Abstract
The incorporation of telemedicine and artificial intelligence for early screening and assessment of severity of life-style disorders has a great potential for better assessment in a busy outpatient clinic and thereby curtail down the related morbidities. A computer based algorithm based upon standardized questionnaire (from established assessment tools) is designed to assess the risk of obstructive sleep apnoea syndrome (OSAS). In addition the incorporation of basic screening questions of anamnesis help in suggesting a probable diagnosis of sleep related disorder as well. The overall data at our center has been analyzed to establish the existing pattern of sleep related disorders. Of 850 healthy subjects screened, prevalence of snoring was 20.47% while OSAS was seen in 4.20% (N = 25) in males and 2.64% (N = 8) in females. The parasomnia was most prevalent (14.71%), followed by insomnia (10.24%), periodic leg movement (6.59%), bruxism (1.65%) and narcolepsy (0.59%). Hypertension, laryngopharyngeal reflux and obesity were the common co-morbidities in OSAS while family history of hypertension and diabetes were common in snorers. A significant association with OSA was seen with diabetes mellitus, neck circumference and nasal obstruction, while, obesity and apnoeic episodes were more significantly associated with OSA than snorers. Increased waist to hip ratio was appreciated in both the OSAS and snorers. The algorithm based online assessment is likely to diagnose the occult clinical cases as well as assess the risk of OSAS. In routine outpatient clinic, a clinician may better assess the patient morbidity with a comprehensive availability of symptoms and moreover enhance the post-treatment compliance. In addition a smartphone based computerized assessment for general population may be designed for other lifestyle disorders as well.
Keywords: Computer algorithm, Artificial intelligence, Obstructive sleep apnoea syndrome, Periodic leg movement, Narcolepsy, Parasomnia, Insomnia
Introduction
The pattern of sleep related disorders in modern era is rapidly evolving due to rapid industrialization, deteriorating life-styles, increasing obesity and immense stress predisposing the mankind to various metabolic, physical and mental consequences. The so-called life-style disorders are often diagnosed late as the busy life-schedule restricts timely medical-consultation. To overcome the time constraints under such circumstances, an online assessment is a ready solution for early screening of a particular problem. Since an early consultation for anticipated morbidity of life-style disorders is often omitted, the incorporation of telemedicine and artificial intelligence for early screening and assessment of severity is a ready solution. This has a great potential to curtail down the related morbidity. Accordingly a user-friendly, easily accessible, minimally expensive and significantly reliable real-time computer-based online assessment for sleep-related disorder needs to be introduced to facilitate general population for directly scoring their complaints. The patient participation this way seems important as a complete sleep assessment in a busy outpatient clinic for every patient by the physician himself is impractical. This is particularly true for India where unlike west the average daily outpatient attendance per specialist varies from 65 to 150. Moreover the patient compliance issues following an intervention can easily be followed through online patient assessment thereby reducing dropouts/non-compliance due to geographical limitations. The patient participation therefore facilitates a better assessment with a better data collection.
The first part of this paper introduces a computer based algorithm that is designed to assess the risk of obstructive sleep apnoea (OSA) and to shortlist a probable diagnosis based upon patient’s responses. Following patient’s responses to the standardized questionnaire online, the basic analysis as per the algorithm further guides the patient to another set of questions. In the process a combination of responses suggests the probable diagnosis and risk of OSA. In addition the relevant sleep log can be better communicated online through another set of algorithm. The second part of the paper analyses the overall data (possible online) to establish the existing pattern of sleep related disorders.
