Abstract
Background
The World Health Organization (WHO) recommends treating all school children at regular intervals with deworming drugs in areas where helminth infection is common. Global advocacy organizations claim routine deworming has substantive health and societal effects beyond the removal of worms. In this update of the 2015 edition we included six new trials, additional data from included trials, and addressed comments and criticisms.
Objectives
To summarize the effects of public health programmes to regularly treat all children with deworming drugs on child growth, haemoglobin, cognition, school attendance, school performance, physical fitness, and mortality.
Search methods
We searched the Cochrane Infectious Diseases Group Specialized Register; Cochrane Central Register of Controlled Trials (CENTRAL); MEDLINE; Embase; LILACS; the metaRegister of Controlled Trials (mRCT); reference lists; and registers of ongoing and completed trials up to 19 September 2018.
Selection criteria
We included randomized controlled trials (RCTs) and quasi‐RCTs that compared deworming drugs for soil‐transmitted helminths (STHs) with placebo or no treatment in children aged 16 years or less, reporting on weight, height, haemoglobin, and formal tests of cognition. We also sought data on other measures of growth, school attendance, school performance, physical fitness, and mortality.
Data collection and analysis
At least two review authors independently assessed the trials for inclusion, risk of bias, and extracted data. We analysed continuous data using the mean difference (MD) with 95% confidence intervals (CIs). Where data were missing, we contacted trial authors. We stratified the analysis based on the background burden of STH infection. We used outcomes at time of longest follow‐up. We assessed the certainty of the evidence using the GRADE approach.
Main results
We identified 51 trials, including 10 cluster‐RCTs, that met the inclusion criteria. One trial evaluating mortality included over one million children, and the remaining 50 trials included a total of 84,336 participants. Twenty‐four trials were in populations categorized as high burden, including nine trials in children selected because they were helminth‐stool positive; 18 with intermediate burden; and nine as low burden.
First or single dose of deworming drugs
Fourteen trials reported on weight after a single dose of deworming drugs (4970 participants, 14 RCTs). The effects were variable. There was little or no effect in studies conducted in low and intermediate worm burden groups. In the high‐burden group, there was little or no effect in most studies, except for a large effect detected from one study area in Kenya reported in two trials carried out over 30 years ago. These trials result in qualitative heterogeneity and uncertainty in the meta‐analysis across all studies (I2 statistic = 90%), with GRADE assessment assessed as very low‐certainty, which means we do not know if a first dose or single dose of deworming impacts on weight.
For height, most studies showed little or no effect after a single dose, with one of the two trials in Kenya from 30 years ago showing a large average difference (2621 participants, 10 trials, low‐certainty evidence). Single dose probably had no effect on average haemoglobin (MD 0.10 g/dL, 95% CI 0.03 lower to 0.22 higher; 1252 participants, five trials, moderate‐certainty evidence), or on average cognition (1596 participants, five trials, low‐certainty evidence). The data are insufficient to know if there is an effect on school attendance and performance (304 participants, one trial, low‐certainty evidence), or on physical fitness (280 participants, three trials, very low‐certainty evidence). No trials reported on mortality.
Multiple doses of deworming drugs
The effect of regularly treating children with deworming drugs given every three to six months on weight was reported in 18 trials, with follow‐up times of between six months and three years; there was little or no effect on average weight in all but two trials, irrespective of worm prevalence‐intensity. The two trials with large average weight gain included one in the high burden area in Kenya carried out over 30 years ago, and one study from India in a low prevalence area where subsequent studies in the same area did not show an effect. This heterogeneity causes uncertainty in any meta‐analysis (I2 = 78%). Post‐hoc analysis excluding trials published prior to 2000 gave an estimate of average difference in weight gain of 0.02 kg (95%CI from 0.04 kg loss to 0.08 gain, I2 = 0%). Thus we conclude that we do not know if repeated doses of deworming drugs impact on average weight, with a fewer older studies showing large gains, and studies since 2000 showing little or no average gain.
Regular treatment probably had little or no effect on the following parameters: average height (MD 0.02 cm higher, 95% CI 0.09 lower to 0.13 cm higher; 13,700 participants, 13 trials, moderate‐certainty evidence); average haemoglobin (MD 0.01 g/dL lower; 95% CI 0.05 g/dL lower to 0.07 g/dL higher; 5498 participants, nine trials, moderate‐certainty evidence); formal tests of cognition (35,394 participants, 8 trials, moderate‐certainty evidence); school performance (34,967 participants, four trials, moderate‐certainty evidence). The evidence assessing an effect on school attendance is inconsistent, and at risk of bias (mean attendance 2% higher, 95% CI 5% lower to 8% higher; 20,650 participants, three trials, very low‐certainty evidence). No trials reported on physical fitness. No effect was shown on mortality (1,005,135 participants, three trials, low‐certainty evidence).
Authors' conclusions
Public health programmes to regularly treat all children with deworming drugs do not appear to improve height, haemoglobin, cognition, school performance, or mortality. We do not know if there is an effect on school attendance, since the evidence is inconsistent and at risk of bias, and there is insufficient data on physical fitness. Studies conducted in two settings over 20 years ago showed large effects on weight gain, but this is not a finding in more recent, larger studies. We would caution against selecting only the evidence from these older studies as a rationale for contemporary mass treatment programmes as this ignores the recent studies that have not shown benefit.
The conclusions of the 2015 edition have not changed in this update.
28 November 2019
Up to date
All studies incorporated from most recent search
All eligible published studies found in the last search (19 Sep, 2018) were included and three ongoing studies identified
Plain language summary
Deworming school children in low‐ and middle‐income countries
Cochrane researchers examined the effects of deworming children in areas where intestinal worm infection is common. After searching for relevant trials up to 19 September 2018, we included 50 trials with a total of 84,336 participants, and an additional trial of one million children.
What is deworming and why might it be important
Soil‐transmitted worms, including roundworms, hookworms, and whipworms, are common in tropical and subtropical areas, and particularly affect children living in poverty where there is inadequate sanitation. The World Health Organization (WHO) currently recommends that school children in many areas are regularly treated with drugs which kill these worms. Some advocates claim such programmes improve child growth, haemoglobin, cognition, school attendance, school performance, physical fitness, and survival.
What the research says
In populations of children living in endemic areas, the effect of the first, single dose of deworming drugs on weight is unclear. There was little or no effect in most studies, except for a large effect detected from one study area in Kenya, reported in two trials carried out over 30 years ago in a school where children were heavily infected with worms. This causes uncertainty, which means we do not know if a first dose or single dose of deworming impacts on weight. For height, most studies showed little or no effect, with the exception of the site in Kenya. A single dose of deworming medicine probably has no effect on haemoglobin and cognition. There is insufficient data to know if there is an effect on school attendance, school performance, or physical fitness or mortality.
In studies where children were regularly treated with deworming medicine there was little or no effect on weight in all but two trials, irrespective of whether children were heavily infected with worms or not. The two trials with large average weight gains included the Kenya study carried out over 30 years ago, and one study from India carried out over 20 years ago in a low worm burden area where later studies in the same area did not show an effect. In trials from 2000 onwards, which are more relevant given the global reduction in worm burden, there is little or no effect. This causes uncertainty and means we do not know if regularly treating children with deworming medicine improves their weight. Regularly deworming children probably has no effect on height, haemoglobin, cognition, and mortality. We do not know if there is an impact on school attendance, since the evidence is inconsistent and at high risk of bias. There is insufficient data to know if there is an effect on physical fitness.
Authors' conclusions
For public health programmes to regularly treat all children in endemic areas with deworming drugs, there is quite substantial evidence of no benefit in terms of haemoglobin, cognition, school performance, and mortality. For weight, contemporary studies do not show an effect, but unusually large effects were seen in studies over 20 years ago.
Summary of findings
Background
Description of the condition
Soil‐transmitted helminth (STH) infections are common in poor children living in conditions where sanitation is inadequate (Strunz 2014). The term refers to the three main STHs which live in the intestine, are transmitted orally from faeces or contaminated soil: Ascaris lumbricoides (roundworm), Trichuris trichiura (whipworm), and hookworm (Ancylostoma duodenale and Necator americanus) (Jourdan 2018).
Current World Health Organization (WHO) estimates suggest that up to a quarter of the world’s population are at risk from STHs, and that 875 million children globally would benefit from regular deworming treatment for STHs (WHO 2018a). Recent data show a steady decline in the estimated burden of disease associated with STHs over recent decades (Vos 2015).
Most children with infections do not have symptoms. Sometimes, when the number of worms is high, this causes clinical illness: for example, Ascaris can cause bowel obstruction; and Ascaris and Trichuris are associated with poor nutritional status; whilst hookworm is associated with anaemia (Vos 2015). Deworming drugs are widely administered as one component of therapy at child health clinics in STH endemic areas for children with weight loss, anaemia, and minor illnesses.
There is no argument that people with symptoms and STH infection should be treated. The infections can be unpleasant. There is no argument that longer‐term changes in living conditions and economic circumstances will help rid communities of these infections, and this is for the better.
Current debate relates to the effectiveness of public health programmes delivering mass treatment with anthelminthic drugs to assure regular treatment of children with asymptomatic infections. Part of the rationale for mass treatment is to reduce transmission, and to capture a few individuals within an infected population that have high worm loads which are impacting on their health. It is known that within infected populations, STHs are “over‐dispersed”, meaning that a few individuals have very high worm loads (Jourdan 2018).
Description of the intervention
“Preventive chemotherapy” is the public health intervention targeted to at‐risk population groups to control morbidity associated with STHs. Since 2002, the WHO has recommended regular mass drug administration with anthelminthic (deworming) medicines, without previous individual diagnosis, to almost all children living in endemic areas. High‐risk groups currently include children, adolescent girls, women of reproductive age, and pregnant women, including those co‐infected with HIV (WHO 2017a). This Cochrane Review is about deworming for children. Pregnancy and deworming is reviewed in Salam 2015.
The current approach includes both mass treatment of whole populations, and school‐based programmes in particular, currently implemented in more than 60 endemic countries. The WHO argues that it is easy to deliver medicines through teaching staff, with estimated costs USD 0.3 per child per year for annual dosing (WHO 2017a).
The strategy requires a population survey to estimate the prevalence and intensity of infection to determine the population worm burden. Treatment is then recommended once per year for low‐risk communities with 20% to 50% prevalence of soil‐transmitted helminth infection, or twice per year in at‐risk communities with more than 50% prevalence of soil‐transmitted helminth infections, since worm populations tend to return rapidly to pretreatment levels in less than a year (Anderson 1991). The WHO does not recommend individual screening and treatment, since the cost of screening is higher than alternative approaches, regardless of the epidemiological setting (WHO 2017a).
Anderson and colleagues have argued that treating individuals in communities reduces transmission in the community as a whole (Anderson 1991), and this leads to health and schooling benefits for the whole population, including those who have not received deworming treatment (Bundy 2009). These ‘spill over' effects, or externalities, are not captured in individually‐randomized controlled trials (RCTs), since any benefit in the control group reduces the overall treatment effect, but they can be detected in cluster‐RCTs that evaluate all children.
How the intervention might work
Deworming for STHs aims to reduce the worm burden in populations and decrease the intensity of infection particularly among heavily‐infected children, since morbidity is more likely among those with high‐intensity infections. The control programme is thus intended to reduce the worm burden in children who are most heavily infected in a particular population and to keep it low through repeated treatments.
The rationale for the effects of deworming programmes on population development has been based on the assumption that reducing the worm load in populations will lead to improvements in nutritional status, and also potential improvements in haemoglobin, and cognition. As a result of these benefits, children are thought to have increased physical well‐being, with improved intellect, and are better able to attend school. Although school attendance was not a focus in the latest WHO guidelines (WHO 2017a), previous WHO documents have promoted the impact of deworming on school attendance, suggesting subsequent impacts on attainment, long‐term societal and population‐level economic benefits (WHO 2005; WHO 2011).
This causal chain is expressed in our logic model (see Figure 1), which provides the basis for this Cochrane Review: the primary outcomes sought are the main effects (increased haemoglobin, nutrition, and improved cognition); measurable aspects of the mediating pathways (school attendance and physical well‐being); and measurable aspects of impact (mortality and school performance).
1.
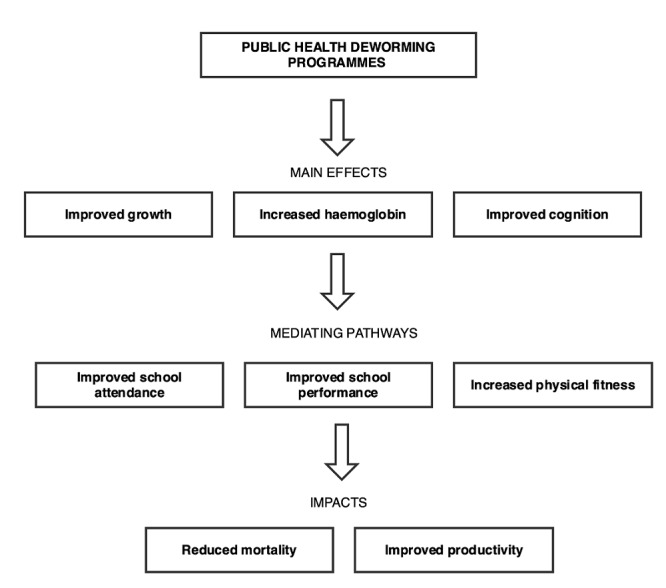
Logic model for public health programmes to regularly treat all children with worms for soil‐transmitted helminth infection in endemic areas
More recently, the WHO have modified the rationale behind recommending deworming: the claimed impact on school attendance, school performance and economic productivity of the whole community is now not evident in the WHO guideline underpinning their recommendations (WHO 2017a), although has been a central tenet in the past (WHO 2005).
Why it is important to do this review
Given the amount of investment of public money in deworming programmes, it is important to be clear whether mass or targeted drug administration is able to contribute to health and development in a substantive way, and that it achieves what the proponents claim in terms of benefits to individuals and society. Although the drugs are cheap to buy, mass treatment programmes require considerable programmatic efforts to organize and deliver.
The policy debates generated by previous versions of this Cochrane Review over the last 18 years are complex. The important background information are placed in Table 4 for those that want more details. Previous editions of this review were instrumental in ensuring the publication of a trial of over one million children in India evaluating deworming; led to a replication analysis of a large stepped‐wedge design study from Kenya (Aiken 2015); and a Campbell review asking an identical question (Welch 2016). More recently an individual patient data (IPD) meta‐analysis has been completed, and is due to be published in 2019.
2. Additional background information.
|
Policy backdrop The intended impacts of deworming programmes are heavily promoted by advocates in the field such as the WHO (Montresor 2002; WHO 2002; WHO 2006b; WHO 2011; WHO 2015,WHO 2017a), the World Bank (World Bank 2003), and the Bill & Melinda Gates Foundation (Hawkes 2013). Furthermore, deworming with albendazole was endorsed in the 2012 Copenhagen consensus statement, as the fourth highest ranking solution to address quote: "big issues facing the planet" in terms of cost and benefit (Copenhagen Consensus Center 2012). The widely‐cited cost‐effectiveness estimates from the Disease Control Priorities in Developing Countries (DCP2) report (Jamison 2006) stated that deworming for STH infections was one of the most cost‐effective interventions for global health. However, the reliability of these estimates has been questioned by the organization GiveWell, which suggests they have been overstated by a factor of about 100 (GiveWell 2011). The most recent edition of the Disease Control Priorities in Developing Countries report concludes that soil‐transmitted helminth (STH) infection levels and morbidity are likely to continue to decline as a result of the combination of high levels of treatment and continuing economic development trends in poor communities (Bundy 2017). Advocates point to the favourable cost‐effectiveness estimates for deworming programmes, with a focus on the putative effect on schooling outcomes and productivity (Evidence Action 2018). The evidentiary basis for this draws on a range of trial designs, including historical econometric trials such as Bleakely 2004, which analysed the Rockefeller Sanitary Commission's campaign to eradicate hookworm in the Southern states of the USA. This showed an association between areas with higher levels of hookworm infection prior to the campaign and greater increases in school attendance and literacy after the intervention, and an association with income gains in the longer term. Another influential trial is Miguel 2004 (Cluster), which is included in this Cochrane Review. Current policies have become even more challenging to assess, as global specialists conflate the evidence on different helminths (Lo 2017). The WHO, for example, has previously suggested that deworming treatment against schistosomes and STH infections helps (1) eradicate extreme poverty and hunger; (2) achieve universal primary education; (3) promote gender equality and empower women; (4) reduce child mortality and improve maternal health; and (5) combat HIV/AIDS, malaria, and other diseases (WHO 2005; WHO 2011). The evidence for the benefit of treating populations with schistosomiasis is fairly clear (Kramer 2014), as the infection has a very substantive effect on health. However, this does not mean that a different drug treating a different helminth species is equally effective. Given the amount of investment of public money in these programmes, it is important to be clear whether mass or targeted drug administration is able to contribute to health and development in a substantive way. Indeed, international donors and developed country governments and tax payers are contributing to the efforts to tackle STH infections in the belief that they will improve the health of children in the way that WHO has previously claimed (WHO 2005). For example, Deworm the World has worked with the Indian Government to treat 140 million children across India in 2015 on the basis of the Copenhagen Consensus Statement (Evidence Action 2015; Mudur 2015). History of the current review Previous editions of this Cochrane Review have advanced the science and the evidence in several ways. •Previous editions highlighted large trials that were not in the public domain. As a result of the review, one of these trials has been published: The DEVTA trial of over one million children was completed in 2005 and published in 2013 (Awasthi 2013 (Cluster). A second important trial with a manuscript date of 2006 of over 2500 children remains unpublished. This trial does not demonstrate an effect, but is included in the Cochrane Review (Hall 2006 (Cluster). •Previous editions highlighted that the weight gain reported in the BMJ in 2007 on 27,955 children in 60 clusters in the Uganda trial, which was reported as "154 g (95% CI 96 to 214)" had not been adjusted for clustering. The authors promptly supplied us with the variance corrected for clustering, which we included in the review. As this did not reach statistical significance, we highlighted this to the BMJ, and a correction was eventually published in 2012 (Alderman 2006 (Cluster)). •Previous editions highlighted methodological concerns with an influential econometric trial from Kenya (Miguel 2004 (Cluster). We highlighted concerns about the quality of the evidence for school attendance on the basis of this trial in the previous version of this Cochrane Review (Taylor‐Robinson 2012b). The development organization 3ie commissioned a replication, which was published in 2015 (Aiken 2014; Aiken 2015; Davey 2015). The authors checked the data and corrected any errors, and then carried out an analysis using exactly the methods in the original publication. The replication highlights important coding errors and this resulted in a number of changes to the results: the previously reported effect on anaemia was not apparent in the replication; the effect on school attendance was similar to the original analysis, although the effect was seen in both children that received the drug and those that did not; and the indirect effects (externalities) of the intervention on adjacent schools also was not demonstrated (Aiken 2015). The statistical replication suggested some impact of the complex intervention (deworming and health promotion) on school attendance, but this varied depending on the analysis strategy, and there was a high risk of bias. The replication showed no effect on exam performance (Davey 2015). •The Cochrane systematic review was subject to an independent replication by the Campbell Collaboration, who used network meta‐analysis. This was published in 2016 (Welch 2016; Welch 2017), confirming the findings of the Cochrane review (Taylor‐Robinson 2017). •We carried out a formal evaluation of the evidence for long‐term impact derived from three studies that have been heavily cited as evidence of developmental impact. The review concluded that all three studies were at substantive risk of methodological bias, and were helpful in generating hypothesis, but not reliable evidence of effects (Jullien 2016). |
Objectives
To summarize the effects of public health programmes to regularly treat all children with deworming drugs on child growth, haemoglobin, cognition, school attendance, school performance, physical fitness, and mortality.
Methods
Criteria for considering studies for this review
Types of studies
Randomized controlled trials (RCTs) and quasi‐RCTs.
Types of participants
Infected children identified by screening in community trials, or children living in endemic areas.
We defined children as aged under 16 years. We excluded trials evaluating deworming as part of the treatment of sick children.
Types of interventions
Intervention
Deworming drugs for soil‐transmitted helminth (STHs), administered at any location (including health facilities, schools, and communities). We included trials examining effects after a single dose and after multiple doses.
The deworming drugs we included are those in the WHO Model List of Essential Medicines for deworming drugs of soil‐transmitted helminths (WHO 2006a). This includes albendazole, levamisole, mebendazole, pyrantel, and ivermectin. Other drugs used are nitazoxanide, piperazine, tetrachlorethylene, and thiabendazole.
We did not exclude trials that also provided some health promotion activities supporting the deworming programmes. We included studies that provided additional interventions (for example, growth monitoring, micronutrient supplementation, malaria chemoprevention, or other drugs) when the additional intervention was given to both the control and intervention arm in equal measure.
Control
Placebo or no treatment.
Types of outcome measures
Primary outcomes
-
Growth, as measured by the following indicators:
weight
height
Haemoglobin
Formal tests of cognition
Secondary outcomes
-
Other growth indicators
mid‐upper arm circumference (MUAC)
skin fold thickness (including triceps and subscapular skin fold)
body mass index (BMI)
-
School attendance
days present at school
number of children dropping out
School performance (measured by examination results)
Measures of physical fitness (e.g. Harvard Step Test)
Mortality
Adverse events
Serious adverse events (death, life‐threatening events, or events leading to hospitalizations)
Other adverse events
Search methods for identification of studies
Electronic searches
The review authors and the Cochrane Infectious Diseases Group (CIDG) Information Specialist, Vittoria Lutje, attempted to identify all relevant trials regardless of language or publication status (published, unpublished, in press, and in progress). The date of the last search was 19 September 2018. The CIDG Information Specialist searched the following databases using the search terms and strategy described in Table 5: CIDG Specialized Register (19 September 2018); Cochrane Central Register of Controlled Trials (CENTRAL), published in the Cochrane Library (2018, Issue 8); MEDLINE (2000 to 19 September 2018); Embase (2000 to 19 September 2018); and LILACS (2000 to 19 September 2018); and reference lists, and registers of ongoing and completed trials. We also searched the metaRegister of Controlled Trials (mRCT) using ‘helminth* OR anthelminth*' (19 September 2018).
3. Search strategy: terms by database.
| Search set | CIDG SRa | CENTRAL | MEDLINEb | EMBASEb | LILACSb |
| 1 | helmint* | helmint* | helmint* | helmint$ | helmint* |
| 2 | Ancylostoma duodenale | Ancylostoma duodenale | Ancylostoma duodenale | Ancylostoma duodenale | Ancylostoma duodenale |
| 3 | Necator americanus | Necator americanus | Necator americanus | Necator americanus | Necator americanus |
| 4 | Ascaris | Ascaris | Ascaris | Ascaris | Ascaris |
| 5 | Enterobius vermicularis | Enterobius vermicularis | Enterobius vermicularis | Enterobius vermicularis | Enterobius vermicularis |
| 6 | trichuris | trichuris | trichuris | trichuris | trichuris |
| 7 | Strongyloid* | Strongyloid* | Strongyloid* | Strongyloid* | Strongyloid* |
| 8 | albendazole | hookworm* | hookworm* | hookworm$ | 1‐7/OR |
| 9 | mebendazole | roundworm* | roundworm* | roundworm$ | albendazole |
| 10 | piperazine | pinworm* | pinworm* | pinworm$ | mebendazole |
| 11 | levamisole | whipworm* | whipworm* | whipworm$ | piperazine |
| 12 | pyrantel | 1‐11/OR | 1‐11/OR | 1‐11/OR | levamisole |
| 13 | tiabendazole | albendazole | albendazole | albendazole | pyrantel |
| 14 | — | mebendazole | mebendazole | mebendazole | tiabendazole |
| 15 | — | piperazine | piperazine | piperazine | 9‐14/OR |
| 16 | — | levamisole | levamisole | levamisole | 8 and 15 |
| 17 | — | pyrantel | pyrantel | pyrantel | Limit 16 to human |
| 18 | — | tiabendazole | tiabendazole | tiabendazole | — |
| 19 | — | 13 or 14 or 15 or 16 or 17 or 18 | 13 or 14 or 15 or 16 or 17 or 18 | 13 or 14 or 15 or 16 or 17 or 18 | — |
| 20 | — | 12 and 19 | 12 and 19 | 12 and 19 | — |
| 21 | — | — | Limit 20 to human | Limit 20 to human | — |
aCIDG Specialized Register. bSearch terms used in combination with the search strategy for retrieving trials developed by Cochrane (Lefebvre 2011).
Data collection and analysis
Selection of studies
David Taylor‐Robinson (DTR) checked the search results for potentially relevant trials and retrieved full‐text articles as required. DTR and Nicola Maayan (NM) independently assessed the trial eligibility using an eligibility form based on the inclusion criteria; where there was uncertainty, all five review authors participated in the decision about inclusion. We checked that trials with multiple publications were managed as one trial. We recorded reasons for the exclusion of trials. When eligibility was unclear or when trials were unpublished, we contacted study authors for information.
Data extraction and management
For this review version, two review authors (NM and DTR) independently extracted data using data extraction forms. We resolved any differences in opinion by discussion. Where methods, data, or analyses were unclear or missing, we contacted trial authors for further details.
We extracted data on type of additional interventions as these potentially confound effects. This includes accompanying health promotion programme including programmes about hygiene and behaviour, water and sanitation, or additional drugs or vitamins. We carefully evaluated whether these interventions were in both intervention and control groups, or only in the intervention group.
For each treatment group of each trial, we extracted the number of patients randomized. For each outcome of interest, we extracted the number of participants analysed in each treatment group of each trial. For continuous outcomes. where change from baseline results were presented alongside results purely based on the end value, we only extracted the change from baseline results.
RCTs that randomized individuals
For dichotomous outcomes, we planned to extract the number of patients with the event. For continuous outcomes, we aimed to extract means and standard deviations (SDs). Where these data were not reported, we extracted medians and ranges or any other summary statistics.
RCTs that randomized clusters
For each cluster‐RCT, we extracted the cluster unit, the number of clusters in the trial, the average size of clusters, and the unit of randomization (such as household or institution). Where possible, we extracted the statistical methods used to analyse the trial along with details describing whether these methods adjusted for clustering or other covariates.
Where a cluster‐RCT adjusted for clustering in their analysis, we extracted the cluster‐adjusted results. When the trial did not account for clustering in their analysis, we extracted the same data as for trials that randomized individuals.
Assessment of risk of bias in included studies
Review authors DTR, PG, NM, SD, and MR independently assessed the risk of bias (Higgins 2011c). We resolved any differences through discussion. We corresponded with trial investigators when methods were unclear.
For RCTs that randomized individuals, we addressed six components: sequence generation; allocation concealment; blinding; incomplete outcome data; selective outcome reporting; and other biases. For cluster‐RCTs, we addressed additional components: recruitment bias; baseline imbalance; loss of clusters; incorrect analysis; compatibility with RCTs randomized by individual. For each component, we placed judgments of low, high, or unclear/unknown risk of bias as described in Appendix 1. We displayed the results in ‘Risk of bias' tables, a ‘Risk of bias' summary, and a ‘Risk of bias' graph.
Measures of treatment effect
We summarized continuous data (means and SDs) using the mean differences (MDs). We used the risk ratio to compare the treatment and control groups for dichotomous outcomes. All treatment effects were presented with 95% confidence intervals (CIs).
Unit of analysis issues
For a particular cluster‐RCT when the analyses had not been adjusted for clustering, we attempted to adjust the results for clustering by estimating the design effect calculated as 1+(m‐1)*ICC where m is the average cluster size and ICC is the intra‐cluster correlation coefficient. To make the adjustment, we estimated a treatment effect that did not adjust for clustering and then multiplied the standard errors of the estimate by the square root of the design effect. When the true ICC was unknown, we estimated it from other included cluster‐RCTs.
Dealing with missing data
We aimed to conduct a complete‐case analysis, such that all patients with a recorded outcome were included in the analysis.
Assessment of heterogeneity
We inspected the forest plots to detect overlapping CIs, applied the Chi² test with a P value of 0.10 used to indicate statistical significance, and also implemented the I² statistic with values of 30% to 60%, 59% to 90%, and 75% to 100% used to denote moderate, substantial, and considerable levels of heterogeneity, respectively.
Assessment of reporting biases
We plotted funnel plots for weight, and we examined these plots for asymmetry, which would indicate the presence of small‐study effects. If small‐study effects had been detected, we would have explored further the possible reasons for these small study‐effects, including publication bias.
Data synthesis
DTR, NM, and SD analysed data using Review Manager 5 (Review Manager 2014).
We structured the analysis into two sections.
First dose
Multiple doses, longest follow‐up
We also grouped trials by worm burden (high, intermediate, and low). We used the cut‐offs in the table below, rather than the simplified prevalence‐based field guide categories that are now used to determine treatment frequency (WHO 2006b; Table 6). For areas with intermediate and high intensity, the WHO recommends regular (at least annual) deworming treatment with albendazole for quote: "all young children, preschool children and school‐age children".
4. WHO community diagnosis classification and treatment strategies.
| Community category (WHO 2002) | Prevalencea | Percentageb | School intervention |
| 1. High prevalence or high intensity | > 70% | > 10% | Targeted treatment of school‐age children 2 to 3 times per year |
| 2. Moderate prevalence and low intensity | > 50% but < 70% | < 10% | Targeted treatment of school‐age children once per year |
| 3. Low prevalence and low intensity | < 50% | < 10% | Selective treatment |
| Category (WHO 2006b) | Prevalencea | Action to be taken | |
| High risk community | > 50% | Targeted treatment of pre‐school and school‐age children 2 or 3 times per year | |
| Low risk community | > 20% but < 50% | Targeted treatment of pre‐school and school‐age children once per year |
aOf any worm infection. bOf moderate to heavy infections.
To combine the prevalence and intensity into burden grouping, we took whichever was higher. For example, if a trial had intermediate prevalence but high intensity, this trial was entered into the high‐burden group. In trials where information on intensity was not provided, we grouped the trial on the basis of quoted prevalence; it is possible that the grouping has been underestimated in these trials. Trials which screened participants and only included those with worm infections were added to the high group.
| Prevalence and intensity | Prevalence of any worm infection | Conditional link | Intensity ‐ percentage of moderate to heavy infections |
| Low | < 20% | and | < 10% |
| Intermediate | > 20% but < 80% | ‐ | ‐ |
| High | > 80% | or | > 10% |
When a trial reported data at multiple time points, we included data collected at the longest follow‐up time in the analysis of ‘after multiple doses', because long‐term outcomes of multiple doses of deworming are of most relevance to policymakers, and short‐term effects are captured in the single‐dose results.
We combined cluster‐RCTs that adjusted for clustering and RCTs that randomized individuals using meta‐analysis. We used a fixed‐effect meta‐analysis when the assessments of heterogeneity did not reveal heterogeneity. In the presence of heterogeneity, we used random‐effects meta‐analysis.
For continuous data, we combined change from baseline results with end value results providing they were from distinct trials (Higgins 2011a; Higgins 2011b). Labels on the meta‐analyses indicate when end values were used.
We presented data that could not be meta‐analysed in additional tables and reported on these in each section, under the heading ‘other data'.
Subgroup analysis and investigation of heterogeneity
We subgrouped the analysis by disease burden. As Ascaris is said to be associated with weight loss and hookworm with anaemia, we stratified the analysis between trials by helminth species burden.
We also sorted the forest plot for weight (in all children in an endemic area after multiple doses) by year that the trial was carried out to visually inspect whether the intervention effect changed over time. There appeared to be a relationship, so we carried out a post‐hoc subgroup analysis by studies published prior to and after the year 2000. The rationale of the cutpoint was to exclude trials carried out in the previous century, when worm loads were likely to be higher. The cutpoint also meant the period covered before 2000 and after 2000 was about similar, and there also happened to be similar numbers of trials in the two subgroups.
Sensitivity analysis
We carried out sensitivity analyses including only those trials with a low risk of bias regarding allocation concealment.
‘Summary of findings' tables
We interpreted results using ‘Summary of findings' tables, which provide key information about the certainty of the evidence for the included trials in the comparison, the magnitude of effect of the interventions examined, and the sum of available data on the main outcomes. Using GRADE profiler (GRADEpro 2014), we imported data from Review Manager 2014; the GRADE display was based on a recent trial of what users prefer (Carrasco‐Labra 2015). We presented the primary outcomes for the review in the ‘Summary of findings' tables, and added height, school attendance, and mortality for multiple‐dose trials.
Results
Description of studies
We identified 51 trials reported in 75 articles that met the inclusion criteria (see Figure 2, Characteristics of included studies and Appendix 2).
2.
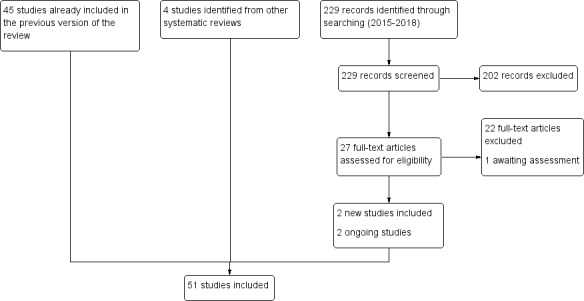
Study flow diagram.
Excluded trials are detailed in Characteristics of excluded studies, and four trials we are aware of, and are finding out if they were ever carried out, or we are awaiting additional data from the authors (see Characteristics of ongoing studies and Characteristics of studies awaiting classification).
We identified three long‐term studies reported across multiple on line unpublished papers that evaluated effects more than nine years after cluster‐randomized trials in Kenya and Uganda (Baird 2016; Ozier 2016; Croke 2014). The Cochrane Infectious Diseases Group has critically appraised and summarized the six iterations of analysis of Baird, the four online iterations of analysis of Ozier 2016, and data from Croke (which were unrelated to the base trial). This systematic review has been published in full (Jullien 2016). The conclusion of this review is that all three studies are at risk of substantial methodological bias and were only helpful in generating hypotheses, but should not be considered to provide reliable evidence of effects. In many of the studies repeated analysis over time with multiple statistical testing raised doubt about any of the conclusions. As these would not be informative and the analysis is now complete and published elsewhere, the results are noted in the discussion of this review, and the studies excluded.
Location
The included trials were undertaken in 25 different countries: Bangladesh (four trials); Cameroon (two trials); Ethiopia (two trials); Guatemala (two trials); Haiti (two trials); India (five trials); Indonesia (four trials); Jamaica (three trials); Kenya (four trials); Malaysia (two trials); South Africa (two trials); Uganda (two trials); Vietnam (three trials); Zanzibar (two trials); Benin, Botswana, China, Nigeria, Papua New Guinea, Peru, Philippines, Sierra Leone, Tanzania, Zaire (one trial in each); China, Philippines and Kenya; China and Myanmar (multi‐centre trials).
Population
Children were recruited from school populations in 30 trials, communities in 13 trials, and in health facilities or by health workers in eight trials. One of these trials recruited children on discharge from hospital (Donnen 1998), and another recruited children whose mothers had participated in the pregnancy phase of the trial (Ndibazza 2012). Olds 1999, and Wiria 2013 (Cluster) also included adolescents 17 to 19 years old, but most participants were under 16 years old.
Forty‐two trials were based on mass‐targeted treatment of an unscreened population. Nine trials studied children who were screened and selected on the basis of their having high worm loads and the purpose of three of these trials was to measure cognitive outcomes. One trial of unscreened children, Stephenson 1993, also studied an infected subgroup of the larger unscreened trial population for cognitive and haemoglobin outcomes.
Twenty trials were conducted in populations where worms were of high prevalence, 22 as intermediate and eight as low. Nine trials were populations with high intensity and 11 low. Thirty‐one trials did not report the intensity, although 12 reported the average eggs per gram (epg) in children infected with worms. Awasthi 2013 (Cluster) did not report any information on the baseline worm prevalence or intensity. We classified this study as low prevalence and low intensity based on previous trials in the same area (Awasthi 1995 (Cluster); Awasthi 2000; Awasthi 2001 (Cluster)). Overall, 24 trials were categorized as high burden, 18 as intermediate, and nine as low (Table 7).
5. Description of studies: STM prevalence and intensity.
| Study | Prevalence | Intensity | Burden |
| The methods for estimating burden are reported in methods | |||
| Alderman 2006 (Cluster) | Intermediate | Not reported | Intermediate |
| Awasthi 1995 (Cluster) | Low | Not reported | Low |
| Awasthi 2000 | Low | Not reported | Low |
| Awasthi 2001 (Cluster) | Low | Not reported | Low |
| Awasthi 2013 (Cluster) | Not reported | Not reported | Low1 |
| Beach 1999 | Intermediate | Low | Intermediate |
| Donnen 1998 | Low | Low | Low |
| Dossa 2001 | Intermediate | Not reported | Intermediate |
| Fox 2005 | Intermediate | Low | Intermediate |
| Freij 1979a (Screened) | High | Not reported | High |
| Freij 1979b (Screened) | High | Not reported | High |
| Garg 2002 | Low | Low | Low |
| Gateff 1972 | High | Not reported | High |
| Goto 2009 | Low | Low | Low |
| Greenberg 1981 | High | High | High |
| Gupta 1982 | Intermediate | Not reported | Intermediate |
| Hadju 1996 | High | High | High |
| Hadju 1997 | High | Not reported | High |
| Hall 2006 (Cluster) | High | Not reported | High |
| Joseph 2015 | Low | Low | Low |
| Kirwan 2010 | Intermediate | Low | Intermediate |
| Kloetzel 1982 | Intermediate | High | High |
| Koroma 1996 | Intermediate | Not reported | Intermediate |
| Kruger 1996 | Intermediate | Not reported | Intermediate |
| Kvalsvig 1991a (Screened) | High | Not reported | High |
| Lai 1995 | Intermediate | High | High |
| Le Huong 2007 | Intermediate | High | High |
| Liu 2017 (Cluster) | Intermediate | Low | Intermediate |
| Michaelsen 1985 | High | Low | High |
| Miguel 2004 (Cluster) | Intermediate | High | High |
| Ndibazza 2012 | Low | Not reported | Low |
| Nga 2009 | Intermediate | Low | Intermediate |
| Nokes 1992 (Screened) | High | High | High |
| Olds 1999 | Intermediate | Not reported | Intermediate |
| Ostwald 1984 | High | Not reported | High |
| Palupi 1997 | Intermediate | Not reported | Intermediate |
| Rousham 1994 (Cluster) | Intermediate | Low | Intermediate |
| Sarkar 2002 (Screened) | High | Not reported | High |
| Simeon 1995 (Screened) | High | High | High |
| Solon 2003 | Intermediate | Not reported | Intermediate |
| Stephenson 1989 | High | Not reported | High |
| Stephenson 1993 | High | Not reported | High |
| Sternberg 1997 (Screened) | High | Not reported | High |
| Stoltzfus 1997 (Cluster) | High | Not reported | High |
| Stoltzfus 2001 | Intermediate | Not reported | Intermediate |
| Sur 2005 | Intermediate | Not reported | Intermediate |
| Tee 2013 (Screened) | High | Not reported | High |
| Watkins 1996 | High | High | High |
| Willett 1979 | Intermediate | Not reported | Intermediate |
| Wiria 2013 (Cluster) | Intermediate | Not reported | Intermediate |
| Yap 2014 (Screened) | High | Not reported | High |
1Based on previous trials in the same area (Awasthi 1995 (Cluster); Awasthi 2000; Awasthi 2001 (Cluster))
Forty studies were in populations with Ascaris, 34 in populations with Trichuris, and 31 with hookworm (Appendix 3). The number of studies with high, intermediate, and low burden are listed in the following table.
| Burden | Ascaris | Trichuris | Hookworm |
| High | 10 | 13 | 7 |
| Intermediate | 19 | 14 | 6 |
| Low | 11 | 7 | 18 |
Twenty‐seven trials included school‐age children older than 59 months, four included preschool children aged 24 to 59 months, two included young children aged 12 to 24 months, and two included infants aged 0 to 12 months. The remaining 16 trials included combinations of infant, young, preschool and school‐aged children (see Table 8). Appendix 4 categorizes age category and worm burden.
6. Description of studies: age categories.
| Age category | N studies | Studies |
| Infants | 2 |
Awasthi 2001 (Cluster) Goto 2009 |
| Infants, young, preschool | 1 | Stoltzfus 2001 |
| Infants, young, preschool, school | 2 |
Donnen 1998 Willett 1979 |
| Young | 2 |
Joseph 2015 Ndibazza 2012 |
| Young, preschool | 5 |
Awasthi 1995 (Cluster) Awasthi 2000 Freij 1979a (Screened) Freij 1979b (Screened) Kirwan 2010 |
| Young, preschool, school | 4 |
Alderman 2006 (Cluster) Awasthi 2013 (Cluster) Greenberg 1981 Kloetzel 1982 |
| Preschool | 4 |
Dossa 2001 Garg 2002 Palupi 1997 Sur 2005 |
| Preschool, school | 3 |
Gupta 1982 Rousham 1994 (Cluster) Sarkar 2002 (Screened) Wiria 2013 (Cluster) |
| School | 27 |
Beach 1999 Fox 2005 Gateff 1972 Hadju 1996 Hadju 1997 Hall 2006 (Cluster) Koroma 1996 Kruger 1996 Kvalsvig 1991a (Screened) Lai 1995 Le Huong 2007 Liu 2017 (Cluster) Michaelsen 1985 Miguel 2004 (Cluster) Nga 2009 Nokes 1992 (Screened) Olds 1999 Ostwald 1984 Simeon 1995 (Screened) Solon 2003 Stephenson 1989 Stephenson 1993 Sternberg 1997 (Screened) Stoltzfus 1997 (Cluster) Tee 2013 (Screened) Watkins 1996 Yap 2014 (Screened) |
Infants: 0 to 12 months
Young: 12 to 23 months
Preschool: 24 to 59 months
School: 59+ months
Interventions
Albendazole
Thirty trials had albendazole only in one treatment arm; in addition, some of these trials had arms with combinations with albendazole and: praziquantel (Olds 1999); ivermectin (Beach 1999); and diethylcarbamazine (Fox 2005); the additional drugs were also given to children in the control arms.
One trial included Giardia treatment, secnidazole, in both intervention and control arms (Goto 2009).
One trial was a deworming programme that included deworming drugs for STHs, praziquantel to treat schistosomiasis in schools with > 30% prevalence, and health promotion interventions (Miguel 2004 (Cluster)).
Other anthelminthic drugs
Eight trials used mebendazole; and three trials used mebendazole in combination with pyrantel. Other deworming drugs used included pyrantel pamoate, piperazine, piperazine citrate, metronidazole, tetrachloroethylene, thiabendazole and levamisole.
