Abstract
Background
Despite the epidemic of cardiovascular disease and the benefits of cardiac rehabilitation (CR), availability is known to be insufficient, although this is not quantified. This study ascertained CR availability, volumes and its drivers, and density.
Methods
A survey was administered to CR programs globally. Cardiac associations and local champions facilitated program identification. Factors associated with volumes were assessed using generalized linear mixed models, and compared by World Health Organization region. Density (i.e. annual ischemic heart disease [IHD] incidence estimate from Global Burden of Disease study divided by national CR capacity) was computed.
Findings
CR was available in 111/203 (54.7%) countries; data were collected in 93 (83.8% country response; N = 1082 surveys, 32.1% program response rate). Availability by region ranged from 80.7% of countries in Europe, to 17.0% in Africa (p < .001). There were 5753 programs globally that could serve 1,655,083 patients/year, despite an estimated 20,279,651 incident IHD cases globally/year. Volume was significantly greater where patients were systematically referred (odds ratio [OR] = 1.36, 95% confidence interval [CI] = 1.35–1.38) and programs offered alternative models (OR = 1.05, 95%CI = 1.04–1.06), and significantly lower with private (OR = .92, 95%CI = .91–.93) or public (OR = .83, 95%CI = .82–84) funding compared to hybrid sources.
Median capacity (i.e., number of patients a program could serve annually) was 246/program (Q25-Q75 = 150–390). The absolute density was one CR spot per 11 IHD cases in countries with CR, and 12 globally.
Interpretation
CR is available in only half of countries globally. Where offered, capacity is grossly insufficient, such that most patients will not derive the benefits associated with participation.
Keywords: Cardiac rehabilitation, Capacity, Density, Preventive cardiology, Global health, Health services
Research in context
Evidence before this study
Cardiac rehabilitation (CR) is an effective secondary prevention strategy for one of the leading burdens of disease and the leading cause of death globally, namely cardiovascular disease.
Reviews of the literature, however, suggested CR was only available in < 40% of countries globally, and density, characterized in only several countries, was highly variable. Therefore, it is unknown how many patients can access these guideline-recommended services around the world, and where the greatest gaps exist.
Added value of this study
Cardiac rehabilitation availability around the world has been established for the first time. Based on primary data collected through this global survey, CR was shown to be available in 54·7% countries (median = 4 programs/country). The 5,753 programs in the world served a median of 157 (Q25–Q75 = 75–350) patients/year each. Programs that had systematic inpatient referral, hybrid funding sources and offered alternative models served significantly more patients, among other factors. Median national capacity in countries with CR was 1500 (Q25–75 = 300–7500) patients/year (120 across all countries globally). Where available, the density was one CR spot per 11 incident annual ischemic heart disease patients globally (lowest in Africa, greatest in Western Pacific).
Implications of all the available evidence
CR availability, capacity, and density are vastly insufficient to serve all patients in need.
Advocacy to develop greater capacity, particularly in Africa and South-East Asia, is needed to ensure all guideline-indicated patients derive the 20% mortality and re-hospitalization reductions associated with participation. Policies should promote greater public funding and support programs in delivering programming outside of clinical centers.
Alt-text: Unlabelled Box
1. Introduction
Cardiovascular diseases (CVDs) are among the leading burdens of disease and disability globally [1], [2]. In 2015, there were 422.7 million CVD cases around the world [2]. Secondary prevention is needed to mitigate the reduced quality and quantity of life in patients with this chronic disease. Cardiac rehabilitation (CR) is a cost-effective model of care shown to reduce cardiovascular mortality and morbidity by 20% [3], [4].
Despite guidelines promoting referral to CR [5], and the clear association between availability and utilization [6], previous estimates suggested it is not available in over 60% of countries worldwide, and where it exists there is insufficient supply to meet growing need [7], [8]. There has been one review of the literature globally [7], and another in low and middle-income countries [9], which has characterized CR availability, but to date there has been no primary study which has ascertained in which countries CR exists. Moreover, there have been a few studies which have characterized CR capacity at national or regional levels but not at a global level [10], [11], [12], and none have juxtaposed supply in relation to burden of diseases indicated for CR as per clinical practice guideline recommendations (i.e., density).
Accordingly, the aims of this study were to establish CR: (1) availability, (2a) volumes served and capacity, and (b) the factors associated with greater volume. Given this was the first study to establish CR volumes globally and no previous research has examined factors associated with program volumes to our knowledge, tests of association were exploratory. The study also aimed to establish CR: (3) density and (4) barriers to broader delivery. As applicable, these were described by program, country (including consideration of CR-indicated disease burden), World Health Organization (WHO) region, and globally. It was hypothesized there would be significant regional variation as well as in terms of disease burden in many of these parameters given the reviews outlined above [7], [9]; however again, these analyses were exploratory given this is the first time CR has been scoped on a global scale.
2. Methods
2.1. Design & Procedure
This was a cross-sectional study. The study procedures were approved by York University's Office of Research Ethics (Toronto, Canada) and Mayo Clinic's Institutional Review Board (Rochester, United States). Participating CR centers provided informed consent electronically.
First, a list of all countries globally was compiled, by cross-referencing several key sources, including WHO [13], [14]. Small islands affiliated with larger countries were considered part of the larger country (e.g., Macau), and United Kingdom countries were considered separately given their disparate CR practices and policies. Two hundred and three countries were considered (Table 1, Table 2). Some of these countries are not categorized by WHO. These countries were allocated to the most applicable geographic region.
Table 1.
Cardiac rehabilitation availability, volume, capacity, and density by country with any cardiac rehabilitation, N = 111.
| WHO Region | Human Development Index* | IHD incidence† | Year 1st CR program | # CR programs in country | Median annual volume/program | Median annual capacity/program | National CR capacity‡ | CR density§ | |
|---|---|---|---|---|---|---|---|---|---|
| CR | |||||||||
| density ranking || | |||||||||
| African (8 countries) | |||||||||
| Algeria | 0.745 | 140,592 | NA | 1 | NA | 55 | 55 | 2556 | 72 |
| Benin | 0.485 | 11,973 | NA | 1 | NA | 55 | 55 | 218 | 57 |
| Kenya | 0.555 | 55,174 | 2010 | 3 | 20 | 50 | 150 | 368 | 62 |
| Mauritius | 0.513 | 3872 | 2013 | 1 | 60 | 60 | 60 | 65 | 46 |
| Nigeria | 0.527 | 223,994 | 2012 | 1 | 50 | 50 | 50 | 4480 | 73 |
| South Africa | 0.666 | 108,455 | 1989 | 23 | 50 | 90 | 2070 | 52 | 41 |
| Tanzania | 0.531 | 64,326 | NA | 1 | NA | 55 | 55 | 1170 | 69 |
| Uganda | 0.493 | 31,951 | NA | 1 | NA | 55 | 55 | 581 | 65 |
| Mean ± SD | 0.564 ± 0.092 | 80,042 ± 74,459 | 2006 ± 11 | 4 ± 8 | 45 ± 15 | 59 ± 13 | 319 ± 708 | 1186 ± 1569 | 61 ± 12 |
| Median (Q25-Q75) | 0.529 (0.498–0.638) | 59,750 (16968–132,558) | 2011 (1994–2013) | 1 (1–3) | 50 (28–58) | 55 (51–59) | 55 (55–128) | 474(103–2210) | 64(49–71) |
| Americas (28 countries) | |||||||||
| Argentina | 0.827 | 122,357 | 1998 | 23 | 1500 | 2000 | 46,000 | 3 | 5 |
| Aruba | NA | NA | NA | 1 | NA | 200 | 200 | NA | NA |
| Barbados | 0.795 | 1240 | 1994 | 1 | 70 | 96 | 96 | 13 | 18 |
| Bermuda | NA | 197 | 2012 | 1 | 220 | 400 | 400 | 1 | 1 |
| Brazil | 0.754 | 529,062 | 1973 | 75 | 60 | 72 | 5400 | 98 | 51 |
| Canada | 0.920 | 91,030 | 1960 | 170 | 300 | 300 | 51,000 | 2 | 3 |
| Chile | 0.847 | 45,008 | 2009 | 10 | 30 | 200 | 2000 | 23 | 28 |
| Colombia | 0.727 | 75,245 | 1972 | 50 | 410 | 390 | 19,500 | 4 | 7 |
