Abstract
To evaluate the type, location, severity of headache and their relation to various nasal and sinus related pathological conditions. All the patients presenting with acute and chronic sinus and nasal infections along with headache were included in the study. The diagnostic confirmation was done with clinical along with radiological and endoscopic evaluation. Various parameters categorized accordingly. Chronic rhinosinusitis/chronic recurrent rhinosinusitis are the most common nasal condition seen in oto-rhino-laryngology OPD which has enormous economic burden and significant morbidity on general population. The headache is the commonest associated symptom which is needed to be given attention. The location, variation, pattern of the headache can guide us towards the correct diagnosis.
Keywords: Headache, Sinusitis, Sinugenic, Non-sinugenic, Migraine
Introduction
“Sinus Headache” is a very common yet merely misdiagnosed and ill-treated condition observed in association with various sinogenic and nonsinogenic conditions in daily clinical practice. The type, pattern, and severity varies patient to patient worldwide. Sinus headache term is widely assigned to the individuals with facial pain. The inappropriate diagnosis of sinus headache can lead to unnecessary diagnostic studies, surgical interventions and medical treatment [1, 2]. Diagnosing sinus headache related to chronic rhiosinusitis disease can be much more difficult depending on patient’s presentation [3]. Since chronic rhinosinusitis and allergic rhinitis both the conditions are very common in daily ENT practice, so their relation and association to headache is really important to be ruled out. There may be many other important factors like mucosal contact points, agar nesi, hellar cells, concha bullosa, enlarged bulla ethmoidelis, aplastic frontal sinuses, narrow fronto-ehmoidal recess can cause and contribute the headache.
Many patients present to otolaryngology and headache clinics with self diagnosed “sinus headache” that ultimately found to be chronic migraine [4, 5], these patients reported to receive insufficient treatment and medications for years in the form of antihistaminics and intranasal corticosteroids [6]. Although a vast majority of the patients diagnosed as having sinus headache represents diagnostic errors.
Headache and facial pain of sinugenic origin are real and often seen in clinical practice [7]. In some conditions the etiology of headache resides in maxillary sinus which is secondary to chronic sinus infection [1, 2] and surgical intervention required to treat these cases [2]. The patients with blocked osteomeatal complex, one or more contact points, spheno-ethmoid complex diseases, nasal polype, and anatomical variations can also cause headache and needs surgical interventions along with medical treatment.
The headache like migraine, cluster headache, tension headache and headache due to refractive errors are very commonly misdiagnosed as “sinus headache”, investigated and treated for the same which increases the economic burden on the patient.
If a specific pattern, course, and type could be identified earlier it would have been very helpful in the diagnosis and treatment of such patients. some specific type of patterns had been identified in chronic rhinosinusitis cases depending on isolated or multiple sinus involvement, like in frontal sinusitis frontal headache/brow pain can be seen with a specific time bound ascending pattern (office headache), in ethmoid sinus involvement there may be retro-orbital pain or headache, sphenoid sinusitis can present as peri-orbital/retro-orbital pain or headache and maxillary sinusitis presents as facial tenderness and fullness. When multiple sinuses are involved (pansinusitis) headache may be band like or pressure headache.
Materials and Methods
The present study “sinus headache” diagnosis and dilemma, was conducted in a tertiary care medical college hospital in central India. All 128 patients included in the study were the patients presenting in routine ENT OPD. The patients having acute rhinosinusitis, chronic rhinosinusitis, allergic rhinitis, and other sinunasal conditions associated with headache were included. A detailed history and examination was done. All patients were specially enquired about headache, its onset, site, duration, type, frequency, progression, aggravating and reliving factors, and diurnal variations. Than a detailed nasal examination with anterior rhinoscopy, and endoscopic examination done to find out any nasal anatomical variation, deformity and mucosal contact points. Routine blood examination, X-ray PNS and CT scan PNS coronal/axial view were done as per requirements. The patients with anatomical variations, contact points, and obstructive chronic rhinosinusitis were subjected to surgical intervention.