Accompanying health promotion activities
Nine trials reported on a range of child health activities (Table 9). In eight trials, the accompanying activities appeared to be applied to both intervention and control arms.
7. Description of studies: accompanying health promotion activities.
| Accompanying intervention | Details from trial | Trials |
| To both intervention and control | Quote: "The AWC workers, usually local women (plus assistants), give pre‐school education, give nutritional supplements to malnourished children, and record births and pre‐school deaths." | Awasthi 2013 (Cluster) |
| Quote:"The parents of all children aged < 7 years were offered a range of health services at child health days, including vaccinations, vitamin A supplements, growth monitoring and promotion, and demonstrations of complementary feeding." | Alderman 2006 (Cluster) | |
| Quote:"The primary job responsibilities of the AWW [anganwadi worker] are to run a creche and provide primary health care and supplementary nutrition for children < six years of age and pregnant and lactating women." | Awasthi 2001 (Cluster) | |
| All children received 10 mL of multivitamins (over two days) as an incentive at each time point. Each 5 mL of multivitamin contained: Vitamin A 3000 IU, Vitamin B2 2.0 mg, Nicotinamide 15.0 mg, Vitamin B1 1.5 mg, Vitamin B6 2.0 mg, Vitamin D2 400 IU, D panthenol 1.0 mg. | Kirwan 2010 | |
| Children attended a mother and child health clinic | Freij 1979a (Screened) | |
| Children in both groups received treatment for other conditions in accordance with the IMCI guidelines. | Garg 2002 | |
| Children were followed up for routine immunisations, and then quarterly, to age 5 years. Children received BCG and oral polio immunisations at birth, polio, diphtheria, pertussis, tetanus, hepatitis B and Haemophilus influenzae type B immunisations at 6, 10 and 14 weeks, and measles immunisation at 9 months. | Ndibazza 2012 | |
| Three schools received fortified soup with 20 mg elemental iron per portion, and 100 mg vitamin C per portion for 6 months. | Kruger 1996 | |
| Only in the intervention group | Treatment schools received worm prevention education through regular public health lectures, wall charts, and the training of teachers in each treatment school on worm prevention. Health education stressed the importance of hand washing to avoid ingesting roundworm and whipworm larvae, wearing shoes to avoid hookworm infection, and not swimming in infected fresh water to avoid schistosomiasis. | Miguel 2004 (Cluster) |
| No additional intervention reported | — | 38 trials |
IMCI: Integrated Management of Childhood Illness; IU: international units
One trial had a comprehensive health promotion programme accompanying the deworming, including regular public health lectures, teacher training, and health education targeted to avoid intestinal helminths and exposure to schistosomiasis (Miguel 2004 (Cluster). These were absent in the control arm.
Control groups
Most trials used placebo or no treatment as a control. Others used vitamin A, vitamin C, or calcium powder.
There were 13 trials where both the treatment and control group received nutritional supplementation: multi‐nutrient, vitamin B, iron, vitamin A, or child health packages, including growth monitoring and health education (Table 9).
Trial design
Ten trials were cluster‐randomized, including one trial with quasi‐random allocation of the 75 clusters (Miguel 2004 (Cluster)). The rest used the individual as the unit of randomization.
Seven of the 10 cluster‐RCTs used an appropriate method to take clustering into account. Awasthi 2001 (Cluster) and Awasthi 1995 (Cluster) used urban slums as the unit of randomization (50 and 124, respectively), and Awasthi 2013 (Cluster) used 72 rural administrative blocks. These three trials were analysed at the cluster level (mean of cluster mean values and associated standard deviation (SDs)). Stoltzfus 1997 (Cluster) randomized 12 schools and adjusted for within‐school correlations using generalized estimating equations. Miguel 2004 (Cluster) adjusted for clustering in their regression estimates, and presented robust standard errors (SEs). Wiria 2013 (Cluster) randomized 954 households and used generalized linear mixed‐effects models that captured the data correlations induced by clustering within households. Liu 2017 (Cluster) randomized 112 townships and used multivariate analyses that took into account clustering at the township level.
The three remaining cluster‐RCTs did not adjust for clustering.
Alderman 2006 (Cluster) had not adjusted the primary outcome for clustering in this trial of 48 parishes containing 27,955 children in total. Upon request, the trial authors provided the adjusted values which we have used in the analysis.
Hall 2006 (Cluster) had 80 units of randomization (schools) containing 2659 children in total. The report presents some regression modelling that adjusts for the cluster design, but the outcomes by randomized comparison do not appear to have been adjusted. We used the ICC calculated from the Alderman 2006 (Cluster) data to adjust the primary weight outcome for inclusion in meta‐analysis. As the average cluster size for Hall 2006 (Cluster) (i.e. 33 children) differed somewhat from that of Alderman 2006 (Cluster) (i.e. 582 children), the true ICC for Hall 2006 (Cluster) may be different to that of Alderman 2006 (Cluster), therefore the adjusted result for weight is merely an approximation.
Rousham 1994 (Cluster) had 13 units of randomization (villages) containing 1476 children in total and had also not adjusted for clustering, but no outcomes from this trial were suitable for meta‐analysis.
Four trials had a factorial design. Awasthi 2013 (Cluster) randomized clusters to usual care, six‐monthly vitamin A, six‐monthly 400 mg albendazole, and both vitamin A and albendazole. Kruger 1996 randomized individual participants to albendazole or placebo, and, also, three of the five schools in the trial received soup fortified with vitamins and iron, and two received unfortified soup. Le Huong 2007 randomized individual participants to iron‐fortified noodles and mebendazole, noodles without iron fortification and mebendazole, iron‐fortified noodles and placebo, noodles without iron fortification and placebo, and iron supplementation and mebendazole. Stoltzfus 2001 randomized households to iron, with random allocation of mebendazole by child, stratified by iron allocation and age‐grouped households; disaggregated data for each treatment allocation group were not provided for each outcome.
Follow‐up periods for the trials that used a single dose ranged from one to 21 months, while the follow‐up periods for trials that used multiple doses ranged from post‐intervention to five years.
Miguel 2004 (Cluster) is a cluster quasi‐randomized stepped‐wedge trial of a combined education and drug‐treatment intervention. The trial included 75 schools with a total of 30,000 pupils enrolled. In addition to helminth treatment, the phased complex intervention included public health lectures, teacher education, and child health education including handwashing, as noted above. In addition, a number of schools in the trial were also mass treated for schistosomiasis. In our previous update of this review, we identified two potential quasi‐randomized comparisons that provide unbiased estimates, one in 1998 and one in 1999, in the stepped‐wedge design. This trial has been re‐analysed by an independent research team, with a full report published on the 3ie website (Aiken 2014), and two subsequent academic papers (Aiken 2015; Davey 2015). In this review update we used data from these sources to assess the methodological quality of the trial. The results are primarily drawn from the replication report, Aiken 2014, which provides estimates corrected for coding errors made by the authors in the original paper. Weight change was calculated from the study dataset following correspondence with the authors.
Outcome measures
Growth
All trials measured growth indicators. Some trials reported absolute values, or changes in absolute values of weight and height (or other growth measures). Many trials presented growth data in terms of z‐scores or percentiles of weight‐for‐age, weight‐for‐height, and height‐for‐age, and compared the trial results to an external reference. Sometimes these values were dichotomized and presented as the prevalence of underweight, stunting or wasting (defined as ‐2 SD z‐scores). The external standard was usually quoted as the National Centre for Health Statistics (NCHS) standard, but a variety of references were quoted (including anthropometric computer packages or country standards). These data have not been used in the meta‐analyses as the results were already incorporated in the values for weight and height. Furthermore, in some trials, outcome data were not reported or were incomplete and could not be used in meta‐analysis.
Haemoglobin
Twenty‐one trials measured haemoglobin. Of these, two trials did not report the measured haemoglobin results (Olds 1999; Solon 2003), two trials only measured this outcome in a subset of the participants (Awasthi 2013 (Cluster); Miguel 2004 (Cluster)), and one trial did not report results by randomized comparisons and these data were therefore not used (Stephenson 1993).
Cognition
Fourteen trials measured intellectual development using formal tests.
School attendance
Six trials measured school attendance through school registers or by direct observation/follow‐up.
School performance
Hall 2006 (Cluster), Liu 2017 (Cluster) and Miguel 2004 (Cluster) measured exam performance. Gateff 1972 measured school grades.
Measures of physical fitness
Three trials measured physical well‐being using the Harvard Step Test, 10 m shuttle run and VO2 max, grip strength and standing broad jump test (Stephenson 1989; Stephenson 1993; Yap 2014 (Screened)).
Mortality
Ndibazza 2012, Awasthi 1995 (Cluster), and Awasthi 2013 (Cluster) provided data on mortality.
Adverse events
Seven trials provided information on adverse events (Fox 2005; Garg 2002; Gateff 1972; Joseph 2015; Michaelsen 1985; Wiria 2013 (Cluster); Yap 2014 (Screened)).
Risk of bias in included studies
See Figure 3 and Figure 4 for ‘Risk of bias' summaries and Characteristics of included studies section for details of the risk of bias and methods used in each trial.
3.
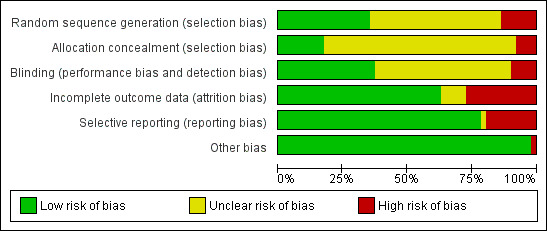
‘Risk of bias’ summary: review authors’ judgements about each risk of bias item presented as percentages across all included studies.
4.
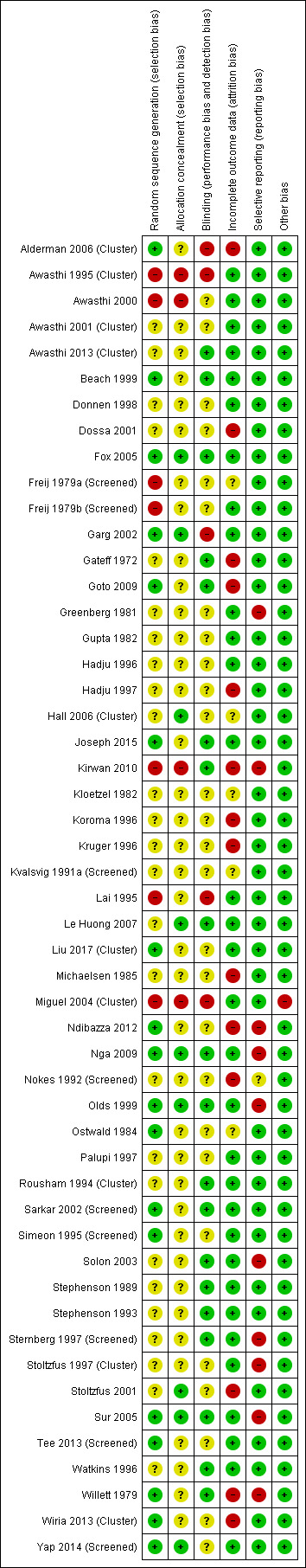
‘Risk of bias’ summary: review authors’ judgements about each risk of bias item for each included study.
Allocation
Sequence generation
In the 41 individually‐randomized trials, the risk of bias was low in 15 trials (see Figure 3 and Figure 4), high in five, and unclear in the other trials. For the 10 cluster‐RCTs, the risk of bias was low in three trials (Alderman 2006 (Cluster); Liu 2017 (Cluster); Wiria 2013 (Cluster)), high in two trials (Awasthi 1995 (Cluster); Miguel 2004 (Cluster)) and unclear in five trials (Awasthi 2001 (Cluster), Awasthi 2013 (Cluster), Hall 2006 (Cluster), Rousham 1994 (Cluster), Stoltzfus 1997 (Cluster).
Allocation concealment
For the 41 individually randomized trials, eight trials were at low risk of bias regarding allocation concealment (Fox 2005; Garg 2002; Le Huong 2007; Nga 2009; Olds 1999; Stoltzfus 2001; Sur 2005; Yap 2014 (Screened)), high in two trials (Awasthi 2000; Kirwan 2010), and unclear in the other trials.
The risk of bias was low in one of the 10 cluster‐RCTs (Hall 2006 (Cluster)), high in two trials (Awasthi 1995 (Cluster); Miguel 2004 (Cluster)), and unclear in the remaining seven trials.
Blinding
We judged 19 trials to be at low risk of bias due to use of blinding or objective outcomes. Five trials were at high risk of bias as they did not use blinding. Details of blinding were unclear in the remaining 27 trials.
Incomplete outcome data
Thirty‐two trials appeared to have low risk of bias in relation to outcome data. Overall, the percentage of randomized participants that were evaluable ranged from 4% to 100%, with 21 trials including 90% or more of the randomized participants (low risk cut‐off).
Fourteen trials were at a high risk of bias due to large amounts of missing data, ranging from 19% to 96%.
Selective reporting
Ten trials had evidence of selective reporting and were judged to be at high risk of bias (Greenberg 1981; Kirwan 2010; Koroma 1996; Ndibazza 2012; Nga 2009; Olds 1999; Solon 2003; Sternberg 1997 (Screened); Stoltzfus 1997 (Cluster); Sur 2005; Willett 1979). The remaining trials did not show evidence of selective reporting.
Other potential sources of bias
In general, quality of the design of the 10 cluster‐RCTs was good: they were judged as low risk for recruitment bias (six trials), baseline imbalance (nine trials), loss of clusters (nine trials), compatibility with RCTs that randomized individuals (one trial).These data are included in Characteristics of included studies.
There were problems with incorrect analysis noted above: Alderman 2006 (Cluster) did not adjust for clustering in the published trial, but gave us the adjusted data (see trial design above), and we used these data to adjust the analysis in Hall 2006 (Cluster).
One trial (Miguel 2004 (Cluster)) was potentially confounded by co‐interventions noted under ‘Accompanying health promotion activities' under interventions (above).
Effects of interventions
Summary of findings for the main comparison. Multiple doses of deworming drugs compared to placebo for soil‐transmitted intestinal worms in children.
| Multiple doses of deworming drugs compared to placebo for soil‐transmitted intestinal worms in children: effects on growth, haemoglobin, cognition, school attendance, school performance, physical fitness, and mortality | ||||||
| Patient or population: public health programmes to regularly treat all children aged 16 years or less Setting: areas endemic for intestinal helminths, or children screened for infection Intervention: multiple doses of deworming drugs Comparison: placebo | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Number of participants (trials) | Certainty of the evidence (GRADE) | Comments | |
| Risk with placebo | Risk with multiple doses of deworming drugs | |||||
| Weight (kg) follow‐up: 6 months to 3 years | The mean change in weight in the control arm ranged from 1.2 kg to 4.73 kg | The mean weight gain in the intervention groups was 0.11 kg more (0.01 kg less to 0.24 kg more) | ‐ | 52,448 (18 trials)a | ⊕⊕⊝⊝
Very low1,2,3 Due to risk of bias, inconsistency and indirectness |
We do not know if there is an effect on average weight change |
| Height (cm) follow‐up: 6 months to 2 years | The mean gain in height in the control groups ranged from 2.39 cm to 16.4 cm | The mean gain in height in the intervention groups was 0.02 cm higher (0.09 cm lower to 0.13 cm higher) | ‐ | 13,700 (13 trials)b | ⊕⊕⊕⊝
Moderate4 Due to risk of bias |
Probably little or no effect on height |
| Haemoglobin (g/dL) follow‐up: 5 months to 2 years | The mean change in haemoglobin in the control groups ranged from ‐0.4 g/dL to 1.99 g/dL | The mean haemoglobin in the intervention groups was 0.01 g/dL lower (0.05 g/dL lower to 0.07 g/dL higher) | ‐ | 5498 (9 trials)c | ⊕⊕⊕⊝
Moderate5 Due to risk of bias |
Probably little or no effect on haemoglobin |
| Formal tests of cognition follow‐up: 6 months to 2 years | ‐ | None of the trials reported a benefit of deworming across multiple tests6 | ‐ | 35,394 (8 trials)d | ⊕⊕⊕⊝
Moderate7 Due to risk of bias |
Probably little or no effect on cognition |
| Physical fitness ‐ not measured | ‐ | ‐ | ‐ | ‐ (0 trials) |
‐ | We do not know if there is an effect on physical fitness |
| School attendance follow‐up: 2 years (longest follow‐up) | The mean school attendance in the control groups ranged from 66% to 90% | The mean school attendance in the intervention groups was 2% higher (5% lower to 8% higher) | ‐ | 20,650 (3 trials)e,8 | ⊕⊝⊝⊝
Very low9,10,11 Due to risk of bias, imprecision and indirectness |
We do not know if there is an effect on school attendance |
| School performance follow‐up: 6 months to 2 years | ‐ | No difference in performance was detected in any trial | ‐ | 34,967 (4 trials)f | ⊕⊕⊕⊝
Moderate12 Due to risk of bias |
Probably little or no effect on school performance |
| Mortality (between ages 1 and 6 years) | 27 per 1000 | 25 per 1000 | RR 0.95 (0.89 to 1.92)g | 1,005,135 (3 trials)h | ⊕⊕⊝⊝
Low13,14 Due to risk of bias and indirectness |
May be little or no effect on mortality |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio; OR: odds ratio. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: we have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1Downgraded by 1 for risk of bias: all trials except one had high or unclear risk of selection bias. 2Downgraded by 1 for inconsistency: one trial had a large effect and in a sensitivity analysis only including high quality trials the heterogeneity was considerably reduced. This trial was from a low prevalence setting (Awasthi 1995 (Cluster); 0.98 kg). A subsequent trial in the same trial area as Awasthi 1995 (Cluster) found no effect. 3Downgraded by 1 for indirectness: the average effect is seen in two trials from the same population of heavily infected children in Kenya from 25 years ago, and one trial from India in a low prevalence setting. Subsequent trials have generally shown no average effect. The meta‐analysis point estimate of 0.11 kg mean difference (95%CI ‐0.01 to 0.24) for all studies compares with meta‐analysis point estimate of 0.02 (95%CI ‐0.04 to 0.08) in an analysis excluding trials published before 2000 4Downgraded by 1 for risk of bias: two trials were considered at high risk of selection bias (Awasthi 2000; Awasthi 1995 (Cluster)), and in the remaining trials the risk was unclear. 5Downgraded by 1 for risk of bias: two trials (Awasthi 2000; Kirwan 2010) were considered at high risk of selection bias and five trials (Dossa 2001; Goto 2009; Kirwan 2010; Kruger 1996; Ndibazza 2012) were considered high risk of incomplete outcome data bias; in the remaining trials the risk was low or unclear. 6Awasthi 2000, with a follow‐up of two years, reported that there was no difference in development between treatment groups in terms of proportion with "normal" development. Ndibazza 2012 measured a range of cognitive tests with a follow‐up post‐treatment and found no effect of deworming. Miguel 2004 (Cluster) measured a range of cognitive tests with a follow‐up of two years, but no deworming effect was demonstrated. Stoltzfus 2001, with a follow‐up of 12 months, found that treatment had no significant effect on motor or language development. Watkins 1996, with a follow‐up of six months, found no difference on any of the tests between treatment groups. Liu 2017 (Cluster) measured development using the Bayley Scales of Infant and Toddler Development and found no effect of deworming. Joseph 2015 measured processing speed and working memory and found no effect on either measure. Simeon 1995 (Screened) measured intellectual development using a wide range achievement test in the main trial, and digit spans and verbal fluency tests in subgroups. The trial authors reported that deworming had no effect on intellectual development scores, but did not report the data. 7Downgraded by 1 for risk of bias: two trials were considered at high risk of selection bias (Awasthi 2000; Miguel 2004 (Cluster)), and in the remaining trials the risk was low or unclear. 8The meta‐analysis includes the two year follow‐up for Miguel 2004 (Cluster). The trial has one‐year follow‐up on two other quasi‐randomized comparisons. These results are shown in Table 2. These demonstrate higher participation in both arms (9.3% and 5.4%) but these estimates are not independent because the control group in one comparison becomes the intervention group in the subsequent year. One additional trial showed no effect but did not provide measures of variance. 9Downgraded by 1 for risk of bias: Miguel 2004 (Cluster) had a high risk of bias for sequence generation, allocation concealment and blinding. 10Downgraded by 1 for imprecision: CIs include 4% lower attendance with deworming to 8% higher. 11Downgraded by 1 for indirectness: the intervention included a comprehensive health education programme in schools, and it not possible to determine which component of the complex intervention led to effects on attendance. 12Downgraded by 1 for risk of bias: Miguel 2004 (Cluster) had a high risk of bias for sequence generation, allocation concealment and blinding. 13Downgraded by 1 for risk of bias: none of the trials adequately described allocation concealment to be considered low risk of bias. 14Downgraded by 1 indirectness: DEVTA was conducted in a low prevalence area and the findings may not be generalizable to higher prevalence areas. aSix cluster‐RCTs (464 clusters, ˜47,000 participants) and 12 individually‐RCTs (5280 participants). bThree cluster‐RCTs (286 clusters, ˜9400 participants) and 10 individually‐RCTs (4300 participants). cOne cluster‐RCT (112 clusters, 2178 participants) and eight individually‐RCTs (3320 participants). dTwo cluster‐RCTs (32,028 participants) and six individually‐RCTs (3366 participants). eOne cluster‐RCT (50 clusters, 20,000 participants) and two individually‐RCTs (650 participants). fThree cluster‐RCTs (234 clusters) and one individually‐RCT (1423 participants). DEVTA dwarfs the other trials, none of which were adequately powered. gResults based on one trial (DEVTA) only. hTwo cluster‐RCTs (158 clusters) and one individually‐RCT (1423 participants). DEVTA dwarfs the other trials, none of which were adequately powered.
Summary of findings 2. A single dose of deworming drugs compared to placebo for soil‐transmitted intestinal worms in children.
| A single dose of deworming drugs compared to placebo for soil‐transmitted intestinal worms in children: effects on growth, haemoglobin, cognition, school attendance, school performance, physical fitness, and mortality | ||||||
| Patient or population: public health programmes to regularly treat all children aged 16 years or less Setting: areas endemic for intestinal helminths, or children screened for infection Intervention: a single dose of deworming drugs Comparison: placebo | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | Number of participants (trials) | Certainty of the evidence (GRADE) | Comments | |
| Risk with placebo | Risk with a single dose of deworming drugs | |||||
| Weight (kg) follow‐up: 4 weeks to 1 year | The mean weight gain in the control group ranged from 0.45 kg to 2.2 kg | The mean weight gain in the intervention group was 0.23 kg more (0.05 kg more to 0.42 kg more) | ‐ | 4970 (14 RCTs) | ⊕⊝⊝⊝
Very lowa,b,c Due to risk of bias, inconsistency, and indirectness |
We do not know if there is an effect on average weight gain |
| Height (cm) follow‐up: 9 weeks to 1 year | The mean height gain in the control group ranged from 1.1 cm to 4.59 cm | The mean height gain in the intervention group was 0.04 cm higher (0.14 cm lower to 0.23 cm higher) | ‐ | 2621 (10 RCTs) | ⊕⊕⊝⊝
Lowa,b Due to risk of bias and inconsistency |
There may be little or no effect on average height gain |
| Haemoglobin (g/dL) follow‐up: 9 weeks to 6 months | The mean change in haemoglobin in the control groups ranged from ‐0.9 to 0.64 g/dL |
The mean change in haemoglobin in the intervention groups was 0.10 g/dL higher (0.03 lower to 0.22 higher) | ‐ | 1252 (5 RCTs) | ⊕⊕⊕⊝
Moderated Due to risk of bias |
Probably little or no effect on haemoglobin |
| Formal tests of cognition follow‐up: 1 to 4 months | Several different tests used across the 5 trials and results varied. The majority of trials did not demonstrate an effect. | Not pooled | 1596 (5 RCTs) | ⊕⊕⊝⊝
Lowb,e Due to risk of bias |
There may be little or no effect on cognition | |
| Physical fitness follow‐up: 6 to 8 months | Trials used different measures of physical fitness, and reported results were inconsistent. | Not pooled | 280 (3 RCTs) | ⊕⊝⊝⊝
Very lowf,g Due to risk of bias and indirectness |
We do not know if there is an effect on physical fitness | |
| School attendance follow‐up: 3 months |
No difference in number of days absent in school was detected in the trial. | ‐ | 304 (1 RCT) |
⊕⊕⊝⊝
Lowh,i Due to risk of bias and imprecision |
There may be little or no effect on school attendance | |
| School performance follow‐up: 3 months |
No difference in school grades was detected in the trial. | ‐ | 304 (1 RCT) |
⊕⊕⊝⊝
Lowh,i Due to risk of bias and imprecision |
There may be little or no effect on school performance | |
| Mortality | No trials reported on mortality | ‐ | 0 (0 RCT) | N/A | N/A | |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: we have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
aDowngraded by 1 for risk of bias: most trials did not adequately describe allocation concealment. bDowngraded by 1 for inconsistency: there is a high level of heterogeneity. cDowngraded by 1 for indirectness: the effect estimate is pulled by studies where the density of worms is much higher than those found now. dDowngraded by 1 for risk of bias: two trials did not adequately describe allocation concealment to be considered low risk of selection bias. eDowngraded by 1 for risk of bias: Kvalsvig 1991a (Screened), with a follow‐up of one month, did not clearly report the changes in cognitive scores since quote: "the dose of mebendazole was inadequate to free children from infection". Nokes 1992 (Screened), with a follow‐up of nine weeks, reported that results of a multiple regression suggest a greater improvement in treated children in 3/10 tests (fluency, digit span forwards, digit span backwards). In the Philippines Solon 2003 reported deworming either had no effect or a negative effect on cognitive test scores, and in Vietnam Nga 2009 reported no difference detected. In Jamaica, Sternberg 1997 (Screened) reported that deworming had no significant effect on any of the cognitive tests. We could not combine data. fDowngraded by 2 for risk of bias: only one of the trials adequately described allocation concealment to be considered low risk of selection bias. Two trials conducted Harvard step tests on small non‐random samples of larger trials. gDowngraded by 1 for indirectness: Small differences in Harvard Step tests in two older trials in Kenya; no differences detected in VO2 and other parameters in a third trial with a small number of participants suggested no differences. hDowngraded by 1 for risk of bias: the trial did not adequately describe allocation concealment. iDowngraded by 1 for imprecision: only one small trial provided data for this outcome.
We stratified the results by worm burden. Within each section, we present the results of the meta‐analysis, and then report any other data from trials that we could not include in the meta‐analysis.
For a trial completed in 2006 but never published, the trial authors provided a manuscript with data we were able to use (Hall 2006 (Cluster)). For Alderman 2006 (Cluster), the trial authors did not adjust the confidence intervals (CIs) to take into account clustering for the primary outcome. For this Cochrane Review, we used the corrected values supplied by the trial author. Weight and height data for Liu 2017 (Cluster), Ndibazza 2012 and Wiria 2013 (Cluster) were provided by the authors of the recent Campbell review (Welch 2016). However, we have not included data for Wiria 2013 (Cluster) in the meta‐analysis as there was a great deal of missing data. At the nine‐month follow‐up analysis, data were available for less than 16% of the 4004 individuals who were included in the trial (for both change score data and end values), and at the 21‐month follow‐up analysis, data were available for 13% of the 4004 individuals (end values data only).
Single dose of deworming drugs
See Table 3.
Growth
For weight, across all burden groups (high, intermediate and low), the mean difference (MD) in weight was 0.23 kg (95% CI 0.05 to 0.42; 14 trials; 4970 participants; Analysis 1.1) favouring deworming but with high heterogeneity (Chi² = 137.48, df = 14, P < 0.00001; I² = 90%; Analysis 1.1). The test for subgroup differences indicated the mean differences differed across disease burdens (Chi² = 6.86, df = 2 ,P = 0.03; I² = 70.9%). With high burden, the mean difference for weight is 0.57 kg (95% CI 0.08 to 1.06; 8 trials; 1221 participants; Analysis 1.1) favouring deworming but with high heterogeneity across trials (Chi² = 76.95, df = 7, P < 0.00001; I² = 91%; Analysis 1.1). Large effects were seen in two trials with an average weight gain of over one kg in both trials (Stephenson 1989; Stephenson 1993). These trials were in a high prevalence area of Kenya. With intermediate burden (2 trials) and low disease burden (four trials), there was no difference in weight with low and moderate heterogeneity, respectively (Analysis 1.1).
1.1. Analysis.
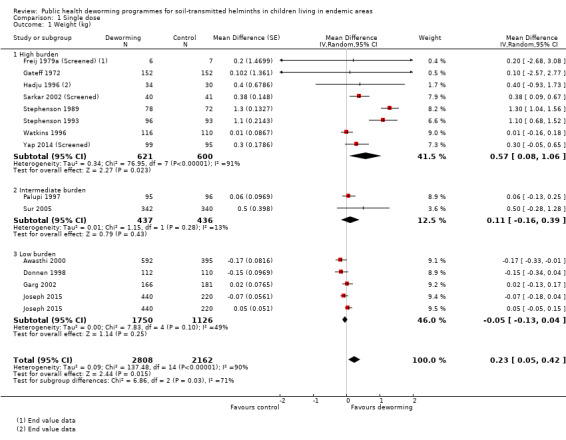
Comparison 1 Single dose, Outcome 1 Weight (kg).
Sensitivity analysis excluding trials that only reported end values did not affect point estimates or account for any heterogeneity.
For height, across all burden groups (high, intermediate and low), there was no difference in height (10 trials; 2621 participants; Analysis 1.2), but with high heterogeneity (Chi² = 28.98, df = 9, P=0.0007; I²=69%; Analysis 1.2). The test for subgroup differences indicated the mean differences differed across disease burdens (Chi² = 6.96, df = 2, P = 0.03; I² = 71.3%). With high burden (6 trials; 874 participants), intermediate burden (1 trial; 191 participants) and low disease burden (3 trials; 1556 participants), there was no difference in height with high heterogeneity for each burden group (Analysis 1.2).
1.2. Analysis.
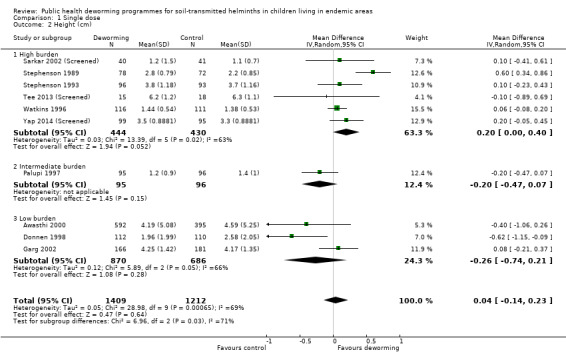
Comparison 1 Single dose, Outcome 2 Height (cm).
For mid‐upper arm circumference (MUAC), across all burden groups (high, intermediate and low), there was no difference in MUAC (7 trials; 1307 participants; Analysis 1.3) but with high heterogeneity (Chi² = 57.35, df = 7, P < 0.00001; I² = 88%; Analysis 1.3). The test for subgroup differences indicated the mean differences differed across disease burdens (Chi² = 15.75, df = 2, P = 0.03; I² = 87.3%). With high burden, the mean difference for MUAC is 0.32 cm (95% CI 0.06 to 0.57; 5 trials; 603 participants; Analysis 1.3) favouring deworming, but with high heterogeneity across trials (Chi² = 27.15, df = 4, P < 0.0001; I² = 85%; Analysis 1.3). With intermediate burden (1 trial; 482 participants), there was no difference in MUAC with no heterogeneity (Analysis 1.3). With low burden, the mean difference for MUAC is 0.30 cm (95% CI ‐0.52 to ‐0.08; 1 trial; 222 participants; Analysis 1.3) favouring control.
1.3. Analysis.
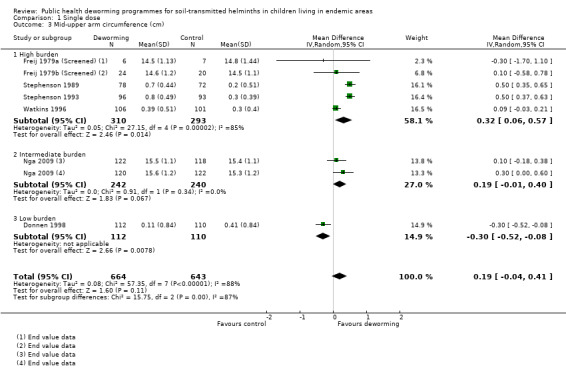
Comparison 1 Single dose, Outcome 3 Mid‐upper arm circumference (cm).
For triceps skinfold thickness, all trials were carried out in areas with high burden; the mean difference for triceps skinfold thickness is 1.34 mm (95% CI 0.72 to 1.97; 3 trials; 352 participants; Analysis 1.4) favouring deworming but with high heterogeneity across trials (Chi² = 15.21, df = 2, P=0.0005; I² = 87%; Analysis 1.4).
1.4. Analysis.
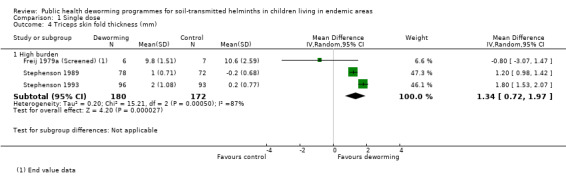
Comparison 1 Single dose, Outcome 4 Triceps skin fold thickness (mm).
For scapular skinfold thickness, all trials were carried out in areas with high burden; the mean difference for scapular skinfold thickness is 1.29 mm (95% CI 1.13 to 1.44; 2 trials; 339 participants; Analysis 1.5) favouring deworming but with low heterogeneity across trials.
1.5. Analysis.
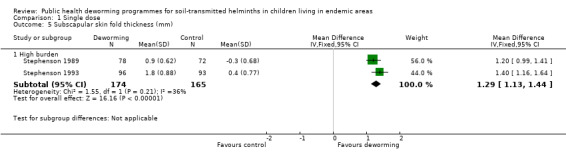
Comparison 1 Single dose, Outcome 5 Subscapular skin fold thickness (mm).
For body mass index (BMI), one trial was carried out in areas with high burden and showed no difference in BMI (407 participants; Analysis 1.6).
1.6. Analysis.
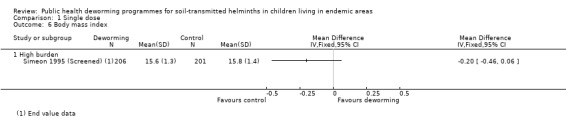
Comparison 1 Single dose, Outcome 6 Body mass index.
Haemoglobin
Two trials were in high, two trials in intermediate, and one in low prevalence/intensity areas. There was no difference in overall mean haemoglobin at the end of five trials with deworming (0.10 g/dL, 95% CI ‐0.03 to 0.22; 1252 participants, I² = 26%; five trials, Analysis 1.7).
1.7. Analysis.
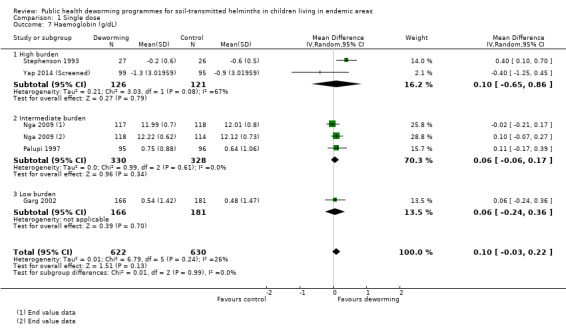
Comparison 1 Single dose, Outcome 7 Haemoglobin (g/dL).
Cognition
Five trials reported on formal tests (Table 2). Kvalsvig 1991a (Screened) did not clearly report change in cognitive scores; Nokes 1992 (Screened) did not report unadjusted data, but results of multiple regression suggested an improvement in treated children in three of the 10 tests carried out (fluency, digit span forwards, digit span backwards). Solon 2003 measured cognitive ability using a standardized written mental‐abilities test, and reported that deworming had either no effect or a negative effect on mental ability scores, but did not report the data. Nga 2009 reported no effects on any cognitive tests measured. Sternberg 1997 (Screened) found no significant effect on any of the 10 cognitive tests measured in the study.
1. Results: tests of cognition.
| Trial details | Outcome measures | Results |
| Single dose | ||
|
Kvalsvig 1991a (Screened) Mebendazole vs placebo, 1 month |
Card sorting task; cancellation task (number of letter 's' in text deleted in a time period). | Changes in cognitive scores are not clearly reported since quote: "the dose of mebendazole was inadequate to free children from infection". |
|
Nga 2009 Albendazole |
Cognitive performance was measured using Raven's Colored Matrices and also a series of cognitive tests from Wechsler's Intelligence Scale for Children III: digit span backward and forward, block design and coding. | Deworming had no significant effect on any of the cognitive tests. |
|
Nokes 1992 (Screened)
Albendazole vs placebo 2.25 months |
Digit span (forward and backward); arithmetic and coding from Wechsler Intelligence Scale for Children; fluency; listening comprehension from the Clinical Evaluation of Language functions; matching familiar figures test. | Mean test scores pre‐ and post‐intervention presented with CIs No comment made on significance of unadjusted data. Results of multiple regression suggest a greater improvement in treated children in 3/10 tests (fluency, digit span forwards, digit span backwards). |
|
Solon 2003
Albendazole vs placebo 16 weeks |
Cognitive ability was measured using a standardized written mental‐abilities test called the Primary Mental Abilities Test for Filipino Children (PMAT‐FC). The test covers general knowledge and comprehension, verbal relationships, fundamental mathematical comprehension and skills, numerical sequencing, and ability to perceive and apply relationships based on meaningless stimuli. | Deworming had either no effect or a negative effect on mental ability scores. Data was not reported. |
|
Sternberg 1997 (Screened) Albendazole vs placebo 2.3 months |
Perceptual speed (Visual Search, 1 and 2), motor speed (Grooved Pegboard‐Dominant Hand and Pegboard‐Nondominant Hand), memory (Free Recall, Digit Span Forward, and Digit Span Backward), and reasoning (Verbal Analogies and Figural Series Completions). | Deworming had no significant effect on any of the cognitive tests. |
| Multiple dose | ||
|
Awasthi 2000 Albendazole vs placebo, 2 years |
1045 participants. Developmental status (Denver Questionnaire). | No difference in development between treatment groups in terms of proportion with "normal" development. |
|
Joseph 2015 Mebendazole vs placebo, 1 year |
880 participants. Bayley Scales of Infant and Toddler Development, Third Edition (Bayley‐III) ‐ cognitive, receptive language, expressive language, and fine motor subtests. | There was no statistically significant benefit of deworming, or effect of timing or frequency, on cognition, language or fine motor development. |
|
Liu 2017 (Cluster) Albendazole vs no treatment, 6 months |
2028 participants. Processing Speed Index Score and Working Memory Index Score from the Mandarin‐language version of the latest Wechsler Intelligence Scale for Children Fourth Edition (WISC‐IV). | Deworming had no significant effect on either of the cognitive tests. |
|
Miguel 2004 (Cluster) Deworming package including albendazole vs placebo 1 year |
30,000 participants. Cognitive tests including picture search, Raven matrix, verbal fluency, digit span, Spanish learning, and a dynamic test using syllogisms measured for all three school groups in 2000. | Outcome data not reported for cognitive tests, though authors state: "Deworming treatment effects are not significantly different than zero for any component of the cognitive exam (results available on request)". |
|
Ndibazza 2012 Albendazole vs placebo, 3.5 years |
870 participants. Block design, Picture vocabulary scale, Sentence repetition, Verbal fluency, Counting span, Running memory, Picture search, Wisconsin card sort test, Tap once tap twice task, Shapes task, Tower of London. | Deworming had no significant effect on any of the cognitive tests. |
| Simeon 1995 (Screened) Albendazole vs placebo 6.5 months |
|
|
| Stoltzfus 2001 Mebendazole vs placebo, 1 year | 359 participants. Motor and language development by parents reporting gross motor and language milestones using scoring system developed specifically for the trial. | Unadjusted data not reported. Treatment had no significant effect on motor or language development. |
| Watkins 1996 Albendazole vs placebo, 6 months | 212 participants. Interamerican vocabulary test; Interamerican reading test; Peabody picture vocabulary test. | All outcome measures reported as unadjusted scores. No difference in any of the tests found between treatment groups. |
School attendance (days present at school)
Gateff 1972 found no effect of deworming on the number of days absent from school (Table 10).
8. Results: school attendance.
| Trial details | Outcome measures | Intervention | Control | Difference |
| Single dose | ||||
| Gateff 1972 | Absenteeism at follow‐up N = 304 |
Not reported | Not reported | 0.05 (SE 2.29) |
| Multiple dose | ||||
| Gateff 1972 | Absenteeism at follow‐up N = 280 |
Not reported | Not reported | 0.31 (SE 5.13) |
| Kruger 1996 | Attendance at follow‐up only (class registers) N = 143 |
97.2% (iron group) 95.6% |
98% (iron group) 95.2% |
‐0.8% 0.4% |
| Liu 2017 (Cluster) | School attendance N = 2028 |
Baseline 87.3% (95% CI 85.3 to 89.4%) Follow‐up 85.30% (95% CI 82.95 to 87.66) |
Baseline 86.7% (95% CI 84.7 to 88.8%) Follow‐up 86.13% (95% CI 83.81 to 88.45) |
0.93% (95% CI 0.57 to 1.54) |
|
Miguel 2004 (Cluster) Group 1 versus 2+3 (1‐year follow‐up) |
School participation N = 30,000 |
84.1% | 73.1% (group 2) 76.6% (group 3) |
9.3% (SE 3.0%) |
|
Miguel 2004 (Cluster) Group 2 versus 3 (1‐year follow‐up) |
School participation N = 20,000 |
71.8% | 66.4% |
5.4% (SE 2.7%) |
|
Miguel 2004 (Cluster) Group 1 versus 3 1999 (2‐year follow‐up) |
School participation N = 20,000 |
71.6% | 66.4% |
5.1% (SE 2.7) |
| Simeon 1995 (Screened) Albendazole vs placebo 6.5 months | Mean % attendance (class registers ) N = 264 |
Baseline 62.6 (SD 20.4) Follow‐up 67.3 (SD 18.4) |
Baseline 66.3 (SD 20.8) Follow‐up 69.3 (SD 17.5) |
2.0% |
| Watkins 1996 6 months | Attendance rates of children actively attending school. N = 243 |
Baseline 92%,
SEM = 1 Follow‐up 88%, SEM = 1 |
Baseline 0.90,
SEM = 1 Follow‐up 89% SEM =1 |
‐3% |
CI: confidence interval; SD: standard deviation; SE: standard error; SEM: standard error of the mean
School performance
Gateff 1972 reported that there were no significant effects of deworming on school grades (Table 11).
