Abstract
Objective
To compare rates of attestation and attrition from the MU program by independent, horizontally integrated, and vertically integrated physicians and to assess whether MU created pressure for independent physicians to join integrated organizations.
Data Source/Study Setting
Secondary Data from SK&A and Medicare MU Files, 2011‐2016. Office‐based physicians in the 50 United States and District of Columbia.
Study Design
We compared attestation rates among physicians that remained independent or integrated throughout the study period. We then assessed the association between changing integration and MU attestation in multivariate regression models.
Principal Findings
Our sample included 291 234 physicians. Forty nine percent of physicians that remained independent throughout the period attested to MU at least once during the program, compared with 70 percent of physicians that remained horizontally or vertically integrated physicians. Only approximately 50 percent of independent physicians that attested between 2011 and 2013 attested in 2015, representing significantly more attrition than we observed among integrated physicians. In multivariate regression models, physicians that joined these organizations were more likely to have attested to MU prior to integrating and this difference increased following integration.
Conclusions
These findings point toward a growing digital divide between physicians who remain independent and integrated physicians that may have been exacerbated by the MU program. Targeted public policy, such as new regional extension centers, should be considered to address this disparity.
Keywords: electronic health records, incentive programs, physician integration
1. INTRODUCTION
Physicians have been gradually moving from small independent practices to larger organizations for decades,1, 2, 3 spurred in part by increasing complexity in the health care delivery system.4, 5 Electronic health records (EHRs), and the public policies creating pressure for their adoption, present challenges for independent practices. Relative to larger integrated organizations with established information technology departments, independent practices may not have the capital or capabilities to adopt, use, and upgrade high‐quality EHR systems.6, 7
Motivated by a belief that EHRs could significantly increase the quality of health care and were being adopted too slowly, policymakers developed the Meaningful Use (MU) program to create additional incentives for providers to adopt highly functional EHRs.8, 9 Beginning in 2011, the MU program provided financial incentives for the adoption of certified electronic health records and the use of those systems to meet specific criteria,8 and many physicians participated in the early years of the program.10 Nevertheless, throughout the MU program, there was widespread concern that independent physicians faced greater barriers to qualifying for MU incentives than did physicians in integrated provider organizations.11, 12, 13 The design of the program, which was intended to proceed across three stages with progressively higher thresholds and lower financial incentives, led to fears that even those smaller practices that successfully attested in early years might struggle to remain in compliance with the program or simply choose not to.14, 15
Given these pressures, the MU program likely altered incentives for both independent physicians and the larger organizations that could acquire them, and prior work has demonstrated that organizational structures can relate closely to EHR strategies.16, 17, 18 Independent physicians that were the least well positioned to engage in MU—those that either used an out of date EHR or no EHR—faced potentially strong incentives to join an integrated organization to qualify for MU. If assistance attesting to MU was a strong motivation for integration, independent physicians that joined an integrated organization would have been unlikely to attest prior to integration and much more likely to attest following integration. Meanwhile, integrated provider organizations could have been more interested in acquiring practices with existing technological competency in order to minimize the costs of assimilation and meeting MU goals. If this selective acquisition occurred, differences in MU attestation by organizational affiliation may emerge because organizations are selecting more technologically advanced and MU‐compliant practices, rather than helping practices attest to MU. This selectivity may leave independent physicians that lacked the capabilities to upgrade to MU‐compliant EHRs without the option of joining an organization that could help them meet MU attestation or otherwise adapt to ongoing policy and delivery system change.
In this context, we sought to describe the interaction between physicians’ organizational affiliations and their ability to achieve and sustain MU benchmarks over the course of the program (2011‐2016). To do so, we combined data on physicians’ attestation to MU with national physician practice survey data from SK&A. We then aimed to characterize differences in independent and integrated physicians’ MU attestation rate and attrition from the program after initially attesting. We also examined whether physicians were more likely to attest to MU after they transitioned into an integrated provider structure, or whether larger provider organizations targeted physicians that attested to MU.
2. DATA AND METHODS
2.1. Data sets
We combined data on ambulatory physician integration status with Medicare MU Attestation data and Medicare payment data. Data on ambulatory physicians were from a commercial research firm, SK&A, and included the years 2011, 2013, and 2015, with more than 500 000 physicians represented in each year of the data. SK&A aims to collect information on all office‐based physician practices in the United States via regularly scheduled phone interviews, and this data source has previously been used to measure physician EHR adoption, practice characteristics, and physician integration behavior.19, 20, 21 We used physician's national provider identifiers (NPIs) to combine these data with the Medicare MU Attestation Eligible Professionals Public Use Files (PUF) (https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/PUF.html) and the Medicare Provider Utilization and Payment Data. The MU files contain data on individual physician attestation to MU in each year of the program from 2011 to 2016, while the payment data contain information on whether the physician received Medicare payment in each year 2012‐2016, a key inclusion criteria.
