Abstract
Objective
To assess the effects of Helicobacter pylori treatment, vitamin supplementation, and garlic supplementation in the prevention of gastric cancer.
Design
Blinded randomized placebo controlled trial.
Setting
Linqu County, Shandong province, China.
Participants
3365 residents of a high risk region for gastric cancer. 2258 participants seropositive for antibodies to H pylori were randomly assigned to H pylori treatment, vitamin supplementation, garlic supplementation, or their placebos in a 2×2×2 factorial design, and 1107 H pylori seronegative participants were randomly assigned to vitamin supplementation, garlic supplementation, or their placebos in a 2×2 factorial design.
Interventions
H pylori treatment with amoxicillin and omeprazole for two weeks; vitamin (C, E, and selenium) and garlic (extract and oil) supplementation for 7.3 years (1995-2003).
Main outcome measures
Primary outcomes were cumulative incidence of gastric cancer identified through scheduled gastroscopies and active clinical follow-up through 2017, and deaths due to gastric cancer ascertained from death certificates and hospital records. Secondary outcomes were associations with other cause specific deaths, including cancers or cardiovascular disease.
Results
151 incident cases of gastric cancer and 94 deaths from gastric cancer were identified during 1995-2017. A protective effect of H pylori treatment on gastric cancer incidence persisted 22 years post-intervention (odds ratio 0.48, 95% confidence interval 0.32 to 0.71). Incidence decreased significantly with vitamin supplementation but not with garlic supplementation (0.64, 0.46 to 0.91 and 0.81, 0.57 to 1.13, respectively). All three interventions showed significant reductions in gastric cancer mortality: fully adjusted hazard ratio for H pylori treatment was 0.62 (95% confidence interval 0.39 to 0.99), for vitamin supplementation was 0.48 (0.31 to 0.75), and for garlic supplementation was 0.66 (0.43 to 1.00). Effects of H pylori treatment on both gastric cancer incidence and mortality and of vitamin supplementation on gastric cancer mortality appeared early, but the effects of vitamin supplementation on gastric cancer incidence and of garlic supplementation only appeared later. No statistically significant associations were found between interventions and other cancers or cardiovascular disease.
Conclusions
H pylori treatment for two weeks and vitamin or garlic supplementation for seven years were associated with a statistically significant reduced risk of death due to gastric cancer for more than 22 years. H pylori treatment and vitamin supplementation were also associated with a statistically significantly reduced incidence of gastric cancer.
Trial registration
ClinicalTrials.gov NCT00339768.
Introduction
In 2018 almost half of the estimated deaths from gastric cancer—the third leading cause of deaths from cancer globally—occurred in China.1 Linqu County, a rural area in Shandong province, northeastern China, has one of the highest mortality rates from gastric cancer worldwide (age adjusted rates per 100 000 were 55 for men and 19 for women in 1980-82).2 Solid evidence from epidemiologic studies links infection with Helicobacter pylori to the progression of precancerous gastric lesions and development of gastric cancer, and shows that diets rich in vitamin and garlic could protect against gastric cancer in high risk people with insufficient vitamin intake.3 4 5 In 1995, the Shandong Intervention Trial was initiated in Linqu to evaluate the effects of three interventions in preventing the progression of precancerous gastric lesions to gastric cancer.6 7 8 9 The interventions included H pylori treatment for two weeks and vitamin and garlic supplementation for just over seven years. After almost 15 years of follow-up (1995-2010), the trial reported a statistically significant reduction in incidence of gastric cancer and a non-statistically significant reduction in deaths due to gastric cancer associated with H pylori treatment, and the trial was recognized as the first to show a clear reduction in gastric cancer incidence with H pylori treatment.8 10 11 Both garlic and vitamin supplementation showed favorable trends for decreased gastric cancer incidence and mortality, but these effects were not statistically significant.8
Although the Shandong Intervention Trial suggested a potential role of H pylori treatment in the prevention of gastric cancer, further follow-up was needed to determine whether the reductions would persist and lead to a noticeable decrease in gastric cancer mortality. It also remained unknown whether vitamin and garlic supplementation would be associated with statistically significant reductions in gastric cancer incidence and mortality in the longer term. We therefore extended the follow-up to just over 22 years after randomization to ascertain gastric cancer incidence and mortality. Secondary outcomes were associations with other cause specific deaths.
Methods
Study population
In 1995 the Shandong Intervention Trial, a blinded randomized factorial placebo controlled trial, was initiated in Linqu, China.6 7 8 The year before the trial, a census of 13 randomly selected villages within four townships in Linqu identified 4010 residents aged 35-64 years. Of 3599 people who agreed to undergo gastroscopy with biopsies and to provide blood for H pylori serology, 3411 were randomly assigned to the trial in 19956 7 8 (see supplementary table 1). After exclusions for not meeting the eligibility criteria, 3365 people were included in the trial. A total of 2258 participants who were seropositive for antibodies to H pylori, as determined by IgG serology from enzyme linked immunoassay in 1994, were randomly assigned to three interventions (H pylori treatment with amoxicillin and omeprazole for two weeks, and/or garlic supplementation for 7.3 years, and/or vitamin supplementation for 7.3 years) or their placebos in a 2×2×2 factorial design. Overall, 1107 participants who were H pylori negative were randomly assigned to garlic supplementation and/or vitamin supplementation or their placebos in a 2×2 factorial design. The research service provider Westat (Rockville, MD) generated the randomized treatment assignments, and the participants received pill bottles bearing assignment codes to mask both participants and investigators to treatment.
From 15 September to 29 November 1995, H pylori positive participants received one capsule of 1 g amoxicillin and 20 mg omeprazole (n=1130) or a look alike placebo capsule (n=1128) twice daily for two weeks for H pylori treatment. To maintain masking, H pylori negative participants received a placebo capsule twice daily during the same period. 13C urea breath tests from January to March 1996 detected 382 participants who were still H pylori positive after initial treatment and they received treatment for a further two weeks. To preserve masking, 383 participants in the placebo group matched on village, age, and sex received repeat placebo treatment. For vitamin supplementation (30 November 1995 to 31 March 2003), participants received one capsule of 250 mg vitamin C, 100 IU vitamin E, and 37.5 μg selenium (n=1677) or a look alike placebo capsule (n=1688) twice daily for 7.3 years. From December 1995 to May 1996, the vitamin supplement also contained 7.5 mg β carotene.6 During this period, participants assigned to garlic supplementation received two capsules each containing 200 mg aged garlic extract and 1 mg steam distilled garlic oil (n=1678), or two look alike placebo capsules (n=1687), twice daily. Minute quantities of garlic oil were added to the placebo bottles to mask assignment.
Follow-up and assessment of study endpoints
We followed participants from date of randomization (23 July 1995). Participants were visited daily for pill countingduring H pylori treatment and participants were visited monthly to distribute supplements and count pills during the period of vitamin and garlic supplementation. In addition, we measured serum levels of vitamin E, vitamin C, and S-allylcysteine in randomly selected participants to monitor use of vitamin and garlic supplementation. Data from pill counts and sampled blood assays showed excellent treatment compliance. The initial follow-up ended on 1 May 2003 and the extended follow-up ended on 1 December 2017.
