Abstract
Purpose
Cancer is the leading cause of mortality among Alaska Native (AN) people. The Alaska Education and Research Towards Health (EARTH) cohort was established to examine risk and protective factors for chronic diseases, including cancer, among AN people. Here, we describe the cancer experience of the Alaska EARTH cohort in relation to statewide- and region-specific tumor registry data, and assess associations with key cancer risk factors.
Methods
AN participants were recruited into the Alaska EARTH cohort during 2004–2006. Data collected included patient demographic, anthropometric, medical and family history, and lifestyle information. This study linked the Alaska EARTH data with cancer diagnoses recorded by the Alaska Native Tumor Registry (ANTR) through 12/31/15. We compared EARTH incidence to ANTR statewide incidence. We examined independent associations of smoking status, diet, BMI, and physical activity with incident all-site cancers using multivariable-adjusted Cox proportional hazards models.
Results
Between study enrollment and 2015, 171 of 3,712 (4.7%) Alaska EARTH study participants were diagnosed with cancer. The leading cancers among Alaska EARTH participants were female breast, lung, and colorectal cancer, which reflected those observed among AN people statewide. Incidence (95% CI) of cancer (all sites) among Alaska EARTH participants was 629.7 (510.9–748.6) per 100,000 person-years; this was comparable to statewide rates [680.5 (660.0–701.5) per 100,000 population]. We observed lower risk of all-sites cancer incidence among never smokers.
Conclusions
Cancer incidence in the Alaska EARTH cohort was similar to incidence observed statewide. Risk and protective factors for leading cancers among AN people mirror those observed among other populations.
Keywords: Indians, North American/statistics & numerical data*, cohort studies, tumor registry, prospective studies, incidence, Neoplasms/epidemiology*, Neoplasms/mortality
Cancer is a leading cause of morbidity and the leading cause of mortality among Alaska Native (AN) people [1]. Furthermore, AN people experience a disproportionate burden of many cancers [2]. For example, colorectal cancer incidence and mortality rates are more than two times higher among AN people than U.S. whites [2], with AN people experiencing incidence among the highest in the world [3, 4]. Additionally, AN incidence of lung and liver cancer are 1.5 times higher, stomach cancer 3.2 times higher, and nasopharyngeal cancer 17.3 times higher among AN people than U.S. whites [2]. Addressing the burden of cancer among AN people will require a comprehensive approach, involving a variety of prevention strategies across the cancer continuum.
The Alaska EARTH cohort study was established to improve understanding of risk and protective factors for cancer and other chronic diseases and to inform the design of more effective primary and secondary prevention strategies among AN people [5, 6]. Previously published reports from this study population demonstrate increased prevalence of several chronic disease risk factors, including tobacco use, physical inactivity, overweight and obesity, and low fruit and vegetable consumption [5, 7, 8]. Cardiometabolic risk factors, including impaired fasting glucose, hypertension, and dyslipidemia, were also more common among Alaska EARTH participants than reported for the general U.S. population by NHANES [8]. Conversely, potential protective factors include reproductive factors such as low nulliparity, decreased use of menopausal estrogen therapy, common use of contraceptive hormones [9], as well as high prevalence of cancer screening [10–12], and participation in AN traditional food use and cultural activities [7].
However, researchers’ ability to directly address associations of risk or protective factors with chronic disease outcomes in these studies are limited, because the extent to which the Alaska EARTH cohort represents the cancer experience of AN people statewide is unknown. The study recruited a convenience sample from three regions of the state, and while it was shown to be representative of these regions by demographic factors including age and education [5], the extent to which it represents AN people in terms of health conditions is unknown. Additionally, previously published studies include only baseline cross-sectional data [5, 7–9], as no longitudinal follow-up data were yet available. The present study addresses these questions by making innovative use of another available resource to understand the cancer burden among AN people: the Alaska Native Tumor Registry (ANTR). The ANTR is a population-based cancer registry that has collected cancer surveillance data for the AN community since 1969. We performed a linkage between the Alaska EARTH cohort and the ANTR database to establish the number and site of incident cancers among the Alaska EARTH cohort since baseline data collection in 2004–2006. We also examined associations of major cancer risk and protective factors with cancer incidence. This study is the first longitudinal cohort study of cancer risk among AN people and provides critical information that will be useful for clinicians, health system administrators, public health program directors, health researchers, and AN people.
