Abstract
OBJECTIVE:
To examine the interactive effects of gestational age and infant fussiness on the risk of maternal depressive symptoms in a nationally representative sample.
METHODS:
Sample included 8200 children from the Early Childhood Longitudinal Study, Birth Cohort. Gestational age categories were: very preterm (VPT, 24–31 weeks), moderate/late preterm (MLPT, 32–36 weeks) and full-term (FT, 37–41 weeks). Maternal depressive symptoms (categorized as non-depressed/mild/moderate-severe), from the modified Center for Epidemiological Studies Depression Questionnaire, and infant fussiness (categorized as fussy/not fussy) were assessed at 9 months from parent-report questionnaires. We examined the interactive effects of infant fussiness and gestational age categories, and estimated adjusted odds ratios (aOR) and 95% confidence intervals (CI) of maternal depressive symptoms using multinomial logistic regression.
RESULTS:
Infant fussiness interacted with gestational age categories in predicting maternal depressive symptoms (p=.04), with severity varying by gestational age and infant fussiness. Compared with mothers of VPT infants without fussiness, mothers of VPT infants with fussiness had higher odds of mild depressive symptoms (aOR=2.32, 95%CI [1.19, 4.53]). Similarly, compared with mothers of MLPT and FT infants without fussiness, mothers of fussy MLPT and FT infants had higher odds of moderate-severe symptoms (aOR=2.30, 95%CI [1.40, 3.80], and aOR=1.74, 95%CI [1.40, 2.16] respectively).
CONCLUSIONS:
Mothers of MLPT and FT infants with fussiness had increased odds of moderate-severe depressive symptoms, and mothers of VPT infants with fussiness had increased risk of mild symptoms. Early screening for infant fussiness in preterm and full-term infants may help identify mothers with depressive symptoms in need of support.
Keywords: ECLS-B (Early Childhood Longitudinal Survey-Birth Cohort), Moderate/Late Preterm, Infant Fussiness, Maternal depressive symptoms
Introduction
Preterm birth, characterized by birth prior to 37 weeks gestation, has an estimated prevalence rate of 11% in the United States.1 Preterm birth is a non-normative transition to parenthood associated with feelings of grief, depression and psychological distress,2–4 with depressive symptoms often persisting for weeks or months after NICU discharge.2,3 Maternal depressive symptoms are associated with suboptimal developmental and behavioral outcomes in preterm infants,5,6 with worse outcomes associated with greater chronicity of symptoms.7
Most studies of maternal depression in preterm infants have focused on infants born very preterm (VPT:< 32 weeks gestation),2–4 although VPT infants account for only 17% of all preterm infants.1 Moderate (GA=32–33 weeks) and late preterm infants (GA=34–36 weeks) account for 83% of preterm infants,1 yet as a population, they are relatively understudied. Because the morbidities associated with moderate preterm birth are similar to late preterms,8 outcomes of moderate and late preterm infants are often examined together.9,10 Recent research has examined the association between moderate and late preterm birth (MLPT) and maternal depressive symptoms, with some inconsistent findings.6,11–14 Whereas two studies found no association between MLPT birth and maternal depressive symptoms,6,11 other studies have found a positive association between MLPT birth and maternal depression.12–14 One reason for the lack of association may be related to the high cutpoints for depressive symptoms used in previous studies which identified individuals with moderate depressive symptoms,6,11 but which may have under-identified individuals with milder symptoms. Because mild (i.e. subclinical) depressive symptoms are likely to persist,15 and are associated with risks to the early parent-infant relationship,16 it is necessary to identify mothers with mild depressive symptoms to initiate appropriate interventions. Because MLPT infants do not receive any specialized developmental follow-up care, the risk for maternal depressive symptoms (especially mild symptoms) may go undetected, resulting in missed opportunities to initiate early interventions.17
An additional explanation for the lack of association between MLPT birth and maternal depressive symptoms is that symptoms may be related to a combination of gestational age (i.e., degree of prematurity) and other infant risks. One infant risk that might confer an added risk for maternal depression is infant negative emotionality, characterized specifically by infant fussiness and difficulty.18 Infant negative emotionality/fussiness has been associated with poorer infant sleep,19 later child behavior problems,20 and maternal depressive symptoms.21 Negative emotionality has been examined in VPT,22,23 but we have identified only one study examining negative emotionality in MLPT infants,14 which suggests a need for additional research. Cumulative risk models suggest that combinations of risks increase the odds of poorer outcomes for children and families,24 yet it is unclear if infant negative emotionality in combination with preterm birth confers an added risk for maternal depression. Establishing such a link could inform anticipatory guidance provided to parents of preterm infants.
Given these factors, the objectives of this study were to examine the association between the degree of prematurity (VPT, MLPT, FT) and severity of maternal depressive symptoms (mild, moderate-severe) at 9-months, and to test whether gestational age and infant negative emotionality (characterized by infant fussiness) have interactive effects in predicting the risk of maternal depressive symptoms. We hypothesized that the combination of risks (e.g., infant fussiness combined with VPT or MLPT birth) would relate to higher odds of mild or moderate-severe maternal depressive symptoms, consistent with a cumulative risk model.
