Abstract
Objective:
To assess the impact of a multi-level nutrition intervention for low-income childcare environments, staff, and center-enrolled children.
Design:
Cluster-randomized controlled trial was conducted among eligible centers. Staff and parent self-report surveys and objective field observations at baseline/follow-up were conducted.
Setting:
22 low-income childcare centers (enrolling ≥25, 2–5- year-old children).
Participants:
Children between 18–71-months-old; 408 children and 97 staff were randomized into intervention (208 children, 50 staff) and waitlist-control groups (200 children, 45 staff). Retention rates were high (87%-children, 93%-staff).
Intervention(s):
A 6-session, 6-month director’s child nutrition course with on-site technical support for center teachers.
Main Outcome Measure(s):
Center nutrition/physical activity environment; staff feeding styles, dietary patterns, and attitudes about food; child food preferences and dietary patterns.
Analysis:
Covariance regression analyses to assess the intervention effect, adjusting for clustering within centers.
Results:
Significant intervention effects found for the center nutrition training/education environment (B=3.01, p=0.03), nutrition total scores (B=1.29, p=0.04), and staff-level prompting/encouraging feeding styles (B=0.38, p=0.04). No significant intervention effects for child-level measures.
Conclusions and Implications:
Curriculum-driven training and implementation support improved nutritional policies/practices and staff-child interactions during meals. Future research should extend the intervention to families and the evaluation to children’s dietary behaviors and weight changes.
Keywords: obesity, health promotion, childcare center, low-income, intervention
Pediatric obesity is a major health concern that often begins early in life and increases risk for lifelong obesity and associated comorbidities,1 including hypertension, asthma, musculoskeletal problems, obstructive sleep disorders, Type II diabetes, depression, and social stigmatization. Based on national 2015–2016 data from NHANES, 26% of 2–5 year-olds are overweight or obese, with elevated rates among children from minority and low-income families.2
Overweight by age 5 increases the risk for obesity by age 14 fourfold,3 suggesting that obesity prevention should focus on early life behavioral patterns. Health policy recommendations are to implement multilevel, rather than single level, strategies early in life,4 making childcare centers an ideal setting for pediatric obesity prevention.5 With their dependency and sensitivity, young children are uniquely influenced by their proximal environments,6 including adults at home and in childcare settings.6,7 More than 63% of 3–5-year-old children are in full-time nonparental care8 and eat at least one to two meals and several snacks, estimated to encompass 50–100% of their Recommended Dietary Allowance.9
With the exception of Head Start, a federal program, childcare programs are primarily state-licensed and regulated. Wellness guidelines for childcare centers are emerging. The Healthy Hunger Free Kids Act of 2010 (HHFKA) focuses on health promotion guidelines for schools, including foods served and wellness policy implementation, and acknowledges the importance of such policies in childcare centers.10 The Academy of Nutrition and Dietetics provides benchmarks for nutrition in childcare centers11 and the United States Department of Agriculture (USDA) Child and Adult Care Food Program (CACFP) provides reimbursement for 3.2 million preschool children daily based on meal pattern requirements that are consistent with the Dietary Guidelines for Americans.12 Under the HHFKA, the USDA is tasked to update meal patterns and nutritional standards in CACFP meals/snacks to align with Dietary Guidelines for Americans.10 Recent CACFP guidelines (October 2017) increase the provision of fruits/vegetables and reduce desserts with grains/sugar in childcare.13 An evaluation of 118 childcare providers in 24 centers in Illinois found that Head Start providers were more likely to adhere to nutritional guidelines than CACFP and non-CACFP providers, likely due to nutrition performance standards and training in Head Start centers.14
In collaboration with the state educational agency and a non-profit agency serving childcare centers, this pilot project examines the impact of a six-month intervention that combined training for childcare center directors on nutritional guidelines with a nutrition education curriculum. It is hypothesized that the intervention would positively impact childcare center nutrition policies and practices, staff nutritional attitudes/behaviors, and child food preferences.