METHODS
The Alaska EARTH Study
Detailed methods of the Alaska EARTH study have been described elsewhere [5, 6]. Alaska EARTH participants were recruited from three regions: Southcentral Alaska, which includes the state’s largest urban center, Anchorage; Southeast Alaska, a largely coastal area including the state capital and 30+ remote communities; and Southwest Alaska, which is comprised of 50+ small remote communities in the Yukon-Kuskokwim Delta. Eligibility criteria included the following: age ≥ 18 years, American Indian/Alaska Native (AI/AN) heritage and eligible for health care through the Indian Health Service, not pregnant, not actively undergoing cancer treatment, and physically and mentally able to read and understand the consent form and to complete survey instruments and medical tests. Informed consent was obtained from all participants recruited into the EARTH study. Approval from the Alaska Area Institutional Review Board, as well as approval from regional tribal health organizations and local community councils, was obtained for all aspects of the Alaska EARTH study, including the present analysis. Appropriate tribal review was obtained before publication of this study.
Baseline data collection for the Alaska EARTH study occurred from March 2004 through August 2006 in 26 communities [5]. The baseline study visit consisted of the following: a written informed consent; intake questionnaire for demographic information; clinical measurements (seated blood pressure, height, weight, waist and hip circumference, and fasting blood glucose and lipid panel) [8]; a validated Diet History Questionnaire (DHQ) [13]; as well as Health, Lifestyle and Physical Activity (HLPA) questionnaire that assessed health behaviors, as well as family and personal medical history. Each participant received a personalized health appraisal at the conclusion of the study visit. A fasting blood sample was obtained by finger stick and tested for glucose and lipid levels using the Cholestech LDX® (Cholestech, Hayward, CA, USA) portable analyzer. Medical record reviews using the International Classification of Diseases, Ninth Edition codes were conducted by study-trained research nurses [14].
For the purposes of this study, we used specific information on dietary intake, physical activity, and smoking; therefore, further description of these sections of the questionnaires are given. The DHQ, used in the present analysis to assess fruit and vegetable intake, was designed specifically for use in this cohort of AI/AN adults. The DHQ assessed intake over the past year, to account for seasonal variation in diet due to subsistence food availability. For each food item, participants were asked whether the food was consumed daily, weekly, monthly, or yearly; how many times (per day, month, or year) they ate the food; their usual serving size; and whether or not the food was consumed seasonally. Tobacco use and physical activity were assessed using the HLPA, a questionnaire specifically designed to be AI/AN culturally-relevant. This section of the HLPA included questions on participants’ age at smoking initiation, years since smoking cessation, and number of cigarettes currently smoked per day. These questions did not ask about ceremonial or traditional tobacco use; however, these tobacco uses are less common among AN compared to AI people in the contiguous 48 states where the plant grows naturally [15]. Regarding physical activity, participants were asked to report activities performed during the past week, as well as activities engaged in throughout the year. For the latter, participants were asked to describe about how many months the activity was performed as well as how much time was spent in the activity. Each activity was also weighted by its relative metabolic equivalent (MET) cost,[16] from which we calculated the sum of the MET-hours per week for each participant.
Cancer diagnoses
Cancer diagnosis information was collected by the ANTR, a member of the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) Program since 1999. The ANTR is a population-based registry that records cancer information on AI/AN people meeting eligibility requirements for Indian Health Service benefits, who have been diagnosed with cancer in the state of Alaska since 1969, and who resided in the state at the time of their cancer diagnosis. Cases were ascertained through a variety of sources, including 1) hospital discharge diagnoses for tribal and non-tribal health facilities in Alaska; 2) tumor registry and pathology files of the ANMC and other in-state healthcare facilities; 3) linkage to the Alaska State Cancer Registry and the Washington State Cancer Registry; and 4) death certificates (<1% cases identified through death certificate only). Cancer information has been collected according to SEER program standards since the inception of the ANTR. Linkage of Alaska EARTH study participants with the ANTR database was performed based on key identifying information including full name, date of birth, and social security number.
Cancer risk and protective factors
We compared body mass index (BMI), smoking status, fruit and vegetable intake, physical activity, and family medical history among participants with and without a primary incident cancer. These factors were chosen because of their established links to cancer outcomes in other populations [17–19] and were categorized as follows. BMI (kg/m2) was calculated as the participant’s study-measured weight in kilograms divided by the square of their height in meters. Participants were defined as non-healthy weight if BMI ≥25 kg/m2, or healthy weight if 18.5–24.9 kg/m2. For smoking status, participants were categorized as never, or ever smokers. Ever smokers were those who reported having smoked at least 100 cigarettes in their lifetime [20], and who either reported current smoking, or having quit smoking prior to enrollment. Participants were categorized as meeting fruit and vegetable intake recommendations [21] if they self-reported consuming at least five servings of either fruits or vegetables per day. Physical activity was classified according to U.S. Government guidelines from the Centers for Disease Control and Prevention [22]. As per this recommendation, participants were classified as “physically active” if their self-reported activity met or exceeded 500 metabolic equivalent (MET) minutes/week. Otherwise, participants were classified as “not physically active.” Family history of breast or colorectal cancers was obtained from the EARTH study family history surveys. An individual was classified as having a family history of breast or colorectal cancer only if they self-reported that a first-degree relative (parent, sibling, or child) had previously received a diagnosis.