Methods
Study Design and Sample
Data were drawn from the Early Childhood Longitudinal Study, Birth Cohort (ECLS-B), a nationally representative, population-based longitudinal study of children born in the United States in 2001. Data were collected from over 10,000 children and their parents at 9 months, with subsequent assessments at 24-months, preschool and kindergarten timepoints. Data collection consisted of home visits with parent interviews and direct child assessments, and included information on children’s development across multiple settings.25
From the original sample of 10,700, this analytical sample excluded children who had chromosomal abnormalities (n=100), included participants whose gestational ages were 24–41 weeks (additional 900 excluded). Participants were also excluded if they were missing maternal depression data (n=1150), or other missing data (e.g., 9-month development T-scores (n=250), and breastfeeding (n=100)). This resulted in the final sample size of 8200. Our study utilized data from 2 timepoints (birth, 9 months), and was considered exempt by the Institutional Review Board because the research involved the use of a publicly available dataset, in which the participants were de-identified, and data could not be linked to the participants.
Measures
Outcome
Maternal Depressive Symptoms:
Maternal depressive symptoms were assessed via parent self-report questionnaire at the 9-month visit using a modified version of the Center for Epidemiological Studies-Depression Scale (CES-D).26 The modified CES-D is a 12-item self-administered scale that assesses the frequency of depressive symptoms experienced in the previous week. The modified CES-D has been validated in other large, national datasets, with internal consistency for the 12-item CES-D previously reported as α=0.85.27 We calculated a measure of internal consistency for the modified CES-D used in our analytic sample (α=0.88), which was similar to reliability reported for the full 20-item CES-D (α=0.89).27
Items were originally scored on a 4-point Likert scale: 1= never to 4= often. Following scoring guidelines suggested in the 9-month ECLS-B user’s manual, items were recoded to 0= never to 3= often, and responses were summed, with potential scores ranging from 0–36, with higher scores indicating more depressive symptoms.25 Cutpoints for categories of depressive symptoms were defined by the ECLS-B as non-depressed (CES-D= 0–4); mild depression (CES-D= 5–9); moderate depression (CES-D= 10), and severe depression (CES-D >10).25 Similar to prior research,27,28 we examined maternal depressive symptoms as a 3-category variable: non-depressed (CES-D= 0–4); mild depression (CES-D= 5–9); moderate-severe depression (CES-D ≥10).
Predictors
Gestational Age:
Gestational age was ascertained from birth certificate data from the ECLS-B restricted use data set. We created a 3-group gestational age category variable, with infants characterized as being very preterm (< 32 weeks), moderate/late preterm (32–36 weeks), and full term (37–41weeks), following gestational age categories defined by clinical convention.1,8
Infant Negative Emotionality/Fussiness:
Infant fussiness was assessed via parent self-report questionnaire at the 9-month visit using a modified version of the Infant/Toddler Symptom Checklist.29 The Modified Infant/Toddler Symptom Checklist (M-ITSC) is a 7-item self-report questionnaire designed to identify children with self-regulatory disorders. Items were scored on a 4-point Likert scale: 0= never; 1= used to be; 2= sometimes; 3= most times. Sample items include, “My child is fussy or irritable;” “my child cries for food or toys.”25 The measure of internal consistency for the M-ITC for our analytic sample was low (α=0.57), suggesting that these 7 items demonstrated poor reliability as a single construct. Because we were interested in the dimension of infant negative emotionality described by infant fussiness/ irritable distress,18 we chose one question from the M-ITSC “my child is fussy or irritable” as our variable of interest. Because there were few infants identified for some of the categories (e.g., “most times fussy”), we had an insufficient sample size to identify meaningful group differences using 3- and 4-group categorizations. As a result, we elected to use a 2-group categorization of infant fussiness. Because parents’ perceptions of infant behavior are formed early and can persist,30 we considered that any experience of infant fussiness may contribute to persistent maternal perceptions of infant fussiness. As such, we dichotomized infant fussiness with scores = 0 (“never fussy”) recoded as 0= “not fussy,” and scores greater than 0 recoded as 1= “fussy.”