METHODS
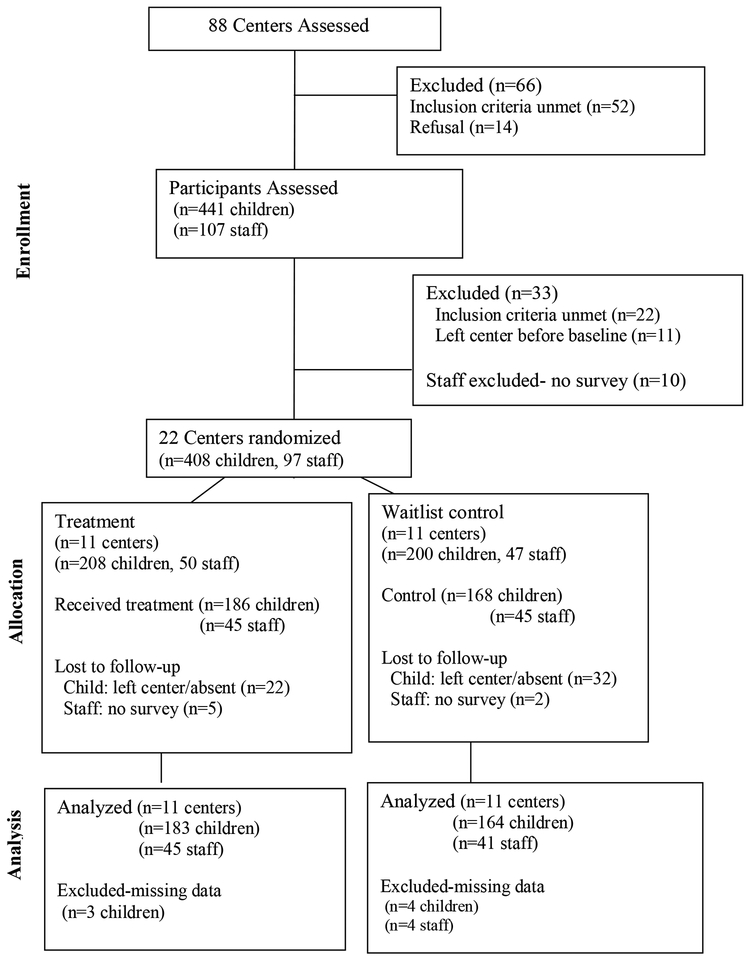
This randomized controlled trial included CACFP-participating childcare centers in three Maryland counties. Eligible centers had at least 25 enrolled children ages 2–5 years and lunch provision. Exclusion criteria were corrective action in the past year or being a Y of Maryland center (due to prior nutrition training). Of 88 screened childcare centers, 36 met eligibility criteria, and 22 agreed to participate (Figure 1). Centers were matched into pairs by size and county. Using a computer-based randomization procedure, one center in each pair was assigned to intervention (n=11) and waitlist-control (n=11).
Figure 1.
Building Blocks Study Design and Sample Selection
Participants
Parents, children, and staff were recruited and completed enrollment assessments prior to randomization. Parents and children were eligible if the child’s age was between 3–5 years and received lunch at the center. Staff were excluded if they had a child enrolled in the trial. The enrollment sample included 408 children (intervention n=208, control n=200) and 381 parents who returned baseline surveys (intervention n=198, control n=183). A total of 97 staff members (intervention n=50, control n=47) were included. The follow-up evaluation was conducted six months following enrollment upon conclusion of the intervention, and included 354 children (86.8% retention: intervention n=186, control n=168) and 90 staff (92.8% retention: intervention n=45, control n=45).
Procedures
The protocol was approved by the university institutional review board. Written informed consent was obtained from all participating parents and staff. Research assistants recruited parents/children and staff at centers during back-to-school nights and drop-off/pick-up times at the start of the academic year (Fall 2014). The multi-level baseline evaluation included observations of center nutrition and physical activity (PA) environments, staff, and parent surveys assessed at baseline and follow-up.
Intervention.
Built on the social ecology behavior change theory and through a collaborative process under the leadership of the state education agency, a training course was developed for center directors/management (Enhancing the Nutrition Environment of Your Child Care Center) on nutrition-promoting activities in childcare centers and a food-based classroom nutrition education curriculum (Maryland’s Building Blocks for Healthy Kids Nutrition Education Toolkit) focusing on children’s acceptance of fruits, vegetables, and whole grains. Lessons were developed by Registered Dietitians from the Blinded for Review (XXX) and using existing Early Care and Education (ECE) nutrition education resources. Weekly classroom lessons and activities focused on shaping positive food preferences and eating habits among preschoolers, specific to fruits, vegetables, and whole grains following the Dietary Guidelines for Americans (Dietary Guidelines),15 the meal pattern revisions that were subsequently incorporated into the Final Rule for CACFP, and recommended CACFP best practices.16
Nutrition trainers administered the nutrition environment curriculum to childcare directors/management at local resource centers for six, three-hour training sessions over six months. Training topics included: (1) Nutrition and PA guidelines/recommendations, (2) Menu planning and food purchasing, (3) Mealtime environment, family style dining, choosy eaters, (4) Partnerships with parents/caregivers, (5) Education for children, staff, and parents/caregivers, and (6) Development and implementation of wellness policies. For the classroom nutrition education curriculum, trained staff provided a monthly nutrition education lesson for children and left 3 additional lessons with accompanying materials (books, activities, etc.) with the classroom teacher to be taught independently over a 3-week period. Both the environment and classroom curricula were administered over a period of six months. Childcare centers received funding ($1,500-$2,400 based on center size) to support curriculum-based activities.
Measures
Center-level measure
Nutrition and PA environment.
Environment and Policy Assessment and Observation (EPAO).
The EPAO17 includes two domains: nutrition and PA, each with eight subscales. Trained field observers conducted observations and document reviews in non-participating childcare centers until achieving inter-rater reliability of 85%. Scores are summed for each subscale and range from 0–20, with higher scores indicating a better-quality nutrition or PA environment.
Staff-level measures
Food attitudes.
