Abstract
Background:
Robotic arm-assisted unicompartmental knee arthroplasty (UKA) has been recommended for treatment of unicompartmental knee osteoarthritis. However, its effectiveness and safeness remain controversial compared with conventional UKA. Therefore, the goal of this study was to perform a meta-analysis to re-evaluate the effects of robotic arm-assisted UKA on clinical functional outcomes.
Methods:
PubMed, Embase, and Cochrane Library databases were searched to screen the relevant studies. Continuous data (surgical time, knee excursion during weight acceptance, American knee society score [AKSS], Oxford knee score [OKS], forgotten joint score [FJS], visual analog scale [VAS], and range of motion [ROM]) were pooled using a standardized mean difference (SMD) with their corresponding 95% confidence intervals (CIs) to estimate the effect size, while dichotomous data (complication rate, revision rate) were pooled to obtain the relative risk (RR) with a 95% CI by STATA 13.0 software.
Results:
Eleven studies involving 498 patients undergoing robotic-assisted UKA and 589 patients receiving conventional UKA were included. Our pooled results demonstrated that robotic-assisted could significantly reduce the complication rate (RR: 0.62, 95% CI: 0.45–0.85; P = .0041) and improve the knee excursion during weight acceptance (SMD: 0.62, 95% CI: 0.25–1.00; P = .001), but prolonged the surgical time (SMD: 0.74, 95% CI: 0.40–1.08; P < .001). No significant difference in the revision rate, AKSS, OKS, FJS, VAS, and ROM between robotic-assisted and conventional UKA groups.
Conclusion:
This meta-analysis demonstrates robotic-assisted UKA may be an effective and safe surgical procedure for treatment of unicompartmental knee osteoarthritis.
Keywords: complication, functional score, gait, robotic arm-assisted, unicompartmental knee arthroplasty
1. Introduction
Unicompartmental knee arthroplasty (UKA) has been a commonly used alternative to total-knee arthroplasty (TKA) for treatment of osteoarthritis of the medial compartment of knee because it can preserve the natural knee kinematics and lead to better recovery of range of motion (ROM), improved functional outcomes, and few postoperative complications, in addition to the advantages of shorter operative time, less blood loss, and reduced hospital stay.[1,2] Nonetheless, recent evidence indicates that there is a considerable revision rate (7–32%) as a result of the failure of UKA prostheses,[3,4] which may influence the satisfaction and limit the wide acceptance of the clinical patients.[5,6] Several experts have proposed poor positioning of the tibial and/or femoral components is an important factor associated with the lower survivorship of UKA prostheses.[7–10] Therefore, how to improve the accuracy of component positioning has become an important topic for the surgeons.
Recent advances in robotics inspire the scholars to use the robotic system to assist planning of implant position and bone resection which are determined based on a preoperative computed tomography scan[11–16] or by an intraoperative real-time feedback.[17,18] Theoretically, implantation accuracy of component should be significantly higher after robotic-assisted UKA compared to conventional UKA, and thus contributed to lower revision rate and better functional outcomes. However, the conclusions among different studies seemed to be controversial. The study of Cobb et al showed the tibiofemoral alignment in the coronal plane within 2° of the planned position, which was defined as the accurate positioning, was achieved in 100% of knee (13/13) of the robotic-assisted group, but only 40% (6/15) in the conventional group. Their difference was statistically significant (P = .001).[16] However, the study of MacCallum et al showed 26% knees (23/87) were properly positioned in the robotic-assisted group compared to 27% (48/177) of the conventional group, which was not statistically significant (P = 1.0).[14] In addition, Blyth et al found the American knee society score (AKSS) score was significantly higher in the robotic-assisted surgery group than that in the conventional surgery group (193 vs 175, P = .0064) at last follow-up,[19] but the study of Gilmour et al demonstrated no statistical difference in AKSS score between 2 groups (168 vs 173, P = .951).[13] Therefore, it is essential to comprehensively evaluate the therapeutic effects of robotic-assisted UKA.