2.2. Population
Our population of interest was all physicians (MDs and DOs) that were eligible to receive MU subsidies throughout the program. The population therefore excluded some doctorate‐holding clinical providers (including Dentists, Chiropractors, and Psychologists) that were eligible.
To facilitate analysis of changing MU and integration status over time, we constructed a balanced panel of physicians that received Medicare payments (and therefore were eligible for MU) in every year public payment data were available (2012‐2016) and were in the SK&A survey every year. Excluding physicians that did not receive payments in every year reduced our sample size to 394,187 (Waterfall diagram depicting sample definition is presented as Figure S1). The vast majority of excluded physicians are from specialties not typically caring for Medicare beneficiaries (eg, pediatrics, neonatology, and obstetrics). We next excluded physicians that were not present in all years of the SK&A survey, which further reduced the sample to 291 234 physicians. These exclusion criteria disproportionately targeted specialties likely to have intermittent office‐based practice (such as anesthesiologists, internal medicine physicians [who may practice as hospitalists], and emergency medicine physicians).
2.3. MU attestation
Our key dependent variable was Medicare MU attestation in each year of the program from 2011 to 2016.
2.4. Physician organizational status
We divided physicians into three organizational statuses: independent, horizontally integrated, and vertically integrated. In each year, we coded physicians as independent if they were not listed as working for a group medical practice or health system in the SK&A. We defined physicians as horizontally integrated if they were listed as working within at least one site owned or managed by a group medical practice but not at a site owned or managed by a health system. We defined physicians as vertically integrated if they worked within at least one site owned or managed by a health system.
2.5. Analytic plan
2.5.1. MU attestation among physicians with persistent organizational status
We first created three subgroups of physicians using the SK&A practice organization information. We selected those physicians with a consistent integration status of independent, horizontal, or vertical over our study period and excluded physicians whose integration status changed during the study period (representing 28.6 percent of the sample)—that is, we eliminated those that transitioned between organizational types. Once we identified these three groups, we calculated the percent of physicians in each group that attested to MU in any year of the program (ie, the cumulative proportion, which has been used by federal agencies to monitor MU participation22) and the percent of physicians in each group that attested to MU in each year of the program to identify whether physicians that were part of integrated provider organizations were more successful than independent physicians in attesting to MU.
2.5.2. MU attrition among physicians with persistent organizational status
To determine whether providers’ attrition from the MU program over time varied across integration status, we next developed cohorts of attesters according to the first year of MU achievement. We focused on three cohorts of physicians: those that first attested in 2011, 2012, and 2013, respectively. Paralleling our previous analysis, we also maintained our three, mutually exclusive physician organizational groupings. Then, for each cohort, we calculated the percent of physicians in each cohort that reached the MU benchmarks within each remaining year of the program (ie, through 2016). These measures speak to the ability of physicians to sustain their MU participation, especially during the more demanding later years of the program. Just as before, heterogeneity across organizational groups may reveal how different practices with varying levels of resources and expertise were able to cope with tougher health IT requirements.
2.5.3. MU association with integration change
To understand the relationship between changing integration status and MU attestation, we employed physician‐level fixed effect panel regressions where the key dependent variable was MU attestation in each year and the key independent variables were (time‐varying) horizontal and vertical integration binary indicators. We also included three additional sets of covariates: practice size (defined as the number of physicians working at the specific practice location, as opposed to the organization overall), whether the physician accepted Medicaid, and year fixed effects. The subsequent coefficients for our integration variables captured the within‐physician correlation between becoming horizontally or vertically integrated and meeting MU requirements. We used heteroskedastic robust standard errors to account for different variance by physician practice membership.
However, the resulting association could be misleading since integrated provider organizations do not randomly choose physician practices to purchase (eg, as noted before, they may target the more technologically savvy independent providers). To investigate a role for strategic selection, we isolated physicians that newly integrated in 2015. We then carried out an event study‐style analysis by comparing attestation rates of this specific subset of physicians in each year against (a) those who remained independent throughout our study period—that is, the “always independent” group defined in our initial analyses and, in supplemental analyses, (b) those that were consistently integrated throughout our study period (the “always horizontal integrated” and “always vertically integrated” groups defined in our initial analyses). The regression models (presented in the appendix) included an interaction term between an indicator variable for changing integration status in 2015 and each individual year—along with our other time‐varying covariates: practice size, whether the physician accepts Medicaid patients, gender, specialty, and practice location. This allowed us to observe how MU attestation evolved for these physicians relative to their comparators before they were owned by a larger entity—in other words, to identify whether trends in MU attestation were parallel across physicians that eventually integrated and those that remained independent prior to the potential change in integration. An increasing difference in attestation rate between physicians that remain independent and physicians that eventually integrate in 2015 during the preceding years (2011‐2013) would provide evidence that integrated organizations were selectively acquiring more technologically competent physician practices, on average. Stable or decreasing difference between these groups, on the other hand, would favor an opposite interpretation: integration was helping physicians achieve the MU standards.
