Abstract
Objective
China have implemented population-based esophageal cancer (EC) screening programs, however, the participant rates were relatively low. This study was conducted to examine the association between cancer prevention knowledge and EC screening participation rates (PRs).
Methods
Data in the analyses were obtained from a population-based cancer screening program in four provinces in China since 2007. In the course of 2007−2016, participants who were evaluated as high risk for EC and subsequently recommended for endoscopy examination were included in the final analysis. One-way analysis of variance test, Chi-square test and logistic regression analysis were applied.
Results
A total of 28,543 individuals assessed as high-risk population for EC were included in this study, with 13,036 males (45.67%) and 15,507 females (54.33%). The prevalence rates of current smoking and alcohol drinking were higher in males (58.25% and 44.22%, respectively) than in females (5.35% and 4.05%, respectively). Participants of females, and those who had older age, lower income, as well as higher education level and cancer prevention knowledge level were more likely to undergo endoscopy. Multivariable analysis showed that higher cancer prevention knowledge was associated with higher PR for endoscopic screening [adjusted odd ratio (aORQ4/Q1) =1.511, 95% confidence interval (95% CI): 1.398−1.632] among our study subjects. This association between cancer prevention knowledge and compliance with endoscopic screening also tends to be strong within subgroups of males, females, aged below 60 years, aged 60 years and above, and lower level of education (illiterate individuals and those with junior high education or less).
Conclusions
Our results displayed a positive relationship between cancer prevention knowledge and PRs for endoscopic screening, implying cancer prevention awareness being an independent influence factor for compliance with EC screening. Promoting public campaigns about comprehensive knowledge of cancer prevention seemed to be a reasonable and effective strategy to improve population PRs for EC screening.
Keywords: Cancer prevention knowledge, esophageal cancer screening, participation rate, compliance
Introduction
Esophageal cancer (EC) was the seventh most common cancer and sixth leading cause of cancer death in the world, with appropriately 570,000 new EC cases and 510,000 EC deaths in 2018 (1). The global distribution of EC burden nevertheless showed a huge variation geographically. According to International Agency for Research on Cancer (IARC), 53.73% and 55.73% of global EC cases and deaths occurred in China, respectively (1). To date, there were about 240,000 new EC cases and 190,000 EC deaths every year in China, accounting for 6.26% of all new cancer cases and 8.04% of all cancer deaths nationwide (2). The 5-year survival rate for EC was only 30.3% in Chinese population (3).
The prevention of EC could be broadly divided into primary and secondary prevention (4). Primary prevention is essentially behavioral modification, seeking to control the etiological agents of EC (4), such as smoking and alcohol drinking. Compared with non-smokers, the risk of developing EC could be 1.47 and 1.24 fold in male and female smokers, respectively, and the relative risk of alcohol drinking for esophageal squamous cell carcinoma (ESCC) could be 1.78 for both males and females (5). In China, the proportions of EC attributed to smoking and alcohol drinking were 18.6% and 19.2% for males, and 1.7% and 3.6% for females according to a pooled analysis targeting Chinese population (5). China had the highest number of tobacco users and alcohol consumers in the world while tremendous difference remained between two genders. In 2010, the prevalence of current smoking was 54.0% for males and 2.6% for females in China and the percentage for alcohol drinking were 57.7% and 14.5%, respectively (6,7).
Secondary prevention for EC mainly relies on early detection and treatment, which can be achieved by cancer screening (4). Many population-based researches on Chinese population in high-risk regions showed that endoscopy screening, early diagnosis and treatment could effectively reduce incidence and mortality rates of EC, as well as increase 5-year survival to more than 88.9% for patients discovered by esophageal endoscopy screening (8-10). The promotion strategies for early detection and treatment of EC were enhanced in China since 2005, however, the compliance of EC screening in Chinese population was still unsatisfactory (11,12). Therefore, it is of vital importance to further explore influencing factors that could increase participation rates (PRs) for population-based EC screening.
