Abstract
It has become increasingly clear in the past decade that surgical management of OSAHS is most successfully managed with multilevel surgery (Cahali in Laryngoscope 113(11):1961–1968, 2003; Friedman et al. in Otolaryngol Head Neck Surg 131:89–100, 2004; Laryngoscope 114:441–449, 2004; Pang and Woodson in Otolaryngol Head Neck Surg 137(1):110–114, 2007; Li and Lee in Laryngoscope 119:2472–2477, 2009; Vicini et al. in Head Neck 36:77–78, 2014; Mantovani et al. in Acta Otorhinolaryngol Ital 32:48–53, 2012; Morgenthaler et al. in Sleep 30:519–529, 2007). In particular, drug-induced sleep endoscopy (DISE) has shown that the nose and soft palate are important anatomic components of obstruction in OSAHS and therefore should be treated as far as possible as a single stage procedure. The nasal patency being pivotal in the outcome of the sleep apnoea surgery. To ascertain the effectiveness and ease of carrying out multilevel single stage procedure in patients of obstructive sleep apnoea, and to use BARB sutures for relocation palatoplasty as a new technique to address level 2 collapse without excising much of soft palatal tissue. We have carried out a prospective study of 50 OSA (mild to severe) patients with nasal and retropalatal obstruction specifically without BOT or hypopharyngeal component of obstruction. The nasal component being treated with various procedures depending on the deformity or nature of obstruction and retropalatal component addressed by barbed relocation pharyngoplasty (BRP) being a relatively new procedure. We observed that nasal surgeries along with BRP can provide as an effective and safe option with very promising results. Adding BRP in the same stage with nasal surgery has been proved to be a simple, easy to learn, safe procedure with promising results in the management of OSA. Key points to be, the level of obstruction noted on DISE and proper patient selection can help us give the patients a good surgical result in a single stage procedure.
Keywords: BARB sutures, Relocation palatoplasty, Soft palate surgery, Palatal surgery in obstructive sleep apnoea (OSA)
Introduction
The decreased efficacy, increased morbidity, increased economic burden and hence lowered compliance for the completion of treatment posed by multiple stage procedures were the concerns that haunted us. Our aim was to give our patients a multilevel single stage surgery with the aim to establish, a patent airway in patients with level 1 and level 2 obstructions in a single sitting. The study was carried out to analyse the efficacy and comfort of doing a multilevel single stage surgery in patients of OSA to achieve the reduction of morbidity of OSA and OSA surgeries, decreasing the economic burden on the patients and increase the compliance to our treatment. A single stage multilevel surgery avoids delay of time in the management of OSA and the need of repeated hospitalization for multiple procedures for OSA surgical management. The combination of the two surgeries is very effective and easily doable in cases of OSA with nasal and retro palatal obstructions.
Nasal surgeries for correction of nasal obstruction have been described and are being done for decades. Conventional septoplasty with various turbinate reduction procedures have been done by ENT surgeons routinely. Rhinoplasty for functional reasons such as internal or external nasal valve obstructions, high anterior septal cartilaginous deviations requiring extracorporeal septoplasties via the open rhinoplasty approach have been described in literature for over 2 decades now. Most ENT surgeons are well aware and well versed with various nasal surgeries done for relieving nasal obstruction, hence we would be only mentioning the surgery we chose in different patients depending on the deformity.
OSA and its surgical management has been constantly evolving and vastly studied, especially for the retro palatal obstruction. The retro palatal region being so highly dynamic in nature, there have been multiple invasive procedures that have been described in the past. The main mechanism of the most classic palatal techniques for relieving snoring/obstructive sleep apnoea syndrome (OSAS) was basically the shortening of the soft palate by trimming the free edge (UPPP and LAUP) or pulling up the uvula and the soft palate. In the last years, many new palatal surgical techniques for snoring and OSAS were devised to address mainly the lateral pharyngeal wall and to enlarge the oropharyngeal inlet laterally (lateral pharyngoplasty [1], Z-palatoplasty [2], uvulopalatoplasty (UP2) [3], expansion sphincter pharyngoplasty (ESP) [4] and relocation pharyngoplasty [5]).
The most recent palatal procedure being barbed relocation pharyngoplasty or barb suture suspension palatoplasty.
