Abstract
Background:
Safety-net hospitals have higher-than-expected readmission rates. The relative roles of the mean disadvantage of neighborhoods the hospitals serve and the disadvantage of individual patients in predicting a patient’s readmission are unclear.
Objective:
To examine the independent contributions of the patient’s neighborhood and the hospitals service area to risk for 30-day readmission.
Design:
Retrospective observational study.
Setting:
Maryland.
Participants:
All Maryland residents discharged from a hospital in 2015.
Measurements:
Predictors included the disadvantage of neighborhoods for each Maryland resident (area disadvantage index) and the mean disadvantage of each hospital’s discharged patients (safety-net index). The primary outcome was unplanned 30-day hospital readmission. Generalized estimating equations and marginal modeling were used to estimate readmission rates. Results were adjusted for clinical readmission risk.
Results:
13.4% of discharged patients were readmitted within 30 days. Patients living in neighborhoods at the 90th percentile of disadvantage had a readmission rate of 14.1% (95% CI, 13.6% to 14.5%) compared with 12.5% (CI, 11.8% to 13.2%) for similar patients living in neighborhoods at the 10th percentile. Patients discharged from hospitals at the 90th percentile of safety-net status had a readmission rate of 14.8% (CI, 13.4% to 16.1%) compared with 11.6% (CI, 10.5% to 12.7%) for similar patients discharged from hospitals at the 10th percentile of safety-net status. The association of readmission risk with the hospital’s safety-net index was approximately twice the observed association with the patient’s neighborhood disadvantage status.
Limitations:
Generalizability outside Maryland is unknown. Confounding may be present.
Conclusion:
In Maryland, residing in a disadvantaged neighborhood and being discharged from a hospital serving a large proportion of disadvantaged neighborhoods are independently associated with increased risk for readmission.
Primary Funding Source:
The National Institute on Minority Health and Health Disparities and the Maryland Health Services Cost Review Commission.
Safety-net hospitals—those caring for large numbers of severely disadvantaged patients—are likely to have higher 30-day readmission rates and therefore to incur more penalties under Medicare’s Hospital Readmissions Reduction Program (1, 2). These penalties have fueled controversy about whether the higher readmission rates result from ineffective care in safety-net hospitals, which would make penalties more consistent with the intent of the program, or from challenges associated with serving severely disadvantaged populations, which would be inconsistent with the program’s intent.
The effect of socioeconomic factors on individual health status and health care delivery and costs is a growing policy issue as policymakers try to find approaches for addressing this problem. The Improving Medicare Post-Acute Care Transformation Act of 2014 (3) directed the U.S. Secretary of Health and Human Services to conduct “a study that examines the effect of individuals’ socioeconomic status on quality measures and resource use….” The Secretary has delivered the first of 2 reports to Congress (4), and the National Academy of Medicine has released a 5-part report titled “Taking Account of Socioeconomic Factors in Medicare Reimbursement” (5). Per the 21st Century Cures Act (6), the Secretary created readmission penalties stratified by the fraction of a hospital’s Medicare beneficiaries who are also eligible for Medicaid. This requirement was implemented for fiscal year 2019 (7).
This study examined whether readmission risk is associated with the area disadvantage index (ADI) of the neighborhood where the patient lives and the safety-net index (mean ADI) of the hospital providing treatment. Our analysis focused on data from Maryland, which has a unique hospital rate-setting system, one of whose aims is to decrease financial risks for hospitals that serve disadvantaged patients. We sought to answer 3 questions. First, is readmission risk higher for a patient from a more disadvantaged neighborhood (one with a higher mean ADI) after the hospital’s safety-net index and clinical factors are controlled for? Second, is readmission risk higher for a patient treated in a hospital with a higher mean ADI (safety-net index) after the neighborhood disadvantage of the patient and clinical factors are controlled for? Third, what are the relative strengths of hospital safety-net index and neighborhood disadvantage as predictors of readmission?
Methods
Overview
We used Maryland’s fiscal year 2015 (1 July 2014 to 30 June 2015) discharge data for this observational study. This analysis was initiated and largely completed as an internal Maryland Health Services Cost Review Commission (MHSCRC) study of whether to use the ADI in the hospital rate-setting process. Thus, in accordance with the MHSCRC and federal (8) policy, the study was exempt from institutional review board approval.
Data Sources and Study Population
We used data from Maryland’s unique all-payer hospital rate-setting system (9–11). Each hospital’s revenues are regulated and each hospital’s charges are essentially the same for patients with Medicare, Medicaid, commercial insurance, and no insurance. Noncollectible charges are pooled, and their burden is shared among all hospitals. During the study, Maryland was also transitioning to regulated global hospital budgets.