Observation
A total of 128 patients of sinus diseases with headache were included in the study, which consisted of 67 female (52.34%) and 61 male (47.65%). Among the studied population 89 (69.53%) were diagnosed with sinugenic headache and 39 (30.46%) with nonsinugenic headache and sinugenic headache was more common in males (57%) as compared to non-sinugenic headache which was more common in females (74%), this was statistically significant p < 0.05 (Chi sq = 10.898, p value 0.000963) (Fig. 1).
Fig. 1.
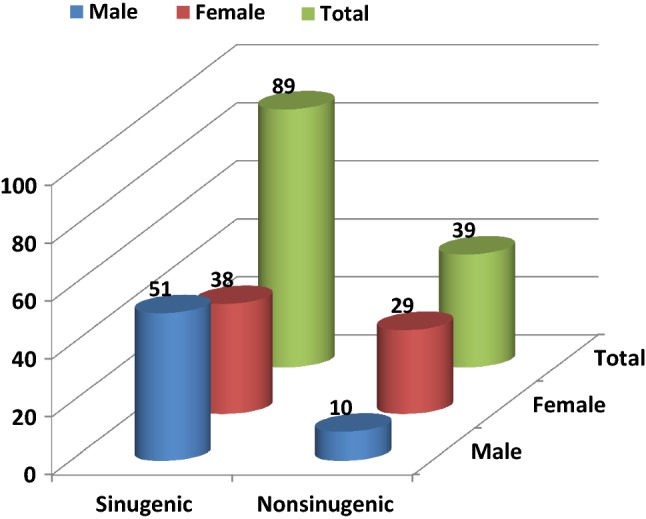
Total and sex-wise distribution of sinugenic and non-sinugenic headache
The mean age was 45 years with participants ranging from 11 to 67 years. Most of the patients in both the groups were found to be in range of 26–40 years and the most common diagnosis was acute and chronic rhinosinusitis (although not statistically significant chi sq = 5.901, p value 0.11652) (Tables 1, 2).
Table 1.
Age distribution among sinugenic and nonsinugenic headache groups
| Age group (years) | Sinugenic | Nonsinugenic |
|---|---|---|
| 10–25 | 20 | 12 |
| 26–40 | 38 | 21 |
| 41–55 | 18 | 05 |
| 55–70 | 13 | 01 |
Table 2.
Age distribution for rhinogenic/sinugenic causes (89 patients)
| Causes | 10–25 years | 26–40 years | 41–55 years | 56–70 years | Total |
|---|---|---|---|---|---|
| Acute sinusitis | 07 | 11 | 2 | 0 | 20 |
| Chronic sinusitis | 13 | 17 | 1 | 1 | 32 |
| Nasal polyp | 03 | 02 | 1 | 0 | 06 |
| OMC disease | 01 | 06 | 3 | 0 | 10 |
| Atrophic rhinitis | 00 | 01 | 1 | 1 | 03 |
| Allergic rhinitis | 07 | 09 | 2 | 0 | 18 |
| Total | 31 | 46 | 10 | 2 | 89 |
Most common symptom was found to be nasal obstruction in 110 patients, and most common sign was inferior turbinate hypertrophy (107 patients) followed by Deviated nasal septum (88 patients), and Osteomeatal complex block (46 patients) in sinugenic headache group (Table 3).
Table 3.
Nasal sign and symptoms (other than headache)
| Nasal symptoms | Patients | Nasal signs | Patients |
|---|---|---|---|
| Nasal obstruction | 110 | Inferior turbinate hypertrophy | 107 |
| Nasal discharge | 72 | Deviated nasal septum | 88 |
| Facial pain and brow pain | 68 | Osteomeatal complex block | 46 |
| Anosmia | 31 | Bluish turbinate and nasal mucasa | 28 |
| Epistaxis | 06 | Polypes | 08 |
| Roomy nasal cavity/crusts | 03 |
In sinugenic headache group out of 89 patients 58 patients were operated for significant DNS, anatomical variations, OMC blockage, and mucosal contact points (41 septoplasty and 17 FESS). In sinugenic headache group, sinugenic headache were etiologically related to chronic rhinosinusits most commonly (29 patients) followed by acute rhinosinusitis (21 patients) and allergic rhinitis (20 patients) (Fig. 2).