| Costa Rica | 0.776 | 8288 | 1985 | 6 | 45 | 120 | 720 | 12 | 17 |
| Cuba | 0.775 | 49,789 | 1973 | 8 | 145 | 180 | 1440 | 35 | 33 |
| Curaçao | NA | NA | NA | 2 | 120 | 200 | 400 | NA | NA |
| Dominican Republic | 0.722 | 193,919 | 2016 | 2 | NA | 200 | 400 | 485 | 64 |
| Ecuador | 0.739 | 27,046 | 1995 | 5 | 36 | 190 | 950 | 29 | 30 |
| El Salvador | 0.680 | 9129 | NA | 2 | NA | 200 | 400 | 23 | 28 |
| Grenada | 0.754 | 296 | NA | 1 | NA | 200 | 200 | 1 | 2 |
| Guam | NA | 311 | NA | 1 | NA | 200 | 200 | 2 | 3 |
| Guatemala | 0.640 | 13,671 | 2011 | 2 | 18 | 60 | 120 | 114 | 52 |
| Honduras | 0.625 | 10,939 | 2005 | 2 | 20 | 20 | 40 | 274 | 58 |
| Jamaica | 0.730 | 8026 | 2006 | 3 | 24 | 60 | 180 | 45 | 39 |
| Mexico | 0.762 | 161,348 | 1944 | 24 | 38 | 250 | 6000 | 27 | 29 |
| Panama | 0.788 | 5039 | 2006 | 1 | 38 | 80 | 80 | 63 | 44 |
| Paraguay | 0.693 | 14,892 | 2011 | 3 | 125 | 200 | 600 | 25 | 29 |
| Peru | 0.740 | 49,967 | 1992 | 10 | 80 | 250 | 2500 | 20 | 25 |
| Puerto Rico | NA | 15,286 | NA | 1 | NA | 200 | 200 | 76 | 47 |
| Trinidad and Tobago | 0.780 | 4759 | NA | 2 | NA | 200 | 400 | 12 | 17 |
| United States of America | 0.920 | 1,344,974 | 1970 | 2632 | 150 | 208 | 547,456 | 3 | 6 |
| Uruguay | 0.795 | 10,656 | 1970 | 12 | 120 | 200 | 2400 | 4 | 8 |
| Venezuela | 0.767 | 45,575 | 1974 | 9 | 103 | 163 | 1467 | 31 | 32 |
| Mean ± SD | 0.763 ± 0.072 | 78,241 ± 233,742 | 1989 ± 20 | 109 ± 496 | 174 ± 320 | 251 ± 354 | 24,670 ± 103,253 | 55 ± 104 | 26 ± 19 |
| Median (Q25-Q75) | 0.762 (0.727–0.795) | 10,656 (1152–47,682) | 1994 (1973–2008) | 3 (1–12) | 80 (37–148) | 200 (131–206) | 500 (200–2475) | 23 (4–49) | 28 (7–41) |
| Eastern Mediterranean (12 countries) | |||||||||
| Afghanistan | 0.479 | 89,056 | 2014 | 1 | 100 | 150 | 150 | 594 | 5766 |
| Bahrain | 0.824 | 3842 | 1998 | 1 | 140 | 500 | 500 | 8 | 12 |
| Egypt | 0.691 | 369,488 | 2010 | 2 | 20 | 100 | 200 | 1847 | 70 |
| Iran | 0.774 | 235,157 | 1994 | 34 | 250 | 475 | 16,150 | 15 | 20 |
| Kuwait | 0.800 | 7648 | NA | 1 | NA | 246 | 246 | 31 | 32 |
| Lebanon | 0.763 | 27,633 | 2014 | 1 | 100 | 300 | 300 | 92 | 49 |
| Morocco | 0.647 | 156,088 | 2016 | 1 | NA | 246 | 246 | 635 | 67 |
| Pakistan | 0.550 | 622,146 | 2004 | 4 | 900 | 1500 | 6000 | 104 | 63 |
| Qatar | 0.856 | 7003 | 2013 | 1 | 157 | 192 | 192 | 37 | 34 |
| Saudi Arabia | 0.847 | 82,510 | NA | 1 | NA | 246 | 246 | 335 | 60 |
| Tunisia | 0.725 | 50,217 | 2010 | 1 | 90 | 150 | 150 | 335 | 59 |
| United Arab Emirates | 0.840 | 21,885 | NA | 1 | NA | 246 | 246 | 89 | 48 |
| Mean ± SD | 0.733 ± 0.121 | 139,389 ± 187,985 | 2008 ± 8 | 4 ± 9 | 220 ± 283 | 363 ± 378 | 1677 ± 4573 | 369 ± 518 | 48 ± 20 |
| Median (Q25-Q75) | 0.763(0.658–0.836) | 66,363 (11,208–215,389) | 2010 (2001–2014) | 1 (1–2) | 120 (93–227) | 246 (161–431) | 246 (194–450) | 213 (32–549) | 54 (33–65) |
| Europe (46 countries) | |||||||||
| Austria | 0.893 | 32,901 | 1962 | 26 | 750 | 200 | 5200 | 6 | 10 |
| Belarus | 0.796 | 88,874 | 1981 | 5 | 300 | 300 | 1500 | 59 | 44 |
| Belgium | 0.896 | 66,985 | 1977 | 48 | 275 | 300 | 14,400 | 5 | 9 |
| Bosnia and Herzegovina | 0.750 | 19,068 | 1959 | 1 | 800 | 2000 | 2000 | 10 | 15 |
| Bulgaria | 0.794 | 55,871 | 1958 | 1 | 2200 | 3000 | 3000 | 19 | 24 |
| Croatia | 0.827 | 26,066 | 1957 | 3 | 940 | 940 | 2820 | 9 | 14 |
| Cyprus | 0.856 | 2665 | NA | 1 | NA | NA | NA | NA | 11 |
| Czech Republic | 0.878 | 66,012 | 1993 | 15 | 65 | 200 | 3000 | 22 | 27 |
| Denmark | 0.925 | 23,455 | 1990 | 35 | 200 | 250 | 8750 | 3 | 6 |
| England | 0.909 | 318,284 | 1978 | 266 | 490 | 500 | 133,000 | 2 | 4 |
| Estonia | 0.865 | 10,938 | 1994 | 2 | 150 | 150 | 300 | 37 | 35 |
| Finland | 0.89 | 25,677 | 1978 | 25 | 55 | 98 | 2450 | 11 | 16 |
| France | 0.897 | 259,251 | 1972 | 130 | 475 | 485 | 63,050 | 4 | 8 |
| FYR of Republic of Northern Macedonia | 0.748S | 8285 | NA | 1 | NA | 375 | 375 | 22 | 27 |
| Georgia | 0.769 | 16,488 | 1994 | 17 | 180 | 600 | 10,200 | 2 | 4 |
| Germany | 0.926 | 385,474 | 1950 | 120 | 800 | 825 | 99,000 | 4 | 8 |
| Greece | 0.866 | 61,036 | 1993 | 4 | 20 | 100 | 400 | 153 | 54 |
| Hungary | 0.836 | 69,698 | 1970 | 33 | 440 | 580 | 19,140 | 4 | 8 |
| Iceland | 0.921 | 1570 | 1983 | 4 | 168 | 185 | 740 | 2 | 4 |
| Ireland | 0.923 | 16,000 | 1985 | 37 | 256 | 300 | 11,100 | 1 | 6 |
| Israel | 0.899 | 23,152 | 1964 | 22 | 1000 | 1000 | 22,000 | 1 | 2 |
| Italy | 0.887 | 359,226 | 1974 | 221 | 350 | 355 | 78,455 | 5 | 9 |
| Kazakhstan | 0.794 | 57,125 | NA | 1 | NA | 375 | 375 | 152 | 53 |
| Kyrgyz Republic | 0.664 | 11,398 | NA | 1 | NA | 375 | 375 | NA | 31 |
| Latvia | 0.830 | 14,743 | 1997 | 2 | 150 | 400 | 800 | 18 | 23 |
| Lithuania | 0.848 | 23,421 | 1977 | 25 | 950 | 1000 | 25,000 | 1 | 2 |
| Luxembourg | 0.898 | 1683 | NA | 4 | NA | 375 | 1500 | 1 | 2 |
| Malta | 0.856 | 1958 | 2012 | 1 | 300 | 900 | 900 | 2 | 4 |
| Moldova | 0.699 | 21,376 | 2016 | 1 | 200 | 400 | 400 | 53 | 42 |
| Montenegro | 0.807 | 3049 | NA | 1 | NA | 375 | 375 | 8 | 13 |
| Netherlands | 0.924 | 88,550 | 1974 | 90 | 555 | 450 | 40,500 | 2 | 4 |
| Northern Ireland | NA | 8811 | 1980 | 13 | 255 | 215 | 2795 | 3 | 6 |
| Norway | 0.949 | 15,197 | NA | 35 | NA | 375 | 13,125 | 41 | 37 |
| Poland | 0.855 | 237,460 | 1973 | 56 | 350 | 375 | 21,000 | 11 | 16 |
| Portugal | 0.843 | 35,884 | 1988 | 23 | 75 | 100 | 2300 | 16 | 21 |
| Romania | 0.802 | 126,835 | 1978 | 3 | 1400 | 2500 | 7500 | 17 | 22 |
| Russia | 0.804 | 1,223,642 | 2010 | 3 | 400 | 500 | 1500 | 816 | 68 |
| Scotland | NA | 30,185 | 1985 | 69 | 356 | 296 | 20,424 | 1 | 2 |
| Serbia | 0.776 | 40,265 | 1968 | 2 | 1345 | 1570 | 3140 | 13 | 19 |
| Slovak Republic | 0.845 | 29,436 | 2015 | 7 | 50 | 200 | 1400 | 21 | 26 |
| Slovenia | 0.890 | 11,135 | 1995 | 2 | 100 | 150 | 300 | 37 | 35 |
| Spain | 0.884 | 175,537 | 1993 | 87 | 120 | 120 | 10,440 | 17 | 22 |
| Sweden | 0.913 | 50,475 | NA | 69 | 150 | 150 | 10,350 | 5 | 9 |
| Switzerland | 0.939 | 29,546 | 1997 | 51 | 255 | 255 | 13,005 | 2 | 4 |
| Turkey | 0.767 | 337,617 | 2010 | 10 | 100 | 350 | 3500 | 97 | 50 |
| Wales | NA | 15,432 | 1986 | 17 | 490 | 375 | 6375 | 2 | 4 |
| Mean ± SD | 0.852 ± 0.065 | 98,429 ± 198,290 | 1984 ± 17 | 35 ± 55 | 466 ± 463 | 550 ± 604 | 14,536 ± 27,142 | 38 ± 122 | 19 ± 17 |
| Median (Q25-Q75) | 0.861(0.804–0.898) | 29,491 (15,084-74,411) | 1984 (1974–1994) | 14 (2–40) | 300 (150–750) | 375 (211–520) | 3070(875–13,444) | 9(2–22) | 14 (6–27) |
| South-East Asia (6 countries) | |||||||||
| Bangladesh | 0.579 | 409,210 | NA | 1 | 160 | 200 | 200 | 2046 | 71 |
| India | 0.624 | 3,313,674 | 1997 | 23 | 200 | 400 | 9200 | 360 | 61 |
| Indonesia | 0.689 | 66,676 | 1985 | 13 | 98 | 100 | 1300 | 51 | 40 |
| Nepal | 0.558 | 66,134 | 2008 | 1 | 2000 | 3000 | 3000 | 22 | 27 |
| Sri Lanka | 0.766 | 66,927 | 2012 | 4 | 114 | 105 | 420 | 159 | 55 |
| Thailand | 0.740 | 199,828 | NA | 5 | NA | 200 | 1000 | 200 | 56 |
| Mean ± SD | 0.659 ± 0.086 | 687,075 ± 1,293,730 | 2001 ± 12 | 8 ± 9 | 514 ± 831 | 668 ± 1148 | 2520 ± 3419 | 473 ± 780 | 52 ± 16 |
| Median (Q25-Q75) | 0.656(0.573–0.747) | 133,378 (66541–1,135,326) | 2003 (1998–2011) | 5 (1–16) | 160 (106–1100) | 200 (104–1050) | 1150 (365–4550) | 179 (44–782) | 56 (37–64) |
| Western Pacific (11 countries) | |||||||||
| Australia | 0.939 | 80,169 | 1970 | 314 | 200 | 200 | 62,800 | 1 | 2 |
| Brunei | 0.865 | 471 | 2004 | 2 | 55 | 80 | 160 | 3 | 6 |
| China | 0.738 | 3,104,203 | 1984 | 216 | 300 | 325 | 70,200 | 44 | 38 |
| Japan | 0.903 | 501,740 | 1990 | 325 | 150 | 300 | 97,500 | 5 | 9 |
| Malaysia | 0.789 | 86,224 | 2007 | 6 | 300 | 250 | 1500 | 58 | 43 |
| Mongolia | 0.735 | 5241 | 2013 | 1 | NA | 250 | 250 | 21 | 25 |
| New Zealand | 0.915 | 10,110 | 1968 | 43 | 200 | 146 | 6278 | 2 | 4 |
| Philippines | 0.682 | 217,107 | 1975 | 10 | 105 | 560 | 5600 | 39 | 36 |
| Singapore | 0.925 | 14,299 | 1979 | 7 | 260 | 438 | 3066 | 5 | 9 |
| South Korea | 0.901 | 94,661 | 2009 | 17 | 200 | 250 | 4250 | 22 | 27 |
| Taiwan | NA | 43,795 | 1978 | 35 | 70 | 180 | 6300 | 7 | 11 |
| Mean ± SD | 0.839 ± 0.094 | 378,002 ± 873,254 | 1989 ± 16 | 89 ± 124 | 181 ± 80 | 271 ± 135 | 23,446 ± 35,315 | 19 ± 20 | 19 ± 15 |
| Median (Q25-Q75) | 0.883 (0.737–0.918) | 80,169 (10110–217,107) | 1984 (1975–2007) | 17 (6–216) | 200 (96–263) | 250 (180–250) | 5600 (1500–4588) | 7(3–6) | 11 (6–36) |
| Global Mean ± SD | 0.782 ± 0.117 | 164,764 ± 464,692 | 1990 ± 18 | 52 ± 254 | 324 ± 426 | 398 ± 534 | 14,911 ± 55,757 | 181 ± 568 | 27 ± 21 |
| Global Median (Q25-Q75) | 0.795 (0.729–0.881) | 40,265 (11267–101,558) | 1992 (1975–2009) | 4 (1–25) | 157 (75–350) | 246 (150–390) | 1500 (300–7500) | 21(4–83) | 25 (8–47) |
*Human Development Index was obtained from United Nations Development Program [31].
