Abstract
Background:
Medicare’s Hospital Readmissions Reduction Program reports risk-standardized readmission rates for traditional Medicare but not Medicare Advantage beneficiaries.
Objective:
To compare readmission rates between Medicare Advantage and traditional Medicare.
Design:
Retrospective cohort study linking the Medicare Provider Analysis and Review (MedPAR) file with the Healthcare Effectiveness Data and Information Set (HEDIS).
Setting:
4748 U.S. acute care hospitals.
Patients:
Patients aged 65 years or older hospitalized for acute myocardial infarction (AMI) (n = 841 613), congestive heart failure (CHF) (n = 1 458 652), or pneumonia (n = 2 020 365) between 2011 and 2014.
Measurements:
30-day readmissions.
Results:
Among admissions for AMI, CHF, and pneumonia identified in MedPAR, 29.2%, 38.0%, and 37.2%, respectively, did not have a corresponding record in HEDIS. Of these, 18.9% for AMI, 23.7% for CHF, and 18.3% for pneumonia resulted in a readmission that was identified in MedPAR. However, among index admissions appearing in HEDIS, 14.4% for AMI, 18.4% for CHF, and 13.9% for pneumonia resulted in a readmission. Patients in Medicare Advantage had lower unadjusted readmission rates than those in traditional Medicare for all 3 conditions (16.6% vs.17.1% for AMI, 21.4% vs. 21.7% for CHF, and 16.3% vs. 16.4% for pneumonia). However, after standardization, patients in Medicare Advantage had higher readmission rates than patients in traditional Medicare for AMI (17.2% vs. 16.9%; difference, 0.3 percentage point [95% CI, 0.1 to 0.5 percentage point]), CHF(21.7% vs. 21.4%; difference, 0.3 percentage point [CI, 0.2 to 0.5 percentage point]), and pneumonia (16.5% vs. 16.0%; difference, 0.5 percentage point [95% CI, 0.4 to 0.6 percentage point]). Rate differences increased between 2011 and 2014.
Limitation:
Potential unobserved differences between populations.
Conclusion:
The HEDIS data underreported hospital admissions for 3 common medical conditions, and readmission rates were higher among patients with underreported admissions. Medicare Advantage beneficiaries had higher risk-adjusted 30-day readmission rates than traditional Medicare beneficiaries.
Primary Funding Source:
National Institute on Aging.
Hospital readmissions are common and burdensome to patients and their caregivers (1) and cost Medicare $26 billion annually (2). Clinicians, hospitals, and payers, particularly Medicare, have focused substantial attention on reducing readmission rates. For instance, the Medicare Hospital Readmissions Reduction Program (HRRP) penalizes hospitals with worse than expected 30-day readmission rates for common medical conditions. In the traditional Medicare program, which covers more than 65% of all Medicare beneficiaries, substantial decreases in readmission rates were observed starting in 2010 (3) and persisted each year through 2015 (4).
The HRRP derives hospitals’ readmission rates using data from traditional Medicare beneficiaries only. The program does not report readmission rates for persons with other sources of insurance coverage, including the rapidly growing Medicare Advantage program. Therefore, there are limited national data for hospitalists, primary care physicians, and postacute care providers to understand readmission risks for their patients in Medicare Advantage and how readmission rates may differ from traditional Medicare beneficiaries. This is important because one third of Medicare beneficiaries (about 19 million people) are currently enrolled in Medicare Advantage (5, 6).
Readmissions are ideal for comparison between traditional Medicare and Medicare Advantage. Traditional Medicare generally reimburses providers with fee-for-service payments that reward the volume and intensity of care, potentially leading to increased rates of hospitalizations and readmissions. In contrast, Medicare Advantage plans receive capitated payments to bear the risk of financing covered services and, therefore, operate under strong incentives to reduce costs of care and hospital readmissions. Further, Medicare Advantage plans may adopt some quality management tools that are not available in traditional Medicare. For instance, plans can selectively contract with higher-performing hospitals or deploy case management and care transition programs to patients at high risk for readmission.
Previous studies have reported lower readmission rates in Medicare Advantage than traditional Medicare (7–9), leading some policy observers to conclude that Medicare Advantage beneficiaries have better post-acute care outcomes (10). However, these studies have been limited by the lack of complete and accurate data on hospitalizations in Medicare Advantage. The Centers for Medicare & Medicaid Services (CMS) does not evaluate readmissions in Medicare Advantage and traditional Medicare using the same data sources and measure specifications.
Using a novel data linkage, we compared 30-day re-admission rates after hospitalization for 3 major conditions included in the HRRP—acute myocardial infarction (AMI), congestive heart failure (CHF), and pneumonia—between Medicare Advantage and traditional Medicare beneficiaries from 2011 to 2014. We hypothesized that readmission rates among traditional Medicare beneficiaries are not higher than those among Medicare Advantage beneficiaries, as previously reported.
Methods
Data
We used the Medicare Provider Analysis and Review (MedPAR) files to identify hospital admissions for patients in traditional Medicare and those in Medicare Advantage. Medicare Advantage status was determined on the basis of the patient’s enrollment on the day of admission. A recent study determined that hospitals that submit MedPAR data for patients in Medicare Advantage accounted for 92% of Medicare discharges between 2011 and 2013 (7). Because readmissions may occur in hospitals that do not report MedPAR data for Medicare Advantage enrollees (11, 12), we linked Med-PAR data with Healthcare Effectiveness Data and Information Set (HEDIS) records. The HEDIS data include hospital admissions and discharge dates and an indicator of whether a patient was admitted within 30 days of discharge at the same or a different hospital. The HEDIS readmission measure requires continuous enrollment in the Medicare Advantage plan for 12 months before and 30 days after the index admission with no gap exceeding 45 days. With the exception of private fee-for-service plans with fewer than 1000 enrollees, all Medicare Advantage plans must report HEDIS data to CMS. The Medicare Master Beneficiary Summary File provided demographic characteristics.