In supplemental analyses, we assessed whether trends related to MU attestation and integration differed for primary care physicians and specialists, were similar when including a 1‐year lag (to allow time for EHR change following integration), and whether our results were robust to exclusion of physicians that accepted Medicaid patients, who may have participated in the Medicaid MU program in some years.
3. RESULTS
3.1. Trends in MU attestation by physician integration status
We summarize some key organizational features of our analytic panel in Table S1. Physicians that remained independent throughout the period were the most common type in the data, representing roughly 28 percent of all respondents in the analytic sample. These physicians also made up a disproportionate share of small practices, primary care specialists and physicians that did not have an EHR. Newly formed horizontal integration played a modest role over this time, while vertical integration affected three times the number of physicians (6.0 percent compared with 18 percent).
By 2016, 62.6 percent of physicians in our sample attested to Meaningful Use in at least 1 year. The proportion of physicians that attested to MU rapidly increased during 2011‐2013, and that increase was most pronounced among integrated physicians (Figure 1). Throughout the study period, physicians that remained independent were far less likely to attest to MU, and only 49 percent had participated in any year of the MU program by its conclusion, while about 70 percent of horizontally and vertically integrated physicians had participated at least once (Figure 1, top panel). These differences were larger when we examined whether physicians attested in each year of the program (Figure 1, bottom panel). Horizontally and vertically integrated practices were between 62 and 63 percent more likely to attest to MU than independent physicians in 2013, the year when the highest number of physicians attested overall. By 2016, this gap had expanded, such that both vertically integrated physicians and horizontally integrated physicians were roughly twice as likely (119 percent and 86 percent, respectively) to attest to MU than independent physicians.
Figure 1.
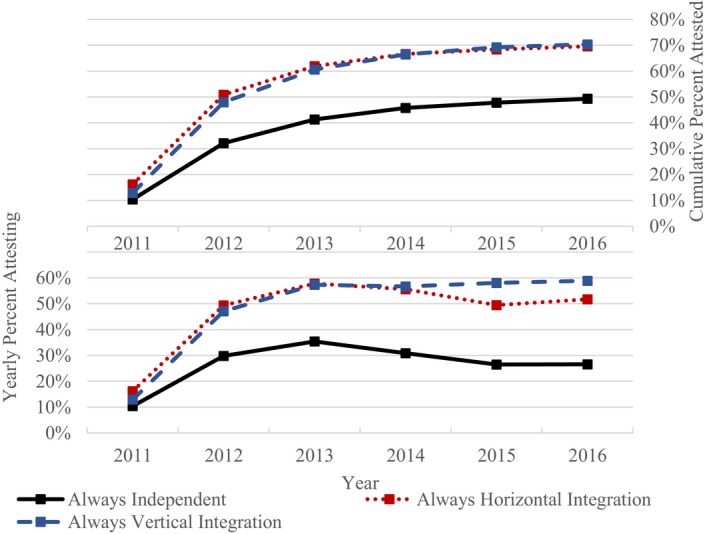
Meaningful use attestation rate by integration status, 2011‐2016. Each point is the (unadjusted) percent of physicians in each group that attested to Meaningful Use in each year. The sample includes 81 698 physicians that were always independent, 58 893 physicians that were always horizontally integrated, and 69 268 physicians that were always vertically integrated. Data are from the SK&A physician office survey for 2011, 2013, and 2015 and Meaningful Use Public Use Attestation Files 2011‐2016 [Color figure can be viewed at wileyonlinelibrary.com]
Figure 2 shows striking attrition from the MU program as criteria for attesting became more challenging and incentive payments decreased. This attrition was especially pronounced among independent physician practices. By 2015, the first year that most physicians were required to achieve the more challenging MU “Stage 2,” only about half of independent physicians that attested in prior years (2011, 2012, and 2013) attested. In contrast, between 65 percent and 76 percent of horizontally integrated physicians that had previously attested and between 82 percent and 86 percent of vertically integrated physicians remained in the program in the final years (2015 and 2016).
Figure 2.