The primary outcomes were gastric cancer incidence and mortality. We also assessed cause specific cancer and cardiovascular disease mortality as secondary outcomes. Incidence of gastric cancer was ascertained from scheduled gastroscopies in 1999 and 2003 for all participants, with biopsy samples taken from seven standard sites; scheduled gastroscopies in 2007 for those with a diagnosis of intestinal metaplasia or dysplasia at any biopsy site in 2003; repeat gastroscopies every six months to one year between 2008 and 2017 for those with a diagnosis of moderate or severe dysplasia at any biopsy site or with mild dysplasia at two or more sites in 2003; or cancer registry or autopsy reports, which were confirmed through medical records. Details of gastroscopy and biopsy procedures and histopathologic criteria are described elsewhere.2 12 We obtained causes of death from the reporting system managed by the Chinese Center for Disease Control and Prevention, which integrates death certificates from hospitals and police and judicial departments in Linqu. To avoid missed records from delayed reporting, a local doctor supervised the follow-up in each village and documented the vital status and occurrence of cancer and major chronic diseases. Staff from Peking University Cancer Hospital visited the villages every three months after 2003 to gather information on gastric cancer incidence and cause specific mortality.
Statistical analysis
In the primary analyses, we examined the risk of gastric cancer incidence and mortality associated with the three interventions. Because gastric cancer was diagnosed in many participants at scheduled gastroscopies in 1999 and 2003, we estimated odds ratios for cumulative incidence of gastric cancer and corresponding 95% confidence intervals. We used conditional logistic regression stratified on baseline histopathology, categorized as moderate chronic atrophic gastritis or less severe gastric lesions, severe chronic atrophic gastritis or superficial intestinal metaplasia, deep intestinal metaplasia, or dysplasia. We adjusted the analyses for other potential confounders, including age, sex, history of ever using alcohol, and history of ever smoking. Conditional logistic regression is helpful when there are only a few participants per stratum, as it eliminates the nuisance intercept, whereas unconditional logistic regression can yield unreliable inference because of the necessity to estimate many intercepts, one per stratum. Our study contained only a few stratums, but as the numbers in each stratum increase, the conditional logistic analysis becomes asymptotically fully efficient. Conditional logistic regression has the additional advantage of paralleling that of stratified Cox regression.
For analysis of gastric cancer mortality, we used the Cox proportional hazards models on the scale of time since randomization to estimate hazard ratios and 95% confidence intervals, stratified on baseline histopathology. The proportional hazards assumption within stratums was tested by including an interaction term between time and treatment (P>0.05 for all tests). In the multivariate adjusted models, Cox regression analyses were further adjusted for age, sex, smoking, and alcohol intake.
Sensitivity analyses included indicators for the other treatments in addition to the treatment being analyzed in the regression models. In secondary analyses, we used the Cox model to assess associations of interventions with all cause mortality and cause specific mortality, including deaths from any cancer, individual cancers with at least 10 deaths among participants who were H pylori positive at baseline, and cardiovascular disease.
For each intervention we plotted Kaplan-Meier survival curves to compare time to all cause mortality and gastric cancer mortality. We further examined the temporal changes in the effects of interventions on cumulative incidence of gastric cancer and on mortality by dividing follow-up into three periods: the initial trial period (from randomization to 1 May 2003),7 the first extended follow-up period (2 May 2003 to 1 August 2010),8 9 and the second extended follow-up period (2 August 2010 to 1 December 2017).
We stratified analyses to determine whether the effects of interventions varied by participants’ baseline histopathology or age. The Q statistic for meta-analysis was used to evaluate heterogeneity of odds ratios or hazard ratios across stratums. To clarify potential effect modification between interventions, we also tested the two way interactions between H pylori treatment, vitamin supplementation, and garlic supplementation on gastric cancer incidence and mortality.
Analyses were performed using the intention-to-treat approach. P values were two tailed. Statistical calculations were performed with SAS statistical software, version 9.4 (SAS institute, Cary, NC).
Patient and public involvement
No patients were involved in setting the research question or the outcome measures, nor were they involved in developing plans for recruitment, design, or implementation of the study. No patients were asked to advise on interpretation or writing of results. Before the trial started, extensive information about gastric cancer was disseminated locally to promote the residents’ participation. Peking University Cancer Hospital has reported and will report the results by publication, presentation at scientific meetings, and public events to promote cancer prevention and control. The results will also be disseminated using social media.
Results
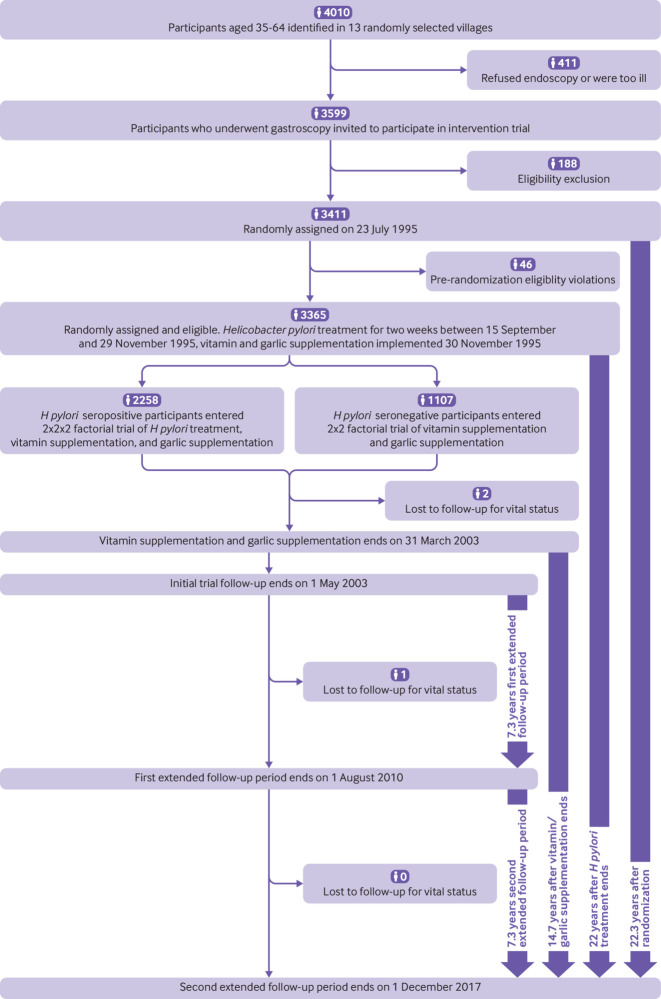
A total of 3365 participants were included in the trial (see supplementary table 2). Block randomized intervention assignments6 ensured balanced distribution in baseline characteristics between treatment and placebo groups for the three interventions. During 22.3 years of follow-up (fig 1), 151 incident cases of gastric cancer and 94 deaths from gastric cancer were identified. Of these, 119 (79%) and 76 (81%), respectively, occurred among participants who were baseline H pylori positive (table 1). Most of the cancers were non-cardia types (see supplementary table 3).
Fig 1.
Flow diagram of trial design and participant follow-up
Table 1.
