Abstract
This study was to investigate the incidence and the risk factors of postpartum stress urinary incontinence (SUI), and the effect of comprehensive care and rehabilitation program (CCRP) on preventing postpartum SUI.
In stage I, 479 puerperae were recruited within 1 week postpartum, then the postpartum SUI incidence at 8th week and its risk factors were investigated. In stage II, 240 vaginal delivery puerperae were enrolled within 1 week postpartum and randomly assigned to CCRP group or control group as 1:1 ratio. The postpartum SUI incidence and pelvic floor muscle function indexes were evaluated at 8th week.
In stage I, the postpartum SUI incidence was 25.7%, and SUI puerperae presented with higher body mass index (BMI), vaginal delivery rate, newborn weight, and larger newborn head diameter compared with non-SUI puerperae. Besides, the vaginal delivery, the elevated age and BMI were independent risk factors for postpartum SUI. In stage II, the postpartum SUI incidence in CCRP group was decreased compared with control group, and the vaginal resting pressure, vaginal squeezing pressure, and vaginal contraction duration were increased in CCRP group compared to control group at 8th week postpartum.
The incidence of postpartum SUI is 25.7%, and the vaginal delivery, increased age, and BMI are independent risk factors for postpartum SUI. More importantly, CCRP strengthens pelvic floor muscle functions and decreases postpartum SUI incidence in puerperae.
Keywords: comprehensive care and rehabilitation program, healthy education, pelvic floor muscle training, puerperae, stress urinary incontinence
1. Introduction
Postpartum stress urinary incontinence (SUI) is a common disease with a prevalence ranging from 4.8% to 35.6%.[1–4] Due to the insufficient support of pelvic floor fascia of postpartum SUI puerperae, the urine easily flows through the urethra when the intraabdominal pressure increases (when coughing, laughing, exercising, sneezing, and so on), resulting in the leakage of urine.[5,6] Although postpartum SUI is not a life-threatening disease, it greatly decreases quality of life and daily activities of puerperae.[7] More importantly, postpartum SUI causes dramatic psychologic disorders to puerperae such as low self-esteem, anxiety, and depression.[6,8] There are a number of treatment options for postpartum SUI including surgical and conservative ones, whereas these treatments are painful, costly or labor-consuming, and sometimes they may bring in other complications as well.[9,10] Therefore, illuminating the risk factors of postpartum SUI and exploring the potential approaches to prevent the occurrence of postpartum SUI are greatly important to minimize its negative impacts on puerperae.
Several approaches contribute to preventing postpartum SUI.[11–15] For instance, pelvic floor muscle training (PFMT) is able to strengthen the functions of pelvic floor muscle which then inhibits the incontinence.[10,16,17] And healthy education eliminates misunderstandings of postpartum SUI for puerperae and alleviates their fear and anxiety, which contribute to decreasing postpartum SUI risk.[12,13] In addition, psychologic counseling improves psychologic state of puerperae and regular supervision enhances the effect of PFMT, both of which are beneficial for postpartum SUI prevention.[14,15] Taken together, a comprehensive care program that includes PFMT, healthy education, psychologic counseling and regular supervision might be effective in preventing postpartum SUI. However, no such programs have been reported, and the effect of the comprehensive care program on preventing postpartum SUI remains to be determined. To this end, we designed a comprehensive care and rehabilitation program (CCRP) for puerperae, which included intensive healthy education, detailed guidance of PFMT, psychologic counseling, and regular supervision. And the objective of this study was to investigate the incidence and the risk factors of postpartum SUI, and to explore the effect of CCRP on preventing postpartum SUI and strengthening pelvic floor muscle functions.
2. Methods
2.1. Study design
This study consisted of 2 stages. In the stage I, a total of 479 puerperae with singleton-term delivery were recruited within 1 week after delivery, and the incidence of postpartum SUI at the 8th week and the risk factors of postpartum SUI were investigated. In the stage II, there were 240 eligible puerperae with singleton-term vaginal delivery being enrolled in the study within 1 week after delivery, and they were randomly assigned to a CCRP group or a control group. And 6-week CCRP was given to the puerperae in the CCRP group, and the usual guidance was given to the women in the control group, then the effect of CCRP on the prevention of postpartum SUI was assessed.
2.2. Participants
In the stage I, 479 puerperae giving birth in the Tongji Hospital, Tongji University School of Medicine between January 2015 and December 2016 were recruited. The inclusion criteria were: singleton term delivery; bladder pressure was normal; and no neurologic bladder dysfunction. The exclusion criteria were: age younger than 18 years old; history of SUI; prenatal urinary incontinence; urinary tract infection or kidney disease; and tumors in the genital area. In the stage II, 240 puerperae with vaginal delivery within 1 week after delivery in the hospital were enrolled, and they were also required to meet following criteria: singleton term vaginal delivery; able to perform a correct pelvic floor muscle contraction, which was judged by the obstetrician; age above 18 years; bladder pressure was normal and no neurologic bladder dysfunction; no history of SUI or prenatal urinary incontinence; no urinary tract infection or kidney disease; and without tumors in the genital area. The current study was approved by the Ethics Committee of the Tongji Hospital, Tongji University School of Medicine, and all enrolled puerperae provided the written informed consents.