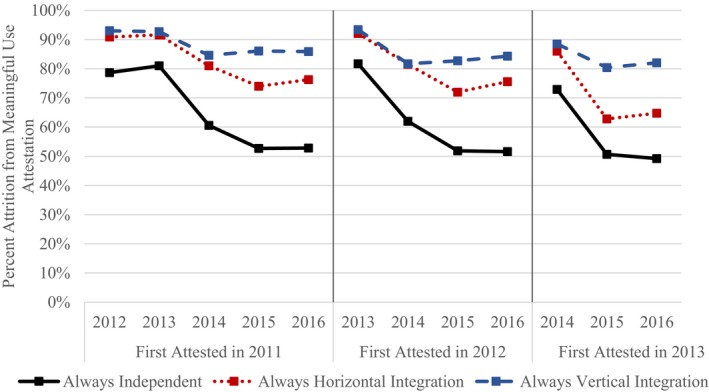
Attrition from meaningful use program, by year first attested and organization type. 119 160 physicians attested to MU by 2013 and had constant integration status. Each point represents the percent of physicians in each integration group that attested to MU in each year, by year of first attestation. Data are from the SK&A physician office survey for 2011, 2013, and 2015 and Meaningful Use Public Use Attestation Files 2011‐2016 [Color figure can be viewed at wileyonlinelibrary.com]
In stratified analyses, independent primary care physicians appeared somewhat less likely to attest and more likely to leave MU than independent specialists (Figures S2 and S3).
3.2. Integration status changes and MU success
Next, we examined the association between newly integrating with a larger organization and the likelihood of meeting MU goals (Table 1). In our physician fixed effects model, becoming horizontally integrated was associated with a 1.9 percentage point increase (5.0 percent relative increase, P < 0.001) in the likelihood of attesting to MU and becoming vertically integrated was associated with a 5.8 percentage point increase (15.5 percent relative increase, P < 0.001). These associations were also stronger among physicians that were part of small and independent practices prior to the introduction of the MU program (Table 1, column 2). The magnitude of the association between both types of integration statuses and MU attestation roughly doubled (to 11.7 percentage points for vertical integration and 3.9 percentage points for horizontal integration P < 0.001 for both), suggesting that this specific subset of physicians drove the overall relationship observed in column 1 of Table 1. Similarly, among primary care physicians the association between MU attestation and horizontal integration doubled while the association with vertical integration increased by over 50 percent (Table S4, column 1). Trends for specialists were roughly equivalent to the trends observed for all physicians (Table S2, column 2). The integration coefficients were highly statistically significant in all models.
Table 1.
Fixed effects regression of integration status on MU attestation
| (1) | (2) | |
|---|---|---|
| All physicians | Small, independent in 2009 | |
| Vertical integration | 0.058*** (0.002) | 0.117*** (0.004) |
| Horizontal Integration | 0.019*** (0.002) | 0.039*** (0.004) |
| Year (Omitted: 2011) | ||
| 2012 | 0.277*** (0.001) | 0.223*** (0.002) |
| 2013 | 0.354*** (0.001) | 0.281*** (0.002) |
| 2014 | 0.332*** (0.001) | 0.247*** (0.002) |
| 2015 | 0.306*** (0.001) | 0.208*** (0.002) |
| 2016 | 0.317*** (0.001) | 0.214*** (0.002) |
| Practice size (Omitted: Solo) | ||
| 2‐5 | 0.011*** (0.002) | 0.017*** (0.003) |
| 6‐9 | 0.017*** (0.003) | 0.057*** (0.007) |
| 10‐19 | 0.014*** (0.003) | 0.065*** (0.009) |
| 20‐49 | 0.015*** (0.003) | 0.060*** (0.014) |
| 50+ | 0.006 (0.005) | 0.056** (0.028) |
| Accepts Medicaid | −0.009*** (0.001) | 0.002 (0.002) |
| Constant | 0.102*** (0.002) | 0.088*** (0.002) |
| Observations | 1 747 404 | 532 464 |
| R‐squared | 0.140 | 0.091 |
| Number of NPI | 291 234 | 88 744 |
Robust standard errors in parentheses.
***P < 0.01.
**P < 0.05.
Despite the compelling patterns that emerged in Table 1, our event study analyses (Figure 3) offered some key nuance for interpreting these findings. When we compared independent physicians that integrated between 2013 and 2015 with those that remained independent, we observed that MU attestation trends were not parallel prior to the integration. Instead, physicians who would eventually integrate by 2015 were strongly trending away from physicians that remained independent (regression results reported in Figure S3). Looking across the two integration types, “future integrators” were 6‐15 percentage points (16.6 percent‐44.3 percent relative difference) more likely to attest to MU in 2013 (ie, prior to the integration) than were physicians who remained independent (P < 0.001 in all comparisons). In supplementary analyses, physicians who transitioned from independent to vertically integrated in 2015 were less likely to have attested in 2013 than were physician who remained vertically integrated throughout, while physicians who horizontally integrated in 2015 were approximately equally likely to have attested in 2013 (Table S3).
Figure 3.