Number of participants with incident gastric cancer and mortality by intervention groups during trial and extended follow-up*
| Intervention groups | No of participants | Incident gastric cancer | Gastric cancer deaths | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Trial period | Extended follow-up 2003-10 | Extended follow-up 2010-17 | Total No | Trial period | Extended follow-up 2003-10 | Extended follow-up 2010-17 | Total No | |||
| Helicobacter pylori treatment: | ||||||||||
| Active | 1130 | 19 | 15 | 7 | 41 | 8 | 10 | 11 | 29 | |
| Placebo | 1128 | 28 | 24 | 26 | 78 | 10 | 14 | 23 | 47 | |
| Total | 2258 | 47 | 39 | 33 | 119 | 18 | 24 | 34 | 76 | |
| Vitamin supplementation: | ||||||||||
| Active | 1677 | 29 | 19 | 12 | 60 | 9 | 8 | 14 | 31 | |
| Placebo | 1688 | 30 | 28 | 33 | 91 | 12 | 18 | 33 | 63 | |
| Total | 3365 | 59 | 47 | 45 | 151 | 21 | 26 | 47 | 94 | |
| Garlic supplementation: | ||||||||||
| Active | 1678 | 30 | 19 | 20 | 69 | 12 | 9 | 18 | 39 | |
| Placebo | 1687 | 29 | 28 | 25 | 82 | 9 | 17 | 29 | 55 | |
| Total | 3365 | 59 | 47 | 45 | 151 | 21 | 26 | 47 | 94 | |
Events from date of randomization to end of initial follow-up (23 July 1995 to 1 May 2003). Number of cases during trial period and first extended follow-up period are described in Ma et al.8
H pylori treatment was inversely associated with risk of gastric cancer, even after multivariate adjustment (odds ratio 0.48, 95% confidence interval 0.32 to 0.71) (table 2). Incidence decreased significantly with vitamin supplementation but not with garlic supplementation (0.64, 0.46 to 0.91 and 0.81, 0.57 to 1.13, respectively).
Table 2.
Odds ratios (95% confidence intervals) for incidence of gastric cancer by Helicobacter pylori treatment, and vitamin and garlic supplementation
| Interventions | Adjusted for baseline histology | Fully adjusted* | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Placebo (No with event/No in group) | Treatment (No with event/No in group) | Odds ratio (95% CI) | P value | Placebo (No with event/No in group) | Treatment (No with event/No in group) | Odds ratio (95% CI) | P value | ||
| H pylori treatment | 78/1123 | 40/1119 | 0.48 (0.33 to 0.72) | <0.001 | 76/1086 | 40/1086 | 0.48 (0.32 to 0.71) | <0.001 | |
| Vitamin supplementation | 90/1679 | 60/1665 | 0.66 (0.47 to 0.92) | 0.02 | 89/1627 | 58/1610 | 0.64 (0.46 to 0.91) | 0.01 | |
| Garlic supplementation | 82/1678 | 68/1666 | 0.82 (0.58 to 1.14) | 0.23 | 81/1631 | 66/1606 | 0.81 (0.57 to 1.13) | 0.22 | |
Number of participants and number of gastric cancer cases is lower than in table 1 because of missing information on baseline histology or other covariates.
Adjusted for baseline histology (moderate chronic atrophic gastritis or less severe gastric lesions, severe chronic atrophic gastritis or superficial intestinal metaplasia, deep intestinal metaplasia, or dysplasia), age, sex, history of ever using alcohol, and history of ever smoking.
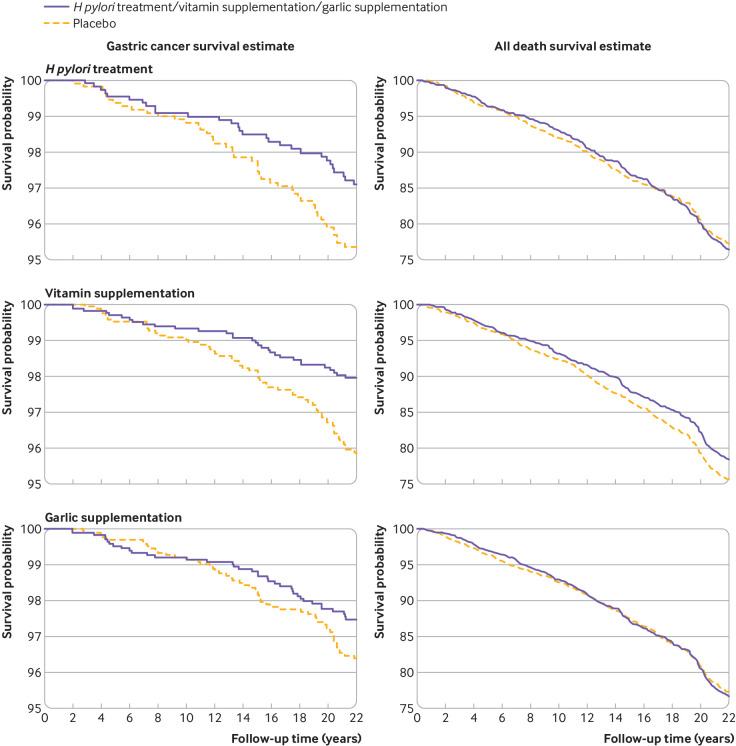
A statistically significant protective effect on gastric cancer mortality was observed for all three interventions: fully adjusted hazard ratio was 0.62 (95% confidence interval 0.39 to 0.99) for H pylori treatment, 0.48 (0.31 to 0.75) for vitamin supplementation, and 0.66 (0.43 to 1.00) for garlic supplementation (table 3). Kaplan-Meier curves showed that the cumulative protective effect on gastric cancer mortality became evident after about eight years for H pylori treatment and vitamin supplementation and after about 12 years for garlic supplementation (fig 2). For both gastric cancer incidence and mortality, sensitivity analyses adjusted for other interventions yielded similar findings (data not shown).
Table 3.