The Food-Life Questionnaire, Short Form (FLQ-SF) addressed childcare staff food beliefs and attitudes.18 Three of the five FLQ-SF subscales were included (weight concern, diet-health orientation, belief in a diet-health linkage). The natural food preferences subscale was removed due to lack of relevance and the food and pleasure subscale was removed due to poor reliability (α < .6). Response options ranged from 1-strongly disagree to 5-strongly agree and were summed for each subscale. The FLQ-SF has adequate internal consistency (α=.75), moderate associations with food choice (r=.32–.64) and strong correlations with the original Food-Life Questionnaire (r=.64–.84).18 As per recommendations,19 Cronbach’s α was acceptable at baseline and follow-up for weight concern (α = .7) and belief in a diet-health linkage (α = .7) on average. Cronbach’s α values were questionable for diet-health orientation (α = .6) after removing the item “I rarely think about the long-term effects of my diet on health” to improve internal reliability.
Feeding Styles.
Childcare staff feeding style was assessed with the Parent Feeding Styles Questionnaire,20 referred to in this study as the Caregiver Feeding Styles Questionnaire (CFSQ). The CFSQ was adapted by adding an option of 0-not applicable and referencing “children at your center” instead of “your child.” The CFSQ includes 27 items and 4 subscales: control feeding, emotional feeding, instrumental feeding, and prompting/encouraging feeding. Staff members rated items from 1-never to 5-almost always. Scores were averaged for each subscale. Internal consistency was above .8 at baseline and follow-up.
Diet.
Diet was assessed using “Starting the Conversation,” an 8-item survey designed to assess eating behavior (e.g., frequency of fruits/vegetables).18 This survey is cross-validated, meaning that it detects diet change over time.21 Staff indicated the frequency of weekly consumption of each food type (≥4 times, 1–3 times, <1 time); total scores were averaged with higher scores indicating less healthful dietary practices. Cronbach’s α was acceptable19 at baseline (α = .7) and follow-up (α =.7).
Demographics.
Staff race/ethnicity, education, and childcare center position were collected via self-administered survey.
Child-level Measures
Anthropometry.
Shoes and heavy outer-clothing were removed prior to measurement. Children were weighed on a calibrated digital scale to the nearest 0.1 kg (Seca, Birmingham, UK) and height was measured using a portable stadiometer (Schorr Board) rounded to the nearest 0.1 cm following standard protocol.22 Measurements were taken three times and averaged. Gender-specific weight-for-age, height-for-age, and body mass index (BMI)-for-age z-scores were calculated according to WHO standards.23 Anthropometry data were collected at baseline only.
Fruit/Vegetable Preference (FVP).
FVP was collected using the Food Preference Computer Assessment.24 This measure has high reliability and predictive validity.24 FVP includes pictures of 15 fruits and 11 vegetables. Following each picture, children point to a “yummy,” “OK,” or “yucky,” face (score=2, 1, 0, respectively). Scores were averaged for fruits, vegetables, and total FVP.
Food consumption/waste.
Lunchtime meal observations were conducted using a real-time visualization method that is reliable and valid against individual item weighing.25 Researchers estimated the amount of each primary food group (protein, fruit, vegetable, grains) remaining on the child’s plate using the quarter-waste method (none, ¼, ½, ¾, or all of food item wasted) and a “gold standard” plate for comparison. Inter-rater reliability was high (kappa>0.90). Grains were removed from analysis due to low reliability. Food waste was recoded into none vs. some/all waste in the analyses.
Demographics.
Parent surveys were administered to collect parent and child demographics: race/ethnicity, parental education, parent BMI (kg/m2; <25=normal weight, ≥25=overweight/obese, based on self-reported weight and height), and poverty ratio (based on family size and income, calculated using federal poverty guidelines).
Analysis
In SAS 9.3, descriptive analyses compared center, staff, and child characteristics by intervention status using Student t tests and chi-square test of independence analyses. To assess the intervention effect on center-level measures (EPAO nutrition and physical activity scales and subscales), covariance linear regression analyses for continuous variables were conducted to assess the difference in follow-up scores between intervention and control groups (intervention effect), adjusting for baseline scores. To assess the intervention effect on the staff-level and child-level measures, multi-level covariance linear regression analyses (continuous variables) and covariance logistic regression analyses (categorical variables, e.g. plate waste) were conducted. The dependent variable is the measure for the staff (e.g. staff food attitude) or child (e.g. child food consumption/waste) at follow up and the predictor is intervention status, adjusting for the same measure at baseline. Multi-level modeling was conducted to account for the clustering of staff or children (level 1) within the centers (level 2). For staff-level or child-level measures, the intraclass correlation coefficients (ICC) were assessed to indicate the correlations between staff members or children within the same centers.
RESULTS
Sample Characteristics
Children were approximately 46 months at baseline (n=347; Table 1) and primarily African American. Overall 24.3% of intervention and 29.9% of control group children were overweight or obese (p=.27). All participating staff (n=86) were female; most had formal Early Childhood Education training (97.6%) and were employed full-time (92.0%). Seventy-three percent of staff (teachers/directors) worked directly with children.