†Incidence of IHD was obtained from Global Burden of Disease study [15].
‡National CR capacity calculated using median number of patients program could serve per year (from survey) multiplied by the number of programs in the country (ascertained from national champions). Value represents the number of patients who could receive CR in a year (i.e., CR spots). For country without a response, national capacity estimated based on regional median program capacity multiplied by number of programs in that country.
§CR density refers to the number of incident IHD cases per year per CR spot (i.e., national CR capacity).
||Ranking based on density, or ratio of need (i.e., IHD incidence) to supply (i.e., national CR capacity). Lower numbers reflect more CR spots per IHD patient (i.e., of 86 countries where CR and sufficient information are available such that 1 represents the most spots per IHD patient and 86 is the least spots per patient).
Acronyms: IHD, ischemic heart diseases; CR cardiac rehabilitation; NA, not available; SD, standard deviation; WHO, World Health Organization.
Table 2.
Estimated annual ischemic heart disease incidence (2016) in countries without cardiac rehabilitation and globally, N = 92.
| Country | WHO region | Human Development Index⁎ | IHD incidence† | IHD incidence/100,000† |
|---|---|---|---|---|
| Ukraine | Europe | 0.743 | 519,761 | 1139 |
| Vietnam | Western Pacific | 0.683 | 238,156 | 253 |
| Ethiopia | Africa | 0.448 | 138,477 | 135 |
| Iraq | Eastern Mediterranean | 0.649 | 117,130 | 297 |
| Sudan | Eastern Mediterranean | 0.490 | 111,063 | 282 |
| Myanmar | South-East Asia | 0.556 | 108,283 | 199 |
| Uzbekistan | Europe | 0.701 | 90,959 | 299 |
| Democratic Republic of the Congo | Africa | 0.592 | 82,818 | 104 |
| Yemen | Eastern Mediterranean | 0.485 | 69,006 | 245 |
| Syria | Eastern Mediterranean | 0.536 | 57,355 | 315 |
| North Korea | South-East Asia | NA | 48,117 | 182 |
| Mozambique | Africa | 0.418 | 41,012 | 142 |
| Ghana | Africa | 0.579 | 36,001 | 127 |
| Madagascar | Africa | 0.512 | 32,640 | 131 |
| Cote d'Ivoire | Africa | 0.474 | 31,106 | 135 |
| Azerbaijan | Europe | 0.759 | 28,593 | 291 |
| Cameroon | Africa | 0.518 | 25,761 | 107 |
| Malawi | Africa | 0.476 | 25,374 | 141 |
| Angola | Africa | 0.533 | 24,579 | 95 |
| Haiti | Americas | 0.493 | 23,896 | 215 |
| Niger | Africa | 0.353 | 23,462 | 117 |
| Cambodia | Western Pacific | 0.563 | 22,764 | 143 |
| Jordan | Eastern Mediterranean | 0.741 | 22,639 | 293 |
| Zimbabwe | Africa | 0.516 | 21,766 | 136 |
| Senegal | Africa | 0.494 | 20,843 | 135 |
| Libya | Eastern Mediterranean | 0.716 | 20,254 | 329 |
| Bolivia | Americas | 0.674 | 19,423 | 175 |
| Burkina Faso | Africa | 0.402 | 19,241 | 103 |
| Zambia | Africa | 0.579 | 18,951 | 114 |
| South Sudan | Africa | 0.418 | 17,290 | 127 |
| Mali | Africa | 0.442 | 17,278 | 96 |
| Guinea | Africa | 0.414 | 16,645 | 129 |
| Chad | Africa | 0.396 | 16,436 | 114 |
| Somalia | Eastern Mediterranean | NA | 15,179 | 146 |
| Burundi | Africa | 0.404 | 13,432 | 116 |
| Tajikistan | Europe | 0.627 | 13,029 | 152 |
| Oman | Eastern Mediterranean | 0.796 | 12,703 | 270 |
| Rwanda | Africa | 0.498 | 11,947 | 99 |
| Armenia | Europe | 0.743 | 11,125 | 366 |
| Papua New Guinea | Western Pacific | 0.516 | 11,091 | 141 |
| Laos | Western Pacific | NA | 10,390 | 144 |
| Togo | Africa | 0.487 | 9988 | 135 |
| Albania | Europe | 0.764 | 9490 | 328 |
| Turkmenistan | Europe | 0.691 | 9388 | 171 |
| Sierra Leone | Africa | 0.420 | 9247 | 140 |
| Nicaragua | Americas | 0.645 | 7341 | 119 |
| Central African Republic | Africa | 0.352 | 6831 | 136 |
| Liberia | Africa | NA | 6669 | 144 |
| Congo | Africa | 0.592 | 5921 | 126 |
| Mauritania | Africa | 0.513 | 5612 | 138 |
| Eritrea | Africa | 0.420 | 5386 | 101 |
| Botswana | Africa | 0.698 | 3569 | 155 |
| Namibia | Africa | 0.640 | 3412 | 136 |
| Lesotho | Africa | 0.497 | 2997 | 140 |
| Guinea-Bissau | Africa | 0.424 | 2797 | 147 |
| Gambia | Africa | 0.452 | 2607 | 127 |
| Gabon | Africa | 0.6971 | 2272 | 129 |
| Swaziland | Africa | 0.541 | 1925 | 144 |
| Guyana | Americas | 0.638 | 1814 | 237 |
| Timor-Leste | South-East Asia | 0.605 | 1695 | 146 |
| Fiji | Western Pacific | 0.736 | 1631 | 189 |
| Suriname | Americas | 0.725 | 1468 | 269 |
| Djibouti | Eastern Mediterranean | 0.473 | 1407 | 145 |
| Bhutan | South-East Asia | 0.607 | 1319 | 165 |
| Equatorial Guinea | Africa | 0.592 | 1105 | 132 |
| Bahamas | Americas | 0.792 | 1063 | 268 |
| Comoros | Africa | 0.497 | 1034 | 133 |
| Cape Verde | Africa | NA | 965 | 176 |
| Solomon Islands | Western Pacific | 0.515 | 753 | 126 |
| Maldives | South-East Asia | 0.701 | 625 | 172 |
| Belize | Americas | 0.706 | 596 | 159 |
| Saint Lucia | Americas | 0.735 | 525 | 288 |
| Vanuatu | Western Pacific | 0.597 | 399 | 144 |
| Andorra | Europe | 0.858 | 336 | 425 |
| Samoa | Western Pacific | 0.704 | 299 | 151 |
| Saint Vincent and Grenadines | Americas | 0.722 | 296 | 268 |
| Sao Tome and Principe | Africa | 0.574 | 263 | 133 |
| Seychelles | Africa | 0.782 | 249 | 257 |
| Antigua and Barbuda | Americas | 0.786 | 235 | 256 |
| Dominica | Americas | 0.726 | 209 | 282 |
| Tonga | Western Pacific | 0.721 | 168 | 156 |
| Kiribati | Western Pacific | 0.588 | 162 | 143 |
| Federated States of Micronesia | Western Pacific | 0.638 | 147 | 142 |
| Greenland | Europe | NA | 99 | 200 |
| Marshall Islands | Western Pacific | NA | 98 | 132 |
| Kosovo | Europe | NA | NA | NA |
| Monaco | Europe | NA | NA | NA |
| Nauru | Western Pacific | NA | NA | NA |
| Palau | Western Pacific | 0.788 | NA | NA |
| Palestine | Eastern Mediterranean | 0.684 | NA | NA |
| Saint Kitts and Nevis | Americas | 0.765 | NA | NA |
| Tuvalu | Western Pacific | NA | NA | NA |
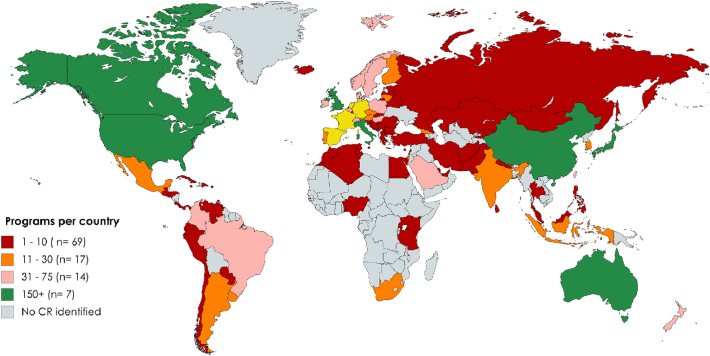
The incidence of CVD (i.e., practice guidelines for most of these diseases recommend CR) in each country [5], to represent the number of patients who would be indicated for CR in a given year (i.e., need), was sought. Estimates from the Global Burden of Disease (GBD) study were used [15], from 2016. Because the CVD grouping included rheumatic heart disease and stroke, to be conservative, ischemic heart disease (IHD) more specifically was selected, as it was the closest diagnostic option to CR-indicated conditions [16]. We created IHD incidence tertiles (Fig. 1). These data were used with the data on availability and capacity collected as per below to compute density.
Fig. 1.
Global availability of cardiac rehabilitation, by age-standardized ischemic heart disease incidence tertile (2016).
Source of incidence estimates: Global Burden of Disease Study [15] IHD, ischemic heart disease; CR, cardiac rehabilitation.
With regard to availability, the following strategies and sources were used to confirm which countries offered any CR: (a) our previously-published review on global availability of CR [7], among other reviews [9], and (b) a search of MEDLINE, EMBASE, and Google Scholar for articles or abstracts on CR. For countries where no CR was in evidence, the authors: (a) searched the internet via Google using the term “cardiac rehabilitation” and country, (b) searched via Google for hospitals within these countries, which were then searched for CR programs, (c) used a snowball sampling strategy via the International Council of Cardiovascular Prevention and Rehabilitation (ICCPR) members and key informants in the field (including European Society of Cardiology national CVD prevention coordinators), as well as (d) attended international conferences of relevant societies to approach experts in the given countries (the latter 2 enabled us to identify programs that may not be advertised in English). Finally, before any country was designated as having no CR, international societies (e.g., International Society of Physical Medicine and Rehabilitation, African Heart Network) were contacted to ascertain whether there were any CR programs in countries where we lacked confirmation of availability.
In countries where CR existed, the total number of programs and contacts to reach those programs for data collection was then sought. First, available CR associations (or broader cardiac society leadership where not available) were contacted. Otherwise, “champions” were identified from the peer-reviewed, or gray literature/internet. Identified leaders were sent an e-mail requesting their collaboration. If there was no “champion” for a given country, the study team directly contacted CR programs that could be identified on the internet or through key informants. Based on the above, the total number of CR programs in each country was collated.
