Abstract
Aim:
Minority sexual orientation (i.e., Lesbian, Gay, Bisexual; LGB) is a risk indicator for mental health and substance use problems. Findings are inconsistent across studies investigating LGB substance use and risk factors, possibly due to heterogeneity in LGB subgroups. To inform models of substance use risk, we identified empirical patterns of substance use and related risk behaviors among LGB individuals.
Method:
LGB participants (N=343; Mage=35.5, SD=11.8; 71.4% = Female; 80.5% = White) were screened in an Emergency Department as part of a randomized controlled trial of an alcohol brief intervention. We conducted latent class analyses users using the AUDIT-C (12 month; frequency, quantity, & binge) and ASSIST (12 month; illicit or misused prescription substance). Multinomial regression was performed to test predictors of class membership including depression symptoms, driving after alcohol or marijuana, and sexually transmitted infection (STI) history.
Results:
A 3-class model fit best and included “low use alcohol, marijuana, and tobacco users,” (Low use; n=244) “hazardous alcohol, tobacco and marijuana users,” (Hazardous; n=74) and “high-risk polysubstance users” (HPU; n=25). The Low use class comprised the largest proportion of the sample across age, race/ethnicity, and sexual orientation. Compared to the Low use class, higher likelihood of depression symptoms, driving after alcohol or marijuana use, and STI was found for both Hazardous and HPU classes.
Conclusion:
Researchers and clinicians should consider substance use patterns within the LGB population to inform interventions that address a variety of complex needs such as allocating more support for LGB individuals endorsing high-risk polysubstance use.
Keywords: Lesbian, Gay, Bisexual, Substance Use, Polysubstance use, Latent Class Analysis
Introduction
Approximately nine million adults in the United States identify as Lesbian, Gay, or Bisexual (LGB) (Gates, 2011). Membership in this sexual orientation minority group is a risk indicator for alcohol and illicit substance use, substance use disorders, and mental health problems (Allen & Mowbray, 2016; Cochran & Mays, 2009; Grant et al., 2001; Livingston et al., 2017; McCabe et al., 2009; Phillips II et al., 2017). Furthermore, LGB adults experience more serious consequences associated with substance use (Kerr, Ding, & Chaya, 2014; Reed et al., 2010). Members of the LGB community are also at risk for mental health problems such as depression and anxiety (Allen & Mowbray, 2016; Cochran & Mays, 2009; Fish & Pasley, 2015), and engage in impulsive risky behaviors (e.g., unsafe sex), perhaps as a result of impaired decision-making associated with a problematic substance use trajectory (Dom et al., 2005; Herrick et al, 2010).
One explanation for the increased risk for substance use among the LGB community is minority stress theory that proposes stigma, prejudice, and discrimination lead to a hostile and stressful social environment that contributes to mental health and substance use problems (Meyer, 2003). LGB individuals face many stressors, including stigma associated with minority status, discrimination, bullying/victimization, negative internalized attitudes about sexual minorities, emotional distress related to acceptance by others, lack of supportive environments, negative reactions to disclosure, and lack of stable housing (Goldblach et al., 2014; Lea, Wit, & Reynolds, 2014; Rosario et al., 2002, 1996). Such stressors are associated with substance use risk in adolescence (Goldblach et al., 2014) and could explain the escalation of substance use into adulthood (Marshal et al, 2008; 2009; Moon et al., 2007). Multiple factors associated with the LGB population are largely attributed to the experience of minority stress (Meyer, 2003; Livingston et al., 2017; Phillips II et al., 2017). Indeed, depression symptoms and sexual risk may be the result of the intersection of multiple minority stress factors (i.e., gender and sexual orientation among lesbians and bisexual females) or the violation of cultural norms about masculinity (e.g., for bisexual men).
Past research identifying substance use patterns associated with LGB orientation almost exclusively compares LGB to heterosexual individuals (for a review see Green & Feinstein, 2012), showing that LGB status is a risk factor for substance use. Studies have documented sexual risk (Centers for Disease Control, 2011) associated with alcohol and illicit drug use among this population (Green & Feinstein, 2012). Although variable-centered approaches provide an overarching understanding of the relations between substance use and risk factors, this approach can overlook important individual-level differences in these associations. Furthermore, a person-centered approach allows an examination of individual-level patterns that emerge based on shared attributes of a heterogeneous population (i.e., LGB individuals) and provides a more nuanced understanding of risk factors based on individual substance use response patterns.