In this study the multilevel single stage surgery described, includes various nasal surgeries for level 1 obstructions (turbinate surgery, septoplasty, open rhinoplasty, adenoid surgery), and barb relocation palatoplasty for level 2 obstruction.
Materials and Methods
Patients and Methods
This preliminary prospective study was conducted at Ghaisas ENT Hospital Pune and Prime ENT Centre Andheri West, Mumbai starting from since Jan 2017. Prior to conduction of the study, an informed detailed consent was taken from each patient. A group of 50 patients clinically diagnosed with OSA and obvious nasal septal deviations were selected. All patients were asked to fill out ESS [9] and STOP BANG questionaire. Each patient underwent a PSG level 3, drug induced sleep endoscopy, Rhinomanometry to ascertain the diagnosis. A 4 phase rhinomanometry was done for objective evaluation of nasal obstruction (Fig. 1a, b).
Fig. 1.
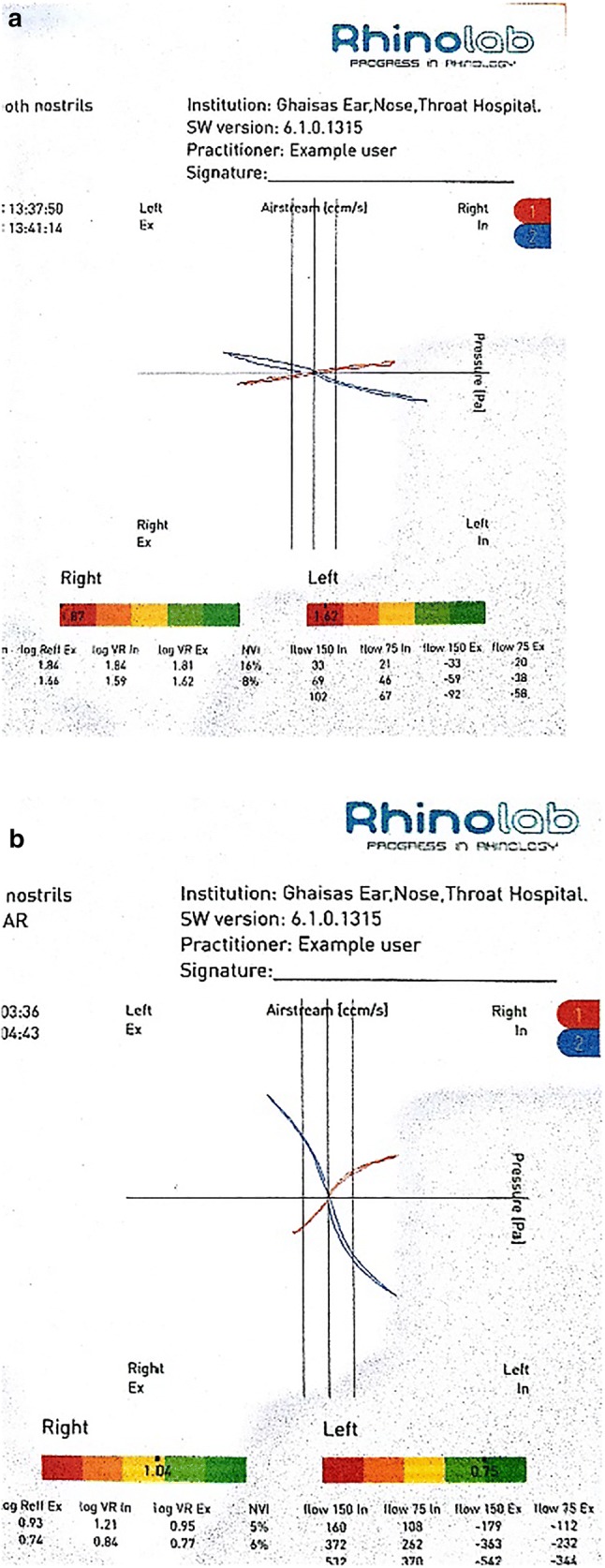
a Pre-op 4 phase rhinomanometery evaluation, b Post-op rhinomanomtery
Inclusion Criteria Included
Age between 25 and 60 years.
Mild to severe OSA with AHI of more than 5 (PSG LEVEL 3).
