated unconditional linear growth curve models separately for each measure of involvement in SPSS MIXED. We included random effects on the intercept and slope, with baseline coded as 0 (i.e., the intercept represented the mean value of the dependent variable at Time 1).
To examine whether yearly fluctuations in parental involvement were associated with changes in adherence and glycemic control, multilevel models estimated both within- and between-person effects of parental involvement (see Hoffman & Stawski, 2009) on adherence and HbA1c. Separate models were estimated for each form of mother and father involvement for each outcome, with person centering at Level 1 and grand centering at Level 2.
Finally, to examine whether parental involvement was most beneficial for individuals who at baseline had lower EF abilities, we tested whether EF moderated the within-person association of parental involvement and adherence or glycemic control (i.e., the β2i effect in equation below). IQ was included as a covariate on the intercept to assess how EF predicted changes in HbA1c and adherence over-and-above the effect of IQ. Additional covariates on the intercept included years since diagnosis, gender, ethnicity, and whether an individual was on a pump.2 The following equations display analyses for mothers’ knowledge predicting HbA1c.
Level 1 (within-person) equation:
Level 2 (between-person) equation:
Results
Changes in Parental Involvement Across Time
As can be seen in Table I, no significant changes were found in emerging adults’ reports of mothers’ or fathers’ acceptance, nor disclosure to mothers, across time. However, significant declines in paternal disclosure (−0.10) and parental knowledge (−0.26 mothers and −0.24 fathers) were observed over the 4-year period. These coefficients reflect modest changes in these aspects of parental involvement across time with the greatest change occurring in knowledge of diabetes activities (moving from 3.38 at baseline, reflecting knows something, to in-between knows a little and knows something after 4 years). Significant random effects for time were found for mothers’ acceptance only, indicating that there was variability in the slopes of maternal acceptance.
Table I.
Growth Curve Models of Parental Involvement Across Time
| Reports of mothers’ involvement | |||
|---|---|---|---|
| Acceptance | Disclosure | Diabetes knowledge | |
| estimate (SE) | estimate (SE) | estimate (SE) | |
| Fixed effects | |||
| Intercept | 4.36 (0.12)*** | 3.37 (0.15)*** | 3.38 (0.16)*** |
| Time | 0.02 (0.03) | −0.03 (0.03) | −0.26 (0.03)*** |
| Years since diagnosis | 0.004 (0.01) | −0.01 (0.02) | −0.02 (0.02) |
| Gendera | −0.08 (0.10) | −0.25 (0.12)* | 0.04 (0.13) |
| Ethnicityb | 0.24 (0.14) | 0.53 (0.17)** | 0.21 (0.19) |
| Pump status c | 0.06 (0.08) | −0.02 (0.09) | −0.05 (0.10) |
| IQ | 0.01 (0.02) | −0.04 (0.02)* | −0.06 (0.02)** |
| Random effects | |||
| Intercept | 0.29 (0.05)*** | 0.55 (0.07)*** | 0.65 (0.08)*** |
| Time | 0.03 (0.01)** | 0.02 (0.01) | 0.02 (0.01) |
|
| |||
| Reports of fathers’ involvement | |||
|
| |||
| Acceptance | Disclosure | Diabetes knowledge | |
|
| |||
| Fixed effects | estimate (SE) | estimate (SE) | estimate (SE) |
|
| |||
| Intercept | 4.31 (0.12)*** | 3.11 (0.16)*** | 2.89 (0.17)*** |
| Time | 0.02 (0.02) | −0.10 (0.03)*** | −0.24 (0.03)*** |
| Years since diagnosis | −0.003 (0.01) | −0.02 (0.02) | −0.04 (0.02)* |
| Gendera | −0.11 (0.10) | −0.07 (0.13) | 0.12 (0.14) |
| Ethnicityb | 0.08 (0.15) | 0.27 (0.19) | −0.13 (0.19) |
| Pump statusc | 0.09 (0.08) | 0.07 (0.10) | 0.04 (0.10) |
| IQ | 0.01 (0.02) | −0.06 (0.02)* | −0.07 (0.02)*** |
| Random effects | |||
| Intercept | 0.37 (0.06)*** | 0.66 (0.08)*** | 0.67 (0.08)*** |
| Time | 0.02 (0.01) | 0.02 (0.01) | 0.01 (0.01) |
−0.5 = female, 0.5 = male.