Previously, there had 1 study to perform a meta-analysis to investigate the influence of robotic-assisted UKA on implant positioning compared with conventional UKA[20] and there were no updated papers until our searching. Thus, it was not necessary to repeat it. However, its effects on the clinical functional outcomes had not been investigated, which was also listed as a limitation in the study of Fu et al.[20] Hereby, the purpose of the current study was, for the 1st time, to conduct a meta-analysis of all accumulated evidence before December 2018 to comprehensively evaluate whether robotic-assisted UKA can reduce the revision rate and result in excellent functional outcomes in comparison with conventional UKA for treatment of unicompartmental knee osteoarthritis.
2. Materials and methods
2.1. Literature search strategy
A systematic literature search was performed in PubMed, Embase, and Cochrane Library databases for screening potentially relevant articles regarding robotic-assisted UKA up to December 2018. The search strategy was: [“Robotic-Assisted” OR “robotic-arm assisted” OR “Robot-Assisted”] AND [“Unicompartmental Knee Arthroplasty” OR “UKA” OR “unicompartmental knee replacement”]. Furthermore, the reference lists of all identified publications were also manually searched for additional studies. The protocol adhered to the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) Guidelines. Ethical approval and patient written informed consent were not required because this was a meta-analysis of previously published studies.
2.2. Inclusion and exclusion criteria
Two independent authors independently selected studies using inclusion criteria as follows: comparing the robotic-assisted UKA with conventional UKA; human studies; inclusion of at least one of the outcome measures, such as surgical time, complications, and functional outcomes; and only English publication languages. The exclusion criteria were: abstracts, letters to editors, case reports, comments, reviews, meta-analysis or cadavers studies; not providing controls; not providing effective data; and literature written in other language. If disagreement between the 2 reviewers occurred, consensus was held with a 3rd party.
2.3. Data extraction
Two authors independently extracted the following data from included studies: 1st author, year of publication, origin of country, study design, sample size, follow-up, surgical time, complications, revision rate and function outcomes (such as gait, AKSS, Oxford knee score [OKS], forgotten joint score [FJS], visual analog scale [VAS], and ROM). Disagreements between the reviewers were resolved by discussion with a 3rd party.
The methodologic quality of each included study was evaluated using the Cochrane Collaboration's tool for assessing risk of bias, which consisted of 6 types of bias: selection (random sequence generation and allocation concealment), performance (blinding of participants and personnel), detection (blinding of outcome assessment), attrition (incomplete outcome data), reporting (selective reporting), and other biases.[21] Each item was graded as low (green), unclear (yellow), or high (red) risk of bias, respectively.
2.4. Statistical analysis
All statistical analyses were performed using STATA 13.0 (STATA Corporation, College Station, TX). Continuous data were pooled using a standardized mean difference (SMD) with their corresponding 95% confidence interval (CI) to estimate the effect size, while dichotomous data were pooled to obtain the relative risk (RR) with a 95% CI. If the study did not provide mean and standard deviation, these parameters were estimated from median and range as described by Hozo et al.[22] Heterogeneity between the trials was tested by using Chi-squared and I2 statistics tests. If there was no evidence of heterogeneity (P > .1 or I2 < 50%), the pooled effects were calculated using a fixed model; otherwise, a random-effects model was used to obtain the pooled effects. The Egger regression test and a funnel plot were performed to assess the publication bias for parameters assessed by at least 3 studies. Sensitivity analysis was performed by omitting one study at a time to assess the influence of each individual study on the pooled SMD or RR. P < .05 was considered to be statistically significant.
3. Results
3.1. Description of the included studies
A flow chart of the literature search is shown in Figure 1. Eleven studies (including 498 patients undergoing robotic-assisted UKA; 589 patients receiving conventional UKA) published between 2005 and 2018 were included for this meta-analysis.[11,13–16,18,19,23–26] Among them, 5 were designed as randomized controlled trials (RCT), 2 quasi-RCT, and 4 prospective cohort trials (PCTs). Seven studies were performed in the United Kingdom, 3 in the United States, and 1 in the France. The follow-up time ranged from 30 days to 5 years. The outcomes assessed of the included studies are summarized in Table 1. Figure 2 shows the methodologic quality and bias risk summary of all studies, which indicated the risk of performance bias to be high in some studies due to the fact that the treatment allocation was not blinded or randomized.
Figure 1.