Materials and Methods
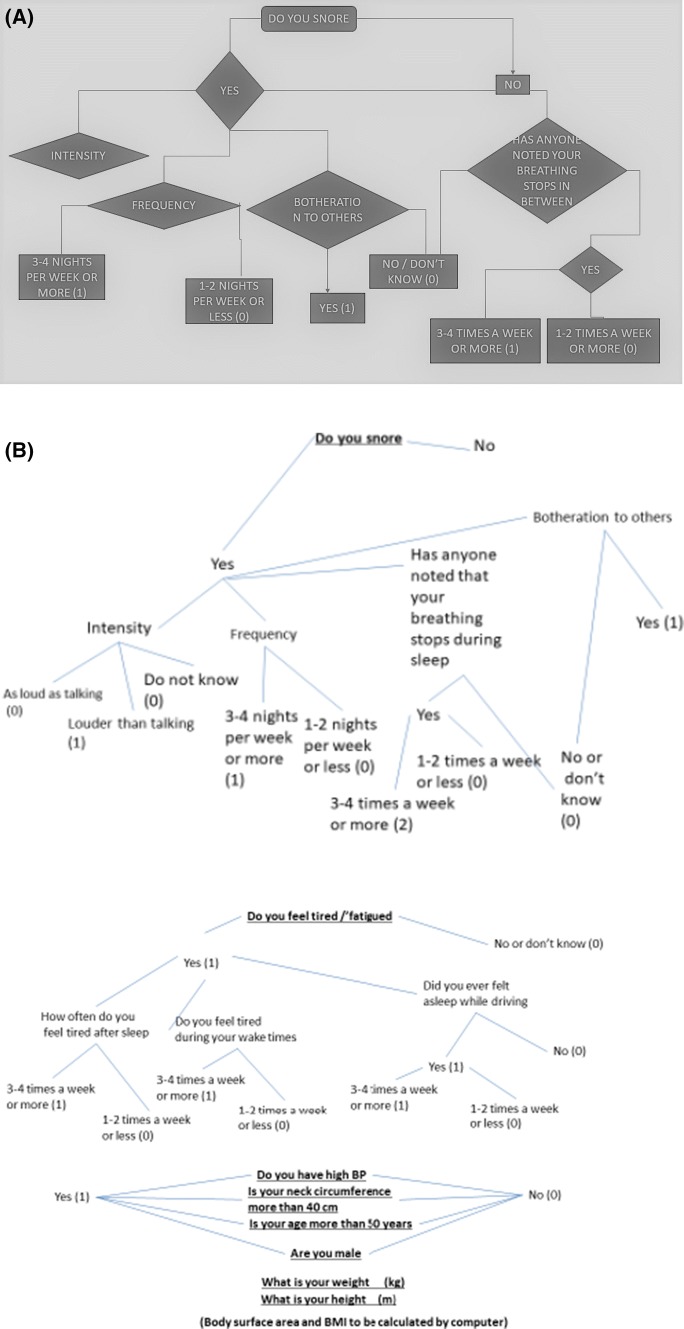
Development of Computer-Based Algorithms
The first step is defining the computer-based algorithm for collecting pre-decided data set online directly as patient-responses. Alternatively the uneducated patients were occasionally assisted by paramedics particularly those with rural background or with no knowledge about computer or some elderly who felt quite uncomfortable with computer usage. A similar information as in online version was obtained through personal interactions to reduce the chances of any potential bias in the computer based data collection. The relevant questions were extracted from institutional protocol as well as from the existing questionnaire-based-assessment tools such as Epworth sleepiness scale [1], Stop-bang scoring [2] and Berlin scale [3] in a systematic manner for developing the computer-based algorithm. A combination of the three scoring systems was integrated to avoid limitations of individual systems in specific situations. Figure 1 shows the flowchart of symptoms (questions) used in framing the first algorithm while the details of sleep log (Table 1) were considered to construct the second algorithm. The first algorithm helped in scoring the risk of OSA and short listing probable diagnosis of sleep related disorder while second algorithm reflected sleep-log per se.
Fig. 1.
a Sample of computer algorithm based on the intergrated questionnaire protocol (Epworth, Stop-Bang, Berlin scoring systems). b Flowchart of intergrated questionnaire
Table 1.