Despite these advantages to a person-centered approach, few studies have used this approach to examine substance use patterns in the LGB community. Such approaches examining substance use patterns have primarily been conducted using general population samples that allowed for the identification of polysubstance use and examination of demographic differences in empirically derived groups (Blow et al., 2011, Monga et al., 2007; Smith, Farrell, Bunting, Houston, & Shevlin, 2011). Furthermore, the studies that have used this approach among sexual minority populations have been restricted to men who have sex with men (e.g., McCarty-Caplan, Jantz, & Swartz, 2014; Newcomb, Ryan, Greene, Garofalo, & Mustanski, 2014). Nevertheless, in one study the majority of the sample comprised the Low use class and the riskier substance use classes was associated with more sexual risk (McCarty-Caplan, Jantz, & Swartz, 2014) and the other found classes that represented alcohol only and alcohol marijuana use were associated with the majority of the sample. These studies were limited by combining certain drug types into specific categories, including some but not all types of drug misuse in analyses or examining only sexual risks associated with use class (McCarty-Caplan, Jantz, & Swartz, 2014) or age and race/ethnicity associated with class membership (Newcomb, Ryan, Greene, Garofalo, & Mustanski, 2014). Thus, the present study fills a gap in the literature by examining substance use patterns in an LGB community, not limiting substances to specific sexual orientations (e.g., erectile dysfunction drugs), not combining drug types (e.g., prescription drug use), and not focusing on one risk factor (e.g., sexual risk, age and race/ethnicity).
Current Study
Due to the limited number of studies using a person-centered approach to examine substance use patterns and associated risk factors in the LGB community, the primary aim of this study was to evaluate these patterns among LGB individuals using latent class analysis. We determined a priori to examine substance use patterns in the LGB population in relation to specific risk factors. We intended for this approach to move beyond the heteronormative paradigm of comparing substance use behaviors between LGB individuals (which assumes a homogeneous group) to heterosexual individuals. In so doing, we also intend to 1) provide validity support to the empirically derived groups and 2) examine whether there are definable classes of LGB individuals who do and do not engage in problematic substance use. Therefore, we examined demographic characteristics of empirically derived groups as predictors of group members. Because prior studies have consistently shown that members of the LGB community are at risk for depression (e.g., Cochran & Mays, 2009), and engage in impulsive risky behaviors possibly due to impaired decision-making associated with substance use (Dom et al., 2005; Herrick et al, 2010), the following risk indicators were also included as predictors of group membership: 1) depression symptoms, 2) history of sexually transmitted diseases, and driving while intoxicated. We hypothesized that classes indicating lower risk substance use behaviors would be associated with lower depression scores, less sexual risk, and less driving while intoxicated.
Methods
Setting, Recruitment, & Procedure
This study reports on a secondary analysis from screening data collected as part of a randomized controlled trial (Project Health Explorer) of an alcohol use brief intervention delivered in the Emergency Department (ED) at the University of Michigan Health System located in Ann Arbor, Michigan, a Level 1 trauma center (see Fernandez et al., 2019). Studyeligible adult patients (ages 21 to 65) presenting to the ED were recruited from February 2012 through May 2014 by study staff and asked to complete a computerized health screening. Interested patients provided written informed consent and then self-administered a 15minute screener on a tablet computer (total N=7635). Exclusion criteria included presenting to the ED with altered cognition that would impact ability to consent (e.g., active psychosis, psychiatric admission, intoxicated, unconscious) or for reasons that would require intensive social work intervention during the ED visit (e.g., suicidal ideation, sexual assault), inability to read/speak English, visual/hearing impairment, violent, participation refusal, blood alcohol content over 0.10, and currently engaging in alcohol treatment. Screened participants were remunerated with a small gift valued at $1.00 (e.g., puzzle book, playing cards, travel mug, pens). Only those identified as LGB who completed screening surveys for the RCT and provided information regarding sexual behaviors (n=343) were included in this study. All procedures were approved by the University of Michigan Institutional Review Board and a Certificate of Confidentiality was obtained from the National Institutes of Health.
Measures
Demographic characteristics and sexual orientation classification.
Demographic items (e.g., age, race, ethnicity, sex) were adapted from prior research (Smith et al., 2006; Office of Applied Studies, 2009). Sexual orientation was assessed by combining each participant’s response to the question asking about their sex (i.e., male or female) with his or her response to a one-item question asking about their current sexual preference (e.g., to only have sex with female(s), to only have sex with male(s), or to have sex with females and males) (Chestnut Health Systems, 2006). Responses were combined to classify each person as a member of one of four sexual minority groups: Lesbian (female who only has sex with females), Gay (male who only has sex with males), Bisexual Female (female who has sex with females or males), and Bisexual Male (male who has sex with females or males).
Substance use measures.
