Abstract
Objective:
Pneumonia is the leading cause of pediatric mortality worldwide among children 0–5 years old. Lung ultrasound can be used to diagnose pneumonia in rural areas as it is a portable and relatively economic imaging modality with ~95% sensitivity and specificity for pneumonia in children. Lack of trained sonographers is the current limiting factor to its deployment in rural areas. In this study, we piloted training of a volume sweep imaging (VSI) ultrasound protocol for pneumonia detection in Peru with rural health workers. VSI may be taught to individuals with limited medical/ultrasound experience as it requires minimal anatomical knowledge and technical skill. In VSI, the target organ is imaged with a series of sweeps and arcs of the ultrasound probe in relation to external body landmarks.
Methods:
Rural health workers in Peru were trained on a VSI ultrasound protocol for pneumonia detection. Subjects were given a brief didactic session followed by hands-on practice with the protocol. Each attempt was timed and mistakes were recorded. Participants performed the protocol until they demonstrated two mistake-free attempts.
Results:
It took participants a median number of three attempts (range 1–6) to perform the VSI protocol correctly. Time to mastery took 51.4 ± 17.7 min. There were no significant differences among doctors, nurses, and technicians in total training time (P = 0.43) or number of attempts to success (P = 0.72). Trainee age was not found to be significantly correlated with training time (P = 0.50) or number of attempts to success (P = 0.40).
Conclusion:
Rural health workers learned a VSI protocol for pneumonia detection with relative ease in a short amount of time. Future studies should investigate the clinical efficacy of this VSI protocol for pneumonia detection.
Key Message:
A volume sweep imaging (VSI) protocol for pneumonia detection can be taught with minimal difficulty to rural health workers without prior ultrasound experience. No difference was found in training performance related to education level or age. VSI involves no significant knowledge of anatomy or technical skill.
Keywords: Ultrasound, Lung ultrasound, Pneumonia, Volume sweep imaging, Global health, Pediatrics
INTRODUCTION
Pneumonia is the leading cause of pediatric mortality worldwide among children 0–5 years old; in 2016, there were an estimated 900,000 deaths from pneumonia in this age group, exceeding the number of deaths from diarrhea and malaria combined.[1,2] There are about 150 million cases of pediatric pneumonia a year globally requiring millions of hospitalizations.[3] Even for experienced clinicians, pneumonia is difficult to diagnose without high-quality imaging. The literature clearly shows that clinical history and physical exam are not reliable predictors of pneumonia as its signs and symptoms are generally non-specific.[4,5] Current approaches to pneumonia diagnosis focused on history and physical exam presently employed in rural areas (community case management) are helpful but insufficient.[6-8]
As a cost-effective and portable imaging modality, ultrasound holds promise in improving diagnosis of pneumonia and therefore, clinical outcomes in these settings. Lung ultrasound (LUS) has been verified by numerous studies as superior in sensitivity and specificity for pneumonia detection when compared to the historic “gold-standard” of chest X-ray in adults and children.[9-15] Ultrasound is ideal in children to assess for pneumonia due to their small thoracic diameter, and it does not expose children to ionizing radiation.[14,16-20] Deployment of this approach, however, is limited by the availability of trained sonographers.
As a solution to this problem, an easy-to-learn volume sweep imaging (VSI) scan procedure that covers the entire lung volume may circumvent the need for experienced sonographers. In VSI, a trained operator captures cine clips of the target organ using a series of sweeps and arcs with the ultrasound probe based on external body landmarks. VSI protocols can be taught in a short amount of time to individuals without significant medical or ultrasound experience as no significant anatomical knowledge or technical skill is required. The images obtained from operators performing VSI protocols may be sent to a central location for interpretation, removing the need for on-site trained readers and sonographers.[21-23] VSI has been piloted in both Uganda and Peru and has many promising potential applications. In these locations, VSI has been employed for the detection of obstetrics, thyroid, and right upper quadrant pathology. To the best of our knowledge, no group has tested a VSI protocol for pneumonia detection.
There is a strong theoretical precedent in the literature for this approach. Many studies have shown minimal training to be effective in teaching LUS among novice residents, medical students, and respiratory technicians.[24-27] For example, novice respiratory technicians without prior training could perform LUS exams independently with <2% of exams requiring assistance and 5% interpretation error after only ten supervised exams.[24] Several other studies have found that novice sonographers, once minimally trained, have technical skills and practical knowledge comparable to seasoned sonographers.[25,28-31] To emphasize, a VSI approach is made even easier than the cited studies as rural health workers are not conducting a full traditional exam or interpreting images. The VSI protocol involves performing a series of preset sweeps and arcs based on external body landmarks and may be performed without looking at the screen as it is completely image independent. In practice, the collected images are sent to a central location for interpretation through telemedicine.
Although literature on LUS and pneumonia is extensive, literature on VSI is scarce. To validate the use of VSI for pneumonia detection, several studies must be undertaken. This study aimed to investigate the feasibility of training rural health workers on a VSI protocol as the first step in this process. Members of the study team traveled to rural Peru to pilot training of rural health workers in local health centers. We hypothesized that rural health workers would learn the VSI protocol with relative ease. Members of the rural health centers underwent training, and a retrospective audit of the training was conducted.