Fig. 2.
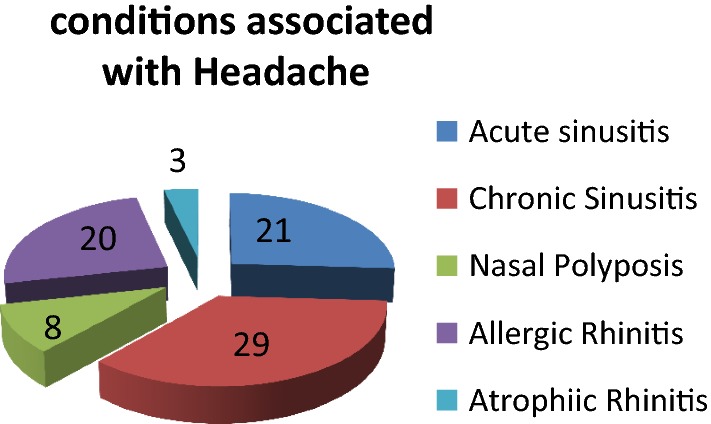
Etiological relation of headache with associated conditions
In almost all the patients a specific pattern was seen on the basis of locations of the headache (Table 4). The most common pattern seen was increasing headache in forehead region and eyebrows (frontal headache—41 patients) with the tendency to decrease or getting diffused with day progresses. Second most common pattern seen was periorbitali and retro-orbital headache (21 patients) with ethmoid and sphenoid sinus involvement, followed by headache with facial pain (heaviness/pressure) seen in 13 patients of maxillary sinusitis. In nonsinugenic group migraine found to be the most common headache type in female of 26–40 years.
Table 4.
Types and localization of sinugenic headache
| Location of pain | No. of cases | Type identified |
|---|---|---|
| Brow pain/above eyes | 42 | Frontal sinusitis |
| Retro-orbital pain | 21 | Spheno-ethmoid sinusitis |
| Peri-orbital | 08 | Ehthmoid sinusitis |
| Facial pain/heaviness | 13 | Maxillary sinusitis |
| Band type headache | 03 | Pan sinusitis |
Many times a combination of more than one type or involved sites were also seen, mostly in the cases of pansinusitis.
Discussion
In our study we observed many types of headache presentations; most common type headache encountered was Frontal headache, presented as brow pain in 47% patients which were consistent with the study done by Pramod Kumar et al. [8].
In this study the majority of sinugenic headache cases were females (67%), in the age group of 26–40 years and in non sinugenic cases of headache were also females which were contrary to the study by Pramod Kumar et al. [8], Wenig et al. and Lebovics et al.
In our study majority of patients with chronic rhinosinusitis had headache (29) followed by acute rhinosinusitis (21), allergic rhinitis (20). Some patients of nasal polyp and atrophic rhinitis also reported with headache. Study by Junior De Fitas for relation of headache and polyps [9] and Wolf for headache patients in allergic rhinitis justifies the headache in above conditions.
For convenience we have divided the patients into sub groups, among them 89 patients had rhinogenic headache and 39 had nonrhinogenic headache. In rhinogenic group moist common patrtern was found to be frontal headache with a male preponderance due to their daily outdoor activity and exposure to external environment, it was consistant with the study done by Wening et al. [10].
Aaseth et al. [11] also found that the patients with chronic rhinosinusitis had ninefold increased risk of chronic headache.
In our study allergic rhinitis had a major contributory factor as a cause of headache. It was associated with headache in 20 patients in sinugenic group which is slightly difficult to explain as in allergic rhinitis patients migraine headache is more common as seen in study done by Ku et al. [12].