An important goal of this system is to minimize the financial risk to hospitals that serve disadvantaged patients. That risk has been blamed for effectiveness of care problems attributed to safety-net hospitals. To measure hospitals’ financial health, we obtained operating profit margins for all hospitals from MHSCRC’s audited cost report data (12). Operating profit margins exclude physician costs and income, philanthropy, and other elements that may vary substantially among hospitals. Although 1 reason for this study was to assess the fairness of Medicare penalties, we could not duplicate Medicare’s risk adjustment methods in our calculations.
All Maryland hospitals report information on all discharges, regardless of source of payment, to the MHSCRC. The database has a unique identifier for each patient, which links admissions and readmissions across hospitals and with the neighborhood where the patient lives. We analyzed data from all discharges for all Maryland residents except newborns, patients who were transferred to another acute care hospital, and those who died.
Predictor Measures
Neighborhood ADI
The ADI, which was developed by Singh and Siahpush (13) and Singh (14) and was updated by Kind (15), Hu (16), and their respective colleagues, combines 17 measures of income, employment, education, and housing collected in the 2009–2013 American Community Survey (17). Kind and colleagues (15) found that, in a national Medicare fee-for-service sample, patients who were discharged with pneumonia, heart failure, and myocardial infarction and who lived in the most disadvantaged 15% of neighborhoods had increased risk for 30-day readmission, even after extensive clinical risk adjustment.
A team at the University of Wisconsin led by 1 of the authors (A.J.H.K.) has computed the ADI for each neighborhood (technically, each census block group) in the United States (18). Each neighborhood received a percentile ranking (with minimum disadvantage in the first percentile and maximum disadvantage in the 100th percentile) that was weighted so that each percentile had the same number of discharges. We applied these neighborhood ADI estimates to each discharge in our data set.
Hospital Safety-Net Index
We defined a hospital’s safety-net index as the mean disadvantage (ADI) of its discharged patients, which is a measure of the weighted mean disadvantage of the neighborhoods from which it draws admissions.
Clinical Readmission Risk Index (Case-Mix Index)
Maryland uses the 3M Health Systems All Patient Refined Diagnosis-Related Groups (APR-DRGs)/Severity of Illness index (19, 20) to perform risk adjustment of discharges. The APR-DRGs assigns each discharge to 1 of 314 DRGs on the basis of the reason for admission and to 1 of 4 levels of severity on the basis of diagnoses and other hospital discharge data, for a total of 1256 cells. The case-mix index is the expected readmission rate per 100 discharges, based on Maryland’s 2014 statewide readmission rates for each APR-DRG cell. We excluded discharges assigned to cells with fewer than 2 cases in either 2014 or 2015.
Outcome Measure
The primary outcome was unplanned 30-day hospital readmission, which we defined as any admission within 1 to 30 days after a discharge that was identified as unplanned using the Yale–Centers for Medicare & Medicaid Services algorithm (21). The algorithm primarily identifies admissions as planned if they are in certain categories (such as chemotherapy or obstetric delivery) or for a procedure without an acute diagnosis. We could not identify readmissions to or from hospitals outside Maryland. We defined the hospital readmission rate as the number of readmissions to any Maryland hospital per 100 discharges.
Statistical Analysis
We sought to estimate the independent association of ADI and safety-net index with readmission after controlling for clinical risk factors and to compare the relative size of these effects. Our basic approach used generalized estimating equations (GEEs) with marginal modeling. This approach treats clustering effects as nuisance effects and does not estimate cluster-specific values. A key question in the analysis of clustered data, such as patients or discharges nested within hospitals, is whether to center covariates of interest. Hospital-specific centering is difficult to interpret in this framework. Following the methods of Begg and Parides (22) and Enders and Tofighi (23), we addressed this issue by specifying safety-net index as the mean ADI percentile for patients discharged from a given hospital. We specified individual ADI as the raw (uncentered) value for that patient’s neighborhood.
We modeled ADI and safety-net index as continuous values rather than categorical measures because diagnostic plots suggested that the association of ADI and safety-net index with readmission risk is linear. To ease interpretation and comparison of coefficients across covariates, we scaled ADI, safety-net index, and case-mix index so that the regression coefficient reflected an increase of 10 units in each covariate.
Fitting a traditional regression model to clustered data usually produces biased SEs. The investigator may use a hierarchical or random-effects approach, which explicitly models the clustering and, depending on the specification, estimates an intercept for each cluster and may estimate a cluster-specific slope for 1 or more covariates. Although such models have many strengths, when applied to binary outcomes they result in regression coefficients that must be interpreted as the effect of a covariate on observations within the same cluster or hospital. This led us to specify a model using a GEE, which yields regression coefficients that may be interpreted as the effect of an explanatory variable after other covariates are controlled for. The GEE models treat correlation of observations within clusters as a nuisance rather than as parameters of analytic interest to be estimated with the model. The GEE models produce regression coefficients of similar magnitude to those from the same class of traditional regression model but adjust the SEs (generally in a positive direction) to account for clustering (24).