9. Results: school performance.
| Trial details | Outcome measures | Results |
| Single dose | ||
|
Gateff 1972 Thiabendazole versus placebo, 3 months |
304 participants. Grades | No statistically significant differences at follow‐up. |
| Multiple dose | ||
|
Gateff 1972 Thiabendazole versus placebo, 8 months |
280 participants. Grades | No statistically significant differences at follow‐up. |
|
Hall 2006 (Cluster) Albendazole versus placebo, 2 years |
2659 participants. Mathematics test score, Vietnamese test score. | No statistically significant differences in test results at start or end of trial. |
|
Liu 2017 (Cluster) ALbedazole versus no treatment, 6 months |
2028 participants. Normalized TIMMS score | There was no significant between‐group difference at follow‐up . |
|
Miguel 2004 (Cluster) Deworming package including albendazole versus placebo |
30,000 participants. Exam score performance (measured by Internationaal Christelijk Steunfonds Africa (ICS) administered English, Mathematics and Science‐Agriculture exams) in pupils in grades 3 to 8. | In the original trial and the pure replication, the trial authors reported no significant difference, but data was not reported. In the statistical replication, this was confirmed. |
TIMMS: Trends in International Mathematics and Science Study
Measures of physical fitness
Two trials in the same high prevalence area of Kenya measured performance on the Harvard Step Test in non‐randomly selected subgroups (Stephenson 1989; Stephenson 1993), and both indicated benefit. Yap 2014 (Screened) found no effect on any of the measures of physical fitness (Table 12).
10. Results: measures of physical fitness.
| Trial details | Outcome measures | Results |
| Single dose | ||
|
Yap 2014 (Screened) Albendazole |
VO2 max estimate (mL kg‐1 min‐1), 20 m running laps completed grip strength (kg), standing broad jump distance (cm). Mean values reported. | No effect was detected on any of the measures of physical fitness (99 in the albendazole group and 95 in the control) |
|
Stephenson 1989 Albendazole versus placebo, 6 months follow‐up |
Harvard Step Test | Deworming significantly improved children’s physical fitness in a non‐randomly selected subgroup of children (33/171) Treatment group: mean = 80, SD = 5.51, N = 18 Placebo group: mean = 74, SD = 4.65, N = 15 MD = 6.00, 95% CI 2.53 to 9.4 |
|
Stephenson 1993 Albendazole versus placebo, 8 months follow‐up |
Harvard Step Test | Deworming significantly improved children’s physical fitness in a non‐random subgroup of children (54/328) Treatment group: mean = 82, SD = 3.64, N = 27 Placebo group: mean = 76, SD = 3.57, N = 26 MD = 6.00, 95% CI 4.06 to 7.94 |
CI: confidence interval; MD: mean difference; SD: standard deviation
Mortality
No trials measured mortality.
Adverse events
Fox 2005 reported none in 46 patients given albendazole. Michaelsen 1985 reported a number of adverse events with tetra‐chloroethylene, a drug no longer used (Table 13).
11. Results: data not included in meta‐analysis.
| Single dose | |
| Beach 1999 Albendazole |
A nutritional benefit of treatment was not detectable after four months for the entire trial population (853 participants, no figures provided). Stratification by infection demonstrated small positive effects in the treatment group for some anthropometric outcomes. In Ascaris‐infected children (51), height gain was 0.62 cm > placebo in the combination treatment group (P = 0.01) at 4 months. In Trichuris‐infected children (158), weight gain was 0.56 kg > placebo in the combination treatment group (P = 0.01) at 4 months. |
| Fox 2005 Albendazole |
No results provided for whole trial population. Results for height and weight only presented in the narrative for subgroups infected with hookworm and Ascaris: no significant anthropometric changes detected (no figures quoted). In those infected with Trichuris, weight gain was greater in the albendazole group (difference compared to placebo 0.28 kg, P = 0.038). Adverse events: no serious adverse events (albendazole 0/46 versus placebo 0/43). Myalgia and cough were reported significantly more frequently in the placebo group compared to albendazole. |
| Greenberg 1981 Piperazine citrate |
Treatment group tended to show worse nutrition than placebo. Comparison showed no significant difference for all measured anthropometric variables for the total group and for subgroups defined by severity of infection (no figures provided). |
| Kloetzel 1982 Mebendazole |
No significant difference was found between the groups. Results reported as the proportion of treatment or control group that improved, deteriorated, or experienced no change. Unclear which anthropological measures were used in this categorization process. Proportions in each category were not significantly different between trial arms (improved: 51% in mebendazole group versus 49% in control; deteriorated: 35% in mebendazole group versus 33% in control; no change: 14% in mebendazole group versus 18% in control; no significance test results quoted). |
| Koroma 1996 Albendazole | Significant increases in weight‐for‐height, weight‐for‐age, and height‐for‐age z‐scores recorded in rural and urban treatment groups at six months. Mean increase in rural treatment group compared to placebo: weight‐for‐height z‐score 0.28 (SE 0.17) P < 0.05; weight‐for‐age z‐score 1.04 (SE 0.03) P < 0.05; and height‐for‐age z‐score 0.83 (SE 0.03) P < 0.001. Mean increase in urban treatment group compared to placebo: weight‐for‐height z‐score 1.04 (SE 0.07) P < 0.05; weight‐for‐age z‐score 1.02 (SE 0.09) P < 0.001; and height‐for‐age z‐score 1.01 (SE 0.02) P <0.05. |
| Michaelsen 1985 Tetra‐chlorethylene |
No significant difference in change in mean for haemoglobin. (tetrachloroethylene 0.22 g/100 mL versus placebo 0.09 g/100 mL; quoted as non‐significant) or weight for height at five months (tetrachloroethylene ‐1.3% of WHO reference mean vversus placebo ‐0.4%; quoted as non‐significant). Adverse events: 17% (19/119: results not given for separate trial arms) of the children suffered adverse effects (nausea and ataxia) that began one and a half hours after treatment. All symptoms disappeared within four hours. Tetrachlorethylene is not in current use as a deworming drug. |
|
Nga 2009 Albendazole |
No significant differences in weight‐for‐height, weight‐for‐age, and height‐for‐age z‐scores and skin fold thickness at four months. There was no statistically significant effect of deworming on weight, height, HAZ scores, WAZ scores, or WHZ scores. There were no statistically significant differences in skin fold thickness after four months of intervention. |
| Nokes 1992 (Screened) Albendazole | Growth measured but not reported: nine weeks cited as too short a follow‐up period to demonstrate a change. |
|
Tee 2013 (Screened) Albendazole |
No significant differences in median change in weight and weight‐for‐height z‐scores, and for mean change in weight‐for‐age, and height‐for‐age z‐scores at 12 months follow‐up. Weight: Median change in weight at follow‐up in treatment group 2.6 (range 1.2 to 7.2) and control group 2.5 (range 1.2 to 6.6) Height‐for‐age z‐score: Mean change at follow‐up in treatment group 1.1 (0.2) and in control group 1.1 (0.2). Weight‐for‐age z‐score: Median change at follow‐up in treatment group ‐1.0 (range 0.6 to 2.3) and in control group 0.8 (range 0.5 to 1.6). Weight‐for‐height z‐score: Mean change at follow‐up in treatment group 0.5 (0.6) and in control group 0.1 (0.6). |
|
Yap 2014 (Screened) Albendazole |
No significant differences in percentage stunted and sum of skinfolds at 6 months follow‐up. Percentage stunted (≤ ‐2 HAZ score): Mean at follow‐up in treatment group 66% (mean change from baseline ‐7.0) and in control group 69% (mean change from baseline ‐7.4). Sum of skinfolds: Mean at follow‐up in treatment group 12 mm (mean change from baseline 1 mm) and in control group 12 mm (mean change from baseline 1 mm). |
| Multiple dose | |
|
Awasthi 1995 (Cluster) Albendazole |
During the trial there were 23 deaths, 13 were in the usual care arm and 10 were in the treatment arm. These data were not adjusted for cluster randomization. |
|
Awasthi 2013 (Cluster) Albendazole |
Deworming showed no effect for death MD in deaths per child‐care centre at ages 1·0–6·0 was 0·16 (SE 0·11); mortality ratio 0·95, 95% CI 0·89 to 1·02). |
|
Gateff 1972 Thiabendazole |
Deworming group had significantly more adverse events The thiabendazole group showed statistically significant more adverse events than the control group, 76.2% versus 34.8%. The following symptoms were measured: vertigo, nausea or vomiting, headache, colic, asthenia or drowsiness. |
| Goto 2009 Albendazole plus secnidazole | No significant differences in mean z‐scores or prevalence of stunting, underweight or wasting between the intervention groups were found, and the changes between intervals (eg between weeks 0 to 12, 0 to 24, 0 to 36, 12 to 24, etc.) did not differ significantly between groups. Height‐for‐age z‐score: at baseline in treatment group ‐1.08 (1.02) and in control group ‐1.21 (1.0). At follow‐up in treatment group ‐1.59 (0.93) and in control group ‐1.70 (0.93). Weight‐for‐age z‐score: at baseline in treatment group ‐1.91 (1.15) and in control group ‐1.85 (1.14). At follow‐up in treatment group ‐2.62 (1.17) and in control group ‐2.59 (1.17). Weight‐for‐height z‐score: at baseline in treatment group ‐1.25 (1.18) and in control group ‐0.96 (1.17). At follow‐up in treatment group ‐1.55 (1.07) and in control group ‐1.83 (1.06). |
| Hadju 1997 Pyrantel pamoate Albendazole | No significant differences detected between treatment groups on basis of multivariate analyses controlling for age, sex, and ‘times’. Change in weight‐for‐age z‐score: placebo 0.02; pyrantel 1 x treatment 0.03; pyrantel 2 x treatments 0.08; albendazole 1 x treatment ‐0.10; albendazole 2 x treatments 0.01. Change in height‐for‐age z‐score: placebo 0.01; pyrantel 1 x treatment 0.00; pyrantel 2 x treatments 0.04; albendazole 1 x treatment ‐0.07; albendazole 2 x treatments 0.01. Change in weight‐for‐height z‐score: placebo 0.02; pyrantel 1 x treatment 0.08; pyrantel 2 x treatments 0.05; albendazole 1 x treatment ‐0.07; albendazole 2 x treatments 0.03. Change mid‐arm circumference z‐score: placebo ‐0.09; pyrantel 1 x treatment ‐0.11; pyrantel 2 x treatments ‐0.11; albendazole 1 x treatment ‐0.07; albendazole 2 x treatments ‐0.01. |
| Hall 2006 (Cluster) Albendazole |
Trial authors reported no difference in final and change in height. MUAC and subscapular skinfold thickness improved significantly in the control group compared to the albendazole group (7.87 versus 7.61, P = 0.005 and 1.22 versus 1.05, P = 0.005, respectively). These results do not appear to have been adjusted for cluster randomization. The results that show no effect, however, will not remain non‐significant even after appropriate adjustment, though the CIs may change. |
|
Joseph 2015 Mebendazole |
No significant difference in WAZ or LAZ between treatment and control group. There were no statistically significant differences in the number of adverse events and serious adverse events. Change in weight‐for‐age Z‐score: placebo ‐0.28 (95%CI ‐0.34 to ‐0.22); mebendazole ‐0.24 (95%CI ‐0.30 to ‐0.22). Change in length‐for‐age Z‐score: placebo ‐0.59 (95%CI ‐0.66 to ‐0.52); mebendazole ‐0.56 (95%CI ‐0.62 to ‐0.49). Adverse events: there were 14 adverse events in the mebendazole group and 13 in the placebo group. Serious adverse events: there were 5 serious adverse events in the mebendazole group and 5 in the placebo group. |
| Lai 1995 Mebendazole plus pyrantel | No difference in height or weight between treatment and control group at the end of 2‐year follow‐up. SDs not provided. Results stratified for males and females: Females: change in height in treatment arm 12.2 cm versus change in height in placebo arm 12.4 cm; change in weight in treatment arm 5.6 kg versus change in weight in placebo arm 5.6 kg. Males: change in height in treatment arm 11.8 cm versus change in height in placebo arm 11.4 cm; change in weight in treatment arm 5.7 kg versus change in weight in placebo arm 4.7 kg. |
| Le Huong 2007 Mebendazole |
No obvious trend in nutrition variable. Anthropometric indices were calculated using WHO/NCHS reference data. Being wasted, stunted and underweight was defined by z‐scores ,< ‐ 2 SD for weight‐for‐height, height‐for‐age and weight‐for‐age, respectively. Percentage underweight: At baseline Fe 41·9, Fe + MEB 51·9, MEB 50·6, Placebo 45·1; after treatment Fe 33·7, Fe + MEB 46·8, MEB 38, Placebo 35·4. Percentage stunted: At baseline Fe 30·2, Fe + MEB 31·6, MEB 41·8, Placebo 31·7; after treatment Fe 29·1, Fe + MEB 27·8, MEB 29·1, Placebo 29·3. Percentage wasted: At baseline Fe 9·3, Fe + MEB 16·5, MEB 13·9, Placebo 12·2; after treatment Fe 5·8, Fe + MEB 17·7, MEB 13·9, Placebo 13·4. |
|
Liu 2017 (Cluster) Albendazole |
No significant differences in HAZ and WAZ between treatment and control group Percentage stunted (HAZ<‐2): At baseline 29.7% in treatment group, 27.0% in control group; at 6 months follow‐up 27.63% in treatment group and 23.48% in control group. No significant between‐group difference at follow‐up (P = 0.367). Percentage underweight (WAZ<‐2): At baseline 28.9% in treatment group, 24.1% in control group; at 6 months follow‐up 24.19% in treatment group and 21.37% in control group. No significant between‐group difference at follow‐up (P = 0.113). |
|
Miguel 2004 (Cluster) Albendazole |
No effect on nutrition or haemoglobin demonstrated For haemoglobin a sample of around 4% (778/20,000) of the quasi‐randomized comparison of group 1 versus group 2 in 1998 was analysed. Height and weight data was collected on all individuals in standards 3‐8 (9102/20000) Difference in weight‐for age z‐score (treatment ‐ control): 0.00 (SE 0.04). Difference in height‐for‐age z‐score end value (treatment ‐ control): 0.09 (SE 0.05). Difference in haemoglobin (g/L) (treatment ‐ control): 1.6 (SE 1.4) |
|
Ndibazza 2012 Albendazole |
During the trial there were 16 ['s, 8 were in the placebo arm and 8 were in the treatment arm. No significant differences in mean z‐scores for weight‐for‐height, weight‐for‐age, and height‐for‐age z‐scores at 5 years of age. Height‐for‐age z‐score: mean difference at follow‐up in treatment group ‐0.43 (1.16) and in control group ‐0.35 (1.19). Weight‐for‐age z‐score: mean difference at follow‐up in treatment group ‐0.54 (0.91) and in control group ‐0.54 (0.93). Weight‐for‐height z‐score: at follow‐up in treatment group ‐0.26 (1.46) and in control group ‐0.28 (1.34). |
| Rousham 1994 (Cluster) Mebendazole |
ANOVAS of the change in z‐scores revealed no significant improvement with treatment. Change in weight‐for‐age and weight‐for‐height z‐scores were significantly worse in the treatment group. Height‐for‐age z‐score (mebendazole 0.25 versus 0.17 in placebo group, P 'non‐significant'), weight‐for‐age z‐score (mebendazole 0.03 versus 0.12 in placebo group, P < 0.05), weight‐for‐height z‐score (mebendazole ‐0.25 versus ‐0.05 in placebo group, P < 0.001), and MUAC were presented (mebendazole 0.33 versus 0.23 in placebo group, P 'non‐significant'). |
| Simeon 1995 (Screened) Albendazole | No significant difference in any reported outcome for whole group. Height‐for‐age z‐score at baseline in treatment group ‐0.48 (0.95) and in placebo group ‐0.39 (0.90). At follow‐up in treatment group ‐0.48 (0.97) and in placebo group ‐0.41 (0.89). Body mass index (kg/m²) at baseline in treatment group 15.3 (1.3) and in placebo group 15.5 (1.3). At follow‐up in treatment group 15.6 (1.3) and in placebo group 15.8 (1.4). |
| Stoltzfus 2001 Mebendazole |
Mebendazole is reported as significantly reducing the prevalence of mild wasting malnutrition in a subgroup of children aged < 30 months only adjusted odds ratio for mebendazole 0.38 (95% CI 0.16 to 0.90) for weight‐for‐height z‐score < ‐1. Mebendazole is reported as significantly reducing the prevalence of poor appetite across the whole group (adjusted odds ratio for mebendazole 0.52 (95% CI 0.30 to 0.89) for weight‐for‐height z‐score < ‐1). Mebendazole had no impact on iron indices. Adjusted effect on motor scores had a tendency to favour mebendazole, but this was not significant. |
| Stoltzfus 1997 (Cluster) Mebendazole |
Weight gain: in a subgroup of under 10 year olds, the twice‐yearly treated group experienced significantly greater weight gain (kg) compared to control (2.38 (SE 0.08) versus 2.11 (SE 0.08), P < 0.05). In the thrice‐yearly treatment group the difference was not significant (2.31 (SE 0.08) versus 2.11 (SE 0.08), no P value stated). Height gain: in under 10 year olds the thrice‐yearly treated group experienced significantly greater height gain (cm) compared to control (4.59 (SE 0.07) versus 4.29 (SE 0.07), P < 0.01). In the twice‐yearly treatment group the difference in height gain was not significant (4.42 (SE 0.07) versus 4.29 (SE 0.07), no P value stated). There were no significant differences found in the subgroup of children aged over 10 years. Haemoglobin change: deworming had no effect on haemoglobin change in an adjusted analysis presented for the whole trial group (g/L): control 11.3 (SE 1.7); twice‐yearly treatment group 10.3 (SE 1.7); and thrice‐yearly group 12.7 (SE 1.7). |
| Willett 1979 Levamisole |
No statistical difference in nutrition in terms of height and weight differences between the 2 groups. Growth rates presented are adjusted for a number of variables. Weight gain (kg/year) in levamisole group 2.08 versus 1.92 in placebo group (P = 0.06). Height gain (cm/year) in levamisole group 7.58 versus 7.73 in placebo group (no significance quoted). |
|
Wiria 2013 (Cluster) Albendazole |
No significant difference in weight and height at 21 months follow‐up in children aged 16 years and less. No adverse events reported. No significant difference in BMI at 21 months follow‐up in children aged 19 years and less. Weight: at 21 months follow‐up in treatment group mean 27.7kg (SD 10.1) N = 261 and in placebo group 29.3kg (SD 11.9) N = 263. Height: at 21 months follow‐up in treatment group mean 133.1cm (SD 15.0) N = 261 and in placebo group 133.8cm (SD 15.5) N = 263. Body mass index (kg/m2): median at follow‐up in treatment group 21.56 (IQR 19.44‐24.12) and in placebo group 22.42 (IQR 19.68 ‐ 25.56). |
Other data
Ten trials reported on results narratively without sufficient statistical parameters (number of children, measures of variance, for example, n = 8); or results reported as medians or changes in z‐scores (n = 2).
Details are in Table 13, and are summarized below. It is notable that eight of these trials stated narratively that no effect was detected, and only two report an effect.
Beach 1999 did not detect a nutritional benefit of treatment after four months for the entire trial population (no figures provided);
Fox 2005 only reported on subgroups infected with worms;
Greenberg 1981 stated there was no significant difference for all measured anthropometric variables for the total group and for subgroups defined by severity of infection (no figures provided).
Kloetzel 1982 reported the proportion of treatment or control group that improved, deteriorated, or experienced no change, but it is not known what anthropological measures were used.
Koroma 1996 found significant increases in weight‐for‐height, weight‐for‐age, and height‐for‐age z‐scores recorded in rural and urban treatment groups at six months.
Michaelsen 1985 found no significant difference in change in mean for haemoglobin or weight for height at five months.
Nga 2009 found no significant difference in weight‐for‐height, weight‐for‐age, and height‐for‐age z‐scores at four months.
Nokes 1992 (Screened) measured growth but did not report the results, as nine weeks was cited as too short a follow‐up period to demonstrate a change.
Tee 2013 (Screened) found no significant differences in median change in weight and weight‐for‐height z‐scores, and for mean change in weight‐for‐age, and height‐for‐age z‐scores at 12 month follow‐up.
Yap 2014 (Screened) found no significant differences in percentage stunted and sum of skinfolds at six‐month follow‐up.
Sensitivity analysis
In the sensitivity analysis including only trials where the risk of bias for allocation concealment was low, no difference between treatment and control groups in weight, height, MUAC, or haemoglobin was evident (Analysis 5.1; Analysis 5.2; Analysis 5.3; Analysis 5.4).
5.1. Analysis.
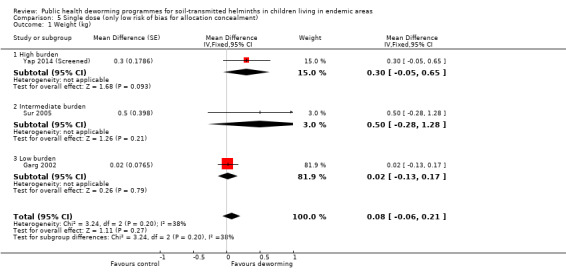
Comparison 5 Single dose (only low risk of bias for allocation concealment), Outcome 1 Weight (kg).
5.2. Analysis.
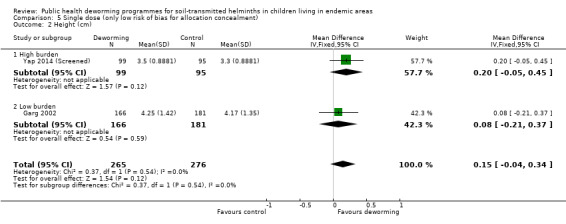
Comparison 5 Single dose (only low risk of bias for allocation concealment), Outcome 2 Height (cm).
5.3. Analysis.
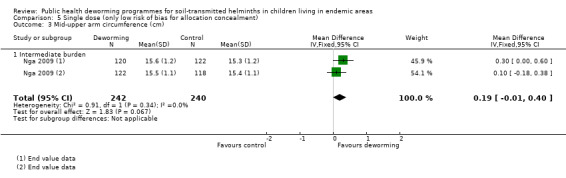
Comparison 5 Single dose (only low risk of bias for allocation concealment), Outcome 3 Mid‐upper arm circumference (cm).
5.4. Analysis.
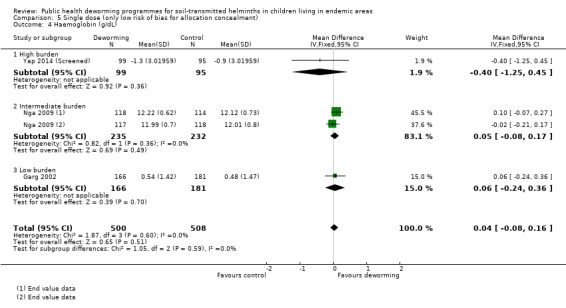
Comparison 5 Single dose (only low risk of bias for allocation concealment), Outcome 4 Haemoglobin (g/dL).
Multiple doses of deworming drugs
See Table 1.
Growth
Across all burden groups (high, intermediate, and low), no difference in weight was observed (18 trials, ˜40,000 participants from cluster trials and 6218 individually‐randomized participants, Analysis 2.1); high heterogeneity was observed in this analysis (Chi² = 89.05, df = 20, P < 0.00001, I2 = 78%). However, the test for subgroup differences indicated the mean differences did not differ across disease burdens (Chi² = 0.30, df = 2 (P = 0.86), I² = 0%). Large effects were seen in two trials with an average weight gain of almost 1 kg in the treatment groups (Stephenson 1993; Awasthi 1995 (Cluster)). Notably, two subsequent trials in the same area as Awasthi 1995 (Cluster) did not demonstrate an effect (Awasthi 2000; Awasthi 2001 (Cluster)).
2.1. Analysis.
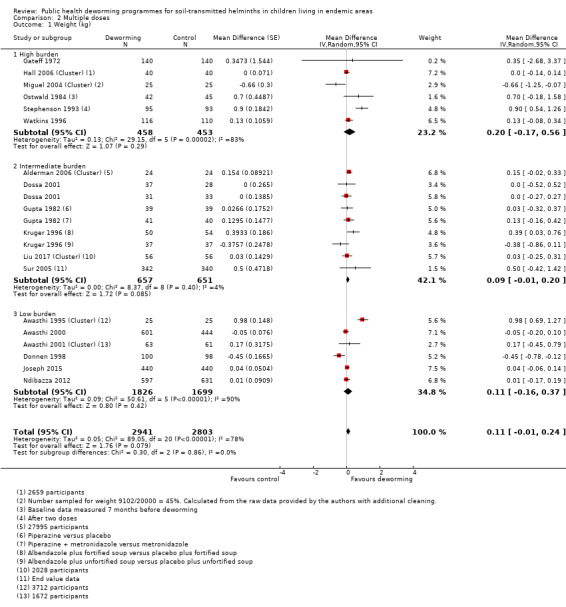
Comparison 2 Multiple doses, Outcome 1 Weight (kg).
A post‐hoc analysis excluding trials published prior to 2000 gave an estimate of average difference in weight gain of 0.02 kg (95% CI from 0.04 loss to 0.08 gain, 10 trials; 4328 participants; I2 = 0%, Analysis 7.2).
7.2. Analysis.
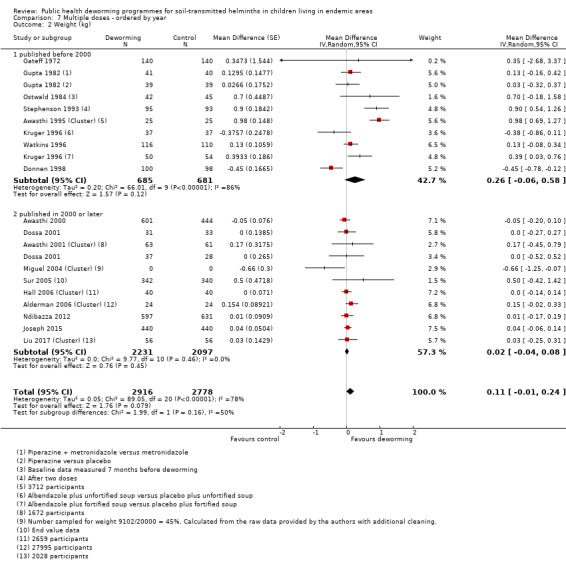
Comparison 7 Multiple doses ‐ ordered by year, Outcome 2 Weight (kg).
Sensitivity analysis excluding trials that only reported end values did not effect point estimates or account for any heterogeneity.
For height, across all burden groups, no difference in height was observed (˜9400 participants from cluster trials and 4300 individually‐randomized participants, 13 trials; Analysis 2.2). No heterogeneity was observed in this analysis (Chi² = 11.59, df = 15, P = 0.71, I2 = 0%).
2.2. Analysis.
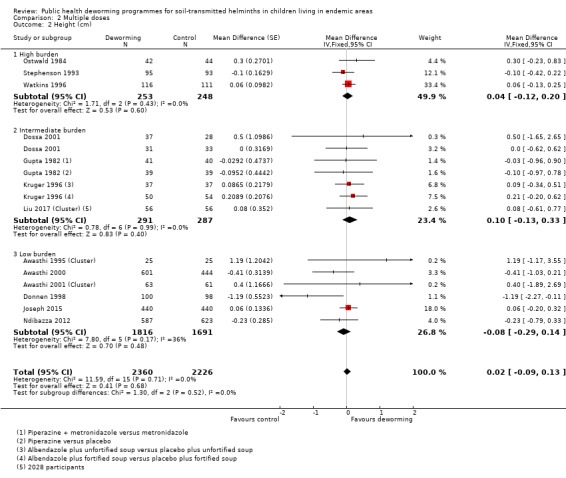
Comparison 2 Multiple doses, Outcome 2 Height (cm).
For MUAC, across all burden groups, no difference in MUAC was observed (Analysis 2.3); high heterogeneity was observed in this analysis (Chi² = 26.34, df = 4, P < 0.0001, I² = 85%). The test for subgroup differences indicated the mean differences differed across disease burdens (Chi² = 7.55, df = 2, P = 0.02; I² = 73.5%). With high burden, no difference in MUAC was observed (Analysis 2.3) with high heterogeneity across trials (Chi² = 11.26, df = 1, P = 0.0008; I² = 91%). With intermediate burden, no difference in MUAC was observed (Analysis 2.3) with no heterogeneity across trials (Chi² = 0.12, df = 1, P = 0.73; I² = 0%). With low burden, the mean difference for MUAC is ‐0.35 cm (95% CI ‐0.65 to ‐0.05; Analysis 2.3) favouring control. Only one trial (198 participants) contributed to the analysis in the low burden disease subgroup.
2.3. Analysis.
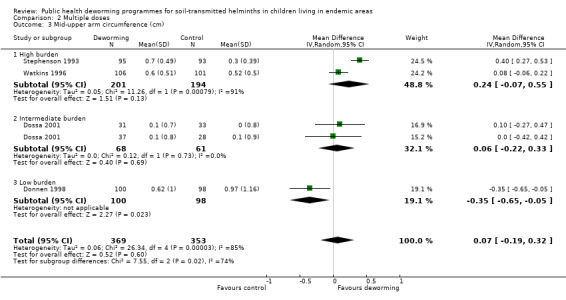
Comparison 2 Multiple doses, Outcome 3 Mid‐upper arm circumference (cm).
For triceps skinfold thickness, across all burden groups, no difference was observed (Analysis 2.4) with high heterogeneity (Chi² = 49.84, df = 2, P < 0.00001, I² = 96%). The test for subgroup differences indicated the mean differences differed across disease burdens (Chi² = 16.31, df = 1, P < 0.0001; I² = 93.9%). With high burden, the mean difference for triceps skinfold thickness is 1.80 mm (95% CI: 1.52 to 2.08, Analysis 2.4) favouring deworming; only one trial (188 participants) contributed data to this subgroup. With intermediate burden, no difference was observed (Analysis 2.4); high heterogeneity was observed in this analysis (Chi² = 3.36, df = 1, P = 0.07; I² = 70%).
2.4. Analysis.

Comparison 2 Multiple doses, Outcome 4 Triceps skin fold thickness (mm).
For subscapular skinfold thickness, Stephenson 1993 showed a gain of 1.5 mm in the treatment group (MD 1.50 mm, 95% CI 1.23 to 1.77; 188 participants, 1 trial, Analysis 2.5).
2.5. Analysis.
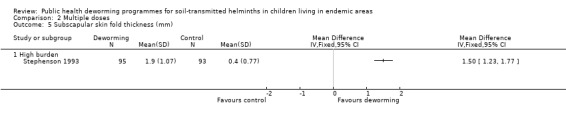
Comparison 2 Multiple doses, Outcome 5 Subscapular skin fold thickness (mm).
For BMI, Simeon 1995 (Screened) did not demonstrate a difference (Analysis 2.6). They also reported height for age z‐score and did not detect a difference (Table 13).
2.6. Analysis.
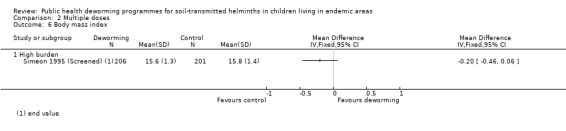
Comparison 2 Multiple doses, Outcome 6 Body mass index.
Haemoglobin
Nine trials reported this, with no difference between intervention and control apparent (Analysis 2.7). In addition, the re‐analysis of Miguel and Kremer (Aiken 2015) reported prevalence of anaemia rather than haemoglobin and found no difference between the groups ("‐2% absolute proportion").
2.7. Analysis.
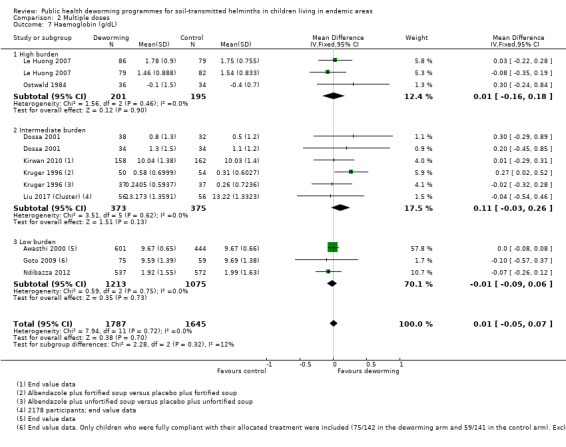
Comparison 2 Multiple doses, Outcome 7 Haemoglobin (g/dL).
Cognition
Eight trials (32,028 participants from cluster trials and 3366 individually‐randomized participants) measured this outcome (Table 2). Ndibazza 2012 measured a range of cognitive tests, Watkins 1996 measured reading and vocabulary, and Stoltzfus 2001 measured motor and language development. All reported that no effect was demonstrated. Miguel 2004 (Cluster) also measured a range of cognitive tests. The results were not reported, but the trial authors stated that no deworming effect was demonstrated. Awasthi 2000 measured developmental status using the Denver Questionnaire, and did not demonstrate an effect of deworming. Liu 2017 (Cluster) measured development using the Bayley Scales of Infant and Toddler Development and found no effect of deworming. Joseph 2015 measured processing speed and working memory and found no effect on either measure. Simeon 1995 (Screened) measured intellectual development using a wide range achievement test in the main trial, and digit spans and verbal fluency tests in subgroups. The trial authors reported that deworming had no effect on intellectual development scores, but did not report the data.
School attendance (days present at school)
Six trials reported on this outcome (Gateff 1972; Kruger 1996; Liu 2017 (Cluster); Miguel 2004 (Cluster); Simeon 1995 (Screened); Watkins 1996; Table 10). Watkins 1996 reported attendance rates of children actively attending school on the basis of school registers, at baseline and after treatment, and no effect was demonstrated. Miguel 2004 (Cluster) reported on end value differences in attendance for girls under 13 years of age and all boys based on direct observation. Gateff 1972 found no effect of deworming on the number of days absent from school (Table 10).
For outcomes measures at the longest follow‐up point, we found no difference in school attendance (MD 2%, 95% CI ‐5% to 8%; Analysis 2.8; 20,000 participants in one cluster trial and 650 participants from two individually‐randomized trials). This uses the longest point of follow‐up from Miguel 2004 (Cluster) at two years (group 1 versus group 3), in line with our analytical plan.
2.8. Analysis.
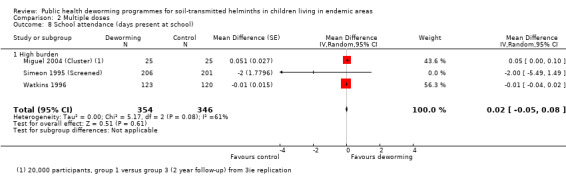
Comparison 2 Multiple doses, Outcome 8 School attendance (days present at school).
School performance
Four trials measured this (Gateff 1972; Hall 2006 (Cluster); Liu 2017 (Cluster); Miguel 2004 (Cluster); Table 11). Miguel 2004 (Cluster) measured exam score performance (English, Mathematics, and Science‐Agriculture exams in pupils in grades 3 to 8). Results showed no difference in performance. This included the results in the original trial analysis, Miguel 2004 (Cluster), in the analysis after coding errors had been corrected, Aiken 2015), and in the statistical replication, Davey 2015. Hall 2006 (Cluster) found no difference in test scores at the end of the trial. Gateff 1972 reported that there were no significant effects of deworming on school grades. Liu 2017 (Cluster) measures normalized Trends in International Mathematics and Science Study (TIMSS) scores and found no difference between groups at follow‐up.
Measures of physical fitness
No trials reported on measures of physical fitness.
Mortality
Deworming showed no effect in the DEVTA cluster trial of over one million children (Awasthi 2013 (Cluster)) in deaths per child‐care centre at ages 1.0 to 6.0 was 0.16 (standard error (SE) 0.11); mortality risk ratio (RR) 0.95, 95% CI 0.89 to 1.02). Ndibazza 2012 reported that during the trial there were 16 deaths, eight in the placebo arm and eight in the treatment arm. Awasthi 1995 (Cluster) reported 23 deaths during the trial, 13 of which were in the usual care arm, and 10 were in the treatment arm.
Adverse events
Wiria 2013 (Cluster) reported none in 3230 participants. Gateff 1972 found there were significantly more adverse effects in the group receiving thiabendazole. Joseph 2015 found no significant differences in adverse events and serious adverse events between groups (Table 13).
Other data
Fifteen trials did not provide data in a form that we could use in meta‐analysis. We have collated these data in Table 13 and Table 10, and have summarized this information below. Thirteen trials did not report statistically significant differences, and two reported significant differences for aspects of nutrition in subgroups of children.
Goto 2009 reported no significant differences in mean z‐scores or prevalence of stunting, underweight or wasting between the intervention groups, and the changes between intervals (i.e. between weeks 0 to 12, 0 to 24, 0 to 36, 12 to 24, etc.) did not differ significantly between groups.
Hadju 1997 reported no significant differences detected between treatment groups on basis of multivariate analyses for change in weight‐for‐age z‐score, change in height‐for‐age z‐score, change in weight‐for‐height z‐score and change mid‐arm circumference z‐score.
Hall 2006 (Cluster) reported no difference in final and change in height.
Joseph 2015 reported no significant differences in WAZ or LAZ between treatment and control group.
Kruger 1996 found that quote: "the rates of absenteeism were similar for all groups", but no measures of variance were provided.
Lai 1995 found no difference in height or weight between treatment and control group at the end of two‐year follow‐up.
Liu 2017 (Cluster) reported no significant differences in HAZ and WAZ between treatment and control group.
Le Huong 2007 reported no obvious trend in nutritional variable.
Miguel 2004 (Cluster) demonstrated no significant effect on weight‐for‐age z‐score, height‐for‐age z‐score, and haemoglobin.
Rousham 1994 (Cluster) reported that ANOVAS of the change in z‐scores revealed no significant improvement with treatment;
Ndibazza 2012 found no significant differences in mean z‐scores for weight‐for‐height, weight‐for‐age, and height‐for‐age z‐scores at five years of age.
Stoltzfus 2001 reported that mebendazole significantly reduced the prevalence of mild wasting malnutrition in a subgroup of children aged < 30 months.
Stoltzfus 1997 (Cluster) reported that in a subgroup of under 10 year olds, the twice‐yearly treated group experienced significantly greater weight gain (kg) compared to control (2.38 (SE 0.08) vs 2.11 (SE 0.08), P < 0.05).
Willett 1979 reported no statistical difference in growth rates in terms of height and weight between the two groups.
Wiria 2013 (Cluster) reported no adverse events and no significant difference in weight, height and BMI at 21 months follow‐up in children aged 16 years and less.
Sensitivity analysis
Including only trials with low risk of bias for allocation of concealment, no significant difference between treatment and control groups was detected in weight or haemoglobin (Analysis 6.1; Analysis 6.2).
6.1. Analysis.
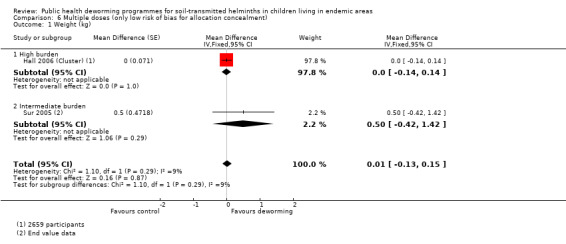
Comparison 6 Multiple doses (only low risk of bias for allocation concealment), Outcome 1 Weight (kg).
6.2. Analysis.
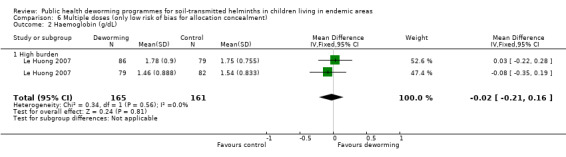
Comparison 6 Multiple doses (only low risk of bias for allocation concealment), Outcome 2 Haemoglobin (g/dL).
Subgroup analysis by worm species (Comparisons 3 and 4).
As Ascaris is said to be associated with weight loss and hookworm with anaemia, we stratified the analysis between trials by helminth species burden (Analysis 3.1; Analysis 3.2; Analysis 4.1; Analysis 4.2); there was no change in the pattern of the results.
3.1. Analysis.
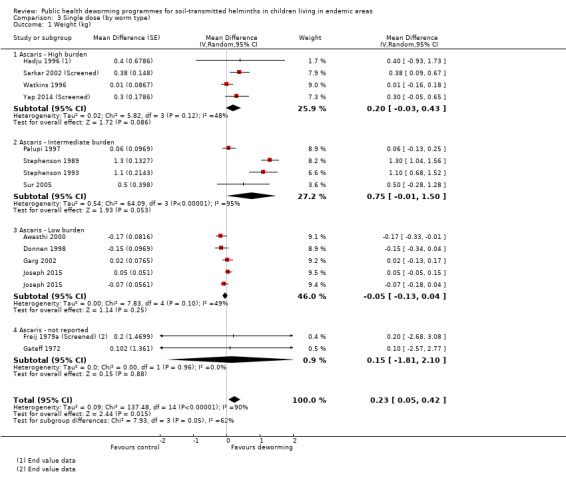
Comparison 3 Single dose (by worm type), Outcome 1 Weight (kg).
3.2. Analysis.
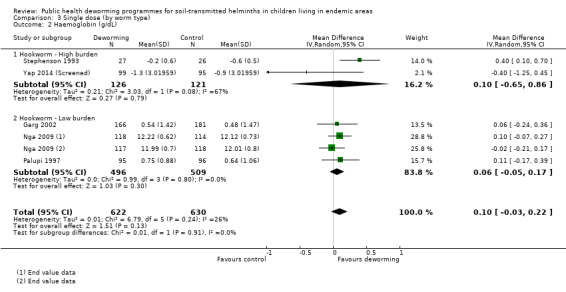
Comparison 3 Single dose (by worm type), Outcome 2 Haemoglobin (g/dL).
4.1. Analysis.
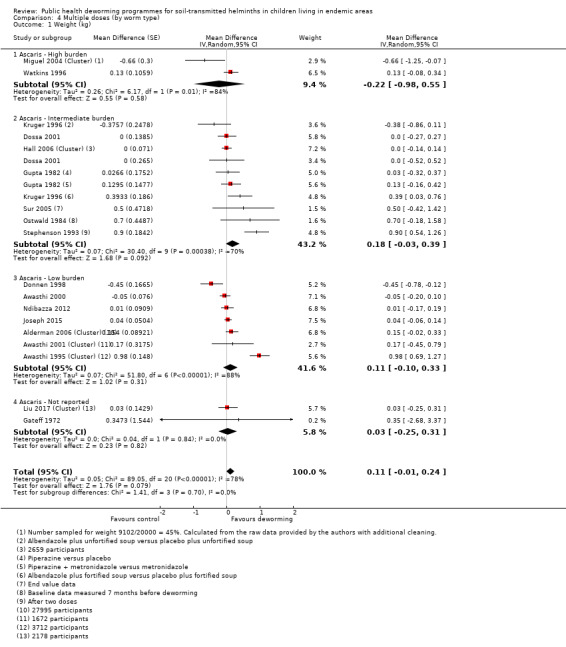
Comparison 4 Multiple doses (by worm type), Outcome 1 Weight (kg).