Many epidemiological studies showed that poor public awareness was the predominant factor of negative health seeking behaviors and low PRs for cancer screening programs (13-16). In addition, an ecological study also revealed the relationship between low cancer awareness and poor cancer prognosis (17). In China, although cancer prevention knowledge or awareness as well as PRs for EC screening has been reported before, the evidence on whether cancer prevention awareness could influence their behaviors of participating in EC screening was scarce but desperately needed for EC prevention and control.
Thus, we undertook this study to explore the association between cancer prevention knowledge and EC screening PRs in an ongoing population-based cancer screening program in rural China.
Materials and methods
Study design and subjects
We performed cross-sectional surveys under the framework of Esophageal, Stomach and Liver Cancer Screening Program (ESLCSP) in four provinces in China. In the ESLCSP for EC screening, all targeted residents aged 40−69 years old living in the selected areas will receive the invitation from our program. In the first year of any selected area in the program, cancer prevention core knowledge questionnaires were investigated by trained medical staff. Signed informed consent was obtained for each participant.
For the present study, data were obtained from ESLCSP for EC screening from 2007 to 2016. The inclusion criteria were: 1) permanent residents in the target counties or villages, aged 40−69 years old, and no history of endoscopic examination within 3 years before the initial interview; 2) no history of cancer, mental disorder, or any contraindications for endoscopy; 3) completed questionnaires of core knowledge on cancer prevention and EC-related risk factors at baseline; 4) received endoscopy examination; and 5) signed informed consents with agreement to complete all phases. In this study, a total of 70,071 participants from 13 counties in Jiangsu, Anhui, Shandong and Henan province, conducting investigations of core knowledge on cancer prevention in the first year of the program were recruited from 2007 to 2016. After excluding participants with invalid risk assessment results (n=1,154), and participants who were diagnosed with cancer (n=8) before recruitment, as well as those assessed as non-high-risk individuals for EC (n=40,366), 28,543 remaining participants were included for the final analysis.
Investigations of core knowledge about cancer prevention
Basic information, including name, gender, date of birth as well as identity number, was collected. Contents of core knowledge on cancer prevention include 9 items consisting of 5 single-choice questions and 4 multiple-choice questions. A detailed description of the items and primary results can be found in our previous articles (18). We allocated 1 point for each correct answer of single item and 1 point for each correct answer of multiple items, resulting in a total score of 0−20 (Supplementary Table S1). The total scores for each individual was finally converted to a percentage system to provide a knowledge score on cancer prevention (ranged 0−100 points).
S1.
Items for cancer prevention knowledge and associated points
| Items | Point |
| Single-choice items | |
| Cancer has been a common disease in China (yes, no) | 1 |
| Cancer has been a common cause of death in China (yes, no) | 1 |
| Do you know that the number of people who has cancer getting more and more since the 70’s (yes, no) | 1 |
| One out of three cancers can be reduced by effective preventive measures (yes, no) | 1 |
| One out of three cancers can be cured if they are discovered, diagnosed or treated in the early stage (yes, no) | 1 |
| Multi-choices items | |
| Which cancers do you think are common in China | |
| Lung cancer, liver cancer, stomach cancer, esophageal cancer (yes, no) | 1 |
| Breast cancer, cervical cancer (yes, no) | 1 |
| Colonic cancer, rectal cancer (yes, no) | 1 |
| Do you know the main factors of cancer in China | |
| Smoking, drinking (yes, no) | 1 |
| Inappropriate dietary habit (yes, no) | 1 |
| Various infectious factors (yes, no) | 1 |
| Hazard of occupational factors (yes, no) | 1 |
| What kind of preventive measures can reduce cancer | |
| Quit smoking, drinking less (yes, no) | 1 |
| Balanced diet and proper workout (yes, no) | 1 |
| Inoculation against the hepatitis vaccine (yes, no) | 1 |
| Eliminate the occupational hazard (yes, no) | 1 |
| Which of the following symptoms do you think that you have to check up | |
| Lump, pain (yes, no) | 1 |
| Inexplicable bleeding (yes, no) | 1 |
| Inexplicable abdominal discomfort (yes, no) | 1 |
| Change or dysfunction in defecation habit (yes, no) | 1 |
Investigation of risk factors and risk assessment
Information on demography (marital status, educational level, yearly income per household unit), source of drinking water, cigarette smoking, alcohol consumption, dietary habits, character and mental health, history of major digestive diseases, family history of cancer, and body mass index (BMI) were collected in the one-on-one questionnaire of EC-related risk factors. For those who were evaluated as high-risk individuals based on factors of cigarette smoking, alcohol drinking, dietary intake of pickled food, hot food and mildew food, unexplained esophageal symptoms and family history of major digestive system cancers (EC or stomach cancer or liver cancer), we recommended them to undergo further endoscopic examination.