We fit a GEE model specifying a Poisson distribution (25). A log-binomial specification, which is a common choice for estimating relative risks with binary data, such as readmissions, did not converge.
We modeled the probability of readmission using covariates reflecting the patient’s ADI, the hospital’s mean ADI, the patient’s case-mix index, and an error term for each patient discharge using the equation:
where i indexes discharges, j indexes hospitals, α is the intercept reflecting mean probability of readmission, and e is a discharge-specific error term.
We evaluated sensitivity of the ADI and safety-net index coefficients to inclusion of a hypothetical unmeasured confounder using the method of VanderWeele and Ding (26).
Cluster-robust SEs can be biased downward with data sets containing fewer than 50 clusters. Because our data set contained 47 clusters, we compared the cluster-robust results with those from a multilevel Poisson model with a random intercept for hospital.
Results
In fiscal year 2015, Maryland had 5 832 291 residents living in 3908 neighborhoods with a mean population of 1492. There were 47 acute care hospitals with 633 989 discharges, of which 144 632 were excluded (Table 1), leaving 489 357 for analysis; 65 698 (13.4% of all discharges) were readmissions. Of the discharges used for analysis, fewer than half would have appeared in an analysis limited to Medicare data. Severely disadvantaged neighborhoods were concentrated in urban Baltimore, which has about 10% of Maryland’s population (27); rural areas, such as the Appalachian region of western Maryland and the agricultural eastern shore of the Chesapeake Bay; and some suburbs (Figure 1).
Table 1.
Geographic Variation in ADI in Maryland 2010–2013
| Variable | Value |
|---|---|
| Payer, % | |
| Medicare | 33.7 |
| Medicaid | 24.1 |
| Medicare and Medicaid | 9.8 |
| Commercial and Blue Cross | 29.2 |
| Self/uninsured/other | 3.6 |
| Final analytic data set, % | 100.0 |
| Total discharges, n | 633 989 |
| Exclusions, n | |
| Not Maryland resident | 40 972 |
| Neonate | 67 410 |
| Transfer | 18 288 |
| Died | 11 799 |
| No valid identifier | 143 |
| No ADI | 6002 |
| No case-mix index | 297 |
| Total | 144 632 |
| Final analytic data set, n | 489 357 |
ADI = area deprivation index.
Figure 1.
Variation in ADI in Maryland. Data are from 2010–2013, the most recent data set available when the analysis was performed (13). ADI = area disadvantage index.
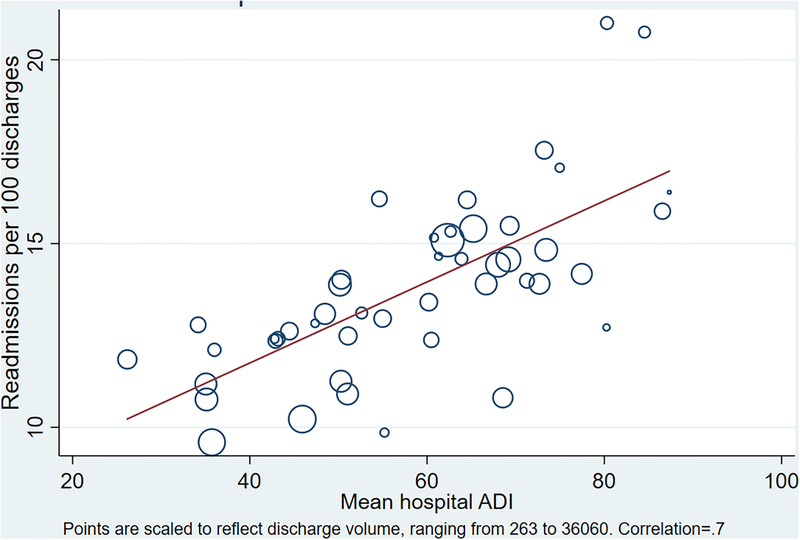
The mean ADI of all Maryland discharges was 57.0. The mean ADI for Maryland residents was 50, indicating that patients from disadvantaged neighborhoods were overrepresented in discharges. The unweighted mean of hospital safety-net index values was 58.5. Figure 2 shows that the readmission rate for Maryland hospitals is strongly associated with the safety-net index even after clinical adjustment.
Figure 2.
Relationship between hospital safety-net index and adjusted readmission rate. Hospital safety-net index is the mean ADI for a hospital’s discharges. Readmission rates were indirectly adjusted for case mix to the statewide average. Points are scaled to reflect discharge volume, which ranged from 263 to 36 060. Correlation = 0.7. ADI = area disadvantage index.