Covariates
Maternal and infant characteristics associated with prematurity or maternal depression were chosen a priori as covariates after a review of the literature. The following maternal characteristics were ascertained from the restricted ECLS-B birth certificate data: maternal age, race/ethnicity, marital status (married/ unmarried), history of prenatal smoking, history of breastfeeding (any breastfeeding, no breast feeding), and plurality (singleton, twin or multiple gestation). Also included were measures of maternal education (< high school; high school graduate; > high school) and poverty (<185% federal poverty line; ≥185% federal poverty line) which were incorporated into a single composite measure of household socioeconomic status (SES) created by ECLS-B at 9 months (α=0.85).25
Because the ECLS-B did not contain a composite measure of neonatal morbidity, we included the following neonatal risks ascertained from birth certificate data: birthweight, fetal growth characterized as small for gestational age (SGA:<10%); and 5-minute Apgar scores (dichotomized as >7 versus ≤7). Because frequent infant nocturnal waking may be associated with maternal affective symptoms,31 we included infant nocturnal waking at 9 months (awakens ≥3 times/ night (yes/no)) as a potential confounder. In addition, because developmental delay may be associated with prematurity and maternal depression6 we included a measure of infant development as a potential confounder. Infant cognitive development was assessed at 9 months using the Bayley Short Form Research Edition (BSF-R), which was formulated from the Bayley Scales of Infant Development, Second Edition (BSID-II). The BSF-R Mental T-Scores were norm-referenced by age to the ECLS-B population, adjusted for prematurity, and were scaled to have a mean=50, SD=10.25 We also included infant gender and receipt of early intervention services at 9-months as covariates.
Statistical Analysis
Maternal and child characteristics were examined using descriptive statistics. Multivariate, multinomial logistic regression utilizing the SURVEYLOGISTIC procedure in SAS was used to examine the association between gestational age categories and infant fussiness with the outcome of maternal depressive categories. We controlled for variables that were related to gestational age and maternal depressive categories to adjust for potential confounding. We also examined whether the association between gestational age categories and severity of maternal depressive symptoms (mild or moderate-severe) was moderated by infant fussiness. Adjusted post-hoc tests examined pairwise differences between preterm categories stratified by infant fussiness and the odds of maternal depressive symptoms at a significance level of p<.05. All analyses were conducted using SAS 9.4 (SAS Institute Inc., Cary, NC). Because of the complex sample design, sample weights and the Jackknife method32 were utilized to account for stratification, clustering and unit non-response, thereby allowing the weighted results to be generalized to the population of U.S. children born in 2001. In accord with the NCES requirements for ECLS-B data usage, reported numbers were rounded to the nearest 50.33
Results
Sample Characteristics
Our final sample of 8200 infants born between 24 and 41 weeks included 800 very preterm (< 32 weeks), 1500 moderate/late preterm (32–36 weeks), and 5900 term infants (37–41 weeks). Gestational age groups differed by select maternal (Table 1) and infant characteristics (Table 2). Compared to infants born full-term, infants born very preterm and moderate/late preterm were more likely to have mothers who were unmarried, have less than a high school education, have income less than 185% below the poverty line, and were less likely to have breastfed. They were also more likely to be of black/non-Hispanic race/ethnicity and were more likely to be the product of a twin or multiple gestation. Very preterm and moderate/late preterm infants were also more likely to have lower birthweights and 5-minute APGAR scores compared to infants born full term. Gestational age groups did not differ by maternal age (p=.95), prevalence of maternal depressive symptoms (p=.08) or percentage of infants rated as being “fussy” (p=.79)
Table 1:
Maternal Characteristics for Weighted Sample
| Mean, SD or Weighted (%) | |||||
|---|---|---|---|---|---|
| Total Sample | Very Preterm | Moderate/ Late Preterm | Full term | p | |
| Unweighted N | 8200 | 800 | 1500 | 5900 | |
| Age (years) | 27.4, 3.5 | 27.3, 9.8 | 27.4, 9.6 | 27.4, 3.8 | .95 |
| Depressive symptoms | .08 | ||||
| No depressive symptoms | 59.2% | 55.1% | 55.8% | 59.7% | |