Table 1.
Sample Characteristics
| Child | Control (n=164) | Intervention (n=183) | T /χ2 |
|---|---|---|---|
| Age (months)a | 46.3 (24.8–70.6) | 47.2 (29.4–70.6) | −0.812 |
| Race | 12.572* | ||
| Black | 78.7% | 93.8% | |
| Otherb | 21.3% | 6.2% | |
| Gender | 0.437 | ||
| Male | 51.9% | 49.3% | |
| Female | 48.1% | 50.3% | |
| BMI z-score | 0.51 (−2.86–6.55) | 0.35 (−2.36–3.35) | 0.17 |
| BMI percentile | 0.486 | ||
| <85th | 70.1% | 75.7% | |
| 85th–95th | 17.8% | 15.3% | |
| >95th | 12.1% | 9.0% | |
| Parent | Control (n=109) | Intervention (n=104) | |
| Gender | 0.395 | ||
| Male | 7.6% | 6.3% | |
| Female | 92.4% | 93.8% | |
| Education | 15.402** | ||
| ≤High school | 24.6% | 20.7% | |
| >High school | 75.4% | 79.3% | |
| BMI | 28.6 (19.8–51.8) | 29.8 (19.4–62.7) | −1.214 |
| Overweight/Obese | 62.5% | 70.2% | |
| Poverty line ≤100% | 37.1% | 19.8% | −4.068*** |
| Staff | Control (n=41) | Intervention (n=45) | |
| Race | 8.653 | ||
| Black | 87.8% | 97.9% | |
| Other | 12.2% | 2.2% | |
| Education | 4.342 | ||
| ≤High school | 32.5% | 18.6% | |
| >High school | 67.5% | 81.4% | |
| Center role | 11.673 | ||
| Teacher | 23 (56.1%) | 31 (67.4%) | |
| Director | 7 (17.1%) | 6 (13.0%) | |
| Owner | 2 (4.9%) | 2 (4.3%) | |
| Other | 9 (22.0%) | 6 (13.3%) |
p<.05,
p<.01,
p<.001
Note: Student t tests and chi-square test of independence analyses test differences by intervention status.
Age/BMI z-score (Body Mass Index) are means and range; all other data are percentages
“Other” race/ethnicity: Caucasian, Hispanic/Latino, other
Center-level Intervention Effect
A significant intervention effect was found for nutrition training and education and for total nutrition (Table 2). Nutrition training and education scores increased for intervention centers by 3.01 more units compared to the control group (B=3.01, SE=1.26, p=0.03), adjusted for baseline scores. Total nutrition scores increased for intervention group centers compared to control centers, with an intervention effect of 1.29 units (B=1.29, SE=0.57, p=0.04). There was an unexpected intervention effect on the sedentary environment; scores increased by 3.91 units for the control group compared to the intervention group (B=−3.91, SE=1.73, p=0.04) due to little change in sedentary environment scores from baseline (5.45) to follow-up (4.85) for intervention centers, but an increase for control centers (baseline: 6.06, follow-up: 9.09).
Table 2.
Center Intervention Effects for the Environment and Policy Assessment and Observation
| Control (n=11) | Intervention (n=11) | ||||
|---|---|---|---|---|---|
| Baseline | Follow up | Baseline | Follow-up | B(SE) | |
| Nutrition | |||||
| Total | 10.01 (1.59) |
10.04 (1.57) |
8.98 (0.60) |
10.67 (1.25) |
1.29 (0.57)* |
| Fruits/Vegetables | 12.39 (2.17) |
12.64 (2.01) |
11.36 (2.06) |
12.82 (2.71) |
0.65 (0.99) |
| Whole Grains/Low Fat Meats | 10.76 (3.19) |
10.00 (3.16) |
8.48 (3.20) |
10.61 (3.96) |
1.06(1.65) |
| High Sugar/High Fat Foods | 13.82 (2.40) |
15.00 (2.97) |
13.55 (2.16) |
14.45 (1.57) |
−0.32 (0.63) |
| Beverages | 11.82 (1.41) |
12.23 (2.80) |
11.24 (1.74) |
12.64 (2.17) |
0.44(1.11) |
| Nutrition Environment | 8.79 (6.01) |
9.70 (4.58) |
7.27 (2.01) |
10.30 (5.47) |
1.42(1.97) |
| Staff Behaviors- Nutrition | 14.39 (2.39) |
13.18 (4.56) |
13.64 (3.15) |
13.48 (3.98) |
0.62(1.82) |
| Nutrition Training/Education | 4.36 (4.18) |
2.18 (2.75) |
2.18 (2.75) |
4.36 (3.32) |
3.01 (1.26)* |
| Nutrition Policy | 3.73 (4.36) |
5.36 (2.85) |
3.96 (4.37) |
5.21 (3.45) |
−0.17 (1.48) |
| Physical Activity | |||||
| Total | 9.71 (2.70) |
10.78 (0.99) |
8.73 (2.28) |
9.53 (1.80) |
−0.98 (0.57) |
| Active Time | 9.32 (3.72) |
9.55 (4.45) |
6.14 (4.09) |
10.68 (3.37) |
0.56(1.85) |
| Sedentary Behaviors | 14.55 (5.01) |
12.73 (4.43) |
12.73 (5.54) |
13.33 (4.94) |
1.36(1.85) |
| Sedentary Environment | 6.06 (4.67) |
9.09 (4.49) |
5.45 (5.83) |
4.85 (5.24) |
−3.91 (1.73)* |
| Fixed Play Environment | 9.20 (4.96) | 8.46 (3.92) |