Study Population
We applied the eligibility criteria used in the publicly reported readmission measures developed by CMS for the HRRP (13–16). For persons aged 65 years or older, we defined an index admission as any hospitalization with a live discharge and a principal diagnosis of AMI, CHF, or pneumonia from nonfederal, short-term, acute care hospitals in any state and the District of Columbia between 1 January 2011 and 30 November 2014 (Supplement, available at Annals.org).
Outcome
Our outcome was all-cause readmission within 30 days after discharge from an index admission (Supplement Table 1, available at Annals.org). Readmissions for patients in traditional Medicare were identified from MedPAR, which is designed to capture all inpatient claims in traditional Medicare. For patients in Medicare Advantage, we used both MedPAR and HEDIS and coded a readmission occurring in either data set (Supplement). We chose this strategy for 2 reasons. First, MedPAR would not capture readmissions that occur in hospitals that do not submit MedPAR data. Second, we have previously found that Medicare Advantage plans may underreport certain quality measures to HEDIS(17), suggesting that underreporting of other measures, such as readmissions, is also possible. Thus, use of both data sets was designed, to the extent possible, to address the lack of comprehensive billing data for patients in Medicare Advantage.
Covariates
Demographic covariates included age (5-year increments), sex, race/ethnicity, annual household income (estimated from residential ZIP codes [18]), education (estimated from the percentage of the population with a college degree residing in the patient’s ZIP code), dual Medicare–Medicaid coverage, and year of hospital admission. These covariates expand on those used by CMS in the HRRP (19–21). Condition-specific comorbid conditions (Supplement Table 2, available at Annals.org) were classified according to published approaches used in the HRRP and derived using principal and secondary diagnosis codes from the index hospitalization and hospitalizations in the previous 12 months (Supplement) (13–16). The CMS uses both inpatient and outpatient claims to ascertain comorbid conditions; we used only inpatient claims because outpatient claims are unavailable for Medicare Advantage (Supplement). A prior analysis found that inclusion of comorbid conditions from out-patient data did not result in meaningful changes in hospitals’ risk-standardized readmission rates (22–24).
Statistical Analysis
We used the Neuhaus–Kalbfleisch method (25) to estimate the within-hospital effect of Medicare Advantage versus traditional Medicare. To do so, we applied a hierarchical logistic regression model with a random intercept for the hospital-specific effect and fixed-effect terms for Medicare Advantage versus traditional Medicare status; the sociodemographic characteristics described earlier; condition-specific comorbid conditions; dual Medicare–Medicaid coverage; year of admission; and the fraction of patients in Medicare Advantage treated in each hospital for AMI, CHF, or pneumonia. Observations with missing covariates (<2%) were not included (Supplement). Accordingly, this analysis estimated the difference on the logit scale in readmission rates between patients in Medicare Advantage and those in traditional Medicare admitted to the same hospital (within-hospital effect) while separating the across-hospital effect. On the basis of this model, we estimated the standardized readmission rates in Medicare Advantage and traditional Medicare using predictive margins (26–28) and subsequently computed the difference in standardized readmission rates for Medicare Advantage versus traditional Medicare (Supplement).
We performed sensitivity and subgroup analyses to assess the robustness of our findings. First, we modeled the outcome without hospital indicators as covariates to estimate the overall contrast of Medicare Advantage versus traditional Medicare—that is, a mixture of the within-hospital effect (primary analysis) and the across-hospital effect. Similarity of this result to the primary result would suggest that the effect of Medicare Advantage on readmission is not modified by the admitting hospital (29). Second, we used a linear probability model with multiway cluster-robust SEs to account for both clustering of observations within hospitals and repeated hospitalizations from the same patient (Supplement). Third, to assess asymmetry resulting from using both HEDIS and MedPAR to ascertain readmissions in Medicare Advantage but only MedPAR to ascertain readmissions in traditional Medicare, we repeated the main analyses by identifying readmissions for Medicare Advantage beneficiaries in MedPAR alone and in HEDIS alone and investigated the linkage between MedPAR and HEDIS data. Fourth, we assessed the robustness of our findings to potential unmeasured covariates using the E-value (30, 31), which measures the minimum strength of association that unmeasured covariates need to have with Medicare Advantage status and read-mission to explain our observed effect of Medicare Advantage on readmission (30) (Supplement). Previous research (7, 8) suggested that 30-day readmission rates among traditional Medicare beneficiaries are higher than those among Medicare Advantage beneficiaries. Using E-values, we examined the sensitivity of our results to un-measured covariates by assessing whether our observed 30-day readmission rate differences between Medicare Advantage and traditional Medicare are no worse than previously published estimates (7, 8) which we assumed to be the true differences (noninferiority) (Supplement Table 3, available at Annals.org). Fifth, we compared 30-day readmission rates between traditional Medicare and Medicare Advantage separately by year. Sixth, we estimated the expected risk for readmission for patients in Medicare Advantage and those in traditional Medicare by standardizing to the risk in the entire study population (Supplement). Finally, we estimated the differences in re-admission rates between Medicare Advantage and traditional Medicare among beneficiaries who had not died before being readmitted within 30 days after discharge (Supplement).