Table 2 shows marginal probabilities of readmission at various levels of safety-net index and ADI. Patients living in neighborhoods at the 90th percentile of disadvantage had a readmission rate of 14.1% (95% CI, 13.6% to 14.5%) compared with 12.5% (CI, 11.8% to 13.2%) for similar patients living in neighborhoods at the 10th percentile. Patients discharged from hospitals at the 90th percentile of safety-net status had a readmission rate of 14.8% (CI, 13.4% to 16.1%) compared with 11.6% (CI, 10.5% to 12.7%) for similar patients discharged from hospitals at the 10th percentile of safety-net index. Thus, the difference in risk associated with moving from the 10th to the 90th percentile of safety-net index (3.2 percentage points [11.6% vs. 14.8%]) was about twice the difference associated with moving from the 10th to the 90th percentile of ADI (1.6 percentage points [12.5% vs. 14.1%]).
Table 2.
Readmission Risk at Different Percentiles of ADI and Safety-Net Index*
| Percentile | Marginal Effect† of Safety-Net Index at Specified Percentile (95% CI) | Marginal Effect† of ADI at Specified Percentile (95% CI) |
|---|---|---|
| 10th | 0.116 (0.105–0.127) | 0.125 (0.118–0.132) |
| 25th | 0.121 (0.113–0.129) | 0.128 (0.121–0.134) |
| 50th | 0.131 (0.126–0.135) | 0.132 (0.127–0.138) |
| 75th | 0.141 (0.132–0.150) | 0.137 (0.133–0.142) |
| 90th | 0.148 (0.134–0.161) | 0.141 (0.136–0.145) |
ADI = area deprivation index of patient’s residence.
Mean ADI among a hospital’s discharged patients.
Estimated with Stata/MP 15 (StataCorp) using the Poisson procedure, the cluster-robust SEs options, and hospital identifier as the clustering variable.
The E-value was 1.14 for ADI and 1.22 for safety-net index, indicating that the observed association between the outcome and the covariate could be explained by an unmeasured confounder with a modest association with both the outcome and the covariate (23). Estimating the amount of confounding necessary to shift an association to the null does not mean that such an unmeasured confounder exists. We estimated results similar to those using a random-effects model, indicating that our results were not biased by the limited number of clusters (hospitals).
Discussion
In Maryland, living in a disadvantaged neighborhood and being discharged from a hospital serving patients from disadvantaged neighborhoods are each independently associated with increased risk for readmission. These findings have practical implications. First, the effect of the neighborhoods in which patients live and which the hospital serves merits the clinician’s awareness because it is associated with readmission, an important clinical outcome. Second, although modest, these effects are similar to the national differences between hospitals that were penalized and those that were not. Third, the association of a hospital’s safety-net index with readmission rates is substantial even though operating profit margins are higher in Maryland hospitals with a high safety-net index. Fourth, the association of a patient’s neighborhood disadvantage with risk for readmission remains highly significant even after adjustment for hospital safety-net index.
In this analysis, we faced 2 methodological issues that are likely to become more important with growing emphasis on the population’s health. First, we emphasize neighborhood disadvantage rather than individual disadvantage because our data characterize neighborhoods, not individuals (28), and the 2 are not interchangeable. Soobader and colleagues (29) reported a correlation of 0.44 between the log of the median neighborhood income and the log of the income of individual residents and 0.41 between mean neighborhood education and individual education. Although statistically significant, these findings mean that neighborhood data predict less than 20% of individual variation in these variables. We should not assume that neighborhood disadvantage is associated with readmission simply because it is a proxy for individual disadvantage.
Public health research is replete with studies of how neighborhood characteristics mediate the link between disadvantage and health outcomes. Mediators include limited primary and urgent care services (30), pollution (31) and poor sanitation, crime (32) and community transience, lead paint and allergens, food deserts (33), and lack of transportation. Overall, the research shows that neighborhoods do affect health (34, 35).
The literature on preventing readmission focuses heavily on the transition from hospital to community (36), but in the weeks after this transition, the characteristics of the neighborhood play a growing role. Arbaje and colleagues (37) found that residents of disadvantaged neighborhoods are less likely to have community supports that would help them to stay out of the hospital. The Moving to Opportunity study (38) showed that diabetes and extreme obesity outcomes improved when participants moved to a more affluent neighborhood, even when the participant’s income did not change. If we see neighborhood disadvantage as no more than a proxy for individual disadvantage, we run 2 risks: We may miss powerful information about potentially remediable neighborhood problems, and we may become mired in unprofitable arguments about ecological fallacies.
A second methodological step is that characterizing a provider by the disadvantage of the neighborhoods it serves may be an important tool in population health analysis, especially if Medicaid continues to become less uniform or if we move toward a single-payer system. The idea that a hospital serves a community rather than individual patients is still evolving, and the mediators that make the safety-net index a predictor of readmission are still uncertain. The traditional explanations have been that safety-net hospitals are government-owned and not well run; are dependent on Medicare, Medicaid, and uninsured patients and therefore underfunded; and are filled with safety-net patients who have greater needs than other patients for whom payments are the same. Maryland has no government-owned hospitals. The MHSCRC’s cost reports showed a modest positive correlation (r = 0.23; P < 0.001) between safety-net index and hospital operating profit. This test is just 1 indicator of financial health but suggests that MHSCRC policy is successful in protecting hospitals from 1 type of financial risk that might be associated with elevated safety-net index.