In our study 58 patients were operated for DNS, OMC (Osteo Meatal Complex) block, and mucosal contact points. Out of 58 patients 48 were relived and 16 patients were come back with recurrence of symptoms. These results were similar to a study done by Parsona et al. [13].
It has been seen in many studies that contact points in nasal cavity also causes headache.
Conclusion
Headache related to the sinunasal inflammation and infections are very common but generally mistaken and misdiagnosed which needs to be addressed correctly in early stage of sinus infection. Identifying the specific pattern and type of headache can help to form correct diagnosis and initiate the treatment. With our study we have tried to identify various types, patterns, headache sites, and common misdiagnosed headache of sinugenic/nonsinugenic origin for the ease of diagnosis. We strongly recommend a very careful ENT examination (physical and radiological) to rule out migraine and diagnose sinus headache as soon as possible for the effective treatment.
Compliance with Ethical Standards
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Ethical Approval
This article does not contain any studies with animals performed by any of the authors.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cady RK, Dodick DW, Lewine HL, et al. Sinus headache: a neurology, otolaryngology, allergy and primary care consensus on diagnosis and treatment. Mayo Clin Proc. 2005;80:908–916. doi: 10.4065/80.7.908. [DOI] [PubMed] [Google Scholar]
- 2.Chow AW, Benninger MS, Brool I, et al. IDSA clinical practice guidelines for acute bacterial rhinosinusitis in children and adults. Clin Infact Dis. 2012;5:72–112. doi: 10.1093/cid/cis370. [DOI] [PubMed] [Google Scholar]
- 3.Seiden AM, Vincent TM. Headache and the frontal sinus. Otolaryngol Clin North Am. 2001;34(1):227–241. doi: 10.1016/S0030-6665(05)70308-X. [DOI] [PubMed] [Google Scholar]
- 4.Levine H, Setgen M, Holy C. Why the confusion about sinus headache? Otolaryngol Cin North Am. 2014;47:169–174. doi: 10.1016/j.otc.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 5.(2015) Sinus headaches. American Academy of Otolaryngology-Head and Neck Surgery. http://www.entnet.org/contant/sinus-headaches. Accessed 23 July 2015
- 6.Keri E, DelGaudio JM. Treatment of sinus headache as migraine: the diagnostic utility of triptans. Laryngoscope. 2008;118:2235–2239. doi: 10.1097/MLG.0b013e318182f81d. [DOI] [PubMed] [Google Scholar]
- 7.Eross EJ, Dodick DW, Eross MD. The sinus, allergy and migraine study (SAMS) Headache. 2014;44:462. doi: 10.1111/j.1526-4610.2006.00688.x. [DOI] [PubMed] [Google Scholar]
- 8.Pramod Kumar et al. (2000) Indian journal of otolaryngolofy. April–June 52(2)
- 9.De Frietas J (2006) Revista Brasilerve de otolaryngologia. Nov–Dec 72(6)
- 10.Wening BH, et al. Frontal sinusitis and its intracranial complications. Int J Pediatr Otorhinolaryngol. 1983;5:285. doi: 10.1016/S0165-5876(83)80042-1. [DOI] [PubMed] [Google Scholar]
- 11.Aaseth K, Grande RB, Kvaerner K, et al. Chronic rhinosinusitis gives a ninefold increased risk of chronic headache. The Akershus study of chronic headache. Cephalalgia. 2010;30:152–160. doi: 10.1111/j.1468-2982.2009.01877.x. [DOI] [PubMed] [Google Scholar]
- 12.Ku M, Silverman B, Prifti N, Ying W, Persaud Y, Schneider A. Prevalance of migraine headache in patients with allergic rhinitis. Ann Allergy Asthma Immunol. 2006;97(2):226–230. doi: 10.1016/S1081-1206(10)60018-X. [DOI] [PubMed] [Google Scholar]
- 13.Parsona DS, Batra PS. FESS outcome for contact point headache. Laryngoscope. 1998;108(5):696–702. doi: 10.1097/00005537-199805000-00013. [DOI] [PubMed] [Google Scholar]