SUBJECTS AND METHODS
We conducted a retrospective audit of VSI LUS training that took place in Quillabamba, Peru, in December 2018. Quillabamba is a rural area about 140 miles away from Cusco, Peru. It is situated in the jungle and its economy is based in agriculture. Training occurred at four health centers in this region. This study was reviewed by the University of Rochester IRB and was determined to be a “training exercise” that did not require full IRB approval. We trained 21 rural health workers during our investigation. Subjects varied in profession and age [Table 1]. Only one subject was male. Three of our subjects had minimal ultrasound training, but the rest had no prior ultrasound experience. After a brief introductory lecture explaining the project, we began individualized training on the VSI protocol. Each participant was given a short (~20 minutes) lecture in Spanish on the VSI protocol. Participants were then given a demonstration of the VSI protocol, and all of their questions were answered.
Table 1:
Overall subject data (n=21).
| Subject data | Value |
|---|---|
| Age (years) | 42.3±8.87 (25–58) |
| Gender | 95.2% female (n=20) |
| Career | 14.3% doctor (n=3), 33.3% nurse (n=7), 52.4% tech (n=11) |
| Total training time (min) | 51.4±17.7 (25–80) |
| Average time for the first attempt (s) | 344.3±74.1 (225–485) |
| Average time for the last attempt (s) | 259.5±44.6 (215–345) |
| Number of attempts for first perfect | 3 (1–6) |
| Number of attempts for second perfect | 4 (2–7) |
| Lung side trained | 52.4% right (n=11) |
Values are mean±standard deviation (range) for age, total training time, and attempt time. Value for number of attempts is median (range)
The participants then underwent hands-on training with the VSI protocol. Each participant then performed the VSI protocol solely from memory without any paper aids or prompting from the study team. A study member served as the model for practice exams. We trained subjects on one hemithorax (right or left lung) for time purposes as the health workers were taking time directly from their workday to participate in the study. Each attempt at performing the protocol was carefully observed and timed by study members. All mistakes with the protocol were recorded and notes were made. During each attempt, at least one study member would observe the trainee for mistakes. Another study member recorded all of the data on an Excel spreadsheet as each exam progressed. Even one mistake resulted in a failed attempt. Possible mistakes included failed arcs and sweeps, not using enough gel, or mis-positioning the probe. A complete report of mistakes is included in the results section, and we employed standardized definitions of each mistake to ensure consistency between the trainees. After each complete attempt, study members explained the mistakes each participant made and answered any questions. Participants continued performing the protocol until they performed it perfectly two consecutive times without error. After this, if time permitted, each subject performed the protocol on the opposite hemithorax until one perfect attempt. Following the training, a brief survey was completed. The ultrasound images themselves were saved for a few representative trainees. These images were not formally reviewed after the study. However, during the study itself, the study members ensured the images were of adequate diagnostic quality. Trainees who did not produce adequate diagnostic images failed that attempt. A sample exam has been included in Supplemental Material A.
VSI protocol
In our VSI protocol, each hemithorax is divided into six areas (two anterior, two posterior, and two lateral) [Figure 1]. The anterior section is between the parasternal line and the anterior axillary line. The lateral section is between the anterior axillary line and the posterior axillary line. The posterior section is between the posterior axillary line and the paravertebral line. Each section is further divided in half to form superior and inferior sections by convention and to assist the trainee in conceptualization. Operators capture images using a series of motions (sweeps and arcs) in relation to external body landmarks to cover the entire volume of lung. This is performed in both longitudinal and transverse orientations in both the right and left hemithorax [Figure 2]. Scans are conducted in transverse and longitudinal views in each section as a previous study found the omission of any lung field or orientation could miss pneumonia.[32] Arcs involve tilting the ultrasound probe a full 180º over about 5 s. Sweeps are translational movements of the probe performed at a rate of about 3 cm/s–4 cm/s. A linear probe is often used in pediatric patients, but a curvilinear probe was used in our training due to the availability of probes in the rural area. The entire exam can be performed in around 10 minutes. The patient can be in any position so long as the arcs and sweeps are performed in the proper location. In our experiences, it is easiest for the patients to lay in the supine position for the anterior and lateral lung exam. For the lateral lung exam, the arm should be placed over the patients head to better expose the lateral lung. The posterior lung exam is best performed while the patient lays prone.
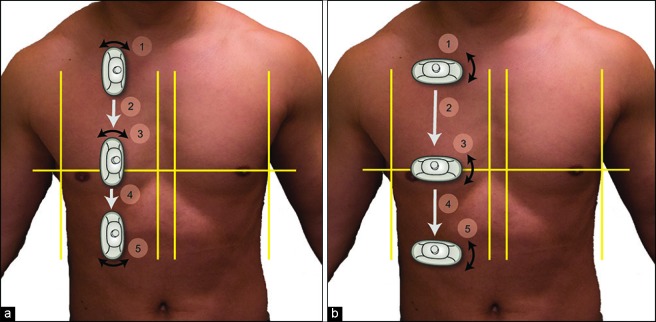
Figure 1:
(a) Anterior (1 and 2) and lateral lung areas (3 and 4). Parasternal line, anterior axillary line, and posterior axillary line are labeled. (b) Posterior lung areas (5 and 6). Posterior axillary line and paravertebral line are labeled.