Statistical analysis
In addition to the descriptive analysis regarding the characteristics of the study population, overall and group-specific PRs were calculated and reported. The general characteristics, behaviors of cigarette smoking and alcohol drinking were examined using one-way analysis of variance (ANOVA) tests for continuous variables, and Chi-square test for categorical variables. Cancer prevention knowledge scores were divided into four groups based on quartile of knowledge scores: Q1 (<40), Q2 (40−55), Q3 (56−70), and Q4 (>70). Crude odds ratios and 95% confidence interval (95% CI) were analyzed by univariate logistic regression, while adjusted odds ratio (aOR) and 95% CI were analyzed by multivariable logistic regression after adjustment for cancer prevention knowledge levels (categorized into <40, 40−55, 56−70, and >70), sex (male and female), age (categorized into 40−49, 50−59, and 60−69 years old), educational background (illiterate, primary school, junior high school and above), income status (<5,000 yuan yearly per household unit, and ≥5,000 yuan yearly per household unit), as well as status of cigarette smoking (yes, no), status of alcohol drinking (yes, no), dietary habits of pickled food (≥once per week, <once per week), hot food (≥once per week, <once per week), and mildew food (≥once per week, <once per week), unexplained esophageal symptoms (yes, no), family history of cancer (yes, no), and study regions.
Results
Baseline characteristics of participants
Demographic characteristics of participants in this survey were summarized in Table 1. Overall, a total of 28,543 participants [13,036 (45.67%) males and 15,507 (54.33%) females] were included with an average age of 54.40 years old. Mean baseline cancer prevention knowledge scores were 57.10±20.37, and males and females shared a similar score of 58.47 and 55.95, respectively. Among participants with high risk for EC, the prevalence rates of current smoking and alcohol drinking were 29.51% and 22.39% (58.25% and 44.22% for males and 5.35% and 4.05% for females), respectively. The rate of family history of cancer was around 23.80% (25.39% with males and 22.46% with females). Compared with females, higher educational background and economic status could be observed in males.
1.
Demographic and behavior characteristics among 28,543 participants, 2007−2016
| Variables | n (%) | P | ||
| Total (N=28,543) | Male (n=13,036) | Female (n=15,507) | ||
Age (
 ) (year) ) (year)
|
54.40±8.17 | 54.62±8.33 | 54.21±8.03 | <0.0001 |
Cancer prevention knowledge scores (
 ) )
|
57.10±20.37 | 58.47±20.37 | 55.95±20.30 | 0.6991 |
| Education level | ||||
| Illiterate | 7,621 (26.70) | 1,523 (11.68) | 6,098 (39.33) | <0.0001 |
| Primary school or junior high school | 20,425 (71.57) | 11,142 (85.48) | 9,283 (59.87) | |
| Senior high school and above | 492 (1.72) | 369 (2.83) | 123 (0.79) | |
| Missing (n) | 5 | 2 | 3 | |
| Yearly income per household unit (RMB) | ||||
| <5,000 | 13,139 (47.11) | 5,564 (43.80) | 7,575 (49.87) | <0.0001 |
| ≥5,000 | 14,752 (52.89) | 7,138 (56.20) | 7,614 (50.13) | |
| Missing (n) | 652 | 334 | 318 | |
| Cigarette smoking | ||||