−0.5 = non-Hispanic, 0.5 = Hispanic.
−0.5 = multiple daily injections, 0.5 = pump.
p < .05, **p < .01, ***p < .001.
Links Between Changes in Parental Involvement and HbA1c Over Time
Significant between-person effects (Table II) were found for both mothers’ and fathers’ acceptance, such that individuals who perceived mothers and fathers as more accepting on average (mean across time) relative to others had lower HbA1c. No within-person effects were found for acceptance. No significant interaction occurred between reports of mothers’ or fathers’ acceptance and EF in predicting HbA1c.
Table II.
Multilevel Models Predicting HbA1c From Parental Involvement With EF as a Moderator
| Outcome: glycemic control |
|||
|---|---|---|---|
| Reports of mothers’ involvement |
|||
| Acceptance estimate (SE) | Disclosure estimate (SE) | Diabetes knowledge estimate (SE) | |
| Intercept | 8.35 (0.26)*** | 8.41 (0.26)*** | 8.50 (0.26)*** |
| Time | 0.31 (0.05)*** | 0.31 (0.05)*** | 0.23 (0.05)*** |
| Within-person parental involvement | −0.05 (0.11) | −0.12 (0.09) | −0.34 (0.09)*** |
| Between-person parental involvement | −0.50 (0.19)* | −0.35 (0.13)** | −0.26 (0.11)* |
| EF | −0.20 (0.06)** | −0.24 (0.06)*** | −0.25 (0.06)*** |
| Within-person parental involvement × EF | 0.04 (0.05) | 0.09 (0.04) | 0.09 (0.04)* |
| Years since diagnosis | 0.03 (0.03) | 0.03 (0.03) | 0.03 (0.03) |
| Gendera | 0.28 (0.21) | 0.25 (0.21) | 0.34 (0.21) |
| Ethnicityb | 0.36 (0.30) | 0.43 (0.30) | 0.31 (0.30) |
| Pump statusc | −0.38 (0.17)* | −0.38 (0.17)* | −0.39 (0.17)* |
| IQ | −0.04 (0.04) | −0.05 (0.04) | −0.05 (0.04) |
|
| |||
| Reports of fathers’ involvement | |||
|
| |||
| Intercept | 8.34 (0.26)*** | 8.44 (0.26)*** | 8.47 (0.27)*** |
| Time | 0.31 (0.05)*** | 0.29 (0.05)*** | 0.24 (0.05)*** |
| Within-person parental involvement | −0.14 (0.11) | −0.22 (0.08)* | −0.29 (0.10)** |
| Between-person parental involvement | −0.47 (0.16)** | −0.31 (0.11)** | −0.16 (0.11) |
| EF | −0.20 (0.06)** | −0.25 (0.06)*** | −0.24 (0.06)*** |
| Within-person parental involvement × EF | 0.02 (0.05) | 0.10 (0.04)* | 0.10 (0.05) |
| Years since diagnosis | 0.03 (0.03) | 0.03 (0.03) | 0.03 (0.03) |
| Gendera | 0.28 (0.21) | 0.31 (0.21) | 0.35 (0.21) |
| Ethnicityb | 0.30 (0.30) | 0.33 (0.30) | 0.23 (0.31) |
| Pump statusc | −0.37 (0.17)* | −0.35 (0.17)* | −0.36 (0.17)* |
| IQ | −0.04 (0.04) | −0.05 (0.04) | −0.05 (0.04) |
Note. EF = executive function; HbA1c = glycated hemoglobin.
−0.5 = female, .5 = male.
−0.5 = non-Hispanic, 0.5 = Hispanic.
−0.5 = Multiple daily injections, 0.5 = pump.
p < .05, **p < .01, ***p < .001.