2.3. Baseline data collection
Both in the stage I and stage II, puerperae’ baseline characteristics were collected using questionnaires after enrollment, which included age, body mass index (BMI), mode of delivery (vaginal delivery or caesarean section), puerperal type (primiparous or multiparous) previous delivery times, labor duration, newborn gender, newborn weight, and newborn head diameter.
2.4. Assessment of postpartum SUI
According to the criteria of International Continence Society (ICS), the SUI was defined as the complaint of involuntary leakage on effort or exertion or on sneezing or coughing.[18] At the 8th week (both in the stage I and stage II), puerperae were asked, “have you leaked even small amounts of urine when you were coughing, sneezing, laughing, or lifting in the past weeks,” and they were classified as SUI if they responded “yes.”[19]
2.5. Sample size calculation in the stage II
The sample size calculation in the stage II was based on the incidence of postpartum SUI in vaginal delivery puerperae in the stage I. We assumed 15% reduction of postpartum SUI incidence in the CCRP group compared with control group. And using a power of 95% and a 2-sided 5% level of significance (α), required sample size was 98 in each group. Considering at least 15% loss to follow-up, the sample size was inflated to 120 puerperae in each group with a total sample size of 240.
2.6. Randomization in the stage II
In the stage II, eligible puerperae were randomly allocated to the CCRP group (N = 120) or control group (N = 120) with a 1:1 ratio by an independent nurse according to a randomization code list, which was created by an analyst using block randomization method. Randomization sequence was created using Stata 9.0 (StataCorp, College Station, TX) statistical software.
2.7. Intervention for CCRP group in the stage II
As for puerperae in the CCRP group, postpartum educational materials were given to them before being discharged from the hospital, and the CCRP was performed in the 2nd week after delivery, which was conducted weekly for a total of 6 weeks and consisted of 4 parts: intensive healthy education, detailed guidance of PFMT, psychologic counseling, and regular supervision.
-
(1)
Intensive healthy education: the puerperae were given the postpartum educational materials after enrollment and were asked to visit the nurse weekly for receiving the educational sessions in the hospital. Each session lasted for 30 minutes containing following 2 aspects: detailed instructions of each item in the health educational materials; knowledge of SUI, the function and structure of the pelvic floor, the effect of childbirth on the pelvic floor, perineal care, good bladder habits, and instructions about avoiding constipation.
-
(2)
Detailed guidance of PFMT: following each healthy education session, the puerperae were given detailed demonstration of PFMT procedures for 30 minutes, and they were asked to exercise three times per day at home. And the details of PFMT were as follows: the exercise started with a near maximal pelvic floor muscle contractions held for 6 to 8 seconds and ended with 3 or 4 fast contractions; the exercises were repeated in lying, sitting, kneeling, and standing positions with legs apart to emphasize the pelvic floor muscles and to help relax the other muscles; and a set of exercises consisted of 12 times maximal pelvic floor muscle contractions.
-
(3)
Psychologic counseling: for the puerperae with psychologic problems (e.g., postpartum depression), nurse would communicate with the them sincerely after each session and attempt to listen, understand, comfort, sympathy, support, and help them manage the negative emotion.
-
(4)
Regular supervision: at the initiation of CCRP, each puerpera was given a poster and sticky red dots to place in relevant places at home (to serve as reminders to do the PFMT) and a manual for recording times of PFMT. At each weekly visit, except for giving the educational sessions to the puerperae, the nurse performed a vaginal palpation to puerperae for correcting the exercise of contraction of the pelvic floor muscles, inquired puerperae how often they practiced the PFMT, reviewed the records of PFMT, and encouraged them to keep exercising.
2.8. Intervention for the control group in the stage II
In the stage II, puerperae in control group were given usual guidance before discharge from hospital, which included healthy education as well as instructions of PFMT. The healthy education was carried out according to the postpartum educational materials (as same as CCRP group) containing postpartum attentions, diet and nutrition, emotion management, puerperal hygiene, postpartum activities and rest, breast care, SUI, contraception, return visit, as well as infant care. As for puerperae who were interested in PFMT, nurses provided more in-depth guidance about PFMT for them.
2.9. Measurement of pelvic floor muscle function in the stage II
In the stage II, puerperae’ pelvic floor muscle function indexes including vaginal resting pressure (VRP), vaginal squeezing pressure (VSP), and vaginal contraction duration (VCD) were measured at the 2nd week (week 2) and 8th week (week 8) after delivery using Phenix Pelvic Floor Rehabilitation Instrument (Shanshan Medical Apparatus & Instruments Industry Co, Ltd, Guangzhou, Guangdong, China).
2.10. Statistical analysis
All 240 puerperae were included in the final analysis in stage II based on the intention-to-treat (ITT) principle with the last observation carried forward (LOCF) method for the missing data. All analyses in the present study were performed by use of SPSS 21.0 statistical software (SPSS Inc, Chicago, IL), and all figures were made using GraphPad Prism 7.02 software (GraphPad Software Inc, San Diego, CA). Quantitative data were expressed as mean value ± standard deviation and determined by t test; qualitative data were described as count (percentage) and determined by Chi-squared test. Factors affecting postpartum SUI were determined by univariate and multivariate logistic regression analyses. P-value <.05 was considered significant.