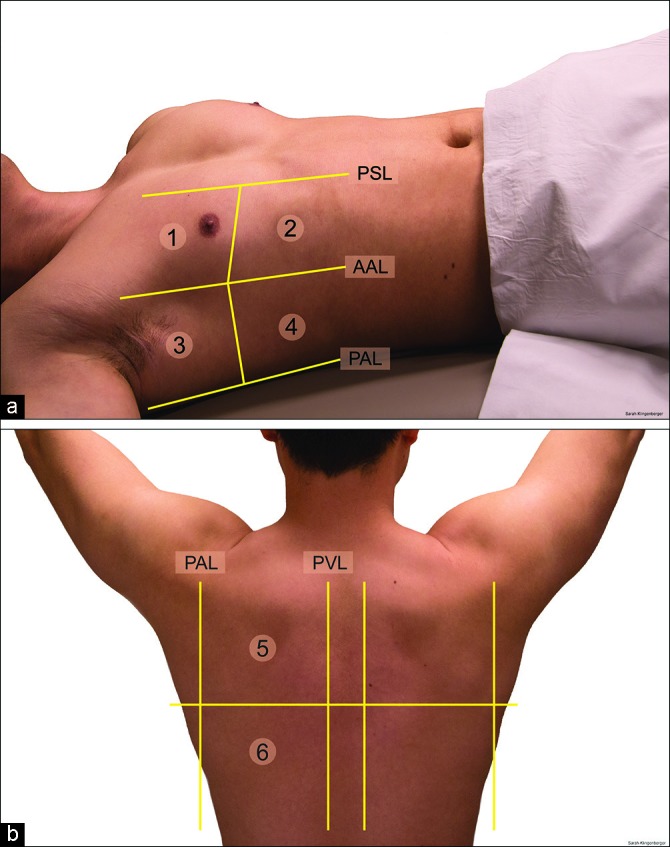
Figure 2:
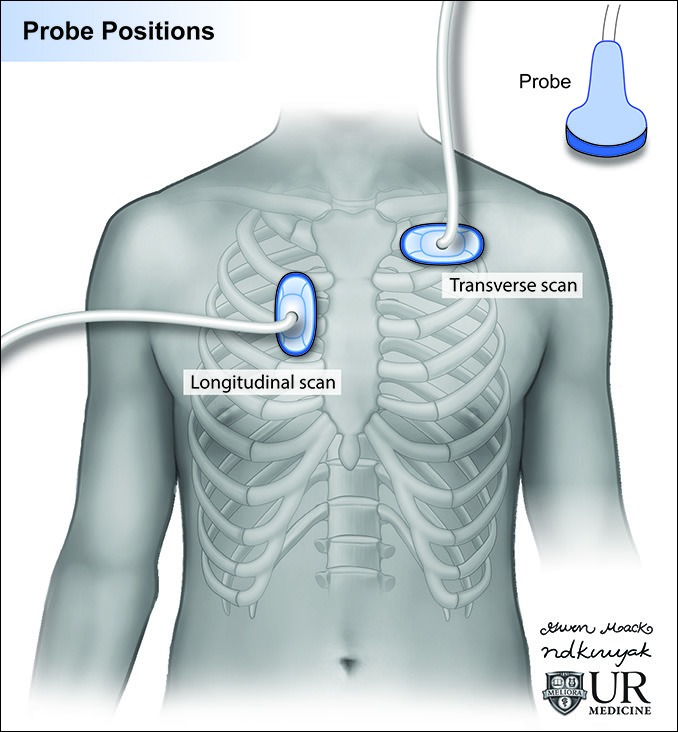
Illustration of the probe position in longitudinal and transverse scans.
The protocol begins in the anterior lung. The operator performs a 180° arc with the ultrasound probe slightly below the level of the clavicle at the midclavicular line. The probe is then swept to about one finger below the nipple where another arc is performed. Finally, the probe is swept to the lower chest where a final arc is performed. The lateral section begins with an arc performed in the axilla followed by a sweep down to the lower chest where another arc is performed. The protocol ends with an examination of the posterior lung and mirrors the anterior lung exam. An arc is performed at the top of the back, followed by a sweep down to the mid-back where an additional arc is performed. This is followed by a final sweep down to the lower back where a final arc is obtained. Operators performing the posterior exam are instructed to base the sweeps and arcs on the anatomical landmarks of the anterior chest. This is summarized in Figures 3-5. A video demonstrating how to perform the protocol is included in Supplemental Material B.
Figure 3:
(a) Longitudinal exam of the right anterior lung. The operator performs an arc (1) followed by a sweep (2) to the nipple. At the nipple another arc is performed (3). Finally, there is a sweep (4) to the lower chest where a final arc is performed (5). (b) Transverse exam follows the same steps with the probe in the transverse orientation.