| Mild depressive symptoms | 24.2% | 23.5% | 27.0% | 23.9% | |
| Moderate-severe depressive symptoms 16.5% | 21.4% | 17.2% | 16.4% | ||
| Race/ ethnicity | < .001 | ||||
| White / Non-Hispanic | 60.2% | 50.6% | 52.3% | 61.3% | |
| Black / Non-Hispanic | 13.9% | 26.1% | 19.5% | 13.0% | |
| Hispanic | 20.3% | 20.2% | 22.2% | 20.0% | |
| Asian | 3.2% | 2.1% | 2.8% | 3.2% | |
| Other | 2.5% | 0.9% | 3.1% | 2.4% | |
| Marital Status | < .001 | ||||
| Married | 68.0% | 61.2% | 61.2% | 68.9% | |
| Unmarried | 32.0% | 38.8% | 38.8% | 31.1% | |
| History of Prenatal Smoking | .59 | ||||
| No | 89.0% | 87.0% | 88.2% | 89.1% | |
| Yes | 11.0% | 13.0% | 11.8% | 10.9% | |
| Plurality | < .001 | ||||
| Singleton | 96.7% | 79.4% | 84.5% | 98.5% | |
| Twin or greater | 3.3% | 20.6% | 15.5% | 1.5% | |
| Ever Breastfed | < .001 | ||||
| No | 30.6% | 44.8% | 38.6% | 29.4% | |
| Yes | 69.4% | 55.2% | 61.4% | 70.6% | |
| Socioeconomic indicators calculated from measures of education and income at 9-months: | |||||
| Maternal Education | .01 | ||||
| Less than high school | 17.3% | 21.4% | 20.7% | 16.8% | |
| High school graduate | 28.3% | 28.1% | 29.1% | 28.2% | |
| > High School | 54.4% | 50.5% | 50.2% | 55.0% | |
| Below poverty threshold | < .001 | ||||
| (<185% federal poverty line) | 46.0% | 55.4% | 53.4% | 44.9% | |
| At or above poverty threshold | |||||
| (≥185% federal poverty line) | 54.0% | 44.6% | 46.6% | 55.1% | |
Table 2:
Infant Characteristics for Weighted Sample
| Mean, SD or Weighted (%) | |||||
|---|---|---|---|---|---|
| Total Sample | Very Preterm | Moderate/ Late Preterm | Full term | p | |
| Unweighted N | 8200 | 800 | 1500 | 5900 | |
| Gestational Age (weeks) | 38.5, 2.5 | 28.8, 3.1 | 35.0, 1.7 | 39.1, 1.6 | < .001 |
| Infant Fussiness/Difficulty | .79 | ||||
| Fussy | 63.5% | 65.5% | 64.2% | 63.3% | |
| Not Fussy | 36.5% | 34.5% | 35.8% | 36.7% | |
| Gender | .60 | ||||
| Male | 51.2% | 49.8% | 52.6% | 51.0% | |
| Female | 48.8% | 50.2% | 47.4% | 49.0% | |
| Birthweight (grams) | 3320.0, 408.4 | 1719.2, 2131.7 | 2806.1, 1005.0 | 3412.6, 392.8 | < .001 |
| Fetal Growth | .03 | ||||
| Small for gestational age (<10%) | 9.9% | 6.6% | 9.1% | 10.1% | |
| 5-Minute Apgar | < .001 | ||||
| >7 | 97.1% | 71.0% | 92.6% | 98.2% | |
| ≤ 7 | 2.9% | 29.0% | 7.4% | 1.8% | |
| 9-month Bayley Mental T-score | 50.1, 23.3 | 44.9, 22.5 | 46.8, 20.4 | 50.6, 19.5 | < .001 |
| Child Awakens ≥3 Times Nightly | |||||
| .04 | |||||
| No | 85.9% | 89.2% | 83.3% | 86.1% | |
| Yes | 14.1% | 10.8% | 16.7% | 13.9% | |
Test of Cumulative Risk Hypothesis
After adjusting for covariates, there was no main effect of gestational age category on the odds of maternal depressive symptoms, but we found evidence of interactive effects between infant fussiness and gestational age categories on the odds of maternal depressive symptoms (p=.04). In adjusted models stratified by infant fussiness, the prevalence and severity of maternal depressive symptoms varied by the degree of prematurity. (Figure 1).
Figure 1.
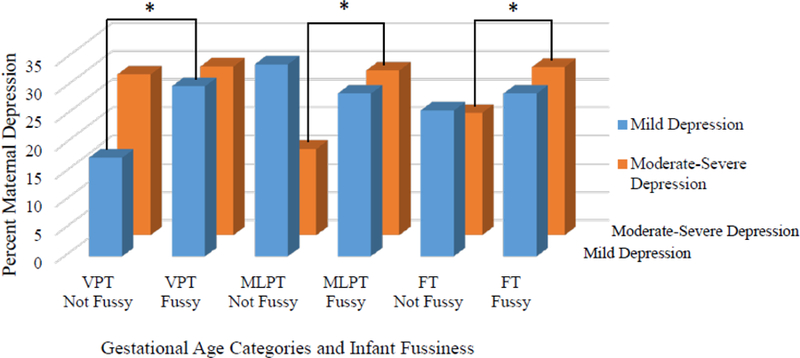
Interactive Effects of Gestational Age Categories and Infant Fussiness on the Severity of Maternal Depressive Symptoms *: significant pairwise differences at a level of p < .05
Very Preterm Infants.
Mothers of VPT infants with fussiness were more likely to experience mild depressive symptoms, compared to mothers of VPT infants without fussiness (30% vs. 17.6% respectively). Mothers of very preterm infants with fussiness had 2.3 greater odds of experiencing mild depressive symptoms compared with mothers of very preterm infants without fussiness (aOR=2.32; 95% CI [l.19 – 4.53]).
Moderate/Late Preterm Infants.
In contrast, among infants born moderate/late preterm, mothers of MLPT infants with fussiness were more likely to experience moderate-severe depressive symptoms, compared to mothers of MLPT infants without fussiness (29.2% vs. 15.3% respectively). Mothers of moderate/late preterm infants with fussiness had 2.3 greater odds of experiencing moderate-severe depressive symptoms compared with mothers of moderate/late preterm infants without fussiness (aOR=2.30; 95% CI [l.40 – 3.80]).
Full-term Infants.
For full-term infants, mothers of FT infants with fussiness were also more likely to experience moderate-severe depressive symptoms, compared to mothers of FT infants without fussiness (29.8% vs. 21.7% respectively). Similar to mothers of MLPT infants, mothers of FT infants with fussiness had a 1.7-greater odds of experiencing moderate-severe depressive symptoms compared with mothers of full-term infants without fussiness (aOR=1.74, 95% CI [1.40–2.16]). (Table 3).