Hazard ratios (95% confidence intervals) for cause specific death by Helicobacter pylori treatment, and vitamin and garlic supplementation
| Causes of death by intervention | Adjusted for baseline histology only | Fully adjusted* | |||||||
|---|---|---|---|---|---|---|---|---|---|
| No in placebo group | No in treatment group | Hazard ratio (95% CI) | P value | No in placebo group | No in treatment group | Hazard ratio (95% CI) | P value | ||
| H pylori treatment: | 1123 | 1119 | 1086 | 1086 | |||||
| Total No of deaths | 272 | 264 | 0.98 (0.83 to 1.16) | 0.79 | 254 | 245 | 1.00 (0.84 to 1.19) | 0.96 | |
| Cause specific deaths: | |||||||||
| All cancer† | 141 | 115 | 0.81 (0.63 to 1.04) | 0.10 | 131 | 105 | 0.81 (0.62 to 1.05) | 0.10 | |
| Gastric cancer | 47 | 29 | 0.62 (0.39 to 0.99) | 0.04 | 45 | 29 | 0.62 (0.39 to 0.99) | 0.05 | |
| Esophageal cancer | 12 | 14 | 1.17 (0.54 to 2.53) | 0.69 | 10 | 11 | 1.12 (0.47 to 2.64) | 0.80 | |
| Liver cancer | 11 | 21 | 1.93 (0.93 to 4.01) | 0.08 | 10 | 18 | 1.78 (0.82 to 3.86) | 0.15 | |
| Colorectal cancer | 12 | 3 | 0.25 (0.07 to 0.89) | 0.03 | 10 | 3 | 0.30 (0.08 to 1.10) | 0.07 | |
| Lung cancer | 40 | 33 | 0.83 (0.52 to 1.31) | 0.42 | 38 | 31 | 0.82 (0.51 to 1.32) | 0.42 | |
| Other cancer | 19 | 15 | 0.79 (0.40 to 1.56) | 0.50 | 18 | 13 | 0.73 (0.36 to 1.50) | 0.40 | |
| Cardiovascular disease | 96 | 106 | 1.11 (0.84 to 1.47) | 0.45 | 90 | 100 | 1.17 (0.88 to 1.55) | 0.29 | |
| Other | 35 | 43 | 1.24 (0.79 to 1.93) | 0.35 | 33 | 40 | 1.27 (0.80 to 2.01) | 0.31 | |
| Vitamin supplementation | 1679 | 1665 | 1627 | 1610 | |||||
| Total No of deaths | 423 | 370 | 0.86 (0.75 to 0.99) | 0.04 | 392 | 345 | 0.87 (0.76 to 1.01) | 0.07 | |
| Cause specific deaths: | |||||||||
| All cancer† | 187 | 166 | 0.89 (0.72 to 1.09) | 0.26 | 175 | 152 | 0.88 (0.71 to 1.09) | 0.23 | |
| Gastric cancer | 62 | 31 | 0.49 (0.32 to 0.76) | 0.001 | 61 | 29 | 0.48 (0.31 to 0.75) | 0.001 | |
| Esophageal cancer | 18 | 15 | 0.84 (0.42 to 1.67) | 0.62 | 16 | 12 | 0.77 (0.36 to 1.63) | 0.50 | |
| Liver cancer | 21 | 25 | 1.20 (0.67 to 2.15) | 0.53 | 18 | 24 | 1.38 (0.75 to 2.55) | 0.30 | |
| Colorectal cancer | 11 | 10 | 0.92 (0.39 to 2.17) | 0.85 | 10 | 8 | 0.81 (0.32 to 2.06) | 0.66 | |
| Lung cancer | 49 | 56 | 1.16 (0.79 to 1.70) | 0.46 | 44 | 53 | 1.23 (0.83 to 1.84) | 0.30 | |
| Other cancer | 26 | 29 | 1.13 (0.66 to 1.91) | 0.66 | 26 | 26 | 1.02 (0.59 to 1.76) | 0.94 | |
| Cardiovascular disease | 168 | 141 | 0.84 (0.67 to 1.05) | 0.12 | 156 | 132 | 0.84 (0.67 to 1.06) | 0.14 | |
| Other | 68 | 63 | 0.93 (0.66 to 1.32) | 0.70 | 61 | 61 | 1.02 (0.71 to 1.45) | 0.92 | |
| Garlic supplementation: | 1678 | 1666 | 1631 | 1606 | |||||
| Total No of deaths | 406 | 387 | 0.96 (0.83 to 1.10) | 0.53 | 383 | 354 | 0.90 (0.78 to 1.04) | 0.17 | |
| Cause specific deaths: | |||||||||
| All cancer† | 185 | 168 | 0.91 (0.74 to 1.12) | 0.36 | 175 | 152 | 0.87 (0.70 to 1.08) | 0.19 | |
| Gastric cancer | 55 | 38 | 0.69 (0.46 to 1.04) | 0.08 | 54 | 36 | 0.66 (0.43 to 1.00) | 0.05 | |
| Esophageal cancer | 18 | 15 | 0.82 (0.42 to 1.64) | 0.58 | 16 | 12 | 0.78 (0.37 to 1.65) | 0.51 | |
| Liver cancer | 22 | 24 | 1.11 (0.62 to 1.98) | 0.73 | 19 | 23 | 1.26 (0.69 to 2.32) | 0.46 | |
| Colorectal cancer | 11 | 10 | 0.93 (0.40 to 2.19) | 0.87 | 11 | 7 | 0.63 (0.24 to 1.64) | 0.34 | |
| Lung cancer | 54 | 51 | 0.95 (0.65 to 1.39) | 0.79 | 51 | 46 | 0.91 (0.61 to 1.36) | 0.66 | |
| Other cancer | 25 | 30 | 1.22 (0.72 to 2.07) | 0.47 | 24 | 28 | 1.21 (0.70 to 2.08) | 0.50 | |
| Cardiovascular disease | 152 | 157 | 1.04 (0.83 to 1.30) | 0.74 | 142 | 146 | 1.04 (0.83 to 1.31) | 0.72 | |
| Other | 69 | 62 | 0.90 (0.64 to 1.26) | 0.53 | 66 | 56 | 0.86 (0.60 to 1.23) | 0.40 | |
Number of participants and number of gastric cancer cases is lower than in table 1 because of missing information on baseline histology or other covariates.
Adjusted for baseline histology (moderate chronic atrophic gastritis or less severe gastric lesions, severe chronic atrophic gastritis or superficial intestinal metaplasia, deep intestinal metaplasia, or dysplasia), age, sex, history of ever using alcohol, and history of ever smoking.
Individual cancers with at least 10 deaths among baseline H pylori positive participants.
Fig 2.
Kaplan-Meier survival estimates for gastric cancer mortality and total mortality by Helicobacter pylori treatment, vitamin supplementation, and garlic supplementation. Follow-up time is from trial randomization
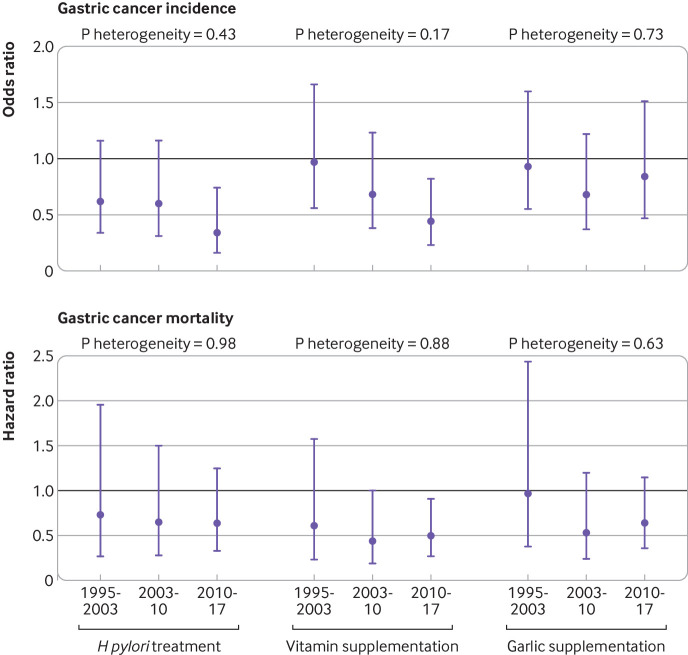
Separate analyses for the three follow-up periods did not show statistically significant heterogeneity in treatment effects in odds ratios for gastric cancer incidence or hazard ratios for gastric cancer mortality (fig 3), possibly owing to limited power. The effects from garlic supplementation were, however, negligible in the initial trial period for both gastric cancer incidence and gastric cancer mortality, and effects only became apparent by 14.7 years and persisted during the 22.3 years of follow-up. The treatment effect for vitamin supplementation in the initial trial period was also negligible for gastric cancer incidence but not for gastric cancer mortality.
Fig 3.
