Abstract
Objective
Academic detailing in partnership with the Opioid Overdose Education and Naloxone Distribution (OEND) program was implemented to increase naloxone access for the prevention of opioid overdose mortality in veterans at the U.S. Department of Veterans Affairs (VA). However, implementation was not uniform leading to varying levels of intervention exposure potentially impacting naloxone prescribing. We examined the impact of implementation strength (proportion of providers exposed to academic detailing) at each station on naloxone prescribing from September 2014 to December 2017.
Study Design and Setting
Retrospective cohort design with fixed effects models at the VA.
Data Collection/Extraction Methods
We used VA Corporate Data Warehouse for data on pharmacy dispensing, station‐, provider‐ and patient‐level characteristics. OEND‐specific academic detailing activities came from data recorded by academic detailers using Salesforce.com.
Principal Findings
VA stations wherein 100 percent of providers exposed to an OEND‐related academic detailing educational outreach visit experienced an increased incident rate of naloxone prescribing that was 5.52 times the incident rate of stations where no providers were exposed; alternatively, this is equivalent to an average monthly increase of 2.60 naloxone prescriptions per 1000 population at risk for opioid overdose.
Conclusions
Our findings highlight the importance of academic detailing's implementation strength on naloxone prescribing. Decision makers must carefully consider the implementation process to achieve the greatest effectiveness from the intervention.
Keywords: academic detailing, educational outreach, implementation, naloxone, opioid overdose, veterans
1. BACKGROUND
Opioid overdose mortality has become a national epidemic and public health policy concern in the United States (U.S.). There were over 47 000 opioid overdose deaths in 2017, which was a 4.1‐fold increase from 2002.1 Compared to the general U.S. population, drug overdose mortality risk was two times higher among veterans; this has been made worse by the increased use of opioids in veterans.2 Between 2001 and 2007, opioid prescribing in veterans increased by 184 percent for methadone, 60 percent for synthetic/semisynthetic opioids, and 35 percent for nonsynthetic opioids.3 In response to the opioid crisis, the U.S. Department of Veterans Affairs (VA) implemented system‐wide programs such as the Opioid Safety Initiative (OSI) in 20134 and the Opioid Overdose Education and Naloxone Distribution (OEND) program in 2014.5 While the goal of OSI is to promote the proper and safe prescribing of opioids for pain management4, 6; the OEND program is focused on educating veterans, their caregivers, and providers on opioid overdose prevention, recognition, response, and proper use of naloxone to reverse opioid‐related overdose events.5
Naloxone is an effective and safe harm reduction strategy for preventing opioid overdose mortality.7 However, lack of knowledge and stigma associated with opioid use disorder has contributed to limited naloxone use in the ambulatory setting, and thereby its effectiveness in preventing opioid overdose mortality.8, 9, 10 In order to change provider prescribing behavior, specifically for veterans, and improve access to naloxone for opioid reversals, the OEND program collaborated with the VA Pharmacy Benefits Management Academic Detailing Service to implement academic detailing as an innovative solution to educate and inform providers on the proper use of naloxone.
Academic detailing is a multifaceted, educational outreach intervention that educates prescribers through interactions with academic detailers using unbiased evidence, educational brochures, and benchmarking tools to align prescribing behavior with evidence‐based practice.11, 12, 13, 14, 15 In the VA, academic detailers (specially trained clinical pharmacist providers) identify prescribers using priority panels of high‐risk veterans, arrange one or more visits with prescribers, and share naloxone prescribing data along with population management tools that highlight veterans at risk for opioid overdose, with the goal of improving access to take‐home naloxone.
On March 27, 2015, the Interim Under Secretary of Health mandated that all VA networks implement academic detailing to address issues related to pain management and mental health by June 30, 2015.16 We previously investigated the impact of this academic detailing program on naloxone prescribing at the VA; we reported that providers who received an academic detailing visit on average had increased naloxone prescribing in the outpatient setting compared to providers who did not receive this intervention.17 However, the impact of academic detailing implementation across the VA networks has not been studied.
The objective of this study was to examine the impact of station‐level implementation strength of academic detailing across the VA on naloxone prescribing from September 2014 to December 2017. We hypothesized that stations (or regional facilities) that implemented academic detailing will have a greater number of naloxone prescriptions prescribed than stations that did not implement academic detailing.
2. DESIGN AND METHODS
This was a retrospective cohort study that investigated the association between implementation strength (proportion of providers exposed to OEND‐specific academic detailing) and the amount of naloxone prescriptions prescribed from September 2014 to December 2017. The study protocol was reviewed and approved by Institutional Review Boards at the Veterans Affairs San Diego Healthcare System and the University of Washington.
2.1. Sample
This study was performed at the U.S. Department of Veterans Affairs, which is the largest, integrated health care system in the U.S. with coverage to all fifty states and its territories and a total enrollment of approximately 9 million veterans.18 In 2017, the VA was comprised of 130 stations, which encompassed 179 Veterans Affairs Medical Centers (VAMCs) and 1061 Community‐Based Outpatient Clinics (CBOCs) that performed approximately 109 million outpatient visits, treated 615 000 inpatients (medical and surgical), and treated 149 000 mental health inpatients.19 The VA has a total workforce of approximately 25 000 physicians, 95 000 nurses, and nearly 8000 pharmacists with an annual operating budget of approximately $72 billion.19, 20
This analysis was performed at the station level; all stations (N = 130) across the VA were included. Each station consists of one or more VAMCs with its surrounding satellites or CBOCs. Providers were assigned to a station but may work at either the VAMC, CBOC, or both.