Figure 5:
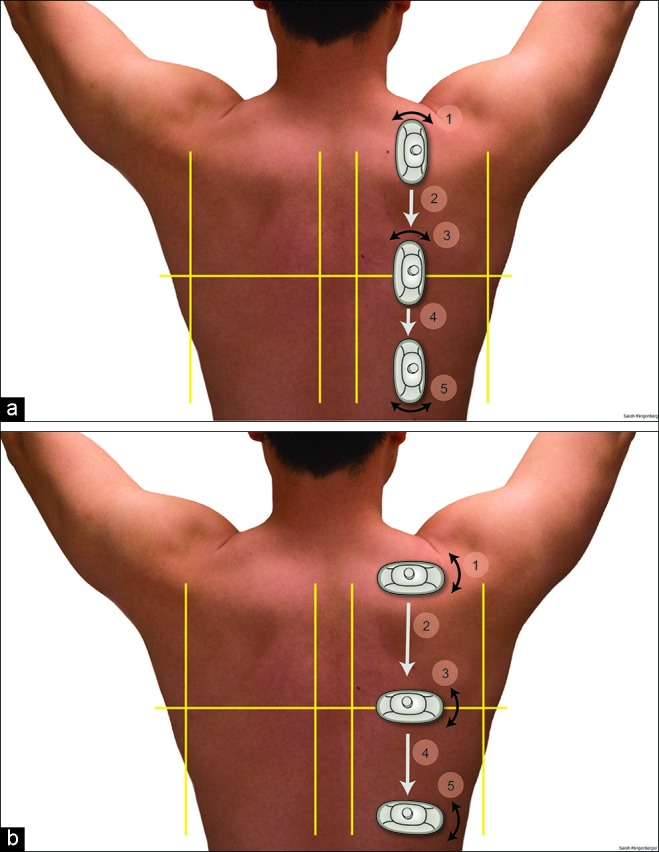
(a) Longitudinal exam of the right posterior lung. The operator performs an arc (1), followed by a sweep (2) to the mid-back. At the mid-back, another arc is performed (3). Finally, there is a sweep (4) to the lower back where a final arc is performed (5). (b) Transverse exam follows the same steps with the probe in the transverse orientation.
Figure 4:
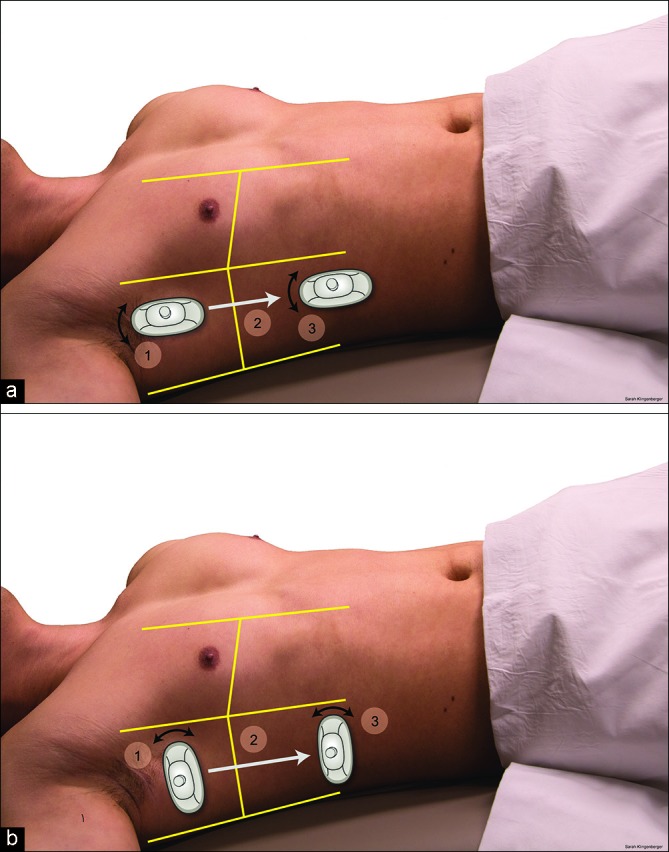
(a) Longitudinal exam of the right lateral lung. The operator performs an arc in the upper axillary region (1), followed by a sweep (2) to the lower chest where a final arc is performed (3). (b) Transverse exam follows the same steps with the probe in the transverse orientation.
Statistical analysis
Differences between nurses, technicians, and doctors were compared using ordinary one-way ANOVA with post hoc pairwise comparison performed using Tukey’s test. Unpaired t-tests were used to compare differences in training between the right and left lungs. Correlation between age and training time or number of attempts to successful execution was computed with the Spearman correlation coefficient.