We used SAS, version 9.4 (SAS Institute), and Stata 15 (StataCorp) for all analyses. All statistical tests were 2-sided at an [H9251] level of 0.05.
Ethics
The Institutional Review Board at Brown University approved this study.
Role of the Funding Source
The National Institute on Aging had no role in the study design, conduct, or analysis; interpretation and reporting of the results; or writing of the manuscript.
Results
Linkage Between MedPAR and HEDIS
Among hospitalizations for Medicare Advantage enrollees who were in a HEDIS-reporting plan during the 12 months before the index admission, 29.2% of admissions for AMI, 38.0% for CHF, and 37.2% for pneumonia (as identified in MedPAR) did not have a corresponding record in HEDIS. Of these, 18.9% for AMI, 23.7% for CHF, and 18.3% for pneumonia (Supplement Tables 4a, 4b, and 4c, respectively, available atAnnals.org) resulted in a readmission that was identified in MedPAR records. In contrast, among the index admissions in this population that appeared in HEDIS,14.4% for AMI, 18.4% for CHF, and 13.9% for pneumonia (Supplement Tables 4a, 4b, and 4c, respectively) resulted in a readmission. When readmissions for patients in Medicare Advantage were ascertained using only MedPAR or HEDIS, the unadjusted and adjusted 30-day readmission risks were lower for patients in Medicare Advantage than traditional Medicare for all 3 conditions (Supplement Table 5, available at Annals.org). Supplement Table 6 (available at Annals.org) shows the agreement between readmissions identified in MedPAR and HEDIS among index admissions that were present in both data sources.
Patient Characteristics
Table 1 shows the number of patients hospitalized and discharged alive with a primary diagnosis of AMI (n = 841 613), CHF (n = 1 458 652), or pneumonia (n = 2 020 365) in any of the 4748 eligible hospitals. For all 3 conditions, patients in Medicare Advantage were slightly younger and less likely to be white than patients in traditional Medicare hospitalized with the same primary diagnosis. The proportion of patients with dual Medicare–Medicaid coverage was higher among traditional Medicare beneficiaries for all 3 conditions.
Table 1.
Characteristics of Traditional Medicare and Medicare Advantage Beneficiaries Hospitalized for AMI, CHF, or Pneumonia Between 2011 and 2014*
| Characteristic | AMI | CHF | Pneumonia | |||
|---|---|---|---|---|---|---|
| Traditional Medicare | Medicare Advantage | Traditional Medicare | Medicare Advantage | Traditional Medicare | Medicare Advantage | |
| Index admissions with live discharges, n | 664 389 | 242 859 | 1 557 741 | 477 499 | 1 937 710 | 497 878 |
| Hospitals, n | 4329 | 3048 | 4673 | 3727 | 4721 | 3899 |
| Beneficiaries, n | 615 482 | 226 131 | 1 111 408 | 347 244 | 1 592 811 | 427 554 |
| Readmissions, n (%)† | ||||||
| All years | 113487(17.1) | 40 217(16.6) | 337 281 (21.7) | 102 093(21.4) | 316831 (16.4) | 80 939(16.3) |
| 2011 | 32 135(18.5) | 9753(17.6) | 94 892 (22.6) | 24 687(22.3) | 88 897(17.1) | 19590(17.1) |
| 2012 | 30 043(17.4) | 10 176(17.1) | 87 345 (22.0) | 24619(21.4) | 82 343(16.6) | 19 608(16.3) |
| 2013 | 27 702(16.4) | 10368(16.1) | 81 683(21.0) | 26 370(21.0) | 79 223(15.8) | 21 422(15.9) |
| 2014 | 23 607(15.8) | 9920(15.7) | 73 361 (20.8) | 26 417(20.9) | 66 368(15.8) | 20 319(15.9) |
| Mean age (SD),y | 78.7(8.3) | 77.5(7.8) | 81.2(8.3) | 79.9(8.1) | 80.7(8.5) | 79.7(8.2) |
| Male, % | 51.3 | 53.5 | 44.3 | 46.8 | 45.5 | 47.5 |
| Race, % | ||||||
| White | 84.7 | 77.9 | 82.1 | 74.5 | 84.6 | 79.4 |
| Black | 7.6 | 9.6 | 10.6 | 14.5 | 7.6 | 9.3 |
| Hispanic | 4.8 | 9.1 | 4.7 | 8.3 | 4.8 | 7.9 |
| Other | 2.7 | 3.2 | 2.4 | 2.6 | 2.9 | 3.3 |
| Dual Medicare-Medicaid coverage‡ | 19.4 | 16.7 | 23.5 | 21.2 | 30.0 | 24.1 |
| Mean condition-specific comorbid | 4.8(3.0) | 4.5(2.8) | 6.1 (4.0) | 5.8(3.8) | 3.1 (4.4) | 2.5(4.0) |
| conditions (SD), n | ||||||
| Beneficiaries, by proportion of | ||||||
| population with college degree, %§ | ||||||
| <7.1% | 23.5 | 24.3 | 24.6 | 25.4 | 23.6 | 24.0 |
| 7.196–8.8% | 23.4 | 25.0 | 24.3 | 26.4 | 24.0 | 26.1 |
| 8.9%–10.9% | 24.6 | 24.6 | 24.7 | 24.7 | 24.9 | 25.3 |
| >10.9% | 26.8 | 24.7 | 24.8 | 22.1 | 25.8 | 23.2 |
| Annual household income, %§ | ||||||
| <$40 032 | 23.1 | 22.8 | 24.0 | 24.3 | 23.8 | 22.4 |
| $40 032–S50 047 | 26.2 | 25.6 | 25.4 | 25.0 | 25.9 | 25.2 |
| $50 048–$65 109 | 25.5 | 27.2 | 25.2 | 26.7 | 25.2 | 27.3 |
| >$65109 | 25.2 | 24.5 | 25.4 | 24.0 | 25.1 | 25.2 |
| Geographic region, % | ||||||
| Midwest | 26.0 | 21.2 | 26.1 | 21.8 | 26.0 | 22.4 |
| Northeast | 19.1 | 22.3 | 20.1 | 24.6 | 18.2 | 22.3 |
| South | 40.2 | 32.6 | 40.7 | 32.1 | 40.7 | 30.9 |
| West | 14.6 | 23.9 | 13.1 | 21.5 | 15.1 | 24.4 |
AMI = acute myocardial infarction; CHF = congestive heart failure.