We used provider‐level data to generate station‐level characteristics (eg, mean age of providers; proportion of providers who are male, physician assistants, nurse practitioners, and mental health specialists). A closed cohort of primary care providers with uninterrupted employment at the VA from September 2014 to December 2017 was selected. Providers were included if they prescribed at least one opioid prescription and had veterans at risk for opioid‐related events (eg, overdose and mortality) in their care. Providers were excluded if they were pharmacists, residents, anesthesiologists, surgeons, oncologists, or worked in the emergency department. All providers had veterans assigned throughout the study period.
Veterans were included if they had been prescribed at least one opioid prescription. High‐risk veterans were defined as having an opioid prescription with at least one of the following: an opioid use disorder (OUD) and dependence diagnosis, at least one methadone prescription, a daily dose of 50 morphine equivalents or greater (50 MEDD), and Risk Index for Overdose or Serious Opioid‐induced Respiratory Depression (RIOSORD) class ≥5. The RIOSORD is a risk tool used by the VA to identify veterans at risk for respiratory depression due to opioid overdose; a class of 5 or greater is associated with a risk of 46 percent.21 See Appendix S1 for list diagnosis codes. Patient assignment to providers was based on the Patient Centered Management Module (PCMM), an enterprise application that assigns veterans to health care teams that deliver comprehensive care.22
3. DATA AND MEASURES
3.1. Data source
Station‐, provider‐, and patient‐level data were accessible using the VA Corporate Data Warehouse (CDW), the central repository for pharmacy, outpatient, inpatient, and staff data.23 Data on provider exposure to academic detailing were obtained from Salesforce.com®, an online cloud‐based platform designed for customer relationship management, data collection, and reporting. Academic detailers recorded their educational outreach activities with providers capturing the date the visit occurred, topics discussed, educational materials shared, and data tools used during the visit.
3.2. Dependent variable
The outcome for the primary aim was the total count of naloxone prescriptions prescribed, compiled from the CDW pharmacy claims data by month and aggregated by station. We also evaluated the station‐level prevalence of naloxone (number of naloxone prescribed per 1000 population) as part of the alternative analysis. Prior to the FDA approval of commercial forms of outpatient naloxone autoinjector (Evzio® 2014) and nasal spray (Narcan® 2016), the VA dispensed naloxone vials accompanied by a syringe or nasal atomizer as a kit.5 Hence, we included these formulations of naloxone in our total count. We did not include formulations of naloxone that contained buprenorphine (Suboxone®) due to its specific indication for OUD.
3.3. Predictor of interest
Academic detailing's implementation strength was measured as the proportion of providers who received OEND‐specific academic detailing at each station per month. We fixed the provider population at each station by using a closed cohort to generate consistent values of the proportion of providers who received OEND‐specific academic detailing. Therefore, newly hired providers could not enter the cohort and providers could not leave the cohort during the study period. The proportion of providers exposed to academic detailing represented the time‐varying measurement of academic detailing implementation strength at each station across time. Providers were categorized as exposed to academic detailing when they received their first educational OEND‐specific outreach visit with an academic detailer.
3.4. Analytic strategy
In the primary aim, we investigated the association between the proportion of providers exposed to academic detailing and the total number of naloxone prescriptions prescribed in a veteran population who received an opioid prescription (Model 1). Based on known opioid overdose risk factors, we evaluated the impact of implementation strength on several subgroups as part of our prespecified secondary aims.21 These subgroups included veterans categorized as high risk (Model 2), prescribed 50 MEDD or greater (Model 3), had a RIOSORD class of 5 or greater (Model 4), were diagnosed with an opioid use disorder or related substance abuse disorders (Model 5), and prescribed methadone (Model 6).
Descriptive analysis was performed on baseline characteristics of the station and provider cohorts. Continuous data were presented as means with standard deviations, and discrete data were presented as frequencies with percentages. We also measured the cumulative number of naloxone prescriptions prescribed between stations that had providers who received and did not receive an academic detailing visit.
Since the dependent variable was the total count of naloxone prescriptions prescribed, a log‐linear model was used to avoid errors in the estimators that may have occurred had we used ordinary least squared models.24 Initially, an unadjusted negative binomial regression model was used to evaluate the association between the proportion of providers exposed to academic detailing and the total number of naloxone prescriptions prescribed. We then used a fixed effects negative binomial regression to estimate the impact of the proportion of providers exposed to academic detailing on the monthly total naloxone prescriptions prescribed controlling for potential confounders.25 We controlled for station‐level time‐varying covariates in our regression models, which included the number of outpatient visits, number of emergency department and urgent care visits, number of inpatient admissions, and number of prescriptions released. Fixed effects regression models are advantageous in addressing omitted variable bias associated with unobserved station‐level time‐invariant covariates.25, 26 Outcomes were reported as incident rate ratios (IRR) with 95% confidence intervals (CI). We then estimated the marginal effect at different levels of the proportion of providers having experienced academic detailing (0 percent, 25 percent, 50 percent, 75 percent, and 100 percent). Model fit was determined using the Akaike information criterion and the Hosmer‐Lemeshow test. Details of the models used are provided in the Online Appendix.
We performed alternative analyses using a linear fixed effects model on the prevalence of naloxone prescribing (number of naloxone prescriptions prescribed per 1000 population at risk for opioid overdose) as the outcome variable and controlled for the same variables as in the fixed effects negative binomial model. This was performed to address concerns that the number of at‐risk veterans varied across different stations by normalizing the number of naloxone prescriptions prescribed per 1000 population. Results were presented as the average monthly prevalence with corresponding 95% CIs.