RESULTS
Overall, rural health workers learned our VSI protocol without difficulty. We trained 21 rural health workers of varying age and careers [Table 1]. The average training time was about 51.4 ± 17.7 minutes, and it took a median number of three attempts for participants to perform the protocol perfectly. The protocol took an average of 259.5 ± 44.6 s to perform on each hemithorax on a participant’s final attempt (about 4 minutes). ANOVA showed no difference between nurses, technicians, and doctors in training time or attempts [Table 2]. Likewise, no correlation was identified between age or training time/attempts (P > 0.5). There were no significant differences between performing the protocol on the right or left lung. Among participants who were tested on the opposite lung after mastery of the protocol on one hemithorax (n = 16), 75% performed the opposite lung exam perfectly. Those who made a mistake (n =4) reversed the direction of the probe marker; on a second attempt, all of these participants performed the protocol perfectly. The most common types of mistakes involved performing arcs and sweeps incorrectly; other mistakes included positioning the probe incorrectly, positioning the marker incorrectly, reversing the orientation of the probe, performing the exam on the wrong lung, not using enough gel, and adding/subtracting a step in the protocol [Tables 3 and 4]. A brief survey suggested that participants found our protocol easy and enjoyable to learn [Table 5].
Table 2:
Differences based on career.
| Variable | Doctor (n=3) | Nurse (n=7) | Tech (n=11) | P value |
|---|---|---|---|---|
| Age (years) | 32.3±8.1 | 43.7±9.5 | 44.2±7.4 | 0.10 |
| Total training time (min) | 46.7±5.8 | 45.7±19.9 | 56.4±18.0 | 0.43 |
| Number of attempts for first perfect attempt | 3±0 | 3.1±1.8 | 3.6±1.5 | 0.72 |
| Number of attempts for a second perfect attempt | 4±0 | 4.1±1.8 | 4.8±1.5 | 0.57 |
Values are mean±standard deviation. P values are results of ordinary one-way ANOVA. Post hoc testing was performed using Tukey’s test to examine pairwise comparisons, no significant differences were found
Table 3:
Overall mistakes made.
| Type of mistake | % of total mistakes (n) |
|---|---|
| Arc mistake | 22.8 (n=28) |
| Sweep mistake | 22.0 (n=27) |
| Marker mistake | 15.4 (n=19) |
| Positioning mistake | 8.9 (n=11) |
| Gel mistake | 7.3 (n=9) |
| Wrong lung mistake | 5.7 (n=7) |
| Orientation (trans/sag) mistake | 6.5 (n=8) |
| Added step mistake | 4.9 (n=6) |
| Subtracted step mistake | 6.5 (n=8) |
Table 4:
Type of mistakes made versus attempt number.
| Type of mistake | Attempt 1 (n=21) (%) | Attempt 2 (n=21) (%) | Attempt 3 (n=19) (%) | Attempt 4 (n=16) (%) | Attempt 5 (n=8) (%) | Attempt 6 (n=7) (%) | Attempt 7 (n=2) (%) |
|---|---|---|---|---|---|---|---|
| Arc | 61.9 | 33.3 | 21.1 | 18.8 | 12.5 | 0.0 | 0.0 |
| Sweep | 42.9 | 47.6 | 21.1 | 12.5 | 25.0 | 0.0 | 0.0 |
| Marker | 38.1 | 14.3 | 21.1 | 18.8 | 12.5 | 0.0 | 0.0 |
| Positioning | 33.3 | 14.3 | 5.3 | 0.0 | 0.0 | 0.0 | 0.0 |
| Gel | 23.8 | 19.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Wrong lung | 19.0 | 9.5 | 0.0 | 6.3 | 0.0 | 0.0 | 0.0 |
| Orientation (trans/sag) | 14.3 | 9.5 | 15.8 | 0.0 | 0.0 | 0.0 | 0.0 |
| Added step | 14.3 | 4.8 | 5.3 | 6.7 | 0.0 | 0.0 | 0.0 |
| Subtracted step | 14.3 | 14.3 | 5.3 | 6.3 | 0.0 | 0.0 | 0.0 |
Values are the percentage of subjects making a particular mistake at a given attempt number. It should be noted that participants stopped performing the protocol after two consecutive mistake-free exams, and the median number of attempts to a mistake-free exam was 3
Table 5:
Survey results.
| Survey item | Average response |
|---|---|
| I feel comfortablecollecting a complete lung ultrasound examination that can be used for the diagnosis of pneumonia | 4.2 |
| I am confident in my ability to conduct a complete lung ultrasound examination that can be used for the diagnosis of pneumonia | 4.2 |
| I am satisfied with my training to complete a lung ultrasound examination that can be used for the diagnosis of pneumonia | 4.4 |
| Learning how to conduct a complete lung ultrasound examination was easy | 4 |
| Learning how to conduct a complete lung ultrasound was something I enjoyed | 4.5 |
Participants were asked if they strongly disagreed (1), disagreed (2), were neutral (3), agreed (4), or strongly agreed (5) to each of these items
DISCUSSION
The last century has seen unprecedented revolutions in the delivery of health care, and the fruits of biomedical research have been responsible for saving millions of lives. Despite these enormous strides, a significant gap in medical care availability remains in the developing world. Radiology has an enormous role to play in closing this gap. In this study, we investigated the feasibility of training rural health workers on a VSI ultrasound protocol in Peru. Widespread deployment of a VSI protocol for pneumonia detection with LUS may provide a cost-effective, high quality, and life-saving diagnostic tool for millions in these underserved areas in synergy with millennium development goal four which aims to reduce childhood mortality.[33]
Our findings show that rural health workers without significant prior ultrasound experience can be taught how to perform a VSI protocol with minimal training. The average training time of ~50 minutes to perform the protocol without errors suggests that deploying VSI in rural areas is feasible from a training perspective. This protocol may be integrated into routine clinical practice without undue disruption as the complete exam may be performed in about 10 minutes, including both longitudinal and transverse views. In theory, the protocol time could be cut in half if only longitudinal or transverse views were obtained. However, there is data in the literature suggesting that both views are needed to maximize sensitivity and specificity, and collecting both views also adds redundancy to control for any errors at the tradeoff of increased time to perform the protocol.[32]
The data show that regardless of age or education, participants learned the protocol equally easily. The implication is that learning a VSI protocol is a simple technical skill and not a function of medical knowledge or dexterity. The surveys we collected showed that the rural health workers we trained enjoyed learning the protocol. In the subjective survey comments, the trainees wrote that this technology would be helpful to implement in their communities. Those we trained also expressed appreciation for being involved in the project on multiple levels. The participants stated that rural communities were traditionally ignored by the government and generally forgotten, so being involved in a study to improve community health in these areas was appreciated. The technicians and nurses were particularly grateful to be involved as they expressed that most of the time, only doctors are involved in medical procedures and education.