DISE indicating a purely nasal and retropalatal obstruction.
BMI of no more than 38.
Patients not accepting or unwilling to use CPAP treatment.
Exclusion Criteria Included
Patients with severe medical illness not fit for GA.
DISE indicating retro lingual or hypopharyngeal component of collapse.
Age more than 60 years. with uncertainty of CPAP compliance.
A careful general, ear nose and throat (ENT) history of each patient was taken with particular attention given to sleep history, preferably by the spouse or family member.
For all cases, the following data were recorded:
Age,
Sex,
BMI,
ESS (Epworth Sleepiness Scale) Pre op and Post op after 1 year,
AHI—Pre and post op after 1 year,
ODI—Pre and Post op after 1 year,
Complications,
Flexible nasopharyngoscopy post-operative.
Surgical Technique
Most cases were operated in a step wise manner, the first being nasal surgery in the form of functional rhinoplasty via open approach/conventional septoplasty/ITH reduction with coblation channelling/concha bullosa excision. The second step being barb relocation palatoplasty (BRP), operated under general anaesthesia, oral intubation with South Pole tube.
Step 1
Nasal surgery was done in each patient as deemed necessary depending on the DISE findings. An open approach rhinoplasty was done for 14 case to treat the nasal component of obstruction with insertion of spreader grafts (figure) to open the internal nasal valve area along with a septoplasty. The turbinate’s if hypertrophic were reduced by coblation channelling. 34 cases underwent a conventional septoplasty with turbinate reduction and 2 case in which the salpingo pharyngeal folds were found to be excessively large, for which submucosal radiofrequency channelling was done with the Sutter RF tongue base channelling probe, along with ITR (Table 1).
Table 1.
Nasal surgeries done along with BRP (in all cases) in the multilevel single stage op
| Nasal obstruction | Nasal surgery of choice | No. of patients |
|---|---|---|
| High anterior nasal septal deviation with internal nasal valve collapse/gross caudal dislocations/external valve collapse | Functional rhinoplasty via open approach − spreader grafts in all/extracorporeal septoplasty | 14 |
| Inferior/bony posterior deviations/limited nasal deviations | Conventional septoplasty + INF turbinate reduction with coblation channelling | 34 |
| Inferior turbinate hypertrophies with enlarged SP fold | Radio frequency channelling | 02 |
Step 2
The oral cavity exposed by a slotted Boyle–Davis mouth gag with head extended in supine position. Extra capsular tonsillectomy done with coblation using EVAC 70 wand. Care was taken to preserve the mucosa over the palatoglossus and palatopharyngeal muscles. The palatopharyngeal muscle bulk was split vertically to release it from its lower fibres so as to ease the mobilization of the muscle bulk anterolaterally. A 2-0 round body, double needle bidirectional barb PDS suture (Fig. 2) was inserted up to the midpoint of the suture length (transition zone of the suture) at the PNS (Posterior Nasal Spine) submucosally. Each end running sub mucosal to the base of the uvula—reinserting submucosal to exit near the pterygoid hamulus or superior end of the pterygomandibular raphe—from the hamulus to the tonsillar bed superior pole—inserting into the bulk of the released palatopharyngeal muscle and re inserting through the tonsillar bed to the pterygomandibular raphe on either side. Thus, giving the soft palate an anterior and lateral pull and expanding the retropalatal space. The suture being knotless was pulled on either sides to the required tension and the nipped off at the last point of exit (Fig. 3).
Fig. 2.

Bidirectional BARB suture
Fig. 3.