Association of Helicobacter pylori treatment, vitamin supplementation, and garlic supplementation with gastric cancer incidence and mortality during three periods (trial period 23 July 1995 to 1 May 2003, first extended follow-up period 2 May 2003 to 1 August 2010, and second extended follow-up period 2 August 2010 to 1 December 2017). Analyses were adjusted for baseline histology (moderate chronic atrophic gastritis or less severe gastric lesions, severe chronic atrophic gastritis or superficial intestinal metaplasia, deep intestinal metaplasia, dysplasia), age, sex, history of ever using alcohol, and history of ever smoking. Whiskers represent 95% confidence intervals
In secondary analyses (table 3), vitamin supplementation was marginally associated with decreased all cause mortality (hazard ratio 0.87, 0.76 to 1.01, P=0.07). No statistically significant associations were found for all cancer mortality or esophageal cancer specific mortality. H pylori treatment was marginally associated with a decrease in risk of colorectal cancer mortality (P=0.07) and a non-significant increase in liver cancer mortality (P=0.15). The associations with other specific causes of death were also non-significant (table 3).
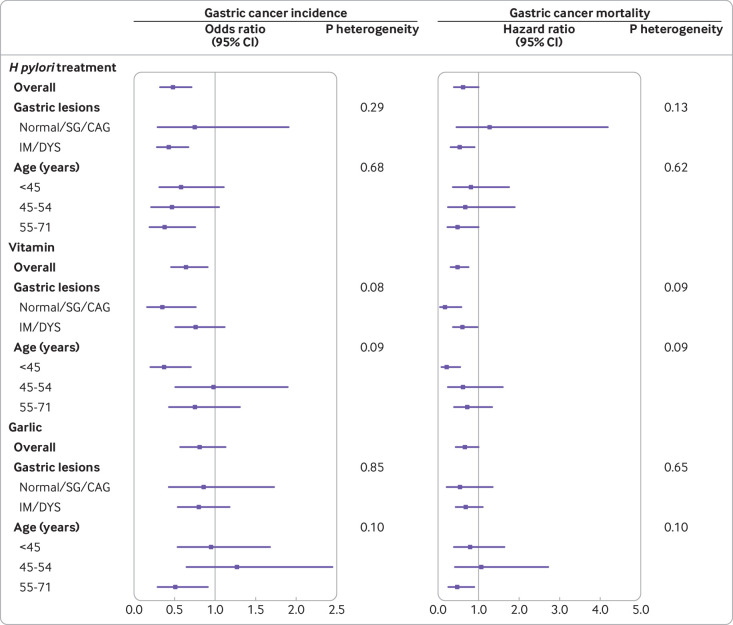
No statistically significant evidence of heterogeneity was found in the effects of H pylori treatment or garlic supplementation for gastric cancer incidence or mortality among participants with differing baseline histopathology, or among different age groups. Although tests for heterogeneity were only marginally significant for vitamin supplementation, the data suggest a greater preventive effect for those with favorable baseline histology (normal, superficial gastritis, chronic atrophic gastritis) and those younger than 45 years, for both gastric cancer incidence and mortality (fig 4).
Fig 4.
Association of Helicobacter pylori treatment, vitamin supplementation, and garlic supplementation with gastric cancer incidence and mortality, stratified by baseline gastric lesions and age. Analyses were adjusted for baseline histology (moderate chronic atrophic gastritis or less severe gastric lesions, severe chronic atrophic gastritis or superficial intestinal metaplasia, deep intestinal metaplasia, dysplasia), age, sex, history of ever using alcohol, and history of ever smoking. SG=superficial gastritis; CAG=chronic atrophic gastritis; IM=intestinal metaplasia; DYS=dysplasia
We tested two way interactions for treatment effects. Among baseline H pylori seronegative participants, a non-significant indication suggested that participants who only took vitamin supplements had a lower incidence of gastric cancer than those who took vitamin or garlic supplements (P for interaction=0.08) (see supplementary table 4). These interaction tests were not adjusted for multiple comparisons, however, and were not nominally statistically significant.
Discussion
In the Shandong Intervention Trial, the preventive effect of short term treatment (two weeks) for Helicobacter pylori infection on risk of gastric cancer continued 22 years post-treatment and was associated with statistically significant fewer deaths due to gastric cancer. We also found a significantly decreased long term risk of gastric cancer associated with vitamin supplementation and a reduced risk of gastric cancer mortality with vitamin or garlic supplementation.
Principal findings and comparison with other studies
Previous intervention trials7 8 9 13 14 15 16 17 18 and recent studies19 20 have examined the effect of H pylori treatment on gastric cancer. Although treatment is recognized as a potential strategy for the prevention of gastric cancer,11 21 major uncertainties require clarification before the strategy can be implemented at community level. As the development of gastric cancer involves progression through multiple histologic stages, the duration of effectiveness of H pylori treatment needs to be studied by long term follow-up.22 Our findings confirm the statistically significant reduction in gastric cancer incidence and favorable although statistically non-significant reduction in gastric cancer mortality after 14.7 years,8 indicating an even greater beneficial effect of H pylori treatment on incidence of gastric cancer than we previously reported at 14.7 years (odds ratio 0.61, 95% confidence interval 0.38 to 0.96).8 The reduction in gastric cancer incidence in the Shandong Intervention Trial was also larger than in recent meta-analyses of intervention trials.23 24 As more gastric cancer deaths occurred during longer follow-up, the reduction in gastric cancer mortality became statistically significant 22.3 years after intervention, although the effect became visible in Kaplan-Meier curves after roughly eight years.
Gaps remain about the full range of beneficial and adverse effects from H pylori treatment. An inverse association of H pylori infection with esophageal adenocarcinoma has been reported.11 25 26 Although uncertainty remains for esophageal squamous cell carcinoma, a meta-analysis found a decreased risk of this cancer associated with H pylori infection in eastern populations.26 The Shandong Intervention Trial provided few events and had little power to detect effects of H pylori treatment on esophageal cancer mortality and cannot distinguish esophageal squamous cell carcinoma from esophageal adenocarcinoma (rare in this region); however, there is little indication of adverse risk. An increased risk of colorectal cancer associated with H pylori infection has also been reported.27 Our study found a reduction in deaths due to colorectal cancer with H pylori treatment, but the number was too small to confirm this effect. In addition, we found a non-significant excess of deaths due to liver cancer with H pylori treatment. Despite prolonged follow-up in our trial, the sample size for H pylori treatment (n=2242) limited our ability to estimate the benefits and risks for many health outcomes.