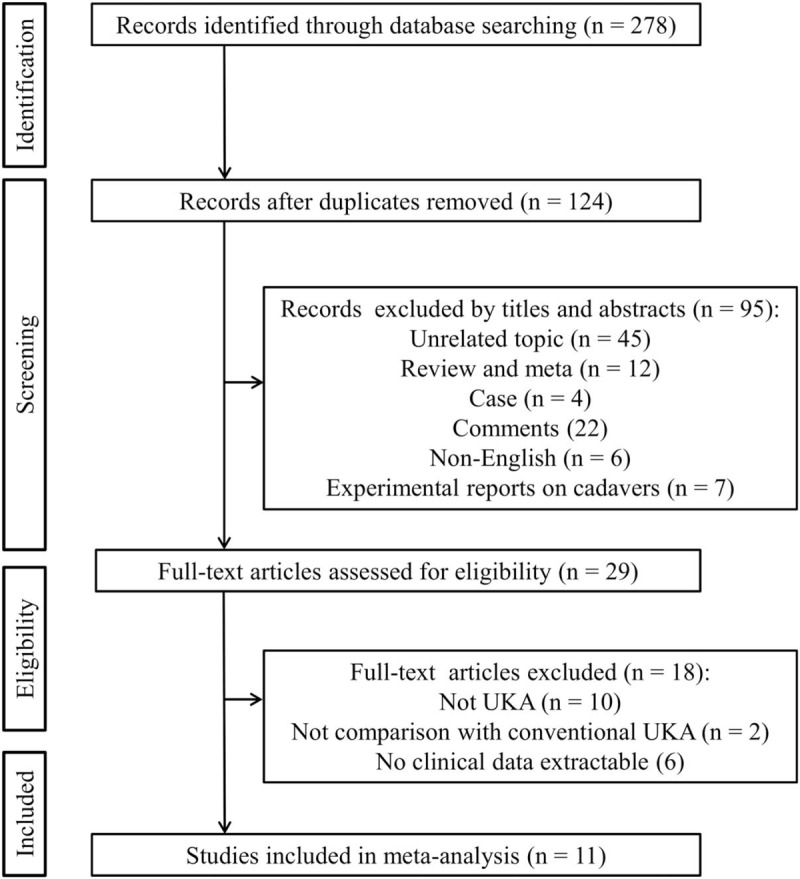
Flowchart of searching relevant studies used in this meta-analysis. UKA = unicompartmental knee arthroplasty.
Table 1.
Baseline characteristics of the studies included.
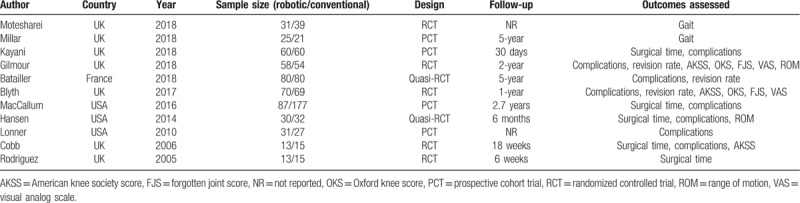
Figure 2.

Risk of bias summary of studies included.
3.2. Meta-analysis of surgical time
Surgical time was assessed by a total of 5 studies.[11,14–16,24] Using a random-effects model (P = .036, I2 = 61.1%), robotic-assisted UKA was found to significantly prolong the time of surgery in comparison to conventional UKA (SMD: 0.74, 95% CI: 0.40–1.08; P < .001; Fig. 3).
Figure 3.
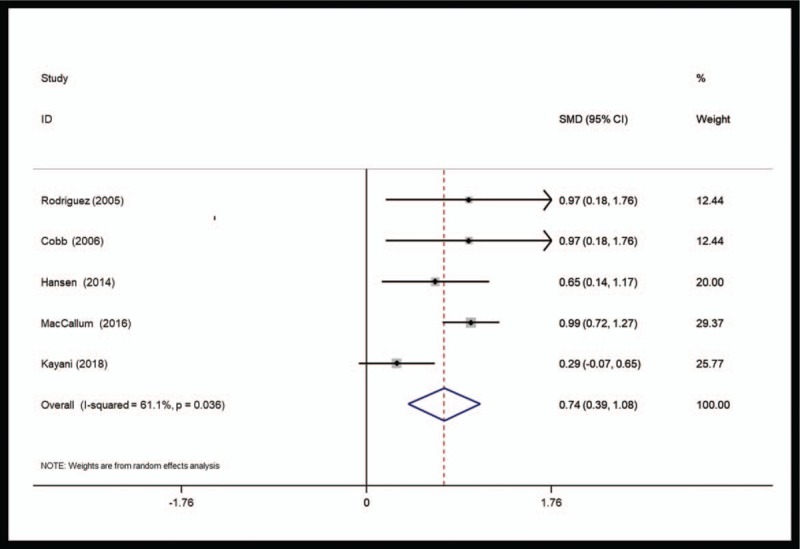
Forest plots of surgical time comparison between robotic-assisted and conventional unicompartmental knee arthroplasty. CI = confidence interval, SMD = standardized mean difference.