| No | 20,120 (70.49) | 5,443 (41.75) | 14,677 (94.65) | <0.0001 |
| Yes | 8,423 (29.51) | 7,593 (58.25) | 830 (5.35) | |
| Alcohol drinking | ||||
| No | 22,151 (77.61) | 7,272 (55.78) | 14,879 (95.95) | <0.0001 |
| Yes | 6,392 (22.39) | 5,764 (44.22) | 628 (4.05) | |
| Family history of cancer | ||||
| No | 21,693 (76.20) | 9,697 (74.61) | 11,996 (77.54) | <0.0001 |
| Yes | 6,775 (23.80) | 3,300 (25.39) | 3,475 (22.46) | |
| Missing (n) | 75 | 39 | 36 | |
PRs in EC screening endoscopy
Characteristics of PRs in endoscopic screening were displayed in Table 2. Overall, a total of 28,543 participants were estimated as high-risk individuals for EC, and 15,810 of them undertook endoscopy as recommended, with overall PR of 55.39%. The PRs for all participants under quartiles of cancer prevention knowledge scores were 54.90%, 53.82%, 54.68% and 58.52%, respectively, with the highest PR for EC screening among participants in the highest quartile cancer prevention knowledge score. PRs were higher among females than males (58.95% and 51.15%, respectively), and were higher among those aged 60−69 (58.90%) than other age groups. In addition, participants with higher educational background and relatively lower incomes are more likely to participate in screening endoscopy according to univariate analysis.
2.
PRs by different groups among 28,543 high-risk population of EC, 2007−2016
| Variables | n (%) | PR (%) | P | |
| Participants with high-risk EC | Participants undertaking endoscopy | |||
| PR, participation rate; EC, esophageal cancer. | ||||
| Total | 28,543 | 15,810 | 55.39 | NA |
| Cancer prevention knowledge levels | ||||
| Q1 (<40) | 5,769 (20.21) | 3,167 (20.03) | 54.90 | <0.0001 |
| Q2 (40−55) | 8,660 (30.34) | 4,661 (29.48) | 53.82 | |
| Q3 (56−70) | 7,228 (25.32) | 3,952 (25.00) | 54.68 | |
| Q4 (>70) | 6,886 (24.13) | 4,030 (25.49) | 58.52 | |
| Sex | ||||
| Male | 13,036 (45.67) | 6,668 (42.18) | 51.15 | <0.0001 |
| Female | 15,507 (54.33) | 9,142 (57.82) | 58.95 | |
| Age (year) | ||||
| 40−49 | 9,224 (32.32) | 4,676 (29.58) | 50.69 | <0.0001 |
| 50−59 | 10,246 (35.90) | 5,790 (36.62) | 56.51 | |
| 60−69 | 9,073 (31.79) | 5,344 (33.80) | 58.90 | |
| Education level | ||||
| Illiterate | 7,621 (26.70) | 4,238 (26.81) | 55.61 | 0.0208 |
| Primary school or junior high school | 20,425 (71.57) | 11,266 (71.28) | 55.16 | |
| Senior high school and above | 492 (1.72) | 302 (1.91) | 61.38 | |
| Yearly income per household unit (RMB) | ||||
| <5,000 | 13,139 (47.11) | 7,670 (49.35) | 58.38 | <0.0001 |
| ≥5,000 | 14,752 (52.89) | 7,873 (50.65) | 53.37 | |
Cancer prevention knowledge in relation to EC screening rates
The association between cancer prevention knowledge scores and PRs for EC screening was displayed in Table 3. After adjusting potential confounding factors such as age, sex, socioeconomic status, EC-related behavioral and dietary factors, clinical symptoms, family history of cancer, as well as study regions, significantly increased PRs were found related to higher cancer prevention knowledge levels (aORQ4/Q1=1.511, 95% CI: 1.398−1.632, aORQ3/Q1=1.225, 95% CI: 1.138−1.319, and aORQ2/Q1=1.086, 95% CI: 1.012−1.165).
3.
