Abstract
Background:
National-level data suggest that sexually transmitted infection (STI) testing rates among young adults are low. The purpose of this study was to evaluate the acceptability of an STI self-testing program at a university health center. Few evaluations on the acceptability of collegiate self-testing programs and their effect on testing uptake have been conducted.
Methods:
To assess acceptability and uptake of self-testing (urine and self-collected vaginal swab), we conducted a brief self-administered survey of students accessing a large US-based university health center from January to December 2015.
Results:
In 2015, University Health Services experienced a 28.5% increase in chlamydia (CT)/gonorrhea (GC) testing for male individuals and 13.7% increase in testing for female students compared to 2013 (baseline). In 2015, 12.4% of male students and 4.8% of female students tested positive for CT/GC via clinician testing, whereas 12.9% of male students and 12.4% of female students tested positive via self-testing. Female students were more likely to test positive for CT/GC when electing to test via self-test versus a clinician test (χ2(1, N = 3068) = 36.54, P < 0.01); no significant difference in testing type was observed for male students. Overall, 22.5% of students who opted for the self-test option completed the acceptability survey; 63% reported that their main reason for testing was unprotected sex. In the past year, 42% reported 4 or more partners. The majority were very satisfied and likely to use the service again (82%).
Conclusions:
Self-testing may be an efficient and effective way to provide STI testing for students and increase testing uptake. Self-reports of multiple partners, unprotected sex, and detected infections suggest that at-risk students are using the service.
In 2015, 15- to 24-year-olds accounted for most reported gonorrhea (GC) and chlamydia (CT) cases, 50% and 67%, respectively.1 Recent data suggest that CT positivity among college students may be higher than the estimated prevalence of CT in the general population (6.5% vs. 4.7%) and may also be higher on 4-year campuses compared with their 2-year counterparts.2 Despite the positivity and sexual risk behaviors, national data estimates suggest that sexually transmitted infection (STI) testing among young adults remains low3; one nationally representative study of youth found that 7.7% of male college students reported STI testing in the past 12 months compared with 20.2% of female college students.4
University health settings are an ideal location for innovative testing methods. Express testing or self-testing for STIs is a quick way of testing patients for CT/GC. Patients can walk-in without an appointment, no sexual history is taken, nor is a medical professional present. Some clinics are now offering female students the option to provide a self-collected vaginal swab (SCVS) specimen, approved for use by the US Food and Drug Administration and the specimen of choice when screening for CT/GC.5,6 In women, the sensitivity and specificity of SCVS have proved superior to a urine sample.7,8 Self-collected vaginal swabs have been shown to be more cost-effective for CT screening relative to cervical swabs and urine screening.8,9 Acceptability research of SCVS among adolescents and younger women has been encouraging, with SCVS being preferred over endocervical swabs.8,10–12 Research on the acceptability of self-collection in the college setting and its effect on testing uptake is limited. One study at a private university in upstate New York offering free STI testing with SCVS to freshmen women found a high rate of participation, low rate of discomfort with SCVS, a high rate of willingness to repeat the test, and low positivity.8 However, further research is needed to assess self-testing acceptability and uptake in different college settings.
On March 3, 2014, Pennsylvania State University’s (PSU) University Park campus introduced the option of STI self-testing at their University Health Services (UHS). As a quality improvement effort, PSU was exploring ways to make STI testing more comfortable and accessible for their students. Fear and stigma surrounding STIs prevent many adolescents and young adults from seeking care.13–15 Some evidence suggests that judgmental attitudes toward patients by health care workers discourage patients, especially those who are asymptomatic, from testing.16 Confidentiality and privacy have also been cited as major concerns among youth when seeking sexual health care, as well as long wait times that can reduce patient anonymity.16–19 Before the initiation of the CT and GC self-testing program, all patients were required to schedule an appointment with a clinician for testing. For women, cervical specimens were collected by the clinician during the examination; men were examined by a clinician and provided urine specimens that were taken to the laboratory for processing (urethral swabs were not offered). Introduction of the self-testing option, available as a walk-in service only, allowed patients to have testing done without seeing a clinician (but could if they wanted to) and eliminated any scheduling barrier.