We used the 3 individual items from the Alcohol Use Disorders Identification Test –Consumption (AUDIT-C) to measure alcohol consumption (frequency, quantity, and binge-drinking [defined as ≥ 5 drinks on any one occasion]) during the past twelve months (Bush et al., 1998). Using the past 12 months as a referent, participants rated the frequency of their alcohol use on a scale from 0 = “Never” to 4 = “Four or more times per week,” the quantity of their alcohol use on a scale from 0 = “1 or 2” to 4 = “10 or more,” and the frequency of binge-drinking on a scale from 0 = “Never” to 4 = “Daily or almost daily.” Each item was dichotomized and entered as a binary indicator in the latent class analyses. Specifically, we used a cutoff of ≥ 3 (2–3 times per week) for frequency, ≥ 3 (7 to 9 drinks) for quantity, and ≥ 3 (Weekly) for binge drinking. We also used items selected from the National Institute on Drug Abuse (NIDA) Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST; WHO ASSIST Working Group, 2002) to measure illicit substance use (i.e., marijuana, cocaine, methamphetamine, inhalants, hallucinogens, and heroin), non-medical use of three prescription drugs (i.e., sedatives, stimulants, opioids), and tobacco use. Participants rated the frequency of use during the past 12 months on a scale from 0 = “Never” to 6 = “Daily or Almost Daily.” We dichotomized use of each substance for analyses (any past 12-month use: yes/no). Thus, substance use classes were indicated by 13 substance use variables.
Depression.
We used the Patient Health Questionnaire – 8 (PHQ-8; Kroenke et al., 2009) to assess symptoms of depression (e.g., “Feeling down, depressed or hopeless,” “Little interest or pleasure in doing things”). This 8-item measure asked participants to rate how frequently he or she experienced several depression symptoms during the two weeks prior to screening on a scale from 0 = “Not at all” to 3 = “Nearly every day.” Total scores greater or equal to 10 indicate clinically significant depression symptoms (Kroenke et al., 2009).
Risky behaviors.
Driving after using marijuana was assessed with one item from the Young Adult Drinking-Driving Questionnaire (Donovan, 1993). Specifically, participants were asked “In the past 12 months, how many times did you drive while a little high on Marijuana and responded on a 5-point scale from 0 = “Never” to 4 = “10 or more times.” Driving after alcohol consumption was measured using one item from the National Highway Traffic Safety Administration (National Survey of Drinking and Driving Attitudes and Behaviors, 2008) that asked “In the past 12 months, have you driven a motor vehicle within 2 hours after drinking any alcoholic beverages?” (yes/no). As an indicator of engaging in risky sexual behaviors, we included one item assessing whether they ever (yes/no) had a sexually transmitted infection (i.e., “Has a doctor or other health care professional ever told you that you had genital herpes, genital warts, gonorrhea (GC or the clap), HPV, syphilis, trichomonas (trich), and/or chlamydia?”) (National Health and Nutrition Examination Survey, 2010).
Analytic Strategy
Latent class analysis was conducted using MPlus version 7.4 (Muthén & Muthén, 2012). LCA was used to estimate the latent structure of 13 binary substance use behavior indicators. Estimated probabilities that an individual would be in a specific latent class and parameters based on a set of item-response probabilities that were linked to a latent class were produced through the LCA (Collins & Lanza, 2010). For the current study, membership probabilities were based on substance use behavior classes and the item-response probabilities were based on the 13 substance use behaviors that also served as guides for labeling and interpreting each latent class. Maximum likelihood with robust standard errors was used for model estimation.
Several fit indices were used to select the latent class structure including Bayesian Information Criteria (BIC; Schwarz, 1978), bootstrapped likelihood ratio test (BLRT; McLachlan & Peel, 2000), and Lo-Mendell-Rubin likelihood ratio test (LMR; Lo et al., 2001), parsimony, and theory. To interpret fit indices, BIC is considered better when lower; BLRT and LMR-LRT significant p-values suggest the current model is preferred to a model with one less class. Entropy was also used to assess overall degree of classification uncertainty with values above 0.80 suggesting more distinction among classes (Celeux & Soromenho, 1996). For the current study, the best model was chosen using a balance of parsimony, theoretical interpretability, and goodness of fit. To examine predictors of class membership, a multinomial regression was conducted simultaneously while fitting each model. Age and race/ethnicity were added as control variables and the following were added as predictors of class membership: depression scores, driving after marijuana use, driving after alcohol use, and ever having a sexually transmitted infection.
Results
Participant Characteristics
Based on responses to items about sexual preferences we classified 126 participants as a bisexual female (36.7%), 119 as lesbian (34.7%), 73 as gay (21.3%), and 25 as a bisexual male (7.3%). Additionally, participants had a mean age of 35.5 (SD=11.8) years, 71.4% were female, and 80.5% were white/Caucasian.