Finally, national champions were asked to circulate a link of the survey to all identified programs, or provide the study team with the email addresses of the programs to survey them directly. Data collection occurred from February 2016–July 2017 via online survey administered through REDCap.
2.2. Sample
The sample was comprised of all CR programs world-wide offering Phase II (i.e., post-acute care discharge) services (including residential programs [17]. Programs that offered: (1) initial assessment, (2) structured exercise, and (3) at least one other strategy to control CV risk factors, were included. All CR programs were contacted in countries with ≤ 350 programs; otherwise, a random non-stratified subsamples of 250 programs were generated electronically (using the simple random sample module SAS institute, Cary, NC) and were contacted.
2.3. Measures
This study focused on four main indicators, namely CR: (1) availability or existence (yes/no; ascertained as described above); (2) program volume, defined as the number of patients served by a program annually, (3) national capacity, or the median number of patients a program could serve annually (as both reported through the survey described below) among the responding programs in a given country, multiplied by the total number of programs in that country (ascertained from champion; Please note for countries where no surveys were completed, national capacity was computed by multiplying the number of programs by regional median program capacity); and (4) density, or national capacity (#3 above) per annual incident IHD case in a country (ascertained from GBD) [15]. The latter was ranked by country.
Development of the survey is described elsewhere [18]; it was pilot-tested in the Arab world and Canada. The final version was translated to Portuguese, Spanish, and traditional Chinese character [19]. The survey assessed annual program volume, capacity (both defined as per the above), and barriers to serving more patients (e.g., referral, human resources; rated on a 5-point Likert scale; and an open-ended item).
Because this was the first study to examine volume worldwide, potential factors associated with volume were selected based on expert opinion of the authors. Potential drivers of volume assessed included: (i) funding source, and the costs per patient, (ii) location of program and proximity to other programs; (iii) type and nature of institution where situated, (iv) healthcare professionals on the CR team, (v) wait times, (vi) number of patients served per session (as well as staff-to-patient ratio and case-mix), (vii) core components and other elements delivered, (viii) dose of CR; (ix) equipment/resources available, and whether patients are monitored during exercise using telemetry, and (x) whether the program offers CR in alternative settings (e.g., home-based, or community-based).
2.4. Statistical Analyses
IBM SPSS version 24 was used for analysis [20], and p < .05 considered statistically significant where exploratory inferential statistics were performed. Descriptive statistics (e.g., frequency with percentage or median with quartiles, as appropriate) were used to characterize CR availability, volumes, capacity, and density, as well as the survey items related to access and barriers. These were described by country, WHO region, and/or IHD incidence tertiles [15].
Herein, data from programs nested within countries is presented. Therefore, clustering of program-level data within countries was taken into consideration in the inferential tests outlined below.
Differences in the CR availability indicators above (dependent variables; i.e., programs per country, program volumes, annual capacity, density) were tested by region and IHD incidence tertile (independent variables) in an exploratory manner via generalized linear mixed models (GLMM), to account for clustering of programs, where country was the random effect. The models were fitted via the Poisson distribution log link function, because the dependent variables were positively skewed. Barriers to broader delivery were tested in the same manner, by WHO region only. Similarly, differences in CR availability (yes/no; dependent variable) were also tested by region via GLMM, but using a binomial distribution with logit link function. For each analysis, the distribution of the residuals was reviewed to consider the model performance.
Finally, potential drivers of volumes were explored using a two-step approach: (a) first in a bivariate manner (using t-tests, analysis of variance or Pearson's correlation as applicable); and where statistically significant, (b) using GLMM, where volume was the dependent variable, and country served as a higher-order variable. A two-step approach was used because multiple potential factors associated with volume were considered as this was exploratory, so by running fewer multivariate models this would minimize type 1 error.
Using “country” as a random effect in the drivers of volume model, the obtained ICC was = (Random effect)/(Random effect + Residual effect)ICC = 1.04/(1.04 + 1.00) = 0.51, i.e. 51.1% of variance in this model is explained by using “country” as random effect. Because volume was positively skewed, the model was fitted via the Poisson distribution log link function.
3. Results
CR was identified to be available in 111/203 countries (54.7%; Table 1). Data were collected in 93 (83.8% country response rate) countries (see [19]), from which 1082 (32.1% program response; rate by country reported elsewhere) surveys were initiated [19]. A random sub-sample of programs was surveyed in the United States only, and a non-random convenience sub-sample (due to champion preference) in Japan, Scotland (1–2 programs per health board/region) and Austria.
3.1. Availability
There were 92 countries in the world that lack any CR (Table 2), of which 12 (6.1% of the 196 countries with 2016 incidence estimates) were estimated to have high IHD incidence (Fig. 1) [15].
Availability of any CR in countries by WHO region was: 46/57 (80.7%) countries in Europe, 28/40 (70.0%) countries in Americas, 6/11 (54.5%) countries in South East Asia, 12/22 (54.5%) countries in the Eastern Mediterranean Region (EMR), 11/26 (42.7%) countries in the Western Pacific, and 8/47 (17.0%) countries in the African region (p < .001).
The first CR program opened in 1944 in Mexico (Table 1). Soon after, programs opened in Eastern Europe (Germany [1950], Croatia [1957], and Bulgaria [1958]). More than half of the participating programs (n = 565; 60.5%), in 30 countries (N = 89; 34.1%), opened since 2000.
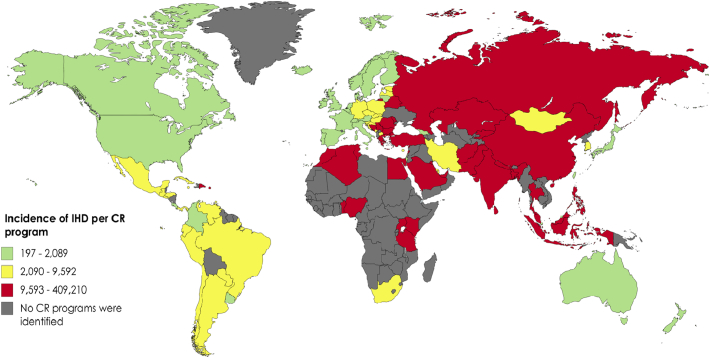
There were 5753 CR programs in the world (counting all programs in the United States).
The median number of programs per country was one; this ranged from a low of zero in the African and Western Pacific regions, to a high of four in Europe (shown in countries with CR in Table 1 and Fig. 2; p < .001). There was a median of zero programs/country in countries with the lowest IHD incidence, one program in countries with moderate IHD incidence, and six programs in countries with the highest IHD incidence (p < .001; again, tertiles shown in Fig. 1).
Fig. 2.
Total number of cardiac rehabilitation programs per country.
3.2. Volume and Its Drivers
Median program volumes ranged from a low around 20 patients/program in several countries (e.g., Guatemala, Honduras, Kenya, Egypt, and Greece), to over 1000 in others (e.g., Scotland, Romania, Serbia, Argentina, Bulgaria, Nepal; Table 1) per year. They were lowest in Africa, and highest in Europe (p < .001). The median program volume was 35 patients in countries with the lowest IHD incidence, 200 patients in countries with moderate IHD incidence, and 250 patients in countries with the highest IHD incidence (p < .001).
In multivariate models, program volume was statistically significantly greater where there were other programs in close proximity, programs were located in hospitals offering advanced cardiac procedures, there was systematic referral in the associated hospital, programs were funded by a combination of private and public sources, programs offered alternative CR models/settings (including residential programs), there was a cardiologist on the CR team, and patients were offered an individual consult with a physician during the program, programs served patients at high-risk of cardiovascular disease (primary prevention), the number of patients served per session and per staff member was larger, and programs offered smoking cessation services. Volume was statistically significantly lower where patients had longer wait times, and programs offered more core components (Table 3).
Table 3.
Drivers of annual cardiac rehabilitation program volume.