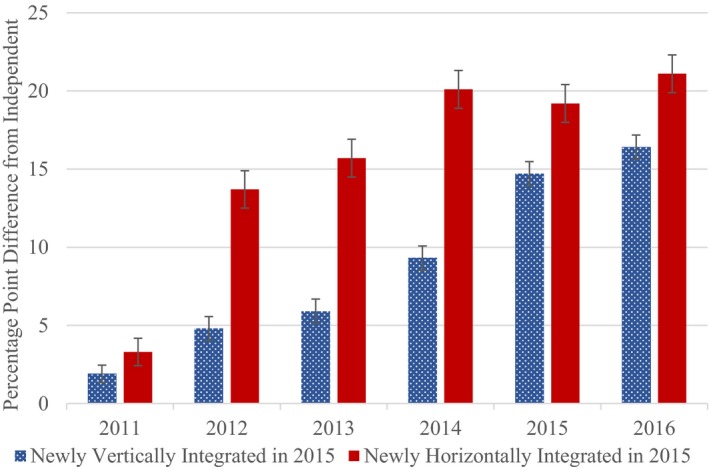
Event study of physician newly integrated between 2013 and 2015, relative to always independent. Bars represent the difference in attestation rate from between physicians that remain independent and those that change status in 2015 in each year derived from linear regressions including practice size, primary vs specialty practice, whether the physician accepts Medicaid, gender, and metropolitan area. The model comparing physicians that join horizontally integrated organizations to physicians who remain independent includes 532 380 observations; the vertically integrated model includes 596 388 observations. Error bars represent 95% confidence intervals using heteroskedastic standard errors [Color figure can be viewed at wileyonlinelibrary.com]
Our results were largely robust to a 1‐year time lag in MU attestation following integration. In the fixed effects models, vertical integration was associated with a 5.3 percentage point increase in attestation (Table S2, column 3) in the following year (instead of 5.8 in our primary model), while horizontal integration was associated with a 1.9 percentage point increase (the same as our primary model). Results of our event study‐style analysis were also similar when we omitted physicians who accepted Medicaid patients, who may have participated in Medicaid MU (Figure S4).
4. DISCUSSION
In our data, physicians’ MU attestation rates were higher among horizontally and vertically integrated practices when compared with independent physician practices, especially in later years of the program when participation criteria were higher and incentives lower. The most striking pattern related to sustained MU attestation over time was thatindependent physicians were much more likely to leave the MU program in later years than were integrated physicians. In comparison, the relationship between changing integration status and MU success was more complex. Our detailed examination revealed evidence of selective targeting of practices already achieving MU by larger (physician acquiring) organizations.
Integration by 2015 appears to have increased attestation rates among integrating providers and/or allowed them to sustain attestation (given the patterns seen in Table 1), but the differences reported in Figure 3 imply some level of strategic selection by larger organizations when deciding which independent practices to acquire. Focusing practice purchases toward physicians achieving MU could have benefited organizations by smoothing the assimilation process and by reducing the need for software purchases or training while allowing them to maximize the accompanying subsidies from the HITECH Act. Vertically integrated systems may have also helped facilitate improved quality and coordination of care offered to patients—consistent with some recent evidence.21, 23
While this finding suggests a positive consequence from vertical integration, it must be interpreted in the context of broader empirical results linked to increasing vertical integration in US health care. Formal tie‐ups between hospitals and physician practices have been shown to strategically alter physicians’ referral patterns and choices over care delivery settings as well as drive higher medical care prices, spending, and treatment intensity—without clear evidence of quality improvements.24, 25, 26 At the same time, prior studies have also shown technology adoption links to vertical integration18, 27 as well as increases in Medicaid acceptance following hospital take‐overs of physician practices3 leaving the net benefits of integration uncertain. Our data cannot inform us if the MU program causally spurred greater vertical integration activity, but they are consistent with the program contributing to the declining appeal of independent practice and therefore adding pressure toward formal integration.
Compared with vertically integrated organizations, horizontally integrated organizations appeared to more selectively target physicians that had attested to MU. The data therefore do not indicate that horizontal integration provided the potential benefit of EHR adoption and MU attestation, and as others have remarked, horizontal integration can threaten the competitive landscape by consolidating physician market power.2, 28, 29, 30 Given the selective integration patterns we observed, future efforts and subsidies aiming to accelerate health IT adoption and advancement may need to be better targeted. If they are not, they may act as a financial boon for larger organizations already well ahead of their smaller, independent competitors.
The high level of independent physicians’ attrition from the MU program in later years is concerning, especially in comparison with the low attrition found in early years of the program in our study and another recent investigation of physician participation in MU.10 Architects of the MU program aimed to create a set of criteria with increasing difficulty over time and “calibrated to reflect both the capacities of providers who face a multitude of real‐world challenges and the maturity of the technology itself.”31 Despite this goal, our finding that about half of independent physicians that attested to Stage 1 MU in 2011‐2013 did not attest in later years suggests that MU criteria and incentives did not align with independent physician's progress toward greater use of EHRs.