Association between cancer prevention knowledge levels and PR for EC screening among 28,543 participants, 2007−2016
| Cancer prevention knowledge levels | Model 1 | Model 2 | Model 3 | ||||||
| OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | ||||
| PR, participation rate; EC, esophageal cancer; OR, odds ratio; 95% CI, 95% confidence interval; Model 1, Adjusted for cancer prevention knowledge levels; Model 2, Additionally, adjusted for sex, age, educational background and income status; Model 3, Additionally, adjusted for status of cigarette smoking, alcohol drinking, dietary habits of pickled food, hot food, and mildew food, unexplained esophageal symptoms, family history of cancer, and study regions. | |||||||||
| Q1 (<40) | Ref | Ref | Ref | ||||||
| Q2 (40−55) | 0.968 (0.905−1.036) | 0.3497 | 0.994 (0.929−1.065) | 0.8709 | 1.086 (1.012−1.165) | 0.0221 | |||
| Q3 (56−70) | 1.020 (0.951−1.095) | 0.5785 | 1.087 (1.012−1.168) | 0.0219 | 1.225 (1.138−1.319) | <0.0001 | |||
| Q4 (>70) | 1.201 (1.118−1.290) | <0.0001 | 1.271 (1.181−1.367) | <0.0001 | 1.511 (1.398−1.632) | <0.0001 | |||
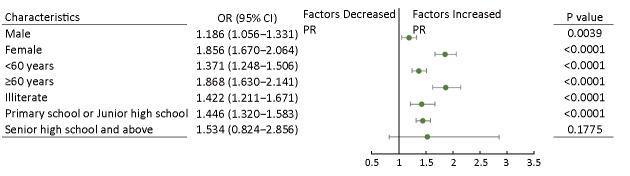
After stratified by major demographic factors, association between cancer prevention knowledge and PR of EC screening also tends to be strong in both males (aORQ4/Q1=1.186, 95% CI: 1.056−1.331) and females (aORQ4/Q1=1.856, 95% CI: 1.670−2.064), in illiterate individuals (aORQ4/Q1=1.422, 95% CI: 1.211−1.671) and those with primary or junior high school diploma (aORQ4/Q1=1.446, 95% CI: 1.320−1.583). In addition, multivariable analysis showed higher cancer prevention knowledge among participants aged below 60 years and those aged 60 years and above was also positively related to higher PR for EC screening, with aORsQ4/Q1of 1.371 (95% CI: 1.248−1.506) and 1.868 (95% CI: 1.630−2.141), respectively (Figure 1).
1.
Association between quartiles of cancer prevention knowledge scores (Quartile 4 vs. Quartile 1) and participation rates (PRs) stratified by different factors. OR, odds ratio; 95% CI, 95% confidence interval.
Discussion
Epidemiological evidence about the link between cancer prevention knowledge and cancer screening rates is important but scarce for EC prevention and control. Here, we presented the report on the association of cancer prevention knowledge with EC screening PRs targeted rural population in Chinese mainland. The analysis showed that a higher cancer prevention knowledge, reflecting a higher awareness towards cancer prevention, was significantly related to an increased PR for EC screening, and the association was also robust after adjusting multiple important confounding factors (age, sex, socioeconomic status, behavioral and dietary factors, clinical symptoms, family history of cancer, as well as study regions). In addition, we observed that the positive association between cancer prevention knowledge and compliance with EC screening occurred in most subgroups such as males, females, those aged below 60 years and those aged 60 years and above, illiterate individuals and participants with primary or junior high school diploma. These findings supported the hypothesis that cancer prevention awareness could be an independent influence factor for compliance with EC screening.