| Factor | n (%)/mean ± SD | Annual program volume (mean ± SD) | Univariate test Statistic | Univariate p |
GLMM OR° |
95% CI |
|---|---|---|---|---|---|---|
| CR Location | F = 0.45 | 0.636 | ||||
| Urban | 774 (71.6%) | 503.9 ± 928.0 | – | – | ||
| Suburban | 155 (14.3%) | 509.9 ± 814.5 | – | – | ||
| Rural | 134 (12.4%) | 410.7 ± 550.5 | – | – | ||
| Other CR program within 20 km | t = 2.57 | 0.010 | ||||
| Yes | 495 (45.7%) | 574.7 ± 1104.5 | 1.20 | 1.19–1.21 | ||
| No | 516 (47.7%) | 420.7 ± 629.0 | – | |||
| Located in referral center/tertiary facility/academic hospital | t = 1.40 | 0.162 | ||||
| Yes | 484 (44.7%) | 549.3 ± 1001.1 | – | – | – | |
| No | 566 (52.3%) | 460.1 ± 809.4 | ||||
| Located in hospital offering coronary bypass surgery | t = 2.68 | 0.008 | ||||
| Yes | 441 (40.8%) | 601.9 ± 1138.5 | 1.25 | 1.24–1.26 | ||
| No | 612 (56.6%) | 422.7 ± 647.6 | – | |||
| Systematic referral in associated hospital | t = 2.92 | 0.017 | 1.36 | 1.35–1.38 | ||
| Yes | 647 (59.8%) | 586.7 ± 856.1 | – | |||
| No | 182 (16.8%) | 439.3 ± 1088.1 | ||||
| CR funding source* | F = 12.30 | < 0.001 | ||||
| Hybrid | 268 (24.8%) | 695.8 ± 1276.1 | – | |||
| Public | 592 (54.7%) | 455.0 ± 619.8 | 0.83 | 0.82–0.84 | ||
| Private | 202 (18.7%) | 344.4 ± 840.7 | 0.92 | 0.91–0.93 | ||
| Any patient funding | ||||||
| Yes | 396 (36.6%) | 535.9 ± 1188.5 | t = 0.87 | 0.387 | – | – |
| No | 668 (61.7%) | 472.4 ± 631.4 | ||||
| Estimated program cost to treat one patient (PPP 2016 USD) | $1560.2 ± 1686.3 | – | r = − 0.01 | 0.817 | – | – |
| Program offers alternative CR models/settings | t = − 2.58 | 0.010 | ||||
| Yes | 285 (26.3%) | 584.5 ± 720.7 | 1.05 | 1.04–1.06 | ||
| No | 630 (58.2%) | 478.6 ± 1017.9 | – | |||
| Residential program | t = 2.16 | 0.0.038 | ||||
| Yes | 24 (2.2%) | 1880.3 ± 2364.5 | 2.41 | 0.39–15.12 | ||
| No | 1058 (97.8%) | 618.3 ± 716.2 | – | |||
| Total number staff on CR team† | 5.0 ± 3.2 | – | r = 0.03 | 0.375 | – | – |
| Cardiologist on the CR team | t = 3.24 | 0.001 | ||||
| Yes | 721 (66.6%) | 543.8 ± 1004.5 | 1.16 | 1.15–1.18 | ||
| No | 205 (18.9%) | 359.5 ± 503.7 | – | |||
| Individual consult with physician | t = 2.18 | 0.029 | ||||
| Yes | 697 (64.4%) | 534.5 ± 1017.7 | 1.33 | 1.31–1.36 | ||
| No | 298 (22.9%) | 408.8 ± 529.9 | – | |||
| Wait times from inpatient discharge to initiate CR (weeks) | 3.5 ± 3.6 | – | r = − 0.86 | 0.015 | 0.91 | 0.90–0.92 |
| Program serves heart failure, transplant and/or VAD patients (i.e., higher-risk/case-mix) | t = 1.49 | 0.129 | ||||
| - | - | |||||
| Yes | 793 (73.3%) | 521.0 ± 911.3 | ||||
| No | 60 (5.5%) | 324.4 ± 491.2 | ||||
| Program serves patients at high-risk of cardiovascular disease (primary prevention) | t = 2.77 | 0.006 | ||||
| Yes | 493 (45.6%) | 579.3 ± 1034.7 | 1.32 | 1.30–1.33 | ||
| No | 360 (33.3%) | 405.4 ± 616.5 | – | |||
| Number of patients served per session | 9.1 ± 5.9 | – | r = 0.31 | < 0.001 | 3.04 | 2.98–3.11 |
| Number of patients served per 1 staff | 4.8 ± 8.0 | – | r = − 0.08 | 0.044 | 0.99 | 0.98–0.99 |
| Supervised dose (hours) ‡ | 35.2 ± 50.9 | – | r = 0.03 | 0.403 | – | – |
| Number of core components offered§ | 7.5 ± 1.7 | – | r = − 0.09 | 0.010 | 0.93 | 0.94–0.95 |
| Risk factor management | t = 1.48 | 0.140 | ||||
| Yes | 928 (85.8%) | 511.1 ± 931.7 | – | – | ||
| No | 17 (1.6%) | 113.0 ± 144.1 | ||||
| Exercise training | t = 0.036 | 0.971 | ||||
| Yes | 898 (83.0%) | 502.6 ± 939.7 | – | – | ||
| No | 54 (5.0%) | 508.2 ± 536.4 | ||||
| Patient Education | t = 1.19 | 0.236 | ||||
| Yes | 860 (79.5%) | 518.5 ± 946.4 | – | – | ||
| No | 28 (2.2%) | 267.0 ± 315.6 | ||||
| Psychological counseling/stress management | t = 1.89 | 0.060 | ||||
| Yes | 651 (60.2%) | 521.9 ± 956.3 | – | – | ||
| No | 297 (27.4%) | 303.2 ± 417.6 | ||||
| Smoking cessation services | t = 1.91 | 0.023 | ||||
| Yes | 692 (64.0%) | 540.7 ± 991.8 | 1.07 | 1.05–1.08 | ||
| No | 252 (23.3%) | 394.0 ± 681.8 | – | |||
| Women-only classes | t = − 2.32 | 0.023 | ||||
| Yes | 110 (10.1%) | 868.6 ± 1774.6 | 1.01 | 1.00–1.03 | ||
| No | 820 (75.8%) | 446.4 ± 706.3 | – | |||
| Total equipment || | 9.3 ± 4.4 | – | r = 0.05 | 0.152 | – | – |
| Telemetry during exercise | t = − 0.80 | 0.421 | ||||
| Yes | 397 (36.7%) | 508.7 ± 982.6 | – | – | ||
| No | 513 (47.4%) | 510.5 ± 773.3 |
*Private sources included healthcare insurance or patients; public included government; or a hybrid source. There was no statistically significant difference between privately and publicly funded program in the volume of patients served, but there was between hybrid and private with more patients for hybrid.
†i.e. cardiologist, physiatrist, sports medicine physician, nurse/practitioner, physiotherapist, exercise specialist/kinesiologist, psychiatrist/psychologist/social worker, dietitian, pharmacist, community health worker, administrative assistant/secretary, other; part-time staff were counted as 0.5.
‡Sessions/week × # weeks in program × # minutes per session.
§Of ten; i.e., initial assessment, risk stratification, supervised exercise, patient education, risk factor management, nutrition counseling, stress management, smoking cessation, prescription of medication, and communication with a primary healthcare provider.
|| e.g., treadmills, cycle ergometers, supplies for cardiovascular risk assessment.
–Not applicable.
°Note that odds ratios can be misleading, and therefore the practical importance of the value should not be over-interpreted.
Acronyms: CR, cardiac rehabilitation; SD, standard deviation; GLMM, generalized linear mixed model; OR, odds ratio; CI, confidence interval; VAD, ventricular assist device; USD, United States dollar; PPP, purchase power parity.
Abbreviations: km, kilometers; Ref, reference.
Note: Due to missing data, percentages are computed where the denominator is the number of valid responses from responding programs.
Globally, there was ≥ 1 program that offered home-based CR in 38 [40.9%] of the 93 countries that offer CR. There were 152 (12.4%) programs offering home-based programs, where an estimated 21.4 ± 22.8% of the programs' total patients were served each year (median of 10.0%; Q1-Q3: 5.0–30.0%). Only 108 (10.0%) programs offered community-based (in 26/93 [28.0%] countries there was ≥ 1 program that offered community-based), where 38.1 ± 32.3% of their patients were served (median of 27.5%; Q1–Q3: 10.0–61.3%). Eighty-nine (8.1%) programs offered a hybrid model (i.e., supervised sessions transitioning to other setting). Eighty-eight (57.9%) programs offering home-based models reported their program had sufficient home-based capacity to meet patient demand for that model, while the rest of the programs (n = 64; 42.1%) reported capacity constraints, such as insufficient human resources (n = 42, 65.6%) and lack of funding (n = 31, 48.4%).
3.3. Capacity
Annual program capacity was lowest in Africa, and highest in Europe (p < .01; Table 1). The median program capacity was 200 patients in countries with the lowest IHD incidence, as well as in countries with moderate IHD incidence, and 250 patients in countries with the highest IHD incidence. On average, program volumes were 82.8% of annual capacity.
Median annual national capacity was lowest in Africa and greatest in the Western Pacific followed by Europe (Table 1; p < .001). Median annual national capacity across all countries (i.e., considering zero for countries without CR) was zero for Africa, and the Western Pacific, 150 for EMR, 200 for South-East Asia, 200 for the Americas, and 2300 for Europe. Median national capacity was zero in countries with the lowest IHD incidence, zero in countries with moderate IHD incidence, and 400 in countries with the highest IHD incidence. Global capacity was 1,655,083 patients/year.
3.4. CR Density
North America, Australia, Japan, and a few countries in Western Europe had the fewest estimated incident IHD patients/program/year (197–2089 patients/program; Fig. 3).
Fig. 3.
Ischemic heart disease incidence by number of cardiac rehabilitation programs in a country.
IHD, ischemic heart disease; CR, cardiac rehabilitation.
CR density in countries with CR ranged from one CR spot per 0.5 incident IHD patient/year (there were three countries with a density less than one suggesting they could treat other guideline-indicated patients as well) in Bermuda to per 4480 patients in Nigeria (Table 1; which should not be over-interpreted as there was only one program in these two countries) [15]. IHD incidence in countries without CR is shown in Table 2, reflecting unmet CR need.
Density was poorest in Africa, and best in the Western Pacific (in countries with CR; Table 1; p < .001). Median annual national density including countries without CR was zero spots in Africa and the Western Pacific, one spot per 22 patients in South-East Asia, per 11 in the EMR, per five in Europe, and per four patients in the Americas.
3.5. Causes