Several factors are likely to have contributed to the high level of attrition among independent physicians. First, purchasing and maintenance costs, as well as initial loss of productivity, are commonly cited barriers slowing physician adoption of an EHR.32, 33, 34 Independent physicians are likely to face higher per‐physician administrative and financial burden than large organizations, which can achieve efficiencies of scale by providing shared administrative and IT support to many providers. Further, independent physicians are more likely than large organizations to lack access to the capital needed to invest in and upgrade to advanced EHRs systems. Second, independent physician's attrition may have been exacerbated by the structure of MU payments, which decreased based on the number of years that physicians had attested and the number of years since the program began. As a result, physicians that first attested in 2011 received $18 000 in 2011 but were only eligible for $1960 for attesting in 2015, when their downside exposure was a 2 percent adjustment to their Medicare payments if they chose not to attest. Third, attrition from the MU program may also have been affected by the design of complementary policy initiatives, most notably the regional extension centers (RECs), which were designed to support EHR adoption by independent and rural physicians.35 Federal REC funding occurred between 2010 and 2014, and most RECs were not able to achieve full financial self‐sufficiency in the following years.36 Therefore, many RECs discontinued or slowed their assistance to providers in upgrading their systems to meet MU Stage 2 requirements. Finally, widely reported frustration using EHRs and the MU program specifically may have further reduced independent physicians interest in attesting to Stage 2.37
In combination, independent providers were faced with increasing challenges in the form of MU Stage 2, decreasing support from RECs, decreasing financial motivation, and frustration with EHRs. Given these forces, it is not surprising that many chose not to attest in later years. Nevertheless, recognition of attrition from the program and potential selective purchasing by integrated organizations does call for new initiatives to support beneficial use of EHRs or other health IT by independent physicians that did not fully participate in MU, some of whom may have not had an option to integrate. This is particularly true for practices in rural settings, where both integrated delivery systems and EHRs are less common.38, 39 These areas also lack a health IT workforce and are the areas where RECs focused their efforts.39, 40 Given the rapid pace of change in health IT, independent physicians that left the MU program may require special assistance from entities like RECs to identify and implement new technologies that best fit the needs of their practices.
The history of MU may validate the approach taken in its successor, the Merit‐Based Incentive Payment Systems’ (MIPS) Promoting Interoperability component. Unlike MU's all‐or‐nothing incentive payment system, Promoting Interoperability assigns points based on the proportion of patients for whom specific interoperability‐related functionalities are used. This structure provides incentives for physicians to participate and to continue to improve but does not mandate a pace at which improvement must happen. However, the requirement that physicians use an EHR that meets the 2015 certification criteria in order to participate in Promoting Interoperability in 2019 may weaken the program's ability to create incentives for a broad population of providers in the future because EHR vendors that are most able to support upgrading to 2015 certification, like Epic, work primarily with integrated organizations. In our sample, only 1.4 percent of attesting independent physicians and 5.4 percent of integrated physicians reported using a 2015‐certified EHR in 2016. If this gap persists, it may lead independent physicians to be further excluded from the program over time.
As the future of Promoting Interoperability is debated, further iterations of the program, or its replacement, may be well served by continuing an approach that rewards improvement regardless of the ability to meet thresholds and that specifically supports independent and rural practices. Such an approach could retire measures as most providers reach ceilings of high performance and introduce new, more challenging metrics gradually. This approach is not without its own set of calibration challenges. Close monitoring of program incentives and participant performance will be required to ensure that new measures and incentives do not reward poor performers, that rewards do not solely accrue to the best resourced organizations, and that both high and low performers face sustained incentives to improve.41 In addition, some groups—such as independent, rural practices—may require additional assistance beyond the general incentive program, but targeting such assistance will be challenging.
Our study is admittedly not without limitations. With the data available, we cannot conclude that integration status was the cause of greater success attesting to MU. Instead, we have documented broad trends for a large sample of physicians that indicates that integrated physicians across the United States had different experiences than independent physicians. Similarly, we may not have observed other correlated changes in physician status that occurred during this period, which could be a source of bias. It is possible that MU and integration status influenced the workforce, perhaps by increasing rates of retirement among some physicians. Our findings are derived from those physicians who remained in the workforce throughout the MU period, and inference applies directly to that group. Our analysis is also focused on the experience of physicians with different integration statuses; many other factors other than MU may have led physicians to join an integrated system, and our analysis does not reveal a causal link between MU and integration status. Finally, our analysis focused on the Medicare MU program because data on physician‐level participation in the Medicaid MU program is not publicly available. While it is possible that inclusion of participation in Medicaid MU would alter our results, we believe the overall impact would likely be small because our results are robust to exclusion of physicians that reported accepting Medicaid (ie, to exclusion of those eligible for Medicaid MU), the Medicare program was about five times larger than the Medicaid program, and whether or not the physician accepted Medicaid was not a strong predictor in our regression models.