All analyses were performed using Stata 15.0 SE (Stata Corp).
4. RESULTS
Our analysis included 130 stations with 40 months of follow‐up for a maximum total of 5200 panel‐level observations. We used data that included a total of 5452 providers (Table 1) spread across 130 stations. Providers were on average 54.4 (9.5) years old (age data were missing for 935 providers); the majority were female (56 percent). All providers were in primary care and composed of physicians (72 percent), nurses (22 percent), and physician assistants (6 percent). A small proportion of primary care providers were also categorized as mental health providers (1 percent). Station‐level characteristics are summarized in Table 2. At the station‐level, there were, on average, 83 280 (SD 51 184) outpatient visits per month, 1714 (SD 1124) emergency department and urgent care visits per month, 492 (SD 384) inpatient admissions per month, and 93 592 (SD 54 618) prescriptions released per month.
Table 1.
Characteristics of primary care providers at the Veterans Health Administration, September 2014 to December 2017
| Variable | Providers (N = 5452) |
|---|---|
| Age (y), mean (SD) | 54.4 (9.5) |
| Male, n (%)a | 1944 (43.0%) |
| Primary care provider type | |
| Physicians, n (%) | 3940 (72.3%) |
| Physician assistants, n (%) | 298 (5.5%) |
| Nurse practitioner, n (%) | 1214 (22.3%) |
| Mental health providers, n (%) | 59 (1.1%) |
a935 providers with missing data.
Table 2.
Station‐level characteristics at the Veterans Health Administration, September 2014 to December 2017
| Variable | Mean | Overall SD | Between SD | Within SD |
|---|---|---|---|---|
| Age of providers (y) | 54.91 | 2.47 | 2.48 | 0.00 |
| Proportion of male providers | 0.44 | 0.12 | 0.12 | 0.00 |
| Proportion of physician assistants | 0.06 | 0.07 | 0.07 | 0.00 |
| Proportion nurse practitioners | 0.24 | 0.13 | 0.13 | 0.00 |
| Proportion mental health providers | 0.01 | 0.04 | 0.04 | 0.00 |
| Monthly number outpatient visits | 83 280 | 51 184 | 50 904 | 6929 |
| Monthly number of emergency department and urgent care visits | 1714 | 1125 | 1101 | 247 |
| Monthly number of inpatient admissions | 492 | 384 | 382 | 48 |
| Monthly number of prescriptions released | 93 592 | 54 618 | 54 517 | 5777 |
| Monthly number of unique detailers | 0.97 | 1.72 | 1.26 | 1.17 |
Abbreviations: MH, mental health provider; NP, nurse practitioner; PA, physician assistant; SD, standard deviation.
Implementation strength of academic detailing varied across stations (Appendix S3). Average station‐level proportion of providers exposed to academic detailing was 0.14 across the study period with an overall standard deviation of 0.23. The minimum proportion of providers exposed to academic detailing was 0.00 and the highest was 0.94. By the end of the study period, 27 stations (21 percent) did not have any exposure to OEND‐specific academic detailing. Overall, the average proportion of providers exposed to academic detailing increased across the study time period (Figure 1).
Figure 1.
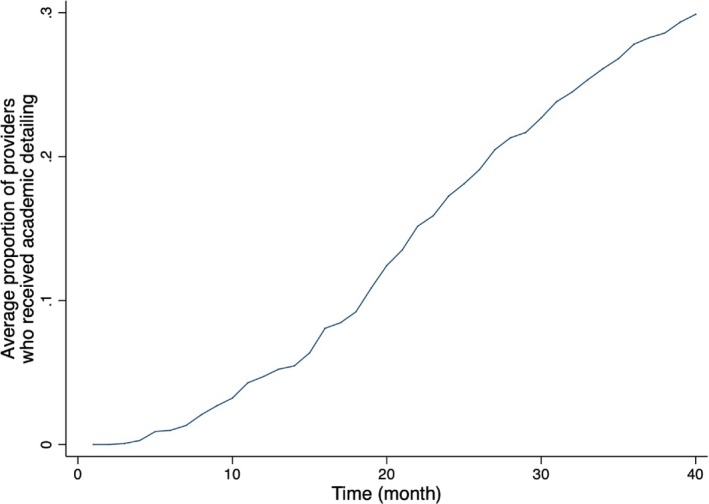
The average station‐level proportion of providers who received OEND‐specific academic detailing from September 2014 to December 2017. For the average station, the proportion of providers who received an OEND‐specific academic detailing educational outreach visit was 0.14 across the study period. The proportion of providers who received an academic detailing visit for each station ranged anywhere between 0.00 and 0.94. OEND, Opioid Overdose Education and Naloxone Distribution [Color figure can be viewed at wileyonlinelibrary.com]
Figure 2 illustrates the trends associated with the average number of naloxone prescriptions prescribed, average proportion of veterans who received naloxone, and the number of naloxone‐eligible veterans by different subgroups. Variations in the trends across different opioid overdose risk groups were apparent. In general, naloxone prescriptions prescribed and the proportion of naloxone‐eligible veterans who received naloxone increased as the number of veterans eligible to receive naloxone decreased over time. Average number of naloxone prescriptions prescribed per month remained constant for the OUD, and methadone subgroups. Few changes were observed in the number of naloxone‐eligible veterans for the methadone subgroup.
Figure 2.