8.89 (2.56) |
9.38 (4.07) |
1.10 (1.48) |
| Portable Play Environment | 13.25 (7.48) |
17.14 (2.21) |
15.06 (4.06) |
13.77 (5.69) |
−3.55 (1.89) |
| Staff Behaviors-Physical Activity | 16.97 (4.58) |
11.82 (5.65) |
13.94 (6.64) |
10.91 (6.68) |
0.59 (2.50) |
| Physical Activity Training/Education | 2.00 (3.22) |
2.73 (3.13) |
2.18 (3.28) |
0.73 (1.62) |
−2.02 (1.08) |
| Physical Activity Policy | 8.33 (9.83) |
18.33 (4.08) |
4.00 (8.94) |
16.00 (5.48) |
−1.45 (2.88) |
| Physical Activity Total | 9.71 (2.70) |
10.78 (0.99) |
8.73 (2.28) |
9.53 (1.80) |
−0.98 (0.57) |
p<.05
Note: Covariance regression analyses were used to assess differences in follow-up scores between intervention and control groups (intervention effect), adjusting for baseline scores. Separate regression analyses were conducted for each Nutrition and Physical Activity scale and subscale of the Environment and Policy Assessment and Observation (EPAO).
Staff-level Intervention Effects
The ICCs between staff within the same center were small for FLQ-SF subscales (weight concern = 0, diet-health orientation = 0.05, belief in diet-health linkage = 0) and Starting the Conversation = 0. ICCs for CFSQ subscales were as follows: controlling = 0.15, emotional = 0.02, instrumental = 0.07 for instrumental, prompting/encouraging = 0. There were no significant intervention effects among staff measures. Analyses were then restricted to staff working directly with children (teachers, directors). There was a significant intervention effect for Prompting/Encouraging Feeding Style (CFSQ subscale; see Table 3). Control group scores were similar between baseline and follow-up, while the intervention group increased from 4.06 to 4.30 points, 0.38 more units compared to the control group (B=0.38, SE=0.18, p=0.04).
Table 3.
Staff Intervention Effects M(SD)
| Control (n=30) | Intervention (n=36) | ||||
|---|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | B(SE) | |
| Food-Life Questionnaire-Short Form | |||||
| Weight Concern | 15.69 (4.99) | 16.19 (2.83) |
16.38 (5.37) |
16.69 (5.10) | 0.10 (0.80) |
| Diet-Health Orientation | 13.15 (2.56) | 12.31(3.16) | 11.81(3.02) | 11.77 (3.06) | −0.13 (0.90) |
| Belief in Diet-Health Linkage | 15.65 (3.58) | 15.81 (3.78) |
15.27 (3.58) |
16.00 (2.95) | 0.33 (0.88) |
| Caregiver Feeding Styles Questionnaire | |||||
| Controlling | 3.36 (1.26) | 3.29 (1.17) | 3.31 (0.98) | 3.39 (0.93) | 0.05 (0.25) |
| Emotional | 1.05 (0.54) | 1.01 (0.26) | 1.08 (0.49) | 1.28 (0.72) | 0.25 (0.14) |
| Instrumental | 1.11 (0.46) | 1.15 (0.43) | 1.30 (0.60) | 1.31 (0.70) | 0.08 (0.16) |
| Prompting/Encouraging | 3.95 (0.84) | 3.86 (0.92) | 4.06 (0.86) | 4.30 (0.62) | 0.38 (0.18)* |
| Starting the Conversation | 8.15 (2.58) | 8.04 (2.68) | 8.89 (3.15) | 8.14 (3.81) | −0.43 (0.70) |
p<.05
Note: Multi-level covariance regression analyses were conducted to assess the difference in follow-up scores between intervention and control groups (intervention effect), adjusting for baseline scores and accounting for clustering of staff members within centers (level 2). Analyses were restricted to staff working directly with children. Separate regression analyses were conducted for each subscale of the Food-Life Questionnaire-Short Form and Caregiver Feeding Styles Questionnaire and for the Starting the Conversation scale.
Child-level Intervention Effects
The ICCs for FVP between children within the same center were small (vegetable preference = 0, fruit preference = 0.01, fruit/vegetable total = 0.005). The ICC for food consumption/waste was 0.63 for protein, and 0.15 for fruit and vegetable consumption. There was no significant intervention effect on either FVP or food waste (Table 4). FVP was examined for each food-item preference, overall score, and fruit/vegetable subscale score, with no intervention effects found. Food waste was examined both as a continuous variable and categorical score (none/some wasted vs. all wasted) with no significant intervention effects.
