Abstract
Rationale:
Actinomyces odontolyticus and Parvimonas micra are very rare causative organisms of lung abscess and acute respiratory failure.
Patient concerns:
A 49-year-old male patient visited the emergency room with a complaint of sudden onset of shortness of breath, and he developed acute respiratory failure rapidly.
Diagnosis:
An abscess in the left lower lung field was diagnosed on the computed tomography scan of chest.
Interventions:
Immediate treatment with intravenous antibiotics was initiated along with a pigtail catheter insertion for pus drainage.
Outcomes:
A odontolyticus was cultured on the drained pus and P micra was identified by a blood culture. The patient was successfully weaned from the mechanical ventilator and the lung abscess was completely resolved.
Lessons:
To the best of our knowledge, this is the first case report of mixed infection with A odontolyticus and P micra, which caused acute respiratory failure in an immune-competent patient. Therefore, physicians should consider the possibility of these organisms as causative pathogens of a fulminant pulmonary infection even in an immune-competent patient.
Keywords: Actinomyces odontolyticus, acute respiratory failure, infection, lung abscess, Parvimonas micra
1. Introduction
Lung abscess is usually caused by polymicrobial infections with anaerobes including Peptostreptococcus, Prevotella, and Bacterioides, and aerobes including Streptococcus, Staphylococcus, and Klebsiella.[1] The incidence of actinomycosis is on the decrease and pulmonary actinomycosis accounts for less than 15% of all forms of actinomycosis. Furthermore, the prognosis of actinomycosis is good and mortality rate is low.[2] However, timely diagnosis and proper management of pulmonary actinomycosis are still important because aggressive forms of pulmonary actinomycosis can develop rarely.[2,3]Parvimonas micra is a commensal of the human oral cavity, which rarely causes pulmonary infections. Only a few cases of such pulmonary infections have been identified in pure culture.[4] In this article, we report a case of lung abscess due to a mixed infection with Actinomyces odontolyticus and P micra, which initially presented with acute respiratory failure. Patient has provided informed consent for publication of the case.
2. Case report
A 49-year-old male patient visited the emergency room with a complaint of sudden onset of dyspnea developed on the day of the hospital visit. He did not complain of cough or purulent sputum, and did not have fever. He was a current smoker with a 20 pack-year smoking history and had a heavy alcohol drinking habit. His past medical history included hypertension.
On examination, the patient was alert and oriented. He had poor oral hygiene with extensive caries. His body temperature was 36.1°C, blood pressure was 130/70 mm Hg, respiratory rate was 35 breaths per minute, heart rate was 120 beats per minute, and oxygen saturation was 76% on room air. Despite the inhalation of 15 L/min oxygen via facial mask, the patient developed acute respiratory failure and therefore, mechanical ventilation was started.
Initial laboratory test showed a white blood cell count of 17,940/mm3 with 90.1% neutrophils, hemoglobin of 11.1 g/dL, platelet count of 589 × 103/mm3, erythrocyte sedimentation rate of 105 mm/h, and C-reactive protein of 275.6 mg/L. Liver function test showed total bilirubin of 1.59 mg/dL, alkaline phosphatase of 513 U/L, aspartate transaminase of 43 U/L, alanine transaminase of 42 U/L. In addition, renal function test showed blood urea nitrogen of 24.9 mg/dL, creatinine of 1.86 mg/dL.
The initial chest radiographs showed a consolidation in the left lower lung field (Fig. 1A). A computed tomography scan of the chest showed a large lung abscess with an air-fluid level in the left lower hemithorax (Fig. 1B). Ceftriaxone and clindamycin were administered promptly and a percutaneous pigtail catheter was inserted to drain the abscess. The drained fluid was purulent in gross appearance. The patient was successfully weaned from the mechanical ventilator on the 6th day of the hospital visit. A odontolyticus was sensitive to penicillin, ampicillin, cephalosporin, tetracycline, clindamycin, and erythromycin. P micra was sensitive to Penicillin, amoxicillin, clindamycin. Therefore, the antibiotics were changed to ampicillin-sulbactam, and the patient recovered faster. The oral examination revealed swelling and redness of gingiva, accumulation of dental calculus, and gingival bleeding on probing. The percutaneous drainage catheter was removed on the 12th day of the hospital visit. The patient was discharged on the 26th day from admission with markedly improved symptoms and general condition. After discharge, oral amoxicillin/clavulanate was prescribed as maintenance therapy for 6 months and the left lung lesion was resolved (Fig. 2).
Figure 1.
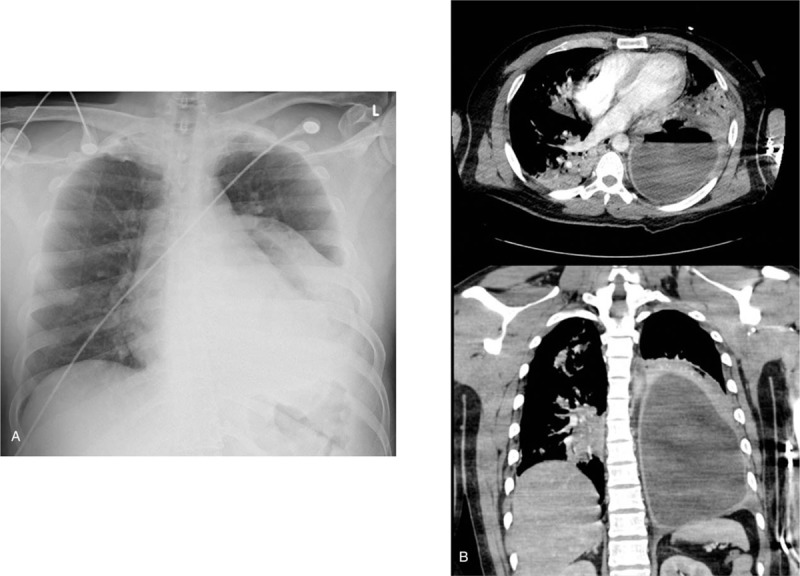
(A) The initial chest x-ray showing infiltration with an air-fluid level in the left lower lung field. (B) The initial chest computed tomography scan before the insertion of a pigtail catheter showing a large lung abscess with internal air and surrounding consolidation in the left thorax.
