Abstract
Preeclampsia is a common pregnancy complication which can have adverse impact on both mother and baby. In addition to the short term effects, a large body of epidemiological evidence has found preeclampsia can exert long-lasting effects on mother and offspring. Studies suggest that offspring exposed to preeclampsia are at a higher risk of developing cardiovascular, metabolic, and neurological diseases, as well as other diseases. However, studies investigating the underlying mechanism are limited, the exact mechanism still remains unclear. In this study, we will review the epidemiological evidence and studies exploring the mechanism underlying long-term effects of preeclampsia on offspring. Further studies should be targeted at this field so as to implement effective clinical management to prevent the exposed offspring from potential diseases.
Keywords: Preeclampsia Offspring, cardiovascular system, neurological disorders, metabolism, DOHaD
Preeclampsia is a pregnancy-specific disorder, characterized by the new onset of hypertension after 20thgestational week, accompanied by one or more of the following conditions, such as proteinuria, thrombocytopenia, renal insufficiency, impaired liver function, pulmonary edema, and cerebral or visual symptoms. 1 It affects 3 to 8% of pregnancy worldwide, which is a major cause of maternal and perinatal morbidity and mortality. The exact etiology of preeclampsia remains unknown. Various pathological mechanisms are involved in the development of preeclampsia including placental ischemia, hypoxia, imbalance between angiogenic and antiangiogenic factors, excessive inflammation, and production of autoantibodies. 2 3 Preeclampsia is a multisystem disorder which can cause damage to various maternal organs and systems. Moreover, it is a major contributor to premature birth, intrauterine growth restriction, and small for gestational age. 4 Currently, the most effective cure for this disease is the delivery of placenta and fetus, 5 whereas the effect of preeclampsia doesn't cease. A line of evidence suggests that preeclampsia not only cause long-term adverse effects to the mother, including increased risks of developing hypertension and other cardiovascular and metabolic diseases, in later life but also affect the fetus's health immediately after delivery into adulthood, such as cardiovascular, metabolic, and neurological system. The mechanism through which preeclampsia exerts effects on offspring is not definitive. One widely accepted theory is Developmental Origins of Health and Disease (DOHaD) which was first proposed by David Barker. 6 A favorable intrauterine environment is essential for the development and growth of fetus. The theory proposed that if the optimal environment is altered by pathological condition during a critical period of fetal development, the fetuses will adapt themselves to the unfavorable condition through developmental programming which can increase the risk of chronic diseases in later life. They found that cardiovascular diseases and type 2 diabetes derived from “developmental plasticity,” as a result of under nutrition during fetal life. 7 This review will focus on the epidemiological evidence of lasting effects of preeclampsia on offspring and current advances on the underlying mechanism.
Cardiovascular Outcomes in Offspring Exposed to Preeclampsia Epidemiological Evidence
We have found 15 relevant articles evaluating the cardiovascular effects of maternal preeclampsia on offspring ( Table 1 ). Nine studies reported blood pressure data of offspring born after preeclampsia and normotensive pregnancy 8 9 10 11 12 13 14 15 16 which had mixed results. Seven studies reported both increased systolic blood pressure (SBP) and diastolic blood pressure (DBP) in offspring exposed to maternal preeclampsia compared with normotensive pregnancy. 8 9 10 11 13 14 15 Participants, who included in these studies, were in their childhood, adolescence, or young adulthood. The increase in SBP are ranged from 0.14 to 2.3 mm Hg, while the range is from 0.03 to 1.71 mm Hg in DBP. Whereas, one study found no significant differences in SBP and DBP between offspring of preeclampsia and normotensive pregnancy, aged 16 years. 12 Alsnes et al found the increase in blood pressure of offspring aged 29 years, who were exposed to preeclampsia, was only existed when they were born from term pregnancy. 8 Staley et al have followed up offspring from 7 to 18 years, both SBP and DBP were elevated in preeclampsia offspring, with the mean differences 1.22 and 0.80 mm Hg, respectively. 10 The difference was consistent across childhood to age 18 years. This finding was similar with other two studies reported by Fraser et al and Lawlor et al. 11 13 Offspring exposed to preeclampsia aged 10.7 years had 1.82 mm Hg higher SBP and 1.40 mm Hg higher DBP than those born after normal pregnancy after adjusting for maternal body mass index (BMI) and offspring age, sex, and BMI. Participants exposed to maternal preeclampsia aged 17 years had both higher SBP and DBP, 1.12 and 1.71 mm Hg, respectively, adjusting for maternal prepregnancy BMI and offspring age and sex. Geelhoed et al reported that offspring of preeclampsia aged 9 years from Avon longitudinal study had 2.05 mm Hg higher SBP and 1.00 mm Hg higher DBP independent of parental and own adiposity; 14 nonetheless, the difference attenuated to null after controlling for birth weight and gestational age, indicating that the increase in blood pressure of offspring was exposed to preeclampsia may be at least partly mediated by the effect of preeclampsia on intrauterine growth restriction. Furthermore, there was a study reporting increased pulmonary artery pressure of offspring exposed to preeclampsia compared with normal pregnancy who were living at the same high altitude 16 ( p < 0.001).
Table 1. Summary of studies on cardiovascular effects on offspring.
| Authors, years of publication | Study design | Study groups ( n ) | Offspring birth year/age when measured | Summary of results | Confounders adjusted for | Definition of preeclampsia |
|---|---|---|---|---|---|---|
| Nahum et al, 22 2018 | Cohort follow-up | Severe preeclampsia (2,174) Mild preeclampsia (7,286) Control (221,765) |
1991–2014 | Hypertension (%): incidence rates Severe preeclampsia: 0.14; mild preeclampsia: 0.11; control: 0.06. p < 0.001 |
Sex of the offspring, IUGR, maternal diabetes, obesity of the offspring. | |
| Boyd et al, 17 2017 | Cohort study |
Early preterm preeclampsia
a
(3,617)
Late preterm preeclampsia (5,512) Term preeclampsia (45,611) Normotensive pregnancy (1,900,142) |
1978–2010 | Congenital heart defect: OR (95% CI) Early preterm preeclampsia = 7.00, 95% CI: 6.11–8.03 Late preterm preeclampsia = 2.82, 95% CI: 2.38–3.34 Term preeclampsia = 1.16, 95% CI: 1.06–1.27. |
Maternal age, parity and delivery year. | |
| Alsnes et al, 8 2017 | Prospective cohort studies | Preterm preeclampsia (27) Term preeclampsia (343) Normotensive pregnancy (15,072) |
Mean 29 years | SBP (mm Hg): mean (95% CI) Term preeclampsia: 2.3 mm Hg (95% CI: 1.1–3.5 mm Hg) higher than normotensive pregnancy. Preterm preeclampsia: no strong evidence of differences between preterm preeclampsia and normotensive pregnancy. DBP (mm Hg): mean (95% CI) term preeclampsia: 1.0 mm Hg (95% CI: 0.1–1.9 mm Hg) higher than normotensive pregnancy. Preterm preeclampsia: no strong evidence of differences between preterm preeclampsia and normotensive pregnancy. BMI (kg/m 2 ): mean (95% CI) Term preeclampsia: 0.93 kg/m 2 (95%CI: 0.41–1.44 kg/m 2 ) higher than normotensive pregnancy. Preterm preeclampsia: no strong evidence of differences between preterm preeclampsia and normotensive pregnancy. |
Offspring age and sex, maternal parity, cardiovascular risk factors including maternal smoking, education BMI, SBP, and DBP. | Sustained increase in blood pressure, ≥ 140 mm Hg systolic and 90 mm Hg diastolic pressure, with onset after 20 weeks of gestation, with proteinuria after gestational week 20. |
| Timpka et al, 18 2016 | Prospective cohort study | Preeclampsia (42) Normotensive pregnancy |
Mean 17.7 years | Relative wall thickness: preeclampsia: 0.025 (95% CI: 0.008–0.043) greater than normotensive pregnancy. | Maternal age, offspring age, and sex, prepregnancy BMI, parity, and glycosuria/diabetes | New hypertension that manifests in previously normotensive women following the 20th week of pregnancy |
| Miliku et al, 9 2016 | Prospective cohort study | Preeclampsia (93) Normotensive pregnancy (4,888) |
Median 6.0 years | SBP (mm Hg): preeclampsia = 0.14 (95% CI: −0.01 to 0.28) higher than normotensive pregnancy. DBP (mm Hg): preeclampsia = 0.03 (95% CI: −0.09 to 0.15) higher than normotensive pregnancy. |
Maternal age, prepregnancy BMI, ethnicity, parity, educational level, smoking during pregnancy, alcohol consumption, and folic acid supplement intake, and childhood current BMI. | Development of SBP ≥ 140 mm Hg and/or DBP ≥ 90 mm Hg after 20 weeks of gestation in previously normotensive women with the presence of proteinuria. |
| Auger et al, 19 2015 | Population based study | Preeclampsia (72,782) Early-onset preeclampsia (5,488) Late-onset preeclampsia (67,215) No preeclampsia (1,869,290) |
Congenital heart defects: overall prevalence; Preeclampsia: 1 6.7/1,000. No preeclampsia: 8.6/1,000. Critical heart defects: prevalence. Preeclampsia: 123.7/100,000, early-onset preeclampsia: 364.4/100,000, late-onset preeclampsia: 104/100,000, no preeclampsia: 75.6/100,000, noncritical heart defects: prevalence, preeclampsia: 1,538.8/100,000, early-onset preeclampsia: 7,306.9/100,000, late-onset preeclampsia: 1069.7/100,000, no preeclampsia: 789.2/100,000. |
Maternal age, parity, multiple birth, socioeconomic deprivation, and period. | Hypertension and proteinuria developing after 20 weeks of gestation in women who were previously normotensive. | |
| Brodwall et al, 20 2016 | Cohort study | Early-onset preeclampsia (2,618) Late-onset preeclampsia (30,246) Normotensive pregnancy (868,090) |
1994–2009 | Severe congenital heart defects: RR. Preeclampsia: RR = 1.3 (95% CI: 1.1–1.5), early-onset preeclampsia: RR = 2.8 (95%CI: 1.8 to 4.4) compared with normotensive pregnancy. |
Birth year, maternal age, parity, and pregestational diabetes. | SBP ≥ 140 mm Hg, DBP ≥ 90 mm Hg and proteinuria. |
| Staley et al, 10 2015 | Cohort study | Preeclampsia (161) No evidence of hypertension (6,716) |
7, 9, 10, 11, 13, 15, 17 y | SBP (mm Hg): mean difference (95% CI). Preeclampsia: 1.22 mm Hg (95% CI: −0.52 to 2.97) higher compared with no evidence of hypertension in 7 y. DBP (mm Hg): mean difference (95% CI) Preeclampsia: 0.80 mm Hg (95% CI: −0.53 to 2.13) higher compared with no evidence of hypertension in 7 y. These differences were consistent across childhood to age 18 y. |
Maternal characteristics: prepregnancy BMI, maternal age, parity, smoking during pregnancy, education, social class and offspring sex, BMI, and height. | proteinuria of at least 1 + on dipstick testing occurring at the same time as the elevated BP. |