Our VSI training exercise provided much data regarding how future VSI training should occur. We identified several common pitfalls that rural health workers made when performing the VSI protocol and solutions [Table 6]. Over the course of the training, our team became more adept at anticipating these potential pitfalls and tailoring training to address them. It should be noted that our training findings are even more impressive when considering that all participants were performing the VSI protocol from memory. If posters or paper instructions/illustrations of the protocol were provided, it would be likely that training time and the number of mistakes made would decrease. Furthermore, many of the mistakes that were made by participants while training would not be clinically significant. For example, misplacing the ultrasound probe marker would result in a flipped image that would still yield clinically useful information.
Table 6:
Common pitfalls and solutions.
| Common pitfalls | Solutions |
|---|---|
| Examining the wrong lung | Identify the patient’s right hand before every step. Training materialsemphasizing the difference between right and left |
| Not positioning the marker correctly | Identify the patient’s right hand before every step. Training materialsemphasizing the difference between right and left. Coloring the marker |
| Not using enough gel | Encouraging excessive gel use |
| Performing arc too fast | Emphasize appropriate arc speed in training |
| Performing sweep too fast | Emphasize appropriate sweep speed in training |
The biggest limitation is that this study was designed to test the ability to train healthcare workers to perform VSI acquisition and was not designed to address the question of the clinical efficacy of the VSI protocol. Although there is ample evidence in literature to suggest LUS is highly sensitive and specific for pneumonia detection, we have no direct data regarding this protocol’s sensitivity and specificity for pneumonia in the hands of rural health workers. The findings of this study justify further investigation into the protocol’s clinical efficacy as it shows that training rural health workers is feasible in a short period of time with high accuracy. A second limitation of this study was that the training session had to be tailored for practicality. We trained rural health center workers over the course of their workday whenever they were available. Many of these workers had to stay late to finish their work or were willing to train with us after hours. The limited time available to train participants required us to streamline our study design. Ideally, we would have trained each participant with the full protocol on the right and left lungs. However, given time constraints, we opted to teach each participant on only one lung with the assumption that mastery of one lung would equate to mastery or near mastery of the other. Our data show that this assumption was correct. Another limitation of this study is that it did not assess retention of the protocol over time. Future training regimens should ideally include some way to monitor the retention of the ability to perform the protocol accurately over time.
CONCLUSION
Our data suggest training rural health workers on a VSI protocol for pneumonia detection is both practical and effective. These findings warrant a future investigation into the ability of this VSI protocol to be implemented in rural areas for pneumonia detection. Future studies will need to assess the clinical efficacy of this protocol, including in the hands of trained rural health workers. If successfully validated, this approach may bring a highly sensitive and specific diagnostic test into rural areas helping better the health of millions in underserved communities.
Acknowledgment
We would like to thank Dr. Carlos Valer, Dr. Egoavil, the health workers, and patients at the Huayanay Health Center, the Potrero Health Center, the Pavayoc Health Center, and the Santa Ana Health Center for their hospitality and participation in this investigation. We would like to thank Dr. Solomon Kim, Mauricio Salazar, Sarah Klingenberger, Nadezhda Kiriyak, and Gwen Mack for their assistance with videos, illustrations, and figures. We would like to thank Dr. Vikram Dogra and Dr. Deborah Rubens for their support in the project.
Footnotes
How to cite this article: Marini TJ, Castaneda B, Baran T, O’Connor TP, Garra B, Tamayo L, et al. Lung ultrasound volume sweep imaging for pneumonia detection in rural areas: Piloting training in rural Peru. J Clin Imaging Sci 2019;9:35.
Financial support and sponsorship
We received a Fischer Fund Grant from the University of Rochester for $4,000 dollars to conduct this research.