3. Results
3.1. Study flow in stage I
A total of 610 puerperae were screened after delivery, among whom 59 puerperae were excluded due to the following reasons: 34 puerperae were unwilling to participate, 18 puerperae were ineligible, and 7 puerperae disagreed to sign informed consents (Fig. 1). Subsequently, the remaining 551 puerperae were recruited within 1 week after delivery, and postpartum SUI was assessed at week 8. Due to that 72 puerperae lost to participate in postpartum SUI assessment, 479 puerperae were included in the final analysis (Fig. 1).
Figure 1.
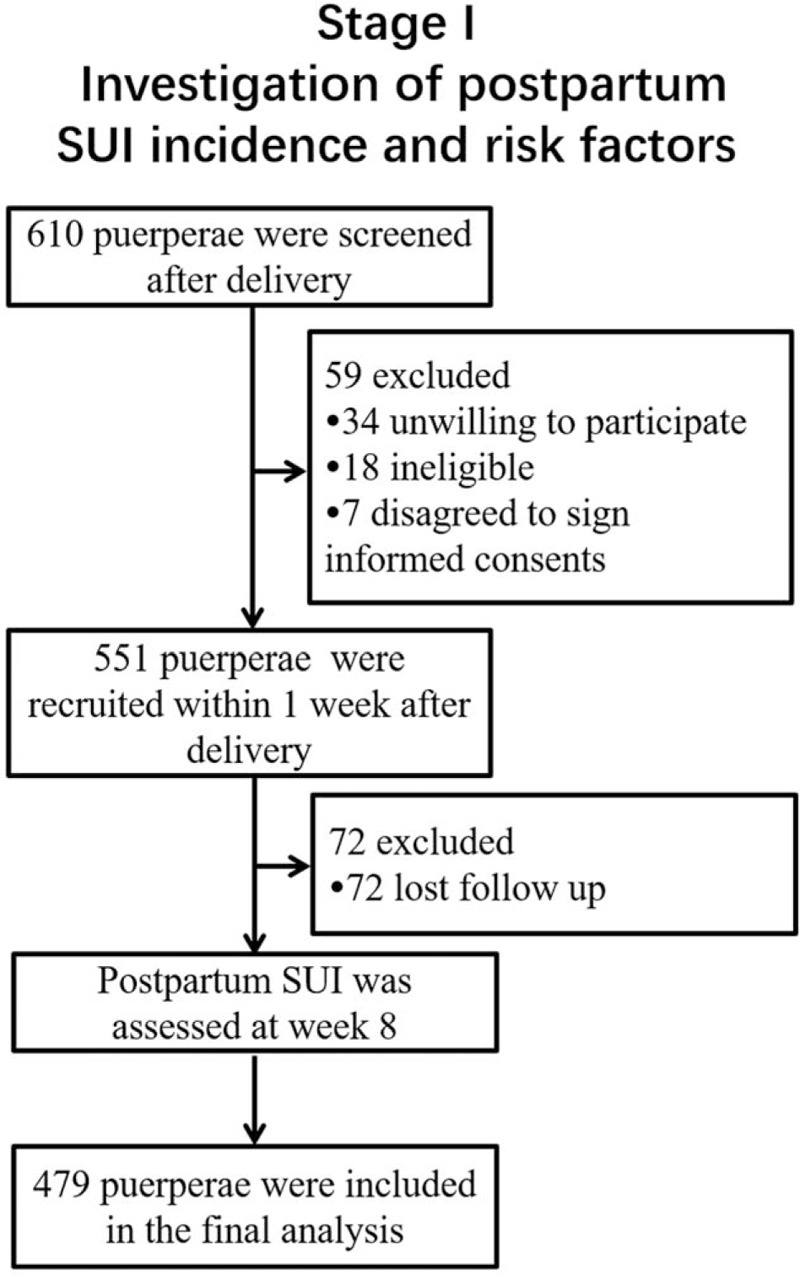
Study flow in stage I.
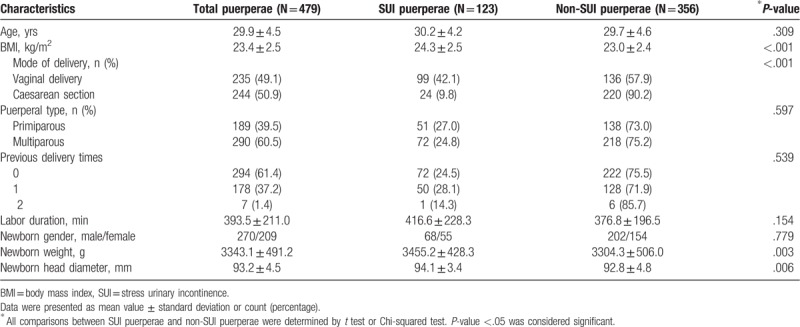
3.2. Characteristics of puerperae in stage I
Mean age and BMI of total puerperae (N = 479) were 29.9 ± 4.5 years and 23.4 ± 2.5 kg/m2, respectively, and 235 (49.1%) puerperae underwent vaginal delivery while 244 (50.9%) puerperae underwent caesarean section (Table 1). Among the 479 puerperae, 123 (25.7%) puerperae occurred postpartum SUI which were then allocated into SUI puerperae group, and the other 356 (74.3%) puerperae did not occurred postpartum SUI which were then allocated into non-SUI puerperae group. And SUI puerperae group exhibited increased BMI (P < .001), vaginal delivery rate (P < .001), newborn weight (P = .003), and newborn head diameter (P = .006), but similar age (P = .309), puerperal type (P = .597), previous delivery times (P = .539), labor duration (P = .154), and newborn gender (P = .779) compared with non-SUI puerperae group. Other detailed characteristics of puerperae are depicted in Table 1.