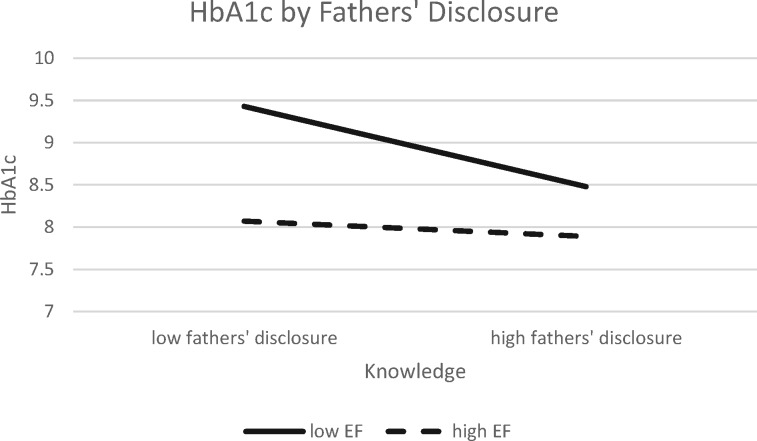
A similar analysis was conducted for disclosure to mothers and fathers (see Table II). Significant between-person effects were found for disclosure to both mothers and fathers, such that individuals who reported they disclosed more on average relative to others displayed lower HbA1c across the four time points. In addition, for fathers, a significant within-person effect was found, such that in years when individuals disclosed more to their fathers than their own average, they experienced lower HbA1c. A significant interaction was found between EF and disclosure to fathers. As can be seen in Figure 1, individuals who scored higher in EF (1 SD above the mean) displayed no association between disclosure to fathers and HbA1c (simple slopes analysis, p > .8). However, individuals who scored lower in EF (1 SD below the mean) displayed lower (better) HbA1c when they disclosed more to fathers (slope = −0.47, t = −4.07, p < .01). The interaction between EF and disclosure to mothers was marginal (p = .05) and was in the same direction as for fathers.
Figure 1.
Executive function moderates associations between disclosure to fathers and HbA1c. HbA1c = glycated hemoglobin.
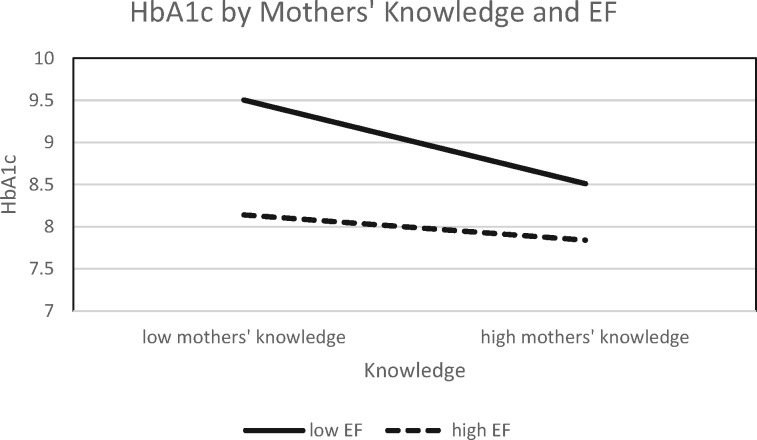
Finally, analyses were conducted examining whether mothers’ and fathers’ knowledge of diabetes activities predicted HbA1c. For mothers’ knowledge of diabetes activities, but not fathers, a significant between-person effect was found, such that individuals who reported that their mothers were more knowledgeable on average relative to others experienced lower HbA1c. For both reports of mothers’ and fathers’ knowledge, significant within-person effects were found, such that in years when individuals reported greater parental knowledge than their own average, they experienced lower HbA1c. Further, a significant interaction between mothers’ knowledge and EF occurred. As seen in Figure 2, individuals who scored higher in EF (1 SD above the mean) displayed no significant relation between mothers’ knowledge and HbA1c (p = .25). However, individuals who scored lower in EF (1 SD below the mean) displayed lower (better) HbA1c in years when mothers’ knowledge was higher (slope = −0.56, t = −4.075, p < .01). This interaction was marginally significant for reports of fathers’ knowledge (p = .06).
Figure 2.
Executive function moderates association between mothers’ knowledge and HbA1c. HbA1c = glycated hemoglobin.