Evaluation of the self-testing program at PSU was designed to investigate (1) acceptability of self-testing to students visiting PSU UHS and whether SCVSs were acceptable among female patients, (2) rates of CT/GC positivity among self-testers compared with clinician-collected testers, (3) changes in CT/GC testing and CT/GC positivity since implementation of the program, and (4) trends in STI testing and positivity at UHS over the course of a school year.
MATERIALS AND METHODS
Pennsylvania State University is situated in the rural town of State College. Student enrollment at PSU’s University Park campus is almost 47,000 students; 46% female and 54% male. The student body is predominately white with African Americans, Asians, and Hispanic or Latinos, each representing approximately 6% of the student body. Approximately 8% of the student body is international. The student health center primarily serves the undergraduate population.
For years 2013 and 2015, we analyzed CT/GC testing data to determine overall positivity, positivity among clinician-versus self-test groups, and trends in clinician-initiated and self-testing. Students who tested positive for either CT or GC were considered positive cases. Year 2013 provided baseline data because self-testing was not yet offered to students. To assess acceptability of the self-test program, PSU conducted a brief self-administered survey of students accessing UHS for self-testing from January to December of 2015 using PDA-based Qualtrics. The survey was adapted based on a previous self-testing satisfaction survey developed by Gaydos, et al.18 and collected student demographics, reasons for testing including risk behaviors such as unprotected sex and signs or symptoms of a possible infection, number of sex partners in the past 12 months, and satisfaction with the self-testing option.
The process for self-testing was as follows. Students reported to the laboratory waiting area and requested self-testing through a printed form to ensure patient confidentiality. Men who requested self-testing provided a urine specimen; women had only the option of the SCVS. Those with symptoms were advised to schedule a clinician appointment rather than self-testing so that treatment could be started sooner. All patients requesting self-testing were fast-tracked, meaning that there was no wait unless a bathroom was occupied. Printed instructions were provided by the receptionist and also posted in the laboratory restrooms. Students received the survey once they returned to the waiting area (which took <5 minutes to complete); no incentive was provided. The cost of self-testing was $30 and advertising of the program during 2015 was minimal (e.g., posters, flyers, and Web site content). All data were de-identified and student survey data could not be linked to STI laboratory test results. Students were notified of test results through secure messaging from a clinician who reviewed the results. Students with positive results were contacted by either a nurse or clinician, additional history was obtained, and disease education and recommendations, including a prescription, were provided.
χ2 Tests were used to explore differences between clinician and self-test groups by sex, specifically changes in CT/GC testing by sex and test type from 2013 to 2015, and changes in CT/GC positivity by sex and test type from 2013 to 2015. Trends by month in testing and positivity were also examined. Institutional review boards at UHS and the Centers for Disease Control and Prevention reviewed and approved the study.
RESULTS
CT/GC Testing, 2013 and 2015
In 2013, 1014 male and 2711 female students used UHS for CT/GC testing. Overall, in 2015, UHS experienced a 28.5% (1014/1303) increase in CT/GC testing for male students and a 13.7% (2711/3082) increase in CT/GC testing for female students as compared with 2013. Despite the increase in CT/GC testing, total student visits to UHS remained stable from 2013 to 2015. In 2013, total student visits numbered 45,603, and in 2015, student visits numbered 45,617. When examined by test type, data indicate that 18.9% of testers opted for self-testing in 2015: 31.0% of male students and 13.6% of female students. At the same time, clinician testing from 2013 to 2015 declined by 11.3% for male students and declined by 1.8% for female students, despite overall increases in GC/CT testing (Table 1).
TABLE 1.
Number of Students Tested for CT/GC at UHS in 2013 and 2015 by Test Type and Sex
| Clinician | Self-test | % Self-tested | % Change Clinician Testing* | |
|---|---|---|---|---|
| Male | ||||
| 2013 | 1014 | — | — | — |
| 2015 | 899 | 404 | 31.0 | −11.3 |
| Female | ||||
| 2013 | 2711 | — | — | — |
| 2015 | 2663 | 419 | 13.6 | −1.8 |
Percent change in students seeking CT/GC testing from clinicians at UHS from 2013 to 2015.