Table 1.
Puerperae’ characteristics in stage I.
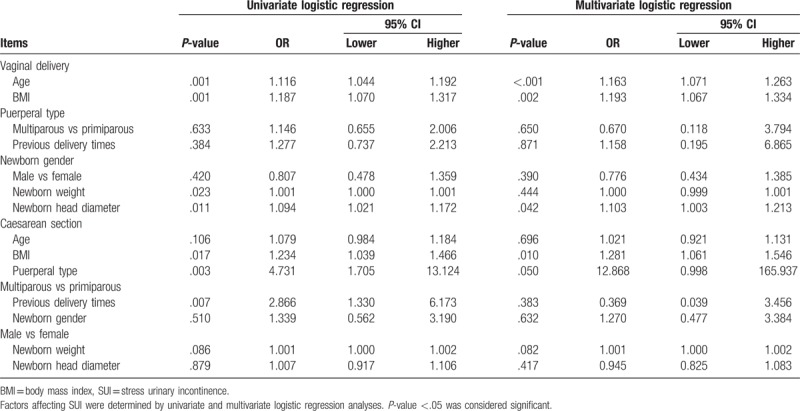
3.3. Analysis of factors affecting postpartum SUI by logistic regression model
Analysis of factors affecting postpartum SUI by univariate logistic regression revealed that the vaginal delivery (P < .001) and the increased BMI (P < .001), newborn weight (P = .004), as well as newborn head diameter (P = .007) were associated with higher probability of postpartum SUI. All factors were further analyzed via multivariate logistic regression, which showed that the vaginal delivery (P < .001) and the elevated age (P = .001) and BMI (P < .001) were independent risk factors for postpartum SUI (Table 2).
Table 2.
Analysis of factors affecting SUI.
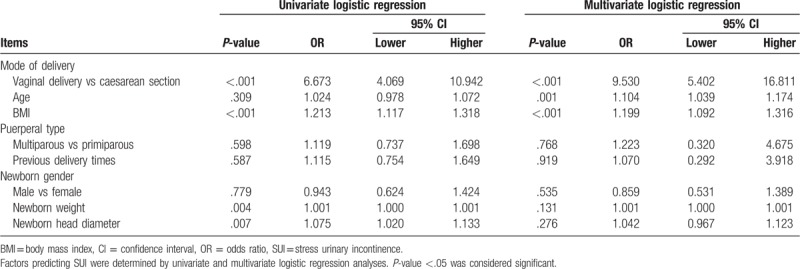
3.4. Analysis of factors affecting postpartum SUI by logistic regression model in vaginal delivery puerperae and caesarean section puerperae, respectively
For vaginal delivery puerperae, univariate logistic regression model analysis revealed that the elevated age (P = .001), BMI (P = .001), newborn weight (P = .023), and newborn head diameter (P = .011) were correlated with increased probability of postpartum SUI. Multivariate logistic regression model analysis showed that the higher age (P < .001), BMI (P = .002), and newborn head diameter (P = .042) were independent risk factors for postpartum SUI. For caesarean section puerperae, the increased BMI (P = .017), multiparous (P = .003), and previous delivery times (P = .007) were associated with elevated probability of postpartum SUI, and the higher BMI (P = .010) and multiparous (P = .050) were independent risk factors for postpartum SUI (Table 3).
Table 3.
Analysis of factors affecting SUI in vaginal delivery puerperae and caesarean section puerperae.
3.5. Study flow in stage II
A total of 362 puerperae with vaginal delivery were invited, whereas 76 puerperae refused to participate, then the remaining 286 puerperae were screened (Fig. 2). During the screening procedure, 31 puerperae were ineligible and 15 puerperae disagreed to sign informed consents. Subsequently, 240 puerperae were recruited within 1 week after delivery and randomized into CCRP group and control group as 1:1 ratio. In CCRP group, puerperae received CCRP at week 2 then postpartum SUI was assessed at week 8 after delivery, and 6 puerperae lost to follow-up during this period. In control group, puerperae received usual guidance before discharge from hospital then postpartum SUI was assessed at week 8 after delivery, and 9 puerperae lost to follow-up during this period. At last, all 120 puerperae in CCRC group and 120 puerperae in control group were included in the analysis based on the ITT principle (Fig. 2).
Figure 2.