| Fraser et al, 11 2013 | Prospective cohort study | Preeclampsia (53) Normotensive pregnancy (2,404) |
Mean 17 y | SPB (mm Hg): mean difference (95% CI).Preeclampsia: 1.12 mm Hg (95% CI: −0.89 to 3.12) higher than normotensive pregnancy. DPB (mm Hg): mean difference (95% CI). Preeclampsia: 1.71 mm Hg (95% CI: 0.23–3.17) higher than normotensive pregnancy. BMI (kg/m 2 ): preeclampsia = 4 Normotensive pregnancy: 22.3, p < 0.05 |
Offspring age, sex, maternal age at delivery, household social class, prepregnancy BMI, parity, and smoking in pregnancy. | SBP ≥ 140 mm Hg or DBP ≥90 mm Hg, measured on at least two occasions after 20 weeks of gestation, with proteinuria, diagnosed if the protein reading on dipstick testing was at least 1 + (30 mg/dL), occurring at the same time as the elevated blood pressure. |
| Miettola et al, 12 2013 | Prospective cohort study | Preeclampsia (197) Normotensive pregnancy (5,045) |
16 y | No significant differences in SBP, DBP, and MAP between offspring of preeclampsia and normotensive pregnancy. | Offspring sex, offspring BMI at age 16 y, birth weight, nulliparity, maternal prepregnancy BMI, and socioeconomic position. | BP ≥ 140/90 mm Hg and proteinuria. |
| Lawlor et al, 13 2012 | Cohort study | Preeclampsia (102) Normotensive pregnancy (3,781) |
10.7 y | SPB (mm Hg): mean difference (95% CI). Preeclampsia: 1.82 mm Hg (95% CI: 0.03–3.62) higher than normotensive pregnancy. DPB (mm Hg): mean difference (95% CI). Preeclampsia: 1.40 mm Hg (95%CI: −0.17 to 2.98) higher than normotensive pregnancy. No statistically significant differences in vascular function including FMD absolute, PWV , and DC. |
Offspring sex and age at the time of outcome measurement, offspring BMI, birth weight, gestational age, and mode of delivery. Maternal age, nulliparity, smoking during pregnancy, prepregnancy BMI, education, and head of household social class. | SBP > 139 mm Hg or a DBP > 89 mm Hg, measured on at least two occasions after 20 weeks of gestation, with proteinuria, diagnosed if the protein reading on dipstick testing was at least 1 + (30 mg/dL), occurring at the same time as the elevated BP. |
| Geelhoed et al, 14 2010 | Cohort study | Preeclampsia (196) Normotensive pregnancy (5,082) |
9 y | SPB (mm Hg): mean difference (95% CI). Preeclampsia: 2.05 mm Hg (95%CI:0.72–3.38) higher than normotensive pregnancy. DPB (mm Hg): mean difference (95% CI). Preeclampsia: 1.00 mm Hg (95%CI: −0.01 to 2.01) higher than normotensive pregnancy. The association of preeclampsia with offspring SBP and DBP attenuated to null after adjusting for birth weight and gestational age. |
Offspring sex and age at the 9-y-old visit, maternal age at delivery, parental prepregnancy BMI, parity, social class, maternal smoking during pregnancy, and offspring weight, height at 9 y-old. | SBP > 139 mm Hg or a DBP > 89 mm Hg, measured on at least two occasions after 20 weeks of gestation, with proteinuria, diagnosed if the protein reading on dipstick testing was at least 1 + (30 mg/dL), occurring at the same time as the elevated BP. |
| Jayet et al, 16 2010 | Cohort study | Preeclampsia (48) Normal pregnancy (90) living at the same high altitude location |
Preeclampsia 13 + 7 y Normal pregnancy 14 + 7 y |
Pulmonary artery pressure (mm Hg): mean + SD Preeclampsia: 32.1 ± 5.6 mm Hg. Normal pregnancy: 25.3 ± 4.7 mm Hg. p < 0.001. Flow-mediated dilation of the brachial artery: mean + SD preeclampsia: 6.3 + 1.2%. Normal pregnancy: 8.3 + 1.4%; p < 0.0001. |
New-onset, persistent elevation of SBP and/or DBP > 140/90 mm Hg or a rise in blood pressure of 30/15 mm Hg from the baseline level that occurred after 20 weeks of gestation; proteinuria on consecutive dipstick measurements; and normalization of blood pressure and disappearance of proteinuria after delivery. | |
| Øglaend et al, 15 2009 | Case control study | Preeclampsia (181) Normotensive pregnancy (356) |
11–12 y | SBP (mm Hg): mean. Preeclampsia: 115.3 mm Hg. Normotensive pregnancy: 113.5 mm Hg, p = 0.03. DPB (mm Hg): mean. Preeclampsia: 66.4 mm Hg. Normotensive pregnancy: 65.3 mm Hg, p = 0.1. After adjustment, the difference in SBP was largely attenuated. |
Maternal BMI and blood pressure, offspring BMI. | At 20-week of gestation, DBP had to be increased by at least 25 mm Hg to a persistent pressure of at least 90 mm Hg, and proteinuria with dipstick + 1 or more should be present in at least one urine sample. |
| Kajantie et al, 21 2009 | Cohort study | Preeclampsia (384) Normotensive pregnancy (4,271) |
1934–1944 |
The crude hazard ratio for all forms of stroke: preeclampsia = 1.9 (1.2–3.0),
p
= 0.01.
Normotensive pregnancies as the comparison group. There was no evidence that preeclampsia was associated with coronary heart diseases in offspring. |
proteinuria + and a SBP of ≥ 140 mm Hg or DBP of ≥ 90 mm Hg. |
Abbreviations: BMI, body mass index; BP, blood pressure; CI, confidence interval; DBP, diastolic blood pressure; DC, distensibility coefficient; FMW, flow mediated dilation; IUGR, intrauterine growth restriction; MAP, mean arterial pressure; OR, odds ratio; PWV, pulse wave velocity; RR, risk ratio; SBP, systolic blood pressure; SD, standard deviation.
Early preterm preeclampsia: preeclampsia necessitating delivery at < 34 weeks; late preterm preeclampsia: preeclampsia necessitating delivery at 34 to 36 weeks; term preeclampsia: preeclampsia with the baby delivered at ≥37 weeks.
Two studies have compared BMI. One study found that offspring aged 29 years of preeclampsia born from term pregnancy had 0.93 kg/m 2 higher BMI than those born term of normal pregnancy. 8 Another study reported 2.1 kg/m 2 higher BMI in preeclampsia offspring aged 17 years ( p < 0.05). 11
Five studies investigated the cardiac structure and function in offspring. 17 18 19 20 21 Timpka et al reported that offspring aged 17.7 years born after preeclampsia had 0.025 greater cardiac relative wall thickness and 0.9 mL smaller left ventricular end-diastolic volume than normotensive pregnancy, 18 which is a concentric type of remodeling, associated with higher risk of coronary heart disease and stroke in adulthood. Nonetheless, Kajantie et al found no evidence that preeclampsia was associated with coronary heart disease in the offspring. 21 The authors believed that a small increase in the risk of coronary heart diseases couldn't be excluded because of the limitation of sample size. Large scale of studies is needed to confirm the relationship between preeclampsia and the risk of coronary heart diseases in the offspring. Boyd et al reported increased risk of congenital heart defect in offspring of preeclampsia compared with normotensive pregnancy. Offspring congenital heart defects were strongly associated with early preterm, late preterm, and term preeclampsia, odds ratio (OR) were 7.0 (95% confidence interval [CI]: 6.11–8.03), 2.82 (95% CI: 2.38–3.34), 1.16 (95% CI: 1.06–1.27), respectively. 17
Auger et al also described a positive association between preeclampsia and congenital heart defects in infants; a total of 1,942,072 neonates were included. 19 They found that the prevalence of congenital heart defects was higher in neonates of preeclamptic women compared with those without preeclampsia, 16.7/1,000 and 8.6/1,000, respectively, especially the early-onset preeclampsia which had significantly higher prevalence of both critical and noncritical congenital heart defects(364.4/100,000 vs. 75.6/100,000 and 7306.9/100,000 vs. 789.2/100,000). Brodwall et al reported that preeclampsia, especially early-onset preeclampsia, was associated with the increased risk of severe congenital heart defects (relative risk preeclampsia, 1.3 [95% CI: 1.1–1.5]; early-onset preeclampsia, 2.8 [95%CI: 1.8–4.4]). 20
Two studies evaluated offspring vascular function. The endothelial function was assessed by brachial artery flow-mediated dilatation (FMD). Arterial stiffness was assessed by carotid to radial pulse wave velocity (PWV) and brachial artery distensibility coefficient (DC). The results were inconsistent. Lawlor et al found no statistically significant differences in vascular function including flow-mediated dilatation absolute, pulse wave velocity, and distensibility coefficient of offspring aged 10.7 years between preeclampsia and normotensive pregnancy. 13 Whereas, Jayet et al reported that offspring in adolescence, who were living at high altitude, born after preeclampsia had lower FMD of the brachial artery than normal pregnancy (preeclampsia: 6.3 ± 1.2%; normal pregnancy: 8.3 ± 1.4%. p < 0.0001). 16 The former study involved large scale of population ( n = 102 with preeclampsia and 3,781 controls with normotensive pregnancy) and was based on general population not living at high altitude. The latter one was smaller and based on selected population who lived at high altitude. The different results might be attributed to the limitation of the sample size. It's also possible that the stress on the vascular system at high altitude allowed associations to emerge, besides, the alteration in vascular function of offspring of preeclampsia might emerge until adolescence.
Kajantie et al found that offspring exposed to preeclampsia born in 1934 to 1944 from Helsinki cohort study were at 1.9 times increased risk of stroke in adult life compared with normal pregnancy after adjusting for birth weight and gestational age. 21
Nahum et al reported that offspring of preeclampsia were at higher risk of developing hypertension compared with normotensive pregnancy (incidence rate of hypertension: severe preeclampsia: 0.14; mild preeclampsia: 0.11; control: 0.06; p < 0.001). 22
The Underlying Mechanism
The mechanism underlying adverse cardiovascular outcome in offspring may be a complex interplay of genetic, shared environmental factors, and fetal programming. It has already been known that genetic factors play a crucial part in the development of preeclampsia which exhibit the familial clusters with the heritability estimated to be 47%. 23 Thus genetic factors may be inherited by the offspring predisposing them to preeclampsia and cardiovascular disease in later life. In addition, environmental factors, shared by the mother and offspring, may also lead to the adverse effects on offspring. 24 However, Jayet et al found that offspring exposed to preeclampsia had approximately 30% higher pulmonary artery pressure and impaired vascular function while their siblings born after the normal pregnancy had normal vascular function which cannot be explained only by genetic components and shared environmental factors. 16 The findings above revealed that the pathological event in the uterus can lead to impaired vascular function and pulmonary dysfunction. The underlying mechanism through which chronic diseases are initiated might be alteration of gene expression, 25 changes in the kidney growth 26 and alterations in homeostatic set points including the hypothalamic-pituitary-adrenal axis, 27 vascular structure and sensitivity, 28 rennin–angiotensin system (RAS) 29 and metabolic and hormonal set-points 30 which can make the affected system more vulnerable to adverse influences in postnatal life.