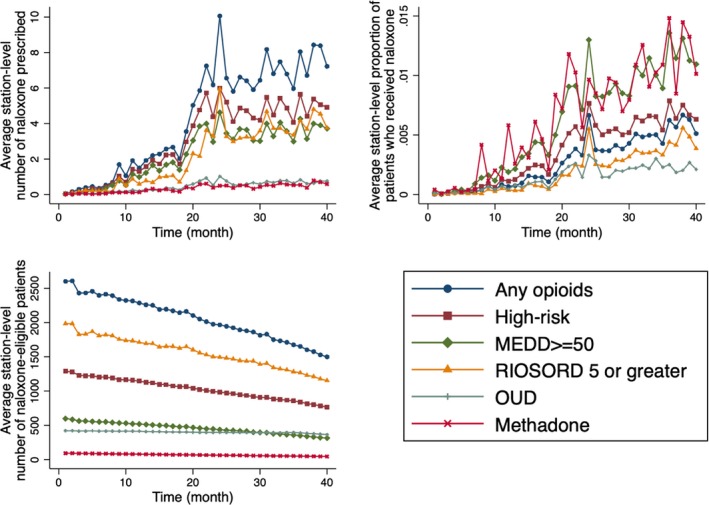
The average station‐level trends by different opioid overdose risk groups, September 2014 to December 2017. For the average station, the monthly number of naloxone prescriptions prescribed and proportion of veterans who received academic detailing increased as the monthly number of naloxone‐eligible veterans decreased from September 2014 to December 2017. MEDD, morphine equivalent daily dose; OUD, opioid use disorder; RIOSORD, risk index for overdose or serious opioid‐induced respiratory depression [Color figure can be viewed at wileyonlinelibrary.com]
4.1. Principle findings
In the crude analyses, there were significant associations between the proportion of providers exposed to academic detailing at each station and the number of naloxone prescriptions prescribed across the various subgroups of veterans. A summary of the main regression results is presented in Table 3. Additional details about the regression results are available in Appendices.
Table 3.
Station‐level results of the fixed effects negative binomial regression models by patient populations, September 2014 to December 2017
| Predictor of interest | (1) | (2) | (3) | (4) | (5) | (6) |
|---|---|---|---|---|---|---|
| Negative binomial unconditional (Opioid population) | Negative binomial unconditional (High‐risk population) | Negative binomial unconditional (MEDD 50 population) | Negative binomial unconditional (RIOSORD Class > 5 population) | Negative binomial unconditional (OUD population) | Negative binomial unconditional (Methadone population) | |
| N | 5200 | 5200 | 5200 | 5200 | 5197 | 5156 |
| Unadjusted model | ||||||
| Proportion of providers exposed to academic detailing | 4.92** (2.43, 9.99) | 5.24** (2.82, 9.74) | 5.16** (2.85, 9.31) | 6.02** (2.58, 14.07) | 4.12** (2.42, 7.03) | 3.42** (1.73, 6.75) |
| Adjusted modela | ||||||
| Proportion of providers exposed to academic detailing | 5.52* (1.87, 16.27) | 4.73* (1.73, 12.93) | 4.49* (1.58, 12.75) | 4.22* (1.16, 15.29) | 2.35 (0.88, 6.26) | 3.93 (0.93, 16.66) |
Results are presented as incident rate ratios (IRR) with 95% confidence intervals (CI).
aModels adjusted for time‐varying covariates (number of outpatient visits, number of emergency department and urgent care visits, number of inpatient admissions, and number of prescriptions released).
*P < 0.05, P < 0.01.
**P < 0.001.
4.1.1. Veterans prescribed an opioid prescription
Overall, among the opioid user population, the prevalence of naloxone prescriptions increased. In September 2014, the average number of naloxone prescriptions prescribed was 0.03 per 1000 population at risk for opioid overdose. By December 2017, the average number of naloxone prescriptions prescribed was 5.12 per 1000 population at risk for opioid overdose. Stations that had none of their providers exposed to academic detailing had a total of 3811 naloxone prescriptions prescribed between September 2014 and December 2017 (Appendix S4). During that same time period, stations that had providers exposed to academic detailing had a total of 18 603 naloxone prescriptions prescribed by their providers.
There was a significant association between the proportion of providers exposed to academic detailing and the total count of naloxone prescriptions at each station per month. In Model 1, a station with 100 percent of providers exposed to academic detailing was significantly associated with a 5.52 times higher incidence rate (95% CI: 1.87, 16.27) in the monthly number of naloxone prescriptions prescribed compared to a station with 0 percent of providers exposed to the intervention. Alternatively, we can interpret this as the marginal effect of increasing the proportion from 0 percent to 100 percent was a 9.13 increase in the number of naloxone prescriptions prescribed. We plotted the relationship between the marginal effect of the intervention at different levels of the proportion of providers exposed to OEND‐specific academic detailing (Appendix S5). As the proportion of providers exposed to academic detailing increased, the marginal effect of the intervention on the number of naloxone prescribed increased. In the alternative analysis (Appendix S6), a station with 100 percent of providers exposed was associated with a 2.60 increase in the monthly number of naloxone prescriptions prescribed per 1000 population at risk for opioid overdose compared to a station that was not exposed (95% CI: 1.00, 4.20).