Conflicts of interest
This project was made possible through partnership with Medical Innovation and Technology. This is a Peruvian company with the goal of bringing low-cost technology to rural areas. Medical Innovation and Technology coordinated our project with the rural health centers we visited. Benjamin Castaneda is a founder of Medical Innovation and Technology and assisted in the study design. Lorena Tamayo, Leslie Trujillo, and Claudia Carlotto assisted in the training and data collection, however, no one from the company was involved in the data analysis or interpretation. This manuscript was completed solely by those from the University of Rochester without financial conflict of interest.
References
- 1.Rudan I, O'Brien KL, Nair H, Liu L, Theodoratou E, Qazi S, et al. Epidemiology and etiology of childhood pneumonia in 2010: Estimates of incidence, severe morbidity, mortality, underlying risk factors and causative pathogens for 192 countries. J Glob Health. 2013;3:10401. doi: 10.7189/jogh.03.010401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McAllister DA, Liu L, Shi T, Chu Y, Reed C, Burrows J, et al. Global, regional, and national estimates of pneumonia morbidity and mortality in children younger than 5 years between 2000 and 2015: A systematic analysis. Lancet Glob Health. 2019;7:e47–57. doi: 10.1016/S2214-109X(18)30408-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rudan I, Boschi-Pinto C, Biloglav Z, Mulholland K, Campbell H. Epidemiology and etiology of childhood pneumonia. Bull World Health Organ. 2008;86:408–16. doi: 10.2471/BLT.07.048769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wipf JE, Lipsky BA, Hirschmann JV, Boyko EJ, Takasugi J, Peugeot RL, et al. Diagnosing pneumonia by physical examination: Relevant or relic ? Arch Intern Med. 1999;159:1082–7. doi: 10.1001/archinte.159.10.1082. [DOI] [PubMed] [Google Scholar]
- 5.Kelsberg G, Safranek S, Ely JW. Clinical inquiries. How accurate is the clinical diagnosis of pneumonia? J Fam Pract. 2003;52:63–4. [PubMed] [Google Scholar]
- 6.Sazawal S, Black RE, Pneumonia Case Management Trials Group. Effect of pneumonia case management on mortality in neonates, infants, and preschool children: A meta-analysis of community-based trials. Lancet Infect Dis. 2003;3:547–56. doi: 10.1016/S1473-3099(03)00737-0. [DOI] [PubMed] [Google Scholar]
- 7.Marsh DR, Gilroy KE, Van de Weerdt R, Wansi E, Qazi S. Community case management of pneumonia: At a tipping point? Bull World Health Organ. 2008;86:381–9. doi: 10.2471/BLT.07.048462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ayieko P, English M. Case management of childhood pneumonia in developing countries. Pediatr Infect Dis J. 2007;26:432–40. doi: 10.1097/01.inf.0000260107.79355.7d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yilmaz HL, Özkaya AK, Sari Gökay S, Tolu Kendir Ö, Senol H. Point-of-care lung ultrasound in children with community acquired pneumonia. Am J Emerg Med. 2017;35:964–9. doi: 10.1016/j.ajem.2017.01.065. [DOI] [PubMed] [Google Scholar]
- 10.Ye X, Xiao H, Chen B, Zhang S. Accuracy of lung ultrasonography versus chest radiography for the diagnosis of adult community-acquired pneumonia: Review of the literature and meta-analysis. PLoS One. 2015;10:e0130066. doi: 10.1371/journal.pone.0130066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yadav KK, Awasthi S, Parihar A. Lung ultrasound is comparable with chest roentgenogram for diagnosis of community-acquired pneumonia in hospitalised children. Indian J Pediatr. 2017;84:499–504. doi: 10.1007/s12098-017-2333-1. [DOI] [PubMed] [Google Scholar]
- 12.Xia Y, Ying Y, Wang S, Li W, Shen H. Effectiveness of lung ultrasonography for diagnosis of pneumonia in adults: A systematic review and meta-analysis. J Thorac Dis. 2016;8:2822–31. doi: 10.21037/jtd.2016.09.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Self WH, Courtney DM, McNaughton CD, Wunderink RG, Kline JA. High discordance of chest x-ray and computed tomography for detection of pulmonary opacities in ED patients: Implications for diagnosing pneumonia. Am J Emerg Med. 2013;31:401–5. doi: 10.1016/j.ajem.2012.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pereda MA, Chavez MA, Hooper-Miele CC, Gilman RH, Steinhoff MC, Ellington LE, et al. Lung ultrasound for the diagnosis of pneumonia in children: A meta-analysis. Pediatrics. 2015;135:714–22. doi: 10.1542/peds.2014-2833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chavez MA, Shams N, Ellington LE, Naithani N, Gilman RH, Steinhoff MC, et al. Lung ultrasound for the diagnosis of pneumonia in adults: A systematic review and meta-analysis. Respir Res. 2014;15:50. doi: 10.1186/1465-9921-15-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ambroggio L, Sucharew H, Rattan MS, O'Hara SM, Babcock DS, Clohessy C, et al. Lung ultrasonography: A viable alternative to chest radiography in children with suspected pneumonia? J Pediatr. 2016;176:93–8. doi: 10.1016/j.jpeds.2016.05.033. [DOI] [PubMed] [Google Scholar]