Latent Class Analysis
Results of the LCA are presented in Table 1. The 3-class model provided the most parsimony, best goodness of fit, and theoretical interpretability. For the 3-class model, BIC was lowest as compared to the 2- and 4-class solutions. Although LMR was significant for the 2-class model, other fit indices supported the 3-class solution. Degree of classification in the 3-class model was highest compared to the 2-and 4-class solutions. Furthermore, the indicators in the 3class model were theoretically supported.
Table 1:
Model Fit and Entropy for Latent Class Analysis
| BIC | BLRT | LMR | Entropy | |
|---|---|---|---|---|
| 2-class model | 2910.37 | p<.001 | p<.001 | 0.83 |
| 3-class model | 2907.87 | p<.001 | p =.119 | 0.84 |
| 4-class model | 2936.03 | p<.001 | p=.023 | 0.82 |
Note: Bold denotes best model fit. BIC = Baysian Information Criteria; BLRT = Bootstrapped likelihood ratio test; LMR = Lo-Mendell-Rubin likelihood ratio test
The probabilities for engaging in substance use behaviors by latent class are depicted in Figure 1 and demographic information based on most likely class membership is presented in Table 2. For the “Low use alcohol, marijuana, and tobacco users” (Low Use) class, individuals had the lowest levels of alcohol use and the lowest rates of tobacco and marijuana use. In the “Hazardous alcohol and marijuana users” (Hazardous) class, individuals engaged in higher levels of alcohol use frequency, quantity, and binge-drinking, tobacco use, and marijuana use, and higher levels of hallucinogen use than the Low use class; however, this class did not report much misuse of prescription substances (e.g., opioids). The “High-risk polysubstance users” (HPU) class engaged in the highest levels of other drug use as well as the highest levels of alcohol use frequency, binge-drinking, and marijuana use, and notably, misuse of prescription substances. Notably, the Low use class represented the oldest and largest percentages of the sample across sex, race/ethnicity, and sexual orientation.
Figure 1.
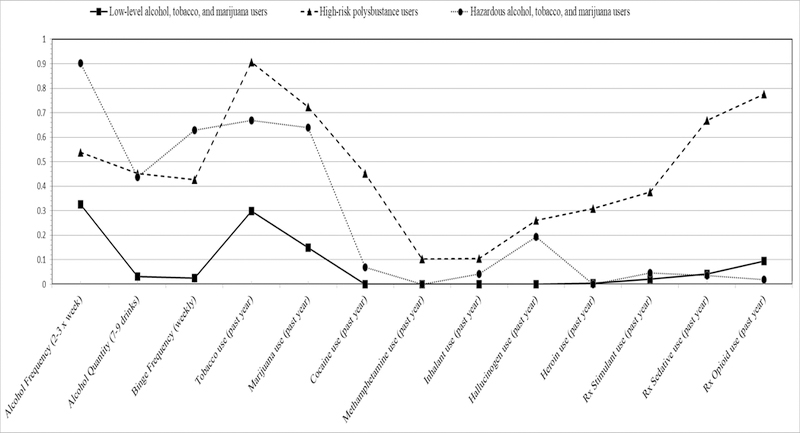
Substance use groups derived by latent class membership
Table 2:
Latent class counts for total sample and demographic information for each class
| Low use alcohol, tobacco, and marijuana users | Hazardous alcohol and marijuana users | High-risk polysubstance users | |
|---|---|---|---|
| Total Sample (n=343) | 244 (71.1%) | 74 (21.6%) | 25 (7.3%) |
| Age - Mean (Standard Deviation) | 36.95 (11.98) | 32.22 (11.32) | 30.80 (9.65) |
| Sex- n (%) | |||
| Male (n=98; 28.6%) | 62 (63.3%) | 32 (32.6%) | 4 (4.1%) |
| Female (n=245; 71.4%) | 182 (74.3%) | 42 (17.1%) | 21 (8.6%) |
| Race/Ethnicity- n (%) | |||
| White (n=276; 80.5%) | 202 (73.2%) | 54 (19.6%) | 20 (7.2%) |
| Other race (n=67; 19.5%) | 42 (62.7%) | 20 (29.9%) | 5 (7.4%) |
| Sexual Orientation- n (%) | |||
| Gay (n=73) | 48 (65.8%) | 24 (32.9%) | 1 (1.3%) |
| Lesbian (n=119) | 99 (83.2%) | 12 (10.1%) | 8 (6.7%) |
| Bisexual - Male (n=25) | 14 (56.0%) | 8 (32.0%) | 3 (12.0%) |
| Bisexual - Female (n=126) | 83 (65.9%) | 30 (23.8%) | 13 (10.3%) |
Note: Sexual orientation was determined by combining sex (i.e., male or female) with current sexual preference (e.g., to only have sex with female[s]): Lesbian (female who only has sex with females), Gay (male who only has sex with males), Bisexual Female (female who has sex with females or males), and Bisexual Male (male who has sex with females or males).