No formal (i.e., null hypothesis testing–based) comparison of baseline characteristics between groups was performed.
Rates were calculated at the index admission level. The denominator was the total number of beneficiary–index admission pairs, and the numerator was the number of beneficiary–readmission pairs.
Includes partial and full coverage.
Calculated using information at the ZIP code level from the U.S. Census Bureau.
30-Day Readmission Rates
Unadjusted 30-day readmission rates were higher for patients in traditional Medicare than Medicare Advantage (17.1% vs. 16.6% for AMI, 21.7% vs. 21.4% for CHF, and 16.4% vs. 16.3% for pneumonia) (Table 1). However, after risk adjustment, the readmission rates were higher for patients in Medicare Advantage (17.2% vs. 16.9% for AMI, 21.7% vs. 21.4% for CHF, and 16.5% vs. 16.0% for pneumonia) (Table 2). The corresponding rate differences between Medicare Advantage and traditional Medicare were 0.3 percentage point (95% CI,0.1 to 0.5 percentage point; P = 0.002) for AMI, 0.3 percentage point (CI, 0.2 to 0.5 percentage point; P <0.001) for CHF, and 0.5 percentage point (CI, 0.4 to 0.6 percentage point; P < 0.001) for pneumonia (Table 2). Among hospitals in which both Medicare Advantage and traditional Medicare beneficiaries were admitted, readmission rates were higher for those in Medicare Advantage in 1098 of 2138 hospitals (51%) after AMI, 1721 of 3373 hospitals (51%) after CHF, and 1920 of 3720 hospitals (52%) after pneumonia.
Table 2.
Within-Hospital Effects of Medicare Advantage Versus Traditional Medicare on 30-Day Readmission After AMI, CHF, or Pneumonia
| Condition | Risk-Adjusted Readmission Rates (95% CI), %* | Rate Difference (95% CI), percentage points | ||
|---|---|---|---|---|
| Medicare Advantage | Traditional Medicare | Within-Hospital Effect of Medicare Advantage vs. Traditional Medicare | P Value | |
| AMI | 17.2(17.0–17.4) | 16.9(16.8–17.0) | 0.3(0.1–0.5) | 0.002 |
| CHF | 21.7(21.6–21.9) | 21.4(21.3–21.5) | 0.3(0.2–0.5) | <0.001 |
| Pneumonia | 16.5(16.4–16.7) | 16.0(15.9–16.1) | 0.5 (0.4–0.6) | <0.001 |
AMI = acute myocardial infarction; CHF = congestive heart failure.
Adjusted for age, sex, condition-specific comorbid conditions, socioeconomic status (at the area level rather than the patient level), dual Medicare–Medicaid coverage status, race/ethnicity, and year of hospitalization.
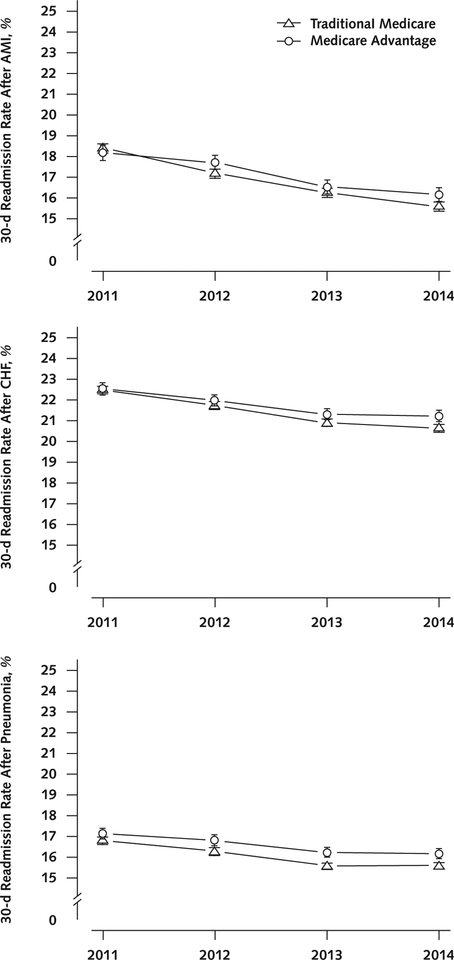
Changes Over Time
With the exception of AMI in 2011, adjusted read-mission rates were higher for Medicare Advantage beneficiaries for each condition in all other years (Figure 1). For AMI, the 30-day readmission rate was 0.2 percentage point (CI, −0.2 to 0.6 percentage point) higher for traditional Medicare beneficiaries than for Medicare Advantage beneficiaries in 2011; however, Medicare Advantage beneficiaries experienced higher rates of readmission than did traditional Medicare beneficiaries in each subsequent year (Figure 1, top), with the largest difference in 2014 (0.6 percentage point [CI, 0.2 to 0.9 percentage point]). For CHF, the adjusted difference in readmission rates between Medicare Advantage and traditional Medicare increased from 0.1 percentage point (CI, −0.2 to 0.4 percentage point) in 2011 to 0.6 percentage point (CI, 0.3 to 0.9 percentage point) in 2014 (Figure 1, middle). For pneumonia, adjusted differences between Medicare Advantage and traditional Medicare beneficiaries increased from 0.3 percentage point (CI, 0.1 to 0.6 percentage point) in 2011 to 0.6 percentage point (CI, 0.3 to 0.8 percentage point) in 2014 (Figure 1, bottom).