Statistical Analyses
For the present study, EARTH study participants were initially excluded for missing information necessary to perform linkage with the ANTR. To determine incidence of primary cancer diagnoses, participants with ANTR-identified histories of cancer diagnoses prior to Alaska EARTH study enrollment were additionally excluded [23]. Of the 3,821 participants recruited into the Alaska EARTH cohort, nine were excluded for missing information which prevented linkage with the ANTR. An additional 100 participants were excluded with ANTR-identified histories of cancer diagnoses prior to enrollment. The final sample size for our analyses was 3,712.
Characteristics of those in the Alaska EARTH cohort with and without an incident cancer during follow up were compared using t-tests for continuous variables, and chi-squared tests for categorical variables. Cancer incidence rates (all-sites and site-specific) were calculated among strata of age, sex, cancer site, and study region before being summarized. Incidence rates were age-adjusted to the 2000 US Standard Population [24]. Person-time for participants of the Alaska EARTH cohort was calculated as the time between date of study enrollment and date of cancer incidence (event), administrative censoring (12/31/15), or death. Statewide and regional incidence rates were calculated directly from ANTR data using population data from the SEER Program [24]. Cases diagnosed during years 2004–2015 were included in these calculations. Cancer site was categorized by site according to SEER site groups (ICD/WHO re-classification; ref). Due to small case numbers, we analyzed site-specific data only for cancers of the female breast (ICDO-3 anatomic site codes C50.0–C50.9); lung and bronchus (C34.0–C34.9); and colon, rectum, and recto-sigmoid junction (summarized as “colorectal”; C18.0–C20.9 and C26.0). All other cancers were grouped into “Other”. Independent associations of smoking, BMI, and physical activity with cancer incidence were assessed using univariate and multivariable-adjusted Cox proportional hazards models, adjusted for demographic variables known to affect cancer risk, including age, sex, and rural/urban residence. Participants recruited to the Alaska EARTH study in the southcentral region, inclusive of and adjacent to Anchorage, were considered “urban”, all others were considered “rural.” All statistical tests were two-sided with α = 0.05. All statistical analyses were conducted using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) or SEER*Stat version 8.3 (Surveillance Research Program, National Cancer Institute [seer.cancer.gov/seerstat]).
RESULTS
Demographic and other characteristics for the study sample, stratified by cancer status (cancer-free and incident cancer diagnosis) are shown in Table 1. Those who experienced a cancer diagnosis during follow-up were substantially older at baseline (mean (SD): 52.9 (13.0), vs. 39.3 (14.5), p <0.0001) than those without a cancer diagnosis. Mean BMI was slightly lower among participants who were cancer-free than among those who experienced a cancer diagnosis during follow up (mean (SD): 29.9 (6.9) vs. 31.2 (7.9), p = 0.01). However, the distribution of participants by BMI category (healthy weight/not healthy-weight) was not significantly different between the two groups (p = 0.35). While a larger number of cancer-free participants reported never smoking (39.1%) than among incident cancer participants (32.3%), this difference was not statistically significant. A greater proportion of cancer-free participants than participants with a cancer diagnosis met physical activity guidelines (45.1% vs. 33.3%, respectively p = 0.003). There was no difference between the groups in terms of sex, educational attainment, smoking, the proportion meeting fruit and vegetable recommendations, or reporting a family history of breast or colorectal cancer.