CT/GC Test Positivity, 2013 and 2015
In 2013, data indicate that 9.7% (98/1007) of male students and 5.0% (135/2700) of female students who sought CT/GC testing at UHS tested positive for CT/GC. In 2015 overall (both clinician and self-testing), 12.6% (163/1297) of male students and 5.9% (180/3068) of female students at UHS tested positive for CT/GC. Overall, male students were significantly more likely to test positive for CT/GC in 2015 than in 2013 (χ2(1, N = 2304) = 4.54, P < 0.05), but no such trend was observed for female students (χ2(1, N = 5768) = 2.09, P = 0.16).
When examined by test type, data indicate that in 2013, 9.7% (98/1007) of male students and 5.0% (135/2700) of female students tested positive for CT/GC via clinician testing. In 2015, 12.4% (111/895) of male students and 4.8% (129/2656) of female students tested positive for CT/GC via clinician testing, whereas 12.9% (52/402) of male students and 12.4% (51/412) of female students tested positive via self-testing. In 2015, female students were more likely to test positive when electing to test via self-test versus a clinician test (χ2(1, N = 3068) = 36.54, P < 0.01). No such significant difference in testing type was observed for male students (Table 2). Thus, overall those choosing the self-test had greater positivity in comparison to those students who chose to be tested via a clinician. In addition, laboratory data indicate that 103 students tested positive in the self-test group. Of those that took the self-report survey, only 23 reported signs or symptoms of STIs (13 male students and 10 female students), suggesting that this was largely an asymptomatic group of students who opted for self-testing.
TABLE 2.
Percent Positivity of all Students Tested for CT/GC at UHS in 2013 and 2015 by Test Type and Sex
| 2013 | 2015 | |||
|---|---|---|---|---|
| n | % | n | % | |
| Male | ||||
| Self-test | — | — | 52 | 12.9 |
| Clinician | 98 | 9.7 | 111* | 12.4 |
| Female | ||||
| Self-test | — | — | 51 | 12.4 |
| Clinician | 135 | 5.0 | 129† | 4.8 |
χ2 = χ2(1, N = 1297) = 0.072, P = 0.79, in the comparison between male students in 2015 for CT/GC positivity when testing via self-test or a clinician test.
χ2 = χ2(1, N = 3068) = 36.5, P < 0.01, in the comparison between female χ2 in 2015 for CT/GC positivity when testing via self-test or a clinician test.
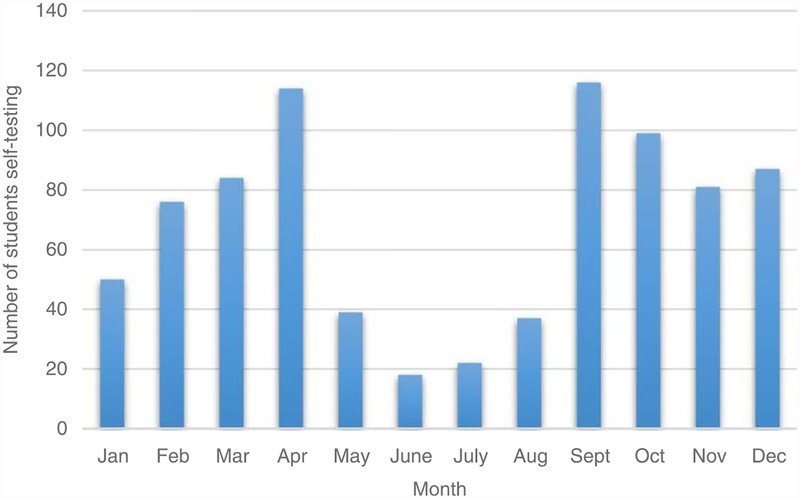
Trends in STI Testing and Positivity, 2015
We examined 2015 testing trends and positivity patterns by month. Of all students tested for CT/GC in 2015, the two most popular months to be tested were in April (12.2% tested) and in September (11.7% tested), with 531 and 512 students testing in April and September of 4385 students who tested for CT/GC in 2015. Positivity did not precisely correlate with testing patterns because February and March indicated the highest months of positivity in 2015 at 9.2% and 11.0%, respectively (Fig. 1).
Figure 1.
Number of self-testing students for CT/GC at UHS in 2015, by month.