4.2. Secondary aims
4.2.1. Veterans labeled as high risk
Overall, among high‐risk population, the prevalence of naloxone prescriptions increased. In September 2014, the average number of naloxone prescriptions prescribed was 0.06 per 1000 population at risk for opioid overdose. By December 2017, the average number of naloxone prescriptions prescribed was 6.31 per 1000 population at risk for opioid overdose. Stations that had none of their providers exposed to academic detailing had a total of 2961 naloxone prescriptions prescribed between September 2014 and December 2017. During that same time period, stations that had providers exposed to academic detailing had a total of 13 030 naloxone prescriptions prescribed by their providers (Appendix S4).
Model 2 evaluated a subgroup of veterans who were categorized as high risk of having an opioid overdose. In Model 2, a station with 100 percent of providers exposed to academic detailing was significantly associated with a 4.73 times higher incidence rate (95% CI: 1.73, 12.93) in the monthly number of naloxone prescriptions prescribed compared to a station with 0 percent of providers exposed to the intervention. Alternatively, we can interpret this as the marginal effect of increasing the proportion from 0 percent to 100 percent was a 5.26 increase in the number of naloxone prescriptions prescribed. Similar to the primary analysis, as proportion of providers exposed to academic detailing increased, the marginal effect of the intervention on the number of naloxone prescribed increased (Appendix S5). In the alternative analysis (Appendix S6), a station with 100 percent of providers exposed was associated with a 4.51 increase in the monthly number of naloxone prescriptions prescribed per 1000 population at risk for opioid overdose compared to a station that was not exposed (95% CI: 2.80, 6.23).
4.2.2. Veterans with 50 MEDD or greater
Overall, among veterans with 50 MEDD or greater, the prevalence of naloxone prescriptions increased. In September 2014, the average number of naloxone prescriptions prescribed was 0.11 per 1000 population at risk for opioid overdose. By December 2017, the average number of naloxone prescriptions prescribed was 10.93 per 1000 population at risk for opioid overdose. Stations that had none of their providers exposed to academic detailing had a total of 2321 naloxone prescriptions prescribed between September 2014 and December 2017 (Appendix S4). During that same time period, stations that had providers exposed to academic detailing had a total of 9632 naloxone prescriptions prescribed by their providers.
Model 3 evaluated a subgroup of veterans who were categorized having an MEDD of 50 or greater. In Model 3, a station with 100 percent of providers exposed to academic detailing was significantly associated with a 4.49 times higher incidence (95% CI: 1.58, 12.75) in the monthly number of naloxone prescriptions prescribed compared to a station with 0 percent of providers exposed to the intervention. Alternatively, we can interpret this as the marginal effect of increasing the proportion from 0 percent to 100 percent was a 3.75 increase in the number of naloxone prescriptions prescribed. There was a positive association between the marginal effect of the intervention with the different levels of exposure; however, the effect was not as steep as in the previous analyses (Appendix S5). In the alternative analysis (Appendix S6), a station with 100 percent of providers exposed was associated with a 7.45 increase in the monthly number of naloxone prescriptions prescribed per 1000 population at risk for opioid overdose compared to a station that was not exposed (95% CI: 4.71, 10.20).
4.2.3. Veterans with a RIOSORD class of 5 or greater
Overall, among veterans with RIOSORD class of 5 or greater, the prevalence of naloxone prescriptions increased. In September 2014, the average number of naloxone prescriptions prescribed was 0.02 per 1000 population at risk for opioid overdose. By December 2017, the average number of naloxone prescriptions prescribed was 3.86 per 1000 population at risk for opioid overdose. Stations that had none of their providers exposed to academic detailing had a total of 1652 naloxone prescriptions prescribed between September 2014 and December 2017 (Appendix S4). During that same time period, stations that had providers exposed to academic detailing had a total of 9715 naloxone prescriptions prescribed by their providers.
Model 4 evaluated a subgroup of veterans who were categorized having a RIOSORD class of 5 or greater. In Model 4, a station with 100 percent of providers exposed to academic detailing was significantly associated with a 4.22 times higher incidence (95% CI: 1.16, 15.29) in the monthly number of naloxone prescriptions prescribed compared to stations with 0 percent of providers exposed to the intervention. Alternatively, we can interpret this as the marginal effect of increasing the proportion from 0 percent to 100 percent was a 4.26 increase in the number of naloxone prescriptions prescribed. The positive association between the marginal effect of the intervention with the different levels of exposure continued to be reported with the subgroup of veterans with RIOSORD class of 5 or greater (Appendix S5). In the alternative analysis (Appendix S6), a station with 100 percent of providers exposed was associated with a 2.19 increase in the monthly number of naloxone prescriptions prescribed per 1000 population at risk for opioid overdose compared to a station that was not exposed (95% CI: 0.64, 3.73).
4.2.4. Veterans with opioid use disorder
Overall, among veterans with OUD, the prevalence of naloxone prescriptions increased. In September 2014, the average number of naloxone prescriptions prescribed was 0.11 per 1000 population at risk for opioid overdose. By December 2017, the average number of naloxone prescriptions prescribed was 2.11 per 1000 population at risk for opioid overdose. Stations that had none of their providers exposed to academic detailing had a total of 412 naloxone prescriptions prescribed between September 2014 and December 2017 (Appendix S4). During that same time period, stations that had providers exposed to academic detailing had a total of 1972 naloxone prescriptions prescribed by their providers.