Multinomial logistic regression
Results of the multinomial logistic regressions for depression, driving after alcohol use, driving after marijuana use, and ever having a sexually transmitted infection, are reported in Table 3. The “Low use” class served as the reference category. After controlling for age and race/ethnicity, those who reported having higher depression scores, more driving after alcohol use, and ever having a sexually transmitted infection were more likely to be in the Hazardous and HPU classes (AORs = 1–09-6.96, ps < .05).
Table 3:
Multinomial Regression for risk behaviors
| AOR | p-value | |
|---|---|---|
| Depression scores | ||
| High-risk polysubstance users | 1.18 | <.001 |
| Hazardous alcohol, tobacco, and marijuana users | 1.09 | .014 |
| Driving after alcohol use | ||
| High-risk polysubstance users | 6.27 | .001 |
| Hazardous alcohol, tobacco, and marijuana users | 5.17 | <.001 |
| Driving after marijuana use | ||
| High-risk polysubstance users | 2.05 | .026 |
| Hazardous alcohol, tobacco, and marijuana users | 2.27 | .005 |
| Sexually Transmitted Infection | ||
| High-risk polysubstance users | 6.96 | .001 |
| Hazardous alcohol, tobacco, and marijuana users | 2.56 | .049 |
Note: Low-level alcohol, tobacco, and marijuana user class is reference category; Age and Race/ethnicity were added as control variables; AOR=Adjusted Odds Ratio; Bold denotes significance at p<.05
Discussion
This is one of the first studies to use a person-centered approach to examine substance use risk behaviors with a LGB sample that overcomes the limitations of focusing primarily on risk factors using variable-centered approaches and using a heteronormative paradigm, while also examining associations with depression, sexual risk, and drugged driving. Empirically derived groups ranged from those primarily engaging in low levels of alcohol, tobacco, and marijuana use to those using a combination of licit, illicit, and prescription substances. Notably, findings indicated the largest class was comprised of a lower risk group of primarily alcohol drinkers with low endorsement of tobacco and marijuana use. Moreover, with the Low use class serving as the reference, there was a higher likelihood of being in the Hazardous and HPU classes among those reporting greater depression symptoms, more driving after alcohol/marijuana use, and having a history of sexually transmitted infections.
In addition to examining specific risk factors associated with substance use and the LGB community, results investigating drugged driving distinguished the lower risk substance use classes from the Hazardous and HPU classes. This is one of the first studies, to our knowledge, to examine drugged driving behaviors among the LGB community. Consistent with other studies of drugged driving, those who less frequently participate in risky alcohol use or marijuana use are less likely to engage in high risk substance-related behaviors such as drugged driving (Bonar et al., 2018; Arterberry, Treloar, & McCarthy, 2017). It appears that the LGB community may have additive risk, where sexual minorities experience specific risk factors associated with minority stress such as depression and sexual risk that may be compounded by other substance use risk factors such as drugged driving that increase the likelihood of acting impulsively and experiencing serious negative consequences. It is critical that clinicians and researchers understand the complexities and synergistic effects of sexual minority status, polysubstance use, and substance use risk factors, when developing targeted interventions within the LGB community.
These findings extend previous literature by examining heterogeneity of substance use behaviors within the LGB population. One-third of the sample was classified in higher risk classes - either Hazardous or HPU. The Hazardous and HPU classes were comprised of mostly women (i.e., bisexual females and lesbians) and bisexual males, which is likely due to the fact that they comprised the majority of the sample. Although caution is warranted in not overgeneralizing demographic characteristics, our findings are consistent with other studies examining substance use in relation to sexual orientation (McCabe et al., 2009; Ploderl & Tremblay, 2015; Lee et al., 2016; Phillips II et al., 2017). Similarly, gay men seemed to be at less risk for risky alcohol use and polysubstance use than bisexual counterparts (Green & Feinstein, 2012), which supports the findings in this study that showed a larger number of gay men being in the Low use or Hazardous classes as opposed to the HPU class. However, caution is warranted in overgeneralizing this finding due to fewer gay men being represented in the present sample. Importantly, prior research regarding sex differences in prescription drug misuse (opioids) suggests women are more likely than men to report misuse (McHugh et al., 2013) and national prevalence rates indicate female sexual minorities engage in prescription opioid misuse more than male counterparts (Medley, Lipari, Bose, Cribb, Kroutil, & McHenry, 2016), which provides some support for our finding that lesbian and bisexual women comprised the highest percentage of the HPU class. Of critical importance is that two-thirds of the sample were in the lowest risk substance use class. This finding highlights the importance of clinicians and researchers recognizing that sexual minority status, in and of itself, may not confer risk for every member of that minority group.