Links Between Parental Involvement and Adherence Over Time
Similar analyses were conducted predicting adherence (Table III). EF did not interact with parental involvement in any analyses. For both mothers’ and fathers’ acceptance between-person associations were found between greater acceptance and higher adherence. For mothers, a within-person effect was found, such that greater acceptance than one’s average was associated with better adherence.
Regarding reports of disclosure (see Table III) to mothers and fathers, there were significant between- and within-person effects, such that greater disclosure to mothers and fathers on average across all time points was associated with better average adherence, and greater disclosure than one’s average was associated with better adherence.
Finally, for reports of mothers’ diabetes knowledge, both between- and within-person effects were found, but for fathers only a between-person effect was found. Greater average levels of mothers’ and fathers’ knowledge were associated with greater average adherence, and greater mothers’ knowledge than one’s average was associated with better adherence.3
Discussion
Changes in Parental Involvement During Early Emerging Adulthood
Across early emerging adulthood, parents’ knowledge about diabetes activities continues to decline, as does disclosure to fathers, but parental acceptance and disclosure to mothers remains stable. These findings extend Lindell and Campione-Barr’s (2017) review of parental involvement among emerging adults without diabetes to the diabetes context. Though individuals report that their parents are less knowledgeable about their diabetes, they still report disclosing aspects of their diabetes care to mothers consistently across early emerging adulthood. As processes of disclosure to mothers are initiated by the emerging adult, disclosure may be an important way in which individuals with diabetes elicit the support they need to effectively manage their diabetes.
Continued Importance of Parental Involvement for Diabetes Management
On average, individual differences in mothers’ and fathers’ acceptance and disclosure, as well as in mothers’ knowledge, were related to better HbA1c and adherence. These results extend the literature in adolescence linking warm and accepting parent-adolescent relationships, diabetes-specific knowledge, and disclosure to positive diabetes management to emerging adulthood (Berg, Butner, et al., 2017). Such results suggest that a foundation of good relationships with parents across childhood and adolescence carry forward to emerging adulthood, and continue to bolster positive health outcomes for those with diabetes (Berg, Butner, et al., 2017).
In addition to the average (between-person) effects, our results indicate that within-person fluctuations (within-person effects) in mothers’ and fathers’ knowledge, and in disclosure to fathers, may be important during emerging adulthood. In years when mothers’ and fathers’ knowledge and disclosure to fathers were above a person’s own average level, HbA1c was lower. In addition, in years when mothers’ knowledge and disclosure to mothers and fathers were above the person’s own average, adherence was better. These within-person effects are impressive in that they occur over-and-above the between-person effects. Thus, even for those individuals who are experiencing higher parental involvement overall, HbA1c and adherence are still better when emerging adults experience higher involvement. Such results indicate that parental involvement is still an important resource that aids emerging adults in adjusting to new challenges that are experienced during this high-risk time of development.
Parental Involvement Is Beneficial for Emerging Adults With Lower EF
Maternal knowledge, and disclosure to fathers, was especially beneficial to emerging adults experiencing lower EF performance. Executive functioning as assessed by performance tests is strongly related to the ability to correctly and consistently execute a variety of instrumental activities of daily living, including skills necessary to manage medical regimens (Stoehr et al., 2008). Those with lower EF performance may experience errors in planning and initiation that are detrimental for diabetes management (Suchy et al., 2016). Maternal knowledge and disclosure to fathers likely serve as buffers against these functional lapses as parents may intervene to help resolve T1D-related problems as they occur. Additionally, mothers who have more knowledge about their emerging adults’ T1D management likely also have more knowledge about other aspects of their emerging adult’s life. As a result, they may be in a position to help their emerging adults anticipate situations in which problems are likely to arise, and help them generate plans to circumvent or prevent lapses in health behaviors. In contrast, emerging adults whose EF is higher likely function on par with more mature adults, making support from a parent less crucial. Of note, although the range of EF scores in the “low EF” group falls between what would be clinically characterized as mildly impaired to low average, the majority of these emerging adults did not display clinical EF impairment.
The pattern of findings that maternal knowledge and disclosure to fathers were not beneficial for adherence differentially by EF, but were differentially associated with HbA1c, suggests that these aspects of parents’ involvement do not facilitate HbA1c primarily through their direct assistance with adherence behaviors. The parent–child relationship characterized by knowledge and open disclosure may be beneficial for those with lower EF through better anticipation of daily problems or through increasing the effectiveness of their adherence attempts.