Table 1:
Demographic characteristics of cancer-free Alaska EARTH study participants (n= 3,539), and participants who experienced a cancer diagnosis during period of follow-up (n = 171).
| Alaska EARTH with no history of cancer | Alaska EARTH matched to ANTR | P-valuea | |||
|---|---|---|---|---|---|
| 95%CI | 95%CI | ||||
| n | 3539 | 171 | |||
| Demographic characteristics | |||||
| Age (years, Mean [SD]) | 39.3 (14.5) | 38.8–39.8 | 52.9 (13.0) | 50.9–54.8 | <0.0001 |
| Age at cancer diagnosis (years, mean [SD]) | - | 58.6 (12.8) | |||
| Sex (% Female) | 2138 (60.4) | 58.8–62.0 | 99 (57.9) | 50.5–65.3 | 0.51 |
| Educational attainment (%≥12 years) | 2773 (78.4) | 77.0–79.7 | 127 (74.3) | 67.7–80.8 | 0.21 |
| Language (% English as the primary language at home) | 3249 (92.1) | 91.3–93.0 | 154 (90.1) | 85.6–94.5 | 0.32 |
| Community type (%) Rural | 2254 (63.4) | 62.1–65.3 | 114 (66.7) | 59.6–73.7 | 0.43 |
| Cancer protective factors | |||||
| BMI (kg/m2)mean (SD) | 29.9 (6.9) | 29.6–30.1 | 31.2 (7.9) | 30.0–32.4 | 0.01 |
| BMI category n (%) | |||||
| healthy weight | 941 (26.6) | 25.1–28.1 | 40 (23.4) | 17.1–29.7 | 0.35 |
| Smoking status | |||||
| Never smoked | 1260 (39.1) | 37.4–40.8 | 51 (32.3) | 25.0–39.6 | 0.09 |
| Meets fruit/vegetable recommendations (% ≥5 servings/day)n =2701 | 1127 (43.8) | 41.9–45.8 | 63 (48.5) | 39.9–57.1 | 0.30 |
| Mean hours of moderate to vigorous physical activity/wk | 25.0 (27.7) | 24.0–26.0 | 17.3 (13.5) | 13.5–21.2 | 0.04 |
| Meets physical activity recommendations (% ≥500 met min/wk) | 1595 (45.1) | 43.4–46.7 | 57 (33.3) | 26.3–40.4 | 0.003 |
P-value for t-test (continuous variables), or Chi-squared (categorical variables)
ANTR: Alaska Native Tumor Registry; BMI: body mass index; EARTH: Education and Research Towards Health; MET: Metabolic equivalent; SD: standard deviation;
We identified 171 new cases of cancer diagnosed among Alaska EARTH study participants during the period of follow-up. The most common cancer sites diagnosed were female breast (n = 41), colorectal (n = 27), and lung and bronchus (n = 27). Less commonly diagnosed cancers included cancers of the stomach (n = 7), prostate (n = 7), and kidney (n = 7); in total, we observed 59 cancers that we classified as “other.” The mean (SD) follow-up time for this cohort was 10.0 (1.9) years for those who did not develop cancer during follow-up, and 8.5 (3.0) years for those who did develop cancer during follow-up.
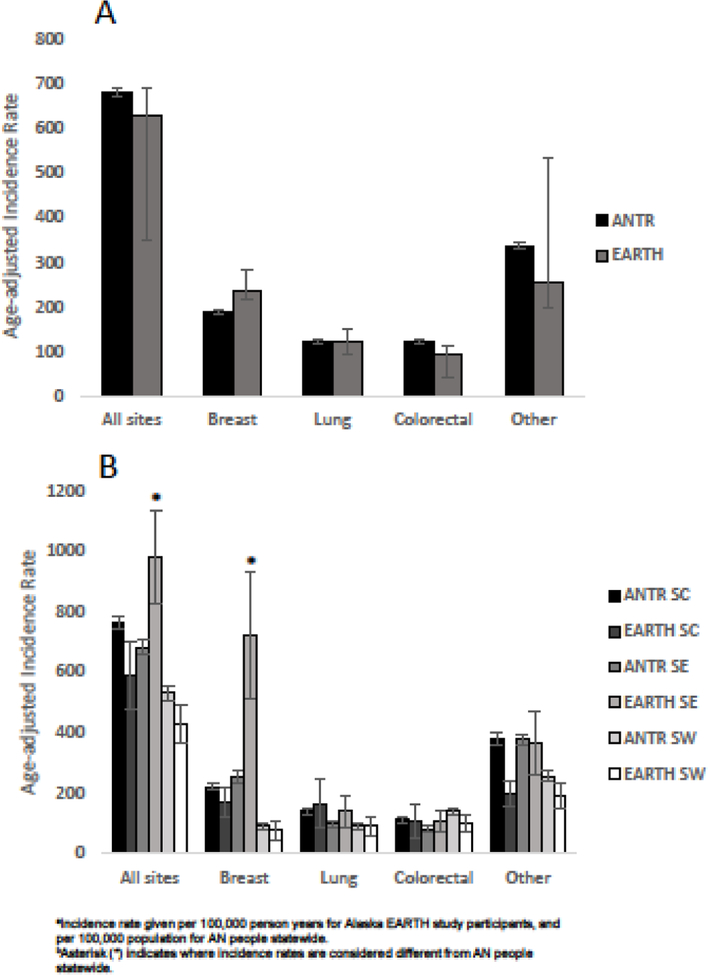
Figure 1 shows age- and region-specific incidence rates for the Alaska EARTH cohort, as well as the corresponding incidence rates for all AN people (statewide, and by each of the three study regions) from the ANTR; supporting data are given in Supplementary Table 1. For all sites and all ages combined, the Alaska EARTH study exhibited slightly lower incidence rates, relative to the statewide ANTR rates. Examining site-specific incidence rates, we observed a possible trend of lower colorectal cancer incidence among Alaska EARTH participants (all regions), relative to AN people statewide. Of note, incidence rates for female breast cancer were significantly higher among Alaska EARTH participants than AN people statewide. In particular, rates of female breast cancer were significantly higher among southeast Alaska EARTH study participants, relative to the all AN women in the southeast region, and AN women statewide. This elevated incidence of female breast cancer in this region also appeared to drive the elevated all-sites cancer incidence rate in the southeast Alaska EARTH participants, relative to all southeast Alaska residents. Rates of “other” cancers were significantly lower among Alaska EARTH study participants than AN people statewide.