Study limitations include social desirability and retrospective recall biases, which may have influenced reporting of sensitive information, such as substance use patterns, sexual behaviors, and risk taking; however, the study employed common procedures to encourage accurate self-report (e.g., computer screeners, assurance of anonymity). Additionally, generalizability of this study is limited by the single geographic location, lack of diverse race/ethnicity, not assessing other minority statuses such as gender identity, and not including sexual behavior, sexual identity, and sexual attraction to ascertain sexual orientation. Lastly, we did not attempt to screen individuals who presented to the ED, indicated problems related to suicidality, elevated BAC, or severe injuries, thus limiting our sample to relatively stable (medically and psychiatrically) individuals who may or may not be more likely to identify as LGB. Given that previous research has shown that LGB individuals are at greater risk for suicidality (Ploderl & Tremblay, 2015), it is possible we did not approach some LGB individuals who may have presented to the ED for this reason and thus may have potentially more severe patterns of substance use. Future research should consider including multiple risk and protective factors that impact minority stress and include a more diverse demographic sample to better understand the processes of multiple minority statuses on substance use protective and risk factors.
Understanding substance use patterns among LGB individuals allows for optimization of resource allocation to those most at risk for problems associated with consumption. Using substance use patterns as a marker for risk obviates problems associated with minority sexual orientation behaviors among individuals who are uncomfortable disclosing their minority status, sexual behaviors, or who do not identify as “gay,” “lesbian,” or “bisexual,” but might otherwise be at risk based on their sexual orientation behaviors or identity. Thus, detecting substance use patterns may be more meaningful than basing risk profiles solely on disclosed sexual minority identification or sexual orientation behavior. Researchers and clinicians should consider the variety of substance use patterns within this population and offer interventions that address a variety of complex needs such as allocating more support for LGB individuals endorsing highrisk polysubstance use, who may be at increased risk for overdose given increased alcohol consumption and misuse of prescription drugs.
Highlights.
Low use class comprised largest proportion of the LGB sample
Greater depression symptoms associated with hazardous and high-risk classes
More driving after alcohol use associated with hazardous and high-risk classes
More driving after marijuana use associated with hazardous and high-risk classes
Positive history of STIs associated with hazardous and high-risk classes
Acknowledgements:
The authors would like to thank the patients and staff at the University of Michigan Emergency Department for their participation and support of this study.
Funding: This study was supported by a grant to FCB from NIAAA (#AA018659). AKD and BJA were supported by an NIAAA T32 postdoctoral training grant (#AA007477), AKD was subsequently supported by a NIDA T32 (#DA07209), and EEB was supported by a NIDA career development award (#DA036008). The funding sources had no role in the design/execution of this study or the interpretation or communication of findings
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of Interest: The authors have no conflicts of interest to declare
References
- Allen JL & Mowbray O (2016). Sexual orientation, treatment utilization, and barriers for alcohol related problems: Findings from a nationally representative sample. Drug and Alcohol Dependence, 161, 323–330. [DOI] [PubMed] [Google Scholar]
- Blow FC, Walton MA, Barry KL, Murray RL, Cunningham RM, Massey LS, Chermack ST, Booth BM (2011). Alcohol and Drug Use among patients presenting to an inner city Emergency Department: A Latent Class Analyses. Addictive Behaviors, 8, 93–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonar EE, Arterberry BJ, Davis AK, Cunningham RM, Blow FC, Collins RL, & Walton MA (2018). Prevalence and motives for drugged driving among emerging adults presenting to an emergency department. Addictive behaviors, 78, 80–84. doi: 10.1016/j.addbeh.2017.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonnell MB, Fihn SD, & Bradley KA, 1998. The AUDIT alcohol consumption questions, AUDIT-C: An effective brief screening test for problem drinking. Arc. Intern. Med 158, 1789–1795. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance, 2011. Atlanta: U.S. Department of Health and Human Services. 2012; Available: http://www.cdc.gov/std/stats11/surv2011.pdf. [Google Scholar]
- Celeux G, & Soromenho G (1996). An entropy criterion for assessing the number of clusters in a mixture model. Journal of classification, 13, 195–212. [Google Scholar]
- Chestnut Health Systems. Global Appraisal of Individual Needs (GAIN). GAIN- I (Initial) version 5.4.0 (2006). (Survey; ) [Google Scholar]