Questionnaire to be recorded daily in morning as per algorithm 2
| 1. | What was the time when you went to bed last night |
| 2. | After how long did you fall asleep (minutes) |
| 3. | How many times did you wake up during the night (numbers) and how long were you awake (minutes) |
| 4. | What was the time when you woke up this morning |
| 5. | How was your feeling in this morning (good, satisfactory, unsatisfactory, bad, worst) |
| 6. | How many naps did you take in the day time (state numbers) |
| 7. | Did you take tea during last 12 h (mention amount if possible) |
| 8. | Did you take coffee/cola drink during last 12 h (mention amount if possible) |
| 9. | Did you take alcohol during last 12 h (mention amount in ml if possible) |
| 10. | Did you smoke bidi/cigarette during one hour of going to bed |
| 11. | Were you under any sort of stress while going to bed |
| 12. | Enumerate your medications that you took in last 24 h with their timing |
Analysis of Data to Define the Existing Pattern of Sleep Related Disorders
A total of 850 apparently healthy subjects were screened for sleep related disorders as per the questionnaire relating to algorithms (Fig. 1, Table 1). This was a prospective study carried out at a tertiary care center of north India. Almost all the data was collected through one to one patient interaction. The age of inclusion ranged from 15 to 65 years, while those with mental retardation, pregnant and non-cooperative statuses were excluded. Apart from routine anamnesis, the data was collected with the aim to suggest a probable diagnosis such as obstructive sleep apnoea syndrome (OSAS), periodic leg movement (PLM), narcolepsy, cataplexy, parasomnia, insomnia, bruxism and altered sleep hygiene as well as nocturnal awakenings. In addition, the risk of OSA/daytime sleepiness was also ranked as per Epworth [1], Stop-bang [2], Berlin [3] scores and medical co-morbidities too were recorded. The initial version of the software included assessment of sleepiness score as per Epworth Index but in the revised version Stop-bang [2], Berlin [3] criteria were also included. Furthermore the use of excessive daily caffeine, alcohol and smoking was also noted. To reduce any potential bias similar information was obtained through personal interactions particularly from uneducated patients and a subset of elderly showing a reluctant attitude towards computer usage. An attempt was made to estimate the prevalence of various sleep related disorders in the adult population as well as to study their current pattern including comparison of the impact of associated variables between OSAS patients with simple snorers. The SPSS software was used for analysis where the Pearson Chi square test with/without Yates continuity correction (as per the case) was considered for analysis and comparison. The X-square and degree of freedom were defined accordingly while significance was considered with p value < 0.05.
Observations
Pattern of Sleep Related Disorders
The prevalence of snoring in adult population is depicted in Table 2. The overall prevalence of snoring was 20.47% while interestingly females between 55 and 65 years age group showed a lower prevalence than their counterpart males.
Table 2.
Distribution of snorers as per age and gender
| Sex and age group | Snorers | Non-snorers | Total | ||
|---|---|---|---|---|---|
| No. | % | No. | % | No. | |
| Male | |||||
| 24–34 | 23 | 17.96 | 105 | 82.03 | 128 |
| 35–44 | 39 | 25.32 | 115 | 74.67 | 154 |
| 45–54 | 37 | 26.24 | 104 | 73.75 | 141 |
| 55–65 | 28 | 22.58 | 96 | 77.41 | 124 |
| Total | 127 | 23.21 | 420 | 76.78 | 547 |
| Female | |||||
| 24–34 | 9 | 9.09 | 90 | 90.90 | 99 |
| 35–44 | 17 | 25.75 | 49 | 74.24 | 66 |
| 45–54 | 13 | 24.07 | 41 | 75.92 | 54 |
| 55–65 | 8 | 9.52 | 76 | 90.47 | 84 |
| Total | 47 | 15.51 | 256 | 84.48 | 303 |
| Grand total | 174 | 20.47 | 676 | 79.52 | 850 |
The prevalence of OSAS was seen in 4.20% (N = 25) in males and 2.64% (N = 8) in females. However the prevalence of other sleep related disorders as per age and sex is depicted in Table 3. The maximum prevalence was seen for parasomnia (14.71%), followed by insomnia (10.24%), PLM (6.59%), bruxism (1.65%) and narcolepsy (0.59%).
Table 3.