Model 5 evaluated a subgroup of veterans who were categorized having an OUD diagnosis. In Model 5, a station with 100 percent of providers exposed to academic detailing was nonsignificantly associated with a 2.35 times higher incidence (95% CI: 0.88, 6.26) in the monthly number of naloxone prescriptions prescribed compared to stations with 0 percent of providers exposed to the intervention. Alternatively, we can interpret this as the marginal effect of increasing the proportion from 0 percent to 100 percent was a 0.40 increase in the number of naloxone prescriptions prescribed. The positive association between the marginal effect of the intervention with the different levels of exposure continued to be reported with the subgroup of veterans with OUD subgroup (Appendix S5). In the alternative analysis (Appendix S6), a station with 100 percent of providers exposed was associated with a 1.23 increase in the monthly number of naloxone prescriptions prescribed per 1000 population at risk for opioid overdose compared to a station that was not exposed (95% CI: 0.27, 2.19).
4.2.5. Veterans with methadone
Overall, among veterans with methadone, the prevalence of naloxone prescriptions increased. In September 2014, the average number of naloxone prescriptions prescribed was 0.41 per 1000 population at risk for opioid overdose. By December 2017, the average number of naloxone prescriptions prescribed was 10.13 per 1000 population at risk for opioid overdose. Stations that had none of their providers exposed to academic detailing had a total of 409 naloxone prescriptions prescribed between September 2014 and December 2017 (Appendix S4). During that same time period, stations that had providers exposed to academic detailing had a total of 1356 naloxone prescriptions prescribed by their providers.
Model 6 evaluated a subgroup of veterans who were categorized having a methadone prescription. In Model 6, a station with 100 percent of providers exposed to academic detailing was nonsignificantly associated with a 3.93 times higher incidence (95% CI: 0.93, 16.66) in the monthly number of naloxone prescriptions prescribed compared to stations with 0 percent of providers exposed to the intervention. Alternatively, we can interpret this as the marginal effect of increasing the proportion from 0 percent to 100 percent was a 1.19 increase in the number of naloxone prescriptions prescribed. Although there continued to be a positive relationship between the marginal effect of the intervention and the different levels of exposure, this was mitigated in the methadone subgroup population (Appendix S5). In the alternative analysis (Appendix S6), a station with 100 percent of providers exposed was associated with a 5.00 increase in the monthly number of naloxone prescriptions prescribed per 1000 population at risk for opioid overdose compared to a station that was not exposed (95% CI: −0.18, 10.18).
5. DISCUSSION
Partnership between the VA OEND program and the Academic Detailing Service has contributed to a noticeable increase in naloxone distribution; VA has dispensed over 100 000 naloxone prescriptions to over 90 000 veterans by the end of November 2017.27 A previous study reported that providers exposed to OEND‐specific academic detailing prescribed a greater number of naloxone prescriptions compared to providers who were not exposed, but did not account for the impact of implementation.17 Our study takes this further by evaluating the strength (or intensity) of implementation in the form of the proportion of providers who received OEND‐specific academic detailing.
These findings highlight the importance of implementation's role in scaling up a national program for academic detailing and OEND. Despite a mandate by the Interim Under Secretary of Health that sites implement academic detailing,16 there were 27 (21 percent) stations that had 0 percent of providers who received an OEND‐specific academic detailing educational outreach visit at the time of this evaluation. Implementing academic detailing at these stations would significantly improve naloxone distribution to veterans who are at risk for opioid‐related overdose events.
We can only hypothesize what type of implementation issues prevented a uniform and rapid diffusion of academic detailing across the VA. It is critical that further investigation include a qualitative analysis to identify themes associated with barriers to rapid diffusion of academic detailing at VA stations with low proportion of providers exposed to the intervention. Rurality and distance from the VA Medical Centers or CBOCs are potential reasons that could limit provider exposure to academic detailing, and advances in video‐based communication may be viable solutions to increase penetration into these difficult areas. Currently, the VA is investigating the feasibility to provide educational outreach to providers using VA Video Connect systems.28 However, it is unclear whether a virtual approach will alter the effect of a one‐on‐one encounter between a provider and an academic detailer. Future analysis will need to address these issues to deepen our understanding about the implementation elements of academic detailing that are effective at promoting naloxone prescribing behavior changes.
We were unable to determine what unique barriers each station experienced when implementing academic detailing. These could potentially impact program success and influence the number of naloxone prescriptions prescribed. We used a fixed effects model in our analysis to address this omitted variable bias by including station‐level fixed effects.26 As long as these unobserved fixed effects are consistent at the station level, then the fixed effects model can generate unbiased estimators of the treatment effect. However, if there are any changes in the unobserved station‐level characteristics over time that we cannot control for (eg, quality and motivation to support academic detailing), the estimators from the fixed effects model will be biased.
During the study period, the VA implemented other strategies to address the opioid epidemic such as the OSI to reduce opioid overuse. Recently, from mid‐2012 to mid‐2016, there was a 25 percent reduction in the number of opioids dispensed per quarter, a 47 percent reduction in the number of veterans on concomitant benzodiazepine and opioid prescriptions, and a 36 percent reduction in the number of veterans receiving opioids doses of 100 MEDD or greater.4 In our study, we reported a decrease in the number of veterans eligible to receive naloxone likely due to other strategies implemented by the VA. While controlling for these time‐varying covariates, we reported a significant increase in monthly total naloxone prescriptions prescribed at stations that implemented academic detailing.
On March 1, 2018, the White House Opioid Summit brought health care key leaders together to discuss strategies that the federal government employs to address the opioid crisis. Dr. Shulkin, former Secretary of the Department of Veterans Affairs, disclosed the S.T.O.P. P.A.I.N. initiative, which is a multifaceted approach to address the opioid crisis by using academic detailing alongside other best practice strategies including the OEND program to target providers and align them with evidence‐based practice for pain management.29 The goals of the Academic Detailing Service and the OEND program were to perform educational outreach visits with providers who care for patients at risk for opioid‐related overdose with the goal of improving their access to take‐home naloxone. The findings from this study support the policies that were recently enacted by the VA and provide empirical support that OEND‐specific academic detailing contributed to increased naloxone prescriptions and potentially reduced opioid overdose mortality.