Vascular and endothelia dysfunction are known to play a critical role in the development and progression of hypertension. 31 Jayet et al showed an impaired vascular function of offspring compared with those of normal pregnancy. 16 Rodent studies also found that vascular function was altered in the offspring of mice with soluble fms-like tyrosine kinase-1 (sFlt-1) induced preeclampsia-like phenotype. 28 Antiangiogenic state has been found in adulthood of offspring born after preeclampsia with elevated level of plasma sFlt-1 and soluble Endoglin (Eng), related to the increase in blood pressure. 32 The antiangiogenic state also be observed in heart defects. 33 This shared pathway may account for the increased risk of congenital heart defects in neonate born after preeclampsia. A study shows that the pathology of preeclampsia begins as early as the start of the pregnancy, near the time of the morphogenesis of fetal heart. 34
The kidney can be programmed by various perinatal insults, such as placental insufficiency. Decreased nephron numbers and subsequent impaired blood pressure regulation in offspring has always been found in rodent model with placental insufficiency. 26 35 Decreased nephron numbers can influence blood pressure through impairing the ability of kidney to maintain sodium homeostasis due to the imbalance in excretory load and capacity. Singh et al found that decreased excretory capacity could arise from altered expression of renal sodium transporters and channels. 36 In addition, the programming of RAS and sympathetic nerve system (SNS) may also be involved in offspring hypertension. Placental insufficiency has been reported to affect RAS programming 37 38 and animal models demonstrated increased sensitivity to anigiotensin II. 39 Additionally, blockage of RAS by angiotensin-converting enzyme inhibitor(ACEI) or angiotensin II type 1 receptor (AT1) blockade could prevent the development of hypertension in adult offspring of dams with reduced uterine perfusion pressure (RUPP), 40 41 suggesting the involvement of RAS in fetal programming. Increased SNS activity is tightly associated with hypertension. Activation of SNS has been found in low-birth-weight human and animal models of placental deficiency. 42 43 Chronic exposure to hypoxia can stimulate hyperinnervation and alterations in renal nerve activity. 44 45 Consequently, placental insufficiency and subsequent hypoxia result in altered renal nerve development and impaired blood pressure in offspring. Researchers discovered that renal denervation normalized hypertension in offspring exposed to placental insufficiency. 46 These studies provide evidence for the programming of kidney, RAS, and SNS in offspring hypertension due to poor intrauterine environment.
Interestingly, there is a line of evidence that prenatal exposure to elevated level of testosterone, observed in preeclamptic women, 30 47 is associated with increased blood pressure during adult life in female offspring. 48 Animal studies found that elevated level of androgen during pregnancy can lead to hyperactivity of hypothalamic-pituitary-gonadal axis and alteration in steroidogenic genes expression in the gonads of the offspring, resulting in increased production of testosterone. 49 50 More et al showed that prenatal exposure to elevated testosterone led to a decrease in the expression of Cyp11b2 resulting in reduced plasma aldosterone level of offspring, but the plasma volume and balance between Na + and K + were normal. 51 However, the level of plasma vasopressin, angiotensin II, vascular responsiveness to angiotensin II, and arterial pressure were increased in adult female offspring exposed to higher testosterone which might serve as compensatory response to maintain plasma volume and the balance between Na + and K + , in the meantime mediate hypertension in adult female offspring prenatally exposed to aldosterone. According to the mentioned above, prenatal exposure to elevated testosterone in pregnancy with preeclampsia might be a possible mechanism through which preeclampsia is associated with increased risk of hypertension in adult life of offspring. Henley et al showed that the level of adrenocorticotropic-hormone (ACTH) and cortisol were significantly elevated in 17-year-old offspring of women with preeclampsia, indicating that the activity of Hypothalamic-Pituitary-Adrenal (HPA) axis was reprogrammed due to the intrauterine exposure to preeclampsia, persisting into adulthood, which might account for the elevated blood pressure of offspring exposed to preeclampsia. 27
Epigenetic changes can be induced when the fetus is exposed to environmental stimuli, especially in the critical window of development. 52 The epigenetic changes include DNA methylation, histone modification, and the expression of noncoding RNA. DNA methylation is a covalent modification of gene with the stability in a heritable transgenerational way. 53 Methylation of critical regulatory sites of gene-like gene promoters can lead to down regulation of the expression of gene. There are some studies analyzing DNA methylation of genes associated with the fetal growth and development which are sensitive to the environmental perturbations in cord blood cells. Researchers found the hypomethylation of the promoter region of 11- β -hydroxysteroid-dehydrogenase-2-enzyme(11- β -HSD-2) in cord blood sample from women with preeclampsia. 54 Hypomethylation was observed in the differentially methylated regions of insulin-like growth factor 2 (IGF-2), which were crucial for the regulation of imprinted genes. 55 On the contrary, there are studies showing a decreased level of gene expression of 11- β -HSD-2 and IGF-2 in placenta from women with preeclampsia. 55 56 Researchers speculate that the discrepancy between the hypomethylation and down regulation of the genes might be a compensatory mechanism. However, it can also be an atypical decrease in the gene expression leading to the metabolic maladaptation. Recently, researchers conducted a genome-scale methylation analysis of cord blood DNAs associated with early-onset preeclampsia. They found hypomethylation or hypermethylation in different subsets of genes involved in lipid regulation and inflammation, suggesting a possible link between maternal preeclampsia and increased risks of cardiometabolic diseases in offspring. 57 Wang et al have showed alterations in methylation level of differentially methylated regions (DMR) of mesoderm specific transcript (MEST) related to adipocyte differentiation and obesity and DLK1 (Delta like non-canonical Notch ligand 1) encoding a protein preadipocye factor-1 (Pref-1) which is an inhibitor of adipocyte differentiation in placenta of preeclampsia 58 which might the mechanism through which preeclampsia is associated with increased risk of metabolic disorder in the later life of offspring. The epigenetic modulation can also occur in the fetus's renin–angiotensin–aldosterone system (RAAS). Human studies discovered that there were decreases in the DNA methylation of genes involved in RAAS in placentas of women exposed to early-onset preeclampsia. 59 Furthermore, researchers observed alterations in the level of cardiovascular and cerebrovascular diseases associated micro-RNAs expression in the umbilical cord blood of preeclampsia compared with normal pregnancy. 60 Micro-RNAs can regulate the expression of gene at the posttranscriptional level through the pathway of RNA interference. It can control gene expression through the cooperation with transcriptional factors as well. Micro-RNA expression changes in umbilical cord blood induced by preeclampsia might result from placenta dysfunctional and lead to the onset of cardiovascular and cerebrovascular diseases in later life of offspring. Recently, researchers found the downregulation of 16 micro-RNAs in fetal endothelial cells of preeclampsia including miR-29a/c-3p 25 which can lead to impaired fetal endothelial cells immigration through the disturbance of the FGF2-stimulated PI3K-AKT1 pathway, indicating that downregulation of micro-RNAs in fetal endothelial cells in preeclampsia might be the result of early fetal programming associated with the increased risks of cardiovascular diseases in later life of offspring since the impaired angiogenesis is a critical characteristic of cardiovascular diseases.
Nonetheless, a recent epidemiological study cast doubt on the hypothesis of “developmental programming.” The population-based study in Norway involving 15,778 participants showed that young adults (mean age: 29 years) born after pregnancy, complicated by preeclampsia, had higher SBP and DBP, an increase in BMI, and wilder waist circumference compared with offspring of normotensive pregnancies. However, after adjustment for maternal factors including maternal BMI and maternal blood pressure, the differences are strongly attenuated. 8 Intriguingly, researchers found that their siblings who were born after normotensive pregnancy had an identical cardiovascular risk profiles as those born after hypertension in pregnancy. The findings are in favor of the idea that most of the increased cardiovascular risk in offspring may be attributed to shared genetic and environmental factors. However, this study can't exclude the effects of intrauterine exposure to maternal hypertension. Lazdam et al found that offspring born after early-onset preeclampsia had higher SBP in childhood compared with those exposed to late-onset preeclampsia, suggesting the severity and duration of fetal exposure to maternal hypertension in pregnancy is critical for the cardiovascular outcome in offspring. 61 The study by Alsnes et al 8 didn't clarify the duration of exposure and short-term exposure to maternal hypertension in pregnancy may have minimal effects on long-term cardiovascular outcomes in offspring compared with genetic and environmental factors. Fig. 1 demonstrated the complex interplay of genetic, environmental factors, and fetal programming on the development of offspring hypertension.
Fig. 1.
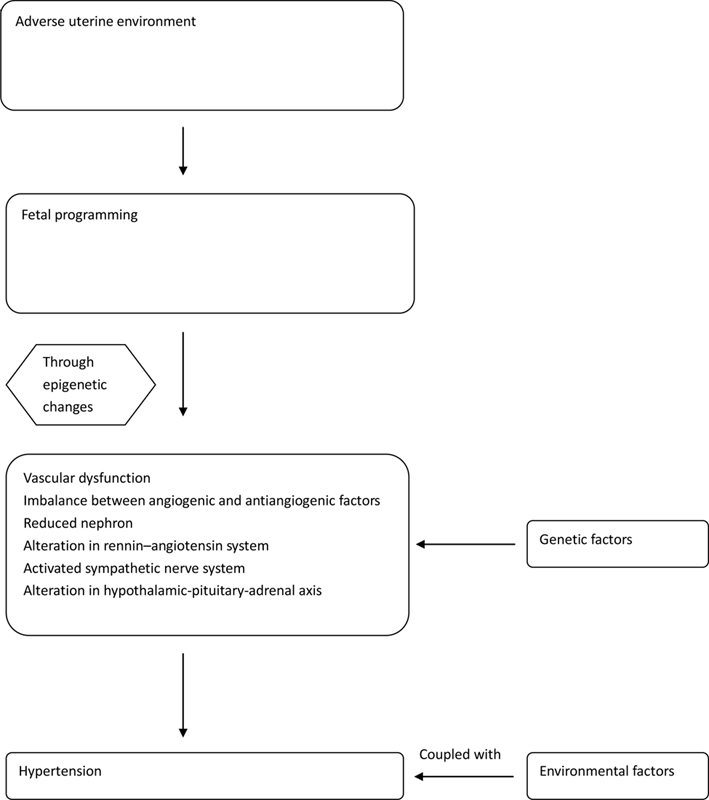
Mechanism underlying the development of hypertension in the offspring exposed to preeclampsia. Preeclampsia cause an adverse uterine environment which will lead to fetal programming. Epigenetic change is critical in programming resulting in disturbances in various pathways, coupled with the effects of genetic and environment factors, leading to hypertension in offspring.
Metabolic Outcome in Offspring. Epidemiological Evidence
Studies investigating metabolic effects indicated that preeclampsia has no significant effects on offspring ( Table 2 ). Five studies reported lipid profile between offspring of preeclampsia and normotensive pregnancy aged 10 to 17 years, 8 11 12 13 62 four of which found no statistically significant difference in total cholesterol, high-density lipoprotein (HDL) cholesterol, non-HDL cholesterol, 11 12 13 62 two of which found no statistically significant difference in triglycerides and lipoprotein, apoA1, apoB. 12 13 Only one study reported that offspring aged 29 years exposed to term preeclampsia had 0.14 (95% CI: 0.03–0.25) mmol/L higher non-HDL cholesterol and 0.13 (95% CI: 0.06–0.21) mmol/L higher serum concentration of triglycerides than term normotensive pregnancy. 8
Table 2. Summary of studies on metabolic effects on offspring.