Prevalence of sleep related disorder in adult population
| Age group | Total | Narcolepsy | PLM | Parasomnia | Insomnia | Bruxism | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | F | M | F | M | F | M | F | M | F | M | F | |||||||||||
| N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | |||
| 24–34 | 128 | 99 | 1 | 0.78 | 0 | 0 | 6 | 4.68 | 3 | 3.03 | 20 | 15.6 | 6 | 6.06 | 14 | 10.93 | 3 | 3.03 | 1 | 0.78 | 2 | 2.08 |
| 35–44 | 154 | 66 | 1 | 0.64 | 0 | 0 | 13 | 8.44 | 7 | 10.6 | 29 | 18.83 | 9 | 13.63 | 19 | 12.33 | 8 | 12.12 | 2 | 1.29 | 2 | 3.03 |
| 45–54 | 141 | 54 | 1 | 0.7 | 1 | 1.8 | 15 | 10.63 | 1 | 1.85 | 31 | 21.98 | 8 | 14.81 | 20 | 14.18 | 8 | 14.18 | 6 | 4.25 | 0 | 0 |
| 55–65 | 124 | 84 | 1 | 0.7 | 0 | 0 | 10 | 8.06 | 1 | 1.19 | 19 | 15.32 | 3 | 3.57 | 13 | 10.48 | 2 | 2.38 | 1 | 0.8 | 0 | 0 |
| Total | 547 | 303 | 4 | 0.73 | 1 | 0.3 | 44 | 8 | 12 | 3.9 | 99 | 18.1 | 26 | 8.6 | 66 | 12.1 | 21 | 6.9 | 10 | 1.8 | 4 | 1.3 |
| Grand total | 850 | 5 (0.5%) | 56 (6.6%) | 125 (14.70%) | 87 (10.20%) | 14 (1.60%) | ||||||||||||||||
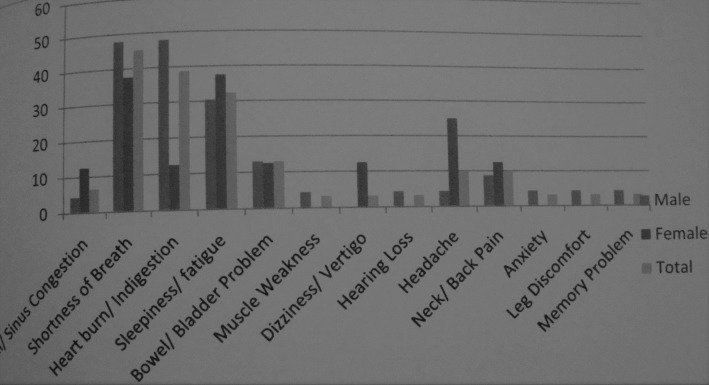
The age and gender distribution of OSAS amongst snorers (N-174) is depicted in Table 4, while the symptoms of OSA is shown in Fig. 2. The prevalence of OSA amongst female snorers between 24 and 34 years age group was maximum (33%) as opposed to males in the same age group that revealed lowest prevalence (13%). The common symptoms included shortness of breath, heartburn and sleepiness/fatigue while muscle weakness, deafness, anxiety and leg discomfort was only noted in males.
Table 4.
Obstructive sleep apnoea syndrome: age and gender distribution
| Age | Sex | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Male | Female | ||||||||
| Total | OSA | Prevalence | Total | OSA | Prevalence | Total | OSA | prevalence | |
| 25–34 | 23 | 3 | 13.04 | 9 | 3 | 33.33 | 32 | 6 | 18.75 |
| 35–44 | 39 | 9 | 23.08 | 17 | 2 | 11.76 | 56 | 1 | 19.64 |
| 45–54 | 37 | 5 | 13.51 | 13 | 2 | 15.38 | 50 | 7 | 14 |
| 55–65 | 28 | 6 | 21.43 | 8 | 1 | 12.5 | 36 | 7 | 19.44 |
| Total | 127 | 23 | 18.11 | 47 | 8 | 17.02 | 174 | 31 | 17.82 |
Fig. 2.
Symptoms in OSAS
Table 5 depicts the co morbidities in adult OSAS and snorers. Hypertension was found to be the most common in OSAS followed closely by laryngopharyngeal reflux disease (LPR) and obesity.
Table 5.