Whether a point exists in H pylori associated gastric carcinogenesis after which treatment would be too late to reduce the risk of gastric cancer is still debatable, as H pylori infection is linked to early precancerous histopathologic changes.12 The Maastricht V/Florence consensus report stated that H pylori eradication results in a clear improvement of gastritis and gastric atrophy but not of intestinal metaplasia.28 A trial also showed that eradication of H pylori did not reduce the incidence of intestinal metaplasia or decrease its histological severity.29 However, the consensus report also recognized that the progression of intestinal metaplasia can be halted by eradicationof H pylori,28 as supported by our intervention trial.7 Advanced gastric lesions occur more often at old ages,2 12 which raises concerns about the effectiveness of prophylactic H pylori eradication among those with advanced gastric lesions and older people. Such concerns have been partly addressed by evidence that H pylori treatment reduces the incidence of metachronous gastric cancer,20 30 but other reports on new gastric cancer with precancerous lesions or metachronous gastric cancer have been contradictory,15 31 and some experts recommend using H pylori treatment only before gastric atrophy or intestinal metaplasia develops.15 Our long term data confirm the earlier finding of the Shandong Intervention Trial9 that H pylori treatment reduces gastric cancer incidence and mortality also in participants with intestinal metaplasia and dysplasia and in those aged 55-71 years at baseline. Thus H pylori infection might promote late stage neoplastic progression. It is also possible that H pylori treatment eliminates non-H pylori bacteria crucial for progression to gastric cancer,9 32 supporting the need to explore other microbiota underlying gastric carcinogenesis. Regardless, H pylori treatment is potentially useful for old as well as young people and for those with advanced as well as early precancerous gastric lesions.
Few intervention trials have been conducted in populations with nutritional deficiencies. The Linxian Nutrition Intervention Trial showed a durable beneficial effect from supplementation for 5.25 years with a combination of selenium, vitamin E, and beta-carotene (“factor D”) on total and gastric cancer mortality, which lasted up to 10 years post-trial but subsequently waned.33 34 35 In Linqu, where the Shandong Intervention Trial was conducted, the mean serum levels of vitamin C and selenium were well below reference ranges.3 36 In this nutritionally deprived population, observational studies showed that the risk of gastric cancer was inversely associated with vitamin C intake.5 A high level of serum vitamin C was also associated with a decreased risk of histologic progression to dysplasia and gastric cancer in Linqu.3 Our previous follow-up for 14.7 years revealed noteworthy, but not statistically significant, reductions in gastric cancer incidence and mortality. Thus, the statistically significant reductions in gastric cancer incidence and mortality after 22.3 years are supported by earlier clinical trial data and observational studies. A marginally significant indication showed that vitamin supplementation is more effective in those with mild histopathology at baseline and younger than 45 years. Similarly, only participants aged less than 55 years benefited from factor D in the Linxian Nutrition Intervention Trial.34
Observational data show a decreased risk of gastric cancer with increased consumption of garlic and allium vegetables in Linqu12 and elsewhere.37 Garlic and its derivatives have antioxidative, antimicrobial, and immune modulation properties.38 39 However, few long term randomized placebo controlled intervention trials have utilized dietary or supplemental allium vegetables for cancer prevention. One trial indicated that aged garlic extract prevented metachronous colorectal adenomas,40 whereas another revealed a statistically significant protective effect of synthetic diallyl trisulfide (allitridum) combined with selenium on gastric cancer incidence in men but not in women.41 After 22.3 years, garlic supplementation led to a non-statistically significant reduction in gastric cancer incidence and a statistically significant reduction in gastric cancer mortality, confirming favorable, but non-statistically significant trends seen at 14.7 years.8
The time course and duration of protective effects is of interest. H pylori treatment was associated with retardation in the progression of precancerous gastric lesions,7 and evidence began to accumulate for protective effects on gastric cancer incidence and mortality in the initial trial period. The beneficial effects on gastric cancer incidence and mortality persisted during 14.7 years8 and again through 22.3 years (fig 3). Neither vitamin nor garlic supplementation significantly retarded histopathologic progression during the initial trial, ending at 2003.7 Vitamin supplementation showed favorable (but not statistically significant) effects on gastric cancer mortality during the trial period; these effects persisted during the extended follow-up over 14.7 and 22.3 years (fig 3). Favorable effects of vitamin supplementation on gastric cancer incidence appeared late but were apparent during the extended follow-up of 14.7 years and persisted. Garlic supplementation first showed favorable effects on gastric cancer incidence and mortality during the extended follow-up of 14.7 years; these effects also persisted. In Kaplan-Meier plots, we also observed that the effects on gastric cancer mortality became apparent after about eight years for H pylori treatment and vitamin supplementation and after about 12 years for garlic supplementation (fig 4). The mechanisms for these time patterns in treatment effects remain to be elucidated.
Although H pylori treatment represents a promising approach to prevention of gastric cancer, it did not eliminate gastric cancer incidence or mortality altogether, and some H pylori strains might become resistant to antibiotics. Other preventive modalities such as vitamin and garlic supplementation are of potential value. Because we found no evidence of negative interactions between H pylori treatment and the supplements, it is likely that combinations of these interventions can further reduce gastric cancer incidence and mortality. Even though nutritional and garlic supplements could take years to impact on gastric cancer incidence and mortality, they might prove less expensive, safe, and robust interventions in the long run.
Strengths and limitations of this study
Strengths of the Shandong Intervention Trial included excellent treatment compliance and long term follow-up, with virtually complete ascertainment of people with gastric cancer and cause specific deaths in a well defined high risk population. The study does, however, have several limitations. Firstly, the numbers of events were too small to be convincing for some causes of death in secondary analyses and also restricted the power for detailed subgroup and interaction analyses for gastric cancer. We do not have the information on cardia or non-cardia cancer for all people with gastric cancer, and the limited number precluded an analysis of cardia gastric cancer separately. Secondly, we cannot disentangle the effect of particular components of vitamin and garlic supplements or characterize a dose-response relation. Thirdly, we did not have information on participants’ H pylori infection status, non-trial treatments for H pylori, or nutritional and garlic supplementation after the trial ended in 2003. Although social and economic changes have occurred in China since 2003 and some participants might have changed their diets or lifestyles, it is unlikely that these changes would have differed by initial intervention assignment, because of the randomized masked trial design. Even so, studies are warranted to explore potential effects of changes in lifestyles and non-trial use of H pylori treatment or nutritional supplements. Fourthly, we conducted scheduled gastroscopies for participants during the trial period and for those with advanced gastric lesions during the extended follow-up. Ascertainment bias is unlikely during the trial period. However, a group with more advanced lesions in 2003 had a greater chance of endoscopically ascertained gastric cancer in extended follow-up. This could pertain to the placebo group for H pylori treatment, as such treatment, but not other interventions, retarded progression of gastric lesions.7 This could result in slight overestimates of the protective effect of H pylori treatment. Such bias is likely to be small, however, because most incident gastric cancer was diagnosed during the trial or through hospital records and not by trial prescribed endoscopy during extended follow-up. Fifthly, our study population was from a high risk rural area with nutritional deficiencies. Although the findings might have implications for populations worldwide, extrapolation to a well nourished population or a population with low incidence of gastric cancer might be problematic.
Conclusions and policy implications
We found statistically significantly decreased risks of gastric cancer incidence and mortality with short term H pylori treatment during 22.3 years of follow-up, showing the longest durable beneficial effect among the major randomized trials of H pylori treatment. Multiyear vitamin supplementation yielded statistically significant reductions in gastric cancer incidence and mortality. Garlic supplementation also yielded a statistically significant decrease in gastric cancer mortality and a promising, but not statistically significant, decrease in gastric cancer incidence. These findings suggest many potential strategies for gastric cancer prevention. However, before major public health campaigns for gastric cancer prevention are launched utilizing antibiotic based H pylori treatment or nutritional regimens, further large scale intervention trials are warranted to delineate the full range of beneficial and adverse effects of H pylori treatment, to confirm the preventive effects of vitamin and garlic supplementation, and to identify possible risks from nutritional regimens.