Previous studies showed that early diagnosis and treatment by endoscopy screening could effectively reduce ESCC incidence and EC-related mortality (10). High PRs in cancer screening are essential for a successful EC screening program (11). The acceptance of endoscopy screening increased gradually in an organized EC screening program in China (19). The overall compliance with screening in our study was 55.39%, which was still lower than the recommended rate of 70% (12). Our findings that females, the aged participants, and participants with high education level had a higher compliance with cancer screening were consistent with the results of previous studies (15,20-24). Economic index showed a conflicting influence on compliance with cancer screening among previous existing studies (16,20,21,25,26). In our study, we observed that participants with lower income were more likely to uptake endoscopy screening, which was consistent with the results targeting rural population (20,25), but was inconsistent with results from many previous studies that explored determinants of screening PRs on cancers of stomach, liver, colorectal, breast, and cervix, where higher incomes were associated with higher PRs (21,26). One possible explanation is that the involved people with lower income had greater disadvantages in health service utilization in rural China (27), therefore they would prefer to participate in screening without financial cost.
Several studies have examined the association between high cancer prevention knowledge and practice of cancer screening for other cancers (13-16). A cross-sectional study for 548 African-American males in Jordan reported that knowledge of prostate cancer seemed to be a significant predictor of adherence in cancer screening (aOR=2.3, 95% CI: 1.2−4.2) (13). An Indian study about knowledge and practice in cervical cancer screening found that female participation behaviors were closely associated with knowledge of cervical cancer screening (OR=2.753, 95% CI: 1.034−7.331), and the knowledge of Pap test (OR=7.098, 95% CI: 2.999−16.796) (15). Additionally, a systematic review based on 3 cohort studies, 27 cross-sectional, and 3 case-control studies targeting indigenous populations living in the USA, Canada, Austria, Nigeria, New Zealand and Norway showed that knowledge about cancer and screening was the second most common factors in relation to affecting behaviors of cancer screening (16). Generally, poor awareness of cancer-related risk factors and early symptoms was considered as predominant barriers for establishment of healthy lifestyle and was also regarded as primary reasons for the delay of detection cancer patients at early stage, ultimately resulting in a poor cancer prognosis (17,28,29). This situation could be well explained by the theory of health belief model that perceived seriousness and susceptibility of a certain disease could influence perceived threat and can positively affect individuals’ medical behaviors (30,31). Our finding that higher cancer prevention knowledge was related to higher PR of endoscopy examination (aORQ4/Q1=1.169, 95% CI: 1.089−1.255) was consistent with the existing results mentioned above, and provided a new evidence on cancer prevention awareness in relation to behaviors of EC screening.
In our stratified analysis, there was no significant association among participants with higher educational level (senior high school and above), which might be explained by limited statistical power and competing risk factors among this sub-population. However, we found a positive association pronounced in most subgroups of males, females, those aged below 60 years and those aged 60 years and above, and those with lower level of education (illiterate individuals and those with junior high education or less), after adjusting major confusing factors. These findings revealed that cancer prevention awareness could be an independent influence factor for compliance with EC screening.
Some strengths in our research were as followed. The thirteen communities were chosen after carefully assessing incidence and mortality rates of EC, work foundations of population-based cancer registry, work skill of epidemiological investigation and hospital levels. Besides, a detailed protocol and management pattern have been established in the population-based EC screening program. Questionnaires of core knowledge on cancer prevention and risk factors related to EC were collected in the standardized manner by trained staffs to ensure the quality of data. In addition, capacity training and review of endoscopy and pathology reports by expert panel were also conducted yearly to enhance the consistency and accuracy of clinical diagnoses. Limitations in this study mainly included that participants in our study could not represent for the whole general Chinese rural population. Although the thirteen communities in 4 provinces were chosen carefully by expert panel, selection bias cannot be ruled out.
Conclusions
Our results indicated a positive relationship between cancer prevention knowledge and PR for EC screening, with similarities within most subgroups which implied that cancer prevention awareness could be an independent influence factor for compliance with EC screening. These findings suggested that public campaigns about comprehensive knowledge of cancer prevention, especially in terms of cancer screening should be given priority to improve public compliance with cancer screening.