- 17.Guerra M, Crichiutti G, Pecile P, Romanello C, Busolini E, Valent F, et al. Ultrasound detection of pneumonia in febrile children with respiratory distress: A prospective study. Eur J Pediatr. 2016;175:163–70. doi: 10.1007/s00431-015-2611-8. [DOI] [PubMed] [Google Scholar]
- 18.Hendaus MA, Jomha FA, Alhammadi AH. Lung ultrasound for the diagnosis of childhood pneumonia: A safe and accurate imaging mode. Ther Clin Risk Manag. 2015;11:1817–8. doi: 10.2147/TCRM.S96222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Iorio G, Capasso M, De Luca G, Prisco S, Mancusi C, Laganà B, et al. Lung ultrasound in the diagnosis of pneumonia in children: Proposal for a new diagnostic algorithm. Peer J. 2015;3:e1374. doi: 10.7717/peerj.1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Urbankowska E, Krenke K, Drobczynski L, Korczynski P, Urbankowski T, Krawiec M, et al. Lung ultrasound in the diagnosis and monitoring of community acquired pneumonia in children. Respir Med. 2015;109:1207–12. doi: 10.1016/j.rmed.2015.06.011. [DOI] [PubMed] [Google Scholar]
- 21.Ross AB, DeStigter KK, Rielly M, Souza S, Morey GE, Nelson M, et al. A low-cost ultrasound program leads to increased antenatal clinic visits and attended deliveries at a health care clinic in rural Uganda. PLoS One. 2013;8:e78450. doi: 10.1371/journal.pone.0078450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pool KL, Garra BS, Bulas DI. Volume sweep imaging: Open-source technology for pediatric global health collaboration. Pediatr Radiol. 2014;44:677–8. doi: 10.1007/s00247-014-2937-9. [DOI] [PubMed] [Google Scholar]
- 23.Ferrer J, Chaumont T, Trujillo L, Fernandez I, Guerrero J, Stewart P, et al. New tele-diagnostic model using volume sweep imaging for rural areas. Conf Proc IEEE Eng Med Biol Soc. 2017;2017:2622–5. doi: 10.1109/EMBC.2017.8037395. [DOI] [PubMed] [Google Scholar]
- 24.See KC, Ong V, Wong SH, Leanda R, Santos J, Taculod J, et al. Lung ultrasound training: Curriculum implementation and learning trajectory among respiratory therapists. Intensive Care Med. 2016;42:63–71. doi: 10.1007/s00134-015-4102-9. [DOI] [PubMed] [Google Scholar]
- 25.Mozzini C, Pasini AM, Garbin U, Cominacini L. Lung ultrasound in internal medicine: Training and clinical practice. Crit Ultrasound J. 2016;8:10. doi: 10.1186/s13089-016-0048-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lim JS, Lee S, Do HH, Oh KH. Can limited education of lung ultrasound be conducted to medical students properly? A pilot study. Biomed Res Int. 2017;2017:8147075. doi: 10.1155/2017/8147075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Breitkreutz R, Dutiné M, Scheiermann P, Hempel D, Kujumdshiev S, Ackermann H, et al. Thorax, trachea, and lung ultrasonography in emergency and critical care medicine: Assessment of an objective structured training concept. Emerg Med Int. 2013;2013:312758. doi: 10.1155/2013/312758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Varshney T, Mok E, Shapiro AJ, Li P, Dubrovsky AS. Point-of-care lung ultrasound in young children with respiratory tract infections and wheeze. Emerg Med. J. 2016;33:603–10. doi: 10.1136/emermed-2015-205302. [DOI] [PubMed] [Google Scholar]
- 29.Ellington LE, Gilman RH, Chavez MA, Pervaiz F, Marin-Concha J, Compen-Chang P, et al. Lung ultrasound as a diagnostic tool for radiographically-confirmed pneumonia in low resource settings. Respir Med. 2017;128:57–64. doi: 10.1016/j.rmed.2017.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dankoff S, Li P, Shapiro AJ, Varshney T, Dubrovsky AS. Point of care lung ultrasound of children with acute asthma exacerbations in the pediatric ED. Am J Emerg Med. 2017;35:615–22. doi: 10.1016/j.ajem.2016.12.057. [DOI] [PubMed] [Google Scholar]
- 31.Baker K, Soong L, Harding T, Wain A, Cheah J, Mitchell G, et al. Sensitivity, specificity and diagnostic accuracy of novices integrating lung ultrasound into the care of breathless older patients. Australas J Ultrasound Med. 2015;18:143–5. doi: 10.1002/j.2205-0140.2015.tb00221.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Milliner BH, Tsung JW. Lung consolidation locations for optimal lung ultrasound scanning in diagnosing pediatric pneumonia. J Ultrasound Med. 2017;36:2325–8. doi: 10.1002/jum.14272. [DOI] [PubMed] [Google Scholar]
- 33.MDG 4: Reduce Child Mortality, United Nations Millenium Declaration. 2015 Available from: https://www.who.int/topics/millennium_development_goals/child_mortality/en [Last accessed 2019 Apr 25]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.