| Authors, years of publication | Study design | Study groups ( n ) | Offspring birth year/ age when measured |
Summary of results | Confounders adjusted for | Definition of preeclampsia |
|---|---|---|---|---|---|---|
| Alsnes et al, 8 2017 | Prospective cohort studies | Preterm preeclampsia (27) Term preeclampsia (343) Normotensive pregnancy (15,072) |
Mean 29 years | Non-HDL cholesterol (mmol/L): mean (95% CI) term preeclampsia: 0.14 mmol/L (95% CI: 0.03–0.25 mmol/L) higher serum concentration of non-HDL cholesterol than normotensive pregnancy. Preterm preeclampsia: no strong evidence of differences between preterm preeclampsia and normo-tensive pregnancy. Triglycerides (mmol/L): mean (95% CI) term preeclampsia: 0.13 mmol/L (95% CI: 0.06–0.21 mmol/L) higher serum concentration of triglycerides than normotensive pregnancy. |
Offspring age and sex, maternal parity, cardiovascular risk factors, including maternal smoking, education, BMI, SBP, and DBP. | Sustained increase in blood pressure, mm Hg systolic and 90 mm Hg diastolic pressure, with onset after 20 weeks of gestation, with proteinuria after 20 th gestational week. |
| Kajantie et al, 64 2017 | Birth cohort study | Preeclampsia, nonsevere (97) Preeclampsia, severe (134) Normotensive pregnancy (3,524) |
50–61 y | Type 2 diabetes: hazard ratio (95% CI). Preeclampsia, nonsevere: 0.94 (95% CI: 0.58–1.53). Preeclampsia, severe: 1.02 (95% CI: 0.69–1.53). Normotensive pregnancy: referent. There was no association between the risk of T2D and maternal nonsevere or severe preeclampsia. |
Length of gestation and birth weight SD score, maternal age, height, BMI, and whether multiparous, childhood, and adult, and socioeconomic position. | Preeclampsia, nonsevere: At least one systolic measurement ≥ 140 mm Hg or diastolic ≥ 90 mm Hg after 20 weeks of gestation, all systolic measurements < 160 mm Hg and diastolic < 110 mm Hg with proteinuria the cut-off of which approximates to 1 mg/mL of albumin. Preeclampsia, severe: at least one systolic measurement ≥ 160 mm Hg or diastolic ≥ 110 mm Hg after 20 weeks of gestation with proteinuria, the cutoff of which approximates to 1 mg/mL of albumin. |
| Seppä et al, 63 2015 | Case control study | Preeclampsia (60) Normotensive pregnancy (60) |
12 y | Insulin sensitivity, serum adiponectin, leptin, IGF-1, IGF-2, IGFBP-1, sex hormone-binding globulin didn't differ between the preeclampsia and the studies didn’t adjust for the confounders. | The development of hypertension and proteinuria (> 300 mg of urinary protein in 24 h) after 20 weeks of gestation. | |
| Alsnes et al, 63 2014 | Nested case-control study | Preeclampsia (228) Nonpreeclampsia (383) |
11 y |
Normotensive pregnancy,
p
> 0.05 for all.
No statistically significant differences in total cholesterol, HDL cholesterol, non-HDL cholesterol, and glucose between offspring of mothers with and without preeclampsia. |
Mild preeclampsia was defined as an increase in DBP of at least 25 mm Hg and proteinuria 1 + on semiquantitative dipstick after 20 gestational wk. Moderate preeclampsia: at least 25 mm Hg increase in DBP and proteinuria 2 + on semiquantitative dipstick. Severe preeclampsia: DBP of at least 110 mm Hg and proteinuria 3 + on semiquantitative dipstick or at least 500 mg/24 h. |
|
| Fraser et al, 11 2013 | Prospective cohort study | Preeclampsia (53) Normotensive pregnancy (2,404) |
Mean 17 y | No strong evidence of differences in fasting insulin, glucose, or lipid concentrations between offspring of preeclampsia and normotensive pregnancy. | Offspring age, sex, maternal age at delivery, household social class, prepregnancy BMI, parity, and smoking in pregnancy. | SBP ≥ 140 mm Hg or DBP ≥ 90 mm Hg, measured on at least two occasions after 20 weeks of gestation, with proteinuria, diagnosed if the protein reading on dipstick testing was at least 1 + (30 mg/dL), occurring at the same time as the elevated blood pressure. |
| Miettola et al, 12 2013 | Prospective cohort study | Preeclampsia (197) Normotensive pregnancy (5,045) |
16 y | No significant differences in cholesterol, LDL, HDL, triglycerides, and lipoprotein, apoA1, apoB, insulin, glucose between offspring of preeclampsia and normotensive pregnancy. | Offspring sex, offspring BMI at age 16 y, birth weight, nulliparity maternal prepregnancy BMI, and socioeconomic position. | bp ≥ 140/90 mm Hg and proteinuria. |
| Lawlor et al, 13 2012 | Cohort study | Preeclampsia (70) Normotensive pregnancy (2,869) |
9.9 y | No statistically significant differences in LDL, HDL, triglycerides, and lipoprotein, apoA1, apoB between offspring of preeclampsia and normotensive pregnancy. | Offspring sex and age at the time of outcome measurement, BMI, birth weight, gestational age, mode of delivery. Maternal age, nulliparity, smoking during pregnancy, prepregnancy BMI, education, and head of household, and social class. |
SBP > 139 mm Hg or a DBP > 89 mm Hg, measured on at least two occasions after 20 weeks of gestation, with proteinuria, diagnosed if the protein reading on dipstick testing was at least 1 + (30 mg/dL), occurring at the same time as the elevated BP. |
Abbreviations: BMI, body mass index; BP, blood pressure; CI, confidence interval; DBP, diastolic blood pressure; HDL, high density lipoprotein; IGF, insulin like growth factor; IGFBP, IGF binding protein; LDL, low density lipoprotein; SD, standard deviation; T2D, type 2 diabetes.
Five studies were involved in glucose metabolism. The results were consistent. There were no differences in the concentration of insulin and glucose between offspring of preeclamptic women and those of women with normal pregnancy in childhood and adolescence. 11 12 62 In accordance with the results above, a recent study showed that insulin sensitivity measured by QUICKI (the Quantitative Insulin Sensitivity Check Index) in 12-year-old offspring born after preeclampsia didn't differ from those from normotensive pregnancy. 63 Kajantie et al found that there was no association between the risk of developing type 2 diabetes in offspring aged from 50 to 61 years and maternal nonsevere or severe preeclampsia, 64 but it should be interpreted with caution due to limited sample size of preeclampsia.
Neurological Effects in Offspring
Preeclampsia and ASD/ADHD in Offspring Epidemiological Evidence
We have found four studies investigating the association between preeclampsia and offspring autism spectrum disorder (ASD; Table 3 ). The epidemiological studies have reached an agreement and demonstrated a statistically significant increase in the odds of ASD in offspring exposed to preeclampsia. The OR ranges from 1.64 to 2.36. 65 66 67 68 Walker et al suggested that the risk of ASD increased with greater severity of preeclampsia(log odds of ASD relative to typical development [TD] in relation to preeclampsia severity: mild preeclampsia,1.69; severe preeclampsia, 2.04; p = 0.0188). 65 Five studies explored the risk of attention deficit hyperactivity disorder (ADHD) among offspring exposed to maternal preeclampsia( Table 3 ). 69 70 71 72 73 Four studies with a large number of participants demonstrated a positive association of preeclampsia and offspring ADHD with OR ranging from 1.19 to 1.34. 69 70 71 73 Silva et al found that preeclampsia was associated with increased risk of ADHD among offspring and female offspring are at higher risk than male offspring (OR: female, 1.28 [95% CI: 1.05–1.56]; male, 1.15 [95% CI: 1.03–1.27]). 69 In contrast, Amiri et al showed a protective association between preeclampsia and ADHD which didn't show statistical significance and take potential confounder into account. 72
Table 3. Summary of studies on neurological effects on offspring.
| Authors, years of publication | Study design | Study groups ( n ) | Offspring birth year/ age when measured |
Summary of results | Confounders adjusted for | Definition of preeclampsia |
|---|---|---|---|---|---|---|
| Walker et al, 65 2015 | Case control study | Autism spectrum disorder (ASD) (408) TD (277) |
24–60 mo | Children with ASD were twice more likely to have been exposed in utero to preeclampsia than controls with TD. OR = 2.36 (95% CI: 1.18–4.68). Risk increased with greater preeclampsia severity ( p = 0.02). |
Maternal educational level, parity, and prepregnancy obesity. | |
| Mann et al, 66 2010 | Children with ASD (472) Children without ASD (87,205) |
1996–2002 | Preeclampsia was significantly associated with greater odds of ASD. OR = 1.69 (95% CI: 1.26–2.28), p = 0.0005. |
Birth weight. | ||
| Burstyn et al, 67 2010 | Case control study | Preeclampsia (2,747) Nonpreeclampsia (212,473) |
1998–2004 | RR (95% CI) of ASD: preeclampsia = 1.49 (95% CI: 1.00–2.23). | ||
| Buchmayer et al, 68 2009 | Case control study | Patients with ASD (1,216) Patients without ASD (6,080) |
1987–2002 | Preeclampsia was associated with increased risk of ASD. OR = 1.64 (95% CI:1.08–2.49). |
Maternal age, smoking, maternal country of birth, whether the mother lived with the father, and maternal schizophrenia. | |
| Silva et al, 69 2014 | Case control study | Male: with ADHD (10,065), without ADHD (23,156) Female: with ADHD (2,926), without ADHD (6,915) |
1981–2003 aged < 25 y | Male: preeclampsia was associated with increased risk of ADHD. OR = 1.15 (95% CI: 1.03–1.27). Female: preeclampsia was associated with increased risk of ADHD. OR = 1.28 (95% CI: 1.05–1.56). |
Maternal age, Apgar's score at 5 min of birth, and SEIFA (data in model available for full dataset from 1981–2003). | |
| Getahun et al, 70 2013 | Nested case- control study |
With ADHD (13,613) Without ADHD (68,065) |
5–11 y | ADHD children were more likely to be exposed to preeclampsia. OR = 1.34 (95% CI: 1.25–1.44). |
Maternal age, education, smoking during pregnancy, parity, prenatal care, household income, psychosocial disorder during pregnancy, child race/ethnicity, and gender. | |
| Halmøy et al, 71 2012 | Case control study | Offspring with ADHD (2,323) Offspring without ADHD (1,170,073) |
1967–1987 | ADHD adults were more likely to be exposed to preeclampsia. OR = 1.2 (95% CI: 1.0–1.6). |
Year of birth, parity, age of mother at birth, educational level of mother, and marital status of mother. | |
| Amiri et al, 72 2012 | Case control study | Offspring with ADHD (164) Offspring without ADHD (166) |
9.2 ± 2.23 y in group with ADHD; 9.02 ± 1.53 y in group without ADHD | The frequency of preeclampsia: with ADHD: 3.7%, without ADHD: 4.9%, p = 0.78. | ||
| Mann and McDermott, 73 2011 | Case control study | Offspring with ADHD (7,911) Offspring without ADHD (76,810) |
1996–2002 |
Preeclampsia was significantly more common in mothers of children with ADHD (6.2 vs. 5.5%),
p
= 0.008.
OR: preeclampsia = 1.19 (95% CI: 1.03–1.37), p = 0.015. |
Infant sex, infant race, maternal education, maternal age, birth weight, alcohol use, and tobacco use. | Identified using ICD-9 codes 642.4–642.7. |
| Rätsep et al, 84 2016 | Cohort study | Preeclampsia (10) Uncomplicated pregnancy (10) |
7–10 y | Offspring of preeclampsia had reduced cognitive function including an impairment in working memory and visuospatial processing. | Children's age and sex | New-onset hypertension (> 140/90 mm Hg) and at least one of proteinuria (> 300 mg/d), thrombocytopenia(platelets < 105/L), renal insufficiency (serum creatinine > 1.1 mg/dL), impaired liver function (blood liver transaminases 2 × normal), pulmonary edema, or cerebral or visual disturbances occurring after the 20th week of gestation. |
| Warshafsky et al, 85 2016 | Prospective cohort study | Severe preeclampsia (95) Normotensive pregnancy (140) |
1–5 y | Offspring of severe preeclampsia exhibited lower social-cognitive and executive functioning development. | Severe preeclampsia:SBP ≥ 1 60 mm Hg, DBP ≥ 110 mm Hg, proteinuria ≥ 5 g in 24 h or ≥ 3 + on dipstick, oliguria (≤ 500 mL in 24 h), cerebral or visual disturbances, epigastric pain, thrombocytopenia (< 150,000 × 109/L), increase in AST (> 46 U/L) and ALT (> 40 U/L), elevated serum creatinine (> 106 pmol/L), pulmonary edema or cyanosis, IUGR, or eclampsia. | |
| Tuovinen et al, 86 2014 | Helsinki birth cohort study | Preeclampsia (24) Normotensive pregnancy (494) |
69.3 + 3.1 y | Problems in adaptive functioning to spouse. Preeclampsia: OR = 4.12 (95% CI: 1.35–12.96), p = 0.01. Normotensive pregnancy as referent. Functional impairment. Preeclampsia: OR = 2.99 (95% CI: 1.08–8.24), p = 0.03. Memory/cognition: Preeclampsia: OR = 3.92 (95% CI: 1.39–11.04), p = 0.01. Depressive symptoms. Preeclampsia: OR = 6.79 (95% CI: 2.41–19.08). |
Sex, year of birth (1934–1938 vs. 1939–1944), gestational age, weight for gestational age, head circumference at birth, placental weight, father's occupational status in patients childhood, parity, mother's age, BMI at delivery, breastfeeding, own maximum level of education in adulthood, and age at completion of the questionnaire. | SBP ≥ 140 mm Hg or DBP ≥ 90 mm Hg occurring after 20 weeks of gestation with a 1 + proteinuria reading on dipstick in random urine sample. |
| Morsing et al, 87 2014 | Case control study | Very preterm birth with exposure to preeclampsia (the exposed PT-IUGR; 11) Very preterm birth without exposure to preeclampsia (the nonexposed PT-IUGR; 23) Appropriate for gestational age without exposure to preeclampsia (PT-AGA; 34) |
5–8 y |
Verbal IQ: mean + SD the exposed PT-IUGR: 74 ± 16, the nonexposed PT-IUGR: 89 ± 15;
p
= 0.013.