Figure 1.
Incidence of all-sites and selected cancers among AN people statewide, and participants of the Alaska EARTH study, overall (A) and stratified by region (B).
We also examined associations of several leading cancer risk and protective factors with all sites cancer incidence (Table 2). For all cancer sites, we observed statistically decreased risk among women, never smokers, and rural residents. Due to small case counts, we were not able to examine associations with site-specific cancer incidence.
Table2.
Associations of protective factors with cancer incidence (all sites and selected cancer sites) among participants of the Alaska EARTH study.a,b
| Univanate Estimates | Multivariable-adjusted Estimates | |||||
|---|---|---|---|---|---|---|
| Variables | Hazard Ratio | 95% CI* | p-value | Hazard Ratio | 95% CI* | p-value |
| Demographic variables | ||||||
| Age, years | 1.1 | 1.0–1.2 | 0.020 | 1.003 | 1.00–1.01 | 0.013 |
| Sex (ref. Male) | 1.1 | 1.1–1.2 | 0.001 | 1.13 | 1.1–1.2 | 0.009 |
| Community (ref. Rural) | 1.1 | 1.04–1.19 | 0.003 | 1.12 | 1.04–1.20 | 0.003 |
| Protective factors | ||||||
| Nonsmoker (ref. ever smoker) | 0.91 | 0.84–0.97 | 0.006 | 0.93 | 0.86–0.99 | 0.04 |
| BMI (ref. ≥ 25) | 1.01 | 0.93–1.08 | 0.88 | 1.0 | 0.92–1.1 | 0.99 |
| Physically Active (ref.<500 met min/wk) | 0.92 | 0.86–0.99 | 0.021 | 0.92 | 0.86–0.99 | 0.02 |
Multivariable-adjusted hazard ratio (95% confidence interval) adjusted for age, sex, and urban/rural residence).
ANTR: Alaska Native Tumor Registry; BMI: body mass index; EARTH: Education and Research Towards Health; MET: Metabolic equivalent.
DISCUSSION
This study provides the first longitudinal examination of cancer incidence in an AN cohort, and presents associations of cancer incidence with several known cancer risk and protective factors. Through linkage with the ANTR, we observed 171 cases of cancer among Alaska EARTH participants during the period of follow up (2004–2006 to 2015); leading cancers mirrored those previously reported for AN people statewide [2]. Critically, we were able to compare incidence rates among Alaska EARTH participants to those observed among AN people statewide, demonstrating few statistically significant differences. The most notable difference that we observed was a higher incidence of female breast cancer among Alaska EARTH participants, particularly those recruited in the Southeast region, relative to AN people statewide. However, overall, our findings indicate that, at the present time, the cancer experience of Alaska EARTH participants is mostly representative of AN people; further follow up of this cohort will indicate whether observed differences in breast cancer incidence remain over time. Despite small case counts, we were able to examine associations of several leading cancer risk and protective factors for cancer for all-sties. Individuals who had never smoked, were female, or lived in a rural area were at slightly decreased risk of developing cancer over the follow-up period. The results of this study are a critical first step to understanding factors that decrease or increase risk among AN people, and provide important novel data to support prevention and control research and programs.