5. CONCLUSION
Over the course of the Medicare Meaningful Use program, physicians who were members of horizontally or vertically integrated provider organizations were more likely to attest to MU and to stay in the program after attesting once than were independent physicians. Independent physicians that integrated into larger organizations were more likely to have already attested to MU, indicating that technological sophistication may have made them more appealing as integration partners. Together, these dynamics appear to have created a digital divide between physicians that remained independent and integrated physicians. Current policy focused on progress toward advanced EHR functionality (eg, interoperability) may need additional flexibility to ensure that physicians that did not participate in MU are incentivized to use health IT in ways that improve patient care. Complementary efforts may be required to help independent physicians that failed to fully participate in MU make up lost ground in the adoption and implementation of health IT capable of improving care quality.
Supporting information
ACKNOWLEDGMENTS
Joint Acknowledgment/Disclosure Statement: Dr. Everson, Dr. Richards, and Dr. Buntin were supported by Vanderbilt University Medical Center. Dr. Richards also received support from the Hankamer School of Business at Baylor University.
Everson J, Richards MR, Buntin MB. Horizontal and vertical integration's role in meaningful use attestation over time. Health Serv Res. 2019;54:1075–1083. 10.1111/1475-6773.13193
REFERENCES
- 1. Isaacs SL, Jellinek PS, Ray WL. The independent physician‐going, going. N Engl J Med. 2009;360(7):655. [DOI] [PubMed] [Google Scholar]
- 2. Baker LC, Bundorf MK, Kessler DP. Vertical integration: hospital ownership of physician practices is associated with higher prices and spending. Health Aff. 2014;33(5):756‐763. [DOI] [PubMed] [Google Scholar]
- 3. Richards MR, Nikpay SS, Graves JA. The growing integration of physician practices: with a Medicaid side effect. Med Care. 2016;54(7):714‐718. Accessed December 1, 2018. [DOI] [PubMed] [Google Scholar]
- 4. Casalino L, Gillies RR, Shortell SM, et al. External incentives, information technology, and organized processes to improve health care quality for patients with chronic diseases. JAMA. 2003;289(4):434‐441. [DOI] [PubMed] [Google Scholar]
- 5. Casalino LP, Wu FM, Ryan AM, et al. Independent practice associations and physician‐hospital organizations can improve care management for smaller practices. Health Aff. 2013;32(8):1376‐1382. [DOI] [PubMed] [Google Scholar]
- 6. Lee J, Cain C, Young S, Chockley N, Burstin H. The adoption gap: health information technology in small physician practices. Health Aff. 2005;24(5):1364‐1366. [DOI] [PubMed] [Google Scholar]
- 7. Brunt CS, Bowblis JR. Health IT adoption, productivity and quality in primary care. Appl Econ. 2014;46(15):1716‐1727. [Google Scholar]
- 8. Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med. 2010;363(6):501‐504. [DOI] [PubMed] [Google Scholar]
- 9. Buntin MB, Burke MF, Hoaglin MC, Blumenthal D. The benefits of health information technology: a review of the recent literature shows predominantly positive results. Health Aff. 2011;30(3):464‐471. [DOI] [PubMed] [Google Scholar]
- 10. Heisey‐Grove D, King JA. Physician and practice‐level drivers and disparities around meaningful use progress. Health Serv Res. 2017;52(1):244‐267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. DesRoches CM, Audet A‐M, Painter M, Donelan K. Meeting meaningful use criteria and managing patient populations: a national survey of practicing physicians. Ann Intern Med. 2013;158(11):791‐799. [DOI] [PubMed] [Google Scholar]
- 12. Monica K. How meaningful use requirements hurt the small specialty practice. 2017. https://ehrintelligence.com/news/how-meaningful-use-requirements-hurt-the-small-specialty-practice. Accessed December 1, 2018.
- 13. Murphy K. What makes meaningful use challenging for small practices? 2014. https://ehrintelligence.com/news/what-makes-meaningful-use-challenging-for-small-practices. Accessed December 1, 2018.
- 14. American Institutes for Research . Evaluation of the Regional Extension Center Program; 2016.
- 15. Advanced MD . Your EHR & Meaningful Use 2: Was it meant to be? 2014. https://www.advancedmd.com/learn/ehr-meaningful-use-2-meant/. Accessed December 1, 2018.