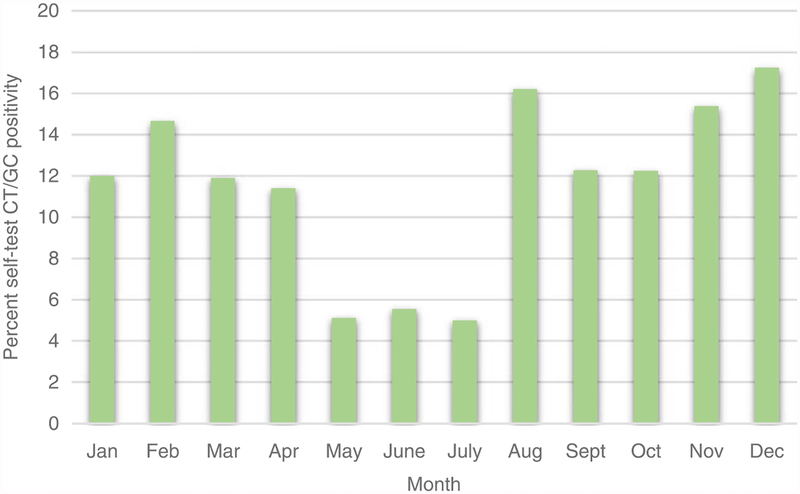
Among the self-test group, although students were self-testing at the greatest numbers in April and September, with 114 and 116 students, positivity was actually at its highest in August and December at 16.2% and 17.2%, respectively (Fig. 2).
Figure 2.
Percentage of self-testing students at UHS who were positive for CT/GC in 2015, by month.
Acceptability of the STI Self-testing Program
Overall, 23.1% (823) students opted for the self-test option in 2015 of all those tested at UHS, of which 22.5% (185) students completed the acceptability survey (Table 3). Among the students surveyed, most were aged 20 to 22 years (59.5%), white (82.7%), female (56.8%), straight/heterosexual (93.0%), and lived off-campus (59.5%). There was a fairly even split between lower classmen and upperclassmen of 44.5% and 48.1%; less than 8% were graduate/postdoctoral students. Of the students surveyed, main reasons for being tested were as follows: “I have had unprotected sex and wish to get tested for STDs” (62.7%), “It’s an important way to take care of myself” (40.5%), and “I get tested for STDs as part of regularly checking my health” (23.2%). In the past 12 months, 44.9% had 2 to 3 sex partners (vaginal or anal intercourse) and more than a third (42.2%) reported 4 or more partners. Only 2 individuals reported having no sex partners in the past 12 months. Ease of testing and no appointment needed were the main reasons for choosing the self-test option (69.2% and 63.2%), followed by confidentiality (38.4%) and cost (26.5%). Most students heard of the self-test option through the UHS Web site (48.1%) and friends/acquaintances (41.1%).
TABLE 3.
Characteristics and Sexual Behavior of STI Self-testing Program Users (N = 185)
| % | n | |
|---|---|---|
| Age, y | ||
| 18–29 | 31.9 | 59 |
| 20–22 | 59.5 | 110 |
| 23–25 | 5.4 | 10 |
| 26+ | 3.2 | 6 |
| Sex | ||
| Male | 42.7 | 79 |
| Female | 56.8 | 105 |
| Genderqueer* | 0.5 | 1 |
| Race | ||
| White | 82.7 | 153 |
| Not white | 17.3 | 32 |
| Enrollment† | ||
| Lower classmen | 44.3 | 82 |
| Upper classmen | 48.1 | 89 |
| Graduate/postdoctoral | 7.6 | 14 |
| Sexual Identity‡ | ||
| Straight | 93.0 | 172 |
| Not straight | 7.0 | 13 |
| Housing | ||
| Residence hall | 27.0 | 50 |
| Off-campus | 59.5 | 110 |
| Greek housing | 13.5 | 25 |
| Primary reason for testing | ||
| Unprotected sex | 62.7 | 116 |
| Important way to take care of myself | 40.5 | 75 |
| Get tested regularly | 23.2 | 43 |
| Partner suggested | 18.4 | 34 |
| Signs/symptoms | 12.4 | 23 |
| Seems like everyone else gets tested | 7.0 | 13 |
| Other | 1.6 | 3 |
| Reason for choosing self-testing | ||
| Ease of testing | 69.2 | 128 |
| No appointment needed | 63.2 | 117 |
| Confidentiality | 38.4 | 71 |
| Cost | 26.5 | 49 |
| Recommended by a friend | 16.2 | 30 |
| Other | 1.6 | 3 |
| No. sex partners in the past 12 mo | ||
| None | 1.1 | 2 |
| 1 | 11.9 | 22 |
| 2–3 | 44.9 | 83 |
| ≥4 | 42.2 | 78 |
Genderqueer was defined to capture individuals who do not subscribe to conventional sex distinctions but identifies with neither, both, or a combination of male and female sexes.