PT-AGA: 96 ± 15, p < 0.001; full scale IQ: mean ± SD the exposed PT-IUGR: 70 ± 19. The nonexposed PT-IUGR: 83 ± 14, p = 0.029; PT-AGA: 90 ± 14, p = 0.001. |
DBP > 90 mm Hg on two or more occasions and proteinuria > 300 mg/L. | |
| Griffith et al, 88 2011 | Case control study | Children with intellectual disability (1,636) Comparison children (79,230) |
3–5 y | Preeclampsia was associated with the increased risk of intellectual disability. OR = 1.579 (95% CI: 1.334–1.870) |
Maternal age, white race, education, birth year, and female sex but not low birth weight or preterm status. | ICD-9 codes |
| Ehrenstein et al, 89 2009 | Follow-up | Preeclampsia (604) Normotensive pregnancy (16,555) |
18–19 y | Preeclampsia was associated with the increased risk of low cognitive function. (IQ < 85) Prevalence ratio: 1.32 (95% CI: 1.08–1.62). | Maternal age, parity, marital status, and history of diabetes; and for conscripts' year of birth, country of birth, birth weight in grams, and being large for gestational age. | New onset of hypertension (> 140/90 mm Hg blood pressure) in the second half of pregnancy with de novo proteinuria (> 0.3 g over 24 h) or edema. |
| Eide et al, 108 2013 | Cohort study | Preeclampsia (15,622) | 1967–1982 | Schizophrenia Preeclampsia: OR = 1.3 (95% CI: 1.0–1.8). |
Maternal age, education, parity; marital status: unmarried, married; sex: male, female, and year of birth. | Increase in blood pressure to at least 140/90 mm Hg after the 20th week of gestation, an increase in DBP ≥ 15 mm Hg or SBP ≥ 30 mm Hg from the level measured before 20th week, with proteinuria (≥ 300 mg/24 h). |
| Tuovinen et al, 107 2010 | Cohort study | Preeclampsia | 60, 63 y | Depressive symptoms: participants born after preeclampsia had over 30% higher depressive symptom scores than normotensive pregnancy, p < 0.04 | Mother's age and BMI at delivery, the participant's body size at birth/length of gestation, sex and childhood socioeconomic status, age and educational attainment at testing | BP ≥ 140/90 mm Hg with proteinuria |
Abbreviations: ADHD, attention deficit hyperactivity disorder; ALT, alanine aminotransferase; ASD, autism spectrum disorder; AST, aspartate aminotransferase; CI, confidence interval; ICD-9, international classification of disease, 9th edition; IQ, intelligence quotient; OR, odds ratio; RR, risk ratio; SD, standard deviation; TD, typical development.
The Underlying Mechanism
Although the mechanism underlying the association of preeclampsia and increased risks of ASD/ADHD in offspring is not clearly identified, insufficient uteroplacental perfusion, placental ischemia, hypoxia, limited nutrient, and oxidative stress and inflammation state in preeclampsia may play a role in the pathogenesis of ASD/ADHD. Evidence from animal studies and neuroimaging studies reported adverse effects of placental ischemia on fetal brain development. 74 75 A line of studies have demonstrated that ADHD is associated with brain abnormalities including decreased global cortical thickness, smaller total brain, and gray matter volume. 76 77 In consistent with these studies, an animal study reported long-term attention deficits in rats that underwent hypoxicischemia, which exhibited global brain atrophy. 78 In recent years, interleukin-6 (IL-6) has raised researcher's awareness. It is an inflammatory cytokines, which can cross the placenta, and have the potential to regulate fetus's neuronal proliferation, differentiation, and function. A population-based study involving 1 million pregnancy showed that higher levels of C-reactive protein which is an inflammatory biomarker in preeclampsia is associated with a 43% increase in the risk of ASD in offspring. Researchers found that exposure of neuron from Sprague–Dawley rat embryos to serum of women with preeclampsia can increase neuron growth. 79 Although, this finding cannot directly suggest a causal relationship with the risk of autism, it indicates that circulating factors in maternal serum of preeclampsia can alter the pattern of fetal neuronal growth. Recently, an literature published in Science discovered that elevated level of maternal IL-17a in the rodent maternal immune activation (MIA) model can lead to cortical defects and associated autism behavior in the offspring. 80 It has been known to us that IL-17 levels are increased in the maternal circulation and the maternal immune response is disturbed with a shift to proinflammatory state in preeclampsia. 81 Therefore, it is reasonable to speculate that the disturbance in immune response in women with preeclampsia may play a role in the neurodevelopmental outcome in the offspring. Future research is needed to clarify whether IL-17 is the underlying intermediate through which preeclampsia affect the offspring's neurodevelopment. It is worth noting that IL-6 has been observed to mediate the effect of MIA on the offspring suggesting IL-6 signaling in placenta can control fetal brain development and behavior. 82 IL-6 activation can serve to relay inflammatory signals to the fetal brain and exert effects on the behaviors and neuropathologies associated with ASDs. In consistent with this, Curran et al found four of five preeclampsia samples those had elevated IL-6 levels compared with control groups. 79 There are other studies investigating the role of maternal cytokines. Jones et al found that mothers of children diagnosed with autism with intellectual disability had increased levels of cytokines and chemokines including IL-6, interferon-r, IL-1a, granulocyte macrophage colony-stimulating factors in midgestation, indicating the potential role of abnormal immune response in pregnancy which are commonly observed in preeclampsia in the increased risk of autism. 83
Preeclampsia and Cognitive Impairment in Offspring Epidemiological Evidence
Six studies analyzed the cognitive function of offspring exposed to maternal preeclampsia ( Table 3 ). 84 85 86 87 88 89 All of them showed that intrauterine exposure to preeclampsia had an adverse effect on offspring cognitive function after controlling for prenatal and demographic covariates. Rätsep et al evaluated the cognitive function among children aged 7 to 10 years who were exposed to preeclampsia and they found those children had an impairment in working memory and visuospatial processing. 84 Warshafsky et al discovered that offspring aged 1 to 5 years exposed to severe preeclampsia exhibited lower sociocognitive and executive functioning development compared with those born after normal pregnancy. 85 Morsing and Maršál calculated intelligence quotient (IQ) among offspring aged 5 to 8 years born very preterm. 87 Those exposed to preeclampsia had statistically significantly lower verbal IQ and full scale IQ compared with those who were not exposed to preeclampsia (verbal IQ: 74 ± 16 vs. 89 ± 15, p = 0.013; full scale IQ: 70 ± 19 vs. 83 ± 14, p = 0.029). In consistent with these studies, Griffith et al found that preeclampsia was associated with increased risk of intellectual disability among children at 3 to 5 years (OR: 1.579 [95% CI: 1.334–1.870]). 88 Ehrenstein et al investigated the association of preeclampsia and offspring cognitive function at 18 to 19 years and they found offspring exposed to preeclampsia were at increased risk of low cognitive function which was defined as IQ < 85 (prevalence ratio: 1.32 [95%CI: 1.08–1.62]). 89 Tuovinen et al evaluated cognitive function in participants from Helsinki birth cohort study aged 69.3 years. 86 Offspring born after preeclampsia were at increased risk of having impairment in memory and cognition (OR: 3.92 [95%CI: 1.39–11.04], p = 0.01) compared with normotensive pregnancy.
The Underlying Mechanism
A rodent study found that the spatial learning and memory ability was impaired in offspring of preeclamptic rat model, which might be associated with the defective neurogenesis in offspring hippocampus observed in this study. 90 91 Zhu et al showed that 8-week-old offspring of preeclampsia-like rat induced by NG-nitro-L-arginine methyl ester(L-NAME) had impaired cognitive ability and had increased expression of glucocorticoid receptor (GR) in the hippocampus 92 which might be the underlying mechanism of the impaired cognitive ability in offspring of preeclampsia.
There is a literature demonstrating the positive effects of improved nutrition on the brain function. 93 Nutrients play an important role in the brain development and the regulation of levels of neurotrophins. 94 95 Neurotrophins have been known to be critical in the maintenance of brain plasticity and cognitive function. Recently, a study has examined the levels of neurotrophins in the offspring of pregnancy-induced hypertension rat. Researchers found that the level of BDNF (brain-derived neurotrophins factor) was lower in the cortex of offspring in pregnancy induced hypertension (PIH) group compared with normotensive group and the cognitive performance was impaired. In another group, in which researchers provided combined micronutrients supplementation to dams during pregnancy including folate, vitamin B12, and DHA (docosahexaenoic acid), all of which are key components of one carbon cycle and have been reported to be altered in the preeclamptic women, 96 the levels of BDNF was higher and cognitive performance was improved. This study discovered an association between the deficiency of neurotrophins in the PIH offspring and impaired cognitive ability. 97
A recent pilot study examined brain structural and vascular anatomy of 7 to 10 years old offspring exposed to preeclampsia compared with matched controls by magnetic resonance imaging (MRI). 98 Researcher found offspring exposed to preeclampsia exhibited enlarged brain regional volume including the temporal lobe, cerebellum, brain stem, and the right and left amygdalae, as well as reduced vessel radii in the occipital and parietal lobes compared with matched controls, which are correlated with the psychometric test showing deficiency in working memory and visuaspatial processing in offspring exposed to preeclampsia. 84 The alterations in brain structure above also shared similarities with those observed in autism. In addition, they showed a decreased level of placental growth factor in the maternal plasma samples from women with preeclampsia. 98 Placental growth factor is a critical angiogenic cytokines expressed at increased level in normal pregnancy to optimize the development of vasculature in decidua basalis and sustain cardiac function in late gestation. 99 100 101 The deficiency in maternal serum placental growth factor (PGF) is associated with an increased risk of preeclampsia which can serve to be a predictive biomarker of preeclampsia, especially when combined with elevated blood pressure and increased level of other antiangiogenic factors, such as soluble sFlt-1. 102 Moreover, rodent studies have demonstrated the critical role of PGF in neurovascular development. Rätsep et al showed that genetically-deleted for placental growth factor mice had detectable alterations in the cerebrovascular including narrower lumen, atypical crossovers, and atypical collateral branching and brain neurological development from midgestation to adulthood, 103 accompanied by impaired cognition. After injury, PGF deficient mice have30% reduced Schwann's cells proliferation and significantly delayed macrophage invasion, leading to worse functional recovery. 104 It has been reported that the timeframes of circle of Wills's formation and suboptimal production of PGF overlap in human. 105 Therefore, it's reasonable to speculate that PGF deficiency in preeclampsia might impair fetal the cerebrovascular and brain neurological development and thus result in impaired cognitive ability. 106 However, it should be noted that the deficiency of PGF in maternal plasma of preeclampsia does not mean that fetal PGF levels are lower than normal. Thus, further research are needed to clarify whether the level of fetal PGF is abnormal and its' exact role in altered cerebral and vascular structure and impaired cognitive function.