Globally, lack of financial resources was the most strongly rated barrier to greater CR delivery, followed by lack of patient referral, then lack of human resources (Table 4). Lack of patient referral was rated as a statistically significantly greater barrier in the Americas and EMR than in Europe (p < .05 for each); no other differences were observed.
Table 4.
Barriers to Broader Cardiac Rehabilitation Delivery, by Country with Cardiac Rehabilitation & WHO Regions [32], N = 111.
| Mean ± standard deviation* | number of CR programs | Lack of patient referral | Lack of equipment | Lack of space | Lack of human resources | Lack of financial resources |
|---|---|---|---|---|---|---|
| Africa | ||||||
| Algeria | 1 | – | – | – | – | – |
| Kenya | 3 | 5.0 ± 0.0 | 2.0 ± 0.0 | 2.0 ± 0.0 | 4.0 ± 0.0 | 2.0 ± 0.0 |
| Mauritius | 1 | 5.0 ± 0.0 | 4.0 ± 0.0 | 5.0 ± 0.0 | 4.0 ± 0.0 | 4.0 ± 0.0 |
| Nigeria | 1 | 5.0 ± 0.00 | 5.0 ± 0.0 | 5.0 ± 0.0 | 5.0 ± 0.0 | 5.0 ± 0.0 |
| South Africa | 23 | 4.4 ± 1.0 | 1.8 ± 0.9 | 1.8 ± 1.1 | 2.0 ± 1.3 | 3.5 ± 1.7 |
| Regional Mean | 5.8 | 4.5 ± 0.9 | 2.1 ± 1.3 | 2.2 ± 1.5 | 2.4 ± 1.5 | 3.5 ± 1.6 |
| Americas | ||||||
| Argentina | 23 | 5.0 ± 0.0 | 3.0 ± 1.7 | 1.7 ± 1.2 | 3.3 ± 1.2 | 3.7 ± 0.6 |
| Barbados | 1 | 5.0 ± 0.0 | 2.0 ± 0.0 | 2.0 ± 0.0 | 5.0 ± 0.0 | 4.0 ± 0.0 |
| Bermuda | 1 | 2.0 ± 0.00 | 2.0 ± 0.0 | 3.0 ± 0.0 | 5.0 ± 0.0 | 5.0 ± 0.0 |
| Brazil | 75 | 4.2 ± 1.2 | 2.4 ± 1.5 | 2.5 ± 1.6 | 2.9 ± 1.7 | 3.4 ± 1.5 |
| Canada | 170 | 2.5 ± 1.5 | 2.7 ± 1.3 | 3.2 ± 1.4 | 3.8 ± 1.4 | 4.3 ± 1.2 |
| Chile | 10 | 5.0 ± 0.0 | 4.0 ± 0.0 | 3.0 ± 0.0 | 3.0 ± 0.0 | 3.0 ± 0.0 |
| Colombia | 50 | 3.9 ± 1.5 | 2.1 ± 1.3 | 2.4 ± 1.3 | 2.3 ± 1.4 | 2.9 ± 1.4 |
| Costa Rica | 6 | 3.5 ± 1.6 | 2.3 ± 2.1 | 2.5 ± 2.0 | 3.0 ± 1.7 | 3.0 ± 1.7 |
| Cuba | 8 | 2.0 ± 1.3 | 3.4 ± 1.5 | 3.5 ± 1.9 | 2.3 ± 1.5 | 2.4 ± 1.5 |
| Curacao | 2 | 4.0 ± 0.0 | 2.0 ± 0.0 | 4.0 ± 0.0 | 4.0 ± 0.0 | 5.0 ± 0.0 |
| Dominican Republic | 2 | 5.0 ± 0.0 | 1.0 ± 0.0 | 1.0 ± 0.0 | 4.0 ± 0.0 | 2.0 ± 0.0 |
| Ecuador | 5 | 5.0 ± 0.0 | 1.5 ± 0.7 | 1.0 ± 0.0 | 1.5 ± 0.7 | 1.5 ± 0.7 |
| Guatemala | 2 | 5.0 ± 0.0 | 3.0 ± 1.4 | 3.0 ± 1.4 | 3.5 ± 2.1 | 2.5 ± 0.7 |
| Honduras | 2 | 3.0 ± 0.0 | 2.0 ± 0.0 | 3.0 ± 0.0 | 3.0 ± 0.0 | 5.0 ± 0.0 |
| Jamaica | 3 | 5.0 ± 0.0 | 2.0 ± 0.0 | 1.0 ± 0.0 | 2.0 ± 0.0 | 1.0 ± 0.0 |
| Mexico | 24 | 4.9 ± 0.3 | 1.9 ± 1.5 | 3.1 ± 1.5 | 3.1 ± 1.5 | 3.9 ± 1.4 |
| Panama | 1 | 5.0 ± 0.0 | 2.0 ± 0.0 | 2.0 ± 0.0 | 4.0 ± 0.0 | 4.0 ± 0.0 |
| Paraguay | 3 | 5.0 ± 0.0 | 2.0 ± 0.0 | 3.3 ± 1.2 | 4.0 ± 0.0 | 3.7 ± 1.5 |
| Peru | 10 | 3.4 ± 1.5 | 3.7 ± 1.5 | 3.3 ± 1.8 | 4.0 ± 1.5 | 4.1 ± 1.2 |
| United States of America | 2632 | 3.5 ± 1.4 | 2.6 ± 1.4 | 3.0 ± 1.4 | 2.9 ± 1.2 | 3.2 ± 1.5 |
| Uruguay | 12 | 4.3 ± 1.5 | 1.5 ± 0.6 | 1.6 ± 0.9 | 1.3 ± 0.5 | 4.5 ± 0.6 |
| Venezuela | 9 | 3.8 ± 1.8 | 3.6 ± 1.8 | 1.9 ± 1.5 | 3.1 ± 1.5 | 4.4 ± 1.1 |
| Regional Mean | 138.7 | 3.5 ± 1.5 | 2.5 ± 1.5 | 2.8 ± 1.5 | 3.1 ± 1.5 | 3.5 ± 1.5 |
| Eastern Mediterranean | ||||||
| Afghanistan | 1 | 4.0 ± 0.0 | 5.0 ± 0.0 | 4.0 ± 0.0 | 5.0 ± 0.0 | 5.0 ± 0.0 |
| Bahrain | 1 | 5.0 ± 0.0 | 2.0 ± 0.0 | 2.0 ± 0.0 | 5.0 ± 0.0 | 3.0 ± 0.0 |
| Egypt | 2 | 5.0 ± 0.0 | 4.0 ± 0.0 | 3.0 ± 0.0 | 4.0 ± 0.0 | 5.0 ± 0.0 |
| Iran | 34 | 4.8 ± 0.5 | 2.3 ± 1.3 | 2.5 ± 1.4 | 2.8 ± 1.5 | 4.0 ± 1.2 |
| Lebanon | 1 | 4.0 ± 0.0 | 1.0 ± 0.0 | 2.0 ± 0.0 | 2.0 ± 0.0 | 5.0 ± 0.0 |
| Morocco | 1 | – | – | – | – | – |
| Pakistan | 4 | 5.0 ± 0.0 | 2.5 ± 2.1 | 3.0 ± 1.4 | 3.5 ± 0.7 | 4.5 ± 0.7 |
| Qatar | 1 | 1.0 ± 0.0 | 3.0 ± 0.0 | 5.0 ± 0.0 | 4.0 ± 0.0 | 4.0 ± 0.0 |
| Tunisia | 1 | 5.0 ± 0.0 | 1.0 ± 0.0 | 1.0 ± 0.0 | 1.0 ± 0.0 | 2.0 ± 0.0 |
| Regional Mean | 5.1 | 4.6 ± 0.9 | 2.4 ± 1.4 | 2.6 ± 1.4 | 3.1 ± 1.4 | 4.1 ± 1.1 |
| Europe | ||||||
| Austria | 26 | 2.4 ± 1.9 | 1.3 ± 0.5 | 1.3 ± 0.5 | 2.0 ± 1.4 | 1.8 ± 1.5 |
| Belarus | 5 | 3.0 ± 0.0 | 1.0 ± 0.0 | 1.0 ± 0.0 | 2.0 ± 0.0 | 2.0 ± 0.0 |
| Belgium | 48 | 4.0 ± 1.1 | 2.1 ± 1.4 | 2.1 ± 1.1 | 2.4 ± 1.4 | 2.9 ± 1.5 |
| Bosnia and Herzegovina | 1 | 1.0 ± 0.0 | 4.0 ± 0.0 | 1.0 ± 0.0 | 4.0 ± 0.0 | 1.0 ± 0.0 |
| Bulgaria | 1 | 2.0 ± 0.0 | 2.0 ± 0.0 | 1.0 ± 0.0 | 4.0 ± 0.0 | 5.0 ± 0.0 |
| Croatia | 3 | 3.7 ± 0.6 | 2.7 ± 1.5 | 2.7 ± 1.5 | 3.0 ± 1.0 | 3.7 ± 1.5 |
| Czech Republic | 15 | 3.8 ± 1.3 | 2.4 ± 1.5 | 3.0 ± 1.9 | 3.4 ± 1.3 | 2.6 ± 1.3 |
| Denmark | 35 | 3.6 ± 0.5 | 2.2 ± 1.2 | 2.7 ± 1.1 | 3.4 ± 1.5 | 3.4 ± 1.8 |
| England | 266 | 2.0 ± 1.3 | 2.1 ± 1.1 | 2.9 ± 1.4 | 3.3 ± 1.3 | 3.3 ± 1.3 |
| Estonia | 2 | 2.0 ± 1.4 | 4.0 ± 1.4 | 5.0 ± 0.0 | 5.0 ± 0.0 | 3.0 ± 0.0 |
| Finland | 25 | 3.8 ± 1.2 | 1.4 ± 0.7 | 2.2 ± 1.5 | 2.8 ± 1.3 | 2.9 ± 1.3 |
| France | 130 | 3.6 ± 1.6 | 2.4 ± 1.5 | 3.3 ± 1.6 | 3.5 ± 1.5 | 2.8 ± 1.1 |
| Georgia | 17 | 2.9 ± 1.3 | 1.1 ± 0.4 | 2.1 ± 1.6 | 2.1 ± 1.0 | 4.0 ± 1.4 |
| Germany | 120 | 4.0 ± 1.3 | 1.6 ± 0.9 | 2.2 ± 1.4 | 2.4 ± 1.3 | 2.9 ± 1.6 |
| Greece | 4 | 4.3 ± 1.5 | 1.0 ± 0.0 | 1.3 ± 0.5 | 1.8 ± 1.5 | 4.8 ± 0.5 |
| Hungary | 33 | 4.2 ± 1.3 | 2.8 ± 1.3 | 2.6 ± 1.2 | 3.1 ± 1.4 | 3.3 ± 1.4 |
| Iceland | 4 | 1.5 ± 0.6 | 2.0 ± 1.4 | 1.3 ± 0.5 | 1.8 ± 1.0 | 4.5 ± 0.6 |
| Ireland | 37 | 2.6 ± 1.1 | 1.8 ± 0.8 | 3.4 ± 1.8 | 3.8 ± 0.8 | 3.0 ± 0.7 |
| Israel | 22 | 2.8 ± 1.8 | 1.4 ± 0.6 | 2.4 ± 1.7 | 3.0 ± 1.9 | 2.8 ± 1.6 |
| Italy | 221 | 3.5 ± 1.5 | 2.6 ± 1.4 | 2.7 ± 1.4 | 3.3 ± 1.5 | 3.6 ± 1.3 |
| Kazakhstan | 1 | 0 | 3.0 ± 0.0 | 2.0 ± 0.0 | 3.0 ± 0.0 | 4.0 ± 0.0 |
| Latvia | 2 | 5.0 ± 0.0 | 4.0 ± 0.0 | 4.0 ± 0.0 | 3.0 ± 0.0 | 5.0 ± 0.0 |
| Lithuania | 25 | 2.6 ± 1.0 | 2.4 ± 1.1 | 2.3 ± 1.1 | 2.9 ± 1.2 | 4.6 ± 0.7 |
| Republic of Northern Macedonia | 1 | 4.0 ± 0.0 | 3.0 ± 0.0 | 1.0 ± 0.0 | 1.0 ± 0.0 | 5.0 ± 0.0 |
| Malta | 1 | 5.0 ± 0.0 | 5.0 ± 0.0 | 5.0 ± 0.00 | 5.0 ± 0.00 | 5.0 ± 0.0 |
| Moldova | 1 | 4.0 ± 0.0 | 4.0 ± 0.0 | 4.0 ± 0.0 | 4.0 ± 0.0 | 4.0 ± 0.0 |
| Netherlands | 90 | 2.1 ± 1.4 | 1.6 ± 1.2 | 2.1 ± 1.5 | 2.4 ± 1.3 | 2.7 ± 1.6 |
| Northern Ireland | 13 | 2.1 ± 1.5 | 2.3 ± 1.5 | 3.2 ± 1.6 | 4.6 ± 1.0 | 4.7 ± 0.9 |
| Poland | 56 | 3.0 ± 1.4 | 2.0 ± 1.3 | 2.9 ± 1.4 | 2.7 ± 1.3 | 3.6 ± 1.4 |
| Portugal | 23 | 4.2 ± 1.3 | 3.1 ± 1.4 | 3.5 ± 1.4 | 3.6 ± 1.5 | 4.6 ± 0.9 |
| Romania | 3 | 4.5 ± 0.7 | 1.5 ± 0.7 | 1.5 ± 0.7 | 2.5 ± 2.1 | 3.0 ± 2.8 |
| Russia | 3 | 4.0 ± 0.0 | 4.0 ± 0.0 | 4.0 ± 0.0 | 4.0 ± 0.0 | 4.0 ± 0.0 |
| Scotland | 69 | 1.9 ± 1.4 | 1.6 ± 0.8 | 2.1 ± 1.1 | 2.8 ± 1.3 | 2.6 ± 1.3 |
| Serbia | 2 | 3.0 ± 0.0 | 2.0 ± 1.4 | 2.5 ± 0.7 | 2.5 ± 0.7 | 3.5 ± 2.1 |
| Slovak Republic | 7 | 3.0 ± 0.0 | 2.0 ± 0.0 | 2.0 ± 0.0 | 2.0 ± 0.0 | 5.0 ± 0.0 |
| Slovenia | 2 | 4.5 ± 0.7 | 2.0 ± 1.4 | 2.5 ± 2.1 | 3.0 ± 1.4 | 3.5 ± 0.7 |
| Spain | 87 | 3.2 ± 1.4 | 3.1 ± 1.4 | 3.2 ± 1.4 | 3.7 ± 1.4 | 3.7 ± 1.4 |
| Sweden | 69 | 1.0 ± 0.0 | 1.0 ± 0.0 | 1.0 ± 0.0 | 3.0 ± 0.0 | 3.0 ± 0.0 |
| Switzerland | 51 | 2.8 ± 1.5 | 1.0 ± 0.0 | 1.0 ± 0.0 | 1.0 ± 0.0 | 1.3 ± 0.5 |
| Turkey | 10 | 4.5 ± 1.4 | 2.4 ± 1.5 | 2.4 ± 1.1 | 3.5 ± 1.2 | 2.4 ± 1.3 |
| Wales | 17 | 2.2 ± 1.4 | 2.3 ± 1.2 | 3.6 ± 1.6 | 4.7 ± 0.6 | 4.6 ± 0.6 |
| Regional Mean | 37.8 | 3.1 ± 1.5 | 2.3 ± 1.3 | 2.7 ± 1.4 | 3.2 ± 1.4 | 3.4 ± 1.4 |
| South-East Asia | ||||||
| Bangladesh | 1 | 5.0 ± 0.0 | 2.0 ± 0.0 | 4.0 ± 0.0 | 5.0 ± 0.0 | 5.0 ± 0.0 |
| India | 23 | 3.9 ± 1.4 | 2.3 ± 1.4 | 2.3 ± 1.4 | 2.4 ± 1.6 | 3.2 ± 1.8 |
| Indonesia | 13 | 3.5 ± 1.7 | 2.9 ± 1.5 | 2.9 ± 1.7 | 2.8 ± 1.6 | 3.0 ± 1.4 |
| Nepal | 1 | 4.0 ± 0.0 | 4.0 ± 0.0 | 5.0 ± 0.0 | 4.0 ± 0.0 | 5.0 ± 0.0 |
| Sri Lanka | 4 | 1.5 ± 0.7 | 3.5 ± 2.1 | 3.0 ± 1.4 | 3.5 ± 2.1 | 1.5 ± 0.7 |
| Regional Mean | 8.4 | 3.7 ± 1.5 | 2.6 ± 1.4 | 2.7 ± 1.4 | 2.7 ± 1.6 | 3.1 ± 1.6 |
| Western Pacific | ||||||
| Australia | 314 | 3.4 ± 1.4 | 2.5 ± 1.3 | 3.1 ± 1.4 | 3.5 ± 1.5 | 3.5 ± 1.4 |
| Brunei | 2 | 4.5 ± 0.7 | 2.5 ± 2.1 | 3.0 ± 2.8 | 3.0 ± 2.8 | 2.0 ± 1.4 |
| China | 216 | 3.1 ± 1.4 | 2.7 ± 1.4 | 3.1 ± 1.5 | 3.3 ± 1.3 | 3.9 ± 1.4 |
| Japan | 325 | 3.0 ± 1.3 | 2.7 ± 1.6 | 3.4 ± 1.4 | 4.3 ± 0.9 | 3.1 ± 1.1 |
| Malaysia | 6 | 3.7 ± 1.5 | 2.7 ± 2.1 | 3.0 ± 1.7 | 3.0 ± 1.7 | 3.3 ± 1.5 |
| Mongolia | 1 | 4.0 ± 0.0 | 4.0 ± 0.0 | 4.0 ± 0.0 | 5.0 ± 0.0 | 5.0 ± 0.0 |
| New Zealand | 43 | 2.9 ± 1.4 | 2.9 ± 1.4 | 3.0 ± 1.6 | 3.4 ± 1.2 | 3.8 ± 1.3 |
| Philippines | 10 | 4.3 ± 0.5 | 3.0 ± 1.2 | 3.6 ± 1.7 | 3.2 ± 1.1 | 3.8 ± 1.3 |
| Singapore | 7 | 4.4 ± 0.5 | 2.0 ± 1.4 | 2.6 ± 1.7 | 4.1 ± 1.1 | 3.4 ± 1.1 |
| South Korea | 17 | 3.1 ± 1.3 | 1.4 ± 0.5 | 1.8 ± 1.1 | 2.1 ± 0.9 | 3.8 ± 1.3 |
| Taiwan | 35 | 3.1 ± 1.4 | 2.6 ± 1.5 | 2.9 ± 1.3 | 3.2 ± 1.4 | 2.4 ± 1.3 |
| Regional Mean | 88.7 | 3.3 ± 1.4 | 2.6 ± 1.4 | 3.0 ± 1.5 | 3.4 ± 1.4 | 3.6 ± 1.4 |
| Global Mean | 61.2 | 3.3 ± 1.5 | 2.4 ± 1.4 | 2.8 ± 1.5 | 3.2 ± 1.4 | 3.5 ± 1.4 |
*Scores range from 1 (this is definitely not an issue) to 5 (this is a major issue).
Acronyms: WHO, World Health Organization; FYR, Former Yugoslav Republic.