Table 3:
Gestational Age Categories, Infant Fussiness, and Odds of Mild and Moderate-Severe Maternal Depressive Symptoms¥
| Level of Depressive Symptoms | VPT with Fussiness vs VPT without Fussiness | MLPT with Fussiness vs MLPT Fussiness | FT with Fussiness vs FT without Fussiness |
|---|---|---|---|
| Mild depressive symptoms | 2.32 [1.19–4.53] | 1.02 [0.69–1.51] | 1.41 [1.21–1.65] |
| Moderate-severe depressive symptoms | 1.42 [0.80–2.52] | 2.30 [1.40–3.80] | 1.74 [1.40–2.16] |
Analyses included the following covariates: smoking, maternal race, plurality, marital status, infant nocturnal awakening, breastfeeding, SES, maternal age, & Bayley 9-month T-scores; W1R0 weight applied to analyses
Maternal and Infant Characteristics Associated with of Mild and Moderate Maternal Depressive Symptoms
Several maternal and infant characteristics were also associated with greater mild and moderate-severe maternal depressive symptoms, including a history of prenatal smoking and being unmarried. Lower odds of mild and moderate-severe maternal depressive symptoms were associated with older maternal age and higher SES. Asian and black race, history of frequent nocturnal waking and having twin or multiple gestation were associated with higher odds of moderate-severe depressive symptoms. (Table 4)
Table 4:
Maternal and Infant Characteristics Associated with Odds of Mild and Moderate-Severe Maternal Depressive Symptoms¥
| Mild Depressive Symptoms | Moderate-Severe Depressive Symptoms | |
|---|---|---|
| Gestational age × Infant Fussiness | Results in Table 3 | Results in Table 3 |
| Prenatal Smoking (Yes) | 1.4 [1.1, 1.8] | 2.2 [1.7, 2.7] |
| Ever Breastfed (yes) | 0.9 [0.8, 1.1] | 1.1 [0.9, 1.3] |
| Maternal Race/Ethnicity | ||
| Other | 1.4 [0.97, 2.1] | 1.4 [0.95, 2.0] |
| Asian | 1.2 [0.99, 1.5] | 1.5 [1.1, 2.0] |
| Hispanic | 0.7 [0.6, 0.9] | 0.6 [0.5, 0.8] |
| Black, Non-Hispanic | 1.2 [0.98, 1.5] | 1.5 [1.1, 1.9] |
| White, Non-Hispanic | REF | REF |
| Plurality (Twin or Multiple Gestation) | 1.1[0.9, 1.4] | 1.3 [1.1, 1.7] |
| Marital Status (Unmarried) | 1.3 [1.1, 1.5] | 1.6 [1.4, 2.0] |
| Maternal Age | 0.98 [0.97, 0.99] | 0.98 [0.97, 0.99] |
| SES (9-months) | 0.8 [0.7, 0.9] | 0.6 [0.57, 0.7] |
| Infant Nocturnal Waking (Yes) | 1.1[0.9, 1.4] | 1.7 [1.4, 2.0] |
| Infant 9-month Cognitive Development | 0.99 [0.99, 1.00] | 0.98 [0.98, 1.00] |
W1R0 weight applied to analyses
Discussion
This is the first study to examine the interactive effects of the degree of prematurity (very preterm, moderate/late preterm, full term) and infant fussiness (fussy vs. not fussy) on the severity of maternal depressive symptoms in a nationally representative sample. Our study is also unique in its focus on predictors associated with both mild (i.e. subclinical) depressive symptoms, as well as more commonly studied moderate-to-severe depressive symptoms. Although there is a paucity of research regarding child outcomes associated with mild depressive symptoms, there is increasing awareness that mild depressive symptoms are common, may progress into more severe depressive symptoms,15 and are associated with risks to the early parent-infant relationship.16 Given these factors, identifying mothers with sub-threshold symptoms may help give professionals the opportunity to provide preventive support to mothers.
Similar to prior research using the ECLS-B,6 our results suggest that the degree of prematurity is not an independent risk associated with maternal depression. However, we found that infant fussiness in combination with the infant gestational age categories was associated with varying severity of maternal depressive symptoms. Using a cumulative risk model,24 we hypothesized that mothers of infants with more biological risk (i.e. being born more preterm) combined with an additional vulnerability (i.e., infant fussiness) would experience more elevated maternal depressive symptoms. Contrary to expectations, we found that infant fussiness was a potent vulnerability factor, especially for later-born infants. In other words, mothers of moderate to late preterm infants with infant fussiness experienced more severe maternal depressive symptoms, while mothers of very preterm fussy infants experienced milder depressive symptoms. In addition, mothers of fussy full-term infants also experienced moderate-severe depressive symptoms, contrary to a cumulative risk hypothesis.