4.2. Analysis.
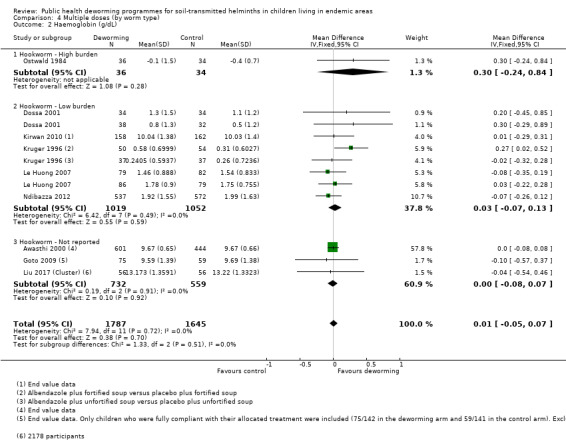
Comparison 4 Multiple doses (by worm type), Outcome 2 Haemoglobin (g/dL).
Effect estimates over time (Comparison 5).
In multiple‐dose studies published in the last 20 years there is no effect demonstrated on mean weight difference (SMD 20 g, 95% CI ‐40 to +80 g; 4328 participants, 10 trials, 2000 to 2018; Analysis 7.2).
Discussion
Summary of main results
We identified 51 trials, including 10 cluster‐randomized controlled trials (RCTs), that met the inclusion criteria. One trial evaluating mortality included over one million children, and the remaining 50 trials included a total of 84,336 participants.
With regard to our logic model in Figure 1, there is substantial evidence that deworming does not improve average height, haemoglobin, cognition, school performance, or mortality. We do not know if there is an effect on school attendance, since the evidence is inconsistent, and at risk of bias. There are insufficient data on physical fitness.
For weight gain, there is evidence of an unusually large impact of deworming drugs in three studies published over 20 years ago. These studies are at high risk of bias. Two of these studies were in the same area of Kenya over 30 years ago, where health services were absent and children very heavily infected. The third study was in India in poor malnourished children over 20 years ago, where subsequent studies in the same area did not show an effect on average weight gain. Contemporary trials provide little or no evidence to support an impact on average weight gain.
Stratifying the analysis according to Ascaris burden for weight and hookworm burden for haemoglobin did not change the pattern of results.
Overall completeness and applicability of evidence
The World Health Organization (WHO), the World Bank, and prominent development economists and parasitologists strongly support community deworming programmes as highly effective. A consensus panel and guideline group was convened by the WHO in 2016 to re‐consider the evidence and make recommendations using WHO approved methods. This exercise was funded by the Bill & Melinda Gates Foundation, which is also a major funder of global deworming programmes The panel considered effects of deworming on infection burden, growth and haemoglobin, morbidity and mortality, and cognitive development and school performance. However, the guidelines use the effects on weight gain to justify the treatment recommendations (WHO 2017a). The advocates argue that average weight gain potentially hides large benefits for a smaller number of children. The 2015 version of this Cochrane Review (Taylor‐Robinson 2015) showed weight gain may be higher in children known to be infected and this was used to justify the policy of treating everyone in a population to potentially benefit the few heavily infected individuals. The WHO guideline recommends annual or bi‐annual treatment preventive chemotherapy in endemic areas, and makes a strong recommendation based on low‐quality evidence (Hawkes 2017; WHO 2017a).The notes explaining the strong recommendation (p21‐22) make it clear that the decision to treat whole populations of children was based on the evidence for impacts of deworming in populations where all the children are known to have worms, rather than whole population level studies.
Our updated analysis shows that there is evidence of an unusually large impact of deworming drugs in three studies published over 20 years ago, with no evidence to support an impact on average weight gain in contemporary populations.
Despite calling for analysis of primary studies using categorical weight change data as an outcome (showing the percentage of children gaining a clinically important amount of weight) in an earlier version of this review, such data have not been made available; and indeed the recent individual patient data (IPD) meta‐analysis has not conducted this analysis either. However, the argument continues, with advocates stating that meta‐analyses of all the data available globally are underpowered (Croke 2016). The argument that some sub‐populations of children may experience important weight gains can neither be demonstrated or refuted by the trials to date, and the researchers have not reported the number of children in intervention and control groups having important weight gains.
The most important remaining uncertainty in our review is around secular trends. The rationale for current WHO policy appears to be driven largely by the unusually large effects on weight gain seen in three old trials, conducted in poor, malnourished populations of children. These effects may mimic the effects seen in children attending clinic with poor nutrition and intense, long‐standing, untreated infection. However, endemicities and worm burden have declined with better water and sanitation, widespread availability through health services of deworming treatments, and possibly deworming programmes; and the later and much larger trials have failed to demonstrate the same effects. It may be that over time the intensity of infection has declined, and that the results from these few trials are simply not applicable to contemporary populations with lighter worm burdens. Since there has been a clear decline in soil‐transmitted helminth (STH) prevalence globally (Vos 2015), this causes a problem with applying evidence generated over 20 years ago to current day levels of infection and infection intensity.
Critics of previous versions of this review (Dickson 2000a), stated that the impact must be considered stratified by the intensity of the infection (Cooper 2000; Savioli 2000), and also that is important to consider worm specific effects. We have done this comprehensively in this version, updating our assessment of worm burden. For example we stratified our analysis to isolate a high burden population that included trials in screened populations where all children had worms, and trials where over 80% of children had worms. We also stratified the analysis according to Ascaris prevalence/intensity for weight and hookworm prevalence/intensity for haemoglobin. No clear pattern of effect is evident.
Expanded age‐range for deworming
In addition to recommending treatment for school‐age children, the new WHO guideline promotes deworming children before they start school, classified into two groups: young children (12 to 23 months of age) and preschool children (24 to 59 months of age). The overlapping nature of these age groups in study populations makes it challenging to undertake subgroup analysis by age group. However, our description of studies by age group demonstrates that the majority of trials have been in school‐age populations (27 studies). Only two trials included exclusively young children aged 12 to 24 months; and four exclusively included preschool children, highlighting the scarcity of evidence in preschool children.
Dispensing deworming to preschool children represents a challenge for health services. The WHO has previously raised concerns about the prevalence of choking in young children (aged between one to three years), with several pages of recommendations in a newsletter about how to administer albendazole in tablet form without children choking. Although common sense might suggest this is a rare occurrence, nevertheless some might argue there is a lack of evidence on the safety of administering deworming drugs to young children in tablet form in a community setting.
Long‐term outcomes
There have been some trials on long‐term follow‐up, none of which met the quality criteria needed in order to be included in this review (Baird 2011; Croke 2014; Ozier 2011; described in Characteristics of excluded studies). A systematic review of these studies conducted by the Cochrane Review team, published in the International Journal of Epidemiology, concluded that these studies were at risk of substantial methodological bias and should not be considered as reliable evidence of effects (Jullien 2016).
Overall, given the evidence of a lack of short‐term effects on haemoglobin and school performance, long‐term population impacts appear unlikely. Previously the WHO had stated that STH programmes improve children’s attendance at school, school performance, and long‐term economic productivity (WHO 2005). The current WHO guidance does not include such claims (WHO 2017a).
Externalities
There have been previous claims that deworming benefits not only the individuals, but also those around them. Whilst not ignoring this, we tried to establish first that there was a benefit to individuals; as this seems debatable, examining for externalities seems less important. Miguel 2004 (Cluster), in their original analysis, stated that externalities had been demonstrated. After correction of coding errors, the independent pure replication of their study failed to find any evidence of externalities (Aiken 2015). Our review included 10 cluster‐RCTs, which may be able to detect externalities accruing as a result of reduced transmission.
Drug resistance
The new WHO guidelines suggest that alternative deworming drugs should be considered in the event that drug resistance against albendazole or mebendazole becomes a significant concern (WHO 2017a). This potentially raises questions about the over‐use of current medications in the absence of clear population benefits.
Polyparasitism
Individuals and communities are often infected with more than one helminth infection (Molyneux 2005), and recent neglected tropical disease (NTD) policy has focused on addressing ‘polyparasitism' by treating the parasites that cause ascariasis, trichuriasis, hookworm, lymphatic filariasis, onchocerciasis, schistosomiasis, and trachoma with ivermectin, albendazole, azithromycin, and praziquantel (Hotez 2009). For example, in 2016 several governments, donors, technical agencies, and pharmaceutical companies jointly signed The London Declaration, committing to a plan for control and elimination of soil‐transmitted helminthiasis, schistosomiasis, and other neglected tropical diseases (Andrews 2017; WHO 2018b).
Thus, mass drug administration for NTDs has been promoted as quote: "one of the lowest cost and cost‐efficient mechanisms for both improving maternal child health and lifting the bottom billion out of poverty" (Hotez 2011b). Significant resources are being invested in this agenda, with the UK Department for International Development committing GBP 50 million in 2008, and the US government committing USD 65 million in 2010 as part of the US Global Health Initiative (Hotez 2011a). More recently the UK has committed £195 million over five years and the US $174 million over two years to support programmes focused on tackling NTDs, including STHs (Patel 2014).
In the absence of clear evidence for treating whole populations for STHs, there is a need to demonstrate which drugs are effective against a particular parasite and to quantify population impacts before combining all the drugs into a basket treatment for all helminth infections, and assuming that all components are effective.
Certainty of the evidence
Conducting field trials to test this intervention is complex and challenging, and researchers have worked hard to generate this body of research evidence. There is now a reasonable amount of evidence from trials in a range of settings, including high‐, moderate‐, and low‐burden areas. There have also been 18 trials that have assessed the effects of multiple doses of deworming (Analysis 2.1), six of which were cluster‐RCTs. These are particularly important because they can detect the ‘real life' community level effects of treatment that include possible effects from a reduction in worm transmission (Bundy 2009).
The certainty of the evidence tends to be moderate to low for most outcomes related to risk of bias, imprecision, inconsistency and indirectness. The certainty is lower for the nutrition outcomes‐mainly because the large effects seen in the three older studies that showed larger effects, and with the other studies showing smaller or no effects. This reduces the certainty of the evidence.
We maintained the meta‐analysis across studies spanning 30 years and downgraded the certainty for heterogeneity and indirectness, as we just do not know whether these older studies reflect current effects with primary health care and lower worm endemicities.
Potential biases in the review process
Statistical errors in analysis
Of the 10 cluster‐RCTs, three did not take adequate account of cluster randomizations (Alderman 2006 (Cluster); Hall 2006 (Cluster); Rousham 1994 (Cluster)). This has the potential substantive impact on the interpretation of the trials. For example, the significant difference between intervention and control quoted on the cover of the BMJ for Alderman 2006 (Cluster) assumed 27,995 children had been individually randomized. When we clarified this with the trial authors, they provided the BMJ with a correction, which showed that no significant difference was detected in weight gain between intervention and control groups; this corrected result has been used in the meta‐analysis in this trial.
School attendance
Advocates of deworming have emphasized the potential impacts on school attendance, on the basis of the influential econometric trial Miguel 2004 (Cluster). The replication trials of Miguel 2004 (Cluster) substantiate our concerns about the high risk of bias in this trial (Aiken 2015; Davey 2015). In particular, the replication trials raise concerns about the validity of combining the school attendance data across years, since this involves a non‐randomized before and after comparison. We have thus presented the corrected separate year estimates in this review, and present the longest follow‐up time point in line with our a priori analysis strategy.
Growth outcomes
The included trials reported a range of nutritional status outcomes. For meta‐analysis, we did not use nutritional data expressed as z‐scores or percentile scores calculated on the basis of reference standards, or dichotomised z‐ or percentile scores (e.g. proportion stunted with height‐for‐age z‐score < ‐2). As these data were derived from the absolute values, we used these values for evidence of benefit. We knew the nutritional data would be captured in the absolute values and wanted to reduce selective reporting through collection of multiple variables from papers that are all derived from the same basic outcomes measured in the trial. We noted that in some trials there was a discrepancy between what was measured and what was reported; e.g. Nokes 1992 (Screened) recorded but did not report anthropometric data. This is a concern as it may indicate selective reporting. However, we have systematically reported all relevant outcomes not included in meta‐analysis in Table 13.
Subgroup analyses
Some trials presented data from subgroups, selected on the basis of factors such as infection status (Beach 1999; Fox 2005; Greenberg 1981), location (Koroma 1996), age (Stoltzfus 2001), frequency of treatment (Stoltzfus 1997 (Cluster)), and sex (Lai 1995). These comparisons were not randomized and have not been included in meta‐analysis. Two trials, one of which one was a cluster‐RCT, demonstrated improvements in nutritional outcomes in subgroup analyses (Stoltzfus 1997 (Cluster); Stoltzfus 2001). We have reported these data in Table 13.
Heterogeneity
For weight outcomes in both single and multiple doses heterogeneity was apparent. We investigated this in a variety of ways: by stratifying by worm burden, by examining the effect of the predominant worm species, by whether values were end or change, and none provided any explanation. The only analysis that helped was the post hoc analysis stratifying trials as "last century" (before 2000) and "this century" (2000 and onwards), with very little effect apparent in the trials conducted over the last 18 years. This is consistent with improved global health, improved access to health services, previous deworming campaigns, and thus lower prevalence and intensity of infection in endemic areas.
Agreements and disagreements with other studies or reviews
Subsequent to the 2015 version of this Cochrane Review, Taylor‐Robinson 2015, the Campbell Collaboration completed a replication. This was published in 2016 (Welch 2016). The study took account some of the criticisms levelled at the Cochrane 2015 version, and included an assessment of the long‐term follow‐up studies. The authors’ findings were virtually identical to those of the 2015 Cochrane Review, and none of the hypothesized effect modifiers (for example, worm‐burden and co‐interventions) altered the main finding. The Campbell review also included the long‐term follow‐up studies and they contributed little data: these studies we appraised and published separately (Jullien 2016). The studies were all at high risk of bias and therefore excluded from this review, as explained in the Description of studies section.
Croke 2016 provided a detail critique of our review in an occasional paper. The comments were in several categories: studies that we had not included or were unpublished when our review was compiled (four studies): these are now included in this edition; data that we did not include in our meta‐analysis, but Croke and colleagues did include by seeking data from the authors, or by imputation and statistical manipulation: this was useful, and our response is detailed in Table 14).
12. Author's point by point responses to Croke 2017.
| Study | Cochrane 2015 | Croke working paper | Conclusion | |
| Not identified or unpublished when the review was compiled | Gateff 1972 | Missed by search | Included in 2018 edition | |
| Ostwald 1984 | Missed by search | Included in 2018 edition | ||
| Joseph 2015 | Unavailable | Included in 2018 edition | ||
| Liu 2017 (Cluster) | Unavailable | Included in 2018 edition | ||
| Not included in meta‐analysis | Willett 1979 | Reported narratively in a summary table (“Growth rates presented are adjusted for a number of variables. Weight gain (kg/year) in levamisole group 2.08 vs 1.92 in placebo group (P = 0. 06)”. | Included in meta‐analysis with SE’s calculated from p‐value | It is unclear from the primary data whether the effect estimate is adjusted. Furthermore, it is not possible to back calculate from the ANOVA p‐value to obtain the standard error for the effect estimate. It is possible to obtain the F ratio statistic from the p value and degrees of freedom (which are known), but there are too many unknown values in the formula for the F ratio to back calculate any further. A method has been described to calculate the t‐test statistic from the ANCOVA F ratio statistic (Knapp & Schafer 2009), This method requires the correlation between the pre and post intervention values within each group to be known. This correlation is unknown for the Willett study. This study cannot be included in the meta‐analysis regardless of whether the effect estimate is adjusted or not. |
| Miguel and Kremer 2004 | Reported narratively as weight for age z score. | We computed the estimated impact on weight using microdata and an ANCOVA specification | Number sampled for weight 9102/20000 = 45%. Calculated from the raw data provided by the authors with additional cleaning. Results included in meta‐analysis are : ‐0.66 kg, SE 0.3 | |
| Ndibazza 2012 | Weight‐for‐age and weight‐for‐height | Data from Campbell | Campbell’s authors supplied data from Campbell review, with authors’ permission, now included in meta‐analysis. | |
| Wiria 2013 (Cluster) | BMI | Data from Campbell “The Campbell Collaboration authors had contacted the original authors and received from them baseline and endline measures of weight and standard deviations of those values for all study participants under age 16, and generously shared these estimates with us. Wiria et al. (2013) does not report variance of changes, so a correlation coefficient is required to impute the standard error of the treatment effect. A correlation coefficient was estimated using a study with author‐provided raw microdata of baseline and endline weight values (Hall et al., 2006).” |
We have examined the data reported in the trial report, and the data provided to the Campbell Collaboration, and observed that there are huge amounts of missing data for both the change scores and end values. We have been unable to clarify the reason for the large quantities of missing data with the trial authors, and so we are therefore excluding this trial from the meta‐analyses. | |
| Stephenson 1993 | Included in children known to be infected. | Included in whole population treatment group | This study was included in our review. In the previous edition it is in the analysis of “all children known to be infected”. In the new edition of the review we have stratified the analysis based upon our updated assessment of worm burden. | |
| Gupta 1982 | Only two units of allocation for relevant comparison | The 4 groups were then allocated 1 of 4 different single treatment regimens; no details given.” (p. 97). Following data extraction principle i, we calculate treatment effects and standard errors from the deworming versus placebo comparisons (n = 78), and the deworming plus giardia treatment versus giardia treatment only comparisons (n = 80) in the published paper. | Now included. | |
| Improved the estimates | Sur 2005 | End value and SE from plot | Baseline and end value estimates and standard errors from the plot in the paper, plus data from p value of change used to calculate change estimate and variance | We accept that it is possible to obtain an estimate of the difference in differences (i.e. the difference in weight gain achieved over a period of 9 months between the control and albendazole group) by digitising Figure 1 in the paper. However, in order to calculate the standard error of this effect estimate, Croke et al. have assumed a t‐test was used to generate the p‐value for this difference in differences. At no point in the paper is it stated that a t‐test was performed to obtain this p‐value, and there are other methods that could be used to obtain this p‐value, such as the ANCOVA method. As previously discussed (see response to Willet 1979), a different method would need to be used to obtain the standard error if the ANCOVA method was used. |
| Hall 2006 (Cluster) | Estimates from paper used | Used ANCOVA estimate adjusting for baseline imbalance in weight at baseline using Hall microdata (unpublished) | It is important that this study is published, and in the public domain. The unpublished manuscript does not provide data on baseline balance. We therefore are using the change values as provided in the manuscript, and decided against the post hoc adjustment re‐analysis of Croke et al. The weight gain in intervention and control group is ZERO in the unpublished manuscript; the post hoc adjusted value used in Croke is 139 g, SE 57 G, p value 0.016. |
|
| Awasthi 2001 (Cluster) | The results (weight gain) in the abstract differ from the text | “Mean (+ SE) weight gain in Kg in control versus ABZ [i.e. treatment] areas was 3.04 (0.03) versus 3.22 (0.03), (p=0.01)” (p. 823). Later in the text, however, a similar treatment effect and level of statistical significance, but a different set of standard errors for the treatment effect, is reported: “The mean weight gain in 1.5 years in the albendazole plus vitamin A group was 5.57% greater than that in the vitamin A group alone (3.22 KG (SD: 2.03, SE: 0.26) vs. 3.05 KG (SD: 1.47 SE: 0.19) P‐value=0.01).” (p. 825). We follow data extraction principle vii in consideration of this issue. In their meta‐analysis, TMSDG use the reported treatment effect (0.17 kg), and appear to calculate the standard error using the second set of values (SE 0.26 and SE 0.19). Based on the p‐values calculated from these numbers, and in contradiction to the p‐value of 0.01 reported in the study, TMSDG refer to these results as not statistically significant, with a standard error of 0.341. By contrast the standard error is 0.0650 if one uses the p‐value of 0.01 and treatment effect of 0.17 to back out a standard error, following, as in section 3, the formulas and procedures in Higgins and Green (2011), section 7.7.3.3. 35” |
We know that this trial was analysed by cluster (Richard Peto, pers. Com). The paper abstract and main results provides differing estimates of variance for weight gain. The abstract gives a standard error of 0.03 for weight gain in both groups, and the results gives a standard error of 0.26 in the intervention and 0.19 in the control. The data in the main results are analysed at the level of the cluster: using the relationship between SE and SD, we calculate n for the intervention as 61, and for the control 60. This corresponds (allowing for rounding errors) with the units randomised in the paper. We therefore used, for weight change, intervention 3.22 (SE 0.26) and control 3.05 (SE 0.19). |
A review of observational studies and RCTs to assess the hypothesis that STH infection is associated with cognitive deficit and educational loss concludes that there were improvements in cognitive domains in STH uninfected/dewormed populations compared to STH infected/not‐dewormed school‐aged children (Pabalan 2018). One explanation for this is that the observational studies are confounded, since no such impacts were identified in the Cochrane and Campbell reviews of experimental studies.
A review and meta‐analysis by Hall 2008, funded by the World Bank, presented evidence in favour of an effect of deworming on weight gain (MD 0.21 kg, 95% CI 0.17 to 0.26, 11 trials). This analysis differs from our analyses of weight gain in a number of respects: it was not a protocol‐driven systematic review; the review excluded trials in lower prevalence areas (< 50%); pooled results were presented without exploration of significant heterogeneity; it combined trials that included both screened and unscreened children; it included trials excluded from our review on the basis of methodological quality; it included data from subgroup analyses; and included data unadjusted for cluster randomization.
The narrative review, Albonico 2008, explored the evidence for the impact of deworming on preschool‐age children, and concluded that deworming has been shown to improve growth. Their analysis differed from our analyses in a number of ways: a different population was considered, although our review considers data from this subgroup; it was not a protocol‐driven systematic review; it included trials excluded from our review; it was a narrative summary rather than meta‐analysis of data; it reported results from subgroup analyses; it reported point estimates without taking into account statistical significance; and it included data unadjusted for cluster randomizations. The authors state: "A few trials have failed to show any impact of deworming on growth". This is at odds with our interpretation of the reliable randomized comparisons of nutritional outcomes in this review, which suggests that most trials have failed to show an effect on nutrition.
Gulani 2007 undertook a systematic review of the effects of deworming on haemoglobin, and reported a marginal increase in mean values that could translate into small reduction (5% to 10%) in anaemia in a population with a high prevalence of intestinal helminths. This systematic review differs from our analysis of haemoglobin in a number of respects: it included trials in adults and pregnant women, and it included trials excluded from our review on the basis of methodological quality.
Authors' conclusions
Implications for practice.
It is good medical practice that children known to be infected with worms should receive treatment. This is obvious and not the subject of this Cochrane Review.
There is now good evidence to show that public health programmes to regularly treat all children with deworming drugs have little or no demonstrable benefit on average height, haemoglobin, cognition, school performance, or mortality. We do not know if there is an effect on school attendance, since the evidence is inconsistent and at risk of bias, and there are insufficient data on physical fitness.
Unusually large effects on weight were seen in three studies that were published over 20 years ago, with numerous more recent large trials showing no impact. This causes uncertainty leading us to conclude that we do not know if repeated doses of deworming drugs impact on average weight.
Whether individual children with heavy worm infections benefit from mass deworming programmes has not been shown empirically. Trials and the recent individual patient data (IPD) meta‐analysis have not analysed the number or proportion of children that make important weight gains in intervention and control groups, which would be needed to evaluate this hypothesis.
We suggest that the current evidence does not support large public health programmes of deworming in low and middle‐income countries.
Implications for research.
Further trials may be justified to evaluate whether subgroups of children in populations stand to benefit from deworming, since it is theoretically possible that deworming could benefit a small number of children that are heavily infected whose weight gain is diluted to become undetectable in population level studies.
The certainty of evidence is graded as moderate on most of the outcomes, in relation to demonstrating little or no effect of community deworming. This means that research could possibly have important impact on the confidence of the results and alter the effect. Therefore, further research may be useful, but this needs to be balanced against the declining worm burdens worldwide and the absence of any good evidence of an effect given the current research.
Authors of trials, whether they are small or large, should publish the results of the trials promptly irrespective of the findings, in line with the basic principles of research integrity (Garner 2013). We encourage the authors of the Vietnam trial to publish their results as it is still not in the public domain.
Feedback
Ted Miguel and Michael Kremer, 11 January 2013
Summary
Dear Dr. Taylor‐Robinson, Dr. Maayan, Dr. Soares‐Weiser, Dr. Donegan, and Dr. Garner:
We are writing to clarify several points that you raise in your recent 2012 Cochrane review of deworming regarding our 2004 paper "Worms: Identifying impacts on education and health in the presence of treatment externalities" in Econometrica.
In particular, we have four main concerns about the discussion of our piece in the recent review, and believe that they could change the assessment of the quality of the evidence presented in our paper. We list these points here in the letter below, with a brief discussion of each point. We then discuss several additional points in the attached document below, following this letter. We hope that these detailed responses to your review will start a productive discussion about the interpretation of the evidence in the Miguel and Kremer (2004) paper.
(All page numbers listed below refer to the July 2012 version of your review, with "assessed as up‐to‐date" as May 31, 2012.)
We recognize that writing a Cochrane review is a major undertaking, and we appreciate the time you have taken to read our paper, and the dozens of other papers covered in the review. We hope that this note can serve as the starting point for discussion, both in writing and via phone, if appropriate.
Our four points all relate to the claim made on page 6 of your review, and repeated throughout the review, about the Miguel and Kremer (2004) paper:
"Miguel 2004 (Cluster) has a high risk of bias for sequence generation, allocation concealment, blinding, incomplete outcome data and baseline imbalance."
We have serious concerns about the claims you make about the risk of bias for baseline imbalance, incomplete outcome data, and sequence generation. We discuss these in turn below.
Point (1): A leading issue is your current assessment of the quality of evidence on school attendance and participation, which is the main outcome measure in the Miguel and Kremer (2004) trial. Several concerns are raised, including: a lack of baseline values for these measures (leading to a risk of baseline imbalance), and statistically significant impacts for only one of the comparisons considered. The quotes from your review are as follows:
[p. 21] "For school attendance (days present at school): (Miguel 2004 (Cluster) Table 6; Analysis 5.4) reported on end values for attendance rates of children (1999, Group 1 versus Group 3), and found no significant effect (mean difference 5%, 95% CI ‐0.5 to 10.5). No baseline values were given so there is potential for any random differences between the groups to confound the end values."
[p. 24] "Similarly, for school attendance, the GRADE quality of the evidence was very low. One quasi‐randomized trial (Miguel 2004 (Cluster) reported an effect, which was apparent in only one of the two comparisons in up to a year of follow‐up, and not apparent in the one comparison after one year. Miguel 2004 (Cluster) measured attendance outcomes directly, unlike the other two trials (Simeon 1995; Watkins 1996) which measured attendance using school registers, which may be inaccurate in some settings. However, in Miguel 2004 (Cluster), the values for school attendance were end values and not corrected for baseline. Thus random differences in baseline attendance between the two groups could have confounded any result."
We feel that these concerns are misplaced, and explain why here. We first discuss concerns about "baseline imbalance".
First, we in fact do have baseline data on school participation (our preferred measure) for one of the comparisons that you focus on. The authors of the Cochrane appear to have missed this data in our paper. In Table VIII, Panel A, there is a comparison of 1998 school participation for both Group 2 and Group 3, when both were control schools. There is no statistically significant difference in school participation across Group 2 and Group 3 in 1998, and if anything school participation is slightly lower in Group 2 (‐0.037, s.e. 0.036). This makes the difference between Group 2 and Group 3 in 1999 (0.055, s.e. 0.028), when Group 2 had become a treatment school, even more impressive, since at baseline Group 2 had slightly lower school participation. We respectfully request that the authors of the Cochrane review include this data as evidence of baseline balance in our key outcome measure, school participation, and that they edit their claim that we do not have any such evidence.
It is interesting to note that, if we take the difference between Group 2 and Group 3 at baseline seriously, then the overall effect for this "year 1" comparison is 3.7 + 5.5 = 9.2 percentage points. This is almost exactly the same as the 9.3 percentage point effect in the other "year 1" comparison that the Cochrane authors focus on (Group 1 versus Groups 2 and 3 in 1998). Taken together, this is quite striking evidence that the first year of deworming treatment significantly improves school participation. The Cochrane authors' repeated concerns in their review about baseline balance being critical in randomized experiments suggests (to us) that they might find it methodologically preferable to use a "difference‐in‐difference" design that explicitly controls for any baseline differences across treatment groups, rather than the standard unbiased "endline" comparison across treatment groups. If this is in fact the case, then the relevant year 1 deworming treatment effect for the Group 2 versus Group 3 comparison (for which we have baseline data, as noted above) is the 9.2 percentage point estimate, which we note is significant at 99% confidence.
Second, regarding baseline data on school attendance, we discuss that there is indeed evidence from school registers that recorded attendance is indistinguishable in the three groups of schools in early 1998 (in Table I). While the register data has its weaknesses – precisely the reason we developed the much more rigorous approach of unannounced school participation checks, combined with tracking of school transfers and drop‐outs – it is used in other trials, and in fact the Cochrane review considers school register data sufficiently reliable to include a trial (Watkins 1996) that uses it in their meta‐analysis of school attendance.
We are puzzled as to why the evidence in the Watkins (1996) trial is included at all in the Cochrane review if similar register data is considered unreliable when Miguel and Kremer (2004) use it. If school register data is considered (largely) unreliable, then the Watkins (1996) article should be excluded from the review, in which case the "meta‐analysis" of school attendance and participation impacts will yield estimated effects that are much larger and statistically significant (since the Watkins impact estimates are close to zero). If the register data is considered (largely) reliable, then the Watkins (1996) trial should be included in the review, but the baseline register data in Miguel and Kremer (2004) should be considered as evidence that we do in fact have baseline balance on school participation. But there is an inconsistency in how register data is considered across the two trials. This seemingly inconsistent approach taken by the authors raises questions about the evenhandedness of the Cochrane review.
In fact, the appropriate use of school register data is more subtle than the Cochrane authors currently consider, since its use as baseline data may in fact be appropriate even if it is inappropriate for use as outcome data. There are at least two reasons why. First, one of the major weaknesses of the school register data used in Watkins (1996) is that it excludes any students who have dropped out, potentially giving a misleading picture about school participation over time. However, this concern about drop‐outs is irrelevant when we use school register data at baseline, since the universe of students considered in the Miguel and Kremer (2004) article was restricted to those currently enrolled in school in January 1998 (at the start of the school year), and thus the exclusion of drop‐outs is not a concern. Note that our use of the school register data at the start of the school year is a likely explanation for why the baseline average attendance rates we obtain using this data are much higher than the average school participation rate that we estimate over the course of the entire school year.
A second related issue is the quality of measured school attendance data conditional on student enrollment in school. Note that to the extent that differences in attendance record‐keeping prior to the introduction of the program are random across schools, they will not bias estimates of treatment impact and any "noise" in these measures will be correctly captured by reported standard errors. However, there are plausible concerns about the quality of school register data collected in treatment versus control schools in the context of an experimental evaluation, with a leading concern being that school officials could erroneously inflate figures in the treatment group. Yet once again these concerns are irrelevant in the Miguel and Kremer (2004) trial context since the baseline 1998 school register data that we present (in Table I, Panel B) was collected before any interventions had even been carried out in the sample schools, once again making the baseline school register data potentially more reliable than school register data used as an outcome.
While the data and measurement issues here are somewhat subtle, if anything they argue in favor of including the baseline school register data in assessing the baseline balance in the Miguel and Kremer (2004) paper, while excluding the school register outcome data in Watkins (1996) as potentially unreliable. Instead, the Cochrane authors completely dismiss the baseline register data in Miguel and Kremer (2004) as unreliable evidence for baseline balance, while including the Watkins (1996) data in their meta‐analysis of school participation impacts, giving it equal weight with the Miguel and Kremer (2004) school participation impact evidence (which uses more rigorous outcome data). Once again, the seemingly selective approach taken by the authors raises questions about the evenhandedness of the Cochrane review.
An important final point has to do with the claim that there might have been "random differences" across groups. Given the randomized design of Miguel and Kremer (2004), there is no systematic difference to expect there to have been such random differences. The endline comparison of outcomes across treatment groups yields unbiased treatment effect estimates. The remarkable balance across the three groups in terms of dozens academic, nutritional, and socioeconomic outcomes at baseline (Table I) makes it even more unlikely that there were large differences in school participation solely by chance. If the Cochrane authors would like to consider other characteristics (other than school participation) to gauge the likelihood that Groups 1, 2 and 3 in our trial are in fact balanced at baseline they should look at the whole range of outcomes presented in Table I of Miguel and Kremer (2004). The lack of significant baseline academic test scores across Groups 1, 2 and 3 in our sample (Table 1, Panel C) is particularly good evidence that schooling outcomes were in fact balanced at baseline, for instance. It is not clear to us why the Cochrane authors remain so concerned about baseline imbalance issues given the experimental design (which leads to unbiased estimates) and the remarkable balance we observe along so many characteristics in Table I of Miguel and Kremer (2004), and their review does not provide compelling justification for their concerns.
Moreover, in the standard statistical methods that we use, only those differences across groups that are too large to have been generated "by chance" are considered statistically significant impacts. In other words, the standard errors generated in the analysis itself are precisely those that address the risk of imbalance "by chance" given our research design and sample size. Of course, random variation that is orthogonal to treatment assignment does not alone generate bias.
Speculating about the possibility that there were simply positive impacts "by chance" in order to cast doubt on one set of results, but not doing the same when there are zero estimated impacts, again raises questions about the evenhandedness of the Cochrane review. (For instance, perhaps the “zero” impacts on Hb outcome measures in our sample were zero simply "by chance", when the real point estimates are in fact strongly positive, like the large school participation impacts we estimate. Yet this possibility is not mentioned in the Cochrane review.) In our view, the Cochrane authors do not provide sufficient justification for their fears about imbalance "by chance" in our sample, and we feel further concrete details about these concerns are needed to substantiate their assertions.
Taken together, the Cochrane review's claim that there is a "high risk of bias for … baseline imbalance" (the claim made on p. 6 and p. 136, and throughout the review) appears highly misleading to us, given the: balance in school participation we observe between Group 2 and Group 3 in 1998; the balanced school attendance based on register data across Groups 1, 2 and 3 at baseline; the balance in other measures of academic performance (including academic test scores) as well as multiple socioeconomic and nutritional characteristics at baseline; and most importantly given the randomized experimental design, which implies that there is no systematic reason why the three treatment groups would differ significantly along unobservable dimensions.
We respectfully request that the authors of the review consider these factors and reconsider their assessment regarding the claimed "high risk of bias for … baseline imbalance" in Miguel and Kremer (2004).
Point (2): There is also an important methodological point to make regarding how the authors of the Cochrane review assess the school participation evidence. At several points they note that only some of the school participation comparisons are statistically significant at 95% confidence. To be specific, the comparisons they focus on have the following estimated impacts and standard errors (from p. 130‐131 of their review):
School participation outcomes measured £ 1 year:
9.3 percentage point gain (s.e. 3.1 percentage points)
5.5 percentage point gain (s.e. 2.8 percentage points) School participation outcomes measured > 1 year:
5.0 percentage point gain (s.e. 2.8 percentage points)
It is unclear to us why the reviewers separate out the three comparisons, rather than combining the groups in a single analysis using standard analytical methods, as their principal assessment of the impact of deworming on school participation. They give no clear methodological justification for this separation. Pooling data from three valid and unbiased "comparisons" still yields an unbiased treatment effect estimate, but with much greater statistical precision, and is thus a methodologically preferable approach. At a minimum, the Cochrane authors should discuss the pooled estimates (which are the focus of Miguel and Kremer 2004) in addition to the three separate comparisons.
One simple approach to doing so that maintains the "comparisons" above, and at least goes part of the way towards using the full sample, would be to pool 1998 and 1999 data for the Group 1 versus Group 3 comparison, since Group 1 is treatment during this entire period and Group 3 is control for the entire period. The distinction between < 1 year and > 1 year outcomes seems rather artificial to us, as discussed further below. It is unclear to us why the Cochrane authors never present this comparison of Group 1 versus Group 3 for 1998 and 1999 pooled together.
The preferred analysis in the Miguel and Kremer (2004) paper pools multiple years of data, and all groups, to arrive at the most statistically precise estimated impact of deworming on schooling outcomes. This includes both school participation outcomes, as well as academic test score outcomes (which the Cochrane authors currently exclude since in the paper we only present these “pooled” test score results, rather than the simple differences across treatment groups). If the Cochrane authors would like to see the simple differences across treatment groups for the academic test scores, we would be delighted to share the data with them. (To be clear, the test score impact estimates in Miguel and Kremer (2004) come from a regression analysis that relies on the experimental comparison between the treatment and control groups, and is not a retrospective analysis based on non‐experimental data.)
In our view, the Cochrane authors do not provide adequate statistical justification for splitting results into the different "comparisons", or into "year 1" versus "year 2" impacts. "Pooling" these different comparisons, as we do in the Miguel and Kremer (2004) paper, is standard with longitudinal (panel) data analysis with multi‐year panels, and is appropriate for those that care about deworming impacts at multiple time frames, ie at less than one year and at more than one year of treatment. Use of our full sample would immediately lead to the conclusion that there are in fact positive impacts of deworming on school participation in our sample, with very large impact magnitudes and high levels of statistical significance. This is the conclusion of the Miguel and Kremer (2004) paper, and a quick look at the comparisons presented above also indicate that there are strong impacts: all three of the comparisons have large impact estimates and all three are statistically significant at over 90% confidence, with one significant at over 99% confidence and another nearly significant at 95% confidence (despite the data being split up into the three different comparisons). By treating each comparison independently and in isolation, the authors are reaching inappropriate conclusions, in our view.
To illustrate why the approach taken by the current version of the Cochrane review is inappropriate, imagine the simple thought experiment of splitting up the data from Miguel and Kremer (2004) into "quarters" (three month intervals) rather than years of treatment. There is no obvious a priori reason why this should not be as valid an alternative approach as the >1 year and <1 year approach in the Cochrane review, as some other reviewers might instead have been interested in the impact of deworming treatment over intervals shorter than one year. Then we would have 2 comparisons in quarter 1 of treatment (Group 1 versus Groups 2 and 3 in early 1998, and Group 2 versus Group 3 in early 1999), 2 comparisons in quarter 2 of treatment, 2 comparisons in quarter 3, 2 comparisons in quarter 4, and 1 comparison in each quarter from 5 through 8 (Group 1 versus Group 3 in 1999). This approach would generate 12 valid "comparisons" of treatment and control schools over multiple time periods, but by slicing up the data ever more finely and reducing the sample size considered in each comparison, it is almost certain that none of these comparisons would yield statistically significant impacts of deworming on school participation at 95% confidence, even though the average estimated effect sizes would remain just as large. This would clearly not be an attractive methodological approach. You could even imagine considering a month by month treatment effect estimate, which would yield 36 different “comparisons”, all of which would be severely underpowered statistically.
However, we view the Cochrane review's slicing of our full dataset into three comparisons (two for year 1 treatment, and one for year 2), rather than conducting the analysis in the full dataset in much the same way. As we show in Miguel and Kremer (2004), when the data from all valid comparisons is considered jointly, in order to maximize statistical precision using standard longitudinal (panel) data regression methods, the estimated impacts are large and highly statistically significant. Just to be clear, we do not use any controversial statistical methods, and our results do not rely on any non‐experimental comparisons. The regression analyses in our paper rely entirely on the variation in treatment status induced by the experimental design of the trial, and thus are just as appropriate analytically as the simple "treatment minus control" differences that the Cochrane authors focus on. In our view, the most robust analytical approach should use our full dataset, rather than the (in our view) more fragmented way of presenting the results in Table 6 of your review, which leads to less statistical precision and no greater insight.
If the Cochrane authors feel that there is a strong a prior reason to focus on year 1 treatment results separately from year 2 treatment results, then at a minimum they should consider both of the year 1 "comparisons" that they focus on jointly (ie Group 1 versus Groups 2 and 3 in 1998, and Group 2 versus Group 3 in 1999), in order to improve statistical precision and thus generate impact estimates with tighter confidence intervals. If they wish to strictly employ the same exact "comparison" groups over time, then they should at a minimum pool the 1998 and 1999 data and focus on the Group 1 versus Group 3 comparison. Doing either would yield an unambiguous positive and statistically significant impact of deworming on school participation in our sample.
We respectfully request that the authors of the review consider these suggestions and reconsider their assessment regarding the claimed lack of statistically significant school participation impacts in Miguel and Kremer (2004).
Point (3): The Cochrane review concludes that our trial has a "high risk of bias for … incomplete outcome data" (p. 90). We believe this point is simply incorrect when applied to our school participation data, as we explain here. The review authors focus on the lack of detail in Miguel and Kremer (2004) regarding the collection of Hb data, but then unfairly use this lack of clarity to downgrade the reliability of all data in the trial, including the school participation data. The exact quote from the review is as follows:
[p. 15] However, results for health outcomes were presented for the 1998 comparison of Group 1 (25 schools) versus Group 2 (25 schools). Details of the outcomes we extracted and present are:
• Haemoglobin. This was measured in 4% of the randomized population (778/20,000). It was unclear how the sample were selected.
The Hb sample was a random (representative) sub‐sample of the full sample, chosen by a computer random number generator. Appendix Table AI of the Miguel and Kremer (2004) paper does discuss how the parasitological and Hb surveys were collected jointly in early 1999. Table V mentions that the parasitological data in 1999 was collected for a random sub‐sample. A random subset of those individuals sampled for parasitological tests also had Hb data collected; this was not explicitly stated but should have been. The reason for the relatively small sample for Hb testing was simply that a random (representative) sub‐sample was selected for this testing. For both Hb and parasitological tests, the time and expense of testing the entire sample of over 30,000 school children was prohibitive, hence the decision to draw a representative sub‐sample. Collection of this data for a representative sample should reduce concerns about bias due to incomplete outcome data and selective attrition.
[p. 15] • Weight and height. This was measured in an unknown sample of the 20,000 children. No sampling method was given.
Section 3.1 of Miguel and Kremer (2004) does state explicitly that the anthropometric data was collected during pupil questionnaires at school during 1998 and 1999. These were collected in standards (grades) 3‐8, rather than in all grades, and for that reason there is only data on a subset of the full sample. Height and weight data was collected on all individuals in standards 3‐8.