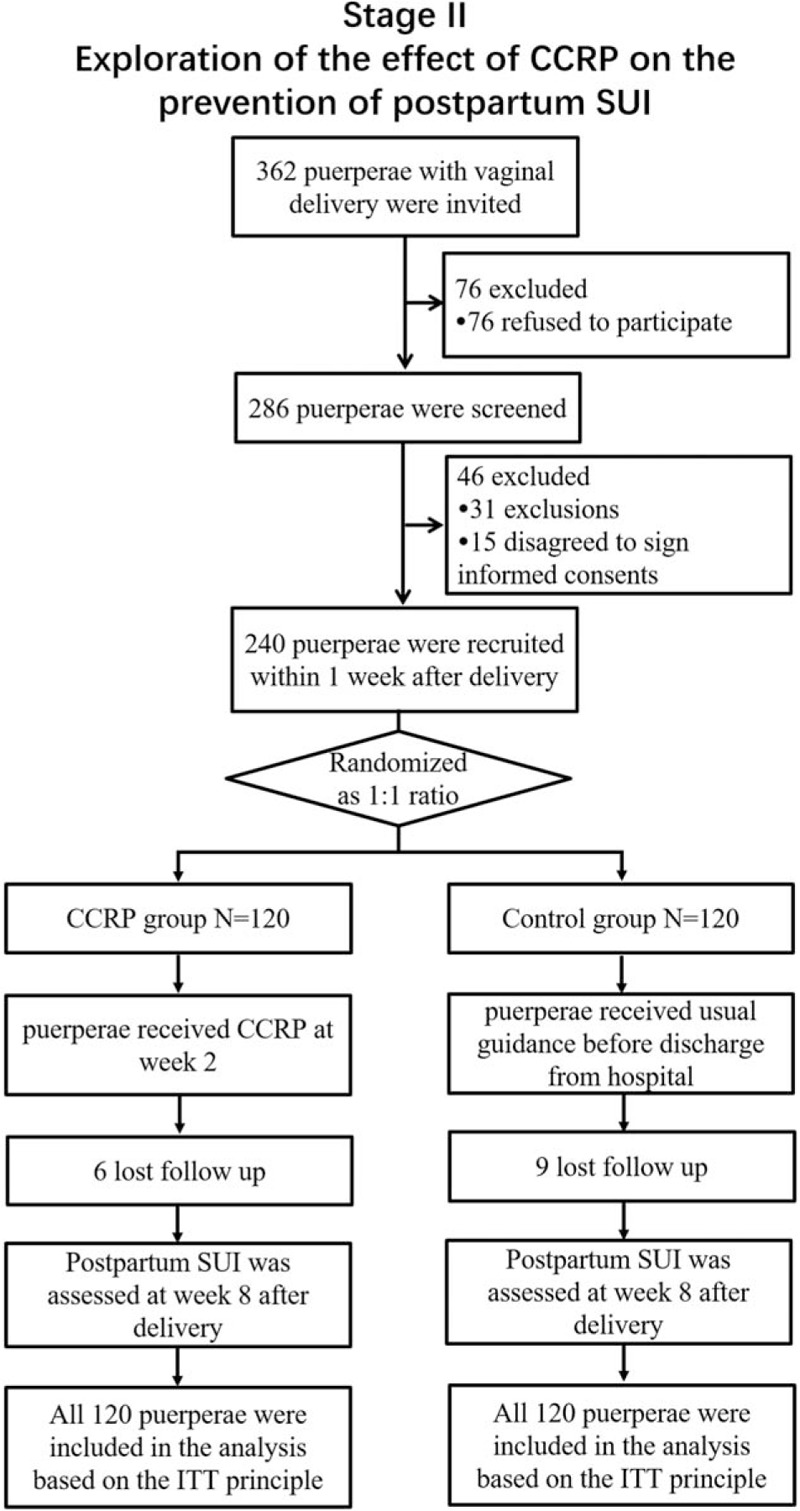
Study flow in stage II.
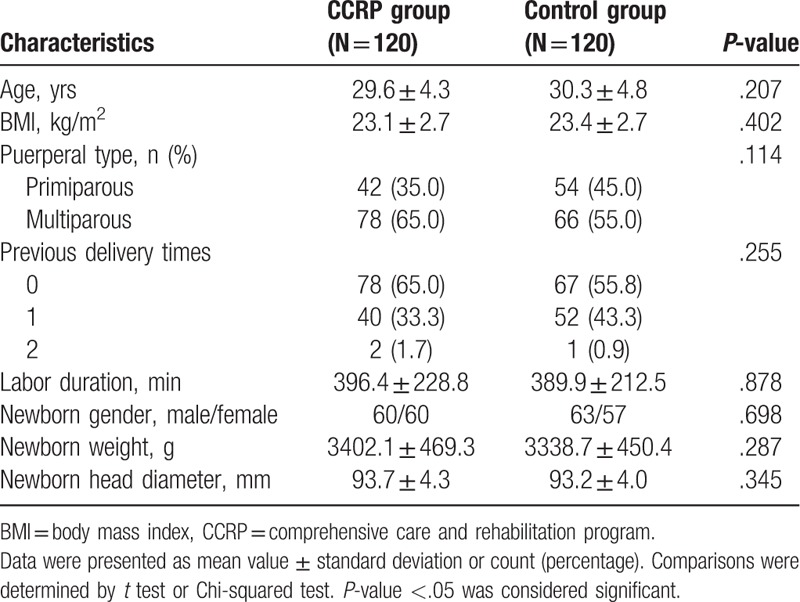
3.6. Baseline characteristics of vaginal delivery puerperae in stage II
In CCRP group, mean age and BMI were 29.6 ± 4.3 years and 23.1 ± 2.7 kg/m2, and the numbers of primiparous puerperae and multiparous puerperae were 42 (35.0%) and 87 (65.0%), respectively (Table 4). In control group, mean age and BMI were 30.3 ± 4.8 years and 23.4 ± 2.7 kg/m2, and the numbers of primiparous puerperae and multiparous puerperae were 54 (45.0%) and 66 (55.0%), respectively. No difference of baseline characteristics between the 2 groups was discovered (all P > .05, Table 4).