Infant negative emotionality, especially the dimension of infant fussiness and irritability, is a well described challenge to the caregiving relationship. Mothers of fussier, less soothable infants report significantly less confidence, lower efficacy, and more stress and depressive symptoms than mothers of less fussy, more soothable infants.34 Concerns about infant fussiness often present to the general pediatrician, and as such, the pediatric primary care visit is an ideal opportunity to assess infant negative emotionality and its influence on the early parent-child relationship. General pediatricians are uniquely poised to observe infant behavior and to inquire about infant fussiness, which may help identify mothers who may experience their infant as challenging, and who may benefit from additional supports or services.
More recently, a growing number of studies have examined early negative emotionality and infant difficulty as a susceptibility factor, rather than an independent risk factor for children. That is, infant negative emotionality may make an infant susceptible, or malleable, to both negative and positive experiences. A recent meta-analysis of 84 longitudinal studies35 found that infants with who were rated by their parents as being more challenging were more vulnerable to negative parenting and also benefitted more from positive parenting, compared to children who were rated as being less challenging, supporting a differential susceptibility interpretation.36 These findings are particularly important when one adds maternal depression into the mix because infants with negative emotionality (i.e. “fussy” infants) who also experience maternal depression, and the negative parenting often accompanying elevated depressive symptoms, are more likely to develop social emotional problems.37 Early screening and intervention for both concerns may prevent such problems from developing.
In addition to the interactive effects of infant fussiness and gestational age, we found that maternal characteristics associated with prenatal stress and socioeconomic disadvantage (i.e., lower SES, unmarried marital status, smoking) were associated with greater odds of both mild and moderate-severe maternal depressive symptoms. Similarly, experiences associated with challenges to caregiving (i.e., history of multiple gestation and increased infant nocturnal waking) were also associated with greater odds of moderate-severe maternal depression. Interestingly, we found that Asian and black race were associated with a greater odds of moderate-severe depressive symptoms, whereas Hispanic ethnicity was associated with a lower odds of maternal depression. This raises the question regarding the role of culture as a potential risk or protective factor in the development of maternal depression.
Multiple resources are available to support parents in the postnatal period. These resources include nursing home-visitation, early intervention, and infant mental health services.38 While these supports are typically offered to parents of very preterm infants, parents of moderate and late preterm infants, as well as full-term infants, are often not referred for such supports. Because our results suggests that infant fussiness occurs at a similar frequency in MLPT infants as VPT infants, and because mothers of fussy MLPT infants experience more severe depressive symptoms than their VPT counterparts, one implication of our study is to consider specialized supports for mothers endorsing infant fussiness (e.g. the Fussy Baby Network which offers telephone support for mothers of difficult infants).39
While very preterm infants have higher morbidity than moderate/late preterm infants, the perinatal care of infants born very preterm may actually help buffer against more severe maternal affective symptoms. Very preterm infants are often cared for in a neonatal ICU setting, where part of the specialized care includes anticipatory guidance focused on the vulnerabilities associated with preterm birth. As the parents of VPT infants transition home, they often receive an enhanced level of postnatal support and developmental follow-up, including referrals to early intervention programs, home visiting, and subsequent care in neonatal follow-up clinics.38 These postnatal supports and services provided to parents of VPT infants may help prepare them for the potential challenges associated with caring for a preterm infant, and may help mitigate the risk for maternal depressive symptoms. In contrast, infants born moderate and late preterm often have a shorter duration of hospitalization,40 receive no specialized neonatal follow-up care, and are less likely to qualify for early intervention services compared to infants born very preterm.41 There is an emerging literature indicating that mothers of late preterm infants are more likely to perceive their infant as being demanding and difficult,14 and rate late preterm infants as having more behavior problems than infants born more preterm.40 In the absence of the psychosocial supports and anticipatory guidance provided to mothers of VPT infants, mothers of moderate and late preterm infants may feel more challenged by MLPT behavior, contributing to more severe maternal depressive symptoms in the context of infant fussiness.
This study had several strengths and limitations. Notable strengths include the use of a large, nationally representative sample that included infants across the full spectrum of gestational age and use of a well-validated measure for maternal depressive symptoms. One limitation is that our study utilized parental reports of both maternal depressive symptoms and infant fussiness and thus, reporter bias and shared method variance are considerations, as mothers with depressive symptoms are more likely to perceive their children as being more difficult.42 Another limitation was that our measure of infant fussiness was based on one question item from a larger questionnaire. Our study design did not permit us to examine causality of maternal depressive symptoms or infant fussiness, and because depressive symptoms were assessed at 9-months, it was not possible to determine whether the depressive symptoms were present prior to, or emerged after the birth of the infant. In addition, while the ECLS-B is a rich dataset and among the only longitudinal cohorts from the US, the data are old, which is an additional limitation. Despite these limitations, our results demonstrated that the risk for maternal depressive symptoms varied by a dimension of infant temperament and degree of prematurity, which has implications for pediatric primary care.