Table 4.
Child Intervention Effects M(SD)
| Control | Intervention | ||||
|---|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | B(SE) | |
| Plate Wastea | |||||
| Protein (n= 100) | 13 (31) | 18 (43) | 18 (43) | 29 (50) | −0.10 (1.66) |
| Fruit (n=l98) | 51 (45) | 37 (33) | 26 (31) | 17 (20) | −0.54 (0.51) |
| Vegetables (n=154) | 45 (65) | 35 (51) | 49 (58) | 40 (47) | −0.01 (0.52) |
| Fruit and Vegetable Preference (FVP) | |||||
| Fruit (n=244) | 1.40(0.48) | 0.44(0.27) | 1.38(0.41) | 1.41(0.38) | 0.01(0.06) |
| Vegetables (n=234) | 1.24(0.53) | 1.20(0.47) | 1.17(0.47) | 1.20(0.49) | 0.02(0.06) |
| Fruit or vegetables total (n=234) | 1.31(0.47) | 1.29(0.40) | 1.26(0.39) | 0.40(0.42) | 0.01(0.05) |
p<.05
Note: Multi-level covariance linear regression analyses (FVP continuous variables) and covariance logistic regression analyses (plate waste categorical variables) were conducted to assess the difference in follow-up scores between intervention and control groups (intervention effect), adjusting for baseline scores, and accounting for clustering of children in the centers. Separate analyses were conducted for protein, fruit, and vegetable categories of plate waste, and for fruit, vegetable, and total scores on the Fruit and Vegetable Preference measure.
Percentage of any waste vs. no waste
DISCUSSION
Prior research on interventions to improve the nutrition and PA environments in early childcare settings is equivocal.5,17,26,27 Results of this pilot study show promising effects for a multilevel obesity prevention intervention in low-income childcare settings at the center and staff levels. Intervention centers improved their nutrition training and education practices, as well as their overall nutrition environment. Nutrition training and education practices included actively involving children in nutrition-related lessons (e.g., using book characters to assess food choices, preparing healthy snacks, and nutrition-focused art activities) and training childcare directors and staff on developing and documenting nutrition curricula.
The improvement in center-level nutrition environments was driven in part by increases in formalized nutrition training and education and in having formal nutrition and wellness-related policies. The intervention provided education, curriculum, and resource materials for directors and staff to engage in wellness activities, suggesting that many of the intervention centers implemented observable changes. Long-term follow-up is necessary to assess whether improvements to the nutrition environment continued after technical assistance ended. Other research on childcare center environmental interventions,17 particularly those offering external training and technical assistance to center staff28 and focusing on policies and practices29 have shown promise for nutrition behavior improvements among children. It is unsurprising that intervention centers did not demonstrate improvements in any physical activity domains of the EPAO as the intervention primarily addressed nutrition.
Changes were observed in feeding behaviors of staff who directly engage with children in childcare centers, specifically increases in prompting/encouraging feeding styles. Although excessive prompting/encouraging can increase risk for obesogenic eating behaviors in childhood,20 encouraging nutritious foods can promote healthy eating for children.30,31 Future research should include observations of the nature and frequency of caregiver feeding encouragement.
There are several possible explanations for the lack of observed changes in child food waste or preferences. First, regarding the food preference measure, not all foods included were specified in the intervention and not all foods specified in the intervention were included in the measure. These results support the need for tailoring such a measure to ensure consistency with the intervention. Second, alterations in food preferences and consumption may require an intervention of longer duration, given that children can refuse unfamiliar fruits/vegetables up to 15 times before willing to try them.32 Finally, variability in foods served across centers may have differentially impacted assessments of child food waste.
Methodological Considerations
Measurement challenges related to child food waste and preference may have prevented an accurate assessment of intervention effects. Variations in the developmental stage of the child, distractions during assessments, and variability in nutrition environments across centers could have had an impact on measure reliability and validity. Validated measures of child diet and food preference are needed for children under age 5 years to ensure that they can be feasibly administered in a large-scale, childcare center-based trial. Evaluations of innovative strategies to assess food intake are emerging, although with mixed results.33,34 The internal consistency for the FLQ-SF diet-health orientation subscale was questionable. Although close to the acceptable range,19 results for this measure should be interpreted with caution and may not be valid given the small staff sample size. Including larger samples in future studies would enable the assessment of moderators, such as children’s age and weight status.