The findings of the current study should be interpreted in the context of limitations. First, the nature of the parent-emerging adult relationship during this developmental transition was captured by three self-report measures that assessed key facets of parental involvement; however, we did not exhaustively measure parental involvement. Including other metrics of parental involvement, such as autonomy support and collaborative problem-solving (Nansel et al., 2009), may prove fruitful for understanding how parents foster diabetes management matched to the capabilities of the emerging adult. Second, the high correlations between perceptions of mothers’ and fathers’ involvement could account for some of the similarities in findings for mothers and fathers. The combined analyses, noted in the supplementary analyses, are suggestive that for emerging adults mothers’ and fathers’ involvement may be reflective of a more general “family” level of involvement across emerging adulthood. Inclusion of parents’ reports of their involvement may help in distinguishing the role of mothers and fathers, although emerging adults’ reports may be more predictive of diabetes outcomes than parents’ reports (Berg et al., 2008). Finally, while the current findings are in line with previous work highlighting the importance of EF in diabetes management (Goethals et al., 2017; Suchy et al., 2016), these findings may not generalize to other chronic illnesses with different cognitive demands related to self-care.
Conclusion
The present study provides compelling evidence for the importance of parents’ continued involvement in diabetes management during the high-risk time of early emerging adulthood. Clinicians who work with emerging adults may wish to draw on families as a resource for emerging adults by involving parents in clinic visits, or by assessing, encouraging, and facilitating emerging adults’ continued connection with parents through normalizing the involvement of parents at this time of development. Frequently, the message to late adolescents and parents in the pediatric care setting is that adolescents should be striving for independence in diabetes management activities as they prepare to transition from pediatric care. Our results suggest that a message of “keeping connected with parents” may be advantageous for emerging adults with lower EF. The task of keeping connected, however, may require interventions in how best to engage around diabetes management tasks, especially as parents and emerging adults are less frequently in the presence of each other. Technologies that keep parents “in the know” about their emerging adult’s diabetes management (e.g., sharing continuous glucose monitoring data) may also serve an important function to increase parental knowledge, possibly cuing emerging adults and parents to discuss diabetes management. Such interventions to promote higher engagement of parents in health care and ongoing illness management might begin in pediatric settings, and be an important component of how to transition successfully to adult care settings.
Supplementary Data
Supplementary data can be found at: https://academic.oup.com/jpepsy.
Supplementary Material
Acknowledgments
We thank the physicians and staff at the Primary Children’s Hospital Diabetes Program, Mountain Vista Medicine, Children’s Medical Center Dallas, and the emerging adults and parents who participated in this study.
Footnotes
As there is controversy as to whether to use MI versus ML to deal with missing data for longitudinal data, we verified that the results with MI reported here are consistent with ML. A ML analysis was conducted in Mplus Version 8, which replicated the pattern of significance for all results, with the exception of one interaction. As our MI approach did not completely account for the random slope or cross-level interaction, we also analyzed the data using BLIMP (Enders et al., 2018), which resulted in identical results as are reported here. Thus, there is convergence of results across different ways of handling missing data. We report the imputation in this paper that is consistent with the larger study.
We conducted analyses to see whether living in the parental home at times 2–4 was associated with outcomes or moderated the parental involvement effects on adherence or HbA1c. Living in the parental home was associated with lower perceptions of acceptance from father, and greater perceptions of both mothers’ and fathers’ knowledge of diabetes activities, but was not associated with any other dependent variable. Living in the parental home did not moderate any of the parental involvement effects or the parental involvement × EF interactions on adherence or HbA1c.
As correlations between mothers’ and fathers’ involvement ranged from 0.40 to 0.77 across time, we conducted an analysis with mother and father variables together predicting outcomes. The results (see Supplementary Table S2) indicated that in some analyses only one parent remains significant. However, such analyses should be interpreted with caution due to the large number of variables that are included and the intercorrelations among the independent variables.