Finally, respondents were asked to list any other barriers, and these included: lack of transport, parking and distance for patients (n = 95, 30.8%), lack of reimbursement/coverage (n = 47, 15.3%), lack of patient knowledge or awareness (n = 36, 11.7%), patient return-to-work (n = 28, 9.1%), lack physician and healthcare administrator awareness (n = 26, 8.4%), perceived lack of patient motivation (n = 3.9%), lack of program capacity (n = 9, 2.9%), and lack of trained personnel (n = 7, 2.3%).
4. Discussion
Despite the WHO Global Action Plan 2013–2020 for the prevention of non-communicable diseases recognizing the important role of CR in stemming the epidemic of CVD [21], for the first time, it has been established that CR is available in only half of the countries of the world. This is disheartening given that CVD is the leading cause of death globally [1], and participation is associated with 20% lower cardiovascular mortality [4]. Almost 19 million more CR spots would be needed to treat all incident IHD patients/year [15], and this does not include heart failure [22], among other patient groups indicated for CR [5].Clearly, millions of patient deaths could be prevented around the world if CR programs were implemented [23], [24], with disproportionately more benefit to be gained in some regions than others. Notably, the Africa region, where CVD mortality is expected to increase more than any other WHO region in the next decade had the lowest CR availability [25], capacity and density (with 1,345,695 more spots needed to treat all incident IHD cases annually). In the countries with CR, one-third has only one program, and another half has ≤ 5 programs.
Where there is the most pressing need (i.e., high IHD incidence and low resources, hence high mortality rates and lack of access to cardiac care), CR is often non-existent. For example, Ukraine, with the highest estimated IHD incidence of 519,761 [15], does not have any CR. Similarly, Vietnam and Ethiopia do not have CR, despite having 238,156 and 138,477 incident IHD cases annually, respectively [15]. Bangladesh, with its estimated 409,210 incident IHD cases has only one program; the same situation exists in Nigeria, with its estimated 223,994 incident IHD cases.
The number of patients served per program was shown for the first time (only previously reported in South America where, consistent with the data herein, a median of 180 patients were served per program) [12], and was surprisingly low. Programs were not quite running at full capacity, but this is likely explained by insufficient referral. Some potentially-modifiable factors associated with greater program volumes were offering alternative models (e.g., home-based CR) and having a mix of private and public program funding sources. We must advocate for governments to invest in CR and enact policies promoting insurance company reimbursement, and we must support CR programs to deliver services outside major clinical centers so we can reach the vast number of patients in need. Some guidance on CR delivery in alternative settings in low-resource countries is available [26], [27]. Indeed in the Americas and Europe where availability and capacity are greatest, there was more often hybrid funding and more programs offered alternative models (data not shown).
The fact that programs served more patients where there were other programs in close proximity, when they were situated in an institution offering advanced cardiac procedures and with systematic inpatient referral, with a cardiologist on staff and where they served more patients per session and per staff member likely reflects the fact that programs at major academic centers are generally in urban centers and larger, and hence have higher volumes. The fact that residential programs, those serving high-risk primary prevention patients, and those where patients received an individual consult with a physician again is somewhat expected, but it is not recommended that programs pursue these avenues to increase reach, as they may be cost-prohibitive. It was disconcerting to find that programs offering more core components served fewer patients, as we do want to ensure reach to all patients in need, while maintaining quality and minimum standards (although higher-volume programs were more often providing smoking cessation services which is encouraging). Research is needed to understand how countries with the greatest capacity have achieved their heights, including the role of session volume, i.e., number of patients per session; while maintaining safety, so that it can be replicated elsewhere.
4.1. Policy Implications
There is grossly insufficient CR availability and capacity to meet global service needs. This problem must be addressed through initiation of new CR programs and increasing capacity of existing programs (this is a key finding of this work as program volumes were surprisingly low in most instances). This requires financial resources, which was the most commonly-reported barrier to broader provision of CR in this study, as well as others [9], [28]. Affordable models of CR delivery should be implemented given the need in low and middle-income countries [27], [29]. Offering alternative models such as home-based and community-based programs could increase capacity of existing CR programs. Information and communications technology should be exploited to increase the number of patients each program can treat, while maintaining program quality and safety [30]. It is essential for CR associations and other international societies to advocate for CR implementation and reimbursement; advocacy tools are available from the ICCPR [28]. This association also offers a certification program for healthcare professionals, which could address the reported barrier of lack of human resources to deliver CR [31].
4.2. Limitations
There are some weaknesses of study methodology, primarily related to generalizability and measurement. First, some programs may not have been identified, especially in countries where no society or champion was identified. Therefore, availability, capacity and density could be under-estimated. Second, though a high response rate at the country-level of 85% was achieved, response rates among programs within countries were only 1/3, and hence there may be bias (i.e., ascertainment bias). In particular, high-resourced programs, which serve a larger number of patients, may have been more likely to be represented in the sample; this could result in over-estimates on capacity indicators.
The other main limitation relates to measurement. First, IHD incidence is estimated by GBD in many countries, and thus measurement error is expected. Second, volume drivers were chosen based on investigator opinion from the variables available in the survey; the survey was developed to assess the nature of programs, not drivers of volume. There are likely unmeasured factors at play. For this reason, readers should use caution when interpreting the results from the test of drivers. These should be considered exploratory at this stage, with future research needed to further investigate. Third, national capacity was computed by multiplying the median capacity in responding programs by the total number of programs; given not all programs responded to the survey where capacity was reported, and that program-reported capacity values were not validated in a random subsample of programs (nor were volumes or drivers of volume assessed); this would also introduce some error. These values were used to compute density estimates, which therefore should also be interpreted with some caution.
On a related note, there are some measurement issues related to CR density specifically. It has been estimated based on IHD incidence only for reasons outlined above, and therefore without considering heart failure, density is surely over-estimated. Additionally, the term CR density has been variably operationalized in the literature (e.g., ratio of population to number of programs), and hence comparisons to values reported in other studies should not be undertaken. This is the first study to have been able to characterize CR density as spots per indicated patient specifically, and it is hoped that in future studies this more accurate approach will be applied. Understanding the incidence of CR-indicated conditions (i.e., IHD and heart failure) on a national basis globally is another important area for further work (crudely, the annual incidence of CVD globally is 422.7 million cases [2]; given the number of CR spots globally, this suggests a density of 1 spot per 255 CVD patients), as is identifying drivers of density.
There also some broader limitations that should be considered. The first concerns practical importance of the findings. The significance of the inferential tests reported herein should not be interpreted to suggest significance from a health system, practice or clinical perspective. Second, due to the nature of the design, causal conclusions should not be drawn. Finally, due to multiple tests, there could be inflated error.