We acknowledge that the discussion of sampling for hemoglobin outcomes was unclear in Miguel and Kremer (2004). However, the fact that we only have Hb data for a random subset in no way affects the attrition rate for school participation data, which was collected for the entire sample. There is no problem with attrition in the main outcome measure in the Miguel and Kremer (2004) trial, namely, school participation. In fact the school participation data is unusually rigorous. We tracked individuals as they transferred across schools, or dropped out of schools, and collected school attendance on unannounced visit days to get a more representative picture of actual school participation. This is in sharp contrast to most other trials.
For instance, Watkins (1996), which shows smaller school attendance impacts than Miguel and Kremer (2004), only considers school attendance based on register data, among those attending school regularly, missing out on school drop‐outs and transfers entirely. Yet that trial surprisingly received equal weight with Miguel and Kremer (2004) in the meta‐analysis of school attendance carried out in this Cochrane review.
Taken together, the claim that there is a "high risk of bias for … incomplete outcome data" (the claim made on p. 6 and p. 136, and throughout the review) appears incorrect to us, given the remarkably high quality of follow‐up data for school participation, which serves as the main outcome of the trial, and the collection of a representative sub sample for both Hb and nutritional measures.
We respectfully request that the authors of the review consider these factors and reconsider their assessment regarding the claimed “high risk of bias for … incomplete outcome data” in Miguel and Kremer (2004), especially in regards to the school participation data.
(One small point: In the summary of findings table on page 5, it is stated that we only have school participation data for 50 clusters, rather than 75 clusters. This is incorrect, since even using the Cochrane authors' three "comparisons", there are 75 distinct clusters that contribute to the year 1 evidence for Group 1 versus Groups 2 and 3 in 1998, for instance.)
Point (4): The Cochrane review also considers the Miguel and Kremer (2004) trial to have “a high risk of bias for sequence generation” [p. 6].
In particular, it discusses the quasi‐random allocation of the 75 clusters:
[p. 14] "Eight trials were cluster randomized (Alderman 2006 (Cluster); Awasthi 2008 (Cluster); Awasthi 2001 (Cluster); DEVTA (unpublished); Hall 2006 (Cluster); Rousham 1994 (Cluster); Stoltzfus 1997 (Cluster)), one was a trial with quasi‐random allocation of the 75 clusters (Miguel 2004 (Cluster))".
It is never clearly specified why the randomization approach makes the trial "quasi‐randomized". It may be due to the use of an alphabetical "list randomization" approach, rather than a computer random number generator, but if so, this is never laid out explicitly by the Cochrane authors. The remarkable baseline balance on a wide range of characteristics (educational, nutritional, socioeconomic, etc. shown in Table I of Miguel and Kremer 2004) across 75 clusters and over 30,000 individuals surely helps alleviate these concerns. We would like to obtain more detailed information from the Cochrane authors on why the research design in Miguel and Kremer (2004) is considered to have a "high risk of bias". This is never explicitly discussed in the review.
We respectfully request that the authors of the review consider these factors and reconsider their assessment regarding the claimed "high risk of bias for … sequence generation" in Miguel and Kremer (2004).
We carefully read through the entire document and noted additional instances where we had questions and concerns below (following this letter), and note the relevant page numbers in your review.
Finally, we also would like to briefly mention two working papers that we believe could usefully be incorporated into future versions of the Cochrane review on deworming. One working paper (Baird et al.) trials long‐term impacts of deworming treatment on labor market outcomes. We are both co‐authors on this paper. We are currently finishing the write up of this paper and hope to submit it to a working paper series and a journal in 2013, and at that point we will share that paper with your group. That trial shows very large long‐run impacts of deworming treatment on labor market outcomes, up to ten years after the start of the primary school deworming project that we trial. The second is a working paper by Dr. Owen Ozier of the World Bank, which examines long‐run educational impacts on individuals who were very young children at the start of the Kenya deworming project, and finds large positive test score effects. One advantage of Ozier’s trial is his ability to compare outcomes across schools and across birth cohorts within those school communities, allowing him to include "school fixed effects" that control for any baseline differences across schools. This methodological approach addresses any lingering concerns about baseline "imbalance" across treatment groups.
We look forward to starting a discussion of these issues with your team, and we thank you for the time you have taken to consider them. We realize that this is an extremely time‐consuming process for your entire team, given the detailed reading you need to carry out for literally dozens of trials, and we appreciate your willingness to consider these points.
Additional comments on the Cochrane review: (Cochrane text noted in italics, page numbers noted)
The Cochrane authors have the following discussion of the exam score data and school sample:
[p. 67] "Participants Number analysed for primary outcome: … Unclear for exam performance and cognitive tests Inclusion criteria: none explicitly stated. “Nearly all rural primary schools” in Busia district, Kenya, involved in a NGO deworming programme were studied, with a total enrolment of 30,000 pupils aged six to eighteen. Exclusion criteria: girls > 13 years old".
The claim that there was no explicit inclusion criteria stated in the paper for the exam data appears inaccurate. Section 7.2 of Miguel and Kremer (2004) discusses our attempts to test all students, including efforts to administer exams even to those students who had since dropped out of school (see footnote 52).
In terms of the inclusion of schools in the sample, there were a total of 92 primary schools in the trial area of Budalangi and Funyula divisions in January 1998. Seventy‐five of these 92 schools were selected to participate in the deworming program, and they form the analysis sample here. The 17 schools excluded schools from the program (and thus the analysis) include: town schools that were quite different from other local schools in terms of student socioeconomic background; single‐sex schools; a few schools located on islands in Lake Victoria (posing severe transportation difficulties); and those few schools that had in the past already received deworming and other health treatments under an earlier small‐scale ICS (NGO) program.
The Cochrane authors make the following point about worm infection rates, which relates to potential baseline imbalance across treatment groups:
[p. 68] "Group 1 schools have an overall prevalence of 38% heavy/moderate worm infection in 1998, compared to the initial survey in control schools in 1999, where it was 52%."
This is a misleading comparison. The comparison of Group 1 worm infection in 1998 versus Group 2 worm infection in 1999 is simply inappropriate, given the well‐known variability across seasons and years in worm infection rates (as a function of local weather, precipitation, temperature, etc.). There is abundant health and nutritional data from pupil surveys for Groups 2 and 3 at baseline in 1998, and they indicate that these groups appear very similar to Group 1 at baseline (see Table I of Miguel and Kremer 2004) but no parasitological data was collected for Groups 2 and 3 in 1998, nor for Group 3 in 1999, since it was considered unethical to collected detailed worm infection data in a group that was not scheduled to receive deworming treatment in that year. Once again, standard errors for the comparison of outcomes among different treatment groups take into account the possibility of random differences at baseline, and thus statistical significance levels already reflect the possibility that there is some random baseline variation across schools, but this variation alone of course does not cause bias.
The Cochrane authors have the following discussion of our health data:
[p. 68] "However, in a personal correspondence the authors state that there is no health data for Group 3 schools for 1999."
This claim is not entirely accurate, and must be the result of a misunderstanding. There is abundant health and nutritional data from pupil surveys for Group 3 in 1999, but no parasitological data was collected for Group 3 in 1999, since it was considered unethical to collected detailed worm infection data in a group that was not scheduled to receive deworming treatment in that year.
[p. 68] 27/75 schools were involved in other NGO projects which consisted of financial assistance for textbook purchase and classroom construction, and teacher performance incentives. The distribution of these other interventions is not clear, but the authors state that these schools were stratified according to involvement in these other programmes.
[p. 70] The intervention was a package including deworming drugs for soil transmitted helminths, praziquantel to treat schistosomiasis in schools with > 30% prevalence, and health promotion interventions. In addition 27/75 schools were involved in other NGO projects which consisted of financial assistance for textbook purchase and classroom construction, and teacher performance incentives. The distribution of the latter interventions is not clear. These co‐interventions confound the potential effects of deworming drugs to treat STHs. However, the authors kindly provided a re‐analysis of their data, with the praziquantel treated schools removed from the analysis. This represents as subgroup analysis of the original quasi‐randomized comparison".
Given that these other interventions had no measurable impacts on educational outcomes (as reported in several other articles), and that they are balanced across our treatment groups, these prior interventions are not a major concern for the analysis.
Sincerely,
Ted Miguel and Michael Kremer
I agree with the conflict of interest statement below:
I certify that we have no affiliations with or involvement in any organization or entity with a financial interest in the subject matter of our feedback.
Reply
We appreciate these helpful and detailed comments. We have checked through these carefully, and responded to the key points below.
Risk of bias assessment contested (point 1).
Miguel and Kremer were concerned that we had been unduly harsh on assessing the risk of bias of their trial in several points in their comments. We have reassessed this in the light of their comments and the recent replication, which is helpful as it clarifies more details on the methods.
Baseline imbalance: We agree and now move the risk of bias in relation to imbalance at baseline to "low". The remaining criteria of the risk of bias remain unaltered.
Incomplete data: Thank you for your additional information about the methods. This is also contained in the replication analysis, and this has been adjusted to low.
Quality of the evidence in relation to schooling and advocacy of combining results (point 2).
Miguel and Kremer were concerned that the quality of the evidence on school attendance was ranked as "very low". We thank them for their concern and have revaluated the reasons for downgrading, taking into account the pure and the statistical replication. It remains ranked as very low with full justification given in the ‘Summary of findings' table footnotes.
Miguel and Kremer also advocate combining results for school participations from the three school participation results from quasi‐randomized comparisons. Just to recap, for year 1 follow‐up, there are results from:
Group 1 vs Groups 2+3;
Group 2 vs Group 3.
And at two years of follow‐up, results from Group 1 vs Group 3.
We have not combined the estimates from the quasi‐randomized comparisons in meta‐analysis because they are not independent. However the separate estimates are all documented in the review.
Due to the trial design the pooled estimate that Miguel and Kremer prefer contains a non‐randomized before and after comparison, as clarified in the replication trials.
The second point the authors raise in the paragraph "However, we view the Cochrane's slicing…". We have addressed this by combining the multiple‐dose trials in one analysis, using the longest follow‐up time point. Justification for this is provided in the review text. This is a helpful comment and has helped with shortening the review.
Losses to follow‐up on haemoglobin and school attendance (point 3).
Thanks for these clarifications about the sampling for height, weight, and Hb. These are noted in the review.
For school attendance, there is downgrading as stated in the table so that the GRADE assessment of the quality is very low, for risk of bias, imprecision, and indirectness. The missing data and many of the methodological issues debated here are now made much clearer in the replication trials. The other information that is highly relevant is the health promotion co‐intervention.
The GRADE table is agreed by all authors after considerable discussion. It is also checked by two other editors. This is based on information in the original trial reports and now, with your trial, the two papers concerning the replication.
Risk of bias on sequence generation; and additional papers (point 4).
Thank you for this information.
This is a quasi‐randomized method of allocation, as described in the Cochrane Handbook for Systematic Reviews of Interventions, and as clarified in the replication trials.
Thanks for these additional papers you mention. They were considered by the authorship team and do not meet the inclusion criteria for the review.
Contributors
David Taylor‐Robinson, Paul Garner, Karla Soares‐Weiser, Sarah Donegan.
Harold Alderman, 14 January 2013
Summary
Shortly after my paper on deworming in Uganda was published in the BMJ, I had an exchange of correspondence with Dr. Garner regarding the standard errors reported in one table. After that exchange I shared the following letter with the BMJ and with him in April 2007:
Dear Editor,
Prof. Paul Garner has kindly pointed out that, in an article published in the BMJ, my coauthors and I inadvertently failed to adjust standard errors in one of the tables for cluster based sampling. While table 2 of that paper reports means for growth in grams of 2413 [CI=2373 ‐ 2454] and 2259 [CI=2216 ‐ 2301] for the treatment and control groups respectively, once the design effect is taken into consideration the confidence intervals should, in fact, be [CI=2295 ‐ 2533] and [CI=2121 ‐ 2396].
The conclusions of the trial, however, are unaffected as they are based on the multivariate regressions reported in table 3 for which the standard errors had been corrected for cluster based sampling. For example, the confidence interval for the finding that the children who attended child health days every six months where deworming medicine was provide had a significantly greater weight gain than similar children who attended child health days at which albendazole was not provided is unaffected; the CI for the difference in weight gain remains [59g ‐ 262 g]."
Recently the BMJ has invited me to submit a letter addressing the earlier comments as well as more recent variations of that theme. I believe that it is sufficient to indicate that the results presented in the multivariate analysis remain the basis for the conclusion of the trial. Given the heterogeneity of ages in the trial population and the fact that the velocity of weight gain is dependent on age, table 2 was presented for background only while the primary analysis was presented in table 3. The results in this table control for these covariates as well as the duration of time between visits or the total time a child participated in the child health days organized for his or her community. These results provide more precise estimates.
Harold Alderman
International food Policy Research Institute
I agree with the conflict of interest statement below:
I certify that I have no affiliations with or involvement in any organization or entity with a financial interest in the subject matter of my feedback.
Reply
Thank you for this information which is duly noted.
Contributors
David Taylor‐Robinson, Paul Garner, Sarah Donegan.
Christian Smith (Givewell ‐ Research Analyst), 4 October 2016
Summary
| Feedback comments | Author response |
| Comment: The research team at GiveWell has a handful of clarifying questions for the authors of the review on deworming treatments for children. | |
| Was there a protocol for the most recent update to the Cochrane Review? If so, could it be shared? | Updates are broadly guided by the original protocol and review and standard practice is to document the changes made in the “history” section. This protocol was first published in 1997 and the first edition of the review was published in 1998. At this time there was no online repository for Cochrane protocols; we have therefore made the original protocol available via the "Related content" section here: http://cidg.cochrane.org/our‐reviews Cochrane policy is that when a team continue updating a review where the question and inclusion criteria stay the same, the team draw on new information, comments and criticisms, and a review of the current debates, background, objectives, inclusion criteria and methods (see Table 2. In Garner et al. BMJ 2016; 354: i3507). No fresh protocol is prepared unless it is a new team, or there are substantial changes to the inclusion criteria or methods used in the analysis. However, the author team should ensure the changes are transparent and summarized in the “What’s new/history section” and that is present. |
| The "History" section at the end of the review notes: "We changed the classification of Stephenson 1989 and Stephenson 1993. Previously these trials were in the ‘all children in an endemic area’ category, whereas now they are classified in the ‘children with infection'. This decision was based on reviewing the trials with parasitologists and examining the prevalence and intensity of the infection where clearly the whole community was heavily infected” (p. 154). Could any information be shared about the process of consulting parasitologists on this topic or the output of those consultations?’ | The Stephenson studies were reviewed as part of our last update, since they were a source of heterogeneity. We were examining how best to take this into account. We noted that in the methods section the authors noted: "The subjects consisted of all available children in the lower grades (Standards I and II) in Mvindeni Primary School in Kwale District, Coast Province, Kenya, an area where our previous work had shown that virtually all of the primary schoolchildren had hookworm (predominantly Necator americanus) and T. trichiura infections and that 50% were infected with A. lumbricoides. "We had missed this information earlier. We consulted with LSTM parasitologists on this. They noted that virtually everyone was infected, and most were infected with at least two parasites and at least a third with three. In addition, the average hookworm loads put all the children into the moderate/heavy infection category. This is why this population was selected for the Stephenson studies. In this respect, the population chosen were equivalent to a population that had been screened to just include infected children. These indeed were quite old studies. So we made a decision that these studies were wrongly included in “treating the whole community” as everyone in the study population was infected. Hence they were reclassified. |
| Did you consult parasitologists about Watkins 1996? If so, how did you reach the conclusion to include that study in the “all children in an endemic area” category? | Our reading of the Stephenson studies was that the intention was to include a population where all children were infected. You ask about some other studies and why these were not reclassified as well (Watkins, Cruz, and Pollitt 1996). These were not in such high prevalence areas, but we take the point about the need to be systematic and will indeed have a closer look at their background prevalence in the update of the review. |
| Could you share any information about the rationale for the change in your classification schema from using "target population treated" to "all children in an endemic area" and "screened for infection" to "children with infection"? Does the change affect the classification of any studies included in the 2012 review other than Stephenson 1989 and Stephenson 1993? | This is because we judged that this was a better way of doing it. If all the children were infected (either because of the massively high worm infection burden, or as a result of screening), this was a clear way to describe the population. This is the whole reason for carrying out updates, to refine the analysis and make it clearer for the reader. |
| Is it the case that the Stephenson 1989 and Stephenson 1993 involved populations where every individual was infected? If not, was there a clear process for determining which studies fit under the "children with infection" classification? We are particularly curious about the rationale for including Stephenson 1993 under the "children with infection" classification while excluding Watkins 1996 from that classification. | As above. Virtually all of the children in the Stephenson studies had hookworm and Trichuris, and half had Ascaris. Indeed, the intention of the authors was to select them on this basis. |
| Croke et al. reported that adding Stephenson 1993 back into a fixed effects version of Analysis 4.1 leads to a statistically significant weight effect, but they do not appear to report the random effects meta‐analysis result (Croke at al. 2016, Table 2, p. 27). How would adding the relevant Stephenson 1993 result affect the random effects meta‐analysis results in Analysis 4.1? | When we realised that Stephenson 1993 was in an area where everyone included was infected we moved the study into a more appropriate comparison, as outlined above. We stand by this analysis and change. What you are proposing is not a sensitivity analysis, but seems to be “what would we get if we did this‐and would it be significant?” We believe it is not helpful to shift the study around or tweak the statistical analysis retrospectively as there is a risk of the analysis being driven by the outcome of the analysis rather than first principles of whether the analysis is appropriate. In addition, statistical significance is not a critical flag of whether something works: the size of the effect is also critical (see below). |
| If Analysis 4.1 resulted in a statistically significant weight gain, would the authors still maintain their position that mass deworming of children in endemic areas “does not improve average nutritional status" (p. 2)? | It is not just a matter of statistical significance. There is a danger in chasing whether a result is statistically significant, this can be misleading, particularly when combined with multiple analyses of the same data. What is more important in drawing conclusions with limited and mixed data is to consider heterogeneity in the meta‐analysis, and to interpret the results in light of this. The GRADE approach is used in the review, and the assessment takes into account the effect size, the precision, the risk of bias, the directness of evidence, and heterogeneity between estimates. The GRADE assessment draws on the estimate of weight change from the main analysis (0.08 kg, 95%CI 0.11 to 0.27; analysis 4.1); and the GRADE uses a sensitivity analysis (6.1). In this analysis, which includes only studies with low risk of bias for allocation concealment, there was no evidence of an effect (0.01, 95%CI ‐0.13 to 0.15; analysis 6.1). This analysis is dominated by a single study, so to double check our inferences for this response, we conducted a further sensitivity analysis with studies at clear risk of bias excluded (Awasthi 2000, and Awasthi 1995); this provides an estimate of ‐0.01 kg (95% CI ‐0.15 to 0.13). Thus our published estimate and GRADE stand, downgraded on risk of bias and inconsistency, and we conclude “there may be little to no effect on weight" based on the main analysis estimate. |
Christian Smith,
Do you have any affiliation with or involvement in any organisation with a financial interest in the subject matter of your comment?
As of October 2016, GiveWell recommends two charities that conduct mass drug administration programs for STH and Schistosomiasis—The Schistosomiasis Control Initiative and the Deworm the World Initiative, led by Evidence Action.
Reply
In the column above.
Contributors
David Taylor‐Robinson, Paul Garner.
What's new
| Date | Event | Description |
|---|---|---|
| 28 November 2019 | Amended | Titles of the Summary of findings tables amended for clarity |
History
Protocol first published: Issue 3, 1997 Review first published: Issue 2, 1998
| Date | Event | Description |
|---|---|---|
| 6 September 2019 | New search has been performed | Changes in this new edition followed a prespecified update plan, which is reported in Table 22. This table was approved by two CIDG Editor before we started the review update. The review author team updated the literature search and included six new trials. |
| 6 September 2019 | New citation required but conclusions have not changed | We included six new trials. We extracted detailed criticisms from a published critique of our review (Croke 2016). The details of our response are given in Table 14. The authors of Croke 2016 submitted a similar, but not identical, set of comments and criticisms through the Cochrane comments and criticisms on‐line feedback system. These were substantially the same as the published critique by Croke 2016. We answered them point by point and our responses were submitted to the Cochrane Editor. Previous criticisms concerned splitting the analysis between people infected and community studies. We took this into account. We conducted a fresh analysis on endemicity by worm type, and then constructed an overall classification of worm burden, and stratified the analysis by burden. We carried out subgroup analysis by burden of Ascaris for weight, and burden of hookworm for haemoglobin. The review authors considered the temporal trends in the data as worm loads may be getting lighter over time. We carried out a post‐hoc subgroup analysis dividing trials into those in this century and those in the previous century. Any dividing line would be arbitrary, but it was roughly midway over the time period that trials had been conducted. |
| 27 July 2015 | Amended | We added an external source of support, the Evidence and Programme Guidance Unit, Department of Nutrition for Health and Development, World Health Organization (WHO), to the Acknowledgements and Sources of support sections. |
| 8 July 2015 | New citation required but conclusions have not changed | A new search was conducted and new trials added. We also responded to feedback. |
| 26 February 2015 | New search has been performed |
|
| 10 October 2012 | New search has been performed | In September 2012, we identified a minor data entry error with a haemoglobin value, which we corrected. We also received feedback on the GRADE assessments. This led to changes in the assessment of the quality of the evidence for several outcomes. Most changes were towards higher quality evidence. We refined the table by adding additional footnotes to clarify the classification. The specific changes were:
We adjusted the wording in the abstract to take these changes into account. |
| 10 October 2012 | New citation required but conclusions have not changed | We updated the 'Summary of findings' tables, updated the abstract, and made minor corrections. |
| 31 May 2012 | New citation required but conclusions have not changed | We updated the review and added new studies. |
| 31 May 2012 | New search has been performed | Substantive update:
|
| 7 May 2008 | Amended | There are two alterations to the review:
|
| 12 August 2007 | New citation required and conclusions have changed | 2007, Issue 4 (substantive update): author team changed; we modified the review title from the original title of "Anthelmintic drugs for treating worms in children: effects on growth and cognitive performance"; we updated methods, reapplied the inclusion criteria, repeated data extraction, added new trials, and included additional analyses as recommended by policy specialists. |
| 31 March 2000 | New citation required and conclusions have changed | 2000, Issue 2 (substantive update): we added new trials and updated the review. |
Acknowledgements
The Academic Editor of this Cochrane Review is Dr Hellen Gelband, and the Sign‐off Editor is Professor Lisa Bero.
We thank all people who gave of their time and expertise to comment on this Cochrane Review. We thank all authors of earlier review versions.
This publication is associated with the Research, Evidence and Development Initiative (READ‐It) project. The CIDG editorial base and READ‐It (project number 300342‐104) is funded by UK aid from the UK government; however, the views expressed do not necessarily reflect the UK government’s official policies. The grant provides salary support for PG, MR, and the funds for the contract with NM.
Appendices
Appendix 1. Authors' judgment on risk of bias
| Potential bias | Authors' judgement |
| Random sequence generation (selection bias) |
High – not randomized or quasi‐randomized Unclear – states "randomized", but does not report method Low – describes method of randomizations |
| Allocation concealment (selection bias) |
High – not concealed, open‐label trial for individually randomised, method of concealment not adequate Unclear – details of method not reported or insufficient details Low – central allocation, sequentially numbered opaque sealed envelopes |
| Blinding (performance bias and detection bias) |
High – personnel, participants or outcome assessors not blinded Unclear – no details reported, insufficient details reported Low – personnel, participants and outcome assessors blinded |
| Incomplete outcome data (attrition bias) |
High – losses to follow‐up not evenly distributed across intervention and control group, high attrition rate (20% or more for the main outcome) Unclear ‐ no details reported, insufficient details reported Low – no losses to follow‐up, losses below 20% and evenly distributed across groups, ITT analysis used. Note: for cluster‐RCTs, the loss relates to the clusters |
| Selective reporting (reporting bias) |
High – did not fully report measured or relevant outcomes Unclear – not enough information reported to judge Low – all stated outcomes reported |
| Other bias |
Low – no obvious other source of bias of concern to reviewers High – major source of bias such as unexplained differences in baseline characteristics |
Appendix 2. Abridged table of characteristics
| TrialID Country | Who was treated? (Age) | How long was the follow‐up? | Trialdesign? (Number of participantsa) | Was it a cluster‐RCT? (No. of clusters) | What intervention? (Dose) | Co‐interventions?b | What control? | How long was the treatment? | Endemic area? (burden) |
|
Alderman 2006 (Cluster) Uganda |
Children (1 to 7 years) | 3 years | RCT (27,995) | Yes (48) | Albendazole (400 mg) | Child health package – both groups | No treatment | Every 6 months | Yes (intermediate) |
|
Awasthi 1995 (Cluster) India |
Children (1 to 4 years) | 2 years | Quasi‐RCT (3712) | Yes (50) | Albendazole (400 mg) | None | Placebo | Every 6 months | Yes (low) |
|
Awasthi 2000 India |
Children (1.5 to 3.5 years) | 2 years | Quasi‐RCT (1045) | No | Albendazole (600 mg) | None | Placebo | Every 6 months | Yes (low) |
|
Awasthi 2001 (Cluster) India |
Children (1 to 4 years) | 1.5 years | RCT (1672) | Yes (124) | Albendazole ± vitamin A (100,000 units) | Child health package – both groups | Placebo + vitamin A | Every 6 months | Yes (low) |
|
Awasthi 2013 (Cluster) India |
Children (≤ 5 years) | 5 years | RCT factorial (8338) | Yes (72) | Albendazole (400 mg) ± vitamin A | Child health package – both groups | Usual care | Every 6 months | Yes (not reported) |
|
Beach 1999 Haiti |
Children (grades 1 to 4) | 4 months | RCT (853) | No | Albendazole (400 mg) Ivermectin (200 to 400 μg/kg) |
None | Placebo + vitamin C (250 mg) | Single dose | Yes (intermediate) |
|
Donnen 1998 Zaire |
Children (0 to 72 months) | 1 year | RCT (222) | No | Mebendazole (500 mg) | None | Placebo + vitamin A (60 mg) No treatment |
Every 3 months | Yes (low) |
|
Dossa 2001 Benin |
Children (3 to 5 years) | 10 months | RCT (65) | No | Albendazole (200 mg) ± iron | None | Placebo | Repeated 1 month later | Yes (intermediate) |
|
Fox 2005 Haiti |
Children (5 to 11 years) | 6 months | RCT (626) | No | Albendazole (400 mg) ± vitamin C (250 mg) Diethylcarbamazine (DEC, 6 mg/kg) |
None | Placebo | Single dose | Yes (intermediate) |
|
Freij 1979a (Screened) Ethiopia |
Children (1.5 to 5 years) | 28 days | Quasi‐RCT (13) | No | Piperazine (3 g) | Child health package – both groups | Placebo | Single dose | Infected children (high) |
|
Freij 1979b (Screened) Ethiopia |
Children (1 to 5 years) | 34 days | Quasi‐RCT (44) | No | Piperazine (3 g x 2) | None | Placebo | Single dose | Infected children (high) |
|
Garg 2002 Kenya |
Children (2 to 4 years) | 6 months | RCT (347) | No | Mebendazole (500 mg) | Child health package – both groups | Placebo | Single dose | Yes (low) |
|
Gateff 1972 Cameroon |
Children (6 to 15 years) | 8 months | RCT (280) | No | Thiabendazole (50mg/kg) | None | Placebo | Three doses every 3 months | Yes (high) |
|
Goto 2009 Bangladesh |
Children (≤ 11 months) | 36 weeks | RCT (410) | No | Albendazole (200 mg) ± secnidazole (0.5 mL/kg, anti‐Giardia) | None | Placebo | Every 12 weeks | Yes (low) |
|
Greenberg 1981 Bangladesh |
Children (1.5 to 8 years) | 11 months | RCT (152) | No | Piperazine citrate (80 mg/kg) | None | Placebo | Two doses in 2 weeks | Yes (high) |
|
Gupta 1982 Guatemala |
Children (24 to 61 months) | 1 year | RCT (159) | No | Piperazine (75 mg/kg) ± metronidazole(25 mg/kg) | None | Placebo ± metronidazole | Every 2 months for 1 year | Yes (intermediate) |
|
Hadju 1996 Indonesia |
Children (6 to 10 years) | 7 weeks | RCT (64) | No | Pyrantel pamoate (10 mg/kg) | None | Placebo | Single dose | Yes (high) |
|
Hadju 1997 Indonesia |
Children (± 8.3 years) | 1 year | RCT (330) | No | Albendazole (400 mg) Pyrantel pamoate (10 mg/kg) |
None | Placebo | Single dose or every 6 months | Yes (high) |
|
Hall 2006 (Cluster) Vietnam |
Children (± 104.5 months) | 2 years | RCT (2,659) | Yes (80) | Albendazole (400 mg) ± retinol (200,000 IU) | None | Placebo | Every 6 months | Yes (high) |
|
Joseph 2015 Peru |
Children (± 12.5 months) | 1 year | RCT (1760) | No | Mebendazole (500 mg) | None | Placebo | Single dose or two doses 6 months apart | Yes (low) |
|
Kirwan 2010 Nigeria |
Children (1 to 5 years) | 14 months | RCT (320) | No | Albendazole (200 to 400 mg) | Child health package – both groups | Placebo | Every 4 months | Yes (intermediate) |
|
Kloetzel 1982 Cameroon |
Children (1 to 8 years) | 10 months | RCT (337) | No | Mebendazole (100 mg x3) | None | Placebo | 3 doses in 3 days | Yes (high) |
|
Koroma 1996 Sierra Leone |
Children (6 to 10 years) | 6 months | RCT (187) | No | Albendazole (400 mg) | None | Placebo | Single dose | Yes (intermediate) |
|
Kruger 1996 South Africa |
Children (6 to 8 years) | 11 months | RCT (178) | No | Albendazole (400 mg) ± soup fortified with iron and vitamin C | Child health package – both groups | Placebo ± soup fortified with iron and vitamin C | Repeated at 4 months | Yes (intermediate) |
|
Kvalsvig 1991a (Screened) South Africa |
Children (primary school) | 1 month | RCT (unclear) | No | Mebendazole (500 mg) | None | Placebo | Single dose | Infected children (high) |
|
Lai 1995 Malaysia |
Children (8 years) | 2 years | RCT (314) | No | Mebendazole (100 mg) + pyrantel (200 mg) | None | Placebo | Every 3 months | Yes (high) |
|
Le Huong 2007 Vietnam |
Children | 6 months | RCT factorial (510) | No | Mebendazole (500 mg) | Iron‐fortified noodles | Placebo | Twice 3 months apart | Yes (high) |
|
Liu 2017 (Cluster) China |
Children (9 to 11 years) | 6 months | RCT (2,240) | Yes (112) | Albendazole (400 mg) | None | No treatment | Twice 6 months apart | Yes (intermediate) |
|
Michaelsen 1985 Botswana |
Children (5 to 14 years) | 5 months | RCT (121) | No | Tetrachloroethylene (0.1 mL/kg) | None | Placebo | Single dose | Yes (high) |
|
Miguel 2004 (Cluster) Kenya |
Children (8 years) | 2 years | RCT (9102) | Yes (65) | Albendazole (400 to 600 mg) | Child health package – only intervention group | No treatment | Every 6 months | Yes (high) |
|
Ndibazza 2012 Uganda |
Children (± 15 months) | Post‐treatment | RCT factorial (1423) | No | Albendazole (200 to 400 mg) | Child health package – both groups | Placebo | ?? | Yes (low) |
|
Nga 2009 Vietnam |
Children (6 to 8 years) | 4 months | RCT (510) | No | Albendazole (400 mg) ± multi‐micronutrient fortified biscuit | None | Placebo | Single dose | Yes (intermediate) |
|
Nokes 1992 (Screened) Jamaica |
Children (9 to 12 years) | 9 weeks | RCT (103) | No | Albendazole (400 mg x3) | None | Placebo | Single dose | Infected children (high) |
|
Olds 1999 China, Philippines and Kenya |
Children (school children) | 6 months | RCT (103) | No | Albendazole (400 mg) ± praziquantel (40 mg/kg) | None | Placebo | Single dose | Yes (intermediate) |
| Ostwald 1984 | Children (7 to 10 years) | 5 months | RCT (105) | No | Mebendazole (not reported) | None | Not reported | Repeated after 2 months | Yes (high) |
|
Palupi 1997 Indonesia |
Children (2 to 5 years) | 9 weeks | RCT (191) | No | Albendazole (400 mg) | Iron | Iron (30 mg weekly) | Single dose | Yes (intermediate) |
|
Rousham 1994 (Cluster) Bangladesh |
Children (2 to 6 years) | 18 months | RCT (1,402) | Yes (13) | Mebendazole (500 mg) Pyrantel pamoate (10 mg/kg) |
None | Placebo | Every 2 months | Yes (intermediate) |
|
Sarkar 2002 (Screened) Bangladesh |
Children (2 to 12 years) | 16 weeks | RCT (81) | No | Pyrantel pamoate (11 mg/kg) | None | Placebo | Single dose | Infected children (high) |
|
Simeon 1995 (Screened) Jamaica |
Children (6 to 12 years) | 26 weeks | RCT (392) | No | Albendazole (800 mg) | None | Placebo | Repeated 3 to 6 months after | Infected children (high) |
|
Solon 2003 Philippines |
Children (grades 1 to 6) | 16 weeks | RCT (851) | No | Albendazole (400 mg) ± multivitamin and iron | None | Placebo | Repeated 3 to 6 months after | Yes (intermediate) |
|
Stephenson 1989 Kenya |
Children (grades 1 to 2) | 6 months | RCT (150) | No | Albendazole (400 mg) | None | Placebo | Single dose | Yes (high) |
|
Stephenson 1993 Kenya |
Children (grades 1 to 5) | 8 months | RCT (284) | No | Albendazole (600 mg) | None | Placebo | Repeated 3 to 6 months after | Yes (high) |
|
Sternberg 1997 (Screened) Jamaica |
Children (± 10.25 years) | 10 weeks | RCT (133) | No | Albendazole (400 mg) | None | Placebno | Single dose | Infected children (high) |
|
Stoltzfus 1997 (Cluster) Tanzania, Zanzibar |
Children (± 10.5 years) | 12 months | RCT (3063) | Yes (12) | Mebendazole (500 mg, 2x or 3x) | None | Placebo | Every 4 or 6 months | Yes (high) |
|
Stoltzfus 2001 Tanzania, Zanzibar |
Children (6 to 59 months) | 12 months | RCT factorial (359) | No | Mebendazole (500 mg) ± iron | None | Placebo | Every 3 months | Yes (intermediate) |
|
Sur 2005 India |
Children (2 to 5 years) | 12 months | RCT (683) | No | Albendazole (400 mg) ± vitamin B | None | Placebo | Every 6 months | Yes (intermediate) |
|
Tee 2013 (Screened) Malaysia |
Children | 12 months | RCT (33) | No | Albendazole (400 mg x 2) | None | Placebo | Single dose | Yes (high) |
|
Watkins 1996 Guatemala |
Children (7 to 12 years) | 6 months | RCT (226) | No | Albendazole (400 mg) | None | Placebo | Repeated at 12 weeks | Yes (high) |
|
Willett 1979 Tanzania |
Children (6 to 91 months) | 12 months | RCT (268) | No | Levamisole (2.5 mg/kg) | None | Placebo | Every 3 months | Yes (intermediate) |
|
Wiria 2013 (Cluster) Indonesia |
Children and adults ≥ 2 years | 21 months | RCT (855) | Yes (954) | Albendazole (400 mg x 3) | None | Placebo | Single dose | Yes (high) |
|
Yap 2014 (Screened) Myanmar, China |
Children (9 to 12 years) | 6 months | RCT (194) | No | Albendazole (400 mg x 3) | None | Placebo | Single dose | Infected children (high) |
aNumber of participants analysed for primary outcome. bFor details on "child health package" please see Table 9: accompanying health promotion activities.