Figure.1.
Time trends in 30-day readmission rates after AMI (top), CHF (middle), and pneumonia (bottom) in Medicare Advantage and traditional Medicare.
AMI = acute myocardial infarction; CHF = congestive heart failure.
Sensitivity and Subgroup Analyses
The E-values for these associations were modest. An unmeasured covariate would have to be associated with both Medicare Advantage enrollment and read-mission risk with relative effects of 1.18 for AMI, 1.21 or1.42 for CHF, and 1.23 for pneumonia to explain the superiority estimates for traditional Medicare observed here and lead to the finding that traditional Medicare is inferior to Medicare Advantage at the degrees of associations observed in previous studies.
Patients in Medicare Advantage had lower expected risk for readmission than those in traditional Medicare for all 3 conditions (Supplement Figures 1 to 5, available at Annals.org). Additional sensitivity analyses appear in the Supplement and in Supplement Tables 7 to 9 (available at Annals.org).
Discussion
Using a novel linkage between MedPAR and HEDIS records, we found that, between 2011 and 2014, HEDIS data underreported hospital admissions for 3 common medical conditions, and admissions that were incorrectly excluded had higher readmission rates than those that appeared in HEDIS data. Despite this, in analyses using the linkage of HEDIS and MedPAR, Medicare Advantage beneficiaries had higher 30-day risk-adjusted readmission rates after AMI, CHF, and pneumonia than did traditional Medicare beneficiaries. Of note, not only were readmission rates higher for Medicare Advantage than traditional Medicare beneficiaries for each condition in all 4 years (except AMI in 2011), but the difference increased between 2011 and 2014, a period that included early implementation of the HRRP and initiation of financial penalties in October 2012. By 2014, we detected an increase in readmission rates of 0.5 to 0.6 percentage point in Medicare Advantage compared with traditional Medicare. This represents a meaningful difference given that, between 2007 and 2015, readmission rates in the traditional Medicare population for the 3 conditions decreased by 3.7 percentage points (4). These differences translate to an excess of approximately 2700 readmissions for AMI, 6000 readmissions for CHF, and 12 000 readmissions for pneumonia for patients in Medicare Advantage during the study period.
Although unadjusted readmission rates were higher for traditional Medicare beneficiaries, the direction of the difference reversed after standardization. This occurred because Medicare Advantage beneficiaries have, on average, a lower expected readmission risk (that is, they are “healthier”). Prior studies have documented that Medicare Advantage plans enroll beneficiaries with fewer comorbid conditions and that high-cost beneficiaries switch from Medicare Advantage to traditional Medicare (32, 33). Our sensitivity analysis using E-values showed that a covariate with moderate association in Medicare Advantage enrollment (relative risk of at least 1.2 for AMI, 1.4 for CHF, or 1.2 for pneumonia) is required to reduce the observed association between Medicare Advantage enrollment and readmission risk to previously reported associations (30, 34). The magnitudes of these E-values imply that the previously reported differences in readmission rates between Medicare Advantage and traditional Medicare and the ones presented in our study are not large in absolute terms; however, when contextualized in a large cohort and relative to the national decreases in readmission rates over time (4), they have important policy implications (34, 35).
The higher readmission rates in Medicare Advantage are unlikely to be influenced by hospital characteristics. Our within-hospital analyses compared outcomes for patients in Medicare Advantage and those in traditional Medicare admitted to the same hospitals, thus accounting for such a hospital effect. Similarly, our findings are not likely to be attributable to differences in observation stays because prior research has found that such stays do not explain the reduction in readmissions in the traditional Medicare program, and their frequency has increased similarly in Medicare Advantage and traditional Medicare (4, 36, 37).
Our results contrast with those of previous studies that have reported lower (7, 9, 38) or statistically similar (8) readmission rates for Medicare Advantage beneficiaries. Our findings may have differed for 4 main reasons. First, we used more comprehensive data than prior studies (7, 8), which relied exclusively on Med-PAR. Using MedPAR alone could miss readmissions for patients in Medicare Advantage readmitted to a hospital that did not report MedPAR data. Our approach captured readmissions that did not generate a MedPAR record but were available in the Medicare Advantage plans’ HEDIS data. Second, our analyses included co-morbid conditions from a well-validated model applied by CMS (16), which we enriched with additional covariates, including socioeconomic status, race/ethnicity, and dual Medicare–Medicaid coverage. Third, we included national data and focused on the 3 conditions that were publicly reported and included in the HRRP from 2011 to 2014. Fourth, 2 prior investigations (7, 9) focused on readmissions among patients discharged to skilled-nursing facilities or inpatient rehabilitation facilities. The association of Medicare Advantage enrollment with readmission may vary across different clinical conditions and postacute settings.