To know whether associations observed among Alaska EARTH participants may be generalizable to AN people statewide, this study sought to determine whether the cancer outcome experience of Alaska EARTH study participants was similar to that observed by the ANTR for AN people statewide. We found that the three leading cancers among Alaska EARTH study participants (female breast, lung, and colorectal cancers) were the same as those reported for AN people statewide during the same time period. Furthermore, incidence rates for many of the leading cancers were very similar among Alaska EARTH study participants and AN people statewide; while there were trends towards lower rates of all sites, colorectal, and other cancers at the statewide and regional levels. These differences typically did not reach statistical significance. In contrast, we did observe significant differences in female breast cancer incidence, which was substantially higher among Alaska EARTH participants from the Southeast region, relative to both the complete Alaska EARTH cohort, and AN women statewide. While this difference is intriguing, it is possible that its magnitude may be artificial; an artifact of small population size, a relatively small regional sample size, and an overall small number of cases reported. However, if this is a “true” difference, it may be due to differences in patient demographic characteristics such as age; we do note that the mean age of study participants was slightly higher in the Southeast region. Alternatively exposure to female breast cancer risk or protective factors may be higher in this group of study participants. Previous studies have shown that research study participants may not be representative of the general population in terms of demographic factors as well as general health [25]. The Alaska EARTH cohort has been shown to be representative of AN people statewide in terms of age and educational attainment [5], yet, its representativeness in terms of other cancer risk factors is unknown. While our findings suggest that the cancer experience of Alaska EARTH participants is likely similar to that among AN people statewide, further surveillance of the Alaska EARTH cohort is necessary to determine whether this remains true as cohort cancer cases change over time.
Our analyses of associations with all-sites cancer incidence were constrained due to our small case counts; however, we were able to identify a significantly decreased risk of cancer among Alaska EARTH study participants with no history of smoking. Smoking has been identified as a key target for cancer and other chronic disease prevention efforts among AN people [26], in part due to the high prevalence of smoking [15, 27]. While small case counts precluded examination of site-specific associations, we hypothesize even stronger protective associations may have been observed for not smoking with specific cancer sites, for example with lung cancer. Given that the strength of associations of many risk and protective factors are known to vary with cancer site [28], we are likely missing important information regarding risk of specific cancers among AN people. Future research should continue to examine risk and protective factor associations with specific cancers over time, as we expect case counts to increase with an aging study population.
This study has several key strengths. The linkage of Alaska EARTH cohort with the ANTR was an innovative way of leveraging established resources to understand and address the cancer burden among AN people. AN people experience a unique pattern of cancer incidence and mortality [2], and both the Alaska EARTH cohort and the ANTR are key resources that can be used to understand and address cancer disparities in this population. This is also the first study to examine longitudinal associations of potential risk and protective factors with incident cancers among AN people, providing some initial data to support new and existing cancer prevention and control programs. Continued linkage of these resources at regular intervals may provide additional information towards this effort. Finally, this study examined protective factors to reinforce the positive outcomes associated with healthy behaviors. This strengths-based approach was intended to demonstrate how healthy behaviors decrease cancer risk, rather than focus exclusively on how less healthful behaviors increase risk.
This study also has several limitations that warrant discussion. The relatively small size of the Alaska EARTH cohort, and the resulting small numbers of cancer cases, limited our statistical power. As a result, confidence intervals around some of our incidence estimates were large, particularly when stratified by region, which limited our ability to reliably quantify differences in rates between regions. We were also limited in our ability to examine associations of cancer incidence with a large range of cancer risk factors. For this reason, we focused only on five leading risk factors previously identified in other populations and their associations with cancer incidence (all sites). Measures of dietary intake and physical activity are known to be particularly prone to error due to participant recall [29, 30]. These and other self-reported measures may have contributed to diminished statistical power to detect associations. Furthermore, we do not know whether the baseline questionnaires are likely to reflect lifetime exposures to risk and protective factors. Finally, the generalizability of our findings may also be limited by convenience sampling of the cohort despite its resemblance to the regional populations in terms of age and years of education [5].
While we assume that risk and protective factors for cancer observed in other, non-Native populations are also relevant to AN people, this assumption has not been tested in any longitudinal studies. Through an innovative linkage of the Alaska EARTH study and the ANTR, this study provides the first examination of cancer incidence among an Alaska AI/AN cohort, as well as the first associations of major cancer risk and protective factors with cancer incidence. Given the cancer experience among Alaska EARTH participants was similar to that observed statewide, we expect that these results should provide an important starting point for understanding cancer risk, and promoting healthful behaviors among all AN people, as well as support for existing and novel cancer prevention and control programs in the Alaska Tribal Health System. Further research with and surveillance of this cohort will determine whether this remains true over time, or if the non-significant trends towards lower incidence of colorectal and other cancers, and higher incidence of breast cancers, becomes important.