Appendix 3. Burden
| Study | Any infection | Ascaris | Trichuris | Hookworm | Comments | ||||||||
| Prevalence | Intensity | Burden | Prevalence | Intensity | Burden | Prevalence | Intensity | Burden | Prevalence | Intensity | Burden | ||
| Alderman 2006 (Cluster) | Intermediate | (average epg) | Intermediate | Low | (average epg) | Low | Low | (average epg) | Low | Intermediate | (average epg) | Intermediate | Previous survey |
| Awasthi 1995 (Cluster) | Low | Not reported | Low | Low | Not reported | Low | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Study comments on prevalence of worms in the sample of children but does not give baseline data |
| Awasthi 2000 | Low | Not reported | Low | Low | Not reported | Low | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Baseline for one species only |
| Awasthi 2001 (Cluster) | Low | Not reported | Low | Low | Not reported | Low | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Baseline for one species only |
| Awasthi 2013 (Cluster) | Not reported | Not reported | Not reported | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | No information reported |
| Beach 1999 | Intermediate | Low | Intermediate | Intermediate | Low | Intermediate | Intermediate | Low | Intermediate | Low | Low | Low | Measured prevalence and intensity for all worms at baseline |
| Donnen 1998 | Low | Low | Low | Low | Low | Low | Not applicable | Not applicable | Not applicable | Low | Low | Low | Measured prevalence and intensity for all worms at baseline |
| Dossa 2001 | Intermediate | Not reported | Intermediate | Intermediate | Not reported | Intermediate | Intermediate | Not reported | Intermediate | Low | Not reported | Low | No information reported on intensity |
| Fox 2005 | Intermediate | Low | Intermediate | Intermediate | Low | Intermediate | Low | Low | Low | Intermediate | Low | Intermediate | Measured prevalence and intensity for all worms at baseline |
| Freij 1979a (Screened) | Screened | Not reported | High | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | None |
| Freij 1979b (Screened) | Screened | Not reported | High | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | None |
| Garg 2002 | Low | Low | Low | Low | Low | Low | Low | Low | Low | Low | Low | Low | Previous cross‐sectional study |
| Gateff 1972 | High | Not reported | High | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | None |
| Goto 2009 | Low | Low | Low | Low | Low | Low | Low | Low | Low | Not applicable | Not applicable | Not applicable | Measured prevalence and intensity for all worms at baseline |
| Greenberg 1981 | High | High | High | High | High | High | Intermediate | Not reported | Intermediate | Low | Not reported | Low | Measured prevalence and intensity for all worms at baseline |
| Gupta 1982 | Intermediate | Not reported | Intermediate | Intermediate | Not reported | Intermediate | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | None |
| Hadju 1996 | High | High | High | High | High | High | High | High | High | Not applicable | Not applicable | Not applicable | Measured prevalence and intensity for all worms at baseline |
| Hadju 1997 | High | (average epg) | High | High | (average epg) | High | High | (average epg) | High | Not applicable | Not applicable | Not applicable | None |
| Hall 2006 (Cluster) | High | (average epg) | High | Intermediate | (average epg) | Intermediate | High | (average epg) | High | Low | (average epg) | Low | None |
| Joseph 2015 | Low | Low | Low | Low | Low | Low | Low | Low | Low | Low | Low | Low | Measured prevalence and intensity for all worms at baseline |
| Kirwan 2010 | Intermediate | Low | Intermediate | Intermediate | Low | Low | Low | Low | Low | Low | (average epg) | Low | Measured prevalence and intensity for all worms at baseline |
| Kloetzel 1982 | Intermediate | High | High | Intermediate | High | High | Intermediate | Not reported | Intermediate | Low | Not reported | Low | No information reported on intensity for Trichuris and hookworm |
| Koroma 1996 | Intermediate | (average epg) | Intermediate | Intermediate | (average epg) | Intermediate | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | None |
| Kruger 1996 | Intermediate | Not reported | Intermediate | Intermediate | Not reported | Intermediate | Intermediate | Not reported | Intermediate | Low | Not reported | Low | No information reported on intensity |
| Kvalsvig 1991a (Screened) | Screened | Not reported | High | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | None |
| Lai 1995 | Intermediate | High | High | Intermediate | High | High | Intermediate | High | High | Low | Not reported | Low | Measured prevalence and intensity for all worms at baseline |
| Le Huong 2007 | Intermediate | High | High | Intermediate | High | High | Intermediate | Low | Intermediate | Low | Low | Low | Measured prevalence and intensity for all worms at baseline |
| Liu 2017 (Cluster) | Intermediate | Low | Intermediate | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | None |
| Michaelsen 1985 | High | Low | High | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | High | Low | High | Baseline data not reported |
| Miguel 2004 (Cluster) | Intermediate | High | High | Intermediate | High | High | Intermediate | ? (intensity=10%) | Intermediate | High | High | Measured prevalence and intensity for all worms at baseline | |
| Ndibazza 2012 | Low | Not reported | Low | Low | Not reported | Low | Low | Not reported | Low | Low | Not reported | Low | No information reported on intensity |
| Nga 2009 | Intermediate | Low | Intermediate | Intermediate | Low | Intermediate | Intermediate | Low | Intermediate | Low | Low | Low | Measured prevalence and intensity for all worms at baseline |
| Nokes 1992 (Screened) | Screened | High | High | Not applicable | Not applicable | Not applicable | Screened | High | High | Low | Low | Low | None |
| Olds 1999 | Intermediate | Not reported | Intermediate | Intermediate | Not reported | Intermediate | Intermediate | Not reported | Intermediate | Intermediate | Not reported | Intermediate | No information reported on intensity |
| Ostwald 1984 | High | Not reported | High | Intermediate | Not reported | Intermediate | Intermediate | Not reported | Intermediate | High | Not reported | High | None |
| Palupi 1997 | Intermediate | (average epg) | Intermediate | Intermediate | (average epg) | Intermediate | Intermediate | (average epg) | Intermediate | Low | Low | Low | None |
| Rousham 1994 (Cluster) | Intermediate | Low | Intermediate | Intermediate | Low | Intermediate | Intermediate | Low | Intermediate | Low | Low | Low | Measured prevalence and intensity for all worms at baseline |
| Sarkar 2002 (Screened) | Screened | Not reported | High | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | None |
| Simeon 1995 (Screened) | Screened | High | High | Intermediate | High | High | Screened | High | High | Not applicable | Not applicable | Not applicable | None |
| Solon 2003 | Intermediate | Not reported | Intermediate | Intermediate | Not reported | Intermediate | Intermediate | Not info | Intermediate | Intermediate | Not reported | Intermediate | No information reported on intensity |
| Stephenson 1989 | High | (average epg) | High | Intermediate | (average epg) | Intermediate | High | (average epg) | High | High | (average epg) | High | None |
| Stephenson 1993 | High | (average epg) | High | Intermediate | (average epg) | Intermediate | High | (average epg) | High | High | (average epg) | High | None |
| Sternberg 1997 (Screened) | High | (average epg) | High | Not applicable | Not applicable | Not applicable | High | (average epg) | High | Not applicable | Not applicable | Not applicable | None |
| Stoltzfus 1997 (Cluster) | High | (average epg) | High | Intermediate | (average epg) | Intermediate | High | (average epg) | High | High | (average epg) | High | None |
| Stoltzfus 2001 | Intermediate | (average epg) | Intermediate | Intermediate | (average epg) | Intermediate | Intermediate | (average epg) | Intermediate | Intermediate | (average epg) | Intermediate | None |
| Sur 2005 | Intermediate | Not reported | Intermediate | Intermediate | Not reported | Intermediate | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | None |
| Tee 2013 (Screened) | Screened | Not reported | High | Not applicable | Not applicable | Not applicable | Screened | Not reported | High | Not applicable | Not applicable | Not applicable | None |
| Watkins 1996 | High | High | High | High | High | High | High | High | High | Low | Low | Low | Measured prevalence and intensity for all worms at baseline |
| Willett 1979 | Intermediate | (average epg) | Intermediate | Low | (average epg) | Low | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | Not applicable | None |
| Wiria 2013 (Cluster) | Intermediate | Not reported | Intermediate | Intermediate | Not reported | Intermediate | Intermediate | Not info | Intermediate | Intermediate | Not reported | Intermediate | No information reported on intensity |
| Yap 2014 (Screened) | Screened | (average epg) | High | High | (average epg) | High | High | (average epg) | High | High | (average epg) | High | None |
Appendix 4. Age categories: weight
1. Single dose
| Age category | Number of studies | ||
| High burden | Intermediate burden | Low burden | |
| Infants, young, preschool, school | 0 | 0 | 1 (Donnen 1998) |
| Young | 0 | 0 | 1 (Joseph 2015) |
| Young, preschool | 1 (Freij 1979a (Screened)) | 0 | 1 (Awasthi 2000) |
| Preschool | 0 | 2 (Palupi 1997; Sur 2005) | 1 (Garg 2002) |
| Preschool, school | 1 (Sarkar 2002 (Screened)) | 0 | 0 |
| School | 6 (Gateff 1972, Hadju 1996, Stephenson 1989, Stephenson 1993, Watkins 1996, Yap 2014 (Screened)) | 0 | 0 |
2. Multiple doses
| Age category | Number of studies | ||
| High burden | Intermediate burden | Low burden | |
| Infants | 0 | 0 | 1 (Awasthi 2001 (Cluster)) |
| Infant, young, preschool, school | 0 | 0 | 1 (Donnen 1998) |
| Young | 0 | 0 | 2 (Joseph 2015; Ndibazza 2012) |
| Young, preschool | 0 | 0 | 2 (Awasthi 1995 (Cluster); Awasthi 2000) |
| Young, preschool, school | 0 | 1 (Alderman 2006 (Cluster)) | 0 |
| Preschool | 0 | 3 (Dossa 2001; Gupta 1982; Sur 2005) | 0 |
| School | 6 (Gateff 1972; Hall 2006 (Cluster); Miguel 2004 (Cluster); Ostwald 1984; Stephenson 1993; Watkins 1996) | 2 (Kruger 1996; Liu 2017 (Cluster)) | 0 |
Data and analyses
Comparison 1. Single dose.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Weight (kg) | 14 | 4970 | Mean Difference (Random, 95% CI) | 0.23 [0.05, 0.42] |
| 1.1 High burden | 8 | 1221 | Mean Difference (Random, 95% CI) | 0.57 [0.08, 1.06] |
| 1.2 Intermediate burden | 2 | 873 | Mean Difference (Random, 95% CI) | 0.11 [‐0.16, 0.39] |
| 1.3 Low burden | 4 | 2876 | Mean Difference (Random, 95% CI) | ‐0.05 [‐0.13, 0.04] |
| 2 Height (cm) | 10 | 2621 | Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.14, 0.23] |
| 2.1 High burden | 6 | 874 | Mean Difference (IV, Random, 95% CI) | 0.20 [‐0.00, 0.40] |
| 2.2 Intermediate burden | 1 | 191 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.47, 0.07] |
| 2.3 Low burden | 3 | 1556 | Mean Difference (IV, Random, 95% CI) | ‐0.26 [‐0.74, 0.21] |
| 3 Mid‐upper arm circumference (cm) | 7 | 1307 | Mean Difference (IV, Random, 95% CI) | 0.19 [‐0.04, 0.41] |
| 3.1 High burden | 5 | 603 | Mean Difference (IV, Random, 95% CI) | 0.32 [0.06, 0.57] |
| 3.2 Intermediate burden | 1 | 482 | Mean Difference (IV, Random, 95% CI) | 0.19 [‐0.01, 0.40] |
| 3.3 Low burden | 1 | 222 | Mean Difference (IV, Random, 95% CI) | ‐0.3 [‐0.52, ‐0.08] |
| 4 Triceps skin fold thickness (mm) | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 High burden | 3 | 352 | Mean Difference (IV, Random, 95% CI) | 1.34 [0.72, 1.97] |
| 5 Subscapular skin fold thickness (mm) | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 High burden | 2 | 339 | Mean Difference (IV, Fixed, 95% CI) | 1.29 [1.13, 1.44] |
| 6 Body mass index | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.1 High burden | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Haemoglobin (g/dL) | 5 | 1252 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.03, 0.22] |
| 7.1 High burden | 2 | 247 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.65, 0.86] |
| 7.2 Intermediate burden | 2 | 658 | Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.06, 0.17] |
| 7.3 Low burden | 1 | 347 | Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.24, 0.36] |
Comparison 2. Multiple doses.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Weight (kg) | 18 | 5744 | Mean Difference (Random, 95% CI) | 0.11 [‐0.01, 0.24] |
| 1.1 High burden | 6 | 911 | Mean Difference (Random, 95% CI) | 0.20 [‐0.17, 0.56] |
| 1.2 Intermediate burden | 6 | 1308 | Mean Difference (Random, 95% CI) | 0.09 [‐0.01, 0.20] |
| 1.3 Low burden | 6 | 3525 | Mean Difference (Random, 95% CI) | 0.11 [‐0.16, 0.37] |
| 2 Height (cm) | 13 | 4586 | Mean Difference (Fixed, 95% CI) | 0.02 [‐0.09, 0.13] |
| 2.1 High burden | 3 | 501 | Mean Difference (Fixed, 95% CI) | 0.04 [‐0.12, 0.20] |
| 2.2 Intermediate burden | 4 | 578 | Mean Difference (Fixed, 95% CI) | 0.10 [‐0.13, 0.33] |
| 2.3 Low burden | 6 | 3507 | Mean Difference (Fixed, 95% CI) | ‐0.08 [‐0.29, 0.14] |
| 3 Mid‐upper arm circumference (cm) | 4 | 722 | Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.19, 0.32] |
| 3.1 High burden | 2 | 395 | Mean Difference (IV, Random, 95% CI) | 0.24 [‐0.07, 0.55] |
| 3.2 Intermediate burden | 1 | 129 | Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.22, 0.33] |
| 3.3 Low burden | 1 | 198 | Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.65, ‐0.05] |
| 4 Triceps skin fold thickness (mm) | 2 | 318 | Mean Difference (IV, Random, 95% CI) | 0.43 [‐1.26, 2.12] |
| 4.1 High burden | 1 | 188 | Mean Difference (IV, Random, 95% CI) | 1.80 [1.52, 2.08] |
| 4.2 Intermediate burden | 1 | 130 | Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐1.28, 0.68] |
| 5 Subscapular skin fold thickness (mm) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 High burden | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Body mass index | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.1 High burden | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Haemoglobin (g/dL) | 9 | 3432 | Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.05, 0.07] |
| 7.1 High burden | 2 | 396 | Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.16, 0.18] |
| 7.2 Intermediate burden | 4 | 748 | Mean Difference (IV, Fixed, 95% CI) | 0.11 [‐0.03, 0.26] |
| 7.3 Low burden | 3 | 2288 | Mean Difference (IV, Fixed, 95% CI) | ‐0.01 [‐0.09, 0.06] |
| 8 School attendance (days present at school) | 3 | 700 | Mean Difference (Random, 95% CI) | 0.02 [‐0.05, 0.08] |
| 8.1 High burden | 3 | 700 | Mean Difference (Random, 95% CI) | 0.02 [‐0.05, 0.08] |
Comparison 3. Single dose (by worm type).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Weight (kg) | 14 | Mean Difference (Random, 95% CI) | 0.23 [0.05, 0.42] | |
| 1.1 Ascaris ‐ High burden | 4 | Mean Difference (Random, 95% CI) | 0.20 [‐0.03, 0.43] | |
| 1.2 Ascaris ‐ Intermediate burden | 4 | Mean Difference (Random, 95% CI) | 0.75 [‐0.01, 1.50] | |
| 1.3 Ascaris ‐ Low burden | 4 | Mean Difference (Random, 95% CI) | ‐0.05 [‐0.13, 0.04] | |
| 1.4 Ascaris ‐ not reported | 2 | Mean Difference (Random, 95% CI) | 0.15 [‐1.81, 2.10] | |
| 2 Haemoglobin (g/dL) | 5 | 1252 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.03, 0.22] |
| 2.1 Hookworm ‐ High burden | 2 | 247 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.65, 0.86] |
| 2.2 Hookworm ‐ Low burden | 3 | 1005 | Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.05, 0.17] |
Comparison 4. Multiple doses (by worm type).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Weight (kg) | 18 | Mean Difference (Random, 95% CI) | 0.11 [‐0.01, 0.24] | |
| 1.1 Ascaris ‐ High burden | 2 | Mean Difference (Random, 95% CI) | ‐0.22 [‐0.98, 0.55] | |
| 1.2 Ascaris ‐ Intermediate burden | 7 | Mean Difference (Random, 95% CI) | 0.18 [‐0.03, 0.39] | |
| 1.3 Ascaris ‐ Low burden | 7 | Mean Difference (Random, 95% CI) | 0.11 [‐0.10, 0.33] | |
| 1.4 Ascaris ‐ Not reported | 2 | Mean Difference (Random, 95% CI) | 0.03 [‐0.25, 0.31] | |
| 2 Haemoglobin (g/dL) | 9 | 3432 | Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.05, 0.07] |
| 2.1 Hookworm ‐ High burden | 1 | 70 | Mean Difference (IV, Fixed, 95% CI) | 0.30 [‐0.24, 0.84] |
| 2.2 Hookworm ‐ Low burden | 5 | 2071 | Mean Difference (IV, Fixed, 95% CI) | 0.03 [‐0.07, 0.13] |
| 2.3 Hookworm ‐ Not reported | 3 | 1291 | Mean Difference (IV, Fixed, 95% CI) | ‐0.00 [‐0.08, 0.07] |
Comparison 5. Single dose (only low risk of bias for allocation concealment).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Weight (kg) | 3 | Mean Difference (Fixed, 95% CI) | 0.08 [‐0.06, 0.21] | |
| 1.1 High burden | 1 | Mean Difference (Fixed, 95% CI) | 0.3 [‐0.05, 0.65] | |
| 1.2 Intermediate burden | 1 | Mean Difference (Fixed, 95% CI) | 0.5 [‐0.28, 1.28] | |
| 1.3 Low burden | 1 | Mean Difference (Fixed, 95% CI) | 0.02 [‐0.13, 0.17] | |
| 2 Height (cm) | 2 | 541 | Mean Difference (IV, Fixed, 95% CI) | 0.15 [‐0.04, 0.34] |
| 2.1 High burden | 1 | 194 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐0.05, 0.45] |
| 2.2 Low burden | 1 | 347 | Mean Difference (IV, Fixed, 95% CI) | 0.08 [‐0.21, 0.37] |
| 3 Mid‐upper arm circumference (cm) | 1 | 482 | Mean Difference (IV, Fixed, 95% CI) | 0.19 [‐0.01, 0.40] |
| 3.1 Intermediate burden | 1 | 482 | Mean Difference (IV, Fixed, 95% CI) | 0.19 [‐0.01, 0.40] |
| 4 Haemoglobin (g/dL) | 3 | 1008 | Mean Difference (IV, Fixed, 95% CI) | 0.04 [‐0.08, 0.16] |
| 4.1 High burden | 1 | 194 | Mean Difference (IV, Fixed, 95% CI) | ‐0.40 [‐1.25, 0.45] |
| 4.2 Intermediate burden | 1 | 467 | Mean Difference (IV, Fixed, 95% CI) | 0.05 [‐0.08, 0.17] |
| 4.3 Low burden | 1 | 347 | Mean Difference (IV, Fixed, 95% CI) | 0.06 [‐0.24, 0.36] |
Comparison 6. Multiple doses (only low risk of bias for allocation concealment).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Weight (kg) | 2 | Mean Difference (Fixed, 95% CI) | 0.01 [‐0.13, 0.15] | |
| 1.1 High burden | 1 | Mean Difference (Fixed, 95% CI) | 0.0 [‐0.14, 0.14] | |
| 1.2 Intermediate burden | 1 | Mean Difference (Fixed, 95% CI) | 0.5 [‐0.42, 1.42] | |
| 2 Haemoglobin (g/dL) | 1 | 326 | Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.21, 0.16] |
| 2.1 High burden | 1 | 326 | Mean Difference (IV, Fixed, 95% CI) | ‐0.02 [‐0.21, 0.16] |
Comparison 7. Multiple doses ‐ ordered by year.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Weight (kg) | 18 | Mean Difference (Random, 95% CI) | 0.11 [‐0.01, 0.24] | |
| 2 Weight (kg) | 18 | 5694 | Mean Difference (Random, 95% CI) | 0.11 [‐0.01, 0.24] |
| 2.1 published before 2000 | 8 | 1366 | Mean Difference (Random, 95% CI) | 0.26 [‐0.06, 0.58] |
| 2.2 published in 2000 or later | 10 | 4328 | Mean Difference (Random, 95% CI) | 0.02 [‐0.04, 0.08] |
7.1. Analysis.
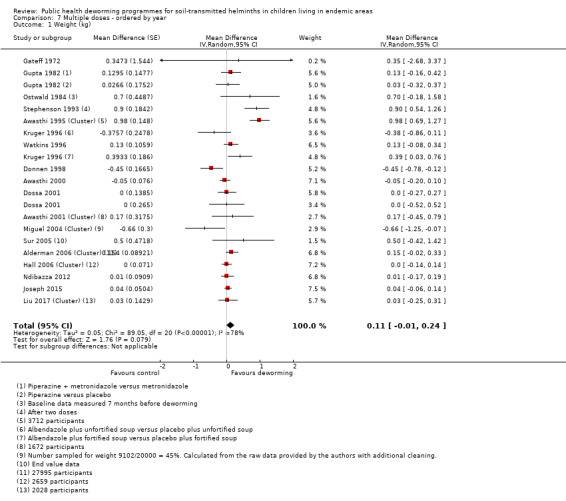
Comparison 7 Multiple doses ‐ ordered by year, Outcome 1 Weight (kg).
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Alderman 2006 (Cluster).
| Methods | Cluster‐RCT Method to adjust for clustering: not adjusted Cluster unit: parish Average cluster size: 560 ICCs: not reported but calculated from adjusted and unadjusted figures to be 0.01. Length of follow‐up: 3 years |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 48 parishes randomized containing 27,995 children Age range: 1 to 7 years Inclusion criteria: children aged 1 to 7 in 50 parishes in Uganda selected by the government on the basis that around 60% of children aged 5 to 10 years in these parishes were infected with intestinal nematodes Exclusion criteria: sick children |
|
| Interventions | Multiple dose vs no treatment
|
|
| Outcomes |
|
|
| Notes | Location: Uganda Burden: intermediate Weight gain data taking into account the effects of cluster randomization provided by the author. Source of funding: the nutrition and early child development project, government of Uganda, the Institute of Public Health and the research committee of the World Bank. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Coin toss Quote: "The randomization was done by a member of the research team (HA) by assigning numbers to all of the parishes and converting these to base two and then determining which of the parishes were to be in the treatment by coin flips". |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | High risk | None. Quote: "It was not possible for us to carry out a double blind trial because of the scale of the programme and because we aimed to assess the effectiveness of giving albendazole […] during standard child health days without any trial specific inputs". |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 75% (27,995/37,165) of members of the randomized clusters were evaluated. |
| Selective reporting (reporting bias) | Low risk | All stated outcomes reported. |
| Other bias | Low risk | Recruitment bias: low risk Baseline imbalance: characteristics similar (low risk) Loss of clusters: nil (low risk) Incorrect analysis: primary outcome in paper not adjusted for clustering (personal communication Harold Alderman), but Cochrane Review adjusts this (low risk) Comparability with RCTs randomizing individuals: unclear |
Awasthi 1995 (Cluster).
| Methods | Cluster‐quasi‐RCT Method to adjust for clustering: cluster used as unit of analysis Cluster unit: urban slum Average cluster size: 74 ICCs: not reported. Length of follow‐up: 2 years |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 50 slums randomized containing 3712 children Age range: 1 to 4 years Inclusion criteria: children aged 1 to 4 from 50 urban slums in Lucknow selected on the basis of geographic convenience Exclusion criteria: none stated |
|
| Interventions | Multiple doses vs placebo
|
|
| Outcomes |
|
|
| Notes | Location: Lucknow, India Burden: low Trial carried out in 1995 and published in 2008. Source of funding: Clinical Trial Service Unit (CTSU), University of Oxford, UK, and co‐funded by the International Clinical Epidemiology Network Inc., Philadelphia, USA. Albendazole was donated by SmithKline Beecham (now GlaxoSmithKline). For the analysis of Awasthi 1995 (Cluster) we took weight from the publication by Awasthi in 2008; height data from INCLEN 1995 monograph (references contained in the main reference). Means of cluster means were used in analysis; details of correspondence from previous review suggest that trial was ongoing; data for 3‐year follow‐up are provided from R. Dickson's correspondence with the author for the Dickson 2000a Cochrane Review, but the loss to follow‐up is very high: only 24% analysed. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quasi‐randomized: Quote: "Random allocation was done by SA, listing the anganwadi centers of each slum area serially in alphabetical order, numbering them from 1 to 50, and then generating a single random number by computer that allocated either all odd or all even numbers to a specific intervention type" |
| Allocation concealment (selection bias) | High risk | Not concealed. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Cluster‐RCT with health staff and participants knowing which group they were allocated to. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1852/1968 children in the treatment group completed all follow‐up visits; 1860/1967 children in the usual care group completed all follow‐up visits. Inclusion of all participants who were randomized within clusters (number evaluable/number randomized): 94% (3712/3935). |
| Selective reporting (reporting bias) | Low risk | All stated outcomes reported. |
| Other bias | Low risk | Recruitment bias: unclear (not known if children shift clinics in the light of the intervention) Baseline imbalance: unclear Loss of clusters: low (none reported) Incorrect analysis: cluster adjusted (low risk) Comparability with RCTs randomizing individuals: unclear |
Awasthi 2000.
| Methods | Quasi‐RCT Length of follow‐up: 2 years |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 1045 Age range: 1.5 to 3.5 years Inclusion criteria: children living in 32 randomly selected urban slums; registered with an Anganwadi worker (health worker); between 1.5 to 3.5 years of age Exclusion criteria: none stated |
|
| Interventions | Multiple doses vs placebo
|
|
| Outcomes |
Not included in review: prevalence of underweight and stunting over 2 years as defined by z‐scores, haemoglobin (visual colour estimation), stool examination (non‐concentration method), incidence of illness, and death |
|
| Notes | Location: Lucknow, India Burden: low Source of funding: International Clinical Epidemiology Network (INCLEN), Philadelphia, USA grant #2002‐94‐623 under the Clinical Economics Small Grants Program. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | 32 Anganwadi centres randomly selected, and then children allocated to a serial number; those with odd or non‐zero ending numbers were assigned to placebo. |
| Allocation concealment (selection bias) | High risk | Not concealed. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Single‐blind (children). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 9/610 children in the albendazole group and 7/451 in the placebo group were lost to follow‐up. Inclusion of all randomized participants (number evaluable/number randomized): 98% (1045/1061). |
| Selective reporting (reporting bias) | Low risk | All stated outcomes reported. |
| Other bias | Low risk | No other obvious source of bias. |
Awasthi 2001 (Cluster).
| Methods | Cluster‐RCT Method to adjust for clustering: cluster used as unit of analysis. Cluster unit: urban slums Average cluster size: 13.5 ICCs: not reported. Length of follow‐up: 1.5 years |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 124 slums randomized containing 1672 children Age range/ mean age: 0.8 years Inclusion criteria: clusters selected if they had functional community workers in slum areas of Lucknow; within each cluster, children recruited if aged between 0.5 and 1 year, on basis of survey register held by each worker of their particular area Exclusion criteria: none stated |
|
| Interventions | Multiple doses vs placebo
|
|
| Outcomes |
Not included in review: stool smear for Ascaris prevalence on a subsample of the group; death rates |
|
| Notes | Location: Lucknow, India Burden: low Means of cluster means used in analysis. The results (weight gain) in the abstract differ from the text. Source of funding: International Clinical Epidemiological Network (INCLEN) Inc, USA and Clinical Trials Unit (CTSU), Oxford, UK. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Cluster‐randomized trial, no further details. |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No details reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat (ITT) analysis; 13.9% lost to follow‐up in albendazole group and 16.2% in the placebo group. Inclusion of all participants who were randomized within clusters (number evaluable/number randomized): 83% (1672/2010). |
| Selective reporting (reporting bias) | Low risk | All stated outcomes reported. |
| Other bias | Low risk | Recruitment bias: unclear (not known if children shift clinics in the light of the intervention) Baseline imbalance: characteristics similar (low risk) Loss of clusters: no loss reported (low risk) Incorrect analysis: cluster adjusted (low risk) Comparability with RCTs randomizing individuals: low |
Awasthi 2013 (Cluster).
| Methods | Cluster‐RCT Method to adjust for clustering: cluster used as unit of analysis ('means of block‐specific numbers of deaths per AWC') Cluster unit: a block of 10,000 to 20,000 children Average cluster size: 9259 approximately (under‐5 population 1 million/108 clusters). ICCs: not reported Length of follow‐up: 5 years |
|
| Participants | All children living in endemic area Number analysed for primary outcome: total population of 1 million children at any one time, with a total of 2 million children ever in the trial Age range: 1 to 6 years Inclusion criteria: all preschool children then aged 1 to 6.0 years in 72 participating blocks near Lucknow that were considered to have a well‐functioning ICDS system with willing district and block directors and with paid workers in most of the block's Anganwadi centres Exclusion criteria: severe anaemia (haemoglobin < 75 g/L) |
|
| Interventions | Multiple doses vs placebo Factorial design in four arms
|
|
| Outcomes |
Not included in review: a subset of 5165 children were assessed for other outcomes (height, weight, BMI, haemoglobin, prevalence of illness in past 4 weeks) |
|
| Notes | Location: Lucknow, India Burden: low Annually about 30 non‐randomly selected preschool children were surveyed for growth, nutritional and morbidity outcomes from one randomly selected AWC per block (10,000 to 20,000 children in about 120 AWCs per block). Source of funding: UK Medical Research Council, USAID OMNI project, World Bank. Albendazole (Zentel) was donated by SmithKlineBeecham. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomly allocated"; "Randomisation (in Oxford) was stratified in groups of 4 neighbouring blocks, where possible in the same district." |
| Allocation concealment (selection bias) | Unclear risk | See above. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Open‐label trial but objective outcome (all cause mortality) so lack of blinding unlikely to affect the outcome. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 89 AWCs (2%) in the albendazole block lost to follow‐up, 86 AWCs (2%) in the placebo block lost to follow‐up. "Loss to follow‐up is defined by having only 1‐6 follow‐up visits (mean only 3, as against 12 in the included AWCs), and was generally because the AWC had ceased to function." Inclusion of all participants who were randomized within clusters (number evaluable/number randomized): Denominator for mortality was all children. A subset of 5165 non‐randomly selected children were assessed for other outcomes. |
| Selective reporting (reporting bias) | Low risk | Mortality is the single outcome for this trial. |
| Other bias | Low risk | Recruitment bias: unclear Baseline imbalance: unclear Loss of clusters: unclear Incorrect analysis: cluster adjusted (low risk) Comparability with RCTs randomizing individuals: unclear |
Beach 1999.
| Methods | RCT Length of follow‐up: 4 months |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 853 Age range/ mean age: 5 to 11 years Inclusion criteria: all children attending 5 schools (grades 1 to 4) Exclusion criteria: haematocrit < 22% |
|
| Interventions | Single dose vs placebo
|
|
| Outcomes |
|
|
| Notes | Location: Haiti Burden: intermediate Results presented in a stratified analysis as per individual infection: disaggregated results not presented; measures of error not given in tables. Source of funding: USAID. Invermectin provided by Philippe Gaxotte (Merck, Inc.) and albendazole by John Horton (SmithKline Beecham). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table. |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants, provider, and assessors were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 29/229 were lost to follow‐up in the placebo group and 25/244 were lost to follow‐up in the albendazole group. Inclusion of all randomized participants (number evaluable/number randomized): 88.4% (853/965). |
| Selective reporting (reporting bias) | Low risk | All stated outcomes reported. |
| Other bias | Low risk | No other obvious source of bias. |
Donnen 1998.
| Methods | RCT Length of follow‐up: 1 year |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 222 Age range: 0 to 72 months Inclusion criteria: children aged 0 to 72 months eligible on discharge from hospital where primary cause for admission is malnutrition Exclusion criteria: none stated |
|
| Interventions | Multiple doses vs placebo and no treatment
|
|
| Outcomes |
Not included in review: vitamin A levels; z‐scores for height‐for‐age, weight‐for‐age, weight‐for‐height (NCHS reference); egg counts (eggs/g: Kato Katz method). |
|
| Notes | Location: Zaire Burden: low Unadjusted data not provided in original paper; results of multiple‐regression models presented on basis of stratifications into vitamin A status and sex; results in meta‐analysis from R Dickson's correspondence with author when preparing the Dickson 2000a Cochrane Review. Source of funding: Fonds de la Recherche Scientifique et Medicale (FRSM), contract 3.4505.94 and the David and Alice Van Buuren Foundation. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomized". No further details reported. |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No details reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Overall, 6% of children were lost to follow‐up, with approximately equal proportions from each group. During the follow‐up period, 25 children died. The final sample included 311 children Inclusion of all randomized participants (number evaluable/number randomized): 86% (311/358). |
| Selective reporting (reporting bias) | Low risk | All stated outcomes reported. |
| Other bias | Low risk | No other obvious source of bias. |
Dossa 2001.
| Methods | RCT Length of follow‐up: 10 months |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 65 Age range: 3 to 5 years Inclusion criteria: children aged 3 to 5 years; not acutely unwell Exclusion criteria: none stated |
|
| Interventions | Multiple doses vs placebo
|
|
| Outcomes |
Not included in review: weight‐for‐height z‐score and height‐for‐age z‐score at 3 and 10 months (both after 2 doses). Measured but not reported: z‐scores for weight‐for‐height, height for age using NCHS reference data; egg count (arithmetic and geometric mean); prevalence, intensity; food intake over 3 days in subset at end of trial (not at baseline). |
|
| Notes | Location: Benin Burden: intermediate Source of funding: The Nestle Foundation (Lausanne, Switzerland).Smithkline Beecham provided the deworming and placebo tablets. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Randomly assigned". No further details provided. |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Quote: "Double‐blind". No further details provided. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 175/177 children finished the trial, but 140 were included in the final analysis: Quote: “One child was treated for severe worm infection and 34 children received other pills during the trial period (iron, vitamins/minerals or deworming pills that were not provided by our research team).” Inclusion of all randomized participants (number evaluable/number randomized): 79% (140/177). |
| Selective reporting (reporting bias) | Low risk | All stated outcomes reported. |
| Other bias | Low risk | No obvious other source of bias. |
Fox 2005.
| Methods | RCT Length of follow‐up: 6 months |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 626 Age range: 5 to 11 years Inclusion criteria: children aged 5 to 11 years attending any of 12 primary schools in Haiti where no other deworming activity was taking place Exclusion criteria: none stated |
|
| Interventions | Single dose vs placebo
|
|
| Outcomes |
Not included in review: worm intensity and prevalence; microfilarial density. |
|
| Notes | Location: Haiti Burden: intermediate Weight and height outcomes are only presented for a subgroup of children infected with Trichuris Source of funding: Emerging Infections Program of the Centers for Disease Control and Prevention (CDC) and an Institutional Strengthening Grant from the WHO to the Hopital Sainte Croix. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random‐number table. |
| Allocation concealment (selection bias) | Low risk | Centrally‐coded allocation system broken after baseline measures taken. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: "Double‐blind". Laboratory personnel, measurement teams and personnel evaluating students for adverse reactions were all blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 626/646 participants analysed for the primary outcome. Reasons for loss to follow‐up unclear. Inclusion of all randomized participants (number evaluable/number randomized): 97% (626/646). |
| Selective reporting (reporting bias) | Low risk | All stated outcomes reported. |
| Other bias | Low risk | No obvious other source of bias. |
Freij 1979a (Screened).
| Methods | Quasi‐RCT Length of follow‐up: 28 days |
|
| Participants | Infected children identified by screening Number analysed for primary outcome: 13 Age range: 1.5 to 5 years Inclusion criteria: boys attending mother and child clinic with Ascaris on stool smear; aged 1.5 to 5 years with no history of diarrhoea for preceding 2 weeks; no fever; no respiratory symptoms; no signs of severe disease Exclusion criteria: children diagnosed with other parasites; excluded girls to eliminate the contamination of samples with urine |
|
| Interventions | Single dose vs placebo
|
|
| Outcomes |
Not included in review: Ascaris worm count |
|
| Notes | Location: Ethiopia Burden: high The trial authors mention that boys were matched in pairs so that if there were dropouts they could be replaced. They do not indicate if there were any dropouts. SDs calculated from individual data. Freij 1979a (Screened) and Freij 1979b (Screened) were reported in the same article. Source of funding: Semper Nutrition Fund, Stockholm; Swedish Medical Research Council. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quasi‐RCT: boys matched into pairs of equal age and nutritional status. |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Described as double‐blind, no further details reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 100% (13/13) of enrolled participants were evaluated. The authors mention that boys were matched in pairs so that if there were dropouts they could be replaced. They do not indicate if there were any dropouts. Inclusion of all randomized participants (number evaluable/number randomized): 100% (13/13). |
| Selective reporting (reporting bias) | Low risk | Authors had intended to measure bicep and tricep skinfolds, but staff were unable to take these measurements. |
| Other bias | Low risk | No obvious other source of bias. |
Freij 1979b (Screened).
| Methods | Quasi‐RCT Length of follow‐up: 34 days |
|
| Participants | Infected children identified by screening Number analysed for primary outcome: 44 Age range: 1 to 5 years Inclusion criteria: 92 children 1 to 5 years from a community morbidity trial Exclusion criteria: none stated |
|
| Interventions | Single dose vs placebo
|
|
| Outcomes |
Not included in review: weight in % of Harvard standard; authors had intended to measure bicep and tricep skinfolds, but staff were unable to take these measurements |
|
| Notes | Location: Ethiopia Burden: high Freij 1979a (Screened) and Freij 1979b (Screened) were reported in the same article. Source of funding: Semper Nutrition Fund, Stockholm; Swedish Medical Research Council. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quasi‐RCT: children matched into pairs of equal age and nutritional status. |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Described as double‐blind, no further details reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 100% (44/44) of enrolled participants were evaluated. Inclusion of all randomized participants (number evaluable/number randomized): 100% (44/44). |
| Selective reporting (reporting bias) | Low risk | Trial authors had intended to measure bicep and tricep skinfolds, but staff were unable to take these measurements. |
| Other bias | Low risk | No obvious other source of bias. |
Garg 2002.
| Methods | RCT Length of follow‐up: 6 months |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 347 Age range: 2 to 4 years Inclusion criteria: sick children 2 to 4 years old presenting to 3 government health centres in Bungamo district, without palmar pallor Exclusion criteria: children with palmar pallor |
|
| Interventions | Single dose vs placebo
|
|
| Outcomes |
Not included in review: z‐scores for weight‐for‐age, height‐for‐age, and weight‐for‐height; egg count (formol‐ethyl acetate concentration method) in categories of intensity. |
|
| Notes | Location: Kenya Burden: low Source of funding: the CDC, Atlanta, USA. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list of random numbers. |
| Allocation concealment (selection bias) | Low risk | Drugs kept in envelope until after baseline assessment. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Quote: "the trial was not double‐blinded". Assessors were blinded; participants unclear; provider not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 93% (347/370) of randomized participants were evaluated, loss to follow‐up balanced across groups. Inclusion of all randomized participants (number evaluable/number randomized): 93% (347/370). |
| Selective reporting (reporting bias) | Low risk | All stated outcomes included. |
| Other bias | Low risk | No obvious other source of bias. |
Gateff 1972.
| Methods | Study design: RCT Length of follow‐up: 8 months |
|
| Participants | All children living in endemic area Number of analysed for primary outcome: 280 Age range: 6 to 15 years Inclusion criteria: children of one school Exclusion criteria: children who differed too much in weight so that they could not be paired |
|
| Interventions | Multiple dose vs placebo
Treatment strategy: three times one dose every 3 months |
|
| Outcomes |
|
|
| Notes | Location: Cameroon Burden: high Source of funding: Merk Sharpe and Dohme laboratories provided the medications |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Children were weighed at the beginning of the study and paired by weight. In each pair, 1 participant would by lottery [tirage au sort] receive medication A and the other medication B. Method of randomisation not reported. |
| Allocation concealment (selection bias) | Unclear risk | No information reported. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | The antihelmInthic treatment was administered using the double‐blind method. The dosage was identical 1 tablet per 10kg of weight in one taking for both medication and placebo. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 280/392 (71.4%) of randomized participants were evaluated. Missing participants (88 children at the first measurement; another 14 at the second, and another 10 at the third) not very clear: Quote: “the missing subjects were missing because of reasons independent of the measurements”. |
| Selective reporting (reporting bias) | Low risk | All stated outcomes reported. |
| Other bias | Low risk | No obvious other source of bias. |
Goto 2009.
| Methods | RCT Length of follow‐up: 36 weeks |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 134 Age range: 0 to 11 months Inclusion criteria: infants under 11 months of age in the local area Exclusion criteria: not stated |
|
| Interventions | Multiple doses vs placebo
Secnidazole: a 70 mg/mL suspension with about 0.5 g of sweetener was made up, and 0.5 mL per kg body weight was given by spoon. If the infant was sick immediately, secnidazole was re‐administrated. Albendazole: a 200 mg (5 mL) suspension given by spoon. |
|
| Outcomes |
Not included in review
|
|
| Notes | Location: Dhamrai Upazila, located 40 km northwest of Dhaka, Bangladesh. Burden: low Drug source: Dhaka, Bangladesh (Essential Drugs Company Ltd for secnidazole; Square Pharmaceuticals Ltd for the secnidazole placebo; Opsonin Chemical Industries Ltd for albendazole; and UniMed and UniHealthManufacturing Ltd for albendazole placebo). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated. Randomized on the basis of their age, sex, height‐for‐age, weight‐for‐age and weight‐for‐height z‐scores, socio‐demographic and economic data and presence of any parasitic infection. |
| Allocation concealment (selection bias) | Unclear risk | Unclear whether the allocation was concealed since patients were randomized by their characteristics. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind. Quote: "Bottles containing the two medications and placebo suspensions were labelled with different colours corresponding to the three intervention groups, but the assistants did not know the relationship between the colour codings and the contents of the bottles." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 134/283 (47.35%) of randomized participants were evaluated. 14 infants were excluded from the trial, as they had either moved away from the trial area (n = 11), or were absent during the trial period (n = 2) or the parents subsequently refused to participate (n = 1). Of the infants who completed the trial (n = 394), data on 64 infants were incomplete (.i.e. they did not provide information for all the 10 z‐scores and four intestinal permeabilities, serological variables and prevalences of parasite infections), and severe anaemic infants were also omitted from the trial. Inclusion of all randomized participants (number evaluable/number randomized): 47% (134/283). |
| Selective reporting (reporting bias) | Low risk | All stated outcomes reported. |
| Other bias | Low risk | No obvious other source of bias. |
Greenberg 1981.
| Methods | RCT Length of follow‐up: 11 months |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 152 aged 1.5 to 8 years Age range: 1.5 to 8 years Inclusion criteria: children aged 1.5 to 8 years living in Nandipara, Bangladesh; 50% entered into trial; only those who provided stool sample and had anthropometric measurements taken at first visit entered Exclusion criteria: none stated |
|
| Interventions | Single dose vs placebo
|
|
| Outcomes |
|
|
| Notes | Location: Bangladesh Burden: high Groups stratified by intensity of Ascaris infection Source of funding not reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Randomly assigned", no further details provided. |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Quote: "Double‐blind". Participants blinded both placebo and treatment given as a flavoured syrup, no information about provider and assessor blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 82% (152/185) of randomized participants were evaluated. Reasons for leaving the trial early not reported. Inclusion of all randomized participants (number evaluable/number randomized): 82% (152/185). |
| Selective reporting (reporting bias) | High risk | Not all stated outcomes reported. |
| Other bias | Low risk | No obvious other source of bias. |
Gupta 1982.
| Methods | RCT Length of follow‐up: 12 months. | |
| Participants | All children living in an endemic area. Number analysed for primary outcome: 159. Age range: 2‐5 years Inclusion criteria: all children aged 24 to 61 months. Exclusion criteria: only had one parent or no parent alive. |
|
| Interventions | Multiple dose vs placebo
Interventions delivered every two months for one year |
|
| Outcomes |
Not included in the review: parasitology, four monthly stool examination for helminths and protozoa. |
|
| Notes | Location: Guatemala. Burden: intermediate. Source of funding: Metrondizole syrup was provided by the McKesson Laboratories (Central America divisions). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomisation not specified. |
| Allocation concealment (selection bias) | Unclear risk | Details of allocation concealment were not reported. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Placebo resembled piperazine in taste and appearance. Does not report whether participants and personnel were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 100% of randomized participants were evaluated. |
| Selective reporting (reporting bias) | Low risk | All stated outcomes reported. |
| Other bias | Low risk | No obvious other source of bias. |
Hadju 1996.
| Methods | Quasi‐RCT Length of follow‐up: 1.75 months (7 weeks) |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 64 Age range: 6 to 10 years Inclusion criteria: boys aged 6 to 10 years attending second grade at 3 primary schools; completed assessment and provided a stool sample; randomized by descending hookworm count (all treated) Exclusion criteria: none stated |
|
| Interventions | Single dose vs placebo
|
|
| Outcomes |
Not included in review: egg counts arithmetic and geometric means (Kato‐Katz); weight‐for‐age (NCHS reference) |
|
| Notes | Location: Indonesia Burden: high Large drops in geometric mean egg counts in placebo noted Source of funding not reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomized: Quote: "Randomly assigned" by descending A. lubricoides egg count" |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Quote: "Double‐blind". Participants blinded both placebo and treatment identical round white tablets, no information about provider and assessor blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 85% (64/75) of randomized participants were evaluated. Reasons for loss to follow‐up included: moved away, refused to be examined, did not return a stool sample, absent during examination. Not clear how many lost from each treatment group. Inclusion of all randomized participants (number evaluable/number randomized): 85% (64/75). |
| Selective reporting (reporting bias) | Low risk | All stated outcomes reported. |
| Other bias | Low risk | No obvious other source of bias. |
Hadju 1997.
| Methods | RCT Length of follow‐up: 12 months |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 330; mean age 8.3 years Inclusion criteria: all primary school children in grades 1, 2, and 3 in 2 schools in slum areas in Indonesia; randomized according to Ascaris egg count and age Exclusion criteria: children > 11; signs of puberty; signs of severe protein energy malnutrition |
|
| Interventions | Multiple doses vs placebo
|
|
| Outcomes |
Results of multivariate analysis using z‐scores presented and could not be used in meta‐analysis; unadjusted results not reported |
|
| Notes | Location: Indonesia Burden: high Placebo group showed an unexplained drop in egg counts at the 3‐month examination Source of funding: Directorate of Higher Education, Department of Education and Culture, Government of Indonesia through Hibah Bersaing Project I & II. Albendazole and placebo provided by Smithkline Beecham Pharmaceuticals Indonesia. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned quote: "by sex and egg count". |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No details reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 65% (330/507) of randomized participants were evaluated, number lost from each treatment group not reported. Inclusion of all randomized participants (number evaluable/number randomized): 65% (330/507). |
| Selective reporting (reporting bias) | Low risk | All stated outcomes reported. |
| Other bias | Low risk | No obvious other source of bias. |
Hall 2006 (Cluster).
| Methods | Cluster‐RCT Method to adjust for clustering: not adjusted (review authors adjusted using the ICC from Alderman 2006) Cluster unit: school Average cluster size: 33 ICCs: not reported Length of follow‐up: 2 years |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 80 schools randomized containing 2659 children in class 3 Mean age: 104.5 months Inclusion criteria: children from class 3 and born in 1990 of 80/81 schools in the Red River delta of north Vietnam Exclusion criteria: none stated |
|
| Interventions | Multiple doses vs placebo
|
|
| Outcomes | Measured
|
|
| Notes | Location: Vietnam Burden: high It is unclear what is meant by quote: "randomization was adjusted so that there were equal numbers of schools in each district of the trial group". It is also appears as if the analysis has not taken into account the effects of cluster randomization. Source of funding not reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: quote: "randomization was adjusted so that there were equal numbers of schools in each district of the trial group" (unclear what this means) |
| Allocation concealment (selection bias) | Low risk | Central allocation. Quote: "...using a list provided by the Ministry of Education". |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Placebo was used, blinding not reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient reporting of attrition/exclusions. 80 schools containing 56,444 pupils randomized, and those from class 3 used in trial. Inclusion of all participants who were randomized within clusters (number evaluable/number randomized): unclear; 80 schools containing 56,444 pupils randomized, and those from class 3 used in trial. |
| Selective reporting (reporting bias) | Low risk | All stated outcomes reported. |
| Other bias | Low risk | Although not adjusted for clustering, we used estimates to adjust in the review. Recruitment bias: low (schools) Baseline imbalance: low (characteristics similar) Loss of clusters: low (no loss reported) Incorrect analysis: not cluster adjusted (high risk) Comparability with RCTs randomizing individuals: unclear |
Joseph 2015.