Lower classmen were classified as students reporting that they were in their first or second year; upper classmen were classified being in their third or fourth year or higher.
Straight was defined as someone who identifies as a heterosexual; not straight was a composite variable of individuals identifying as gay (n = 7), lesbian (n = 1), bisexual (n = 4), or other (n = 1).
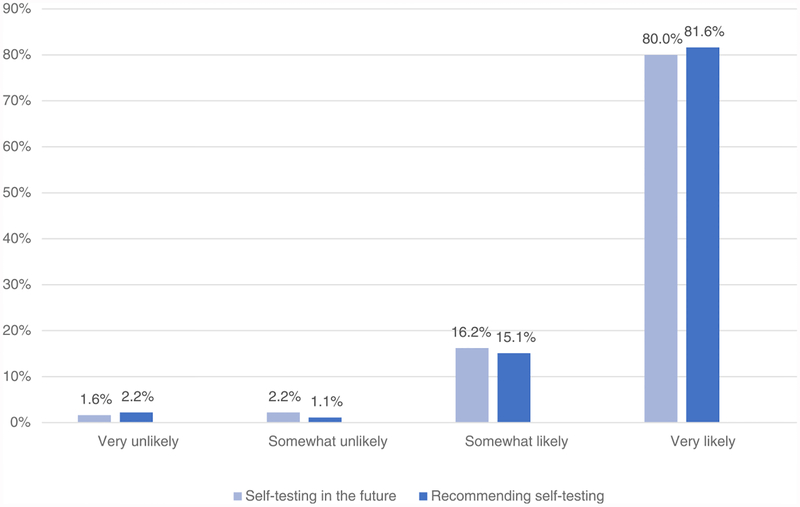
Overall, 96.3% of patients were “very satisfied” or “somewhat satisfied” with the self-testing program. Few students had difficulty with the self-testing process, with 97.8% of patients reporting that the testing experiences was “very easy” or “somewhat easy.” Similarly, 96.7% of clients said it was “very easy” or “somewhat easy” to understand the instructions. No significant differences were found between male and female students (i.e., urine vs. SCVS). The only noticeable, nonsignificant difference was that a small percentage of female students (<6.0%) said that they experienced some difficulty understanding instructions. Satisfaction with the program was overwhelming by both male and female students. Most students reported they would likely use the self-testing service again (80%) and recommend to friends (82.2%; Fig. 3).
Figure 3.
Likelihood of self-testing again and recommending self-testing among university students using self-testing at UHS (N = 185).
DISCUSSION
Introducing STI self-testing in the university health setting may be an opportunity to increase the rates of student testing by offering additional ways in which to interact with health services. In 2015, PSU’s UHS saw an increase in overall STI testing, suggesting that increases in testing may be attributable to the introduction of the STI self-testing program. Female students using the self-test program were significantly more likely to test positive for STIs than those who opted for a clinician-centered visit. Sexually transmitted infection positivity did not precisely correlate with testing patterns. Trends in testing may warrant further examination to determine when marketing pushes for testing should be implemented on campus. Consistent with other studies,8,10 overall student satisfaction with the self-testing program was high and self-testing was reported as an “easy” procedure.
Our findings reveal that the self-testing program was successful in catching asymptomatic cases because self-report data indicate that less than one quarter of students reported any signs or symptoms of STIs before testing. Results also suggest that the self-testing program may be an effective way in which to get at-risk female and male students in for testing, because 14% of female students and 31% of male students opted into the self-testing program. Historically, public health has struggled with getting men into care and tested, and in recent decades, more emphasis has been placed on women’s reproductive health care than men’s, at least heterosexual men.19 Moreover, CT/GC positivity among male students was high, suggesting that it is not just the worried-well presenting for testing.