Supplementary Material
Funding
Dr. Nash, Mr. Zimpelman and the Alaska Native Tumor Registry are supported by the National Cancer Institute (NCI) Surveillance, Epidemiology and End Results Program, NCI contract number HHSN26120130010I, Task Order HHSN26100005. Ms. Day, Dr. Hiratsuka, and Dr. Koller are supported by a Native American Research Centers for Health grant from National Institute of General Medical Sciences, grant number U261IHS0084. Dr. Hiratsuka is additionally supported by the NIGMS grant number 1S06GM123545. The Alaska EARTH study was funded by NCI grants CA88958 and CA96095.
Abbreviations:
- AI/AN:
American Indian/Alaska Native
- AN
Alaska Native
- ANTR
Alaska Native Tumor Registry
- BMI
Body Mass Index
- EARTH
Education and Research Towards Health
- SEER
Surveillance, Epidemiology and End Results
LITERATURE CITED
- 1.Blake I, Holck P, Provost EM, Alaska Native Mortality Update: 2009–2013. 2016, Alaska Native Epidemiology Center: Anchorage, AK. [Google Scholar]
- 2.Carmack A, Schade TL, Sallison I, Provost EM, Kelly JJ, Cancer in Alaska Native People: 1969–2013, The 45 Year Report. 2015, Alaska Native Epidemiology Center, Alaska Native Tribal Health Consortium: Anchorage, AK. [Google Scholar]
- 3.Center MM, Jemal A, and Ward E, International trends in colorectal cancer incidence rates. Cancer Epidemiology and Prevention Biomarkers, 2009. 18(6): p. 1688–1694. [DOI] [PubMed] [Google Scholar]
- 4.Kelly JJ, Alberts SR, Sacco F, and Lanier AP, Colorectal cancer in alaska native people, 2005–2009. Gastrointest Cancer Res, 2012. 5(5): p. 149–54. [PMC free article] [PubMed] [Google Scholar]
- 5.Lanier AP, Redwood DG, and Kelly JJ, The Alaska Education and Research Towards Health (EARTH) Study: cancer risk factors. J Cancer Educ, 2012. 27(1 Suppl): p. S80–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Slattery ML, Schumacher MC, Lanier AP, Edwards S, Edwards R, Murtaugh MA, Sandidge J, Day GE, Kaufman D, Kanekar S, Tom-Orme L, and Henderson JA, A prospective cohort of American Indian and Alaska Native people: study design, methods, and implementation. Am J Epidemiol, 2007. 166(5): p. 606–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Redwood DG, Ferucci ED, Schumacher MC, Johnson JS, Lanier AP, Helzer LJ, Tom-Orme L, Murtough MA, and Slattery ML, Traditional foods and physical activity patterns and associations with cultural factors in a diverse Alaska Native population. Int J Circumpolar Health, 2008. 67(4): p. 335–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Redwood DG, Lanier AP, Johnston JM, Asay ED, and Slattery ML, Chronic disease risk factors among Alaska Native and American Indian people, Alaska, 2004–2006. Prev Chronic Dis, 2010. 7(4): p. A85. [PMC free article] [PubMed] [Google Scholar]
- 9.Redwood DG, Lanier AP, Johnston JM, Murphy N, and Murtaugh MA, Reproductive cancer risk factors among Alaska Native women: the Alaska Education and Research Towards Health (EARTH) Study. Womens Health Issues, 2012. 22(4): p. e387–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schumacher MC, Slattery ML, Lanier AP, Ma KN, Edwards S, Ferucci ED, and Tom-Orme L, Prevalence and predictors of cancer screening among American Indian and Alaska native people: the EARTH study. Cancer Causes Control, 2008. 19(7): p. 725–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Breast Cancer Screening. [cited 2017 03/15].
- 12.Colorectal Cancer Screening. [cited 2018 11/21/2018].