Successful implementation involves many factors;30, 31 however, it is challenging to generate implementation metrics that properly capture its impact on a program's outcome. We decided to use proportion of providers who received OEND‐specific academic detailing to represent implementation strength due to the availability of data. We did not have data on implementation fidelity, quality, and adaptability, which are informative when assessing the program's impact on naloxone prescribing.30 Regardless, we took advantage of this natural experiment and focused on implementation strength to represent the quantity of academic detailing delivered as well as penetration into each station, which enabled us to capture the impact of implementation strength on naloxone prescribing.
In our secondary aim, we ran a series of subgroup analyses using different patient populations at risk for opioid overdose to test the sensitivity of our findings. Our conclusions were consistent with the primary findings when evaluating veterans who were prescribed an opioid categorized as high risk, who received 50 MEDD or greater, and had a RIOSORD class ≥5. However, among veterans who had an opioid use disorder diagnosis or were on methadone, the association between the predictor of interest (proportion of providers exposed to academic detailing) and outcome (total count of naloxone prescriptions prescribed) was not significant. One possible explanation is that patient groups that did not yield significant associations may have inherent characteristics that were not considered in these models. Additionally, pharmacists were excluded as providers even though 41 percent of pharmacists have prescribing privileges.20 Not all pharmacists are considered providers at the VA, and their duties were not easily determined from the current data. Moreover, pharmacists with prescribing authorization also wrote orders on behalf of other providers, which would have inflated their numbers. We could not confidently assess whether pharmacists were prescribing naloxone due to their own prescriptive authority or because they were fulfilling orders for another provider. Hence, we removed them in order to reduce this potential bias.
Finally, the findings from our study were generated from the VA population, which has a greater overdose mortality rate compared to the general U.S. population.3 Although veterans have other comorbid conditions that differentiate them from the general population, these findings may help to inform decision makers about the merits of academic detailing's role in increasing naloxone distribution in large, integrated health care systems similar to the VA.
6. CONCLUSIONS
This was the first study to evaluate academic detailing's implementation strength on naloxone prescriptions prescribed at the VA. Stations with larger proportion of providers who received an OEND‐specific academic detailing educational outreach visit had a greater amount of naloxone prescriptions prescribed. Successful implementation of academic detailing is critical in getting naloxone prescriptions to veterans at risk for opioid overdose. Failure to implement academic detailing denies veterans at risk for opioid overdose from necessary treatment and minimizes the ability of the VA to fulfill President Lincoln's promise: “To care for him who shall have borne the battle, and for his widow, and his orphan.” The insights gained from these findings will help decision makers develop implementation strategies in order to achieve meaningful outcomes.
Supporting information
ACKNOWLEDGMENTS
Joint Acknowledgment/Disclosure Statement: We would like to acknowledge the Veterans Health Administration Pharmacy Benefits Management leadership, Virginia Torrise and Michael Valentino, for their support and promotion of academic detailing. We also want to thank Elizabeth M. Oliva for collaborating with us on the Opioid Overdose Education and Naloxone Distribution (OEND) program at the VA. Finally, the comments from the peer reviewers were instrumental in improving our manuscript; we are grateful for their time and advice. No other disclosures.
Bounthavong M, Devine EB, Christopher MLD, Harvey MA, Veenstra DL, Basu A. Implementation evaluation of academic detailing on naloxone prescribing trends at the United States Veterans Health Administration. Health Serv Res. 2019;54:1055–1064. 10.1111/1475-6773.13194
REFERENCES
- 1. National Institute on Drug Abuse . Overdose Death Rates. 2018. https://www.drugabuse.gov/related-topics/trends-statistics/overdose-death-rates. Accessed August 18, 2018.