PE and other Neurological Outcome in Offspring
Epidemiological Evidence
Tuovinen et al also evaluated depressive symptoms in offspring exposed to preeclampsia. 86 107 They found participants born after preeclampsia had over 30% higher depressive symptom scores than normotensive pregnancy( p < 0.04) at the age of 60 and 63 years. 107 Offspring aged 69.3 years exposed to preeclampsia were also at higher risk of having depressive symptoms (OR: 6.79 [95%CI: 2.41–19.08]) after accounting for birth weight and gestational age. 86 They were also at increased risk of having problems in adaptive functioning to spouse (OR: 4.12 [95% CI: 1.35–12.96], p = 0.01). 86 There was a study reporting a positive association between preeclampsia and schizophrenia in offspring. Eide et al conducted a population-based cohort study with large scale of population showed that offspring exposed to preeclampsia were at increased risks of schizophrenia and the risk was 37% higher compared with nonexposed offspring. 108
The Underlying Mechanism
Preeclampsia is associated with reduced function of 11- β -HSD-2 in placenta 109 which can catalyze the conversion of maternal circulating cortisol into inactive cortisone. Therefore, fetus might be overexposed to maternal glucocorticoids which have the potential to program fetal HPA axis. The alteration in HPA axis is highly associated with biology underlying depression. 110 However, the extent to which this mechanism is involved in the association between preeclampsia and increased risks of depression in offspring remains unanswered.
Conclusion
We not only made a review of epidemiological studies investigating lasting effects of preeclampsia on offspring but also comprehensively reviewed the possible mechanism. A large number of studies suggest that maternal preeclampsia has an overall negative effect on offspring cardiovascular and neurological health. Whereas, there is no significant difference in lipid profile and glucose metabolism between offspring born after preeclampsia and normotensive pregnancy. However, the agreement on the exact mechanism through which preeclampsia exert long-lasting effects on offspring has not been reached; therefore, further studies are needed to clarify it. Based on the epidemiological evidence, it is necessary to take the long-term health outcome of offspring into account in the clinical management of preeclampsia and early prevention and intervention strategies should be taken.
Funding Statement
Funding Information This study was supported by the National Natural Science Foundation of China 81571460.
Footnotes
Conflict of Interests The Authors declare that there is no conflict of interest.
References
- 1.Brown M A, Magee L A, Kenny L C et al. The hypertensive disorders of pregnancy: ISSHP classification, diagnosis & management recommendations for international practice. Pregnancy Hypertens. 2018;13:291–310. doi: 10.1016/j.preghy.2018.05.004. [DOI] [PubMed] [Google Scholar]
- 2.Phipps E A, Thadhani R, Benzing T, Karumanchi S A.Pre-eclampsia: pathogenesis, novel diagnostics and therapiesNat Rev Nephrol2019; (e-pub ahead of print) Doi: 10.1038/s41581-019-0119-6 [DOI] [PMC free article] [PubMed]
- 3.Lu H Q, Hu R.The role of immunity in the pathogenesis and development of preeclampsiaScand J Immunol2019; (e-pub ahead of print) Doi: 10.1111/sji.12756 [DOI] [PubMed]
- 4.Lisonkova S, Joseph K S. Incidence of preeclampsia: risk factors and outcomes associated with early- versus late-onset disease. Am J Obstet Gynecol. 2013;209(06):5440–5.44E14. doi: 10.1016/j.ajog.2013.08.019. [DOI] [PubMed] [Google Scholar]
- 5.Amaral L M, Cunningham M W, Jr., Cornelius D C, LaMarca B. Preeclampsia: long-term consequences for vascular health. Vasc Health Risk Manag. 2015;11:403–415. doi: 10.2147/VHRM.S64798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barker D J. Adult consequences of fetal growth restriction. Clin Obstet Gynecol. 2006;49(02):270–283. doi: 10.1097/00003081-200606000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Barker D J, Bagby S P, Hanson M A. Mechanisms of disease: in utero programming in the pathogenesis of hypertension. Nat Clin Pract Nephrol. 2006;2(12):700–707. doi: 10.1038/ncpneph0344. [DOI] [PubMed] [Google Scholar]
- 8.Alsnes I V, Vatten L J, Fraser A et al. Hypertension in pregnancy and offspring cardiovascular risk in young adulthood: prospective and sibling studies in the HUNT study (Nord-Trøndelag health study) in Norway. Hypertension. 2017;69(04):591–598. doi: 10.1161/HYPERTENSIONAHA.116.08414. [DOI] [PubMed] [Google Scholar]
- 9.Miliku K, Bergen N E, Bakker H et al. Associations of maternal and paternal blood pressure patterns and hypertensive disorders during pregnancy with childhood blood pressure. J Am Heart Assoc. 2016;5(10):e003884. doi: 10.1161/JAHA.116.003884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Staley J R, Bradley J, Silverwood R J et al. Associations of blood pressure in pregnancy with offspring blood pressure trajectories during childhood and adolescence: findings from a prospective study. J Am Heart Assoc. 2015;4(05):e001422. doi: 10.1161/JAHA.114.001422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fraser A, Nelson S M, Macdonald-Wallis C, Sattar N, Lawlor D A. Hypertensive disorders of pregnancy and cardiometabolic health in adolescent offspring. Hypertension. 2013;62(03):614–620. doi: 10.1161/HYPERTENSIONAHA.113.01513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miettola S, Hartikainen A L, Vääräsmäki M et al. Offspring's blood pressure and metabolic phenotype after exposure to gestational hypertension in utero. Eur J Epidemiol. 2013;28(01):87–98. doi: 10.1007/s10654-013-9763-5. [DOI] [PubMed] [Google Scholar]
- 13.Lawlor D A, Macdonald-Wallis C, Fraser A et al. Cardiovascular biomarkers and vascular function during childhood in the offspring of mothers with hypertensive disorders of pregnancy: findings from the Avon Longitudinal Study of Parents and Children. Eur Heart J. 2012;33(03):335–345. doi: 10.1093/eurheartj/ehr300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Geelhoed J J, Fraser A, Tilling K et al. Preeclampsia and gestational hypertension are associated with childhood blood pressure independently of family adiposity measures: the Avon Longitudinal Study of Parents and Children. Circulation. 2010;122(12):1192–1199. doi: 10.1161/CIRCULATIONAHA.110.936674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Øglaend B, Forman M R, Romundstad P R, Nilsen S T, Vatten L J. Blood pressure in early adolescence in the offspring of preeclamptic and normotensive pregnancies. J Hypertens. 2009;27(10):2051–2054. doi: 10.1097/HJH.0b013e328330052a. [DOI] [PubMed] [Google Scholar]
- 16.Jayet P Y, Rimoldi S F, Stuber T et al. Pulmonary and systemic vascular dysfunction in young offspring of mothers with preeclampsia. Circulation. 2010;122(05):488–494. doi: 10.1161/CIRCULATIONAHA.110.941203. [DOI] [PubMed] [Google Scholar]
- 17.Boyd H A, Basit S, Behrens I et al. Association between fetal congenital heart defects and maternal risk of hypertensive disorders of pregnancy in the same pregnancy and across pregnancies. Circulation. 2017;136(01):39–48. doi: 10.1161/CIRCULATIONAHA.116.024600. [DOI] [PubMed] [Google Scholar]
- 18.Timpka S, Macdonald-Wallis C, Hughes A D et al. Hypertensive disorders of pregnancy and offspring cardiac structure and function in adolescence. J Am Heart Assoc. 2016;5(11):e003906. doi: 10.1161/JAHA.116.003906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Auger N, Fraser W D, Healy-Profitós J, Arbour L. Association between preeclampsia and congenital heart defects. JAMA. 2015;314(15):1588–1598. doi: 10.1001/jama.2015.12505. [DOI] [PubMed] [Google Scholar]
- 20.Brodwall K, Leirgul E, Greve G et al. Possible common aetiology behind maternal preeclampsia and congenital heart defects in the child: a cardiovascular diseases in Norway project study. Paediatr Perinat Epidemiol. 2016;30(01):76–85. doi: 10.1111/ppe.12252. [DOI] [PubMed] [Google Scholar]
- 21.Kajantie E, Eriksson J G, Osmond C, Thornburg K, Barker D J. Pre-eclampsia is associated with increased risk of stroke in the adult offspring: the Helsinki birth cohort study. Stroke. 2009;40(04):1176–1180. doi: 10.1161/STROKEAHA.108.538025. [DOI] [PubMed] [Google Scholar]
- 22.Nahum Sacks K, Friger M, Shoham-Vardi I et al. Prenatal exposure to preeclampsia as an independent risk factor for long-term cardiovascular morbidity of the offspring. Pregnancy Hypertens. 2018;13:181–186. doi: 10.1016/j.preghy.2018.06.013. [DOI] [PubMed] [Google Scholar]
- 23.Salonen Ros H, Lichtenstein P, Lipworth L, Cnattingius S. Genetic effects on the liability of developing pre-eclampsia and gestational hypertension. Am J Med Genet. 2000;91(04):256–260. [PubMed] [Google Scholar]
- 24.Bergvall N, Cnattingius S. Familial (shared environmental and genetic) factors and the foetal origins of cardiovascular diseases and type 2 diabetes: a review of the literature. J Intern Med. 2008;264(03):205–223. doi: 10.1111/j.1365-2796.2008.01974.x. [DOI] [PubMed] [Google Scholar]
- 25.Zhou C, Zou Q Y, Li H et al. Preeclampsia downregulates microRNAs in fetal endothelial cells: roles of miR-29a/c-3p in endothelial function. J Clin Endocrinol Metab. 2017;102(09):3470–3479. doi: 10.1210/jc.2017-00849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wlodek M E, Westcott K, Siebel A L, Owens J A, Moritz K M. Growth restriction before or after birth reduces nephron number and increases blood pressure in male rats. Kidney Int. 2008;74(02):187–195. doi: 10.1038/ki.2008.153. [DOI] [PubMed] [Google Scholar]
- 27.Henley D, Brown S, Pennell C, Lye S, Torpy D J. Evidence for central hypercortisolism and elevated blood pressure in adolescent offspring of mothers with pre-eclampsia. Clin Endocrinol (Oxf) 2016;85(04):583–589. doi: 10.1111/cen.13092. [DOI] [PubMed] [Google Scholar]
- 28.Byers B D, Betancourt A, Lu F et al. The effect of prepregnancy obesity and sFlt-1-induced preeclampsia-like syndrome on fetal programming of adult vascular function in a mouse model. Am J Obstet Gynecol. 2009;200(04):4320–4.32E9. doi: 10.1016/j.ajog.2009.01.044. [DOI] [PubMed] [Google Scholar]
- 29.Ojeda N B, Grigore D, Yanes L L et al. Testosterone contributes to marked elevations in mean arterial pressure in adult male intrauterine growth restricted offspring. Am J Physiol Regul Integr Comp Physiol. 2007;292(02):R758–R763. doi: 10.1152/ajpregu.00311.2006. [DOI] [PubMed] [Google Scholar]