This study had 2 limitations. First, our analyses focused on a single state. Figure 2 confirms that national findings of excess adjusted readmissions in safety-net hospitals are also present in Maryland and supports application of the findings to other states. However, Maryland has the highest median household income in the United States (39), while children in Baltimore have the worst earning prospects among the 50 largest U.S. cities (40). This diversity may make the effects of disadvantage easier to detect. Maryland’s hospital rate-setting system is also unique; thus, findings may differ in states where the financial status of safety-net hospitals is more precarious, where the financial incentives to prevent readmissions are different, or where hospital revenue is not largely set by the state. Testing our findings in other states should be a priority, but we acknowledge that some of our findings (such as the effects of protecting hospitals that serve disadvantaged patients) resulted from Maryland’s rate-setting experiment and will be hard to test elsewhere.
Second, our findings are subject to potential confounding. We measured neighborhood characteristics but not individual characteristics, such as socioeconomic status and race, which may be associated with ADI, safety-net index, and readmission. Our sensitivity analysis indicated that our study is at least moderately sensitive to such confounding. Although we adjusted for clinical risk, the case-mix index probably does not completely account for patient factors, such as disabilities (41), which may also be related to readmission. However, Kind and colleagues (15), Bernheim and associates (42), and we all found that disadvantage was associated with higher risk for readmission despite using different approaches to case mix (multivariate adjustment, the Centers for Medicare & Medicaid Services method, and APR-DRGs, respectively). Therefore, we doubt that further refinements of codes or algorithms would yield improvements of the magnitude needed to explain away our results.
We were motivated to conduct this study by concern for the fairness of readmission penalties for safety-net hospitals and patients from disadvantaged neighborhoods. Other researchers have addressed whether refined social and clinical measures would or should reduce or eliminate the penalties that safety-net hospitals face (43, 44). That is, in part, an ethical rather than a technical issue: Some are loath to adjust a policy that seems to accept inferior care and outcomes for disadvantaged persons, whereas others see such adjustments as the most practical way to level the playing field for hospitals that serve those patients.
Our analysis suggests that neighborhood disadvantage is associated with excess risk for readmission in 2 ways. One is the patient’s exposure to disadvantage in the neighborhood where they live and often recover after hospitalization. Individual patients bear this risk compared with patients from more advantaged neighborhoods treated in similar hospitals. The other, which is associated with roughly twice the variation in risk for readmission, is indirect, hospital-level exposure that can be measured by the mean disadvantage of a hospital’s discharged patients. This indirect exposure is largely independent of a patient’s direct exposure to neighborhood disadvantage and deserves further exploration.
This study clarifies the problem more than the solution, which may be paying more for care of patients from disadvantaged neighborhoods (4, 5, 45, 46), decreasing penalties, investing in improving neighborhoods (46, 47), or using a wait-and-see strategy. Although this report does not prove, or even assert, that disadvantaged neighborhoods are the major cause of excess readmissions, it adds to evidence that the association is too strong to ignore.
Demonstrating the association of risk for readmission both with patient exposure to neighborhood disadvantage and the collective disadvantage of a hospital’s patients does not tell us what mediates or causes those associations. We urgently need studies that clarify which of the mechanisms linking disadvantage and safety-net patients to readmissions are strongest and most likely to yield returns on investment in preventing readmissions.
Acknowledgment:
The authors thank Bill Buckingham for assistance with the ADI, Carol Hermann and Sarah Keller for assistance with manuscript formatting, and Talia Pindyck for critiquing the manuscript.
Financial Support: This project was supported by a National Institute on Minority Health and Health Disparities of the National Institutes of Health Award (R01MD010243 [principal investigator, Dr. Kind]. Drs. Jencks and Brock did not receive support for this work. Drs. Schuster, Dougherty, and Gerovich were employed by the MHSCRC. This material is the result of work also supported with resources and the use of facilities at the William S. Middleton Memorial Veterans Hospital Geriatric Research, Education and Clinical Center in Madison, Wisconsin (GRECC-Manuscript #2016–010), and the University of Wisconsin Department of Medicine.