- 16. Miller AR, Tucker C. Health information exchange, system size and information silos. J Health Econ. 2014;33:28‐42. [DOI] [PubMed] [Google Scholar]
- 17. Holmgren AJ, Ford EW. Assessing the impact of health system organizational structure on hospital electronic data sharing. J Am Med Inform Assoc. 2018;25(9):1147‐1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lammers E. The effect of hospital–physician integration on health information technology adoption. Health Econ. 2013;22(10):1215‐1229. [DOI] [PubMed] [Google Scholar]
- 19. Richards MR, Smith CT, Graves AJ, Buntin MB, Resnick MJ. Physician competition in the era of accountable care organizations. Health Serv Res. 2018;53(2):1272‐1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Barnes H, Richards MR, McHugh MD, Martsolf G. Rural and nonrural primary care physician practices increasingly rely on nurse practitioners. Health Aff. 2018;37(6):908‐914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lammers EJ, McLaughlin CG, Barna M. Physician EHR adoption and potentially preventable Hospital Admissions among Medicare Beneficiaries: panel data evidence, 2010–2013. Health Serv Res. 2016;51(6):2056‐2075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Vest JR. More than just a question of technology: factors related to hospitals’ adoption and implementation of health information exchange. Int J Med Informatics. 2010;79(12):797‐806. [DOI] [PubMed] [Google Scholar]
- 23. Lammers EJ, McLaughlin CG. Meaningful use of electronic health records and Medicare expenditures: evidence from a panel data analysis of US Health Care Markets, 2010–2013. Health Serv Res. 2017;52(4):1364‐1386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Robinson JC, Miller K. Total expenditures per patient in hospital‐owned and physician‐owned physician organizations in California. JAMA. 2014;312(16):1663‐1669. [DOI] [PubMed] [Google Scholar]
- 25. Scott KW, Orav EJ, Cutler DM, Jha AK. Changes in hospital–physician affiliations in US hospitals and their effect on quality of care. Ann Intern Med. 2017;166(1):1‐8. [DOI] [PubMed] [Google Scholar]
- 26. Koch TG, Wendling BW, Wilson NE. How vertical integration affects the quantity and cost of care for Medicare beneficiaries. J Health Econ. 2017;52:19‐32. [DOI] [PubMed] [Google Scholar]
- 27. McCullough JS, Snir EM. Monitoring technology and firm boundaries: physician–hospital integration and technology utilization. J Health Econ. 2010;29(3):457‐467. [DOI] [PubMed] [Google Scholar]
- 28. Dunn A, Shapiro AH. Do physicians possess market power? J Law Econ. 2014;57(1):159‐193. [Google Scholar]
- 29. Berenson RA, Ginsburg PB, Kemper N. Unchecked provider clout in California foreshadows challenges to health reform. Health Aff. 2010;29(4):699‐705. [DOI] [PubMed] [Google Scholar]
- 30. Muhlestein DB, Smith NJ. Physician consolidation: rapid movement from small to large group practices, 2013–15. Health Aff. 2016;35(9):1638‐1642. [DOI] [PubMed] [Google Scholar]
- 31. Blumenthal D, Tavenner M. The, “meaningful use” regulation for electronic health records. N Engl J Med. 2010;2010(363):501‐504. [DOI] [PubMed] [Google Scholar]
- 32. Jamoom EW, Patel V, Furukawa MF, King J. EHR adopters vs. non‐adopters: Impacts of, barriers to, and federal initiatives for EHR adoption. Healthcare. 2014;2(1):33–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Meigs SL, Solomon M. Electronic health record use a bitter pill for many physicians. Perspect Health Inf Manag. 2016;13(Winter):1d. [PMC free article] [PubMed] [Google Scholar]
- 34. Kruse CS, Kristof C, Jones B, Mitchell E, Martinez A. Barriers to electronic health record adoption: a systematic literature review. J Med Syst. 2016;40(12):252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Boas SJ, Bishop TF, Ryan AM, Shih SC, Casalino LP. Electronic health records and technical assistance to improve quality of primary care: lessons for regional extension centers. Paper presented at: Healthcare. 2014;2(2):103–106. [DOI] [PubMed] [Google Scholar]
- 36. Maxson E, Jain S, Kendall M, Mostashari F, Blumenthal D. The regional extension center program: helping physicians meaningfully use health information technology. Ann Intern Med. 2010;153(10):666‐670. [DOI] [PubMed] [Google Scholar]
- 37. Emani S, Ting DY, Healey M, Lipsitz SR, Karson AS, Bates DW. Physician beliefs about the meaningful use of the electronic health record: a follow‐up study. Appl Clin Inform. 2017;8(04):1044‐1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. MacKinney AC, Mueller KJ, McBride TD. The march to accountable care organizations—how will rural fare? J Rural Health. 2011;27(1):131‐137. [DOI] [PubMed] [Google Scholar]
- 39. Casey MM, Moscovice I, McCullough J. Rural primary care practices and meaningful use of electronic health records: the role of regional extension centers. J Rural Health. 2014;30(3):244‐251. [DOI] [PubMed] [Google Scholar]
- 40. Skillman SM, Andrilla CHA, Patterson DG, Fenton SH, Ostergard SJ. Health information technology workforce needs of rural primary care practices. J Rural Health. 2015;31(1):58‐66. [DOI] [PubMed] [Google Scholar]
- 41. Das A, Norton EC, Miller DC, Ryan AM, Birkmeyer JD, Chen LM. Adding a spending metric to Medicare's value‐based purchasing program rewarded low‐quality hospitals. Health Aff. 2016;35(5):898‐906. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