| Methods | RCT Length of follow‐up: 12 months | |
| Participants | All children living in an endemic area Number analysed for primary outcome: 1760 children Age range/mean: 12.5 months Inclusion criteria: 1) children attending any one of the 12 participating health centres for their 12‐month CRED visit; and 2) children living in Belén, Iquitos, Punchana or San Juan districts. Exclusion criteria: 1) children attending the health centre for suspected STH infection; 2) children who had received deworming treatment in the six months prior to the trial; 3) children whose families planned to move outside of the study area within the next 12 months; 4) children under 12 months of age or 14 months of age or older; and 5) children with any serious congenital or chronic medical condition. | |
| Interventions | Single dose and multi‐dose vs placebo
|
|
| Outcomes |
Not included in review: changes in STH infection prevalence and intensity |
|
| Notes | Location: Iquitos, Peruvian Amazon Burden: low |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “Computer‐generated randomly ordered blocks of eight and twelve were used to randomly assign children to each intervention group in a 1:1:1:1 allocation ratio” |
| Allocation concealment (selection bias) | Unclear risk | Quote: “Research personnel not directly involved in the trial prepared small envelopes containing the randomly assigned intervention for each visit.” |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: “The placebo was identical to the deworming tablet in terms of size, colour and markings” Quote: “All health centre and research personnel, and parents of participants were blinded to intervention status.” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 388/440 children in the mebendazole/placebo group,
398/440 in the placebo/mebendazole group, 381/440 in the mebendazole/mebendazole and 396/440 in the placebo/placebo group were lost to follow‐up. Inclusion of all randomized participants (number evaluable/number randomized): 93% (1563/1760). |
| Selective reporting (reporting bias) | Low risk | All stated outcomes reported. |
| Other bias | Low risk | No obvious other sources of bias. |
Kirwan 2010.
| Methods | RCT Length of follow‐up: 14 months |
|
| Participants | All children living in endemic area
Number analysed for primary outcome: 320 Age range: 12 to 59 months Inclusion criteria: pre‐school children aged 12 to 59 months, either sex Exclusion criteria: severe anaemia < 5 g/dL, severe malaria |
|
| Interventions | Multiple doses vs placebo
Treatment strategy: 200 mg (one tablet) albendazole was given to children aged 1 year, 400 mg (two tablets) albendazole was given to children aged 2, 3, and 4 years. Children who were in the placebo group were given one or two (1 year) placebo (2 to 4 years) tablets. Treatment or placebo was given at baseline, 4, 8, and 12 months and then followed up for the last time at 14 months. Children in the placebo group were treated with albendazole at 14 months. |
|
| Outcomes |
Unable to use: nutritional status and anthropometric measures, at baseline and 14 months, no data were reported for these outcomes. Not included in review: infection with STHs, measured at baseline and 4, 8, 12, and 14 months (eggs or worms in stool sample). Incidence of malaria and malaria attacks, measured at baseline and 4, 8, 12, and 14 months. Adverse events not fully reported for albendazole treatment vs placebo. |
|
| Notes | Location: 4 semi‐urban villages, Osun State, Nigeria Burden: intermediate No adverse events reported in the albendazole treatment group. Not reported for control group. Source of funding: Health Research Board (HRB) (Ireland). GlaxoSmithKline sponsored the drug albendazole which was used in the trial. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quasi‐randomized, Quote: "During the first assessment each alternate child was assigned tablet B". |
| Allocation concealment (selection bias) | High risk | Alternation, one of the investigators quote: "placed the albendazole and placebo tablets in containers labelled either A or B" later "The treatment coordinator [...] oversaw the allocation of treatments to the children". |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants and key personnel were blinded. Quote: "Experienced physicians […] enrolled all participants, measured all trial endpoints, and were kept masked to treatment allocation of children. Field workers involved in data collection and mothers of participating children were also masked to the treatment allocation." Quote: "Albendazole and placebo tablets were identical". |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 320 children (out of 1228, 26.1%) complied with all the follow‐up assessments and were included in the analyses. Inclusion of all randomized participants (number evaluable/number randomized): 26% (320/1228). |
| Selective reporting (reporting bias) | High risk | Nutritional status and anthropometric measures not reported. Main paper states these outcomes are reported in the companion paper; no data reported for these outcomes in the companion paper. |
| Other bias | Low risk | No obvious other source of bias. |
Kloetzel 1982.
| Methods | RCT Length of follow‐up: 10 months |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 337; unclear how many randomized Age range: 1 to 8 years old Inclusion criteria: enlisted from 9 rural communities in Pariquera‐Acu state of Sao Paulo Exclusion criteria: none stated |
|
| Interventions | Single dose vs placebo
|
|
| Outcomes |
|
|
| Notes | Location: Cameroon Burden: high Results reported as changes in nutritional status grouped into 3 categories: improved, deteriorated, no change (unclear on basis of which parameter), and proportions compared Source of funding: Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Randomized", no further details provided. |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Described as double‐blind, no details reported. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No details about losses to follow‐up reported; quote: "the present report only deals with those 337 that could be followed throughout the entire 10 months". Inclusion of all randomized participants (number evaluable/number randomized): unclear (337 analysed). |
| Selective reporting (reporting bias) | Low risk | All stated outcomes reported. |
| Other bias | Low risk | No obvious other sources of bias. |
Koroma 1996.
| Methods | RCT Length of follow‐up: 6 months |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 187 Age range: 6 to 10 years Inclusion criteria: selected (unclear how) urban and rural school primary children aged 6 to 10 years Exclusion criteria: not stated |
|
| Interventions | Single dose vs placebo
|
|
| Outcomes |
|
|
| Notes | Location: Sierra Leone Burden: intermediate Source of funding: Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Randomized", no further details provided. |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No details reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 76% (187/247) of randomized participants were evaluated. Reasons for loss to follow‐up not reported. Inclusion of all randomized participants (number evaluable/number randomized): 76% (187/247). |
| Selective reporting (reporting bias) | Low risk | All stated outcomes reported. |
| Other bias | Low risk | No obvious other sources of bias. |
Kruger 1996.
| Methods | RCT Length of follow‐up: 11 months |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 74 Age range: 6 to 8 years Inclusion criteria: 65 pupils in first year of school randomly selected from each of 5 primary schools; schools included in a feeding scheme Exclusion criteria: age > 9 years; current use of iron supplements; inclusion in an iron fortification trial; infection (raised white cell count) |
|
| Interventions | Multiple doses vs placebo
Also: whole population 3/5 schools also allocated soup fortified with 20 mg elemental iron per day, and 100 mg vitamin C for 6 months; unclear whether this intervention was cluster randomized. All schools taking part in feeding programme providing bread, soup, and peanut butter to all pupils. |
|
| Outcomes |
Not included in review: other iron indices; stool egg counts (Visser filter method); z‐scores for weight‐for‐age, height for age, and weight‐for‐height. |
|
| Notes | Location: South Africa Burden: intermediate Data were combined for all treatment groups. Data stratified by baseline iron stores into 2 groups that were combined for meta‐analysis. Source of funding: Fortified and unfortified soup provided by Funa Foods, Zentel and placebo provided by SmithKline Beecham Pharmaceuticals (Pty) Ltd. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Randomly assigned", no further details provided. |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No details reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 72% (179/247) of randomized participants were evaluated. Reasons for loss to follow‐up not reported. Inclusion of all randomized participants (number evaluable/number randomized): 72% (179/247). |
| Selective reporting (reporting bias) | Low risk | All stated outcomes reported. |
| Other bias | Low risk | No obvious other source of bias. |
Kvalsvig 1991a (Screened).
| Methods | RCT Length of follow‐up: 1 month |
|
| Participants | Infected children identified by screening Number analysed for primary outcome: unclear Age range: unclear Inclusion criteria: most severely infected 100 children in a primary school Exclusion criteria: children with schistosomiasis |
|
| Interventions | Single dose vs placebo
|
|
| Outcomes |
Not included in review: height; weight at baseline; standardized using NCHS standards; stool examination (intensity index designed for this trial); no nutritional outcomes reported that can be used in the review |
|
| Notes | Location: South Africa Burden: high No data used in meta‐analysis since SDs not provided. Source of funding: Janssen Pharmaceutica, South African Medical Research Council. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Assigned randomly", no further details provided. |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Quote: "A 'blind' procedure was adopted; the research assistant did not know whether a particular child had received drug or placebo". No further details provided. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No details reported. Inclusion of all randomized participants (number evaluable/number randomized): unclear. |
| Selective reporting (reporting bias) | Low risk | All stated outcomes reported. |
| Other bias | Low risk | No obvious other source of bias. |
Lai 1995.
| Methods | Quasi‐RCT Length of follow‐up: 2 years |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 314 Mean age: 8 years Inclusion criteria: school children aged 8 who provided a stool sample Exclusion criteria: concurrent illness; antIhelminth treatment in previous 3 months |
|
| Interventions | Multiple doses vs placebo
|
|
| Outcomes | Measured
|
|
| Notes | Location: Malaysia Burden: high No data used in meta‐analysis since SDs not provided Source of funding not reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quasi‐randomized: block assignment design by school, then by sex, then by presence of worms as none, light, or moderate/heavy, and then by rank order of body weight in the group; used odd and even numbers; in urban area the odd numbered children were assigned to treatment; in the peri‐urban area the even numbered children were assigned to the treatment group. |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants were blinded; trial staff not blinded to group assignment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 89% (314/353) of randomized participants were evaluated. Inclusion of all randomized participants (number evaluable/number randomized): 89% (314/353). |
| Selective reporting (reporting bias) | Low risk | All stated outcomes reported. |
| Other bias | Low risk | No obvious other sources of bias. |
Le Huong 2007.
| Methods | RCT Length of follow‐up: 6 months |
|
| Participants | All children living in endemic area (children screened for anaemia then randomized and all children treated) Number analysed for primary outcome: 510 randomized Mean age: ˜7.3 years Inclusion criteria: children in Grades 1 to 3 with haemoglobin < 110 g/L but not < 70 g/L Exclusion criteria: haemoglobin concentrations < 70 g/L |
|
| Interventions | Multiple dose vs placebo Factorial design Mebendazole 500 mg at 0 and 3 months
|
|
| Outcomes |
Not included in review: Ferritin; serum transferrin; worm prevalence; C‐reactive protein (CRP). |
|
| Notes | Location: Vietnam Burden: high Source of funding: Neys‐van Hoogstraten Foundation, Ellison Medical Foundation and the Ministry of Education and Training, Vietnam. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomized, no further details. |
| Allocation concealment (selection bias) | Low risk | Central allocation. Quote: "Randomization was carried out by a researcher [...] who did not know the children and could not introduce bias in the randomization". |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants and key personnel blinded. Quote: "Children, teachers and researchers were blinded to the treatment". Placebo identical to intervention drug. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 409/425 participants were evaluated. Reason for dropout: refusal (n = 16, intervention: 4.7%, placebo: 2.3%). Inclusion of all randomized participants (number evaluable/number randomized): 96% (409/425). |
| Selective reporting (reporting bias) | Low risk | Pre‐specfied outcomes reported. |
| Other bias | Low risk | No obvious other sources of bias. |
Liu 2017 (Cluster).
| Methods | Cluster‐RCT Method to adjust for clustering: multivariate analyses taking into account paired fixed effects and clustering at the township level Cluster unit: township Average cluster size: 20 ICCs: not reported Length of follow‐up: 6 months | |
| Participants | All children living in an endemic area Age range: 9 to 11 years Number analysed for primary outcome: 112 townships randomised containing 2,240 children from 146 villages Inclusion criteria: children 9 to 11 years of age attending any primary schools within the township for the 2013 to 2014 school year. Exclusion criteria: townships and villages that housed the local township government, since these are typically wealthier and more urbanized | |
| Interventions | Multi‐dose vs no treatment
|
|
| Outcomes |
Not included in review: STH infection prevalence, treatment compliance rates. |
|
| Notes | Location: 7 rural counties in Qiandongnan Prefecture in Guizhou Province, China Burden: intermediate Weight and height data were provided by the authors of the recent Campbell review (Welch 2016). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “All randomized selection and allocation was performed using a computerized random sequence generator.” Quote: “used baseline survey information to assign the sample townships in each county into two pairs, using an optimal matching algorithm.” |
| Allocation concealment (selection bias) | Unclear risk | Quote: “All randomized selection and allocation was performed using a computerized random sequence generator.” |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Quote: “Students in the intervention group, as well as their parents or teachers, were not told explicitly that the purpose of the study was to examine the effect of a trial intervention.” Quote: “Participants in the control group were not aware that they were in a randomized trial.” Quote: “Trained enumerators and local health practitioners who assisted with baseline and follow‐up surveys were not explicitly informed of the treatment assignment of participants.” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 84/1084 children in the albendazole group and 67/1095 in the no treatment group were lost to follow‐up. Inclusion of all participants who were randomized within clusters (number evaluable/number randomized): 93% (2028/2179). |
| Selective reporting (reporting bias) | Low risk | All stated outcomes reported. |
| Other bias | Low risk | Recruitment bias: low (schools) Baseline imbalance: low (characteristics similar) Loss of clusters: low (none reported) Incorrect analysis: cluster adjusted (low risk) Comparability with RCTs randomizing individuals: unclear |
Michaelsen 1985.
| Methods | RCT Length of follow‐up: 5 months |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 121 for nutritional outcomes Age range: 5 to 14 years Inclusion criteria: children from a school identified as having high prevalence of hookworm on the basis of a previous survey Exclusion criteria: children with height above 137 cm girls and 145 cm for boys since these were the upper limits in the reference ranges |
|
| Interventions | Single dose vs placebo
|
|
| Outcomes | Measured
Reported
|
|
| Notes | Location: Botswana Burden: high Source of funding not reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Random sample of half the children" were give the treatment and the remaining the placebo; no further details reported. |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No details reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 53% (121/228) of randomized participants were evaluated. Inclusion of all randomized participants (number evaluable/number randomized): 53% (121/228). |
| Selective reporting (reporting bias) | Low risk | Pre‐specfied outcomes reported. |
| Other bias | Low risk | No obvious other sources of bias. |
Miguel 2004 (Cluster).
| Methods | Cluster quasi‐randomized stepped‐wedge trial Method to adjust for clustering: CIs adjusted for clustering in regression modelling, robust standard errors presented (confirmed in correspondence with authors) Cluster unit: schools Average cluster size: 400 ICCs: not reported Length of follow‐up: one year for phased quasi‐randomized comparisons for health outcomes. Two years for school attendance |
|
| Participants | All children living in endemic area Number analysed for primary outcomes: 75 primary schools randomized containing 778 children analysed for haemoglobin. 9102 children analysed for weight and height, 32% and 34% of eligible population analysed for exam performance and cognitive tests, and 100% of eligible population analysed for school attendance Age range/mean age: school children 12 years or under Inclusion criteria: children from 75 primary schools in the trial area Exclusion criteria: girls > 13 years old |
|
| Interventions | Deworming package of interventions vs no treatment
|
|
| Outcomes |
Not included in review: worm prevalence and intensity, self‐reported sickness, worm prevention behaviours: proportion "clean" as per health worker observation, proportion wearing shoes as per health worker observation, self‐reported contact with fresh‐water in past week, access to home latrine, malaria/fever. |
|
| Notes | Location: Kenya Burden: high Source of funding: Sponsored by the World Bank and the Partnership for Child Development. This study has been the subject of an independent re‐analysis, with a full report published on the 3ie website (Aiken 2014), which also includes a response from the authors (New Reference); and two subsequent academic papers (Aiken 2015; Davey 2015). In this edition of the Cochrane Review, we used new information on conduct of the trial, on the thorough evaluation for potential biases, and also corrected data from the replication, including the measure of variance for school attendance (Aiken 2014). Weight change was calculated from the study dataset following correspondence with the authors. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Schools in a deworming project were stratified by zone, their involvement with other NGO programmes, and then listed alphabetically and every third school assigned to start the programme in 1998, to start it in 1999, or to be a control. |
| Allocation concealment (selection bias) | High risk | Not concealed (see above). |
| Blinding (performance bias and detection bias) All outcomes | High risk | Pragmatic cluster implementation trial with no blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | For haemoglobin, weight and height the outcomes have been measured on a random sub‐sample of the quasi‐randomized population. For haemoglobin, a sample of around 4% (778/20,000) of the quasi‐randomised comparison of group 1 vs group 2 in 1998 was analysed. |
| Selective reporting (reporting bias) | Low risk | Outcome data not reported for cognitive tests, though authors state: Deworming treatment effects are not significantly different than zero for any component of the cognitive exam (results available on request). |
| Other bias | High risk | Recruitment bias: low (no asymmetric migration between schools) Baseline imbalance: low Loss of clusters: low (none reported) Incorrect analysis: low (correctly adjusted for clustering). Comparability with RCTs randomizing individuals: low Other sources of bias: high for confounding due to a co‐intervention. The drug intervention is accompanied by intensive health promotion that could account for some of the effects with key outcomes such as school attendance. |
Ndibazza 2012.
| Methods | RCT Length of follow‐up: 5 years |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 1423 Mean age: 15 months (randomized at 1.5 years) Inclusion criteria: 15 month old children whose mothers participated in the pregnancy phase of the trial (pregnant healthy women from the area, planning to deliver at Entebbe Hospital) Exclusion criteria: none stated |
|
| Interventions | Multiple dose vs placebo Factorial designa
aMothers when pregnant had been randomized in a 1:1:1:1 ratio to receive single‐dose albendazole (400 mg) + praziquantel (40 mcg/kg), albendazole + praziquantel placebo, albendazole placebo + praziquantel, or albendazole placebo + praziquantel placebo. |
|
| Outcomes |
Not included in review: immune response at age 5 years to BCG and tetanus immunisation, incidence of malaria, diarrhoea, pneumonia, measles, and tuberculosis, measures of fine motor function and gross motor function. |
|
| Notes | Location: Entebbe, Uganda Burden: low Source of funding: Wellcome Trust Weight, height and haemoglobin data were provided by the authors of the recent Campbell review (Welch 2016). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization code generated by statistician using Stata version 7. |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Participants and provider blinded. Not reported for assessors. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Inclusion of all randomized participants (number evaluable/number randomized): 71% (1423/2016) of randomized participants. |
| Selective reporting (reporting bias) | High risk | Serious adverse events not reported. |
| Other bias | Low risk | No other obvious source of bias. |
Nga 2009.
| Methods | RCT Length of follow‐up: 4 months |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 510 randomized Age range: 6 to 8 years Inclusion criteria: school children aged 6 to 8 years and written informed consent from parents/caregivers Exclusion criteria: haemoglobin concentrations < 80 g/L, chronic illness, congenital abnormalities, mental or severe physical handicap, severe malnutrition ([z‐scores for weight‐for‐height (WHZ) < ‐3.0 SD), obesity (BMI ≥ 25 or z‐scores for WHZ > +2 SD), or receiving deworming within the previous 6 months |
|
| Interventions | Single dose vs placebo
|
|
| Outcomes |
Not included in review: changes in zinc, iodine, and ferritin concentration; worm prevalence Measured but not reported: weight and height recorded at baseline and end point but only baseline data reported. Skin fold thickness recorded at baseline and end point, but no data reported. |
|
| Notes | Location: Vietnam Burden: intermediate This trial was supported by the Neys‐van Hoogstraten Foundation, the Netherlands, and the Ellison Medical Foundation. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated. Quote: "pupils were allocated to 1 of the 4 intervention groups based on a computer generated list, matched on age (12‐mo age groups) and sex, and using a block size of 8 by one of the researchers not involved in the field work". |
| Allocation concealment (selection bias) | Low risk | Central allocation. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants and key personnel were blinded. Quote: "All investigators, field assistants, teachers, and children did not know the codes of the trial groups". Placebo identical to treatment (orange chewable tablet). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 482/510 randomized participants were evaluated. Reasons for dropout: moved (n = 12), surgery (n = 2), refusal to participate (n = 14), balanced across intervention groups. Inclusion of all randomized participants (number evaluable/number randomized): 94.5% (482/510). |
| Selective reporting (reporting bias) | High risk | Three outcomes (weight, height and skin fold thickness) not reported adequately. |
| Other bias | Low risk | No obvious other source of bias. |
Nokes 1992 (Screened).
| Methods | RCT Length of follow‐up: 2.25 months (9 weeks) |
|
| Participants | Infected children identified by screening Number analysed for primary outcome: 103 Age range: 9 to 12 years Inclusion criteria: children from 3 schools in Mandeville; Trichuris egg counts > 1900, but low hookworm counts on 2 occasions before the trial separated by 3 months Exclusion criteria: twins; severe illness; physical handicaps; neurological disorders |
|
| Interventions | Single dose vs placebo
|
|
| Outcomes | Cognitive tests: digit span forwards/backwards; arithmetic and coding from Wechsler Intelligence Scale for Children; fluency and listening comprehension from the Clinical Evaluation of Language functions; and matching familiar figures test. Not included in review: stool egg counts at baseline and 10 days (prevalence and arithmetic mean); height and weight (expressed as % NCHS standard) iron status; school attendance; IQ; socioeconomic status; educational opportunity measures at baseline. Outcomes not reported: nutritional outcomes at 9 weeks cited as too short a follow‐up period to demonstrate a change;school attendance only measured at baseline. |
|
| Notes | Location: Jamaica Burden: high There was an infected placebo group and an quote: "uninfected control group" Source of funding not reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Randomly assigned"; no further details reported. |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No details reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 73% (103/140) of randomized participants were evaluated. Inclusion of all randomized participants (number evaluable/number randomized): 73% (103/140). |
| Selective reporting (reporting bias) | Unclear risk | Pyschometric tests reported; other outcomes such as nutrition not reported. |
| Other bias | Low risk | No obvious other source of bias. |
Olds 1999.
| Methods | RCT Length of follow‐up: 6 months for randomized comparison |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 1518 randomized, 90% followed up at 6 months Age range/mean age: 10.5 years Inclusion criteria: school age children Exclusion criteria: failure to submit 2 stool specimens prior to the initial treatment, known allergy to either drug, treatment with either drug within 6 months, lack of consent, and marriage or possible pregnancy |
|
| Interventions | Single dose vs placebo Albendazole (400 mg) plus praziquantel (40 mg/kg) Praziquantel plus an albendazole placebo Albendazole plus a praziquantel placebo Both placebos |
|
| Outcomes | No useable data. Not included in review: ultrasound, physical examination and history findings, duplicate stool and urine measurements of egg counts Measured but not reported: weight, height, skinfold thickness (subscapular, triceps, and abdominal) and haemoglobin recorded at baseline and end point but only baseline data reported; data for side effects not useable in review |
|
| Notes | Location: China, Philippines and Kenya Burden: intermediate randomized comparison up to 6 months at which point all infected children were treated as needed, and followed up until one year. There was no difference between the side effect rate from albendazole or the double placebo Result text: quote: "No statistically significant improvement was seen in haemoglobin after albendazole treatment. In the trial population as a whole, no significant differences between treatment groups were seen in any of the growth and anthropometric measurements." Source of funding: Tropical Disease Research (TDR) of the WHO. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated. Quote: "Randomization lists were prepared by WHO/TDR using a randomized block design with a block size of 80". |
| Allocation concealment (selection bias) | Low risk | Central allocation. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants, key personnel, and outcome assessment was blinded. Quote: "The randomization code was not broken until after the 6‐month results were tabulated and submitted to WHO". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1518 participants, 90% at 6 months follow‐up, 83% at one year, no further details. Inclusion of all randomized participants (number evaluable/number randomized): 90% (1366/1518). |
| Selective reporting (reporting bias) | High risk | Weight, height, skinfold thickness, and haemoglobin recorded at baseline and end point but only baseline data reported. |
| Other bias | Low risk | No obvious other source of bias. |
Ostwald 1984.
| Methods | RCT Length of follow‐up: 5 months |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 105 Age range/mean age: 7 to 10 years Inclusion criteria: Children in standards 1 and 3, the youngest classes, of the Community school at Lufa Station, Eastern Highlands Province, Papua New Guinea Exclusion criteria: none reported |
|
| Interventions | Multiple dose vs placebo
|
|
| Outcomes |
Not included in the review: weight/height, egg counts, hematologic and biochemical measurements (ferritin, transferrin, serum folate and serum ascorbate) |
|
| Notes | Location: Papua New Guinea Burden: high Source of funding: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "the children divided into control and treatment. Pairs with matching hookworm loads were randomised to either treatment or control by coin toss." |
| Allocation concealment (selection bias) | Unclear risk | No details reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No details reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 118 children enrolled into the study. Randomisation occurred after 7 months. Number randomised was not reported. Data from 87 were obtained at follow‐up. |
| Selective reporting (reporting bias) | Low risk | Pre‐specfied outcomes reported. |
| Other bias | Low risk | No obvious other source of bias. |
Palupi 1997.
| Methods | RCT Length of follow‐up: 9 weeks (2.25 months) |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 191 Age range: 2 to 5 years Inclusion criteria: children ages 2 to 5 years registered at village health centres Exclusion criteria: none stated |
|
| Interventions | Single dose vs placebo
|
|
| Outcomes |
Not included in review: z‐scores for height‐for‐age, weight‐for‐age, and weight‐for‐height (NCHS reference) |
|
| Notes | Location: Java, Indonesia Burden: intermediate Source of funding: Kimia Farma Indonesia. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The children were randomly divided into three, equal‐sized treatment groups". No further details reported. |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Described as double‐blind. Participants were blinded, unclear whether provider and assessor were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 97% (289/299) of enrolled participants were evaluated. Inclusion of all randomized participants (number evaluable/number randomized): 97% (289/299). |
| Selective reporting (reporting bias) | Low risk | Pre‐specfied outcomes reported. |
| Other bias | Low risk | No obvious other source of bias. |
Rousham 1994 (Cluster).
| Methods | Cluster‐RCT Method to adjust for clustering: not adjusted Cluster unit: village Average cluster size: 114 ICCs: not reported Length of follow‐up: 18 months |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 13 villages randomized containing 1402 children Age range: 2 to 6 years Inclusion criteria: children ages 2 to 6 years from 13 villages surrounding a mother and child health centre; subgroup living in 8 villages within waking distance of health centre analysed for additional outcomes Exclusion criteria: none stated |
|
| Interventions | Multiple doses vs placebo
|
|
| Outcomes |
|
|
| Notes | Location: Bangladesh Burden: intermediate No adjustment made for cluster randomization Source of funding: the Overseas Development Administration and the University of Cambridge Maintenance Fund. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The trial was described as randomized, no further details reported. |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants and field workers were blinded, unclear if assessment was blinded. Quote: "The treatment and placebo tablets were given in a double‐blind manner; neither the field workers nor the parents were aware of the group to which they belonged". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 94% (1402/1476) of enrolled participants were evaluated. Inclusion of all participants who were randomized within clusters (number evaluable/number randomized): 94% (1402/1476). |
| Selective reporting (reporting bias) | Low risk | Not all pre‐specified outcomes reported. |
| Other bias | Low risk | Recruitment bias: unclear (not known if children shift clinics in the light of the intervention) Baseline imbalance: low (no differences apparent) Loss of clusters: low (none reported) Incorrect analysis: not adjusted (high risk) Comparability with RCTs randomizing individuals: unclear |
Sarkar 2002 (Screened).
| Methods | RCT Length of follow‐up: 4 months (16 weeks) |
|
| Participants | Infected children identified by screening Number analysed for primary outcome: 81 Age range: 2 to 12 years Inclusion criteria: children ages 2 to 12 living in Mirpur slum infected with Ascaris Exclusion criteria: none stated |
|
| Interventions | Single dose vs placebo
|
|
| Outcomes |
Not included in review: median % weight‐for‐age, weight‐for‐height, and height‐for‐age |
|
| Notes | Location: Bangladesh Burden: high Source of funding: research grant from the World Bank and was funded by the Bangladesh National Nutrition Council. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Random table". |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: "Double‐blind"; "The syrups were identical in appearance and flavor and were packaged in identical containers. Randomized patient numbers were labeled on the bottles to maintain the double blind design". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 94% (81/85) of randomized participants were evaluated. Inclusion of all randomized participants (number evaluable/number randomized): 94% (81/85). |
| Selective reporting (reporting bias) | Low risk | Pre‐specfied outcomes reported. |
| Other bias | Low risk | No obvious other source of bias. |
Simeon 1995 (Screened).
| Methods | RCT Length of follow‐up: 6.5 months (26 weeks) |
|
| Participants | Infected children identified by screening Number analysed for primary outcome: 392 Age range: 6 to 12 years Inclusion criteria: children in grades 2 to 5 of 14 schools in Jamaica with intensities of Trichura > 1200 eggs/g Exclusion criteria: children with mental handicaps identified by their teachers |
|
| Interventions | Multiple doses vs placebo
|
|
| Outcomes |
Other outcomes measured but not reported: stool at baseline and at 8 weeks after second treatment round (Kato): prevalence and intensity, weight, height, z‐scores (NCHS standard) |
|
| Notes | Location: Jamaica Burden: high Source of funding: grant from the James S. McDonnell Foundation. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random‐numbers table. |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Paricipants blinded; unclear whether assessors were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 96% (392/407) of randomized participants were evaluated. Inclusion of all randomized participants (number evaluable/number randomized): 96% (392/407). |
| Selective reporting (reporting bias) | Low risk | All stated outcomes reported. |
| Other bias | Low risk | No obvious other source of bias. |
Solon 2003.
| Methods | RCT Length of follow‐up: 16 weeks |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 808/851 Age range/ mean age: 10 years Inclusion criteria: children in grades 1 to 6 Exclusion criteria: children with Haemoglobin < 8 g/dL |
|
| Interventions | Single dose vs placebo
|
|
| Outcomes | No useable data Not included in review: urine iodine, stool egg count. Measured but not reported: weight, height, haemoglobin, physical fitness (Harvard step test), heart rate, cognitive ability measured by the Primary Mental Abilities Test for Filipino Children. The test measures verbal, non verbal and quantitative skills. |
|
| Notes | Location: Philippines Burden: intermediate Narrative results: No significant difference in change in weight. Deworming improved the iron status of a subgroup of moderately to severely participants. Deworming had either no effect or a negative effect on fitness scores, and the effect on heart rate was inconclusive. Deworming had either no effect or a negative effect on mental ability scores. Sources of support: The Nutrition Center of the Philippines, The Procter & Gamble Co. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization at individual level, no further details. |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Double‐blind trial. Quote: "Both the researchers and the trial participants were blinded to the treatment assignment of each child". Quote: "Placebo beverage and placebo anthelmintic pills were indistinguishable from their counterparts in appearance, smell and taste". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 808/851 (95%) enrolled participants were evaluated, no reasons for withdrawal reported. Inclusion of all randomized participants (number evaluable/number randomized): 95% (808/851). |
| Selective reporting (reporting bias) | High risk | Nutritional and haemoglobin outcomes not fully reported. |
| Other bias | Low risk | No obvious other source of bias. |
Stephenson 1989.
| Methods | RCT Length of follow‐up: 6 months |
|
| Participants | Infected children (all children in the school were known to be infected) Number analysed for primary outcome: 150 Age range/mean age: 8.5 years Inclusion criteria: all available children in lower grades (standards 1 and 2) in Mvindeni Primary School, Kwale district (unscreened); subgroup of 36 boys chosen; haemoglobin > 8 g/dL; willing to co‐operate in physical tests; pre‐pubertal Exclusion criteria: haemoglobin < 8 g/dL |
|
| Interventions | Single dose vs placebo
|
|
| Outcomes |
Not included in review: all above converted to % median for sex and age; prevalence and mean egg counts (arithmetic and geometric means) Test heart rates and score for subgroup |
|
| Notes | Location: Kenya Burden: high Source of funding: Smith Kline & French Laboratories, Ltd., and the Edna McConnell Clark Foundation, grant 284‐0120. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "allocated at random within sex", no further details reported. |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants blinded, tablets identical for treatment and placebo. Quote: "Both examinations were carried out with the same team of workers, each doing the same procedures, and were done in a blind fashion". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 88% (150/171) of randomized participants were evaluated, reasons for losses to follow‐up not reported. Inclusion of all randomized participants (number evaluable/number randomized): 88% (150/171). |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported. |
| Other bias | Low risk | No obvious other source of bias. |
Stephenson 1993.
| Methods | RCT Length of follow‐up: 3.6 months (subgroup) and 8.2 months (main trial) |
|
| Participants | Infected children (all children in the school were known to be infected) Number analysed for primary outcome: 284 Age range/ mean age: 7 to 13 years Inclusion criteria: all school children (unscreened) in grades 1 to 5 in Mvindeni Primary School Subgroup (53 analysed) of 60 boys chosen because haemoglobin > 80 g/L, willing to cooperate in physical tests and appetite tests, pre‐pubertal, infected with at least 1 of helminths (screened), hookworm < 20,000 eggs/g; hookworm or Trichuris count > 1000 eggs/g or Ascaris > 4000 eggs/g Exclusion criteria: Severe anaemia (haemoglobin < 75 g/L) |
|
| Interventions | Multiple doses vs placebo
|
|
| Outcomes |
Not included in review: prevalence, eggs/g: geometric and arithmetic mean; converted to percentage of median for age and sex using NCHS references; % weight‐for‐age, % height for age; % weight‐for‐height; % arm circumference for age; % triceps for age; % subscapular for age; appetite (self‐rating and snack consumed intake in kJ) |
|
| Notes | Location: Kwale, Kenya Burden: high Source of funding: supported in part by Thrasher Research Fund and SmithKline Beecham, Ltd. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "at random within sex by descending hookworm egg count". |
| Allocation concealment (selection bias) | Unclear risk | No details reported |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants blinded, tablets identical for treatment and placebo. Quote: "Both examinations were conducted by the same team, each doing the same procedures, and were done in a blind fashion". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 86% (284/328) of randomized participants were evaluated, reasons for losses to follow‐up not reported. Inclusion of all randomized participants (number evaluable/number randomized): 86% (284/328). |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported |
| Other bias | Low risk | No obvious other source of bias |
Sternberg 1997 (Screened).
| Methods | RCT Length of follow‐up: 2.3 months (10 weeks) |
|
| Participants | Infected children identified by screening Number analysed for primary outcome: 133 Age range/mean age: 10.25 years Inclusion criteria: children in Grades 4 and 5 in nine primary schools in central Jamaica with mild to‐moderate infections of T. Trichiura (> 1200 eggs per g of stool) Exclusion criteria: none reported |
|
| Interventions | Single dose vs placebo
|
|
| Outcomes | Cognitive tests: two tests of perceptual speed; motor speed using grooved pegboard test‐dominant/nondominant hand; memory using free recall, digit span forward/backwards; reasoning using verbal analogies and figural series completions. Not included in the review: stool egg counts at baseline and 10 weeks; socioeconomic status. Outcomes not reported: height, weight and BMI (measured at baseline and end of study, only reported at baseline). |
|
| Notes | Location: Jamaica Burden: high There was an infected placebo group and an quote: "uninfected control group" Source of funding: James S. McDonnell Foundation. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “The infected children were paired by sex within each class. If no match was available within the same class, then a child from the same grade of the school was chosen. The children in each pair were then randomly assigned to either treatment or placebo group.” |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: “control groups received inert placebo tablets, which looked identical to the albendazole ones” Quote: “These tests were administered individually in the order in which they are listed above by one of two testers, who was unaware of the child's group assignment.” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No children were lost to follow‐up. Inclusion of all randomized participants (number evaluable/number randomized): 100% (133/133). |
| Selective reporting (reporting bias) | High risk | Quote: “All children had their heights and weights measured on enrollment and at the end of the study.” Height and weight only reported at baseline. |
| Other bias | Low risk | No other obvious source of bias. |
Stoltzfus 1997 (Cluster).
| Methods | Cluster‐RCT Method to adjust for clustering: generalised estimating equations Cluster unit: school Average cluster size: 255 ICCs: not reported Length of follow‐up: 12 months |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 12 schools randomized containing 3063 children Mean age: 10.5 years Inclusion criteria: children in grades 1 to 5 from 12 randomly selected schools on Pemba island; only grades 1 to 4 included in evaluation of nutritional effect Exclusion criteria: none stated |
|
| Interventions | Multiple doses vs placebo
|
|
| Outcomes |
Estimates are provided from multiple regression models taking into account various baseline differences for 2 subgroups above and below 10 years old. Unadjusted outcomes not presented. (These 2 groups were combined in the Dickson 2000a Cochrane Review.) Other outcomes measured but not reported: micronutrient status (blood) for protoporphyrin and serum ferritin; stool egg count (Kato‐Katz); z‐scores for height‐for‐age and weight‐for‐height; body mass index. |
|
| Notes | Location: Zanzibar, Tanzania Burden: high Appropriate adjustment made for cluster randomization using general estimating equation Source of funding: funded through cooperative agreement DAN‐5116‐1‐00‐8051‐00 between The Johns Hopkins University and the Office of Health and Nutrition, United States Agency for International Development. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 3 schools randomly selected from each of the 4 districts, and then allocated. |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No details reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 84% (3063/3605) of randomized participants were evaluated, reasons for losses to follow‐up not reported. Inclusion of all participants who were randomized within clusters (number evaluable/number randomized): 84% (3063/3605). |
| Selective reporting (reporting bias) | High risk | Not all pre‐specified outcomes reported adequately. |
| Other bias | Low risk | Recruitment bias: low (Unlikely to change schools) Baseline imbalance: low (no differences apparent) Loss of clusters: low (none reported) Incorrect analysis: cluster adjusted (low risk) Comparability with RCTs randomizing individuals: unclear |
Stoltzfus 2001.
| Methods | RCT (factorial design) Length of follow‐up: 12 months |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 359 in mebendazole arm aged 6 to 59 months Age range: 3 to 56 months Inclusion criteria: all children in Kengeja village, with age reported as 3 to 56 months by parents; 3 months before planned start of trial (pre‐school children) Exclusion criteria: severe anaemia (< 70 g/L) |
|
| Interventions | Multiple doses vs placebo
Treatment strategy: randomized and treated all children Both groups also received: 0.5 mL ferrous sulphate (20 mg/mL); 10 mg iron daily for 1 year or placebo as per factorial design |
|
| Outcomes |
Not included in review: prevalence and egg counts (no SD/SEM); motor and language scores (results of multiple regression and correlations; raw data not reported) haemoglobin (results not reported by randomized comparisons) Others measured but not reported: stool (Kato‐Katz); weight; height; malaria film; ferritin; appetite as reported by mothers |
|
| Notes | Location: Zanzibar, Tanzania Burden: intermediate Factorial design, with households randomized to iron, random allocation of mebendazole by child, stratified by iron allocation and age grouped households. An iron with mebendazole treatment term was tested in all regression models, but it did not reach significance Source of funding: Thrasher Research Fund between The Johns Hopkins University and the United States Agency for International Development, AL Pharma, Baltimore, MD, and Pharmamed, Malta. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomized by quote: "blocks of 4", no further details reported. |
| Allocation concealment (selection bias) | Low risk | Pills in bottles with unique treatment codes, assigned by 1 investigator, codes kept in sealed envelopes. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Participants and provider were blinded; unclear whether assessor was blinded. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 52% (359/684) enrolled participants were evaluated. Inclusion of all randomized participants (number evaluable/number randomized): 52% (359/684 = 52%). |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported. |
| Other bias | Low risk | No obvious other source of bias. |
Sur 2005.
| Methods | RCT Length of follow‐up: 12 months |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 683 Age range: 2 to 5 years Inclusion criteria: all children aged 2 to 5 in slum area of Tiljala identified and enrolled Exclusion criteria: major illnesses; birth defects; and unwillingness to participate |
|
| Interventions | Multiple doses vs placebo
|
|
| Outcomes |
Other outcomes measured but not reported: stool samples from random sample of 30% (formalin concentration technique) for prevalence of Ascaris; weight‐for‐age; diarrhoeal episodes |
|
| Notes | Location: India Burden: intermediate Source of funding: Indian Council of Medical Research, New Delhi, India. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers sequence. |
| Allocation concealment (selection bias) | Low risk | Identical coded bottles. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Participants and key personnel were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 97% (683/702) of enrolled participants were evaluated. Inclusion of all randomized participants (number evaluable/number randomized): 97% (683/702). |
| Selective reporting (reporting bias) | High risk | Incomplete reporting of some outcomes (prevalence of Ascaris in stools; weight‐for‐age; diarrhoeal episodes). |
| Other bias | Low risk | No obvious other source of bias. |
Tee 2013 (Screened).
| Methods | RCT Length of follow‐up: 12 months |
|
| Participants | Infected children identified by screening Mean age: 7.3 years Number analysed for primary outcome: 33 Inclusion criteria: children with confirmed Trichus trichiura in a rural school Exclusion criteria: none reported |
|
| Interventions | Single dose vs placebo
|
|
| Outcomes |
Not included in review: urinary tumour necrosis factor (TNF)‐alpha levels |
|
| Notes | Location: Sekolah Rendah Kebangsaan Tawang, Kelantan, Malaysia Burden: high Source of funding: Universiti Sains Malaysia Short Term Grant. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization software was used. |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Quote: "For participants and assessors, no details were reported." Quote: "Both the active drug and placebo were repackaged by a pharmacist blinded to the trial groups". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 33/37 participants analysed for the primary outcome; reasons for loss to follow‐up unclear. Inclusion of all randomized participants (number evaluable/number randomized): 89% (33/37). |
| Selective reporting (reporting bias) | Low risk | All stated outcomes reported. |
| Other bias | Low risk | No obvious other source of bias. |
Watkins 1996.
| Methods | RCT Length of follow‐up: 6 months |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 226 for nutritional outcomes, reduced for cognitive outcomes Age range: 7 to 12 years Inclusion criteria: children attending grades 1 to 4 in primary schools in the Guatemalan highlands Exclusion criteria: > 12 years; deworming medicine in last year |
|
| Interventions | Multiple doses vs placebo
|
|
| Outcomes |
Not included in review: egg counts (Kato‐Katz: arithmetic and geometric mean); z‐scores (NCHS‐CDC‐WHO reference) for weight‐for‐age, change in weight‐for‐age, height, change in height, height‐for‐age, change in height‐for‐age, weight‐for‐height, and change in height‐for‐age. |
|
| Notes | Location: Guatemala Burden: high Source of funding: Pew Charitable Trusts, the US Agency for International Development University Development and Linkage Program, the Children’s Miracle Network Telethon, and the ARCS Foundation. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "stratified by gender and age and then randomly assigned". |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: "The children and field workers were unaware of treatment group assignment". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 90% (226/250) of randomized participants were evaluated. Quote: "No differences were detected in treatment group assignment, initial age, anthropometry, socioeconomic status, and worm status between the 228 children who remained in the trial and the 18 who dropped out.” Sample size for nutritional data is smaller due to missing data. Inclusion of all randomized participants (number evaluable/number randomized): 90% (226/250). |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes reported. |
| Other bias | Low risk | No other obvious source of bias. |
Willett 1979.
| Methods | RCT Length of follow‐up: 12 months |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 268 Age range: 6 to 91 months Inclusion criteria: pre‐school children from Ubiri village who attended clinic and produced a stool sample Exclusion criteria: none stated |
|
| Interventions | Multiple doses
|
|
| Outcomes |
Measured but not reported: height; length; stool egg count in subgroup (Kato method); growth rates using least square method. |
|
| Notes | Location: Tanzania Burden: intermediate Source of funding: Research and Publications Committee, University of Dar es Salaam. Analysis was supported by a training grant (HL 05998‐04) from the National Heart, Lung and Blood Institute, NIH, DHEW Bethesda, MD. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random‐numbers table. |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Quote: "children were weighed and measured as before by a person unaware of their treatment status"; placebo and treatment given as a flavoured syrup. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 78% (268/341) of randomized participants were evaluated; inclusion of all randomized participants (number evaluable/number randomized): 78% (268/341). |
| Selective reporting (reporting bias) | High risk | Not all pre‐specified outcomes reported. |
| Other bias | Low risk | No obvious other source of bias. |
Wiria 2013 (Cluster).
| Methods | Cluster‐RCT Method to adjust for clustering: primary outcome of BMI was not adjusted for clustering Cluster unit: household Average cluster size: 4 ICCs: not reported Length of follow‐up: 21 months |
|
| Participants | All children living in endemic area Number analysed for primary outcome: 906 households containing 3230 participants Age range/mean age: Children aged 19 years and less Inclusion criteria: all household in members except those < 2 years old or pregnant Exclusion criteria: none stated |
|
| Interventions | Multiple dose vs placebo
|
|
| Outcomes |
aWeight and height in children aged 16 and less. bBMI measured in children aged 19 years and less. Not included in review: Malaria‐like symptoms questionnaire, finger prick blood test for malaria, skin prick tests, symptoms of asthma and atopic dermatitis, stool sample for Tichuris and hookworms. |
|
| Notes | Location: Ende district of Flores Island, Indonesia Burden: intermediate Source of funding: The Royal Netherlands Academy of Arts and Science (KNAW), European, Prof. Dr. P.C. Flu Foundation. Weight and height data were provided by the authors of the recent Campbell review (Welch 2016). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Random Allocation software" used. |
| Allocation concealment (selection bias) | Unclear risk | No details reported. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Participants and personnel blinded. Quote: "The treatment code was concealed from trial investigators and participants. The un‐blinding of treatment codes occurred after all laboratory results had been entered into the database." Not reported whether the assessors for height and weight were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 19% (3230/4004) of children lost to follow‐up. 5% (906/954) of clusters lost to follow‐up. |
| Selective reporting (reporting bias) | Low risk | All stated outcomes reported. |
| Other bias | Low risk | Recruitment bias: low (unlikely to change households) Baseline imbalance: low (no differences apparent) Loss of clusters: low (ITT analysis done; in the albendazole arm 61 people moved to a house that was assigned to placebo while in the placebo arm 62 people moved to a house that was assigned to albendazole) Incorrect analysis: cluster adjusted (low risk) Comparability with RCTs randomizing individuals: unclear |
Yap 2014 (Screened).
| Methods | RCT Length of follow‐up: 6 months |
|
| Participants | Infected children identified by screening Number analysed for primary outcome: 194 Age range: 9 to 12 years Inclusion criteria: children aged 9 to 12 years from 5 primary schools, with at least one type of STH infection. Exclusion criteria: deworming treatment within 6 months before the current trial. |
|
| Interventions | Single dose vs placebo
|
|
| Outcomes |
Not included in review: parasitological examination. |
|
| Notes | Location: Bulanghsam township bordering Myanmar, a sub‐division of Menghai county in Xishuangbanna Dai autonomous prefecture, situated in Yunnan province, P.R. China Burden: high Source of funding: Swiss Tropical and Public Health Institute in Basel, Switzerland and the National Institute of Parasitic Diseases, Chinese Center of Diseases Control and Prevention in Shanghai, P.R. China. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The treatment allocation sequence was generated by a statistician using block randomization with randomly varying block sizes of 2, 4, and 6." |
| Allocation concealment (selection bias) | Low risk | Quote: "Albendazole and placebo tablets were packaged by staff not involved in the field work into sealed envelopes marked with unique identifiers." |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Participants and personnel blinded. Not reported whether the assessors for height and weight were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Inclusion of all randomized participants (number evaluable/number randomized): 92% (194/211). |
| Selective reporting (reporting bias) | Low risk | All stated outcomes reported. |
| Other bias | Low risk | No other obvious risk of bias. |
AWC: Anganwadi child‐care centre; BMI: body mass index; CDC: Centers for Disease Control and Prevention; CI: confidence interval; ICC: intracluster correlation coefficient; ICDS: Integrated Child Development Service; IGg: immunoglobulin g; ITT: intention‐to‐treat; IU: international unit; MUAC: mid‐upper arm circumference; NCHS: National Center for Health Statistics; NGO: non‐governmental organisation; RCT: randomized controlled trial; SD: standard deviation; SEM: standard error of the mean; STH: soil‐transmitted helminth; WHO: World Health Organization.