Disclosures: Dr. Jencks reports personal fees and nonfinancial support from the Maryland Health Services Cost Review Commission during the conduct of the study and personal fees and nonfinancial support from the American College of Cardiology outside the submitted work. Dr. Brock reports being a full-time employee of Telligen and work under a quality improvement contract from the Centers for Medicare & Medicaid Services (CMS). In her quality improvement work, she used the area disadvantage index to guide implementation strategies that account for the effect of social determinants of health and to interpret performance measurement. The work done for this article did not use CMS data sources and was done outside of her contracted responsibilities. Dr. Brock also reports being the recipient of research funding originating with the Patient-Centered Outcomes Research Institute through a subcontract with the University of Kentucky to study patient preferences and provider activities to implement care transition improvements. Some of the analyses associated with this research also incorporated area disadvantage indices as adjustment factors. Dr. Kind reports grants from the National Institutes of Health during the conduct of the study and grants from the Commonwealth Fund and the U.S. Department of Veterans Affairs outside the submitted work. Authors not named here have disclosed no conflicts of interest. Disclosures can also be viewed at www.acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum=M16-2671.
Role of the Funding Source
This project was supported by a National Institute on Minority Health and Health Disparities of the National Institutes of Health Award (R01MD010243 [principal investigator, Dr. Kind]). This material is the result of work also supported with resources and use of facilities at the William S. Middleton Memorial Veterans Hospital Geriatric Research, Education and Clinical Center in Madison, Wisconsin, and the University of Wisconsin Department of Medicine. Because this study started as an MHSCRC internal analysis, the MHSCRC had a role in the design, conduct, data collection, management, and early analysis and interpretation of this work. The MHSCRC had no role in the final analysis or the preparation, review, or approval of the manuscript. The National Institutes of Health had no role in any of these functions.
Reproducible Research Statement: Study protocol: See the Methods section of the text. Statistical code: Available from Dr. Schuster (alyson.schuster@maryland.gov). Data set: Hospital-level data are largely available from the Maryland Health Services Cost Review Commission Web site (www.hscrc.state.md.us/pages/default.aspx). Census block group–level ADI estimates are available from reference 18. Person-level data are available only by special application to the Maryland Health Services Cost Review Commission.
Footnotes
Publisher's Disclaimer: Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, the U.S. Department of Veterans Affairs, the MHSCRC, or Telligen Colorado.
Contributor Information
Stephen F. Jencks, Baltimore, Maryland.
Alyson Schuster, Maryland Health Services Cost Review Commission, Baltimore, Maryland.
Geoff B. Dougherty, Maryland Health Services Cost Review Commission, Baltimore, Maryland.
Sule Gerovich, Mathematica Policy Research, Woodlawn, Maryland.
Jane E. Brock, Telligen Colorado, Greenwood Village, Colorado.
Amy J.H. Kind, University of Wisconsin School of Medicine and Public Health and Geriatric Research Education and Clinical Center (GRECC), William S. Middleton Hospital, U.S. Department of Veterans Affairs, Madison, Wisconsin.
References
- 1.Boccuti C, Casillas G. Aiming for fewer hospital U-turns: the Medicare Hospital Readmission Reduction Program. Washington, DC: Kaiser Family Foundation; 2017. Accessed at https://www.kff.org/medicare/issue-brief/aiming-for-fewer-hospital-u-turns-the-medicare-hospital-readmission-reduction-program/on 8 May 2019. [Google Scholar]
- 2.Gilman M, Adams EK, Hockenberry JM, Milstein AS, Wilson IB, Becker ER. Safety-net hospitals more likely than other hospitals to fare poorly under Medicare’s value-based purchasing. Health Aff (Millwood) 2015;34:398–405. [PMID: 25732489] doi: 10.1377/hlthaff.2014.1059 [DOI] [PubMed] [Google Scholar]
- 3.Improving Medicare Post-Acute Care Transformation Act of 2014. Pub L No 113–185, 128 Stat 1952.