Funding
This work was supported by the National Institute of Diabetes and Digestive and Kidney Diseases at the National Institutes of Health (Grant Number R01 DK092939). The methods of this study are based on a study first reported in Berg et al. (2014), Journal of Pediatric Psychology.
Conflicts of interest: None declared.
References
- Berg C. A., Butler J. M., Osborn P., King G., Palmer D. L., Butner J., Wiebe D. J. (2008). Role of parental monitoring in metabolic control of type 1 diabetes. Diabetes Care, 31, 678–683. doi:10.2337/dc07-1678 [DOI] [PubMed] [Google Scholar]
- Berg, C. A., Butner, J., Wiebe, D. J., Hughes, A. E., Osborn, P., King, P. S., Palmer, D. L., & Butler, J. M. (2017). Developmental model of parent-child coordination for self-regulation in type 1 diabetes management across childhood and into emerging adulthood. Developmental Review, 46, 1–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg, C. A., Wiebe, D. J., Suchy, Y., Hughes, A. E., Anderson, J. Godbey, E., Butner, J., Tucker, C., Franchow, E. I., Pihlaskari, A. K., King, P., Murray, M. A., White, P. C. (2014) Individual differences and day-to-day fluctuations in perceived self-regulation associated with daily adherence in teens with type 1 diabetes. Journal of Pediatric Psychology, 39, 1039–1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg C. A., Queen T. L., Butner J. E., Turner S. L., Lansing A. H., Main A., Wiebe D. J. (2017). Adolescent disclosure to parents and daily management of type 1 diabetes. Journal of Pediatric Psychology, 42, 75–84. doi:10.1093/jpepsy/jsw056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg, C. A., Wiebe, D. J., Suchy, Y., Turner, S. L., Butner, J., Munion, A., Lansing, A. H., White, P., Murray, M. (2018). Executive function predicting change in type 1 diabetes management during the transition into emerging adulthood. Diabetes Care, 41 (11), 2281–2288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delis D. C., Kaplan E., Kramer J. H. (2001). Delis-Kaplan executive function system: Examiner's Manual. (D-KEFS ) San Antonio, TX: Psychological Corporation. [Google Scholar]
- Desrocher M., Rovet J. (2004). Neurocognitive correlates of type 1 diabetes mellitus in childhood. Child Neuropsychology, 10, 36–52. doi:10.1076/chin.10.1.36.26241 [DOI] [PubMed] [Google Scholar]
- Duke D. C., Harris M. A. (2014). Executive function, adherence, and glycemic control in adolescents with type 1 diabetes: A literature review. Current Diabetes Reports, 14, 532..doi:10.1007/s11892-014-0532-y [DOI] [PubMed] [Google Scholar]
- Enders C. K., Keller B. T., Levy R. (2018). A fully conditional specification approach to multilevel imputation of categorical and continuous variables. Psychological Methods, 23, 298–317. doi:10.1037/met0000148 [DOI] [PubMed] [Google Scholar]
- Epstein S. (1983). Scoring and interpretation of the Mother-Father-Peer scale ( Unpublished manuscript; ) Amherst, MA. [Google Scholar]
- Goethals E. R., Oris L., Soenens B., Berg C. A., Prikken S., Van Broeck N., Luyckx K. (2017). Parenting and treatment adherence in type 1 diabetes throughout adolescence and emerging adulthood. Journal of Pediatric Psychology, 42, 922–932. doi:10.1093/jpepsy/jsx053 [DOI] [PubMed] [Google Scholar]
- Graham J. W. (2009). Missing data analysis: Making it work in the real world. Annual Review of Psychology, 60, 549–576. doi:10.1146/annurev.psych.58.110405.085530 [DOI] [PubMed] [Google Scholar]
- Hanna K. M., Weaver M. T., Stump T. E., Guthrie D., Oruche U. M. (2014). Emerging adults with type 1 diabetes during the first year post-high school: Perceptions of parental behaviors. Emerging Adulthood, 2, 128–137. doi:10.1177/2167696813512621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helgeson V. S., Palladino D. K., Reynolds K. A., Becker D., Escobar O., Siminerio L. (2014). Early adolescent relationship predictors of emerging adult outcomes: Youth with and without type 1 diabetes. Annals of Behavioral Medicine, 47, 270–279. doi:10.1007/s12160-013-9552-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helgeson V. S., Vaughn A. K., Seltman H., Orchard T., Becker D., Libman I. (2018). Relation of parent knowledge to glycemic control among emerging adults with type 1 diabetes: A mediational model. Journal of Behavioral Medicine, 41, 186–194. doi:10.1007/s10865-017-9886-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman L., Stawski R. S. (2009). Persons as contexts: Evaluating between-person and within-person effects in longitudinal analysis. Research in Human Development, 6, 97–120. doi:10.1080/15427600902911189 [Google Scholar]