3.3. Meta-analysis of complications
Complication was recorded in a total of 8 studies with 9 data sets.[11,13,14,16,18,19,24,26] Using a fixed-effects model (P = .177, I2 = 30.2%), robotic-assisted UKA was found to significantly reduce the incidence of complications compared with conventional UKA (RR: 0.62, 95% CI: 0.45–0.85; P = .0041; Fig. 4).
Figure 4.
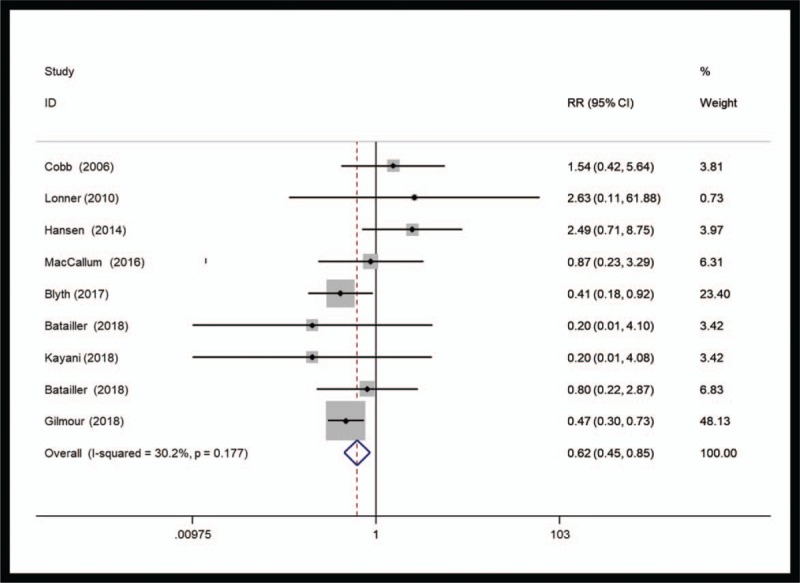
Forest plots of complication rate comparison between robotic-assisted and conventional unicompartmental knee arthroplasty. CI = confidence interval, RR = relative risk.
3.4. Meta-analysis of revision rate
The revision rate was reported in a total of 3 studies with 4 data sets.[13,18,19] Using a fixed-effects model (P = .524, I2 = 0%), no significant difference was found in the revision rate between robotic-assisted UKA and conventional UKA (RR: 0.49, 95% CI: 0.17–1.41; P = .188).
3.5. Meta-analysis of functional outcomes
The gait (knee excursion during weight acceptance) was determined in 2 studies.[23,25] Using a fixed-effects model (P = .470, I2 = 0%), knee excursion degree was shown to be significantly larger in patients after robotic-assisted UKA than those undergoing conventional UKA (SMD: 0.62, 95% CI: 0.25–1.00; P = .001; Fig. 5).
Figure 5.
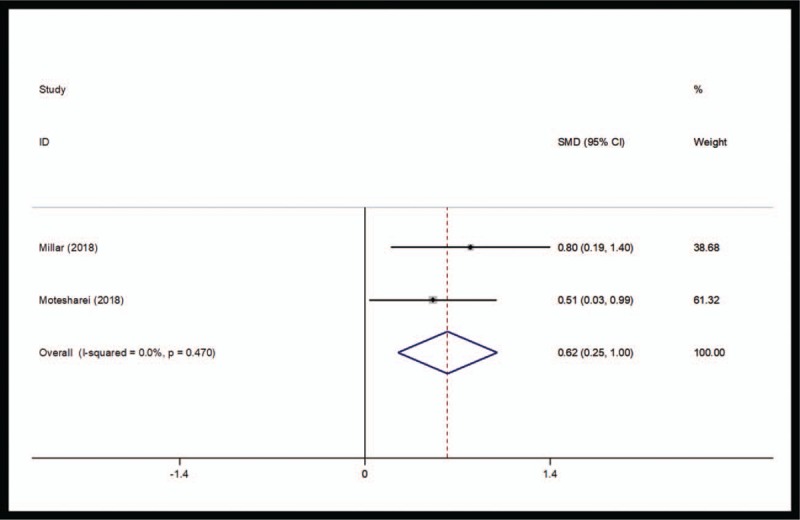
Forest plots of knee excursion during weight acceptance comparison between robotic-assisted and conventional unicompartmental knee arthroplasty. CI = confidence interval, SMD = standardized mean difference.