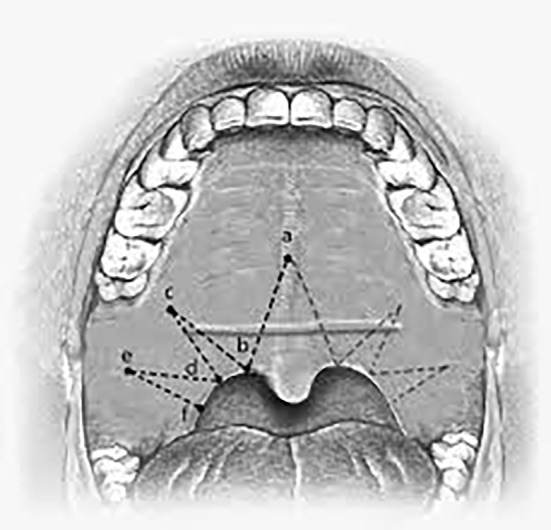
Diagrammatic representation of the suturing technique and landmarks. Point a—Post nasal spine; Point b—base of the uvula; Point c—pterygoid hamulus; Point d—tonsillar fossa superior; Point e—Pterygomandibular raphe; Point f—posterior pillar
Results
The pre-operative and post-operative results in terms od AHI, ODI and ESS were measured in each patient operated for obstructive sleep apnoea. All patients underwent a flexible nasopharyngoscopy to visualize the patency of the velum and nose postoperatively along with a postoperative PSG level 3 to compare the pre and post-operative AHI and ODI values (Fig. 4a, b). We observed that the mean AHI value preoperatively of 40.6 had reduced to 10.2 (Table 2); the mean preoperative ODI reduced from 42.7 to a mean of 12.6 (Table 3); on comparison of the ESS score, a reduction of 10 points was noted (Table 4).
Fig. 4.
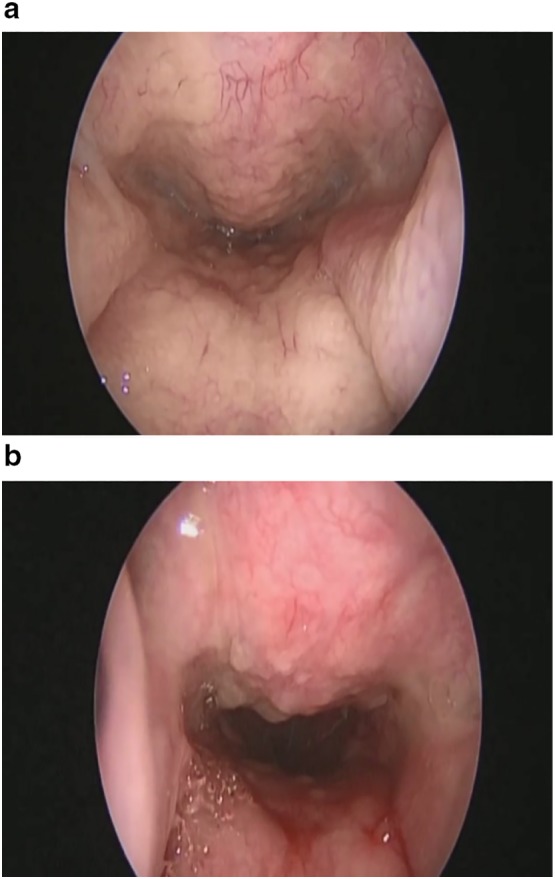
a Preoperative velum patency, b post-operative velum patency after 1 year
Table 2.
Pre-op and post op AHI
| Pre-op AHI | Post op AHI after 1 year |
|---|---|
| 40.6 | 10.2 |
Table 3.
Pre-op and post op ODI
| Pre-op ODI | Post op ODI after 1 year |
|---|---|
| 42.7 | 12.6 |
Table 4.
Pre-op and post op ESS
| Pre-op ESS | Post op ESS after 1 year |
|---|---|
| 13 | 03 |
Complications and Post Op Observations
Since a large number of patients underwent a functional rhinoplasty, the complications associated with an open rhinoplasty approach like nasal dorsal and tip swelling (usually subsides within 1–3 months post op), displacement of various grafts inserted, aesthetic disfigurement etc. were looked for in the complete post op period. There were no such complications noted in any of the patients during the post op period of 1 year. 2 patients out of the 14, were operated for cosmetic rhinoplasty along with BRP, where in paramedian/transverse and lateral nasal osteotomies were done. These 2 patients did have infra orbital hematoma and mild discoloration but this resolved within 3 weeks post op.