- 30.Ghorashi V, Sheikhvatan M. The relationship between serum concentration of free testosterone and pre-eclampsia. Endokrynol Pol. 2008;59(05):390–392. [PubMed] [Google Scholar]
- 31.Dharmashankar K, Widlansky M E. Vascular endothelial function and hypertension: insights and directions. Curr Hypertens Rep. 2010;12(06):448–455. doi: 10.1007/s11906-010-0150-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lewandowski A J, Davis E F, Yu G et al. Elevated blood pressure in preterm-born offspring associates with a distinct antiangiogenic state and microvascular abnormalities in adult life. Hypertension. 2015;65(03):607–614. doi: 10.1161/HYPERTENSIONAHA.114.04662. [DOI] [PubMed] [Google Scholar]
- 33.Llurba E, Sánchez O, Ferrer Q et al. Maternal and foetal angiogenic imbalance in congenital heart defects. Eur Heart J. 2014;35(11):701–707. doi: 10.1093/eurheartj/eht389. [DOI] [PubMed] [Google Scholar]
- 34.Roberts J M, Bell M J.If we know so much about preeclampsia, why haven't we cured the disease? J Reprod Immunol 201399(1,2):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wlodek M E, Mibus A, Tan A, Siebel A L, Owens J A, Moritz K M. Normal lactational environment restores nephron endowment and prevents hypertension after placental restriction in the rat. J Am Soc Nephrol. 2007;18(06):1688–1696. doi: 10.1681/ASN.2007010015. [DOI] [PubMed] [Google Scholar]
- 36.Singh R R, Denton K M, Bertram J F, Jefferies A J, Moritz K M. Reduced nephron endowment due to fetal uninephrectomy impairs renal sodium handling in male sheep. Clin Sci (Lond) 2010;118(11):669–680. doi: 10.1042/CS20090479. [DOI] [PubMed] [Google Scholar]
- 37.Grigore D, Ojeda N B, Robertson E B et al. Placental insufficiency results in temporal alterations in the renin angiotensin system in male hypertensive growth restricted offspring. Am J Physiol Regul Integr Comp Physiol. 2007;293(02):R804–R811. doi: 10.1152/ajpregu.00725.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang D Y, Lumbers E R, Simonetta G et al. Effects of placental insufficiency on the ovine fetal renin-angiotensin system. Exp Physiol. 2000;85(01):79–84. [PubMed] [Google Scholar]
- 39.Rasch R, Skriver E, Woods L L. The role of the RAS in programming of adult hypertension. Acta Physiol Scand. 2004;181(04):537–542. doi: 10.1111/j.1365-201X.2004.01328.x. [DOI] [PubMed] [Google Scholar]
- 40.Alwasel S H, Kaleem I, Sahajpal V, Ashton N. Maternal protein restriction reduces angiotensin II AT(1) and AT(2) receptor expression in the fetal rat kidney. Kidney Blood Press Res. 2010;33(04):251–259. doi: 10.1159/000317739. [DOI] [PubMed] [Google Scholar]
- 41.Manning J, Vehaskari V M. Low birth weight-associated adult hypertension in the rat. Pediatr Nephrol. 2001;16(05):417–422. doi: 10.1007/s004670000560. [DOI] [PubMed] [Google Scholar]
- 42.IJzerman R G, Stehouwer C D, de Geus E J, van Weissenbruch M M, Delemarre-van de Waal H A, Boomsma D I. Low birth weight is associated with increased sympathetic activity: dependence on genetic factors. Circulation. 2003;108(05):566–571. doi: 10.1161/01.CIR.0000081778.35370.1B. [DOI] [PubMed] [Google Scholar]
- 43.Sanders M W, Fazzi G E, Janssen G M, de Leeuw P W, Blanco C E, De Mey J G. Reduced uteroplacental blood flow alters renal arterial reactivity and glomerular properties in the rat offspring. Hypertension. 2004;43(06):1283–1289. doi: 10.1161/01.HYP.0000127787.85259.1f. [DOI] [PubMed] [Google Scholar]
- 44.Rouwet E V, Tintu A N, Schellings M W et al. Hypoxia induces aortic hypertrophic growth, left ventricular dysfunction, and sympathetic hyperinnervation of peripheral arteries in the chick embryo. Circulation. 2002;105(23):2791–2796. doi: 10.1161/01.cir.0000017497.47084.06. [DOI] [PubMed] [Google Scholar]
- 45.Maduwegedera D, Kett M M, Flower R L et al. Sex differences in postnatal growth and renal development in offspring of rabbit mothers with chronic secondary hypertension. Am J Physiol Regul Integr Comp Physiol. 2007;292(02):R706–R714. doi: 10.1152/ajpregu.00458.2006. [DOI] [PubMed] [Google Scholar]
- 46.Alexander B T, Hendon A E, Ferril G, Dwyer T M. Renal denervation abolishes hypertension in low-birth-weight offspring from pregnant rats with reduced uterine perfusion. Hypertension. 2005;45(04):754–758. doi: 10.1161/01.HYP.0000153319.20340.2a. [DOI] [PubMed] [Google Scholar]
- 47.Salamalekis E, Bakas P, Vitoratos N, Eleptheriadis M, Creatsas G. Androgen levels in the third trimester of pregnancy in patients with preeclampsia. Eur J Obstet Gynecol Reprod Biol. 2006;126(01):16–19. doi: 10.1016/j.ejogrb.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 48.Sathishkumar K, Elkins R, Yallampalli U, Balakrishnan M, Yallampalli C. Fetal programming of adult hypertension in female rat offspring exposed to androgens in utero. Early Hum Dev. 2011;87(06):407–414. doi: 10.1016/j.earlhumdev.2011.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chinnathambi V, Balakrishnan M, Yallampalli C, Sathishkumar K.Prenatal testosterone exposure leads to hypertension that is gonadal hormone-dependent in adult rat male and female offspring Biol Reprod 20128605137, 1–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wu X Y, Li Z L, Wu C Y et al. Endocrine traits of polycystic ovary syndrome in prenatally androgenized female Sprague-Dawley rats. Endocr J. 2010;57(03):201–209. doi: 10.1507/endocrj.k09e-205. [DOI] [PubMed] [Google Scholar]
- 51.More A S, Mishra J S, Hankins G D, Kumar S. Prenatal testosterone exposure decreases aldosterone production but maintains normal plasma volume and increases blood pressure in adult female rats. Biol Reprod. 2016;95(02):42. doi: 10.1095/biolreprod.116.141705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jiménez-Chillarón J C, Díaz R, Martínez D et al. The role of nutrition on epigenetic modifications and their implications on health. Biochimie. 2012;94(11):2242–2263. doi: 10.1016/j.biochi.2012.06.012. [DOI] [PubMed] [Google Scholar]
- 53.Orozco L D, Rubbi L, Martin L J et al. Intergenerational genomic DNA methylation patterns in mouse hybrid strains. Genome Biol. 2014;15(05):R68. doi: 10.1186/gb-2014-15-5-r68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hu W, Weng X, Dong M, Liu Y, Li W, Huang H. Alteration in methylation level at 11β-hydroxysteroid dehydrogenase type 2 gene promoter in infants born to preeclamptic women. BMC Genet. 2014;15:96. doi: 10.1186/s12863-014-0096-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Aufdenblatten M, Baumann M, Raio L et al. Prematurity is related to high placental cortisol in preeclampsia. Pediatr Res. 2009;65(02):198–202. doi: 10.1203/PDR.0b013e31818d6c24. [DOI] [PubMed] [Google Scholar]
- 56.Bourque D K, Avila L, Peñaherrera M, von Dadelszen P, Robinson W P. Decreased placental methylation at the H19/IGF2 imprinting control region is associated with normotensive intrauterine growth restriction but not preeclampsia. Placenta. 2010;31(03):197–202. doi: 10.1016/j.placenta.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 57.Ching T, Ha J, Song M A et al. Genome-scale hypomethylation in the cord blood DNAs associated with early onset preeclampsia. Clin Epigenetics. 2015;7:21. doi: 10.1186/s13148-015-0052-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wang X, Wan L, Weng X et al. Alteration in methylation level at differential methylated regions of MEST and DLK1 in fetus of preeclampsia. Hypertens Pregnancy. 2018;37(01):1–8. doi: 10.1080/10641955.2017.1397689. [DOI] [PubMed] [Google Scholar]
- 59.Blair J D, Yuen R K, Lim B K, McFadden D E, von Dadelszen P, Robinson W P. Widespread DNA hypomethylation at gene enhancer regions in placentas associated with early-onset pre-eclampsia. Mol Hum Reprod. 2013;19(10):697–708. doi: 10.1093/molehr/gat044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hromadnikova I, Kotlabova K, Ivankova K, Vedmetskaya Y, Krofta L. Profiling of cardiovascular and cerebrovascular disease associated microRNA expression in umbilical cord blood in gestational hypertension, preeclampsia and fetal growth restriction. Int J Cardiol. 2017;249:402–409. doi: 10.1016/j.ijcard.2017.07.045. [DOI] [PubMed] [Google Scholar]
- 61.Lazdam M, de la Horra A, Diesch J et al. Unique blood pressure characteristics in mother and offspring after early onset preeclampsia. Hypertension. 2012;60(05):1338–1345. doi: 10.1161/HYPERTENSIONAHA.112.198366. [DOI] [PubMed] [Google Scholar]
- 62.Alsnes I V, Janszky I, Forman M R, Vatten L J, Økland I. A population-based study of associations between preeclampsia and later cardiovascular risk factors. Am J Obstet Gynecol. 2014;211(06):6570–6.57E9. doi: 10.1016/j.ajog.2014.06.026. [DOI] [PubMed] [Google Scholar]
- 63.Seppä S, Voutilainen R, Tenhola S. Markers of insulin sensitivity in 12-year-old children born from preeclamptic pregnancies. J Pediatr. 2015;167(01):125–130. doi: 10.1016/j.jpeds.2015.04.015. [DOI] [PubMed] [Google Scholar]
- 64.Kajantie E, Osmond C, Eriksson J G. Gestational hypertension is associated with increased risk of type 2 diabetes in adult offspring: the Helsinki Birth Cohort Study. Am J Obstet Gynecol. 2017;216(03):2810–2.81E9. doi: 10.1016/j.ajog.2016.10.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Walker C K, Krakowiak P, Baker A, Hansen R L, Ozonoff S, Hertz-Picciotto I. Preeclampsia, placental insufficiency, and autism spectrum disorder or developmental delay. JAMA Pediatr. 2015;169(02):154–162. doi: 10.1001/jamapediatrics.2014.2645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mann J R, McDermott S, Bao H, Hardin J, Gregg A. Pre-eclampsia, birth weight, and autism spectrum disorders. J Autism Dev Disord. 2010;40(05):548–554. doi: 10.1007/s10803-009-0903-4. [DOI] [PubMed] [Google Scholar]
- 67.Burstyn I, Sithole F, Zwaigenbaum L. Autism spectrum disorders, maternal characteristics and obstetric complications among singletons born in Alberta, Canada. Chronic Dis Can. 2010;30(04):125–134. [PubMed] [Google Scholar]
- 68.Buchmayer S, Johansson S, Johansson A, Hultman C M, Sparén P, Cnattingius S. Can association between preterm birth and autism be explained by maternal or neonatal morbidity? Pediatrics. 2009;124(05):e817–e825. doi: 10.1542/peds.2008-3582. [DOI] [PubMed] [Google Scholar]
- 69.Silva D, Colvin L, Hagemann E, Bower C. Environmental risk factors by gender associated with attention-deficit/hyperactivity disorder. Pediatrics. 2014;133(01):e14–e22. doi: 10.1542/peds.2013-1434. [DOI] [PubMed] [Google Scholar]