Given that STI positivity was greater in the self-testing group, the ability to track testing trends among this at-risk group may be helpful toward program improvement, especially in regard to staffing or campaign implementation. Self-testers were presenting for testing most frequently in April and September. We speculate that an increase in testing could be due to post–spring break anxiety and football season. However, positivity was actually at its highest in August and December, suggesting that students may be at greatest risk when they return to school after holiday breaks. Supporting these findings, TheStateofEducation.com examined Google Trends results in the United States for health queries containing the phrase, “chlamydia symptoms” between July 2015 and June 2016. Searches for “chlamydia symptoms” appeared to correspond with academic holiday breaks.20 The 2 largest peaks were late September and mid-January, coinciding with the start of the school year and the return to school after Christmas break. Other peaks corresponded closely with spring break and Thanksgiving, suggesting that CT rates may rise around breaks when students are less focused on academics and more on socializing.
Campaign pushes for testing and condom use may be useful directly before and after breaks. Fielder et al.8 had a 64% participation rate, but most of their participants reported hearing about the program through a mass mailing that went out to 1400 students. During the course of our study, UHS was without a health promotion employee, so advertising and promotions were minimal; most students heard about the program through the UHS Web site. An evidence-based program to bring students in for testing like the GYT: Get Yourself Tested campaign21 paired with the self-testing program could be a strong combination intervention.
Regarding acceptability of the self-testing program, our findings of high satisfaction with the program and ease of testing were consistent with other studies.8,10 Different from Fielder et al., who found a low prevalence of sexually transmitted diseases (1.0%) in their sample, we found high STI positivity. Although unable to link positivity to the survey data, acceptability findings give us a glimpse into the characteristics of self-testers. We found that self-testing is especially appealing to older college students and those living independently, suggesting that convenience of the program may be a draw. Finally, most students reported having multiple partners and unprotected sex, suggesting that the self-testing program is capturing students whom may be at risk for STI acquisition.
Limitations and Future Directions
These findings may not be generalizable to other colleges or sexually transmitted disease programs, because this evaluation was conducted on only one university campus. Findings could be strengthened by being able to link survey data to positivity data. For example, we were unable to determine if the 23 students who said they had symptoms were in fact positive cases. Likewise, positivity data did not contain individual characteristics such as age, race/ethnicity, sexual orientation or practices (i.e., type of sex), which could have provided more insight into the types of individuals using the program and determined whether they needed extragenital STI testing (i.e., male students identifying as gay or bisexual may have needed pharyngeal and/or rectal tests). We were also unable to determine if any cases were repeat testers. Finally, cost may have been a potential confounder in our study; however, the cost of self-testing almost doubled between 2014 (program onset) and 2015 ($18–$30). Likewise, before 2015, PSU did not bill insurance plans outside of their own plan so costs were low. In 2015, they started accepting and participating in multiple insurance plans, so one might infer that if more students were on their parent’s plan as a result of the Affordability Care Act, that clinician-centered STI services would be more affordable/accessible. Instead, it may be more likely that confidentiality concerns acted as a confounder; that is, students may have opted to self-test in 2015 (paying out of pocket) to prevent their parents from receiving an explanation of benefits. Trends and barriers such as these should be further evaluated.
Self-testing in the university health setting may be an efficient and effective way to provide STI testing for asymptomatic students, increase testing uptake, catch at-risk female students, and draw male students into care. This easily replicable program could be implemented on other university campuses and nontraditional testing sites to facilitate identification of more infection earlier.
Acknowledgments:
This evaluation would not have been possible without technical assistance from Linda LaSalle, PhD (Director, UHS Health Promotion and Wellness), and Vicki Dugan, MT (UHS Manager for Laboratory Services).
Footnotes
Conflict of Interest and Sources of Funding: None declared.