Conclusions
Mothers of VPT with infant fussiness experienced increased odds of mild depressive symptoms while mothers of “fussy” MLPT and FT infants had increased odds of moderate-severe depressive symptoms, suggesting a potential need for closer surveillance and supports for these mothers. Pediatric providers can query mothers about their experiences of infant fussiness, which can help identify which mothers would benefit from additional depression screening, and referrals for additional services (e.g. preventative programs targeting maternal emotional well-being),16 thus improving the postnatal care of dyads at risk.
WHAT’S NEW:
In a nationally representative sample, maternal depression risk varied by gestational age and infant fussiness. Mothers of VPT infants with fussiness had higher mild depressive symptoms, while mothers of fussy MLPT or FT infants had higher moderate-severe depressive symptoms.
Acknowledgement of Funding Sources:
University of Michigan, NICHD (K08HD078506), The funding sources had no involvement in the study design, collection, analysis, interpretation of data, in the writing of the report, or in the decision to submit the article for publication
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: NONE
Financial Disclosure: None
References
- 1. https://www.childtrends.org/indicators/preterm-births.
- 2.Holditch-Davis D, Santos H, Levy J, et al. Patterns of psychological distress in mothers of preterm infants. Infant Behavior and Development 2015;41:154–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Helle N, Barkmann C, Bartz-Seel J, et al. Very low birth-weight as a risk factor for postpartum depression four to six weeks postbirth in mothers and fathers: Cross-sectional results from a controlled multicentre cohort study. Journal of Affective Disorders 2015;180:154–161. [DOI] [PubMed] [Google Scholar]
- 4.Rogers CE, Kidokoro H, Wallendorf M, Inder TE. Identifying mothers of very preterm infants at-risk for postpartum depression and anxiety before discharge. Journal Of Perinatology 2012;33:171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McManus BM, Poehlmann J. Parent–child interaction, maternal depressive symptoms and preterm infant cognitive function. Infant Behavior and Development 2012;35(3):489–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cheng ER, Kotelchuck M, Gerstein ED, Taveras EM, Poehlmann-Tynan J. Postnatal Depressive Symptoms Among Mothers and Fathers of Infants Born Preterm: Prevalence and Impacts on Children’s Early Cognitive Function. Journal of Developmental and Behavioral Pediatrics 2016;37(1):33–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Trapolini T, McMahon CA, Ungerer JA. The effect of maternal depression and marital adjustment on young children’s internalizing and externalizing behaviour problems. Child: care, health and development 2007;33(6):794–803. [DOI] [PubMed] [Google Scholar]
- 8.Shapiro-Mendoza CK, Lackritz EM. Epidemiology of late and moderate preterm birth. Seminars in Fetal and Neonatal Medicine 2012;17(3):120–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Odd DE, Emond A, Whitelaw A. Long‐ term cognitive outcomes of infants born moderately and late preterm. Developmental Medicine and Child Neurology 2012;54(8):704–709. [DOI] [PubMed] [Google Scholar]
- 10.Shah PE, Kaciroti N, Richards B, Lumeng JC. Gestational age and kindergarten school readiness in a national sample of preterm infants. The Journal of Pediatrics 2016;178:61–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McDonald SW, Benzies KM, Gallant JE, McNeil DA, Dolan SM, Tough SC. A comparison between late preterm and term infants on breastfeeding and maternal mental health. Matern Child Health J 2013;17(8):1468–1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gambina I, Soldera G, Benevento B, et al. Postpartum psychosocial distress and late preterm delivery. Journal of Reproductive and Infant Psychology 2011;29(5):472–479. [Google Scholar]
- 13.Mehler K, Mainusch A, Hucklenbruch-Rother E, Hahn M, Hünseler C, Kribs A. Increased rate of parental postpartum depression and traumatization in moderate and late preterm infants is independent of the infant’s motor repertoire. Early human development 2014;90(12):797–801. [DOI] [PubMed] [Google Scholar]
- 14.Voegtline KM, Stifter CA. Late-preterm birth, maternal symptomatology, and infant negativity. Infant Behavior & Development 2010;33(4):545–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hermens ML, van Hout HP, Terluin B, et al. The prognosis of minor depression in the general population: a systematic review. General Hospital Psychiatry 2004;26(6):453–462. [DOI] [PubMed] [Google Scholar]
- 16.Moehler E, Brunner R, Wiebel A, Reck C, Resch F. Maternal depressive symptoms in the postnatal period are associated with long-term impairment of mother–child bonding. Archives of Women’s Mental Health 2006;9(5):273–278. [DOI] [PubMed] [Google Scholar]