Co-morbidities in adult OSAS and snorers
| CO-Morbidities | Age groups (years) | |||
|---|---|---|---|---|
| 24–34 | 35–44 | 45–54 | 55–65 | |
| OSAS (total N) | 6 | 11 | 7 | 7 |
| Snorers (total N) | 32 | 56 | 50 | 36 |
| Hypertension | ||||
| OSAS | ||||
| Male %(N) | 16.7 (1) | 18.2 (2) | 42.9 (3) | 42.9 (3) |
| Female %(N) | 16.7 (1) | 9.1 (1) | 14.3 (1) | 0 |
| Snorers | ||||
| Male %(N) | ||||
| Female %(N) | ||||
| Obesity | ||||
| OSAS | ||||
| Male %(N) | 50 (3) | 81.8 (9) | 71.5 (5) | 85.7 (6) |
| Female %(N) | 50 (3) | 18.2 (2) | 28.6 (2) | 14.3 (1) |
| Snorers | ||||
| Male %(N) | 3 | 9 | 5 | 6 |
| Female %(N) | 3 | 2 | 2 | 1 |
| Diabetes mellitus | ||||
| OSAS | ||||
| Male %(N) | 16.7 (1) | 63.6 (7) | 14.3 (1) | 57.1 (4) |
| Female %(N) | 33.3 (2) | 9.1 (1) | 28.6 (2) | 0 |
| Snorers | ||||
| Male %(N) | 1 | 6 | 5 | 7 |
| Female %(N) | 0 | 0 | 1 | 3 |
| Laryngopharyngeal reflux | ||||
| OSAS | ||||
| Male %(N) | 33.3 (2) | 36.4 (4) | 42.9 (3) | 57.1 (4) |
| Female %(N) | 33.3 (2) | 9.1 (1) | 14.3 (1) | 14.3 (1) |
| Snorers | ||||
| Male %(N) | 6 | 9 | 12 | 14 |
| Female %(N) | 4 | 6 | 3 | 4 |
| ESS | ||||
| OSAS | ||||
| Male %(N) | 0 | 18.2 (2) | 14.3 (1) | 0 |
| Female %(N) | 0 | 0 | 0 | 0 |
| Snorers | ||||
| Male %(N) | 8 | 9 | 5 | 5 |
| Female %(N) | 1 | 0 | 0 | 3 |
An analysis of family history in patients with snoring (Table 6) reveals hypertension and diabetes as being overall most common while asthma was more common amongst females and laryngopharyngeal reflux (LPR) amongst males.
Table 6.
Family history in adult snorers
| Male-127 | Female-47 | Total-174 | |
|---|---|---|---|
| Hypertension | 78 (61.4) | 21 (44.6) | 99 (56.9) |
| Diabetes | 66 (51.9) | 19 (40.4) | 85 (48.9) |
| Angina | 20 (15.7) | 6 (12.7) | 26 (14.9) |
| Stroke | 1 (0.7) | 0 (0) | 1 (0.5) |
| Asthma | 30 (17.2) | 10 (21.2) | 40 (23.0) |
| Reflux | 23 (13.2) | 5 (10.6) | 28 (16.0) |
| Thyroid ds | 16 (12.6) | 4 (8.5) | 20 (11.5) |
| Deviated nasal septum | 2 (1.5) | 3 (6.4) | 5 (2.8) |
| High cholesterol | 5 (3.9) | 0 (0) | 5 (2.8) |
| Sinus Ds | 3 (2.30) | 2 (4.2) | 5 (2.9) |
| Arthritis | 4 (3.1) | 0 (0) | 4 (2.3) |
The variables that revealed significant association with OSA included LPR (Pearson Chi square test with Yates continuity correction, X-square = 5.8791, df = 1, p = 0.0153), diabetes mellitus (Pearson Chi square test with Yates continuity correction, X-square = 30.3305, df = 1, p = 0), obesity (Pearson Chi square test with Yates continuity correction, X-square = 80.388, df = 1, p = 0), neck circumference (Pearson Chi square test without Yates continuity correction, X-square = 9.8989, df = 3, p = 0.0194) and nasal obstruction (Fisher exact test p < 0.001). Furthermore, obesity was more significantly associated with OSA than snorers and similar was the case for apnoeic episodes as expected (Pearson Chi square test without Yates continuity correction, X-square = 9.0339, df = 3, p = 0.0288). The increased waist to hip ratio was appreciated in both the OSAS and snorers. In most OSAS male patients (69.6%) there was a high ratio that was universally (100%) encountered in the age group of 24–34 years. All the female OSAS patients showed an extreme such ratio.