The ROM was determined in 2 studies.[11,13] Using a random-effects model (P = .005, I2 = 87.2%), no significant difference was found in the ROM between robotic-assisted UKA and conventional UKA groups (SMD: −0.08, 95% CI: −0.96 to 0.80; P = .851).
The VAS was assessed in 2 studies.[13,19] Using a fixed-effects model (P = .781, I2 = 0%), no significant difference was found in the VAS between robotic-assisted UKA and conventional UKA (SMD: −0.06, 95% CI: −0.31 to 0.19; P = .649).
There were 3 studies to investigate the changes in the AKSS.[13,16,19] Using a random-effects model (P = .005, I2 = 81.2%), robotic-assisted UKA did not significantly improve the AKSS compared with conventional UKA (SMD: 0.37, 95% CI: −0.24 to 0.98; P = .239).
There were 2 studies to investigate the changes in the OKS.[13,19] Using a fixed-effects model (P = .473, I2 = 0%), robotic-assisted UKA did not significantly improve the OKS compared with conventional UKA (SMD: 0.01, 95% CI: −0.24 to 025; P = .965).
Two studies were performed to investigate the changes in the FJS.[13,19] Using a fixed-effects model (P = .463, I2 = 0%), no statistically significant difference was observed regarding FJS between robotic-assisted UKA and conventional UKA groups (SMD: 0.13, 95% CI: −0.12 to 0.37; P = .324).
3.6. Publication bias
The evaluation of publication bias using Egger test indicated that the publication bias was not significant for surgical time (P = .956), complications (P = .068), revision rate (P = .188), and AKSS (P = .356). No obvious asymmetry was also observed in the funnel plot (Fig. 6). These results revealed no evidence of publication bias.
Figure 6.
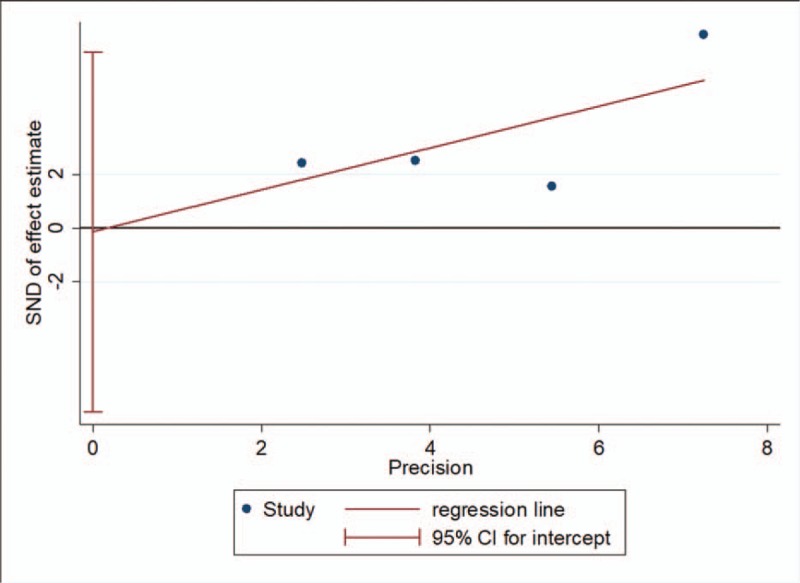
Funnel plot for the assessment of potential publication bias for surgical time. CI = confidence interval, SMD = standardized mean difference.
3.7. Sensitivity analyses
An individual study was deleted each time to investigate its influence on the pooled SMD or RR. The results showed that no individual study could materially affect the pooled SMD or RR in the present meta-analysis (Fig. 7).