- King P. S., Berg C. A., Butner J. E., Butler J. M., Wiebe D. J. (2014). Longitudinal trajectories of parental involvement in type 1 diabetes and adolescents’ adherence. Health Psychology, 33, 424–432. doi:10.1037/a0032804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Greca A. M., Follansbee D., Skyler J. S. (1990). Developmental and behavioral aspects of diabetes management in youngsters. Children’s Health Care, 19, 132–139. doi:10.1207/s15326888chc1903_1 [Google Scholar]
- Lezak M. D., Howieson D. B., Bigler E. D., Tranel D. (2013). Neuropsychological assessment (5th edn). New York, NY:Oxford University Press. [Google Scholar]
- Lindell A. K., Campione-Barr N. (2017). Continuity and change in the family system across the transition from adolescence to emerging adulthood. Marriage and Family Review, 53, 388–416. doi:10.1080/01494929.2016.1184212 [Google Scholar]
- Luyckx K., Seiffge-Krenke I. (2009). Continuity and change in glycemic control trajectories from adolescence to emerging adulthood: relationships with family climate and self-concept in type 1 diabetes. Diabetes Care, 32, 797–801. doi:10.2337/dc08-1990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majumder E., Cogen F. R., Monaghan M. (2017). Self-management strategies in emerging adults with type 1 diabetes. Journal of Pediatric Health Care, 31, 29–36. doi:10.1016/j.pedhc.2016.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller M. M., Rohan J. M., Delamater A., Shroff-Pendley J., Dolan L. M., Reeves G., Drotar D. (2013). Changes in executive functioning and self-management in adolescents with type 1 diabetes: A growth curve analysis. Journal of Pediatric Psychology, 38, 18–29. doi:10.1093/jpepsy/jss100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nansel T. R., Rovner A. J., Haynie D., Iannotti R. J., Simons-Morton B., Wysocki T., Laffel L. (2009). Development and validation of the collaborative parent involvement scale for youths with type 1 diabetes. Journal of Pediatric Psychology, 34, 30–40. doi:10.1093/jpepsy/jsn058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osborn P., Berg C. A., Hughes A. E., Pham P., Wiebe D. J. (2013). What mom and dad don’t know CAN hurt you: Adolescent disclosure to and secrecy from parents about type 1 diabetes. Journal of Pediatric Psychology, 38, 141–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seiffge-Krenke I. (2006). Leaving home or still in the nest? Parent-child relationships and psychological health as predictors of different leaving home patterns. Developmental Psychology, 42, 864–876. [DOI] [PubMed] [Google Scholar]
- Stoehr G. P., Lu S. Y., Lavery L., Bilt J.V., Saxton J. A., Chang C. C. H., Anguli M. (2008). Factors associated with adherence to medication regimens in older primary care patients: The steel valley seniors survey. American Journal Geriatric Pharmacotherapy, 6, 255–263. doi:10.1016/j.amjopharm.2008.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suchy, Y. Turner, S. L., Queen, T. L., Durracio, K., Wiebe, D., J., Butner, J., & ... Berg, C. A. (2016). The relation of questionnaire and performance-based measures of executive functioning with type 1 diabetes outcomes among late adolescents. Health Psychology, 35, 661–669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. (2008). Wechsler Adult Intelligence Scale (4th edn). San Antonio, TX: Pearson. [Google Scholar]
- Weissberg-Benchell J., Wolpert H., Anderson B. J. (2007). Transitioning from pediatric to adult care: A new approach to the post-adolescent young person with type 1 diabetes. Diabetes Care, 30, 2441–2446. doi:10.2337/dc07-1249 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.