- Cochran SD & Mays VM (2009). Burden of psychiatric morbidity among lesbian, gay, and bisexual individual in the California Quality of Life Survey. Journal of Abnormal Psychology, 118, 647–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins LM, & Lanza ST (2010). Latent class and latent transition analysis: With applications in the social, behavioral, and health sciences (Vol. 718). Wiley. [Google Scholar]
- Dom G, sabbe B, Hustijn W & Van Den Brink W (2005). Substance use disorders and the orbitofrontal cortex: Systematic review of behavioral decision-making and neuroimaging studies. The British Journal of Psychiatry, 187, 209–220. [DOI] [PubMed] [Google Scholar]
- Donovan J (1993). Young Adult Drinking-Driving: Behavioral and Psychosocial Correlates. J. Stud. Alcohol 54: 600–613. [DOI] [PubMed] [Google Scholar]
- Fernandez AC, Waller R, Walton MA, Bonar EE, Ignacio RV, Chermack ST, … & Blow FC (2019). Alcohol use severity and age moderate the effects of brief interventions in an emergency department randomized controlled trial. Drug and alcohol dependence, 194, 386–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fish JN & Pasley K (2015). Sexual (monitory) trajectories, mental health, and alcohol use: A longitudinal study of youth as they transition to adulthood. Journal of Youth and Adolescence, 44, 1508–1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gates GJ (2011). How many people are lesbian, gay, bisexual, and transgender? Executive Summary: The Williams Institute, 1–8.
- Goldblach JT, Tanner-Smith EE, Bagwell M, & Dunlap S (2014). Minority stress and substance use in sexual minority adolescents: A meta-analysis. Prevention Science, 15, 350–363. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS & Harford TC (2001). Age at onset of alcohol use and DSM-IV alcohol abuse and dependence: A 12-year follow-up. Journal of Substance Abuse, 13, 493–504. [DOI] [PubMed] [Google Scholar]
- Green KE, & Feinstein BA (2012). Substance Use in Lesbian, Gay, and Bisexual Populations: An Update on Empirical Research and Implications for Treatment. Psychology of Addictive Behaviors, 26(2), 265–278. 10.1037/a0025424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrick AL, Matthews AK & Garafalo R (2010). Heath risk behaviors in an urban sample of young women who have sex with women. Journal of Lesbian Studies, 14, 80–92. [DOI] [PubMed] [Google Scholar]
- Kerr DL, Ding K, & Chaya J (2014). Substance use of lesbian, gay, bisexual and heterosexual college students. American Journal Of Health Behavior, 38, 951–962. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Strine TW, Spitzer RL, Williams JBW, Berry JT, & Mokdad AH (2009). The PHQ-8 as a measure of current depression in the general population. Journal of Affective Disorders, 114, 163–173. [DOI] [PubMed] [Google Scholar]
- Lea T, de Wit J, & Reynolds R (2014). Minority stress in lesbian, gay, and bisexual young adults in Australia: Associations with psychological distress, suicidality, and substance use. Archives of Sexual Behavior, 43, 1571–1578. [DOI] [PubMed] [Google Scholar]
- Levahot K & Simoni JM (2011). The impact of minority stress on mental health and substance use among sexual minority women. Journal of Consulting and Clinical Psychology, 79, 159–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston NA, Flentje A, Heck NC, Szalda-Petree A, & Cochran BN (2017). Ecological momentary assessment of daily discrimination experiences and nicotine, alcohol, and drug use among sexual and gender minority individuals. Journal of Consulting and Clinical Psychology, 85, 1131–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo Y, Mendell N & Rubin D (2001). Testing the number of components in a normal mixture. Biometrika, 88, 767–778. [Google Scholar]
- Marshal MP, Friedman MS, Stall R, King KM, Miles J, Gold MA, Bukstein OG, & Morse JQ (2008). Sexual orientation and adolescent substance use: A meta-analysis and methodological review. Addiction, 103, 546–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshal MP, Friedman MS, Stall R & Thompson AL (2009). Individual trajectories of substance use in lesbian, gay, and bisexual youth and heterosexual youth. Addiction, 104, 974–981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Hughes TL, Bostwick WB, West BT, & Boyd CJ (2009). Sexual orientation, substance use behaviors and substance dependence in the United States. Addiction, 104, 1333–1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarty-Caplan D, Jantz I, & Swartz J (2014). MSM and drug use: A latent class analysis of drug use and related sexual risk behaviors. AIDS and Behavior, 18, 1339–1351. [DOI] [PubMed] [Google Scholar]
- McHugh RK, DeVito EE, Dodd D, Carroll KM, Potter JS, Greenfield SF, … & Weiss RD (2013). Gender differences in a clinical trial for prescription opioid dependence. Journal of substance abuse treatment, 45, 38–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLachlan G, & Peel D (2000). Wiley series in probability and statistics. Finite Mixture Models, 420–427.