Figure 7.
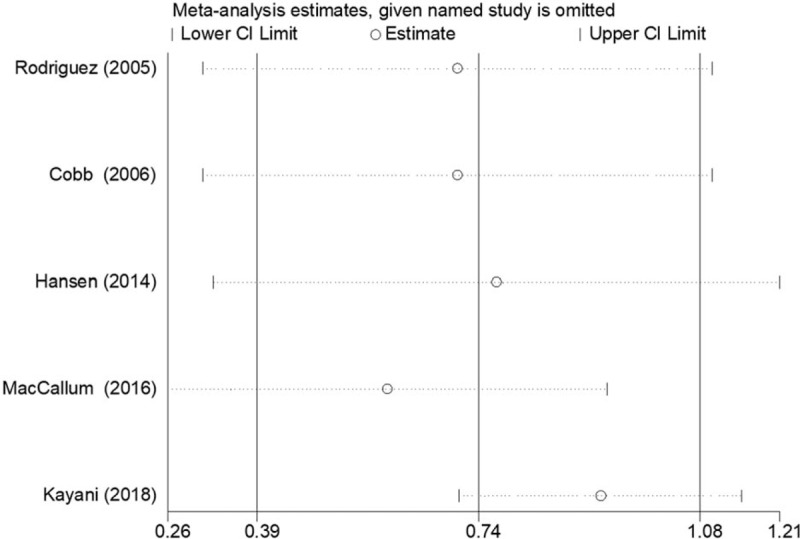
Sensitivity analysis for the assessment of potential publication bias for surgical time. CI = confidence interval.
4. Discussion
In the current study, we re-evaluated the effects of robotic-assisted and conventional UKA on surgical time, complications, and functional outcomes in treating unicompartmental knee osteoarthritis using a meta-analysis based on the accumulated evidence. The results showed that robotic-assisted UKA could significantly reduce the complication rate and improve the knee excursion during weight acceptance, but also prolonged the surgical time. No significant difference in the revision rate, AKSS, OKS, FJS, VAS, and ROM between robotic-assisted and conventional UKA groups.
Surgical time and complications had also been assessed by the meta-analysis study performed by Fu et al.[20] However, the conclusion of complications in our study seemed not to be in line with the study of Fu et al[20] who demonstrated the rate of adverse events between robotic-assisted and conventional UKA was of no statistical significance (RR: 1.56, 95% CI: 0.77–3.19; P = .22). This controversial finding may be attributed to more articles (8 vs 4) and more patients (robotic-assisted: 376; conventional: 541 vs robotic-assisted: 161; conventional: 251) included in our study. Thus, our conclusion may be more credible. The longer surgical time of robotic-assisted UKA proved by our meta-analysis and the study of Fu et al[20] may be due to the influence of learning curve. The surgical time may be decreased when the surgeon became increasingly familiar and adept with robotic technology. This hypothesis had been supported by the study of Kayani et al[24] and other studies on robotic-guided TKA.[27,28] Thus, this disadvantage of robotic-assisted UKA compared with conventional UKA may be eliminated by increased experience in the surgeon.
The knee prosthesis is designed for use under normal gait conditions. Abnormal gait patterns induced by knee arthroplasty may accelerate damage to the prosthesis and lead to increased likelihood of revision surgery subsequently.[29] Therefore, the gait parameter (knee excursion during weight acceptance) was also assessed in this study. Our results showed that knee excursion degree was shown to be significantly higher in patients after robotic-assisted UKA than those undergoing conventional UKA (SMD: 0.62, 95% CI: 0.25–1.00; P = .001). Also, the knee excursion degree (18 ± 4.9°) after robotic-assisted UKA[23,29] was approximated to normal range for knee flexion for healthy patient (18°–20°)[30] in comparison with conventional UKA. This finding indicated the revision rate may be reduced by robotic-assisted UKA, which had been observed in our included studies (4/80 vs 7/80[18]; 0 vs 2.18%[13]), although the statistical difference was not achieved.