Strengths of this study include the ability to deliver and assess center-level policy and environmental changes using objective observations by trained researchers. Staff expressed a high level of buy-in, with retention rates over 90%, which was essential for implementing the child-centered nutrition curriculum and achieving recommended environmental changes. Study results suggest that interventions in early childcare settings may benefit from testing and refining multi-level interventions involving personnel at all levels, as well as children and families, and include additional follow-up assessments to determine the long-term effects of the intervention.28 Additional research is needed to identify the specific elements of multi-level, multi-component interventions with the strongest impact on improving nutrition and PA outcomes.27,28
Implications for Research and Practice
There were several lessons learned during this pilot study. First, the priorities of directors varied across centers, which often meant prioritizing staff management, addressing child and parent needs, and other administrative duties with constrained time and financial resources. Directors also faced external barriers to fully participate in intervention components targeting menu planning and food purchasing as some did not have the authority to alter contracts with food vendors or negotiate menu changes. Infrastructure presented as a barrier in some centers as kitchen and food service space varied widely. Some had limited space to store fresh food items or had minimal meal preparation time. Other external barriers included limitations in center budgets for meal planning as well as CACFP meal requirements and reimbursement rates. This is consistent with barriers to obesity prevention in early childcare settings that have been previously identified (e.g., cost of healthier foods, limited time/resources, limited resources for health literacy within centers, and for parental engagement).35 Although this pilot study addresses several known barriers, results suggest that providing technical support and menu planning/nutrition environment recommendations better aligned with individual center resources and infrastructure may be beneficial for future intervention development.
This pilot study shows initial promise for improving childcare center nutrition environments with a multi-level intervention that includes education and training for center administrative staff, as well as hands-on nutrition education activities for center staff and children at CACFP-participating childcare centers. As demonstrated by this pilot, improvements in nutrition environments can be successfully supported and evaluated via collaborations with state and local agencies.5,26 These results suggest benefits of targeting early childhood education settings, particularly aspects of the nutrition environment, wellness policies that support healthy diets and adhere to national dietary recommendations,12 aspects of PA, such as structured and unstructured play, and reducing length and frequency of time spent in sedentary activities. Results also suggest support for ongoing professional development opportunities provided to center staff and administration to implement health promotion activities.
Early childhood education environments remain an ideal setting to target obesity prevention efforts. Given the limited number of methodologically rigorous intervention studies involving preschoolers,36 the unrelenting national trends of overweight and obesity,2 and the disproportionate impact of obesity on health disparities among lower-income, racially and ethnically diverse communities,26 additional research is needed on obesity prevention childcare centers.
Acknowledgements:
Funded in part by the USDA 2013 Team Nutrition Training Grant CFDA # 10.574, and University of Maryland’s contributions were partly funded by the National Institute of Diabetes and Digestive and Kidney Diseases R01 DK107761. We thank the Maryland State Department of Education’s Office of School and Community Nutrition Programs, the Maryland Family Network, and the Building Blocks team.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307(5):483–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Skinner AC, Ravanbakht SN, Skelton JA, Perrin EM, Armstrong SC. Prevalence of obesity and severe obesity in US children, 1999–2016. Pediatrics. 2018;141(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cunningham SA, Kramer MR, Narayan KV. Incidence of childhood obesity in the United States. New England Journal of Medicine. 2014;370(5):403–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Black MM, Hager ER. Commentary: Pediatric obesity: Systems science strategies for prevention. Journal of Pediatric Psychology. 2013;38(9):1044–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buscemi J, Kanwischer K, Becker AB, Ward DS, Fitzgibbon ML, Committee SoBMHP. Society of Behavioral Medicine position statement: early care and education (ECE) policies can impact obesity prevention among preschool-aged children. Translational Behavioral Medicine. 2014;5(1):122–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ochoa A, Berge JM. Home environmental influences on childhood obesity in the Latino population: a decade review of literature. Journal of Immigrant and Minority Health. 2017;19(2):430–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lanigan JD. The relationship between practices and child care providers’ beliefs related to child feeding and obesity prevention. Journal of Nutrition Education and Behavior. 2012;44(6):521–529. [DOI] [PubMed] [Google Scholar]
- 8.National Center for Education Statistics. Enrollment of 3-, 4-, and 5-year-old children in preprimary programs, by age of child, level of program, control of program, and attendance status: Selected years, 1970 through 2015. 2016; https://nces.ed.gov/programs/digest/d16/tables/dt16_202.10.asp?current=yes. Accessed April 4, 2019. [Google Scholar]
- 9.US Department of Health Human Services. 2015–2020 Dietary guidelines for Americans. Washington (DC: ): USDA; 2015. [Google Scholar]
- 10.Healthy Hunger-Free Kids Act, Pub L No 111–296, §124 Sta 3183 (2010).