Publisher's Disclaimer: Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
REFERENCES
- 1.CDC. Sexually Transmitted Disease Surveillance 2015. Atlanta: US Department of Health and Human Services, 2016. [Google Scholar]
- 2.Habel MA, Leichliter JS, Torrone E. Exploring chlamydia positivity among females on college campuses, 2008–2010. J Am Coll Health 2016; 64:496–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Trepka MJ, Kim S. Prevalence of human immunodeficiency virus testing and high-risk human immunodeficiency virus behavior among 18 to 22 year-old students and nonstudents: Results of the National Survey of Family Growth. Sex Transm Dis 2010; 37:653–659. [DOI] [PubMed] [Google Scholar]
- 4.Cuffe KM, Newton-Levinson A, Gift TL, et al. Sexually transmitted infection testing among adolescents and young adults in the United States. J Adolesc Health 2016; 58:512–519. [DOI] [PubMed] [Google Scholar]
- 5.Fang J, Husman C, DeSilva L, et al. Evaluation of self-collected vaginal swab, first void urine, and endocervical swab specimens for the detection of Chlamydia trachomatis and Neisseria gonorrhoeae in adolescent females. J Pediatr Adolesc Gynecol 2008; 21:355–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schachter J, Chernesky MA, Willis DE, et al. Vaginal swabs are the specimens of choice when screening for Chlamydia trachomatis and Neisseria gonorrhoeae: Results from a multicenter evaluation of the APTIMA assays for both infections. Sex Transm Dis 2005; 32:725–728. [DOI] [PubMed] [Google Scholar]
- 7.Hobbs MM, van der Pol B, Totten P, et al. From the NIH: Proceedings of a workshop on the importance of self-obtained vaginal specimens for detection of sexually transmitted infections. Sex Transm Dis 2008; 35:8–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fielder RL, Carey KB, Carey MP. Acceptability of sexually transmitted infection testing using self-collected vaginal swabs among college women. J Am Coll Health 2013; 61:46–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blake DR, Maldeis N, Barnes MR, et al. Cost-effectiveness of screening strategies for Chlamydia trachomatis using cervical swabs, urine, and self-obtained vaginal swabs in a sexually transmitted disease clinic setting. Sex Transm Dis 2008; 35:649–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Paudyal P, Llewellyn C, Lau J, et al. Obtaining self-samples to diagnose curable sexually transmitted infections: A systematic review of patients’ experiences. PLoS One 2015; 10:e0124310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Doshi JS, Power J, Allen E. Acceptability of chlamydia screening using self-taken vaginal swabs. Int J STD AIDS 2008; 19:507–509. [DOI] [PubMed] [Google Scholar]
- 12.Wiesenfeld HC, Lowry DL, Heine RP, et al. Self-collection of vaginal swabs for the detection of chlamydia, gonorrhea, and trichomoniasis: Opportunity to encourage sexually transmitted disease testing among adolescents. Sex Transm Dis 2001; 28:321–325. [DOI] [PubMed] [Google Scholar]
- 13.Hood J, Friedman A. Unveiling the hidden epidemic: A review of stigma associated with sexually transmissible infections. Sex Health 2011; 8:159–170. [DOI] [PubMed] [Google Scholar]
- 14.Loosier PS, Malcarney MB, Slive L, et al. Chlamydia screening for sexually active young women under the Affordable Care Act: New opportunities and lingering barriers. Sex Transm Dis 2014; 41:538–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ford CA, Best D, Miller WC. The pediatric forum: Confidentiality and adolescents’ willingness to consent to sexually transmitted disease testing. Arch Pediatr Adolesc Med 2001; 155:1072–1073. [PubMed] [Google Scholar]
- 16.Tilson EC, Sanchez V, Ford CL, et al. Barriers to asymptomatic screening and other STD services for adolescents and young adults: Focus group discussions. BMC Public Health 2004; 4:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ford CA, Millstein SG, Halpern-Felsher BL, et al. Influence of physician confidentiality assurances on adolescents’ willingness to disclose information and seek future health care. A randomized controlled trial. JAMA 1997; 278:1029–1034. [PubMed] [Google Scholar]
- 18.Gaydos CA, Barnes M, Aumakham B, et al. Can E-technology through the Internet be used as a new tool to address the Chlamydia trachomatis epidemic by home sampling and vaginal swabs? Sex Transm Dis 2009; 36:577–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kissinger P Issues in men’s reproductive health care In: Sexually Transmitted Diseases: Vaccines, Prevention, and Control. London: Academic Press, 2013:165–188. [Google Scholar]
- 20.TheStateofEducation.com. Sexual Health in Higher Education. 2016. Available at: http://www.thestateofeducation.com/research/college-sexual-health. Accessed June 14, 2017.
- 21.Friedman AL, Brookmeyer KA, Kachur RE, et al. An assessment of the GYT: Get Yourself Tested campaign: An integrated approach to sexually transmitted disease prevention communication. Sex Transm Dis 2014; 41:151–157. [DOI] [PMC free article] [PubMed] [Google Scholar]