Rigorous comparison of clinical performance in Medicare Advantage and traditional Medicare is a first-order health policy priority because federal policy has stimulated enrollment of beneficiaries in Medicare Advantage plans. Forty percent of all Medicare beneficiaries are projected to be enrolled in Medicare Advantage by 2028 (10, 39). The Medicare Payment Advisory Commission has estimated that payments for Medicare Advantage beneficiaries, which were $210 billion in 2017, are higher than those for comparable traditional Medicare beneficiaries (6, 40, 41). Therefore, our study suggests the need to track outcomes for patients in both insurance programs using comparable methods, data sources, and risk-adjustment approaches (42).
Our findings also have important implications for reporting of readmission data and other HEDIS quality metrics for Medicare Advantage plans. As in our previous analysis of another HEDIS measure (18), we found that Medicare Advantage plans’ HEDIS data on read-missions seemed to be inaccurate. Plans incorrectly excluded hospitalizations that should have qualified for the readmission measure, and readmission rates were substantially higher among incorrectly excluded hospitalizations. These findings are concerning because CMS uses HEDIS performance to construct composite quality ratings and assign payment bonuses to Medicare Advantage plans. Our study suggests a need for improved monitoring of the accuracy of HEDIS data, particularly the measures’ denominators.
Our study had limitations. First, although we used a claims-based risk-standardization approach similar to that used by CMS, claims data do not include detailed measures of health status, function, illness severity, and social determinants. Second, our study could not identify the causal mechanisms driving the observed differences in readmission rates between Medicare Advantage and traditional Medicare. Third, although we used more comprehensive data sources than prior studies, some readmissions may not have been captured for patients in Medicare Advantage and comorbid conditions may not have been equally recorded in Medicare Advantage and traditional Medicare data. However, Medicare Advantage plans reimburse hospitals using the same payment methods and rates as traditional Medicare, which presumably would reduce incentives for a given hospital to code comorbid conditions differently for patients in Medicare Advantage and those in traditional Medicare admitted with the same condition (43). Fourth, our findings apply to index hospitalizations in hospitals that report data for patients in Medicare Advantage; these hospitals account for 92% of all admissions for traditional Medicare beneficiaries (7). Fifth, our data lacked detailed information on the type of Medicare Advantage plan and did not extend beyond 2014. Sixth, Medicare Advantage plans incorrectly excluded index admissions in HEDIS, and MedPAR may miss some readmissions for Medicare Advantage but not traditional Medicare. This potential flaw in the CMS data would imply that our estimated readmission rates in Medicare Advantage might be conservative, representing a lower bound of the underestimated Medicare Advantage rates. Finally, use of area-level socioeconomic data can result in measurement error and incomplete adjustment, and measurement errors in covariates can bias results in either direction (44, 45).
Overall, despite underreporting of readmissions in HEDIS data and incomplete ascertainment of readmissions for Medicare Advantage beneficiaries in MedPAR data, we found no evidence that readmission rates for 3 common medical conditions were higher in traditional Medicare than in Medicare Advantage. Patients in traditional Medicare discharged between 2011 and 2014 with a primary diagnosis of AMI, CHF, or pneumonia did not have higher risk-adjusted rates of readmission within 30 days than patients in Medicare Advantage. Incorporating outcomes for Medicare Advantage beneficiaries into hospital performance measures would allow for more comprehensive quality assessments.
Supplementary Material
Acknowledgment:
The authors thank Kirsten R. Voorhies, BS, and Derek Lake, MSc (Brown University), for their help with figures.
Financial Support:
By grants R01AG047180 and P01AG027296 from the National Institute on Aging of the National Institutes of Health.
Disclosures:
Dr. Keohane reports grants from the National Institute on Aging during the conduct of the study. Dr. Rivera-Hernandez reports grants from the National Institute on Aging and the National Institute of General Medical Sciences during the conduct of the study. Dr. Mor reports personal fees from HCR ManorCare and naviHealth outside the submitted work. Dr. Trivedi reports grants from the National Institute on Aging during the conduct of the study. Authors not named here have disclosed no conflicts of interest. Disclosures can also be viewed at www.acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum=M181795.
Footnotes
Publisher's Disclaimer: Disclaimer: The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the U.S. government.
Reproducible Research Statement: Study protocol and data set: Not available. Statistical code: Available from Dr. Panagiotou (e-mail, orestis_panagiotou@brown.edu).