Acknowledgements
This study was supported by the National Key R&D Program of China (No. 2018YFC1313100) and the Special Fund for Health Research in the Public Interest (No. 2016-12M-2-004). We gratefully acknowledge all staff in our study who have made a great contribution to the data collection, auditing, database management and verification. We thank all individuals who have contributed to this study.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Ferlay J, Colombet M, Soerjomataram I, et al Global and Regional Estimates of the Incidence and Mortality for 38 Cancers: GLOBOCAN 2018. Lyon: International Agency for Research on Cancer/World Health Organization; 2018 [Google Scholar]
- 2.Zheng RS, Sun KX, Zhang SW, et al Report of cancer epidemiology in China, 2015. Zhonghua Zhong Liu Za Zhi. 2019;41:19–28. doi: 10.3760/cma.j.issn.0253-3766.2019.01.005. [DOI] [PubMed] [Google Scholar]
- 3.Zeng H, Chen W, Zheng R, et al Changing cancer survival in China during 2003-15: a pooled analysis of 17 population-based cancer registries. Lancet Glob Health. 2018;6:e555–e67. doi: 10.1016/S2214-109X(18)30127-X. [DOI] [PubMed] [Google Scholar]
- 4.Adami HO, Day NE, Trichopoulos D, et al Primary and secondary prevention in the reduction of cancer morbidity and mortality. Eur J Cancer. 2001;37:S118–27. doi: 10.1016/s0959-8049(01)00262-3. [DOI] [PubMed] [Google Scholar]
- 5.Chen W, Xia C, Zheng R, et al Disparities by province, age, and sex in site-specific cancer burden attributable to 23 potentially modifiable risk factors in China: a comparative risk assessment. Lancet Glob Health. 2019;7:e257–e69. doi: 10.1016/S2214-109X(18)30488-1. [DOI] [PubMed] [Google Scholar]
- 6.Liu S, Zhang M, Yang L, et al Prevalence and patterns of tobacco smoking among Chinese adult men and women: findings of the 2010 national smoking survey. J Epidemiol Community Health. 2017;71:154–61. doi: 10.1136/jech-2016-207805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Center for Chronic and Non-communicable Disease. Chinese Center of Disease Control and Prevention. Report On Chronic Disease Risk Factor Surveillance In China (2010). Beijing: Military Medical Science Press, 2012.
- 8.Zou XN Epidemic trend, screening, and early detection and treatment of cancer in Chinese population. Cancer Biol Med. 2017;14:50–9. doi: 10.20892/j.issn.2095-3941.2016.0047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang GQ, Hao CQ, Wei WQ Long-term survival rate of precancerous lesions and early esophageal cancers after endoscopic mucosal resection. Zhonghua Xiao Hua Nei Jing Za Zhi. 2008;25:584–6. [Google Scholar]
- 10.Wei WQ, Chen ZF, He YT, et al Long-term follow-up of a community assignment, one-time endoscopic screening study of esophageal cancer in China. J Clin Oncol. 2015;33:1951–7. doi: 10.1200/JCO.2014.58.0423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dong ZW, Qiao YL, Kong LZ, et al The strategy and implementation for early detection of cancer in China. Zhongguo Zhong Liu. 2008;17:256–63. doi: 10.3969/j.issn.1004-0242.2008.04.001>. [DOI] [Google Scholar]
- 12.Dong ZW. Guidelines for cancer screening and early diagnosis and treatment in China. Beijing: Peking University Medical Press, 2005.