There are several limitations in this current meta-analysis. First, the sample size was not large for several clinical parameters, such as the revision rate, AKSS, OKS, FJS, VAS, and ROM, which may influence the assessment of the difference between robotic-assisted and conventional UKA. Second, the follow-up time was heterogeneous among different studies, which may also affect the results of follow-up related outcomes. Third, some studies were not RCT, which may lead to some potential bias. Accordingly, our results should be further confirmed by more RCTs and large-scale studies.
5. Conclusion
This meta-analysis demonstrates robotic-assisted UKA may be an effective and safe surgical procedure for treatment of unicompartmental knee osteoarthritis, with significantly reduced complication rate and improved knee excursion during weight acceptance compared with conventional UKA group.
Author contributions
Conceptualization: Fengjun Zhang.
Data curation: Fengjun Zhang, Hongcai Li, Zhaochen Ba.
Formal analysis: Fengjun Zhang, Hongcai Li.
Investigation: Zhaochen Ba, Chunguang Bo.
Methodology: Chunguang Bo.
Software: Zhaochen Ba.
Validation: Kai Li.
Writing – original draft: Fengjun Zhang.
Writing – review & editing: Fengjun Zhang.
Footnotes
Abbreviations: AKSS = American knee society score, CI = confidence interval, FJS = forgotten joint score, OKS = Oxford knee score, PCT = prospective cohort trials, RCT = randomized controlled trials, ROM = range of motion, RR = relative risk, SMD = standardized mean difference, TKA = total-knee arthroplasty, UKA = unicompartmental knee arthroplasty, VAS = visual analog scale.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Arirachakaran A, Choowit P, Putananon C, et al. Is unicompartmental knee arthroplasty (UKA) superior to total knee arthroplasty (TKA)? A systematic review and meta-analysis of randomized controlled trial. Eur J Orthop Surg Traumatol 2015;25:799–806. [DOI] [PubMed] [Google Scholar]
- [2].Siman H, Kamath AF, Carrillo N, et al. Unicompartmental knee arthroplasty vs total knee arthroplasty for medial compartment arthritis in patients older than 75 years: comparable reoperation, revision, and complication rates. J Arthroplasty 2017;32:1792–7. [DOI] [PubMed] [Google Scholar]
- [3].Rodriguez-Merchan EC. Medial unicompartmental osteoarthritis (MUO) of the knee: unicompartmental knee replacement (UKR) or total knee replacement (TKR). Arch Bone Jt Surg 2014;2:137–40. [PMC free article] [PubMed] [Google Scholar]
- [4].Horikawa A, Miyakoshi N, Shimada Y, et al. Comparison of clinical outcomes between total knee arthroplasty and unicompartmental knee arthroplasty for osteoarthritis of the knee: a retrospective analysis of preoperative and postoperative results. J Orthop Surg Res 2015;10:168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Von KA, Sodha S, Collins J, et al. Patient satisfaction after primary total and unicompartmental knee arthroplasty: an age-dependent analysis. Knee 2014;21:180–4. [DOI] [PubMed] [Google Scholar]
- [6].Bhattacharya R, Scott CEH, Morris HE, et al. Survivorship and patient satisfaction of a fixed bearing unicompartmental knee arthroplasty incorporating an all-polyethylene tibial component. Knee 2012;19:348–51. [DOI] [PubMed] [Google Scholar]
- [7].Kim KT, Song L, Kim TW, et al. The influence of postoperative tibiofemoral alignment on the clinical results of unicompartmental knee arthroplasty. Knee Surg Relat Res 2012;24:85–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Barbadoro P, Ensini A, Leardini A, et al. Tibial component alignment and risk of loosening in unicompartmental knee arthroplasty: a radiographic and radiostereometric study. Knee Surg Sports Traumatol Arthrosc 2014;22:3157–62. [DOI] [PubMed] [Google Scholar]
- [9].Collier MB, Eickmann TH, Sukezaki F, et al. Patient, implant, and alignment factors associated with revision of medial compartment unicondylar arthroplasty. J Arthroplasty 2006;21:108–15. [DOI] [PubMed] [Google Scholar]