References
- 1.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–28. [PMID: 19339721] doi: 10.1056/NEJMsa0803563 [DOI] [PubMed] [Google Scholar]
- 2.Hines AL, Barrett ML, Jiang HJ, Steiner CA. Conditions With the Largest Number of Adult Hospital Readmissions by Payer, 2011. Rockville: Agency for Healthcare Research and Quality; 2014. [PubMed] [Google Scholar]
- 3.Wasfy JH, Zigler CM, Choirat C, Wang Y, Dominici F, Yeh RW. Readmission rates after passage of the Hospital Readmissions Reduction Program: a pre-post analysis. Ann Intern Med. 2017;166: 324–31. [PMID: 28024302] doi: 10.7326/M16-0185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, observation, and the Hospital Readmissions Reduction Program. N Engl J Med. 2016;374:1543–51. [PMID: 26910198] doi: 10.1056/NEJMsa1513024 [DOI] [PubMed] [Google Scholar]
- 5.Jacobson G, Damico A, Neuman T, Gold M. Medicare Advantage 2017 Spotlight: Enrollment Market Update. Washington, DC: The Henry J. Kaiser Family Foundation; June 2017. Accessed at www.kff.org/medicare/issue-brief/medicare-advantage-2017-spotlight-enrollment-market-updateon15April2019. [Google Scholar]
- 6.The Henry J Kaiser Family Foundation. Medicare Advantage . Washington, DC: The Henry J. Kaiser Family Foundation; 2017. Accessed at www.kff.org/medicare/fact-sheet/medicare-advantageon15April2019. [Google Scholar]
- 7.Huckfeldt PJ, Escarce JJ, Rabideau B, Karaca-Mandic P, Sood N. Less intense postacute care, better outcomes for enrollees in Medicare Advantage than those in fee-for-service. Health Aff (Millwood). 2017;36:91–100. [PMID: 28069851] doi: 10.1377/hlthaff.2016.1027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Henke RM, Karaca Z, Gibson TB, Cutler E, Barrett ML, Levit K, et al. Medicare Advantage and traditional Medicare hospitalization intensity and readmissions. Med Care Res Rev. 2018;75:434–53. [PMID: 29148332] doi: 10.1177/1077558717692103 [DOI] [PubMed] [Google Scholar]
- 9.Kumar A, Rahman M, Trivedi AN, Resnik L, Gozalo P, Mor V. Comparing post-acute rehabilitation use, length of stay, and outcomes experienced by Medicare fee-for-service and Medicare Advantage beneficiaries with hip fracture in the United States: a secondary analysis of administrative data. PLoS Med. 2018;15:e1002592 [PMID: 29944655] doi: 10.1371/journal.pmed.1002592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Neuman P, Jacobson GA. Medicare Advantage checkup. N Engl J Med. 2018;379:2163–72. [PMID: 30428276] doi: 10.1056/NEJMhpr1804089 [DOI] [PubMed] [Google Scholar]
- 11.Research Data Assistance Center. Differences between the inpatient and MedPAR files. 2016. Accessed at www.resdac.org/articles/differences-between-inpatient-and-medpar-fileson1May2019.
- 12.Research Data Assistance Center. Identifying Medicare managed care beneficiaries from the master beneficiary summary or denominator files. 2011. Accessed at www.resdac.org/articles/identifying-medicare-managed-care-beneficiaries-master-beneficiary-summary-or-denominatoron1May2019. [Google Scholar]
- 13.Krumholz HM, Lin Z, Drye EE, Desai MM, Han LF, Rapp MT, et al. An administrative claims measure suitable for profiling hospital performance based on 30-day all-cause readmission rates among patients with acute myocardial infarction. Circ Cardiovasc Qual Outcomes. 2011;4:243–52. [PMID: 21406673] doi: 10.1161/CIRCOUTCOMES.110.957498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Keenan PS, Normand SL, Lin Z, Drye EE, Bhat KR, Ross JS, et al. An administrative claims measure suitable for profiling hospital performance on the basis of 30-day all-cause readmission rates among patients with heart failure. Circ Cardiovasc Qual Outcomes. 2008; 1:29–37. [PMID: 20031785] doi: 10.1161/CIRCOUTCOMES.108.802686 [DOI] [PubMed] [Google Scholar]
- 15.Lindenauer PK, Normand SL, Drye EE, Lin Z, Goodrich K, Desai MM, et al. Development, validation, and results of a measure of 30-day readmission following hospitalization for pneumonia. J Hosp Med. 2011;6:142–50. [PMID: 21387551] doi: 10.1002/jhm.890 [DOI] [PubMed] [Google Scholar]
- 16.Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation. 2016 Condition-Specific Measures Updates and Specifications Report: Hospital-Level 30-Day Risk-Standardized Readmission Measures. Baltimore: Centers for Medicare & Medicaid Services; 2016. [Google Scholar]
- 17.Cooper AL, Kazis LE, Dore DD, Mor V, Trivedi AN. Underreporting high-risk prescribing among Medicare Advantage plans: a cross-sectional analysis. Ann Intern Med. 2013;159:456–62. [PMID: 24081286] doi: 10.7326/0003-4819-159-7-201310010-00005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krieger N Overcoming the absence of socioeconomic data in medical records: validation and application of a census-based methodology. Am J Public Health. 1992;82:703–10. [PMID: 1566949] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barnett ML, Hsu J, McWilliams JM. Patient characteristics and differences in hospital readmission rates. JAMA Intern Med. 2015; 175:1803–12. [PMID: 26368317] doi: 10.1001/jamainternmed.2015.4660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gornick ME, Eggers PW, Reilly TW, Mentnech RM, Fitterman LK, Kucken LE, et al. Effects of race and income on mortality and use of services among Medicare beneficiaries. N Engl J Med. 1996;335: 791–9. [PMID: 8703185] [DOI] [PubMed] [Google Scholar]