Table 4.
Characteristics of puerperae with vaginal delivery in stage II.
3.7. Comparison of postpartum SUI incidence between CCRP group and control group in stage II
The incidence of postpartum SUI was decreased in CCRP group (15.0%) compared with control group (31.7%) after the interventions (P = .002, Fig. 3).
Figure 3.
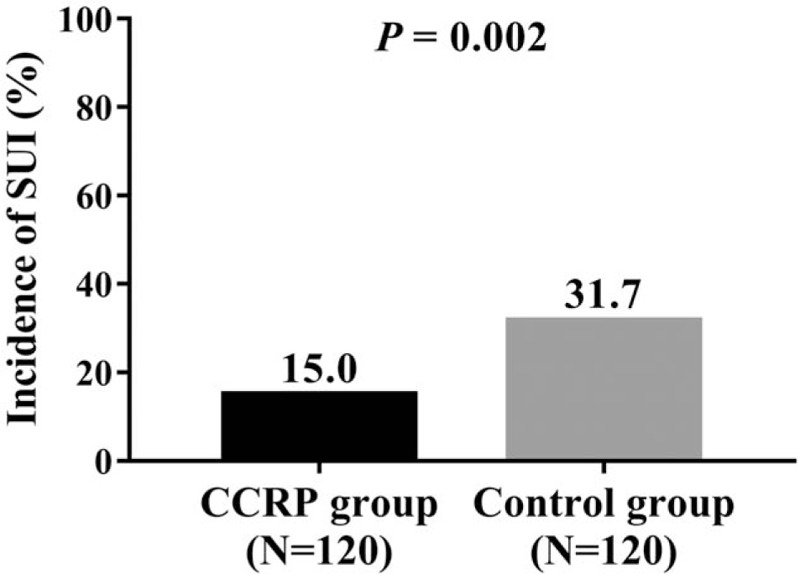
Comparison of postpartum SUI incidence between 2 groups in stage II. Postpartum SUI incidence in CCRP group was reduced compared with control group. Comparison between 2 groups was determined by Chi-squared test. P < .05 was considered significant. SUI = stress urinary incontinence, CCRP = comprehensive care and rehabilitation program.
3.8. Comparison of VRP, VSP, and VCD between CCRP group and control group at week 2 and week 8
At week 2, VRP (P = .741, Fig. 4A), VSP (P = .692, Fig. 4B), and VCD (P = .692, Fig. 4C) were similar between CCRP group and control group. Whereas at week 8, VRP (P < .001, Fig. 4A), VSP (P < .001, Fig. 4B), and VCD (P < .001, Fig. 4C) were elevated in CCRP group compared with control group. These data implied that the pelvic floor muscle function of puerperae was enhanced in CCRP group than that in control group, which contributed to decreasing postpartum SUI risk.
Figure 4.
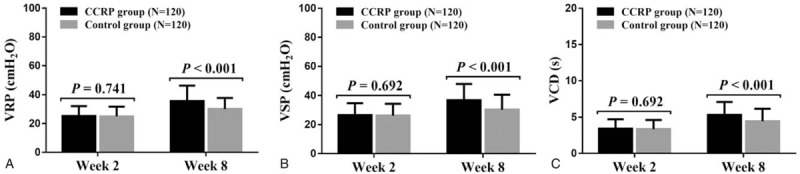
Comparison of VRP, VSP, and VCD between 2 groups at week 2 and week 8. VRP (A), VSP (B), and VCD (C) were similar between CCRP group and control group at week 2, while they were elevated in CCRP group compared with control group at week 8. Comparison between 2 groups was assessed by t test. P < .05 was consider significant. CCRP = comprehensive care and rehabilitation program, VCD = vaginal contraction duration, VRP = vaginal resting pressure, VSP = vaginal squeezing pressure.
4. Discussion
In the present study, we discovered the following results:
-
1.
The incidence of postpartum SUI was 25.7%. Meanwhile, the vaginal delivery and the increased age and BMI were independent risk factors for postpartum SUI.
-
2.
CCRP group exhibited lower incidence of postpartum SUI while higher pelvic floor muscle function indexes compared with control group.