- [10].Chatellard R, Sauleau V, Colmar M, et al. Medial unicompartmental knee arthroplasty: does tibial component position influence clinical outcomes and arthroplasty survival? Orthop Traumatol Surg Res 2013;99:S219–25. [DOI] [PubMed] [Google Scholar]
- [11].Hansen DC, Kusuma SK, Palmer RM, et al. Robotic guidance does not improve component position or short-term outcome in medial unicompartmental knee arthroplasty. J Arthroplasty 2014;29:1784–9. [DOI] [PubMed] [Google Scholar]
- [12].Bell SW, Anthony I, Jones B, et al. Improved accuracy of component positioning with robotic-assisted unicompartmental knee arthroplasty: data from a prospective, randomized controlled study. J Bone Joint Surg Am 2016;98:627–35. [DOI] [PubMed] [Google Scholar]
- [13].Gilmour A, Maclean A, Rowe P, et al. Robotic-arm assisted versus conventional unicompartmental knee arthroplasty. the 2 year clinical outcomes of a randomised controlled trial. J Arthroplasty 2018;33:S109–15. [DOI] [PubMed] [Google Scholar]
- [14].Maccallum KP, Danoff JR, Geller JA. Tibial baseplate positioning in robotic-assisted and conventional unicompartmental knee arthroplasty. Eur J Orthop Surg Traumatol 2016;26:93–8. [DOI] [PubMed] [Google Scholar]
- [15].Rodriguez F, Harris S, Jakopec M, et al. Robotic clinical trials of uni-condylar arthroplasty. Int J Med Robot 2005;1:20–8. [DOI] [PubMed] [Google Scholar]
- [16].Cobb J, Henckel J, Gomes P, et al. Hands-on robotic unicompartmental knee replacement: a prospective, randomised controlled study of the acrobot system. J Bone Joint Surg [Br] 2006;88-B:188–97. [DOI] [PubMed] [Google Scholar]
- [17].Herry Y, Batailler C, Lording T, et al. Improved joint-line restitution in unicompartmental knee arthroplasty using a robotic-assisted surgical technique. Int Orthop 2017;41:2265–71. [DOI] [PubMed] [Google Scholar]
- [18].Batailler C, White N, Ranaldi FM, et al. Improved implant position and lower revision rate with robotic-assisted unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2019;27:1232–40. [DOI] [PubMed] [Google Scholar]
- [19].Blyth M, Anthony I, Rowe P, et al. Robotic arm-assisted versus conventional unicompartmental knee arthroplasty: exploratory secondary analysis of a randomised controlled trial. Bone Joint Res 2017;6:631–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Fu J, Wang Y, Li X, et al. Robot-assisted vs. conventional unicompartmental knee arthroplasty: systematic review and meta-analysis. Orthopade 2018;47:1006–14. [DOI] [PubMed] [Google Scholar]
- [21].Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 2005;5:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Motesharei A, Rowe P, Blyth M, et al. A comparison of gait one year post operation in an RCT of robotic UKA versus traditional Oxford UKA. Gait Posture 2018;62:41–5. [DOI] [PubMed] [Google Scholar]
- [24].Kayani B, Konan S, Pietrzak JRT, et al. The learning curve associated with robotic-arm assisted unicompartmental knee arthroplasty. Bone Joint J 2015;100-B:1033–42. [DOI] [PubMed] [Google Scholar]
- [25].Millar LJ, Banger M, Rowea PJ, et al. A five-year follow up of gait in robotic assisted vs conventional unicompartmental knee arthroplasty. Gait Posture 2018;65:31–2. [Google Scholar]
- [26].Lonner JH, John TK, Conditt MA. Robotic arm-assisted UKA improves tibial component alignment: a pilot study. Clin Orthop Relat Res 2010;468:141–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Sodhi N, Khlopas A, Piuzzi NS, et al. The learning curve associated with robotic total knee arthroplasty. J Knee Surg 2017;31:17–21. [DOI] [PubMed] [Google Scholar]
- [28].Redmond JM, Asheesh G, Hammarstedt JE, et al. The learning curve associated with robotic-assisted total hip arthroplasty. J Arthroplasty 2015;30:50–4. [DOI] [PubMed] [Google Scholar]
- [29].Milner CE. Is gait normal after total knee arthroplasty? Systematic review of the literature. J Orthop Sci 2009;14:114–20. [DOI] [PubMed] [Google Scholar]
- [30].Kerrigan DC, Todd MK, Della CU, et al. Biomechanical gait alterations independent of speed in the healthy elderly: evidence for specific limiting impairments. Arch Phys Med Rehabil 1998;79:317–22. [DOI] [PubMed] [Google Scholar]