- 13.Murtaugh MA, Ma KN, Greene T, Redwood D, Edwards S, Johnson J, Tom-Orme L, Lanier AP, Henderson JA, and Slattery ML, Validation of a dietary history questionnaire for American Indian and Alaska Native people. Ethn Dis, 2010. 20(4): p. 429–36. [PMC free article] [PubMed] [Google Scholar]
- 14.Koller KR, Wilson AS, Asay ED, Metzger JS, and Neal DE, Agreement Between Self-Report and Medical Record Prevalence of 16 Chronic Conditions in the Alaska EARTH Study. J Prim Care Community Health, 2014. 5(3): p. 160–5. [DOI] [PubMed] [Google Scholar]
- 15.Redwood D, Lanier AP, Renner C, Smith J, Tom-Orme L, and Slattery ML, Differences in cigarette and smokeless tobacco use among American Indian and Alaska Native people living in Alaska and the Southwest United States. Nicotine Tob Res, 2010. 12(7): p. 791–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, O Brien WL, Bassett DR, Schmitz KH, and Emplaincourt PO, Compendium of physical activities: an update of activity codes and MET intensities. Medicine and science in sports and exercise, 2000. 32(9; SUPP/1): p. S498–S504. [DOI] [PubMed] [Google Scholar]
- 17.Johnson NB, Hayes LD, Brown K, Hoo EC, and Ethier KA, CDC National Health Report: leading causes of morbidity and mortality and associated behavioral risk and protective factors--United States, 2005–2013. MMWR Suppl, 2014. 63(4): p. 3–27. [PubMed] [Google Scholar]
- 18.Steele CB, Thomas CC, Henley SJ, Massetti GM, Galuska DA, Agurs-Collins T, Puckett M, and Richardson LC, Vital Signs: Trends in Incidence of Cancers Associated with Overweight and Obesity - United States, 2005–2014. MMWR Morb Mortal Wkly Rep, 2017. 66(39): p. 1052–1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Henley SJ, Thomas CC, Sharapova SR, Momin B, Massetti GM, Winn DM, Armour BS, and Richardson LC, Vital Signs: Disparities in Tobacco-Related Cancer Incidence and Mortality - United States, 2004–2013. MMWR Morb Mortal Wkly Rep, 2016. 65(44): p. 1212–1218. [DOI] [PubMed] [Google Scholar]
- 20.Wang TW, Asman K, Gentzke AS, Cullen KA, Holder-Hayes E, Reyes-Guzman C, Jamal A, Neff L, and King BA, Tobacco product use among adults—United States, 2017. Morbidity and Mortality Weekly Report, 2018. 67(44): p. 1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marmot M, Atinmo T, Byers T, Chen J, Hirohata T, Jackson A, James W, Kolonel L, Kumanyika S, and Leitzmann C, Food, nutrition, physical activity, and the prevention of cancer: a global perspective. 2007.
- 22.Health, U.D.o. and H. Services, 2008 physical activity guidelines for Americans: Be active, healthy, and happy! http://www.health.gov/paguidelines, 2008.
- 23.Nash SH, Day G, Hiratsuka VY, Zimpelman GL, and Koller KR, Agreement between self-reported and central cancer registry-recorded prevalence of cancer in the Alaska EARTH study. Int J Circumpolar Health, 2019. 78(1): p. 1571383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Surveillance, E., and End Results (SEER) Program (www.seer.cancer.gov), Surveillance, Epidemiology, and End Results (SEER) Program Populations (1969–2014) (www.seer.cancer.gov/popdata), D. National Cancer Institute, Surveillance Research Program, Surveillance Systems Branch, Editor. March 2016. [Google Scholar]
- 25.Batty GD, Shipley M, Tabák A, Singh-Manoux A, Brunner E, Britton A, and Kivimäki M, Generalizability of occupational cohort study findings. Epidemiology, 2014. 25(6): p. 932–933. [DOI] [PubMed] [Google Scholar]
- 26.Nash SH and Redwood DG, Potentially Preventable Cancers Among Alaska Native People. Cancer Health Disparities, 2018. E pub ahead of print. [Google Scholar]
- 27.Center, A.N.E. Adult Current Smoking <http://anthctoday.org/epicenter/healthData/factsheets/adult_current_smoking_statewide_1_10_2017.pdf>. October 1st 2017 April 26th 2018].
- 28.Sylvester B, Olipade OI, and Offerman MK, The biology of cancer and its relationship to disparities in cancer occurrence and outcomes, in Cancer disparities : causes and evidence-based solutions Elk R, Landrine H, and A.C. Society, Editors. 2012, Springer: New York, NY. [Google Scholar]
- 29.Prentice RL, Measurement error and results from analytic epidemiology: dietary fat and breast cancer. J Natl Cancer Inst, 1996. 88(23): p. 1738–47. [DOI] [PubMed] [Google Scholar]
- 30.Thiebaut AC, Kipnis V, Schatzkin A, and Freedman LS, The role of dietary measurement error in investigating the hypothesized link between dietary fat intake and breast cancer--a story with twists and turns. Cancer Invest, 2008. 26(1): p. 68–73. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.