- 4.Assistant Secretary for Planning and Evaluation. Report to Congress: Social Risk Factors and Performance Under Medicare’s Value-Based Purchasing Programs. Washington, DC: U.S. Department of Health & Human Services; 2016. [Google Scholar]
- 5.Kwan LY, Stratton K, Steinwachs DM. Accounting for Social Risk Factors in Medicare Payment. Washington, DC: National Academies Pr; 2017. [PubMed] [Google Scholar]
- 6.21st Century Cures Act. Pub L No 114–255, 130 Stat 1033. [Google Scholar]
- 7.Department of Health and Human Services, Centers for Medicare & Medicaid Services. Hospital inpatient prospective payment systems. Fed Regist 2018;83:41147. [Google Scholar]
- 8.Protection of Human Subjects. 45 CFR 46.101(b)(4) and (5). [Google Scholar]
- 9.Rajkumar R, Patel A, Murphy K, Colmers JM, Blum JD, Conway PH, et al. Maryland’s all-payer approach to delivery-system reform. N Engl J Med 2014;370:493–5. [PMID: 24410022] doi: 10.1056/NEJMp1314868 [DOI] [PubMed] [Google Scholar]
- 10.Patel A, Rajkumar R, Colmers JM, Kinzer D, Conway PH, Sharfstein JM. Maryland’s global hospital budgets—preliminary results from an all-payer model. N Engl J Med 2015;373:1899–901. [PMID: 26559570] doi: 10.1056/NEJMp1508037 [DOI] [PubMed] [Google Scholar]
- 11.Roberts ET, McWilliams JM, Hatfield LA, Gerovich S, Chernew ME, Gilstrap LG, et al. Changes in health care use associated with the introduction of hospital global budgets in Maryland. JAMA Intern Med 2018;178:260–8. [PMID: 29340564] doi: 10.1001/jamainternmed.2017.7455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The Maryland Health Services Cost Review Commission Maryland Hospitals’ Audited Financial Statements 2015. Baltimore: State of Maryland; 2015. Accessed at www.hscrc.state.md.us/Pages/data.aspx.on 30 December 2018 [Google Scholar]
- 13.Singh GK, Siahpush M. Increasing inequalities in all-cause and cardiovascular mortality among US adults aged 25–64 years by area socioeconomic status, 1969–1998. Int J Epidemiol 2002;31:600–13. [PMID: 12055162] [DOI] [PubMed] [Google Scholar]
- 14.Singh GK. Area deprivation and widening inequalities in US mortality, 1969–1998. Am J Public Health 2003;93:1137–43. [PMID: 12835199] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kind AJ, Jencks S, Brock J, Yu M, Bartels C, Ehlenbach W, et al. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: a retrospective cohort study. Ann Intern Med 2014;161:765–74. [PMID: 25437404] doi: 10.7326/M13-2946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hu J, Kind AJH, Nerenz D. Area deprivation index predicts readmission risk at an urban teaching hospital. Am J Med Qual. 2018;33:493–501. [PMID: 29357679] doi: 10.1177/1062860617753063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.United States Census Bureau. American Community Survey. Washington, DC: U.S: Department of Commerce; 2018. Accessed at www.census.gov/programs-surveys/acs/about.htmlon 30 December 2018. [Google Scholar]
- 18.Kind AJH, Buckingham WR. Making neighborhood-disadvantage metrics accessible: the neighborhood atlas. N Engl J Med 2018;378:2456–8. [PMID: 29949490] doi: 10.1056/NEJMp1802313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.3M Health Information Systems. APR DRG Software 2012. Accessed at https://www.3m.com/3M/en_US/company-us/all-3m-products/~/3M-APR-DRG-Software/?N=5002385+3290603192&rt=rudon 8 May 2019.
- 20.Averill RF, Goldfield N, Hughes JS, Bonazelli J, McCullough EC, Steinbeck BA, et al. All Patient Refined Diagnosis-Related Groups (APR-DRGs), Version 20.0: Methodology Overview. Salt Lake City: 3M Health Information Systems; 2012. [Google Scholar]
- 21.Horwitz LI, Partovian C, Lin Z, Grady JN, Herrin J, Conover M, et al. Development and use of an administrative claims measure for profiling hospital-wide performance on 30-day unplanned readmission. Ann Intern Med 2014;161:S66–75. [PMID: 25402406] doi: 10.7326/M13-3000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Begg MD, Parides MK. Separation of individual-level and cluster-level covariate effects in regression analysis of correlated data. Stat Med 2003;22:2591–602. [PMID: 12898546] [DOI] [PubMed] [Google Scholar]
- 23.Enders CK, Tofighi D. Centering predictor variables in cross-sectional multilevel models: a new look at an old issue. Psychol Methods 2007;12:121–38. [PMID: 17563168] [DOI] [PubMed] [Google Scholar]
- 24.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics 1986;42:121–30. [PMID: 3719049] [PubMed] [Google Scholar]
- 25.Yelland LN, Salter AB, Ryan P. Performance of the modified Poisson regression approach for estimating relative risks from clustered prospective data. Am J Epidemiol 2011;174:984–92. [PMID: 21841157] doi: 10.1093/aje/kwr183 [DOI] [PubMed] [Google Scholar]
- 26.VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med 2017;167:268–74. [PMID: 28693043] doi: 10.7326/M16-2607 [DOI] [PubMed] [Google Scholar]
- 27.United States Census Bureau. QuickFacts: Baltimore City, Maryland (county); United States. Washington, DC: U.S. Department of Commerce; 2018. Accessed at www.census.gov/quickfacts/table/PST045215/24510,00on 30 December 2018. [Google Scholar]
- 28.LaVeist T, Pollack K, Thorpe R Jr, Fesahazion R, Gaskin D. Place, not race: disparities dissipate in southwest Baltimore when blacks and whites live under similar conditions. Health Aff (Millwood) 2011;30:1880–7. [PMID: 21976330] doi: 10.1377/hlthaff.2011.0640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Soobader M, LeClere FB, Hadden W, Maury B. Using aggregate geographic data to proxy individual socioeconomic status: does size matter? Am J Public Health 2001;91:632–6. [PMID: 11291379] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Office of Disease Prevention and Health Promotion. Access to Health Services Washington, DC: U.S. Department of Health and Human Services; 2018. Accessed at www.healthypeople.gov/2020/topics-objectives/topic/Access-to-Health-Services on 30 December 2018. [Google Scholar]
- 31.Hajat A, Diez-Roux AV, Adar SD, Auchincloss AH, Lovasi GS, O’Neill MS, et al. Air pollution and individual and neighborhood socioeconomic status: evidence from the Multi-Ethnic Study of Atherosclerosis (MESA). Environ Health Perspect 2013;121:1325–33. [PMID: 24076625] doi: 10.1289/ehp.1206337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.U.S. Department of Housing and Urban Development. Neighborhoods and violent crime Accessed at www.huduser.gov/portal/periodicals/em/summer16/highlight2.html on 30 December 2018.