- 11.Neelon SEB, Briley ME. Position of the American Dietetic Association: Benchmarks for nutrition in child care. Journal of the American Dietetic Association. 2011;111(4):607–615. [DOI] [PubMed] [Google Scholar]
- 12.USDA Food and Nutrition Service. Child and Adult Care Food Program: Meal Pattern Revisions Related to the Healthy, Hunger-Free Kids Act of 2010. In: Service FaN, ed. 2015–00446 Vol 80 FR 20372015:24. [PubMed] [Google Scholar]
- 13.Food USDA and Service Nutrition. Child and Adult Care Food Program (CACFP). 2017; https://www.fns.usda.gov/cacfp/child-and-adult-care-food-program. Accessed April 4, 2019. [Google Scholar]
- 14.Dev DA, McBride BA, Harrison K, et al. Academy of nutrition and dietetics benchmarks for nutrition in child care 2011: are child-care providers across contexts meeting recommendations? Journal of the Academy of Nutrition and Dietetics. 2013;113(10):1346–1353. [DOI] [PubMed] [Google Scholar]
- 15.US Department of Agriculture and US Department of Health and Human Services. Dietary Guidelines for Americans, 2010. In. 7 ed. Washington, DC: Government Printing Office; 2010. [Google Scholar]
- 16.United States Department of Agriculture. Updated Child and Adult Care Food Program Meal Patterns: Child and Adult Meals In: Program CaACF, ed. Washington, DC: United States Department of Agriculture; n.d. [Google Scholar]
- 17.Ward D, Hales D, Haverly K, et al. An instrument to assess the obesogenic environment of child care centers. American Journal of Health Behavior. 2008;32(4):380–386. [DOI] [PubMed] [Google Scholar]
- 18.Sharp G, Hutchinson AD, Prichard I, Wilson C. Validity and reliability of the Food-Life Questionnaire. Short form. Appetite. 2013;70:112–118. [DOI] [PubMed] [Google Scholar]
- 19.George DM, Mallery YP(2003). SPSS for Windows step by step: A Simple Guide and Reference. 11.0 Update. In: Boston: Allyn & Bacon. [Google Scholar]
- 20.Wardle J, Sanderson S, Guthrie CA, Rapoport L, Plomin R. Parental feeding style and the inter - generational transmission of obesity risk. Obesity. 2002;10(6):453–462. [DOI] [PubMed] [Google Scholar]
- 21.Paxton AE, Strycker LA, Toobert DJ, Ammerman AS, Glasgow RE. Starting the conversation. American Journal of Preventive Medicine. 2011;40(1):67–71. [DOI] [PubMed] [Google Scholar]
- 22.Cogill B Anthropometric indicators measurement guide. 2003. [Google Scholar]
- 23.World Health Organization. WHO child growth standards: head circumference-for-age, arm circumference-for-age, triceps skinfold-for-age and subscapular skinfold-for-age: methods and development. World Health Organization; 2007. [Google Scholar]
- 24.Jaramillo SJ, Yang S-J, Hughes SO, Fisher JO, Morales M, Nicklas TA. Interactive computerized fruit and vegetable preference measure for African-American and Hispanic preschoolers. Journal of Nutrition Education and Behavior. 2006;38(6):352–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hanks AS, Wansink B, Just DR. Reliability and accuracy of real-time visualization techniques for measuring school cafeteria tray waste: validating the quarter-waste method. Journal of the Academy of Nutrition and Dietetics. 2014;114(3):470–474. [DOI] [PubMed] [Google Scholar]
- 26.Fox T, Corbett A, Duffey K. Early Care and Education Policies and Programs to Support Healthy Eating and Physical Activity: Best Practices and Changes Over Time. Research Review: 2010–2016. 2018. https://healthyeatingresearch.org/wp-content/uploads/2018/01/her_ece_011718-1.pdf. Accessed April 7, 2019. [Google Scholar]
- 27.Wolfenden L, Jones J, Finch M, et al. Strategies to improve the implementation of healthy eating, physical activity and obesity prevention policies, practices or programmes within childcare services. Cochrane Database of Systematic Reviews 2016(10):1–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ward DS, Welker E, Choate A, et al. Strength of obesity prevention interventions in early care and education settings: a systematic review. Preventive Medicine. 2017;95:S37–S52. [DOI] [PubMed] [Google Scholar]
- 29.Kakietek J, Dunn L, O’Dell SA, Jernigan J, Khan LK. Peer Reviewed: Training and Technical Assistance for Compliance With Beverage and Physical Activity Components of New York City’s Regulations for Early Child Care Centers. Preventing Chronic Disease. 2014;11(E177). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics. 2007;120:S164–S192. [DOI] [PubMed] [Google Scholar]
- 31.Pesch MH, Appugliese DP, Kaciroti N, Rosenblum KL, Miller AL, Lumeng JC. Maternal encouragement and discouragement: Differences by food type and child weight status. Appetite. 2016;101:15–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Daniel C Economic constraints on taste formation and the true cost of healthy eating. Social Science & Medicine. 2016;148:34–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Valanou E, Naska A, Barbouni A, et al. Evaluation of food photographs assessing the dietary intake of children up to 10 years old. Public Health Nutrition. 2018;21(5):888–895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nicklas T, Islam NG, Saab R, et al. Validity of a Digital Diet Estimation Method for Use with Preschool Children. Journal of the Academy of Nutrition and Dietetics. 2018;118(2):252–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hughes CC, Gooze RA, Finkelstein DM, Whitaker RC. Barriers to obesity prevention in Head Start. Health Affairs. 2010;29(3):454–462. [DOI] [PubMed] [Google Scholar]
- 36.Waters E, de Silva-Sanigorski A, Burford BJ, et al. Interventions for preventing obesity in children. Cochrane Database of Systematic Reviews. 2011(12):1–226. [DOI] [PubMed] [Google Scholar]