In conclusion, despite guideline recommendations that CVD patients should access CR, it is only available in half of countries around the world, and where available, density was grossly insufficient to serve all patients in need. Programs offering alternative models and that are funded by multiple sources treated more patients than those that are not. Advocacy for more programs that each serve the maximal number of patients safely is needed to ensure all guideline-indicated patients achieve the reductions in cardiovascular mortality and morbidity associated with CR participation.
Funding
This research was supported by a grant from York University's Faculty of Health. The funder had no role in study design, data collection, data analysis, interpretation or writing of the report.
Authors' Contributions
KTA contributed to study design, data acquisition (i.e., identifying countries with cardiac rehabilitation and contacting champions to collect data from programs), data analysis and co-drafted the manuscript; MS conducted data collection; FLJ had substantial contributions to conception and design of work; facilitation of data collection in South America; EP assisted in data cleaning and drafting display items; RD, RB, BBW, WD, AA, ASB, CAS, SKJ, LC, TJY, DS, KA, GG, VG, DV, EV, JC, EK, IY, CK, BB, ERE, RF, BR, DG, AS, SYC, BR, JCM, LM, GB, RS, HL, MS, ES, AH, ETP, MA, LN, EA, HK, ZE, SF, JH, EP, SD, CS, CZ, BP, AK, NS, CB, RT, and DH arranged data collection from the cardiac rehabilitation programs in their country (sampling) and revised the manuscript critically for important intellectual content. S.L.G. was responsible for the conception and design of the work, interpretation of the data, and drafting the manuscript. All authors had full access to all of the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis. All authors interpreted data and critically revised and approved the final manuscript. KTA is the guarantor. The corresponding author attests that all listed authors meet authorship criteria.
Declaration of Competing Interest
Dr. Derman reports some financial activities that were outside the submitted work (i.e., grants from International Olympic and Paralympic Committees, as well as personal fees from 2 advisory boards). All other authors declare no financial or personal interests.
Acknowledgment
On behalf of the International Council of Cardiovascular Prevention and Rehabilitation through which this study was undertaken, we are grateful to others who collaborated with us to identify and reach programs in their country, namely: Dr. Alexander Aleksiev, Dr. Artur Herdy, Dr. Robyn Gallagher, Dr. Josef Niebauer, Dr. Martin Heine, Maria Mooney, Dr. Borut Jug, Dr. Aashish Contractor, Dr. Batgerel Oidov, Dr. Henrik Schirmer, and Dr. Fernando Sepuvelda. We also thank Ms. Anfal Adawi for assisting with display items. We thank the following associations for assisting with program identification: Korean Academy of Cardiopulmonary Rehabilitation Medicine, the British Association of Cardiovascular Prevention and Rehabilitation, the International Society of Physical and Rehabilitation Medicine, Associação Brasileira de Fisioterapia Cardiorrespiratória e Fisioterapia em Terapia Intensiva (ASSOBRAFIR), the Australian Cardiovascular Health and Rehabilitation Association (ACRA) and World Heart Federation (who also formally endorsed the study protocol). We are also grateful to Dr. Carmen Terzic who shared the CR program survey administered in Latin America with the investigative team; this work informed development of the survey administered in this study. Finally, we would like to thank York University for supporting this study by a research grant through York University's Faculty of Health.
Footnotes
Prof. Sherry Grace confirmed that she had full access to all the data in the study and had final responsibility for the decision to submit for publication.
References
- 1.Mendis S., Puska P., Norrving B. World Health Organization; Geneva: 2011. Global atlas on cardiovascular disease prevention and control. [Google Scholar]
- 2.Roth G.A., Johnson C., Abajobir A., Abd-Allah F., Abera S.F., Abyu G. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. 2017;70:1–25. doi: 10.1016/j.jacc.2017.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shields G.E., Wells A., Doherty P., Heagerty A., Buck D., Davies L.M. Cost-effectiveness ofcardiac rehabilitation: a systematic review. Heart. 2018 doi: 10.1136/heartjnl-2017-312809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anderson L., Oldridge N., Thompson D.R., Zwisler A.D., Rees K., Martin N. Exercise-based cardiac rehabilitation for coronary heart disease. J Am Coll Cardiol. 2016;67:1–12. doi: 10.1016/j.jacc.2015.10.044. [DOI] [PubMed] [Google Scholar]
- 5.Smith S.C., Benjamin E.J., Bonow R.O., Braun L.T., Creager M.A., Franklin B.A. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. J Am Coll Cardiol. 2011;58:2432–2446. doi: 10.1016/j.jacc.2011.10.824. [DOI] [PubMed] [Google Scholar]
- 6.Gaalema D.E., Higgins S.T., Shepard D.S., Suaya J.A., Savage P.D., Ades P.A. State-by-state variations in cardiac rehabilitation participation are associated with educational attainment, income, and program availability. J Cardiopulm Rehabil Prev. 2014;34:248–254. doi: 10.1097/HCR.0000000000000059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Turk-Adawi K., Sarrafzadegan N., Grace S.L. Global availability of cardiac rehabilitation. Nat Rev Cardiol. 2014;11:586–596. doi: 10.1038/nrcardio.2014.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gaziano T.A., Bitton A., Anand S., Abrahams-Gessel S., Murphy A. Growing epidemic of coronary heart disease in low- and middle-income countries. Curr Probl Cardiol. 2010;35:72–115. doi: 10.1016/j.cpcardiol.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ragupathi L., Stribling J., Yakunina Y., Fuster V., Mclaughlin M.A., Vedanthan R. Availability, use, and barriers to cardiac rehabilitation in LMIC. Glob Heart. 2016;12:323–334. doi: 10.1016/j.gheart.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 10.Goto Y., Saito M., Iwasaka T., Daida H., Kohzuki M., Ueshima K. Poor implementation of cardiac rehabilitation despite broad dissemination of coronary interventions for acute myocardial infarction in Japan: a nationwide survey. Circ J. 2007;71:173–179. doi: 10.1253/circj.71.173. [DOI] [PubMed] [Google Scholar]
- 11.Korenfeld Y., Mendoza-Bastidas C., Saavedra L., Montero-Gómez A., Perez-Terzic C., Thomas R.J. Current status of cardiac rehabilitation in Latin America and the Caribbean. Am Heart J. 2009;158:480–487. doi: 10.1016/j.ahj.2009.06.020. [DOI] [PubMed] [Google Scholar]
- 12.Cortes-Bergoderi M., Lopez-Jimenez F., Herdy A.H., Zeballos C., Anchique C., Santibañez C. Availability and characteristics of cardiovascular rehabilitation programs in South America. J Cardiopulm Rehabil Prev. 2013;33:33–41. doi: 10.1097/HCR.0b013e318272153e. [DOI] [PubMed] [Google Scholar]
- 13.One World Nations Online Population figures for all countries. http://www.nationsonline.org/oneworld/population-by-country.htm
- 14.World Health Organization Countries. http://www.who.int/countries/en/
- 15.Institute for Health Metrics and Evaluation (IHME) Global burden of disease results. 2016. http://ghdx.healthdata.org/gbd-results-tool
- 16.Fihn S.D., Gardin J.M., Abrams J., Berra K., Blankenship J.C., Dallas A.P. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease. J Am Coll Cardiol. 2012;60:e44–e164. doi: 10.1016/j.jacc.2012.07.013. [DOI] [PubMed] [Google Scholar]
- 17.Pesah E., Supervia M., Turk-Adawi K., Grace S.L. A review of cardiac rehabilitation delivery around the world. Prog Cardiovasc Dis. 2017;60:267–280. doi: 10.1016/j.pcad.2017.08.007. [DOI] [PubMed] [Google Scholar]
- 18.Turk-Adawi K.I., Terzic C., Bjarnason-Wehrens B., Grace S.L. Cardiac rehabilitation in Canada and Arab countries: comparing availability and program characteristics. BMC Health Serv Res. 2015;15 doi: 10.1186/s12913-015-1183-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Supervia M., Turk-Adawi K., Lopez Jimenez F., Pesah E., Ding R., Britto R. Quality of cardiac rehabilitation around the globe: Nature of Cardiac Rehabilitation Around the Globe. eClinicalMedicine. 2019 [Google Scholar]
- 20.International Buisness Machines Corporation . IBM Cor; Armonk, NY: 2016. Statistical package for the social sciences software. [Google Scholar]
- 21.Chestnov O., World Health Organization . World Health Organization; Geneva: 2013. Global action plan for the prevention and control of noncommunicable diseases. [Google Scholar]
- 22.Yancy C.W., Jessup M., Bozkurt B., Butler J., Casey D.E., Jr., Drazner M.H. ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 2013;2013(62):e147–e239. doi: 10.1016/j.jacc.2013.05.019. [DOI] [PubMed] [Google Scholar]
- 23.Kottke T.E., D a Faith, Jordan C.O., Pronk N.P., Thomas R.J., Capewell S. The comparative effectiveness of heart disease prevention and treatment strategies. Am J Prev Med. 2009;36:82–88. doi: 10.1016/j.amepre.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 24.Mendis S. World Health Organization; Geneva: 2014. World Health Organization global status report on noncommunicable diseases. [DOI] [PubMed] [Google Scholar]
- 25.Grace S.L., Turk-Adawi K.I., Contractor A., Atrey A., Campbell N.R., Derman W. Cardiac rehabilitation delivery model for low-resource settings: an International Council of Cardiovascular Prevention and Rehabilitation consensus statement. Prog Cardiovasc Dis. 2016;59:1–20. doi: 10.1016/j.pcad.2016.08.004. [DOI] [PubMed] [Google Scholar]
- 26.Grace S.L., Turk-Adawi K.I., Contractor A., Atrey A., Campbell N.R., Derman W. Cardiac rehabilitation delivery model for low-resource settings. Heart. 2016;102:1449–1455. doi: 10.1136/heartjnl-2015-309209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Babu A.S., Lopez-Jimenez F., Thomas R.J., W3 Isaranuwatchai, Herdy A.H., Hoch J.S. Advocacy for outpatient cardiac rehabilitation globally. BMC Health Serv Res. 2016;16:471. doi: 10.1186/s12913-016-1658-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moghei M., Turk-adawi K., Isaranuwatchai W., Sarrafzadegan N., Oh P., Chessex C. Cardiac rehabilitation costs. Int J Cardiol. 2017;244:322–328. doi: 10.1016/j.ijcard.2017.06.030. [DOI] [PubMed] [Google Scholar]
- 29.Grace S.L., Turk-Adawi K., Pio CS de A., Alter D.A. Ensuring cardiac rehabilitation access for the majority of those in need: a call to action for Canada. Can J Cardiol. 2016;32:S358–S364. doi: 10.1016/j.cjca.2016.07.001. [DOI] [PubMed] [Google Scholar]
- 30.International Council of Cardiovascular Prevention and Rehabilitation ICCPR Cardiovascular Rehabilitation Foundations Certification (ICCPR CRFC) 2017. http://globalcardiacrehab.com/training-opportunities/certification/
- 31.Jahan S. Human development report 2016 human development for everyone. 2016. http://hdr.undp.org/sites/default/files/2016_human_development_report.pdf New York.
- 32.World Bank World Bank country and lending groups. 2017. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups [Accessed December 6, 2017]