- 21.Martsolf GR, Barrett ML, Weiss AJ, Kandrack R, Washington R, Steiner CA, et al. Impact of race/ethnicity and socioeconomic status on risk-adjusted hospital readmission rates following hip and knee arthroplasty. J Bone Joint Surg Am. 2016;98:1385–91. [PMID: 27535441] doi: 10.2106/JBJS.15.00884 [DOI] [PubMed] [Google Scholar]
- 22.Centers for Medicare & Medicaid Services. Hospital-Wide All-Cause Unplanned Readmission Measure (HWR). Baltimore: Centers for Medicare & Medicaid Services; 2015. [Google Scholar]
- 23.Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation. Testing Publicly Reported 30-Day Acute Myocardial Infarction, Heart Failure, and Pneumonia Risk-Standardized Mortality and Readmission Measures in California All-Payer Data. Baltimore: Centers for Medicare & Medicaid Services; 2011. [Google Scholar]
- 24.Centers for Medicare & Medicaid Services. Hospital-Wide All-Cause Unplanned Readmission Measure (HWR). Baltimore: Centers for Medicare & Medicaid Services; 2012. [Google Scholar]
- 25.Neuhaus JM, Kalbfleisch JD. Between- and within-cluster covariate effects in the analysis of clustered data. Biometrics. 1998;54:638–45. [PMID: 9629647] [PubMed] [Google Scholar]
- 26.Williams R Using the margins command to estimate and interpret adjusted predictions and marginal effects. Stata J. 2012;12: 308–31. [Google Scholar]
- 27.Muller CJ, MacLehose RF. Estimating predicted probabilities from logistic regression: different methods correspond to different target populations. Int J Epidemiol. 2014;43:962–70. [PMID: 24603316] doi: 10.1093/ije/dyu029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sato T, Matsuyama Y. Marginal structural models as a tool for standardization. Epidemiology. 2003;14:680–6. [PMID: 14569183] [DOI] [PubMed] [Google Scholar]
- 29.Localio AR, Berlin JA, Ten Have TR, Kimmel SE. Adjustments for center in multicenter studies: an overview. Ann Intern Med. 2001; 135:112–23. [PMID: 11453711] [DOI] [PubMed] [Google Scholar]
- 30.VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167:268–74. [PMID: 28693043] doi: 10.7326/M16-2607 [DOI] [PubMed] [Google Scholar]
- 31.Localio AR, Stack CB, Griswold ME. Sensitivity analysis for un-measured confounding: E-values for observational studies [Editorial]. Ann Intern Med. 2017;167:285–6. [PMID: 28693037] doi: 10.7326/M17-1485 [DOI] [PubMed] [Google Scholar]
- 32.Morgan RO, Virnig BA, DeVito CA, Persily NA. The Medicare-HMO revolving door—the healthy go in and the sick go out. N Engl J Med. 1997;337:169–75. [PMID: 9219704] [DOI] [PubMed] [Google Scholar]
- 33.Rahman M, Keohane L, Trivedi AN, Mor V. High-cost patients had substantial rates of leaving Medicare Advantage and joining traditional Medicare. Health Aff (Millwood). 2015;34:1675–81. [PMID: 26438743] doi: 10.1377/hlthaff.2015.0272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ioannidis JPA, Tan YJ, Blum MR. Limitations and misinterpretations of E-values for sensitivity analyses of observational studies. Ann Intern Med. 2019. [PMID: 30597486] doi: 10.7326/M18-2159 [DOI] [PubMed] [Google Scholar]
- 35.VanderWeele TJ, Mathur MB, Ding P. Correcting misinterpretations of the E-value. Ann Intern Med. 2019;170:131–2. [PMID: 30597489] doi: 10.7326/M18-3112 [DOI] [PubMed] [Google Scholar]
- 36.Mechanic R Post-acute care—the next frontier for controlling Medicare spending. N Engl J Med. 2014;370:692–4. [PMID: 24552315] doi: 10.1056/NEJMp1315607 [DOI] [PubMed] [Google Scholar]
- 37.Lind KD, Noel-Miller CM, Sangaralingham LR, Shah ND, Hess EP, Morin P, et al. Increasing trends in the use of hospital observation services for older Medicare Advantage and privately insured patients. Med Care Res Rev. 2019;76:229–39. [PMID: 29148348] doi: 10.1177/1077558717718026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Friedman B, Jiang HJ, Steiner CA, Bott J. Likelihood of hospital readmission after first discharge: Medicare Advantage vs. fee-for-service patients. Inquiry. 2012;49:202–13. [PMID: 23230702] [DOI] [PubMed] [Google Scholar]
- 39.Medicare—CBO’s April 2018 baseline. Accessed at www.cbo.gov/sites/default/files/recurringdata/51302-2018-04-medicare.pdfon1May2019.
- 40.Frakt AB. The cost of Medicare Advantage. JAMA. 2016;315: 2387–8. [PMID: 27299607] doi: 10.1001/jama.2016.6790 [DOI] [PubMed] [Google Scholar]
- 41.Medicare Payment Advisory Commission. Report to Congress: Medicare Payment Policy. Washington, DC: Medicare Payment Advisory Commission; 2017. [Google Scholar]
- 42.Brennan N, Ornstein C, Frakt AB. Time to release Medicare Advantage claims data. JAMA. 2018;319:975–6. [PMID: 29459940] doi: 10.1001/jama.2017.21519 [DOI] [PubMed] [Google Scholar]
- 43.Berenson RA, Sunshine JH, Helms D, Lawton E. Why Medicare Advantage plans pay hospitals traditional Medicare prices. Health Aff (Millwood). 2015;34:1289–95. [PMID: 26240241] doi: 10.1377/hlthaff.2014.1427 [DOI] [PubMed] [Google Scholar]
- 44.Stefanski LA, Carroll RJ. Covariate measurement error in logistic-regression. Ann Stat. 1985;13:1335–51. [Google Scholar]
- 45.Keogh RH, White IR. A toolkit for measurement error correction, with a focus on nutritional epidemiology. Stat Med. 2014;33:2137–55. [PMID: 24497385] doi: 10.1002/sim.6095 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.