However no statistical significance was appreciated amongst OSA vs snorers for alcohol use (Pearson Chi square test without Yates continuity correction, X-square = 2.3333, df = 4, p = 0.6747), caffeine intake (Pearson Chi square test without Yates continuity correction, X-square = 4.0895, df = 5, p = 0.5366), and smoking (Pearson Chi square test without Yates continuity correction, X-square = 2.9193, df = 4, p = 0.5704). Similarly no difference was seen for the excessive day time sleepiness (Pearson Chi square test with Yates continuity correction, X-square = 0.7402, df = 1, p = 0.3896) and snoring intensity (Pearson Chi square test without Yates continuity correction, X-square = 1.7861, df = 3, p = 0.618) amongst OSA vs snorers.
Assessment of risk of excessive daytime sleepiness through computer-based algorithm as per Epworth sleepiness scale revealed a high risk in about 75% snorers. Assessment of risk of OSAS as per Berlin scale revealed a high risk in 87.5% snorers. In addition the Stop-bang scale revealed 6.25% cases with low risk of OSA while the rest with intermediate to high risk of OSA.
Discussion
The first algorithm is extremely important for suggesting the risk (severity) of OSA (dysfunction) and suggesting/short listing a diagnosis of a probable sleep related disorder. The final result of this composite subjective assessment through integrated scoring algorithm is Epworth, stop-bang and berlin scores separately. This facilitates a composite decision and prevents bias based on individual scores separately. The second algorithm defining the sleep-log seems extremely useful as a follow up measure of sleep performance following any intervention, thus solving issues of non-compliance due to geographical logistics. The designing author (AK) plans to release these software algorithms on the internet (and subsequently through smartphone based mobile apps) to be used absolutely free in the due course.
India being the hub of diabetes across the world and with its population genetically predisposed for the same, an increasing trend of obesity/sleep disorders can be expected. This seems particularly true as the current data reveals a significant association with diabetes mellitus as well as with the family history of diabetes. Since obesity is a well-known risk factor related to diabetes, the ongoing lifestyle stress further complicates hyperlipidemia and poor diabetic control in young/middle aged population. The assessment of basic epidemiology of sleep related disorders was possible using the questions used in algorithms. In general since Indians do not exercise regularly their tendency of central obesity further increases their waist to hip ratio and neck circumference. The later predisposes to oropharyngeal obstruction and if to a morbid extent can result in OSAS. Furthermore the nasal obstruction was seen to be associated with such patients and while this might not be the primary factor for obstruction per se but certainly can contribute to aggravate the situation. The increased obesity/accumulation of fat in snorers resulted in a high waist-hip ratio and a further progression possibly caused enhanced neck circumference, often associated with presentation of choking/apnoic episodes. Hence an enhanced waist-hip ratio may be regarded as an early precursor/predictor of OSAS amongst those who continue to have a weight gain. Similarly the apnoic episodes as expected would have been significant in the OSAS patients than in simple snorers signifying fat accumulation across the upper airway. The caffeine did not have any effect on severity of snoring or onset of OSAS despite the fact that coffee is known to disturb sleep. The similar result was appreciated with alcohol that is well known for its depressant action/loss of muscular tone. However such insignificant relationships further needs to be validated specially with a larger sample size. Moreover smoking also did not shown any difference in association with OSAS vs snorers. Such conclusion cannot be drawn from this study unless the details of smoking (frequency, pack-years, type of smoking) be analyzed. Surprisingly however an insignificant difference was appreciated in the sleepiness score as well as snoring-intensity (that is definitely expected to be more with OSAS) between OSAS and snorers. This further suggests that a larger sample needs to be studied for concluding the same and by including this software in the process of patient management, such study would be much more feasible.
Absolute (100%) compliance can be expected through the use of the second algorithm based online software. Since OSAS is a disease of the ‘rich’, this population has a definite access and knowhow of computers. A timely, self-reported data free of any observer-bias is likely to provide a timely assessment of the disease course as well as help in accumulating a quality data through patient participation. Till date a lot of applications and reports [4–6] regarding incorporation of computer algorithms and artificial intelligence have appeared with an aim of better assessment and management of sleep related disorders. However none has focused on the subjectivity of the risk (severity) and for screening the occult disturbance in evolution in general population. In addition no reports have further targeted the compliance issues. Hence this concept of assessment of symptom subjectivity as well as improving the compliance will facilitate a better patient care.