- 13.Myers RE, Hyslop T, Wolf TA, et al African-American men and intention to adhere to recommended follow-up for an abnormal prostate cancer early detection examination result. Urology. 2000;55:716–20. doi: 10.1016/S0090-4295(99)00588-9. [DOI] [PubMed] [Google Scholar]
- 14.Lyimo FS, Beran TN Demographic, knowledge, attitudinal, and accessibility factors associated with uptake of cervical cancer screening among women in a rural district of Tanzania: three public policy implications. BMC Public Health. 2012;12:22. doi: 10.1186/1471-2458-12-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aswathy S, Quereshi MA, Kurian B, et al Cervical cancer screening: Current knowledge & practice among women in a rural population of Kerala, India. Indian J Med Res. 2012;136:205–10. [PMC free article] [PubMed] [Google Scholar]
- 16.Kolahdooz F, Jang SL, Corriveau A, et al Knowledge, attitudes, and behaviours towards cancer screening in indigenous populations: a systematic review. Lancet Oncol. 2014;15:e504–16. doi: 10.1016/S1470-2045(14)70508-X. [DOI] [PubMed] [Google Scholar]
- 17.Niksic M, Rachet B, Duffy SW, et al Is cancer survival associated with cancer symptom awareness and barriers to seeking medical help in England? An ecological study. Br J Cancer. 2016;115:876–86. doi: 10.1038/bjc.2016.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li H, Zeng HM, Zou XN, et al Awareness of cancer prevention knowledge among rural residents in the middle of China. Zhongguo Zhong Liu. 2018;27:561–7. doi: 10.11735/j.issn.1004-0242.2018.08.A001>. [DOI] [Google Scholar]
- 19.Wang GQ, Wei WQ, Qiao YL The practice and experience of screening and early detection for esophageal cancer. Zhongguo Zhong Liu. 2010;19:4–8. doi: 10.3760/j.issn:0253-3766.2004.06.006>. [DOI] [Google Scholar]
- 20.Sankaranarayanan R, Rajkumar R, Arrossi S, et al Determinants of participation of women in a cervical cancer visual screening trial in rural south India. Cancer Detect Prev. 2003;27:457–65. doi: 10.1016/j.cdp.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 21.Choi B, Um TR, Lee KS Factors related to cancer screening behaviors. Epidemiol Health. 2018;40:e2018011. doi: 10.4178/epih.e2018011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim RB, Park KS, Hong DY, et al Factors associated with cancer screening intention in eligible persons for national cancer screening program. J Prev Med Public Health (in Korean) 2010;43:62–72. doi: 10.3961/jpmph.2010.43.1.62. [DOI] [PubMed] [Google Scholar]
- 23.Byrne MM, Davila EP, Zhao W, et al Cancer screening behaviors among smokers and non-smokers. Cancer Epidemiol. 2010;34:611–7. doi: 10.1016/j.canep.2010.06.017. [DOI] [PubMed] [Google Scholar]
- 24.Ko YJ, Kim S, Kim KH, et al Cancer screening adherence of Asian women according to biochemically-verified smoking status: Korea National Health and Nutrition Examination Survey. Asian Pac J Cancer Prev. 2015;16:4081–8. doi: 10.7314/apjcp.2015.16.9.4081. [DOI] [PubMed] [Google Scholar]
- 25.Crosby RA, Stradtman L, Collins T, et al Community-based colorectal cancer screening in a rural population: Who returns fecal immunochemical test (FIT) kits? J Rural Health. 2017;33:371–4. doi: 10.1111/jrh.12210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kwak MS, Park EC, Bang JY, et al Factors associated with cancer screening participation, Korea. J Prev Med Public Health. 2005;38:473–81. [PubMed] [Google Scholar]
- 27.Qian Y, Zhou Z, Yan J, et al An economy-ralated equity analysis of health service utilization by women in economically underdeveloped regions of western China. Int J Equity Health. 2017;16:186. doi: 10.1186/s12939-017-0667-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alshammari FD, Ahmed HG, Alshammari D, et al Population insight of the relationship between lifestyle and cancer: A population-based survey. AIMS Public Health. 2019;6:34–48. doi: 10.3934/publichealth. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hammond D, McDonald PW, Fong GT, et al Do smokers know how to quit? Knowledge and perceived effectiveness of cessation assistance as predictors of cessation behaviour. Addiction. 2004;99:1042–8. doi: 10.1111/j.1360-0443.2004.00754.x. [DOI] [PubMed] [Google Scholar]
- 30.Rosenstock IM, Strecher VJ, Becker MH Social learning theory and the Health Belief Model. Health Educ Q. 1988;15:175–83. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- 31.Prochaska JO, DiClemente CC, Norcross JC In search of how people change. Applications to addictive behaviors. Am Psychol. 1992;47:1102–14. doi: 10.3109/10884609309149692. [DOI] [PubMed] [Google Scholar]