- 2. Bohnert ASB, Ilgen MA, Galea S, McCarthy JF, Blow FC. Accidental poisoning mortality among patients in the Department of Veterans Affairs Health System. Med Care. 2011;49(4):393‐396. [DOI] [PubMed] [Google Scholar]
- 3. Bohnert ASB, Ilgen MA, Trafton JA, et al. Trends and regional variation in opioid overdose mortality among Veterans Health Administration patients, fiscal year 2001 to 2009. Clin J Pain. 2014;30(7):605‐612. [DOI] [PubMed] [Google Scholar]
- 4. Gellad WF, Good CB, Shulkin DJ. Addressing the opioid epidemic in the United States: lessons from the Department of Veterans Affairs. JAMA Intern Med. 2017;177(5):611‐612. [DOI] [PubMed] [Google Scholar]
- 5. Oliva EM, Christopher MLD, Wells D, et al. Opioid overdose education and naloxone distribution: development of the Veterans Health Administration's national program. J Am Pharm Assoc (2003). 2017;57(2S):S168‐S179.e4. [DOI] [PubMed] [Google Scholar]
- 6. Lin LA, Bohnert ASB, Kerns RD, Clay MA, Ganoczy D, Ilgen MA. Impact of the opioid safety initiative on opioid‐related prescribing in veterans. Pain. 2017;158(5):833‐839. [DOI] [PubMed] [Google Scholar]
- 7. Coffin PO, Behar E, Rowe C, et al. Nonrandomized intervention study of naloxone coprescription for primary care patients receiving long‐term opioid therapy for pain. Ann Intern Med. 2016;165(4):245‐252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Beletsky L, Rich JD, Walley AY. Prevention of fatal opioid overdose. JAMA. 2012;308(18):1863‐1864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Binswanger IA, Koester S, Mueller SR, Gardner EM, Goddard K, Glanz JM. Overdose education and naloxone for patients prescribed opioids in primary care: a qualitative study of primary care staff. J Gen Intern Med. 2015;30(12):1837‐1844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Matheson C, Pflanz‐Sinclair C, Aucott L, et al. Reducing drug related deaths: a pre‐implementation assessment of knowledge, barriers and enablers for naloxone distribution through general practice. BMC Fam Pract. 2014;15:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Farhadian S, Yee MV, Christopher MLD. Fostering the use of clozapine in the severely mentally ill through academic detailing. Mental Health Clinician. 2011;1(5):94‐98. [Google Scholar]
- 12. Fischer MA, Avorn J. Academic detailing can play a key role in assessing and implementing comparative effectiveness research findings. Health Aff. 2012;31(10):2206‐2212. [DOI] [PubMed] [Google Scholar]
- 13. Avorn J. Learning about the safety of drugs–a half‐century of evolution. N Engl J Med. 2011;365(23):2151‐2153. [DOI] [PubMed] [Google Scholar]
- 14. Soumerai SB, Avorn J. Principles of educational outreach (‘academic detailing’) to improve clinical decision making. JAMA. 1990;263(4):549‐556. [PubMed] [Google Scholar]
- 15. Avorn J, Soumerai SB. Improving drug‐therapy decisions through educational outreach. A randomized controlled trial of academically based “detailing”. N Engl J Med. 1983;308(24):1457‐1463. [DOI] [PubMed] [Google Scholar]
- 16. US Congressional House Committee on Veterans’ Affairs . Statement of Dr. Carolyn Clancy Interim Secretary for Health Veterans Health Administration Department of Veterans Affairs Before the Subcommittee on Oversight and Investigations Committee on Veterans’ Affairs United States House of Representatives. Washington, DC. 2015.
- 17. Bounthavong M, Harvey MA, Wells DL, et al. Trends in naloxone prescriptions prescribed after implementation of a National Academic Detailing Service in the Veterans Health Administration: a preliminary analysis. J Am Pharm Assoc (2003). 2017;57(2):S68‐S72. [DOI] [PubMed] [Google Scholar]
- 18. US Department of Veterans Affairs . About VHA ‐ Veterans Health Administration. 2018. https://www.va.gov/health/aboutVHA.asp. Accessed March 19, 2018.
- 19. U.S. Department of Veterans Affairs . Veterans Health Administration Fiscal Year 2017 Annual Report: Modernizing Veteran Health Care. Washington, DC: U.S. Department of Veterans Affairs; 2018. [Google Scholar]
- 20. Ourth H, Groppi J, Morreale AP, Quicci‐Roberts K. Clinical pharmacist prescribing activities in the Veterans Health Administration. Am J Health Syst Pharm. 2016;73(18):1406‐1415. [DOI] [PubMed] [Google Scholar]
- 21. Zedler B, Xie L, Wang L, et al. Risk factors for serious prescription opioid‐related toxicity or overdose among Veterans Health Administration patients. Pain Med. 2014;15(11):1911‐1929. [DOI] [PubMed] [Google Scholar]
- 22. US Department of Veterans Affairs . Patient Centered Management Module (PCMM) For Primary Care. Veterans Health Administration Director 1406. Washington, DC: US Department of Veterans Affairs; 2017. [Google Scholar]
- 23. US Department of Veterans Affairs . 172VA10P2: VHA Corporate Data Warehouse – VA. 79 FR 4377. Department of Veterans Affairs; 2017.
- 24. Hilbe JM. Negative Binomial Regression, 2nd ed Cambridge, UK: Cambridge University Press; 2013. [Google Scholar]
- 25. Allison PD, Waterman RP. Fixed‐effects negative binomial regression models. Sociol Methodol. 2002;32(1):247‐265. [Google Scholar]
- 26. Allison PD. Fixed Effects Regression Models, 1st ed Thousand Oaks, CA: SAGE Publications, Inc.; 2009. [Google Scholar]
- 27. U.S. Department of Veterans Affairs . Opioid overdose education and naloxone distribution. Office of Research & Development. 2018. https://www.research.va.gov/research_in_action/Opioid-overdose-education-and-naloxone-distribution.cfm. Accessed May 12, 2018.
- 28. US Department of Veterans Affairs . VA Video Connect. 2018. https://mobile.va.gov/app/va-video-connect. Accessed May 13, 2018.
- 29. US Department of Veterans Affairs Office of Public and Intergovernmental Affairs . VA Answers Governor Christie's Call on Opioid, Launches S.T.O.P. P.A.I.N Advices and Guidelines. 2017. https://www.va.gov/opa/pressrel/pressrelease.cfm?xml:id=2934. Accessed March 21, 2018.
- 30. Durlak JA, DuPre EP. Implementation matters: a review of research on the influence of implementation on program outcomes and the factors affecting implementation. Am J Commun Psychol. 2008;41(3–4):327‐350. [DOI] [PubMed] [Google Scholar]
- 31. Hoekstra F, van Offenbeek MAG, Dekker R, et al. Implementation fidelity trajectories of a health promotion program in multidisciplinary settings: managing tensions in rehabilitation care. Implement Sci. 2017;12: 143. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