What is already known on this topic
Helicobacter pylori infection is an established risk factor for gastric cancer and H pylori eradication could be a potential strategy for preventing gastric cancer
The duration of effectiveness of H pylori treatment on gastric cancer prevention and the related full range of beneficial and adverse effects needs to be studied by long term follow-up
Few nutrition intervention trials have been done in populations with nutritional deficiencies, whereas nutrition supplementation effects on gastric cancer need to be assessed with long term follow-up
What this study adds
Short term H pylori treatment was associated with a significantly decreased risk of gastric cancer incidence and mortality during 22.3 years of follow-up and was not significantly associated with total mortality or other major cancer specific mortality
Both vitamin (C, E, and selenium) and garlic (extract and oil) supplementation for 7.3 years yielded statistically significant reductions in gastric cancer mortality, whereas a favorable effect of long term vitamin supplementation on gastric cancer incidence was also observed
These findings offer potential opportunities for gastric cancer prevention, but further large scale intervention trials are required to confirm the favorable effects of vitamin and garlic supplementation and to identify any possible risks of H pylori treatment, and vitamin and garlic supplementation
Acknowledgments
We thank Joseph F Fraumeni Jr (National Cancer Institute) for his help before and during the trial period; the residents, field staff, and government of Linqu County for supporting this trial; Wakunaga of America for performing assays of S-allyl cysteine and providing garlic supplements; Shanghai Squibb for providing vitamin supplements; and Astra Corporation for providing amoxicillin and omeprazole. These study sponsors attended a planning meeting in April 2005 at which elements of the protocol and provision of intervention materials were discussed, but these sponsors did not write or approve the protocol, participate in data collection (apart from providing assays for S-allyl cysteine), interpret the data, participate in writing this article, or influence the decision to submit this article for publication. We also thank members of the data safety and monitoring committee for guidance and oversight during the trial. This trial is also listed on the National Cancer Institute’s Physician Data Query database (No NCI-OH-95-C-N029; www.cancer.gov/clinicaltrials).
Web extra.
Extra material supplied by authors
Supplementary information: additional tables 1-4
Contributors: WQL, KFP, and WCY were conceived and designed the study. WQL, JYZ, YG, KFP, and WCY acquired, analyzed, and interpreted the data. WQL and JYZ wrote the initial draft of the manuscript. WQL and JYZ contributed equally to this paper. All the authors were involved in preparing this manuscript and contributed to the critical revision of the manuscript. WQL, KFP, and WCY are guarantors. WCY supervised the study. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria were omitted.
Funding: This study was supported by the Intramural Research Program of the National Institutes of Health, National Cancer Institute, and in part by National Cancer Institute contracts NO2-CP-71103 and NO2-CP-21169. Additional support was from the National Basic Research Program of China (973 program: 2004CB518702 and 2010CB529303). The funding sources had no role in the study design; collection, analysis, and interpretation of data; writing of the report; or decision to submit the article for publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: The original trial and study extension were approved by review boards of Peking University Cancer Hospital, and the US National Cancer Institute, and participants provided written informed consent.
Data sharing: Further information on the trial design and follow-up available on request.
The lead author (WQL, KFP, and WCY) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
References
- 1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394-424. 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2. You WC, Blot WJ, Chang YS, et al. Diet and high risk of stomach cancer in Shandong, China. Cancer Res 1988;48:3518-23. [PubMed] [Google Scholar]
- 3. You WC, Zhang L, Gail MH, et al. Gastric dysplasia and gastric cancer: Helicobacter pylori, serum vitamin C, and other risk factors. J Natl Cancer Inst 2000;92:1607-12. 10.1093/jnci/92.19.1607. [DOI] [PubMed] [Google Scholar]
- 4. Zhang L, Blot WJ, You WC, et al. Helicobacter pylori antibodies in relation to precancerous gastric lesions in a high-risk Chinese population. Cancer Epidemiol Biomarkers Prev 1996;5:627-30. [PubMed] [Google Scholar]
- 5. You WC, Blot WJ, Chang YS, et al. Diet and high risk of stomach cancer in Shandong, China. Cancer Res 1988;48:3518-23. 10.1016/0168-8510(90)90388-T. [DOI] [PubMed] [Google Scholar]
- 6. Gail MH, You WC, Chang YS, et al. Factorial trial of three interventions to reduce the progression of precancerous gastric lesions in Shandong, China: design issues and initial data. Control Clin Trials 1998;19:352-69. 10.1016/S0197-2456(98)00016-6. [DOI] [PubMed] [Google Scholar]
- 7. You WC, Brown LM, Zhang L, et al. Randomized double-blind factorial trial of three treatments to reduce the prevalence of precancerous gastric lesions. J Natl Cancer Inst 2006;98:974-83. 10.1093/jnci/djj264. [DOI] [PubMed] [Google Scholar]
- 8. Ma JL, Zhang L, Brown LM, et al. Fifteen-year effects of Helicobacter pylori, garlic, and vitamin treatments on gastric cancer incidence and mortality. J Natl Cancer Inst 2012;104:488-92. 10.1093/jnci/djs003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Li WQ, Ma JL, Zhang L, et al. Effects of Helicobacter pylori treatment on gastric cancer incidence and mortality in subgroups. J Natl Cancer Inst 2014;106:dju116. 10.1093/jnci/dju116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Herrero R, Parsonnet J, Greenberg ER. Prevention of gastric cancer. JAMA 2014;312:1197-8. 10.1001/jama.2014.10498. [DOI] [PubMed] [Google Scholar]
- 11.Helicobacter pylori eradication as a strategy for preventing gastric cancer. IARC working group reports www.iarc.fr/en/publications/pdfs-online/wrk/wrk8/index.php
- 12. You WC, Li JY, Blot WJ, et al. Evolution of precancerous lesions in a rural Chinese population at high risk of gastric cancer. Int J Cancer 1999;83:615-9. [DOI] [PubMed] [Google Scholar]
- 13. Correa P, Fontham ET, Bravo JC, et al. Chemoprevention of gastric dysplasia: randomized trial of antioxidant supplements and anti-helicobacter pylori therapy. J Natl Cancer Inst 2000;92:1881-8. 10.1093/jnci/92.23.1881. [DOI] [PubMed] [Google Scholar]
- 14. Leung WK, Lin SR, Ching JY, et al. Factors predicting progression of gastric intestinal metaplasia: results of a randomised trial on Helicobacter pylori eradication. Gut 2004;53:1244-9. 10.1136/gut.2003.034629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wong BC, Lam SK, Wong WM, et al. China Gastric Cancer Study Group Helicobacter pylori eradication to prevent gastric cancer in a high-risk region of China: a randomized controlled trial. JAMA 2004;291:187-94. 10.1001/jama.291.2.187. [DOI] [PubMed] [Google Scholar]