Figure 2.

The follow-up chest x-ray showing an improvement of the lung abscess in the left lower lung field.
3. Discussion
Lung abscess due to A odontolyticus or P micra is very rare, and co-infection with both organisms causing lung abscess and acute respiratory failure had not been reported. The Actinomyces species are gram-positive bacteria and are facultative anaerobes.[2,3]P micra is also a facultative, anaerobic, gram-positive bacterium.[4] These 2 species are often found in the human oropharynx.[3,4] Pulmonary infection by A odontolyticus or P micra result from the aspiration of these species into the lungs. In this article, we reported a case of lung abscess and respiratory failure in an immune-competent patient caused by these 2 organisms.
A prompt diagnosis and an adequate treatment of pulmonary actinomycosis are important even though it is a relatively rare disease with a low mortality rate. The computed tomography findings of pulmonary actinomycosis provide limited information; therefore, the confirmative diagnosis of pulmonary actinomycosis is made by a microscopic examination of pus or lung biopsy sample.[2,5] A case of pulmonary actinomycosis of periodontal origin by Actinomyces naeslundii and Actinomyces viscosus was reported previously.[6] A case of periodontal disease-associated septic pulmonary embolism by Actinomyces species was also reported, but the specific species was not mentioned.[7] This case highlights the potential pathogenic role of A odontolyticus of periodontal origin as a risk factor for lung infection.
The pulmonary infection by P micra is also very rare and P micra is rarely identified in pure culture. This organism usually causes periradicular diseases and periodontitis, with other microorganisms.[4] Poetter et al reported a case of pleural empyema in which P micra was cultured from the pleural pus.[4] In our case, A odontolyticus was identified by the pleural fluid culture and P micra was identified by the blood culture.
Although pulmonary actinomycosis is rare and difficult to diagnose, prognosis is relatively good if it is properly treated.[2,8] There are no guidelines for antibiotics treatment for pulmonary actinomycosis and P micra infection yet. The recommended therapy for these infections is 4 to 6 weeks of intravenous penicillin followed by a 6 to 12 months oral regimen.[2,4,9] In this case, the patient was treated with intravenous antibiotics for 15 days along with percutaneous drainage and further treated with oral antibiotics for several months.
This case highlights the potential pathogenic role of A odontolyticus and P micra in immune-competent patients with lung abscess. Physicians should consider these organisms as causative pathogens of lung abscess and acute respiratory failure, especially when the evidence of periodontitis exists.
Author contributions
Conceptualization: Jong Deog Lee, Seung Jun Lee.
Data curation: Hyun Seop Cho, Seung Jun Lee.
Investigation: Yu Ji Cho, Yi Yeong Jeong.
Software: Hyun Seop Cho.
Validation: Hyun Seop Cho, Manbong Heo, Jong Hwan Jeong, Ho Cheol Kim.
Visualization: Manbong Heo, Jong Hwan Jeong.
Writing – original draft: Sang Suk Yun, Seung Jun Lee.
Writing – review and editing: Hyang Rae Lee, Sunmi Ju, Ju-Young Kim, Jung Wan You, Seung Jun Lee.
Footnotes
SSY and HSC contributed equally to this work.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Kuhajda I, Zarogoulidis K, Tsirgogianni K, et al. Lung abscess-etiology, diagnostic and treatment options. Ann Transl Med 2015;3:183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Mabeza G, Macfarlane J. Pulmonary actinomycosis. Eur Respir J 2003;21:545–51. [DOI] [PubMed] [Google Scholar]
- [3].Takiguchi Y, Terano T, Hirai A. Lung abscess caused by Actinomyces odontolyticus. Intern Med 2003;42:723–5. [DOI] [PubMed] [Google Scholar]
- [4].Poetter C, Pithois C, Caty S, et al. Hiding behind confusion: pleural empyema caused by Parvimonas micra. Surg Infect 2014;15:356–7. [DOI] [PubMed] [Google Scholar]
- [5].Fahim A, Teoh R, Kastelik J, et al. Case series of thoracic actinomycosis presenting as a diagnostic challenge. Respir Med CME 2009;2:47–50. [Google Scholar]
- [6].Suzuki JB, Delisle AL. Pulmonary actinomycosis of periodontal origin. J Periodontol 1984;55:581–4. [DOI] [PubMed] [Google Scholar]
- [7].Endo S, Mishima E, Takeuchi Y, et al. Periodontitis-associated septic pulmonary embolism caused by Actinomyces species identified by anaerobic culture of bronchoalveolar lavage fluid: a case report. BMC Infect Dis 2015;15:552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Park JY, Lee T, Lee H, et al. Multivariate analysis of prognostic factors in patients with pulmonary actinomycosis. BMC Infect Dis 2014;14:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Choi J, Koh W-J, Kim TS, et al. Optimal duration of IV and oral antibiotics in the treatment of thoracic actinomycosis. Chest 2005;128:2211–7. [DOI] [PubMed] [Google Scholar]