- 17.Kerker BD, Storfer-Isser A, Stein RE, et al. Identifying Maternal Depression in Pediatric Primary Care: Changes Over a Decade. Journal of Developmental and Behavioral Pediatrics 2016;37(2):113–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goodnight JA, Donahue KL, Waldman ID, et al. Genetic and Environmental Contributions to Associations between Infant Fussy Temperament and Antisocial Behavior in Childhood and Adolescence. Behavior Genetics 2016;46(5):680–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weisman O, Magori-Cohen R, Louzoun Y, Eidelman AI, Feldman R. Sleep-Wake Transitions in Premature Neonates Predict Early Development. Pediatrics 2011;128(4):706. [DOI] [PubMed] [Google Scholar]
- 20.Hartz K, Williford A. Child negative emotionality and caregiver sensitivity across context: Links with children’s kindergarten behaviour problems. Infant and Child Development 2015;24(2):107–129. [Google Scholar]
- 21.McGrath JM, Records K, Rice M. Maternal depression and infant temperament characteristics. Infant Behavior and Development 2008;31(1):71–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Poehlmann J, Hane A, Burnson C, Maleck S, Hamburger E, Shah PE. Preterm infants who are prone to distress: differential effects of parenting on 36-month behavioral and cognitive outcomes. Journal of Child Psychology and Psychiatry 2012;53(10):1018–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gueron‐ Sela N, Atzaba‐ Poria N, Meiri G, Marks K. Temperamental susceptibility to parenting among preterm and full‐ term infants in early cognitive development. Infancy 2016;21(3):312–331. [Google Scholar]
- 24.Atkinson L, Beitchman J, Gonzalez A, et al. Cumulative risk, cumulative outcome: a 20-year longitudinal study. PloS one 2015;10(6):e0127650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nord C, Andreassen C, Branden L, et al. Early Childhood Longitudinal Study, Birth Cohort (ECLS-B), User’s Manual for the ECLS-B Nine-Month Public-Use Data File and Electronic Code Book. US Department of Education, NCES, Washington, DC: 2004. [Google Scholar]
- 26.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement 1977;1(3):385–401. [Google Scholar]
- 27.Poulin C, Hand D, Boudreau BJCD, Canada Ii. Validity of a 12-item version of the CES-D [Centre for Epidemiological Studies Depression scale] used in the National Longitudinal Study of Children and Youth. Chronic Diseases and Injuries in Canada 2005;26(2–3):65. [PubMed] [Google Scholar]
- 28.Surkan PJ, Ettinger AK, Ahmed S, Minkovitz CS, Strobino D. Impact of maternal depressive symptoms on growth of preschool-and school-aged children. Pediatrics 2012:peds. 2011–2118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.DeGangi GA. Infant/Toddler Symptom Checklist: A screening tool for parents Psychological Corp; 1995. [Google Scholar]
- 30.Pauli-Pott U, Mertesacker B, Bade U, Haverkock A, Beckmann D. Parental perceptions and infant temperament development. Infant Behavior and Development 2003;26(1):27–48. [Google Scholar]
- 31.Lee S-Y, Hsu H-C. Stress and health-related well-being among mothers with a low birth weight infant: The role of sleep. Social science & medicine 2012;74(7):958–965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wicklin R Statistical programming with SAS/IML software SAS Institute; 2010. [Google Scholar]
- 33. https://nces.ed.gov/ecls/birthdatainformation.asp.
- 34.Crockenberg S, Leerkes EJ. Infant negative emotionality, caregiving, and family relationships. In: Crouter ABE Ann C., ed. Children’s Influence on Family Dynamics: The Neglected Side of Family Relationships Mahwah, New Jersey: Lawrence Erlbaum Associates; 2003:57–78. [Google Scholar]
- 35.Slagt M, Dubas JS, Dekovic M, van Aken MA. Differences in sensitivity to parenting depending on child temperament: A meta-analysis. Psychological Bulletin 2016;142(10):1068–1110. [DOI] [PubMed] [Google Scholar]
- 36.Belsky J, Pluess M. Beyond diathesis stress: Differential susceptibility to environmental influences. Psychological Bulletin 2009;135(6):885. [DOI] [PubMed] [Google Scholar]
- 37.Miner JL, Clarke-Stewart KA. Trajectories of externalizing behavior from age 2 to age 9: relations with gender, temperament, ethnicity, parenting, and rater. Developmental Psychology 2008;44(3):771–786. [DOI] [PubMed] [Google Scholar]
- 38.Murch TN, Smith VC. Supporting Families as They Transition Home. Newborn and Infant Nursing Reviews 2016;16(4):298–302. [Google Scholar]
- 39. www.erikson.edu/fussybaby/national-network.
- 40.Shah PE, Robbins N, Coelho RB, Poehlmann J. The paradox of prematurity: The behavioral vulnerability of late preterm infants and the cognitive susceptibility of very preterm infants at 36 months post-term. Infant Behavior and Development 2013;36(1):50–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kalia JL, Visintainer P, Brumberg HL, Pici M, Kase J. Comparison of Enrollment in Interventional Therapies Between Late-Preterm and Very Preterm Infants at 12 Months’ Corrected Age. Pediatrics 2009;123(3):804–809. [DOI] [PubMed] [Google Scholar]
- 42.Chilcoat HD, Breslau N. Does psychiatric history bias mothers’ reports? An application of a new analytic approach. Journal of the American Academy of Child Adolescent Psychiatry 1997;36(7):971–979. [DOI] [PubMed] [Google Scholar]