- Medley G, Lipari RN, Bose J, Cribb DS, Kroutil LA, & McHenry G (2016). Sexual orientation and estimates of adult substance use and mental health: Results from the 2015 National Survey on Drug Use and Health. Substance Abuse and Mental Health Services Administration
- Meyer I (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129, 674697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moon MW, Fornili K & O’Briant AL (2007). Risk comparison among youth who repot sex with same-sex versus both-sex partners. Youth & Society, 38, 267–284. [Google Scholar]
- Monga N, Rehm J, Fischer B, Brissette S, Bruneau J, El-Guebaly N, … & Fallu JS (2007). Using latent class analysis (LCA) to analyze patterns of drug use in a population of illegal opioid users. Drug & Alcohol Dependence, 88, 1–8. [DOI] [PubMed] [Google Scholar]
- Muthén LK and Muthén BO (1998–2015). Mplus User’s Guide. Seventh Edition. Los Angeles, CA: Muthén & Muthén. National Health and Nutrition Examination Survey (NHANES, 2010). Sexual Behavior – SXQ http://www.cdc.gov/nchs/data/nhanes/nhanes_09_10/ai_sxq_f.pdf
- National Survey of Drinking and Driving Attitudes and Behaviors (2008). National Highway Traffic Safety Administration ( NHTSA) http://www.nhtsa.gov/Driving+Safety/Impaired+Driving/National+Survey+of+Drinking+and+Driving+Attitudes+and+Behaviors:+2008 [DOI] [PubMed]
- Newcomb ME, Ryan DT, Greene GJ, Garofalo R, & Mustanski B (2014). Prevalence and patterns of smoking, alcohol use, and illicit drug use in young men who have sex with men. Drug & Alcohol Dependence, 141, 65–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of Applied Studies. (2009). 2010 National Survey on Drug Use and Health: CAI Specifications for Programming English Version Rockville, MD: Substance Abuse and Mental Health Services Administration; [Available at http://oas.samhsa.gov/] [Google Scholar]
- Phillips G II, Turner B, Salamanca P, Birkett M, Hatzenbuehler ML, Newcomb ME, Marro R, & Mutanski B (2017). Victimization as a mediator of alcohol use disparities between sexual minority subgroups and sexual majority youth using the 2015 National Youth Risk Behavior Survey. Drug and Alcohol Dependence, 178, 355–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ploderl M & Tremblay P (2015). Mental health of sexual minorities. A systematic review. International Review of Psychiatry, 27, 367–385. [DOI] [PubMed] [Google Scholar]
- Reed E, Prado G, Matsumoto A, & Amaro H (2010). Alcohol and drug use and related consequences among gay, lesbian and bisexual college students: Role of experiencing violence, feeling safe on campus, and perceived stress. Addictive Behaviors, 35, 168–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosario M, Rotheram-Borus M & Reid H (1996). Gay-related stress and its correlates among gay and bisexual adolescents of predominately black and Hispanic background. Journal of Community Psychology, 24, 136–159. [Google Scholar]
- Rosario M, Schrimshaw EW, Hunter J & Gwadz M (2002). Gay-related stress and emotional distress among gay, lesbian, and bisexual youths: A longitudinal examination. Journal of Consulting and Clinical Psychology, 70, 967–975. [DOI] [PubMed] [Google Scholar]
- Schwarz G (1978). Estimating the dimension of a model. The Annals of Statistics, 6, 461–464. [Google Scholar]
- Smith GR, Burnam MA, Mosley CL, Hollenberg JA, Mancino M, Grimes W (2006). Reliability and validity of substance abuse outcomes module. Psychiatric Services, 57, 1452–1460. [DOI] [PubMed] [Google Scholar]
- Smith GW, Farrell M, Bunting BP, Houston JE, & Shevlin M (2011). Patterns of polydrug use in Great Britain: Findings from a national household population survey. Drug & Alcohol Dependence, 113(2), 222–228. [DOI] [PubMed] [Google Scholar]
- WHO ASSIST Working Group, 2002. The Alcohol, Smoking, and Substance Involvement Screening Test, ASSIST: development reliability and feasibility. Addiction 97, 1183–1194. [DOI] [PubMed] [Google Scholar]