- 70.Getahun D, Rhoads G G, Demissie K et al. In utero exposure to ischemic-hypoxic conditions and attention-deficit/hyperactivity disorder. Pediatrics. 2013;131(01):e53–e61. doi: 10.1542/peds.2012-1298. [DOI] [PubMed] [Google Scholar]
- 71.Halmøy A, Klungsøyr K, Skjærven R, Haavik J. Pre- and perinatal risk factors in adults with attention-deficit/hyperactivity disorder. Biol Psychiatry. 2012;71(05):474–481. doi: 10.1016/j.biopsych.2011.11.013. [DOI] [PubMed] [Google Scholar]
- 72.Amiri S, Malek A, Sadegfard M, Abdi S. Pregnancy-related maternal risk factors of attention-deficit hyperactivity disorder: a case-control study. ISRN Pediatr. 2012;2012:458064. doi: 10.5402/2012/458064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mann J R, McDermott S. Are maternal genitourinary infection and pre-eclampsia associated with ADHD in school-aged children? J Atten Disord. 2011;15(08):667–673. doi: 10.1177/1087054710370566. [DOI] [PubMed] [Google Scholar]
- 74.Tolsa C B, Zimine S, Warfield S K et al. Early alteration of structural and functional brain development in premature infants born with intrauterine growth restriction. Pediatr Res. 2004;56(01):132–138. doi: 10.1203/01.PDR.0000128983.54614.7E. [DOI] [PubMed] [Google Scholar]
- 75.Mallard E C, Rees S, Stringer M, Cock M L, Harding R. Effects of chronic placental insufficiency on brain development in fetal sheep. Pediatr Res. 1998;43(02):262–270. doi: 10.1203/00006450-199802000-00018. [DOI] [PubMed] [Google Scholar]
- 76.Batty M J, Liddle E B, Pitiot A et al. Cortical gray matter in attention-deficit/hyperactivity disorder: a structural magnetic resonance imaging study. J Am Acad Child Adolesc Psychiatry. 2010;49(03):229–238. doi: 10.1016/j.jaac.2009.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Carmona S, Vilarroya O, Bielsa A et al. Global and regional gray matter reductions in ADHD: a voxel-based morphometric study. Neurosci Lett. 2005;389(02):88–93. doi: 10.1016/j.neulet.2005.07.020. [DOI] [PubMed] [Google Scholar]
- 78.Miguel P M, Schuch C P, Rojas J J et al. Neonatal hypoxia-ischemia induces attention-deficit hyperactivity disorder-like behavior in rats. Behav Neurosci. 2015;129(03):309–320. doi: 10.1037/bne0000063. [DOI] [PubMed] [Google Scholar]
- 79.Curran E A, O'Keeffe G W, Looney A M et al. Exposure to hypertensive disorders of pregnancy increases the risk of autism spectrum disorder in affected offspring. Mol Neurobiol. 2018;55(07):5557–5564. doi: 10.1007/s12035-017-0794-x. [DOI] [PubMed] [Google Scholar]
- 80.Choi G B, Yim Y S, Wong Het al. The maternal interleukin-17a pathway in mice promotes autism-like phenotypes in offspring Science 2016351(6276):933–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Darmochwal-Kolarz D, Kludka-Sternik M, Tabarkiewicz J et al. The predominance of Th17 lymphocytes and decreased number and function of Treg cells in preeclampsia. J Reprod Immunol. 2012;93(02):75–81. doi: 10.1016/j.jri.2012.01.006. [DOI] [PubMed] [Google Scholar]
- 82.Wu W L, Hsiao E Y, Yan Z, Mazmanian S K, Patterson P H. The placental interleukin-6 signaling controls fetal brain development and behavior. Brain Behav Immun. 2017;62:11–23. doi: 10.1016/j.bbi.2016.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Jones K L, Croen L A, Yoshida C K et al. Autism with intellectual disability is associated with increased levels of maternal cytokines and chemokines during gestation. Mol Psychiatry. 2017;22(02):273–279. doi: 10.1038/mp.2016.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Rätsep M T, Hickman A F, Maser B et al. Impact of preeclampsia on cognitive function in the offspring. Behav Brain Res. 2016;302:175–181. doi: 10.1016/j.bbr.2016.01.030. [DOI] [PubMed] [Google Scholar]
- 85.Warshafsky C, Pudwell J, Walker M, Wen S W, Smith G N; Preeclampsia New Emerging Team.Prospective assessment of neurodevelopment in children following a pregnancy complicated by severe pre-eclampsia BMJ Open 2016607e010884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Tuovinen S, Aalto-Viljakainen T, Eriksson J G et al. Maternal hypertensive disorders during pregnancy: adaptive functioning and psychiatric and psychological problems of the older offspring. BJOG. 2014;121(12):1482–1491. doi: 10.1111/1471-0528.12753. [DOI] [PubMed] [Google Scholar]
- 87.Morsing E, Maršál K. Pre-eclampsia- an additional risk factor for cognitive impairment at school age after intrauterine growth restriction and very preterm birth. Early Hum Dev. 2014;90(02):99–101. doi: 10.1016/j.earlhumdev.2013.12.002. [DOI] [PubMed] [Google Scholar]
- 88.Griffith M I, Mann J R, McDermott S. The risk of intellectual disability in children born to mothers with preeclampsia or eclampsia with partial mediation by low birth weight. Hypertens Pregnancy. 2011;30(01):108–115. doi: 10.3109/10641955.2010.507837. [DOI] [PubMed] [Google Scholar]
- 89.Ehrenstein V, Rothman K J, Pedersen L, Hatch E E, Sørensen H T. Pregnancy-associated hypertensive disorders and adult cognitive function among Danish conscripts. Am J Epidemiol. 2009;170(08):1025–1031. doi: 10.1093/aje/kwp223. [DOI] [PubMed] [Google Scholar]
- 90.Liu X, Zhao W, Liu H et al. Developmental and functional brain impairment in offspring from preeclampsia-like rats. Mol Neurobiol. 2016;53(02):1009–1019. doi: 10.1007/s12035-014-9060-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Akande V O, Hendriks A M, Ruiter R A, Kremers S P. Determinants of dietary behavior and physical activity among Canadian Inuit: a systematic review. Int J Behav Nutr Phys Act. 2015;12:84. doi: 10.1186/s12966-015-0252-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Zhu H, Zhu W, Hu R, Wang H, Ma D, Li X. The effect of pre-eclampsia-like syndrome induced by L-NAME on learning and memory and hippocampal glucocorticoid receptor expression: A rat model. Hypertens Pregnancy. 2017;36(01):36–43. doi: 10.1080/10641955.2016.1228957. [DOI] [PubMed] [Google Scholar]
- 93.Nyaradi A, Li J, Hickling S, Foster J, Oddy W H. The role of nutrition in children's neurocognitive development, from pregnancy through childhood. Front Hum Neurosci. 2013;7:97. doi: 10.3389/fnhum.2013.00097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Rathod R S, Khaire A A, Kale A A, Joshi S R. Beneficial effects of omega-3 fatty acids and vitamin B12 supplementation on brain docosahexaenoic acid, brain derived neurotrophic factor, and cognitive performance in the second-generation Wistar rats. Biofactors. 2015;41(04):261–272. doi: 10.1002/biof.1222. [DOI] [PubMed] [Google Scholar]
- 95.Sharma S, Zhuang Y, Gomez-Pinilla F. High-fat diet transition reduces brain DHA levels associated with altered brain plasticity and behaviour. Sci Rep. 2012;2:431. doi: 10.1038/srep00431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Wadhwani N S, Narang A S, Mehendale S S, Wagh G N, Gupte S A, Joshi S R. Reduced maternal erythrocyte long chain polyunsaturated fatty acids exist in early pregnancy in preeclampsia. Lipids. 2016;51(01):85–94. doi: 10.1007/s11745-015-4098-5. [DOI] [PubMed] [Google Scholar]
- 97.Kemse N, Kale A, Chavan-Gautam P, Joshi S. Increased intake of vitamin B 12 , folate, and omega-3 fatty acids to improve cognitive performance in offspring born to rats with induced hypertension during pregnancy . Food Funct. 2018;9(07):3872–3883. doi: 10.1039/c8fo00467f. [DOI] [PubMed] [Google Scholar]
- 98.Rätsep M T, Paolozza A, Hickman A F et al. Brain structural and vascular anatomy is altered in offspring of pre-eclamptic pregnancies: a pilot study. AJNR Am J Neuroradiol. 2016;37(05):939–945. doi: 10.3174/ajnr.A4640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Carmeliet P, Ferreira V, Breier Get al. Abnormal blood vessel development and lethality in embryos lacking a single VEGF allele Nature 1996380(6573):435–439. [DOI] [PubMed] [Google Scholar]
- 100.Aasa K L, Zavan B, Luna R L et al. Placental growth factor influences maternal cardiovascular adaptation to pregnancy in mice. Biol Reprod. 2015;92(02):44. doi: 10.1095/biolreprod.114.124677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Vrachnis N, Kalampokas E, Sifakis S et al. Placental growth factor (PlGF): a key to optimizing fetal growth. J Matern Fetal Neonatal Med. 2013;26(10):995–1002. doi: 10.3109/14767058.2013.766694. [DOI] [PubMed] [Google Scholar]
- 102.Powers R W, Roberts J M, Plymire D A et al. Low placental growth factor across pregnancy identifies a subset of women with preterm preeclampsia: type 1 versus type 2 preeclampsia? Hypertension. 2012;60(01):239–246. doi: 10.1161/HYPERTENSIONAHA.112.191213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Rätsep M T, Carmeliet P, Adams M A, Croy B A. Impact of placental growth factor deficiency on early mouse implant site angiogenesis. Placenta. 2014;35(09):772–775. doi: 10.1016/j.placenta.2014.07.006. [DOI] [PubMed] [Google Scholar]
- 104.Chaballe L, Close P, Sempels M et al. Involvement of placental growth factor in Wallerian degeneration. Glia. 2011;59(03):379–396. doi: 10.1002/glia.21108. [DOI] [PubMed] [Google Scholar]
- 105.Luna R L, Kay V R, Rätsep M T et al. Placental growth factor deficiency is associated with impaired cerebral vascular development in mice. Mol Hum Reprod. 2016;22(02):130–142. doi: 10.1093/molehr/gav069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Dang F, Croy B A, Stroman P W, Figueiró-Filho E A. Impacts of preeclampsia on the brain of the offspring. Rev Bras Ginecol Obstet. 2016;38(08):416–422. doi: 10.1055/s-0036-1584515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Tuovinen S, Räikkönen K, Kajantie E et al. Depressive symptoms in adulthood and intrauterine exposure to pre-eclampsia: the Helsinki Birth Cohort Study. BJOG. 2010;117(10):1236–1242. doi: 10.1111/j.1471-0528.2010.02634.x. [DOI] [PubMed] [Google Scholar]
- 108.Eide M G, Moster D, Irgens L M et al. Degree of fetal growth restriction associated with schizophrenia risk in a national cohort. Psychol Med. 2013;43(10):2057–2066. doi: 10.1017/S003329171200267X. [DOI] [PubMed] [Google Scholar]
- 109.Kajantie E, Dunkel L, Turpeinen U et al. Placental 11 beta-hydroxysteroid dehydrogenase-2 and fetal cortisol/cortisone shuttle in small preterm infants. J Clin Endocrinol Metab. 2003;88(01):493–500. doi: 10.1210/jc.2002-021378. [DOI] [PubMed] [Google Scholar]
- 110.Brown E S, Varghese F P, McEwen B S. Association of depression with medical illness: does cortisol play a role? Biol Psychiatry. 2004;55(01):1–9. doi: 10.1016/s0006-3223(03)00473-6. [DOI] [PubMed] [Google Scholar]