The SUI is the most prevalent subtype of urinary incontinence which accounts for approximately 61% of urinary incontinence populations in China. SUI commonly occurs in puerperae and its incidence has been reported in a few studies.[20,21] For instance, a previous study that is conducted in Norway reveals that 58 (35.6%) puerperae occur postpartum SUI within 6 weeks after delivery.[4] In another study conducted in Taiwan, 139 (16.1%) puerperae occur postpartum SUI within 3 months after delivery.[7] Besides, similar study conducted in Iran shows that the prevalence of postpartum SUI is 14.1% for all puerperae, 15.9% for vaginal delivery puerperae, and 10.7% for elective cesarean section puerperae within 4 months after delivery.[21] In the current study, the prevalence of postpartum SUI was 25.7%, which was within from previous studies. The possible reasons might derive from the difference of delivery mode, evaluation time or characteristics of puerperae such as BMI and newborn weight. As for risk factors, we found that the vaginal delivery and the increased age and BMI were independent risk factors for postpartum SUI, which were in line with previous studies.[2,7,22,23] The possible explanations for the results might be that:
-
1.
Vaginal delivery aggravates strain on pelvic floor muscles and traction trauma on pudendal nerve, which subsequently leads to the insufficient support of pelvic floor fascia.[2,7] Therefore, vaginal delivery contributes to higher postpartum SUI risk.
-
2.
It is reported that the detrusor morphology, detrusor innervation, and bladder metabolism are greatly changed in aged people, thus the elevated age might associate with dysregulated detrusor function, thereby causing the incontinence.[22,24]
-
3.
Higher BMI produces higher intraabdominal pressure, which also contributes to incontinence.
Considering the high incidence of postpartum SUI, effort that facilities the prevention of postpartum SUI has been made. For example, a newly published clinical trial investigates the role of an educational program in improving pelvic floor muscle functions and preventing urinary incontinence in 99 women, which shows that the educational program exhibits little effect on improving pelvic floor muscle functions of women, but it improves their knowledge about the pelvic floor.[12] In another study, the effect of postpartum PFMT on SUI prevention is explored, which reveals that puerperae who exercise PFMT regularly after delivery for 8 weeks exhibit increased pelvic floor muscle function indexes while decreased postpartum SUI risk compared with controls.[11] However, no comprehensive care program has been reported to prevent postpartum SUI. In the current study, a comprehensive care program that consisted of intensive healthy education, detailed guidance of PFMT, psychologic counseling and regular supervision was set up, and its preventive effect for postpartum SUI was assessed. The assessment data showed that CCRP obviously reduced the incidence of postpartum SUI and enhanced the pelvic floor muscle functions of puerperae compared with usual guidance. The possible explanation for the results might be that:
-
1.
Puerperae who receive CCRP can access to more intensive health education compared with control, which assure them a more in-depth knowledge and a more positive attitude towards postpartum SUI. As a result, puerperae who receive CCRP are more likely to corporate and they are less likely to occur postpartum SUI.
-
2.
Puerperae in CCRP group receive more detailed guidance of PFMT and regular supervision compared to control group, hence they strengthen their muscle functions of pelvic floor more pronouncedly, which contribute to a lower postpartum SUI risk.
-
3.
Through psychologic counseling, puerperae in CCRP group are less likely to suffer from psychologic disorders such as depression or anxiety compared with puerperae in control group, and they are more willing to corporate and do PFMT, which also decrease their postpartum SUI risk.
There were still some limitations which should not be ignored. Firstly, we only evaluated the incidence of postpartum SUI in a short time, thus the incidence of postpartum SUI in a longer period was not assessed. However, the incidence of postpartum SUI is highest in the short time after delivery because the weaken function of pelvic floor muscle postpartum will recover with the time in most puerperae. Secondly, the current study evaluated the effect of postpartum CCRP in preventing postpartum SUI, while the effect of antenatal CCRP in postpartum SUI prevention remained to be determined in the future studies. Besides, the study was monocentric that most of puerperae were from same area; hence multicentric clinical trials are needed in the further.
In conclusion, the incidence of postpartum SUI is 25.7%, and the vaginal delivery, increased age, and BMI are independent risk factors for postpartum SUI. More importantly, CCRP strengthens pelvic floor muscle functions and decreases postpartum SUI incidence in puerperae.
Author contributions
Data curation: Juan Shan.
Formal analysis: Lei Peng.
Methodology: Xiaowen Qi.
Writing – original draft: Lei Peng, Cuihong Zhang.
Writing – review & editing: Fanglei Xu.
Fanglei Xu orcid: 0000-0001-6381-304X.