- 33.Institute of Medicine and National Research Council. The Public Health Effects of Food Deserts: Workshop Summary. Washington, DC: National Academies Pr; 2009. Accessed at www.nap.edu/catalog/12623/the-public-health-effects-of-food-deserts-workshop-summaryon 12 August 2018. [PubMed] [Google Scholar]
- 34.Ludwig J, Duncan GJ, Gennetian LA, Katz LF, Kessler RC, Kling JR, et al. Neighborhood effects on the long-term well-being of low-income adults. Science 2012;337:1505–10. [PMID: 22997331] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sampson RJ. Sociology. Moving and the neighborhood glass ceiling. Science 2012;337:1464–5. [PMID: 22997316] [DOI] [PubMed] [Google Scholar]
- 36.Kansagara D, Chiovaro JC, Kagen D, Jencks S, Rhyne K, O’Neil M, et al. So many options, where do we start? An overview of the care transitions literature. J Hosp Med 2016;11:221–30. [PMID: 26551918] doi: 10.1002/jhm.2502 [DOI] [PubMed] [Google Scholar]
- 37.Arbaje AI, Wolff JL, Yu Q, Powe NR, Anderson GF, Boult C. Postdischarge environmental and socioeconomic factors and the likelihood of early hospital readmission among community-dwelling Medicare beneficiaries. Gerontologist 2008;48:495–504. [PMID: 18728299] [DOI] [PubMed] [Google Scholar]
- 38.Ludwig J, Sanbonmatsu L, Gennetian L, Adam E, Duncan GJ, Katz LF, et al. Neighborhoods, obesity, and diabetes—a randomized social experiment. N Engl J Med 2011;365:1509–19. [PMID: 22010917] doi: 10.1056/NEJMsa1103216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Posey KG. Household Income: 2015. Washington, DC: U.S. Census Bureau; 2016 Accessed at www.census.gov/library/publications/2016/acs/acsbr15-02.html. on 30 December 2018 [Google Scholar]
- 40.Chetty R, Hendren N. The impacts of neighborhoods on intergenerational mobility II: county-level estimates. Q J Econ 2018;133:1163–228. Accessed at 10.1093/qje/qjy006. on 30 December 2018 [DOI] [Google Scholar]
- 41.Barnett ML, Hsu J, McWilliams JM. Patient characteristics and differences in hospital readmission rates. JAMA Intern Med 2015;175:1803–12. [PMID: 26368317] doi: 10.1001/jamainternmed.2015.4660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bernheim SM, Parzynski CS, Horwitz L, Lin Z, Araas MJ, Ross JS, et al. Accounting for patients’ socioeconomic status does not change hospital readmission rates. Health Aff (Millwood) 2016;35:1461–70. [PMID: 27503972] doi: 10.1377/hlthaff.2015.0394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Krumholz HM, Bernheim SM. Considering the role of socioeconomic status in hospital outcomes measures. Ann Intern Med 2014;161:833–4. [PMID: 25437411] doi: 10.7326/M14-2308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chokshi DA, Chang JE, Wilson RM. Health reform and the changing safety net in the United States. N Engl J Med 2016;375:1790–6. [DOI] [PubMed] [Google Scholar]
- 45.Phillips RL, Liaw W, Crampton P, Exeter DJ, Bazemore A, Vickery KD, et al. How other countries use deprivation indices—and why the United States desperately needs one. Health Aff (Millwood). 2016;35:1991–8. [PMID: 27834238] [DOI] [PubMed] [Google Scholar]
- 46.Rogan E, Bradley E. Investing in Social Services for States’ Health: Identifying and Overcoming the Barriers. New York: Milbank Memorial Fund; 2016. [Google Scholar]
- 47.Taylor LA, Tan AX, Coyle CE, Ndumele C, Rogan E, Canavan M, et al. Leveraging the social determinants of health: what works? PLoS One 2016;11:e0160217 [PMID: 27532336] doi: 10.1371/journal.pone.0160217 [DOI] [PMC free article] [PubMed] [Google Scholar]