During palatal surgery the complications that can be expected are post tonsillectomy bleeding, but with the advent of coblation we didn’t face any such post-operative bleed. All nasal surgeries were uneventful and no post op bleed. In 2 patients, slipping of the palatopharyngeal muscle due to tear through, leading to the barb suture loop showing within the tonsillar fossa and causing foreign body sensation, this was treated by diluted hydrogen peroxide gargles and anti-inflammatory drugs. Out of these two patients who had a slippage/tear through of the muscle we had to cut out the loop which was visible in the tonsillar fossa, since the patient didn’t tolerate it. This eventually led to extrusion of the entire suture length approximately 4th week post op. This failure of the barb suture holding in place or the cut through of the palatopharyngeal muscle bulk was attributed to the inadequate inferior release/level of the transverse cut taken on the muscle, which was noted and corrected in the following cases. Most patients complained of post op foreign body sensation in the soft palate which resolved about 1 month after the surgery. None of the patient complained of velopalatal insufficiency (VPI) or a permanent change in voice quality (Table 5).
Table 5.
Complications
| Complications | No. of patients |
|---|---|
| Nasal bleed post op/residual nasal septal deviation | 0 |
| Barb suture failure/cut through of the palatopharyngeal muscle | 2 |
| Velopharyngeal insufficiency | 0 |
| Permanent change in quality of voice | 0 |
Discussion
Open rhinoplasty or open approach rhinoplasty for functional nasal symptoms has been a well-known concept and has been practiced for over 4 decades now. Internal nasal valve collapse is treated with spreader grafts that helps to increase the internal nasal valve dimensions to facilitate breathing through the nose, while external nasal valve collapse being corrected with lower alar batten grafts or Onlay grafts. Extracorporeal rhinoplasties for anterior and high nasal septal deviations in grossly crooked noses with breathing difficulties have proved to be a treatment of choice instead of conventional septoplasties.
Barbed reposition pharyngoplasty is deeply inspired by the relocation pharyngoplasty (RP) as devised and published by Li et al. [5]. The purpose is to use a series of sutures to widen the oropharyngeal isthmus laterally and to relocate anteriorly the lateral insertion of the soft palate to increase the retropalatal airway.
The anterior sustaining anatomical structure is the more stable fibrous pterygomandibular raphe instead of the weaker palatoglossus muscle; this solution is inspired to Mantovani technique [7]. Pterygomandibular raphe is a fibrous band joining the pterygoid hamulus to the mandible relatively variable in the different subjects; it is always easy to locate during surgery by inspection or, may be better, by palpation. It lies anteriorly and laterally to the posterior pillar, in the best position for an effective pulling direction to increase the transversal oropharyngeal dimension and to widen the retropalatal anteroposterior distance. Its anatomical location is far from significant nerves and vessels preventing undesired complications during suturing.
The repositioned muscle is the palatopharyngeal muscle, after a preliminary inferior release; this solution is inspired to Cahali technique [1]. The inferior muscle release is planned to allow an easier and more stable repositioning of the posterior pillar in a more lateral and anterior location without any significant tension.
The bidirectional barbed suture instead of a conventional series of single stitches; this solution is inspired to Mantovani technique [7]. Barbed suture proved to be much faster and easier to handle, because it is a knotless technology (knotting inside the pharynx may be not easy for the less experienced surgeons, and even for the most experienced ones, it takes obviously more time). Also, barbed suture allows running more thread loops around the muscle, creating a sort of dense net, for a better distribution of the repositioning forces over the muscle flap. In comparison to Pang–Woodson technique [4], the pulling suture works with a 90 angle on the muscle fibres array, with a much less risk to tear the flap tip. 4.
An anterior pillar totally sparing approach for tonsillectomy proved to be very useful for the better tensionless reconstruction of the mucosal covering at the end of the procedure. Two more remarks about the posterior pillar repositioning are given. If properly located between the upper third and the inferior two-thirds of the posterior pillar, the first suture loop will produce a sort of ‘‘posterior pillar steal’’, inspired to the same concept of lateral crural steal technique in tip rhinoplasty. The meaning is that the upper part of the posterior pillar will be transposed into the soft palate free edge, which will be transversally enlarged in a very significant way. The posterior pillar mucosa is not dissected free from the flap, but follows it in its repositioning. The meaning is less surgical time, no potential mucosal damage, immediate mucosal closure, probably faster recovery and less pain [8].