Footnotes
Abbreviations: BMI = body mass index, CCRP = comprehensive care and rehabilitation program, ICS = International Continence Society, ITT = intention-to-treat, LOCF = last observation carried forward, PFMT = pelvic floor muscle training, SUI = stress urinary incontinence, VCD = vaginal contraction duration, VRP = vaginal resting pressure, VSP = vaginal squeezing pressure.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Wang H, Ghoniem G. Postpartum stress urinary incontinence, is it related to vaginal delivery? J Matern Fetal Neonatal Med 2017;30:1552–5. [DOI] [PubMed] [Google Scholar]
- [2].Zhu L, Li L, Lang JH, et al. Prevalence and risk factors for peri- and postpartum urinary incontinence in primiparous women in China: a prospective longitudinal study. Int Urogynecol J 2012;23:563–72. [DOI] [PubMed] [Google Scholar]
- [3].Perera J, Kirthinanda DS, Wijeratne S, et al. Descriptive cross sectional study on prevalence, perceptions, predisposing factors and health seeking behaviour of women with stress urinary incontinence. BMC Women Health 2014;14:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Bo K, Hilde G, Tennfjord MK, et al. Does episiotomy influence vaginal resting pressure, pelvic floor muscle strength and endurance, and prevalence of urinary incontinence 6 weeks postpartum? Neurourol Urodyn 2017;36:683–6. [DOI] [PubMed] [Google Scholar]
- [5].Lasak AM, Jean-Michel M, Le PU, et al. The role of pelvic floor muscle training in the conservative and surgical management of female stress urinary incontinence: does the strength of the pelvic floor muscles matter? PM R 2018;10:1198–210. [DOI] [PubMed] [Google Scholar]
- [6].Thomaz RP, Colla C, Darski C, et al. Influence of pelvic floor muscle fatigue on stress urinary incontinence: a systematic review. Int Urogynecol J 2018;29:197–204. [DOI] [PubMed] [Google Scholar]
- [7].Lin YH, Chang SD, Hsieh WC, et al. Persistent stress urinary incontinence during pregnancy and one year after delivery; its prevalence, risk factors and impact on quality of life in Taiwanese women: An observational cohort study. Taiwan J Obstet Gynecol 2018;57:340–5. [DOI] [PubMed] [Google Scholar]
- [8].Radziminska A, Weber-Rajek M, Straczynska A, et al. The impact of pelvic floor muscle training on the myostatin concentration and severity of urinary incontinence in elderly women with stress urinary incontinence - a pilot study. Clin Interv Aging 2018;13:1893–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Blaivas JG, Simma-Chiang V, Gul Z, et al. Surgery for stress urinary incontinence: autologous fascial sling. Urol Clin North Am 2019;46:41–52. [DOI] [PubMed] [Google Scholar]
- [10].Liu YJ, Wu WY, Hsiao SM, et al. Efficacy of pelvic floor training with surface electromyography feedback for female stress urinary incontinence. Int J Nurs Pract 2018;24:e12698. [DOI] [PubMed] [Google Scholar]
- [11].Morkved S, Bo K. Effect of postpartum pelvic floor muscle training in prevention and treatment of urinary incontinence: a one-year follow up. BJOG 2000;107:1022–8. [DOI] [PubMed] [Google Scholar]
- [12].de Andrade RL, Bo K, Antonio FI, et al. An education program about pelvic floor muscles improved women's knowledge but not pelvic floor muscle function, urinary incontinence or sexual function: a randomised trial. J Physiother 2018;64:91–6. [DOI] [PubMed] [Google Scholar]
- [13].De Gagne JC, Park S, So A, et al. A urinary incontinence continuing education online course for community health nurses in South Korea. J Contin Educ Nurs 2015;46:171–8. [DOI] [PubMed] [Google Scholar]
- [14].Sangi-Haghpeykar H, Mozayeni P, Young A, et al. Stress urinary incontinence and counseling and practice of pelvic floor exercises postpartum in low-income Hispanic women. Int Urogynecol J Pelvic Floor Dysfunct 2008;19:361–5. [DOI] [PubMed] [Google Scholar]
- [15].Konstantinidou E, Apostolidis A, Kondelidis N, et al. Short-term efficacy of group pelvic floor training under intensive supervision versus unsupervised home training for female stress urinary incontinence: a randomized pilot study. Neurourol Urodyn 2007;26:486–91. [DOI] [PubMed] [Google Scholar]
- [16].Dumoulin C, Cacciari LP, Hay-Smith EJC. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev 2018;10:CD005654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Kannan P, Winser SJ, Fung B, et al. Effectiveness of pelvic floor muscle training alone and in combination with biofeedback, electrical stimulation, or both compared to control for urinary incontinence in men following prostatectomy: systematic review and meta-analysis. Phys Ther 2018;98:932–45. [DOI] [PubMed] [Google Scholar]
- [18].Abrams P, Cardozo L, Fall M, et al. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology 2003;61:37–49. [DOI] [PubMed] [Google Scholar]
- [19].Chiarelli P, Cockburn J. Promoting urinary continence in women after delivery: randomised controlled trial. BMJ 2002;324:1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Zhu L, Lang J, Liu C, et al. The epidemiological study of women with urinary incontinence and risk factors for stress urinary incontinence in China. Menopause 2009;16:831–6. [DOI] [PubMed] [Google Scholar]
- [21].Eftekhar T, Hajibaratali B, Ramezanzadeh F, et al. Postpartum evaluation of stress urinary incontinence among primiparas. Int J Gynaecol Obstet 2006;94:114–8. [DOI] [PubMed] [Google Scholar]
- [22].Luber KM. The definition, prevalence, and risk factors for stress urinary incontinence. Reviews in urology 2004;6Suppl 3:S3–9. [PMC free article] [PubMed] [Google Scholar]
- [23].Tennstedt SL, Link CL, Steers WD, et al. Prevalence of and risk factors for urine leakage in a racially and ethnically diverse population of adults: the Boston Area Community Health (BACH) Survey. Am J Epidemiol 2008;167:390–9. [DOI] [PubMed] [Google Scholar]
- [24].Nordling J. The aging bladder–a significant but underestimated role in the development of lower urinary tract symptoms. Exp Gerontol 2002;37:991–9. [DOI] [PubMed] [Google Scholar]