The concept of pre-clinical self/assisted assessment through a computer software can revolutionize the management of each and every disease that otherwise seems trivial but can have devastating long-term consequences. This may further be translated into a Android smart-phone based application as well. A country like India with largest and cheapest Mobile network can well enable a better patient screening/management/follow-up assessment, especially considering the enormous patient vs. doctor ratio. Moreover the data so collected can be well utilized for assessment of the burden/pattern of various diseases and hence may be extremely useful for policy planning in due course. This can further enhance the rapidly upcoming concept of maintaining detailed electronic clinical records world-wide. India with its enormous population is very likely to contribute to a large data while incorporating the concept of big-data management and artificial intelligence with such computer based programs, will definitely revolutionize the approach towards global health.
Acknowledgements
AM would like to acknowledge Dr. GK Shukla Professor of statistics for his kind help.
Author Contributions
AK, a 3rd year graduate student of computer science from SRM Institute/University, Chennai India was the key person to think and design this computer program. PM and MS assisted her partially wherein PM gave specific inputs in electronic elaboration of biological sufferrings of patients. AK was enrolled in an undergraduate internship program in 2018 at Sleep laboratory of department of Pulmonary Medicine, King George’s Medical University, Lucknow India under the guidance of SK, RG & AS who were critical in teaching her the basic laboratory techniques and their interpretation. Moreover RG of department of pulmonary medicine was critical in initiating a collaboration with department of Otorhinolaryngology (VV, AM) for AK to further organize the institutional data along with her work. In accordance the master thesis work of VY under the chief guidance of AM was integrated with the prospects of this computerized program. VY was the key person to recruit the patients wherein PM participated in patient counselling and data collection. The corresponding author (AM) who was the chief guide and supervisor of VY was the the main person to draft the manuscript and obtaining inputs from AK, VV, SK, RG, AS and Dr GK Shukla (of statistics). All authors read and approved the final manuscript.
Compliance with Ethical Standards
Conflict of interest
The computer based algorithm has been designed primarily by AK with partial assistance by PM & MS. In addition www.arth.com of CA USA has been of moderate help generating this idea and helping AK to design the additional algorithm pertaining to body movements and so shares the joint intellectual rights in this regard. In addition AK has also worked in collaboration with www.neodigitech.com (Mr. Ritesh) to manufacture the computer program per se. Furthermore AK intends to utilize the same algorithm to develop a smartphone based free application for general population in order to screen the disorder and to assess the severity of the problem.
Ethical Standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 2.Carpi MTM, Alonso DP, Marín SG, Mañes CV, Cacacho ALF, Paz CP, Saez SG, Trigo JMM, Vallés EC, Dronda SB. Stop-Bang questionnaire in obstructive sleep apnea syndrome: a severity predictor. Eur Respir J. 2015;46:PA2343. [Google Scholar]
- 3.Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999;131(7):485–491. doi: 10.7326/0003-4819-131-7-199910050-00002. [DOI] [PubMed] [Google Scholar]
- 4.Royant-Parola S, Hartley S, Aussert F, Dagneaux S, Brion A, Aisenberg N, Londe V, Poirot I, Martinot C, Escourrou P. Use of a computer algorithm for defining the care pathway of patients suffering from sleep disorders. Sleep Med. 2017;40(1):e283–e284. doi: 10.1016/j.sleep.2017.11.832. [DOI] [Google Scholar]
- 5.Lee YK, Bister M, Salleh YM (2007) A generic algorithm for detecting obstructive sleep apnea hyponea events based on oxygen saturation. In: 2006 3rd Kuala Lumpur international conference on biomedical engineering proceedings, pp 338–341
- 6.Young R. Researchers use AI algorithm to help those suffering from sleep disorders. http://trendintech.com/2017/08/15/researchers-use-ai-algorithm-to-help-those-suffering-from-sleep-disorders/. Accessed 4 Nov 2018