- 16. Wong BC, Zhang L, Ma JL, et al. Effects of selective COX-2 inhibitor and Helicobacter pylori eradication on precancerous gastric lesions. Gut 2012;61:812-8. 10.1136/gutjnl-2011-300154. [DOI] [PubMed] [Google Scholar]
- 17. Saito D, Boku N, Fujioka T, et al. Impact of H-pylori eradication on gastric cancer prevention: Endoscopic results of the Japanese intervention trial (JITHP-study). A Randomized multi-center trial. Gastroenterology 2005;128:A4 http://apps.webofknowledge.com/full_record.do?product=UA&search_mode=GeneralSearch&qid=1&SID=7BNunrXU4HfMV4sD5Uw&page=1&doc=1 [Google Scholar]
- 18. Zhou L. Ten-year follow-up study on the incidence of gastric cancer and the pathological changes of gastric mucosa after H. pylori eradication in China. Gastroenterology 2008;134:A233-233. 10.1016/S0016-5085(08)61077-X www.sciencedirect.com/science/article/pii/S001650850861077X [DOI] [Google Scholar]
- 19. Leung WK, Wong IOL, Cheung KS, et al. Effects of Helicobacter pylori Treatment on Incidence of Gastric Cancer in Older Individuals. Gastroenterology 2018;155:67-75. 10.1053/j.gastro.2018.03.028. [DOI] [PubMed] [Google Scholar]
- 20. Choi IJ, Kook MC, Kim YI, et al. Helicobacter pylori Therapy for the Prevention of Metachronous Gastric Cancer. N Engl J Med 2018;378:1085-95. 10.1056/NEJMoa1708423. [DOI] [PubMed] [Google Scholar]
- 21. Suzuki H, Matsuzaki J. Gastric cancer: evidence boosts Helicobacter pylori eradication. Nat Rev Gastroenterol Hepatol 2018;15:458-60. 10.1038/s41575-018-0023-8. [DOI] [PubMed] [Google Scholar]
- 22. Correa P. Human gastric carcinogenesis: a multistep and multifactorial process--First American Cancer Society Award Lecture on Cancer Epidemiology and Prevention. Cancer Res 1992;52:6735-40. [PubMed] [Google Scholar]
- 23. Ford AC, Forman D, Hunt RH, Yuan Y, Moayyedi P. Helicobacter pylori eradication therapy to prevent gastric cancer in healthy asymptomatic infected individuals: systematic review and meta-analysis of randomised controlled trials. BMJ 2014;348:g3174. 10.1136/bmj.g3174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lee YC, Chiang TH, Chou CK, et al. Association Between Helicobacter pylori Eradication and Gastric Cancer Incidence: A Systematic Review and Meta-analysis. Gastroenterology 2016;150:1113-1124.e5. 10.1053/j.gastro.2016.01.028. [DOI] [PubMed] [Google Scholar]
- 25. Graham DY. Helicobacter pylori update: gastric cancer, reliable therapy, and possible benefits. Gastroenterology 2015;148:719-31.e3. 10.1053/j.gastro.2015.01.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Xie FJ, Zhang YP, Zheng QQ, et al. Helicobacter pylori infection and esophageal cancer risk: an updated meta-analysis. World J Gastroenterol 2013;19:6098-107. 10.3748/wjg.v19.i36.6098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Butt J, Varga MG, Blot WJ, et al. Serological response to Helicobacter pylori proteins associated with risk of colorectal cancer among diverse populations in the United States. Gastroenterology 2019;156:175-186.e2. 10.1053/j.gastro.2018.09.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Malfertheiner P, Megraud F, O’Morain CA, et al. European Helicobacter and Microbiota Study Group and Consensus panel Management of Helicobacter pylori infection-the Maastricht V/Florence Consensus Report. Gut 2017;66:6-30. 10.1136/gutjnl-2016-312288. [DOI] [PubMed] [Google Scholar]
- 29. Lee YC, Chen TH, Chiu HM, et al. The benefit of mass eradication of Helicobacter pylori infection: a community-based study of gastric cancer prevention. Gut 2013;62:676-82. 10.1136/gutjnl-2012-302240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Fukase K, Kato M, Kikuchi S, et al. Japan Gast Study Group Effect of eradication of Helicobacter pylori on incidence of metachronous gastric carcinoma after endoscopic resection of early gastric cancer: an open-label, randomised controlled trial. Lancet 2008;372:392-7. 10.1016/S0140-6736(08)61159-9. [DOI] [PubMed] [Google Scholar]
- 31. Choi J, Kim SG, Yoon H, et al. Eradication of Helicobacter pylori after endoscopic resection of gastric tumors does not reduce incidence of metachronous gastric carcinoma. Clin Gastroenterol Hepatol 2014;12:793-800.e1. 10.1016/j.cgh.2013.09.057. [DOI] [PubMed] [Google Scholar]
- 32. Freedberg DE, Abrams JA, Wang TC. Prevention of gastric cancer with antibiotics: can it be done without eradicating Helicobacter pylori? J Natl Cancer Inst 2014;106:dju148. 10.1093/jnci/dju148. [DOI] [PubMed] [Google Scholar]
- 33. Blot WJ, Li JY, Taylor PR, et al. Nutrition intervention trials in Linxian, China: supplementation with specific vitamin/mineral combinations, cancer incidence, and disease-specific mortality in the general population. J Natl Cancer Inst 1993;85:1483-92. 10.1093/jnci/85.18.1483. [DOI] [PubMed] [Google Scholar]
- 34. Qiao YL, Dawsey SM, Kamangar F, et al. Total and cancer mortality after supplementation with vitamins and minerals: follow-up of the Linxian General Population Nutrition Intervention Trial. J Natl Cancer Inst 2009;101:507-18. 10.1093/jnci/djp037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Wang SM, Taylor PR, Fan JH, et al. Effects of Nutrition Intervention on Total and Cancer Mortality: 25-Year Post-trial Follow-up of the 5.25-Year Linxian Nutrition Intervention Trial. J Natl Cancer Inst 2018;110:1229-38. 10.1093/jnci/djy043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Zhang L, Blot WJ, You WC, et al. Serum micronutrients in relation to pre-cancerous gastric lesions. Int J Cancer 1994;56:650-4. 10.1002/ijc.2910560508. [DOI] [PubMed] [Google Scholar]
- 37. Zhou Y, Zhuang W, Hu W, Liu GJ, Wu TX, Wu XT. Consumption of large amounts of Allium vegetables reduces risk for gastric cancer in a meta-analysis. Gastroenterology 2011;141:80-9. 10.1053/j.gastro.2011.03.057. [DOI] [PubMed] [Google Scholar]
- 38. Nicastro HL, Ross SA, Milner JA. Garlic and onions: their cancer prevention properties. Cancer Prev Res (Phila) 2015;8:181-9. 10.1158/1940-6207.CAPR-14-0172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Pan Y, Lin S, Xing R, et al. Epigenetic Upregulation of Metallothionein 2A by Diallyl Trisulfide Enhances Chemosensitivity of Human Gastric Cancer Cells to Docetaxel Through Attenuating NF-κB Activation. Antioxid Redox Signal 2016;24:839-54. 10.1089/ars.2014.6128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Tanaka S, Haruma K, Kunihiro M, et al. Effects of aged garlic extract (AGE) on colorectal adenomas: a double-blinded study. Hiroshima J Med Sci 2004;53:39-45. [PubMed] [Google Scholar]
- 41. Li H, Li HQ, Wang Y, et al. An intervention study to prevent gastric cancer by micro-selenium and large dose of allitridum. Chin Med J (Engl) 2004;117:1155-60. 10.3760/j.issn:0366-6999.2004.08.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary information: additional tables 1-4