Conclusion
Multilevel single stage surgery has been described in literature and also is being carried out for OSA management. This not only helps to reduce the time consumption and economic burden on the patients by avoiding repeated hospitalization and need for anaesthesia, but also helps us as surgeons to give our patient safe and less invasive procedure than ESP/ZETA, yet very effective. In this prospective study we have specifically chosen only level 1–2 obstructions for surgical management. We observed that nasal surgeries along with BRP can provide as an effective and safe option with very promising results. Nasal surgeries being done routinely by ENT surgeons, adding BRP in the same stage has been proved to be a simple, easy to learn, safe procedure with promising results in the management of OSA. Key points to be, the level of obstruction noted on DISE and proper patient selection can help us give the patients a good surgical result in a single stage procedure. Moreover, BRP is easy to learn even for the inexperienced surgeons and less time consuming and with no significant complications. The minimal muscle and mucosal resection and the absence of knots in the pharynx are well tolerated and accepted by the patient in terms of invasiveness.
As BRP is being presented as a step procedure in a multilevel single stage operation, the individual role of BRP in these complex managements of OSA is yet to be studied. The number of patients being minimal for proving the long-term efficacy of BRP, we are working on the topic and hopefully shall present more data with larger number of patients.
Compliance with Ethical Standards
Conflict of interest
We the author’s, N N Madkikar, Shailesh Pandey, Virendra Ghaisas here by declare that we do not have any conflict of interest.
Ethical Approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards.
Informed Consent
An informed and written consent was obtained from all subjects included within the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Nilesh Madkikar, Email: drnileshmadkikar@gmail.com.
Shailesh Pandey, Email: shail1974@gmail.com.
References
- 1.Cahali MB. Lateral pharyngoplasty: a new treatment for obstructive sleep apnea hypopnea syndrome. Laryngoscope. 2003;113(11):1961–1968. doi: 10.1097/00005537-200311000-00020. [DOI] [PubMed] [Google Scholar]
- 2.Friedman M, Ibrahim HZ, Vidyasagar J, et al. Z-palatoplasty (ZPP): a technique for patients without tonsils. Otolaryngol Head Neck Surg. 2004;131:89–100. doi: 10.1016/j.otohns.2004.02.051. [DOI] [PubMed] [Google Scholar]
- 3.Friedman M, Ibrahim HZ, Lowenthal S, Vidyasagar J, Joseph NJ. Uvulopalatoplasty (UP2): a modified technique for selected patients. Laryngoscope. 2004;114:441–449. doi: 10.1097/00005537-200403000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Pang KP, Woodson BT. Expansion sphincter pharyngoplasty: a new technique for the treatment of obstructive sleep apnea. Otolaryngol Head Neck Surg. 2007;137(1):110–114. doi: 10.1016/j.otohns.2007.03.014. [DOI] [PubMed] [Google Scholar]
- 5.Li HY, Lee LA. Relocation pharyngoplasty for obstructive sleep apnea. Laryngoscope. 2009;119:2472–2477. doi: 10.1002/lary.20634. [DOI] [PubMed] [Google Scholar]
- 6.Vicini C, Montevecchi F, Pang K, Bahgat A, Dallan I, Frassineti S, Campanini A. Combined transoral robotic tongue base surgery and palate surgery in obstructive sleep apnea–hypopnea syndrome: expansion sphincter pharyngoplasty versus uvulopalatopharyngoplasty. Head Neck. 2014;36:77–78. doi: 10.1002/hed.23271. [DOI] [PubMed] [Google Scholar]
- 7.Mantovani M, Minetti A, Torretta S, Pincherle A, Tassone G, Pignataro L. The velo-uvulo-pharyngeal lift or “roman blinds” technique for treatment of snoring: a preliminary report. Acta Otorhinolaryngol Ital. 2012;32:48–53. [PMC free article] [PubMed] [Google Scholar]
- 8.Morgenthaler T, Alessi C, Friedman L, et al. Practice parameters for the use of actigraphy in the assessment of sleep and sleep disorders: an update for 2007. Sleep. 2007;30:519–529. doi: 10.1093/sleep/30.4.519. [DOI] [PubMed] [Google Scholar]
- 9.Vignatelli L, Plazzi G, Barbato A, et al. Italian version of the Epworth sleepiness scale: external validity. Neurol Sci. 2003;23:295–300. doi: 10.1007/s100720300004. [DOI] [PubMed] [Google Scholar]