Burden: a measure of the prevalence and intensity of infection (see Table 5)
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Araujo 1987 | Not an RCT. |
| Assaré 2016a | Intervention comprised of water, sanitation and hygiene plus albendazole versus albendazole. |
| Assaré 2016b | No relevant outcomes. |
| Baird 2011 | From stepped‐wedge design, long‐term follow‐up. Evaluated in a separately published review and at high risk of bias. |
| Baird 2016 | Long‐term follow‐up study. Results appraised in separate review (Jullien 2016) and at high risk of bias and therefore excluded. |
| Beasley 1999 | Treatment regimen comprised of albendazole for soil‐transmitted helminths and praziquantel against schistosomiasis versus placebo. |
| Bhargava 2003 | Treatment regimen comprised of albendazole for soil‐transmitted helminths and praziquantel against schistosomiasis versus placebo. |
| Bhutta 2009 | Population with significant comorbidity – 6‐ to 24‐month old children with severe anaemia (< 70 g/L), in a population with severe anaemia. |
| Boivin 1993 | Factorial‐designed RCT with children allocated to deworming and iron supplementation, and in which the analysis compares the results for the levamisole and iron group against all the other groups combined. Thus, the analysis is confounded by the iron co‐intervention (Included in the Dickson 2000a Cochrane Review). |
| Bruckner 2015 | No relevant outcomes. |
| Bruckner 2016 | No relevant outcomes. |
| Campbell 2015 | Intervention comprised of water, sanitation and hygiene plus albendazole versus albendazole. |
| Campbell 2016 | Intervention comprised of water, sanitation and hygiene plus albendazole versus albendazole. |
| Campbell 2017 | Intervention comprised of water, sanitation and hygiene plus albendazole versus albendazole. |
| Chen 2016 | Included anaemic children. |
| Cooper 2006 | Trial of allergy with no outcomes of interest. |
| Cowden 2000 | Not an RCT. |
| Croke 2014 | 3% (1097/37,165) of randomized participants were evaluated in 46% (22/48) of the original parishes from the initial Alderman 2006 (Cluster) trial. All children were offered treatment after the initial trial, and therefore potentially all of these children received treatment for deworming. Appraised in a separate systematic review by Jullien 2016 and classified as high risk of bias and excluded. |
| de Ruiter 2017 | No relevant outcomes. |
| Diouf 2002 | Intervention comprised mebendazole, vitamin A, and iron supplementation and metronidazole as a combined intervention versus placebo. |
| Evans 1986 | Treatments randomized, but some placebo groups accessed treatment. Analysis was by the treatment received, and randomization was ignored (included in the Dickson 2000a Cochrane Review). |
| Fernando 1983 | Two villages allocated to treatment or no treatment on the basis of a coin toss. Essentially a cluster‐RCT with 2 large clusters (Included in the Dickson 2000a Cochrane Review, which reported that no conclusions could be drawn from the results due to selective reporting). |
| Forrester 1998 | Treatment regimen comprised of 3 days of albendazole versus 1 day of albendazole and 2 days of placebo vs 1 day of pyrantel and 2 days of placebo. |
| Friis 2003 | Combined treatment regimen albendazole for soil‐transmitted helminths and praziquantel for Schistosoma mansoni versus placebo. |
| Gilgen 2001 | Population consisted of adults. |
| Hadidjaja 1998 | Cluster‐RCT with 2 units of allocation to mebendazole and placebo. Trial authors stated that there were differences in environmental sanitary conditions in the clusters (Included in the Dickson 2000a Cochrane Review, but it was noted that the groups were not comparable and there was high loss to follow‐up). |
| Hamidu 2014 | No relevant outcomes. |
| Hathirat 1992 | Treatment regimen comprised of albendazole for soil‐transmitted helminths and iron versus placebo. |
| Hosseini 2017 | Intervention comprises levamisole plus Hepatitis B vaccine versus placebo + Hepatitis B vaccine. Less than 10% of participants were under 20 years of age. |
| Jalal 1998 | No relevant outcomes. |
| Jinabhai 2001a | Treatment regimen comprised of albendazole for soil‐transmitted helminths and praziquantel against schistosomiasis versus placebo. |
| Jinabhai 2001b | Treatment regimen comprised of albendazole for soil‐transmitted helminths and praziquantel against schistosomiasis versus placebo. |
| Karyadi 1996 | Not an RCT. |
| Klarmann‐Schulz 2017 | Population consisted of adults. |
| Krubwa 1974 | Not an RCT. |
| Kvalsvig 1991b | The researchers were unable to collect outcome data after treatment due to major floods in the area. |
| Latham 1990 | Population with schistosomiasis treated with praziquantel. |
| Marinho 1991 | Treatment regimen comprised of mebendazole and metronidazole versus placebo. |
| Mofid 2015 | Population consisted of postpartum women. |
| Moser 2016 | No relevant outcomes. |
| Mwaniki 2002 | Treatment regimen albendazole for soil‐transmitted helminths and praziquantel for schistosomiasis versus placebo. |
| Ozier 2011 | Long‐term follow‐up study. Results appraised in separate review (Jullien 2016) and at high risk of bias and therefore excluded. |
| Ozier 2016 | Long‐term follow‐up study. Results appraised in separate review (Jullien 2016) and at high risk of bias and therefore excluded. |
| Pollitt 1991 | Not described as randomized; conference proceedings. |
| Rohner 2010 | Treatment regimen albendazole for soil‐transmitted helminths and praziquantel for schistosomiasis versus placebo. |
| Srichaikul 2016 | Population consisted of adults. |
| Steinmann 2008 | No relevant outcomes. |
| Stephenson 1980 | Treatment consisted of levamisole with no untreated controls. |
| Stephenson 1985 | Treatment regimen metrifonate used to treat Schistosoma haematobium versus placebo. |
| Stobaugh 2017 | Population consisted of children who had recovered from moderate acute malnutrition. Intervention consisted of a package of health and nutrition interventions plus albendazole versus nutrition counselling only. |
| Tahapary 2015 | Only those > 16 years of age were assessed. |
| Tahapary 2017 | Only those > 16 years of age were assessed. |
| Tanumihardjo 1996 | No relevant outcomes. |
| Tanumihardjo 2004 | The only randomization is the timing of the deworming medicine. |
| Taylor 2001 | Treatment regimen albendazole for soil‐transmitted helminths and praziquantel for S. haematobium versus placebo. |
| Thein‐Hlaing 1991 | 3/21 intervention villages were not randomly allocated, and unclear how intervention and control villages were allocated as there was a large imbalance (8 intervention and 13 non‐intervention villages). |
| Trehan 2016 | Albendazole plus micronutrients versus placebo. |
| Uscátegui 2009 | Trial in population with malaria. |
| Van der Zalm 2016 | No relevant outcomes. |
| Wammes 2016 | No relevant outcomes. |
| Wang 2017 | Intervention consisted of albendazole plus zinc plus multiple micronutrient powder versus placebo. |
| Wright 2009 | No relevant outcomes. |
| Yang 2003 | Did not consider nutritional or cognitive outcome measures. |
RCT: randomized controlled trial.
Characteristics of studies awaiting assessment [ordered by study ID]
Carmona‐Fonseca 2015.
| Methods | Clinical, randomized, controlled trial with parallel groups |
| Participants | Children |
| Interventions | Administration of pyrantel pamoate (pamoate) (< 2 years) or albendazole (≥ 2 years), with or without oral vitamin A |
| Outcomes | Worm prevalence and load, haemoglobin and retinol levels. |
| Notes | Awaiting clarification on randomization. |
Characteristics of ongoing studies [ordered by study ID]
NCT00367627.
| Trial name or title | Relative efficacy of two regimens of ante‐helminthic treatment |
| Methods | Clinical trial |
| Participants | Total enrolment: 200 Inclusion criteria: age 2 to 5 years; not suffering from serious chronic illness; stool test positive for STHs; not taken any anthelminthic drug in previous 6 months; parents/guardian agree their child's participation Exclusion criteria: age < 2 years and > 5 years; stool test negative for any intestinal helminth; suffering from serious chronic illness; parents/guardian not willing to give consent for their child's participation; if he/she receives any anthelminthic drug after survey but before the trial interventions |
| Interventions |
|
| Outcomes | Primary
Secondary
|
| Starting date | December 2006 |
| Contact information | Mohammad M Alam MBBS, Principal Investigator, ICDDR,B: Centre for Health and Population Research, masud_icddrb@yahoo.com |
| Notes | ClinicalTrials.gov identifier: NCT00367627 Sources of support: International Centre for Diarrhoeal Disease Research, Bangladesh (sponsor) Anticpated completion May 2008 |
NCT02725255.
| Trial name or title | Design and clinical evaluation of a school meal with deworming properties |
| Methods | Clinical trial |
| Participants | Total enrolment: 326 Inclusion criteria: children 4 to 12 years Exclusion criteria: children with known allergy to papaya fruit products |
| Interventions |
|
| Outcomes | Primary
Secondary
|
| Starting date | May 2015 |
| Contact information | Elijah M Songok, PhD, Kenya Medical Research Institute |
| Notes | ClinicalTrials.gov identifier: NCT02725255 Sources of support: Kenya Medical Research Institute Completed March 2016 |
NCT02754583.
| Trial name or title | Sanitation, water, and instruction in face‐washing for trachoma |
| Methods | Clinical trial |
| Participants | Estimated enrolment: 220,000 Inclusion criteria
Exclusion criteria
|
| Interventions |
|
| Outcomes | Primary
Secondary
|
| Starting date | November 2015 |
| Contact information | Dionna M Fry, MPH Jeremy D Keenan, MD, MPH |
| Notes | ClinicalTrials.gov identifier: NCT02754583 Sources of support: Francis I. Proctor Foundation, The Carter Center, Bahir Dar Regional Health and Research Laboratory, Emory University, National Eye Institute (NEI) Anticipated completion July 2019 |
STHs: soil‐transmitted helminths
Differences between protocol and review
We amended the title of the review from ‘Deworming drugs for soil‐transmitted intestinal worms in children: effects on nutritional indicators, haemoglobin, and school performance' to ‘Public health deworming programmes for soil‐transmitted helminths in children living in endemic areas'.
We revised the protocol, and changes are listed in Table 22.
13. Prespecified analytical plan for 2019 update.
| David Taylor‐Robinson, Nicola Maayan, and Paul Garner 8 Jan 2018 | ||
|
Why is updating the review a priority at this time? •The 2015 version of the review stimulated significant policy debate, and led to the Campbell collaboration undertaking a review of the same subject, which strongly corroborated the Cochrane findings •We have received formal feedback on the 2015 version of the review, which we need to address •Croke and colleagues have undertaken an alternative meta‐analysis of the outcome for weight gain •A critical analysis of long‐term follow‐up studies of deworming has been published in 2017 •The new WHO guidelines for deworming were published in 2017, citing the evidence in the 2015 Cochrane review •We performed a search in November 2017 and at least two new studies have been published that meet the inclusion criteria for our review •All review authors from the previous 2015 Cochrane Review on have been invited to opt in as authors on this updated review | ||
| Protocol section | Appraisal points | Refreshing the protocol |
| Background and research question | • Review and update background section, including supporting references to take account of any changes that may have occurred. This should include updating any new information and current policy debates on the topic. • Assess whether the current review question remains relevant to patients and practice. | •We will update information on the policy context following the publication of the new WHO guidelines, and summarise the policy debate since the publication of the 2015 review. Cochrane provide a timeline here: http://www.cochrane.org/news/deworming‐debate •Our 2015 Cochrane Review informed the WHO guidelines, and we tool part in the guideline development process. The main review question remains relevant. |
| • Consider whether the existing PICO(s) remain(s) current, in the light of new knowledge. • Identify any new understanding of definition of patient populations. • Identify new interventions, or those that have been withdrawn, that are no longer in use. • Identify any changes in usual care standards. • Check for standardised core outcomes sets, such as those developed in collaboration with the core outcome measures in effectiveness trials (COMET) initiative (www.comet‐initiative.org) or by guideline groups since the original review. • Check for any relevant patient reported outcomes to include subsequent to the original review. • Consider any new studies with less risk of bias that might warrant a stricter study design inclusion criteria (where the older version, when there was a dearth of evidence, included observational or quasi‐randomised comparisons). | •We plan to add an analysis that takes into account worm prevalence and intensity, building on the analysis of community category in our previous update •There are no patient reported outcomes that we are aware •Our inclusion criteria in terms of study design will remain the same. The Campbell collaboration have undertaken a review including non‐RCT designs •In October 2017, Vittoria Lutje performed a scoping search and we 2 new studies for inclusion in the review, following screening of the abstracts and full‐text review. | |
| Methods | • Appraise and update the methods pending relevant methodological advancements or developments. For example, if (1) there are new tools for assessing the risk of bias of individual studies or appraising the quality of a body of evidence (e.g. GRADE); or (2) new and efficient search approaches are feasible, such as a targeted approach to searching, taking into account the quality of the original search, and ensuring that the search for the update is of high quality. • Update or include a 'Summary of findings' table, which is recommended for all systematic reviews, because it improves the clarity, understanding, and interpretation of the findings of a systematic review, and rapidly reduces the amount of time readers require to find key information | •We will revise our description of studies to include an assessment of the age of children included; and the prevalence/intensity of each worm infection •For prevalence, we are using percentage of population infected with each worm species < 20 % low, 20‐80% intermediate, 80+high •For intensity high if >=10% of children have moderate/heavy infections, low if <10% of children have moderate/heavy infections •We will document if data is missing on intensity/prevalence •We will revise our analysis to include an updated stratification based upon the prevalence/intensity of helminth infection •As in the previous review, we will use the GRADE approach to assess the quality of evidence •We will update the Summary of Findings Tables. |
Contributions of authors
DTR wrote the protocol, applied inclusion criteria, assessed quality, extracted data, conducted data analysis, and wrote the first draft of earlier versions of this review.
NM conducted the data re‐extraction and the re‐analysis for the previous version and this edition. NM applied inclusion criteria, assessed quality, extracted data, conducted data analysis, and drafted the results of the update.
SD assessed risk of bias and extracted data for a subset of the trials, and contributed to the analysis and the writing of the review.
MR applied inclusion criteria, assessed quality, extracted data, conducted data analysis, and contributed to the analysis and the writing of the review.
PG provided advice at all stages of the review production, applied inclusion criteria, assessed quality, quality assured data extraction, helped construct the comparisons, carried out the first draft of the GRADE assessment, and helped write the review.
In this review update, all authors participated in regular meetings, conference calls, and decisions about the data, the analysis, the responses to criticisms, the adjustment of the analysis plans and the interpretation.
Sources of support
Internal sources
Liverpool School of Tropical Medicine, UK.
External sources
-
Department for International Development, UK.
Project number 300342‐104
Evidence and Programme Guidance Unit, Department of Nutrition for Health and Development, WHO, Switzerland.
-
Medical Research Council (MRC), UK.
David Taylor‐Robinson is funded by the MRC on a Clinician Scientist Fellowship (MR/P008577/1).
Declarations of interest
None of the review authors receive salary, payment, or academic fees for the promotion or delivery of soil‐transmitted helminth deworming programmes in low‐ and middle‐income countries (LMICs).
DTR is funded by the MRC on a Clinician Scientist Fellowship (MR/P008577/1), and has no known conflicts of interest.
NM worked on this update as both an employee of Cochrane Response and then as an independent consultant. She has no known conflicts of interest.
SD has no known conflicts of interest.
MR has no known conflicts of interest.
PG is the Director of the Research, Evidence and Development Initiative (READ‐It) project, that aims to increase the number of decisions in the health sector in LMICs based on reliable evidence. He has no known conflicts of interest.
Employed at Cochrane Response until January 2018, and completed the review under current affiliation 2
Edited (no change to conclusions)
References
References to studies included in this review
Alderman 2006 (Cluster) {published data only}
- Alderman H, Konde‐Lule J, Sebuliba I, Bundy D, Hall A. Correction. BMJ 2012;345:e8724. [DOI: 10.1136/bmj.e8724] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alderman H, Konde‐Lule J, Sebuliba I, Bundy D, Hall A. Effect on weight gain of routinely giving albendazole to preschool children during child health days in Uganda: cluster randomised controlled trial. BMJ 2006;333(7559):122. [DOI] [PMC free article] [PubMed] [Google Scholar]
Awasthi 1995 (Cluster) {published data only}
- Awasthi S, Peto R, Fletcher R, Glick H. Controlling parasitic infection in children under five years of age: giving albendazole in conjunction with an Indian government Vitamin A supplement program. Treating Parasitic Infestations in Children [Monograph No. 3]. Philadelphia: International Clinical Epidemiology Network (INCLEN), 1995. [Google Scholar]
- Awasthi S, Peto R, Pande VK, Fletcher RH, Read S, Bundy DA. Effects of deworming on malnourished preschool children in India: an open‐labelled, cluster‐randomized trial. PLOS Neglected Tropical Diseases 2008;2(4):e223. [DOI] [PMC free article] [PubMed] [Google Scholar]
Awasthi 2000 {published and unpublished data}
- Awasthi S, Pande VK, Fletcher RS. Effectiveness and cost‐effectiveness of albendazole in improving nutritional status of pre‐school children in urban slums. Indian Pediatrics 2000;37(1):19‐29. [PubMed] [Google Scholar]
Awasthi 2001 (Cluster) {published data only}
- Awasthi S, Pande VK. Six‐monthly de‐worming in infants to study effects on growth. Indian Journal of Pediatrics 2001;68(9):823‐7. [DOI] [PubMed] [Google Scholar]
Awasthi 2013 (Cluster) {unpublished data only}
- Awasthi S, Peto R, Read S, Richards S, Pande V, Bundy DA, DEVTA team. Population de‐worming with 6‐monthly albendazole: DEVTA, a cluster‐randomised trial among 1 million preschool children in North India. [unpublished manuscript].
- University of Oxford and the United States Agency for International Development (USAID). Deworming and Enhanced Vitamin A Supplementation DEVTA Project (The DEVTA Trial). https://clinicaltrials.gov/ct2/show/NCT00222547 (accessed 23 February 2012).
Beach 1999 {published data only}
- Beach MJ, Streit TG, Addiss DG, Prospere R, Roberts JM, Lammie PJ. Assessment of combined ivermectin and albendazole for treatment of intestinal helminth and Wuchereria bancrofti infections in Haitian schoolchildren. American Journal of Tropical Medicine and Hygiene 1999;60(3):479‐86. [DOI] [PubMed] [Google Scholar]
Donnen 1998 {published data only}
- Donnen P, Brasseur D, Dramaix M, Vertongen F, Zihindula M, Muhamiriza M, et al. Vitamin A Supplemenation but not deworming improves growth of malnourished preschool children in eastern Zaire. Journal of Nutrition 1998;128(8):1320‐7. [DOI] [PubMed] [Google Scholar]
Dossa 2001 {published data only}
- Dossa RA, Ategbo EA, Koning FL, Raaij JM, Hautvast JG. Impact of iron supplementation and deworming on growth performance in preschool Beninese children. European Journal of Clinical Nutrition 2001;55(4):223‐8. [DOI] [PubMed] [Google Scholar]
Fox 2005 {published data only}
- Fox LM, Furness BW, Haser JK, Desire D, Brissau JM, Milord MD, et al. Tolerance and efficacy of combined diethylcarbamazine and albendazole for treatment of Wuchereria bancrofti and intestinal helminth infections in Haitian children. American Journal of Tropical Medicine and Hygiene 2005;73(1):115‐21. [PubMed] [Google Scholar]
Freij 1979a (Screened) {published data only}
- Freij L, Meeuwisse GW, Berg NO, Wall S, Gebre‐Medhin M. Ascariasis and malnutrition. A study in urban Ethiopian children. American Journal of Clinical Nutrition 1979;32(7):1545‐53. [DOI] [PubMed] [Google Scholar]
Freij 1979b (Screened) {published data only}
- Freij L, Meeuwisse GW, Berg NO, Wall S, Gebre‐Medhin M. Ascariasis and malnutrition. A study in urban Ethiopian children. American Journal of Clinical Nutrition 1979;32(7):1545‐53. [DOI] [PubMed] [Google Scholar]
Garg 2002 {published data only}
- Garg R, Lee LA, Beach MJ, Wamae CN, Ramakrishnan U, Deming MS. Evaluation of the Integrated Management of Childhood Illness guidelines for treatment of intestinal helminth infections among sick children aged 2‐4 years in western Kenya. Transactions of the Royal Society of Tropical Medicine and Hygiene 2002;96(5):543‐8. [DOI] [PubMed] [Google Scholar]
Gateff 1972 {published data only}
- Gateff C, Lemarinier G, Labusquiere R. [Chimiotherapie antihelminthique,systematique au thiabendazole en milieu scolaire African]. Annales de la Société Belge de Médecine Tropicale 1972;52(2):103‐12. [PubMed] [Google Scholar]
Goto 2009 {published data only}
- Goto R, Mascie‐Taylor CG, Lunn PG. Impact of anti‐Giardia and anthelminthic treatment on infant growth and intestinal permeability in rural Bangladesh: a randomised double‐blind controlled study. Transactions of the Royal Society of Tropical Medicine and Hygiene 2009;103(5):520‐9. [DOI] [PubMed] [Google Scholar]
Greenberg 1981 {published data only}
- Greenberg BL, Gilman RH, Shapiro H, Gilman JB, Mondal G, Maksud M, et al. Single dose piperazine therapy for Ascaris lumbricoides: an unsuccessful method of promoting growth. American Journal of Clinical Nutrition 1981;34(11):2508‐16. [DOI] [PubMed] [Google Scholar]
Gupta 1982 {published data only}
- Gupta MC, Urrutia JJ. Effect of periodic antascaris and antigiardia treatment on nutritional status of preschool children. American Journal of Clinical Nutrition 1982;36(1):79‐86. [DOI] [PubMed] [Google Scholar]
Hadju 1996 {published data only}
- Hadju V, Stephenson LS, Abadi K, Mohammed HO, Bowman DD, Parker RS. Improvements in appetite and growth in helminth‐infected schoolboys three and seven weeks after a single dose of pyrantel pamoate. Parasitology 1996;113(Pt 5):497‐504. [DOI] [PubMed] [Google Scholar]
Hadju 1997 {published data only}
- Hadju V, Satriono, Abadi K, Stephenson LS. Relationship between soil‐transmitted helminthiases and growth in urban slum school children in Ujung Pandang, Indonesia. International Journal of Food Sciences and Nutrition 1997;48(2):85‐93. [DOI] [PubMed] [Google Scholar]
Hall 2006 (Cluster) {unpublished data only}
- Hall A, Nguyen Bao Khanh L, Bundy D, Quan Dung N, Hong Son T, Lansdown R. A randomized trial of six monthly deworming on the growth and educational achievements of Vietnamese school children. Unpublished manuscript.
Joseph 2015 {published data only}
- Joseph SA, Casapia M, Gyorkos TW. The effect of deworming timing and frequency on growth in early preschool‐age children: Results of a randomized‐controlled trial of mebendazole in one to two‐year old children in the Peruvian Amazon. American Journal of Tropical Medicine and Hygiene. 2014; Vol. Conference: 63rd Annual Meeting of the American Society of Tropical Medicine and Hygiene, ASTMH 2013 New Orleans, LA United States. Conference Start: 20141102 Conference End: 20141106. Conference Publication: (var.pagings). 91 (5 SUPPL. 1):386.
- Joseph SA, Casapia M, Lazarte F, Rahme E, Pezo L, Blouin B, et al. The effect of deworming on early childhood development in Peru: A randomized controlled trial. SSM ‐ Population Health 2015;1:32‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph SA, Casapia M, Montresor A, Rahme E, Ward BJ, Marquis GS, et al. The effect of deworming on growth in one‐year‐old children living in a soil‐transmitted helminth‐endemic area of Peru: a randomized controlled trial. PLOS Neglected Tropical Diseases 2015;9(10):e0004020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph SA, Montresor A, Casapia M, Pezo L, Gyorkos TW. Adverse events from a randomized, multi‐arm, placebo‐controlled trial of mebendazole in children 12‐24 months of age. American Journal of Tropical Medicine and Hygiene 2016;95(1):83‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PLOS Neglected Tropical Diseases Staff. Correction: The effect of deworming on growth in one‐year‐old children living in a soil‐transmitted helminth‐endemic area of Peru: a randomized controlled trial. PLOS Neglected Tropical Diseases 2015;9(12):e0004288. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kirwan 2010 {published data only}
- Kirwan P, Asaolu SO, Molloy SF, Abiona TC, Jackson AL, Holland CV. Patterns of soil‐transmitted helminth infection and impact of four monthly albendazole treatments in preschool children from semi‐urban communities in Nigeria: a double‐blind placebo‐controlled randomised trial. BMC Infectious Diseases 2009;9:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirwan P, Jackson AL, Asaolu SO, Molloy SF, Abiona TC, Bruce MC, et al. Impact of repeated four‐monthly anthelmintic treatment on Plasmodium infection in preschool children: a double‐blind placebo‐controlled randomized trial. BMC Infectious Diseases 2010;10:277. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kloetzel 1982 {published data only}
- Kloetzel K, Merluzzi Filho TJ, Kloetzel D. Ascaris and malnutrition in a group of Brazilian children ‐ a follow‐up study. Journal of Tropical Pediatrics 1982;28(1):41‐3. [DOI] [PubMed] [Google Scholar]
Koroma 1996 {published data only}
- Koroma MM, Williams RA, Haye RR, Hodges M. Effects of albendazole on growth of primary school children and the prevalence and intensity of soil‐transmitted helminths in Sierra Leone. Journal of Tropical Pediatrics 1996;42(6):371‐2. [DOI] [PubMed] [Google Scholar]
Kruger 1996 {published data only}
- Kruger M, Badenhorst CJ, Mansvelt EP, Laubscher JA, Benade AJ. The effect of iron fortification in a school feeding scheme and anthelminthic therapy on the iron status and growth of 6‐8 year old school children. Food and Nutrition Bulletin 1996;17(1):11‐21. [Google Scholar]
Kvalsvig 1991a (Screened) {published data only}
- Kvalsvig JD, Cooppan RM, Connolly KJ. The effects of parasite infections on cognitive processes in children. Annals of Tropical Medicine and Parasitology 1991;85(5):551‐68. [DOI] [PubMed] [Google Scholar]
Lai 1995 {published data only}
- Lai KP, Kaur H, Mathias RG, Ow‐Yang CK. Ascaris and Trichuris do not contribute to growth retardation in primary school children. Southeast Asian Journal of Tropical Medicine and Public Health 1995;26(2):322‐8. [PubMed] [Google Scholar]
Le Huong 2007 {published data only}
- Huong T, Brouwer ID, Nguyen KC, Burema J, Kok FJ. The effect of iron fortification and de‐worming on anaemia and iron status of Vietnamese schoolchildren. British Journal of Nutrition 2007;97(5):955‐62. [DOI] [PubMed] [Google Scholar]
Liu 2017 (Cluster) {published data only}
- Liu C, Lu L, Zhang L, Luo R, Sylvia S, Medina A, et al. Effect of deworming on indices of health, cognition, and education among schoolchildren in rural China: a cluster‐randomized controlled trial. American Journal of Tropical Medicine and Hygiene 2017;96(6):1478‐89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu L, Liu C, Medina A, Smith DS, Zhang L, Rozelle S. Effect of deworming on nutritional indicators, cognitive abilities and school performance among school children in rural China: a cluster randomized controlled trial. American Journal of Tropical Medicine and Hygiene 2015;93(4 Suppl):16‐7. [Google Scholar]
Michaelsen 1985 {published data only}
- Michaelsen KF. Hookworm infection in Kweneng District, Botswana. A prevalence survey and a controlled treatment trial. Transactions of the Royal Society of Tropical Medicine and Hygiene 1985;79(6):848‐51. [DOI] [PubMed] [Google Scholar]
Miguel 2004 (Cluster) {published data only}
- Aiken A, Davey C, Hargreaves J, Hayes R. Re‐analysis of health and educational impacts of a school‐based deworming program in western Kenya: a pure replication. International Journal of Epidemiology 2015; Vol. DOI 10.1093/ije/dyv127. [DOI] [PMC free article] [PubMed]
- Aiken AM, Davey C, Hargreaves JR, Hayes RJ. Reanalysis of health and educational impacts of a school‐based deworming program in western Kenya: Part 1, pure replication, 3ie Replication Paper 3, part 1. Washington, DC: International Initiative for Impact Evaluation (3ie). 2014. www.3ieimpact.org/media/filer_public/2015/01/07/3ie_rps3_worms_replication_1.pdf (accessed 10 July 2015).
- Davey C, Aiken AM, Hayes RJ, Hargreaves JR. Re‐analysis of health and educational impacts of a school based deworming program in Western Kenya: a statistical replication of a cluster quasi‐randomized stepped‐wedge trial. International Journal of Epidemiology 2015;44(5):1581‐92. [DOI: 10.1093/ije/dyv128] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miguel E, Kremer M. Worms: Identifying impacts on education and health in the presence of treatment externalities. Econometrica 2004;72(1):159‐217. [Google Scholar]
Ndibazza 2012 {published data only}
- Ndibazza J, Mpairwe H, Webb EL, Mawa PA, Nampijja M, Muhangi L, et al. Impact of anthelminthic treatment in pregnancy and childhood on immunisations, infections and eczema in childhood: a randomised controlled trial. PLOS One 2012;7(12):e50325. [DOI: 10.1371/journal.pone.0050325] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nga 2009 {published data only}
- Nga TT, Winichagoon P, Dijkhuizen MA, Khan NC, Wasantwisut E, Furr H, et al. Multi‐micronutrient‐fortified biscuits decreased prevalence of anemia and improved micronutrient status and effectiveness of deworming in rural Vietnamese school children. Journal of Nutrition 2009;139(5):1013‐21. [DOI] [PubMed] [Google Scholar]
- Nga TT, Winichagoon P, Dijkhuizen MA, Khan NC, Wasantwisut E, Wieringa FT. Decreased parasite load and improved cognitive outcomes caused by deworming and consumption of multi‐micronutrient fortified biscuits in rural Vietnamese schoolchildren. American Journal of Tropical Medicine and Hygiene 2011;85(2):333‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nokes 1992 (Screened) {published data only}
- Nokes C, Grantham‐McGregor SM, Sawyer AW, Cooper ES, Bundy DA. Parasitic helminth infection and cognitive function in school children. Proceedings of The Royal Society of London. Series B: Biological sciences 1992;247(1319):77‐81. [DOI] [PubMed] [Google Scholar]
- Nokes C, Grantham‐McGregor SM, Sawyer AW, Cooper ES, Robinson BA, Bundy DA. Moderate to heavy infections of Trichuris trichiura affect cognitive function in Jamaican school children. Parasitology 1992;104(Pt 3):539‐47. [DOI] [PubMed] [Google Scholar]
Olds 1999 {published data only}
- Olds GR, King C, Hewlett J, Olveda R, Wu G, Ouma J, et al. Double‐blind placebo‐controlled study of concurrent administration of albendazole and praziquantel in school children with schistosomiasis and geohelminths. Journal of Infectious Diseases 1999;179(4):996‐1003. [DOI] [PubMed] [Google Scholar]
Ostwald 1984 {published data only}
- Ostwald R, Fitch M, Arhold R, Sheild J, Louie D, Kilner J, et al. The effect of intestinal parasites on nutritional status in well‐nourished school‐age children in the highlands of Papua New Guinea. Nutrition Reports International 1984;30(6):1409‐21. [Google Scholar]
Palupi 1997 {published data only}
- Palupi L, Schultink W, Achadi E, Gross R. Effective community intervention to improve hemoglobin status in preschoolers receiving once‐weekly iron supplementation. American Journal of Clinical Nutrition 1997;65(4):1057‐61. [DOI] [PubMed] [Google Scholar]
Rousham 1994 (Cluster) {published data only}
- Northrop‐Clewes CA, Rousham EK, Mascie‐Taylor CN, Lunn PG. Anthelmintic treatment of rural Bangladeshi children: effect on host physiology, growth, and biochemical status. American Journal of Clinical Nutrition 2001;73(1):53‐60. [DOI] [PubMed] [Google Scholar]
- Rousham EK, Mascie‐Taylor CG. An 18‐month study of the effect of periodic anthelminthic treatment on the growth and nutritional status of pre‐school children in Bangladesh. Annals of Human Biology 1994;21(4):315‐24. [DOI] [PubMed] [Google Scholar]
Sarkar 2002 (Screened) {published data only}
- Sarkar NR, Anwar KS, Biswas KB, Mannan MA. Effect of deworming on nutritional status of ascaris infested slum children of Dhaka, Bangladesh. Indian Pediatrics 2002;39(11):1021‐6. [PubMed] [Google Scholar]
Simeon 1995 (Screened) {published data only}
- Gardner JM, Grantham‐McGregor S, Baddeley A. Trichuris trichiura infection and cognitive function in Jamaican school children. Annals of Tropical Medicine and Parasitology 1996;90(1):55‐63. [DOI] [PubMed] [Google Scholar]
- Simeon DT, Grantham‐McGregor SM, Callender JE, Wong MS. Treatment of Trichuris trichiura infections improves growth, spelling scores and school attendance in some children. Journal of Nutrition 1995;125(7):1875‐83. [DOI] [PubMed] [Google Scholar]
- Simeon DT, Grantham‐McGregor SM, Wong MS. Trichuris trichiura infection and cognition in children: results of a randomized clinical trial. Parasitology 1995;110(Pt 4):457‐64. [DOI] [PubMed] [Google Scholar]
Solon 2003 {published data only}
- Solon FS, Sarol JN, Bernardo AB, Solon JA, Mehansho H, Sanchez‐Fermin LE, et al. Effect of a multiple‐micronutrient‐fortified fruit powder beverage on the nutrition status, physical fitness, and cognitive performance of schoolchildren in the Philippines. Food and Nutrition Bulletin 2003;24(4 Suppl):S129‐40. [DOI] [PubMed] [Google Scholar]
Stephenson 1989 {published data only}
- Stephenson LS, Latham MC, Kinoti SN, Kurz KM, Brigham H. Improvements in physical fitness of Kenyan school boys infected with hookworm, Trichuris trichiura, and Ascaris lumbricoides following a single dose of albendazole. Transactions of the Royal Society of Tropical Medicine and Hygiene 1990;84(2):277‐82. [DOI] [PubMed] [Google Scholar]
- Stephenson LS, Latham MC, Kurz KM, Kinoti SN, Brigham H. Treatment with a single dose of albendazole improves growth of Kenyan schoolchildren with hookworm, Trichuris trichiura, and Ascaris lumbricoides infections. American Journal of Tropical Medicine and Hygiene 1989;41(1):78‐87. [PubMed] [Google Scholar]
Stephenson 1993 {published data only}
- Adams EJ, Stephenson LS, Latham MC, Kinoti SN. Physical activity and growth of Kenyan school children with hookworm, Trichuris trichiura and Ascaris lumbricoides infections are improved after treatment with albendazole. Journal of Nutrition 1994;124(8):1199‐206. [DOI] [PubMed] [Google Scholar]
- Stephenson LS, Latham MC, Adams EJ, Kinoti SN, Pertet A. Physical fitness, growth and appetite of Kenyan school boys with hookworm, Trichuris trichiura and Ascaris lumbricoides infections are improved four months after a single dose of albendazole. Journal of Nutrition 1993;123(6):1036‐46. [DOI] [PubMed] [Google Scholar]
- Stephenson LS, Latham MC, Adams EJ, Kinoti SN, Pertet A. Weight gain of Kenyan school children infected with hookworm, Trichuris trichiura and Ascaris lumbricoides is improved following once‐ or twice‐yearly treatment with albendazole. Journal of Nutrition 1993;123(4):656‐65. [DOI] [PubMed] [Google Scholar]
Sternberg 1997 (Screened) {published data only}
- Sternberg RJ, Powell C, McGrane P, Grantham‐McGregor S. Effects of a parasitic infection on cognitive functioning. Journal of Experimental Psychology: Applied 1997;3(1):67. [Google Scholar]
Stoltzfus 1997 (Cluster) {published and unpublished data}
- Stoltzfus RJ, Albonico M, Chwaya HM, Tielsch JM, Schulze KJ, Savioli L. Effects of the Zanzibar school‐based deworming program on iron status of children. American Journal of Clinical Nutrition 1998;68(1):179‐86. [DOI] [PubMed] [Google Scholar]
- Stoltzfus RJ, Albonico M, Tielsch JM, Chwaya HM, Savioli L. School‐based deworming program yields small improvement in growth of Zanzibari school children after one year. Journal of Nutrition 1997;127(11):2187‐93. [DOI] [PubMed] [Google Scholar]
Stoltzfus 2001 {published data only}
- Stoltzfus RJ, Chway HM, Montresor A, Tielsch JM, Jape JK, Albonico M, et al. Low dose daily iron supplementation improves iron status and appetite but not anemia, whereas quarterly anthelminthic treatment improves growth, appetite and anemia in Zanzibari preschool children. Journal of Nutrition 2004;134(2):348‐56. [DOI] [PubMed] [Google Scholar]
- Stoltzfus RJ, Kvalsvig JD, Chwaya HM, Montresor A, Albonico M, Tielsch JM, et al. Effects of iron supplementation and anthelmintic treatment on motor and language development of preschool children in Zanzibar: double blind, placebo controlled study. BMJ 2001;323(7326):1389‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sur 2005 {published data only}
- Sur D, Saha DR, Manna B, Rajendran K, Bhattacharya SK. Periodic deworming with albendazole and its impact on growth status and diarrhoeal incidence among children in an urban slum of India. Transactions of the Royal Society of Tropical Medicine and Hygiene 2005;99(4):261‐7. [DOI] [PubMed] [Google Scholar]
Tee 2013 (Screened) {published data only}
- Tee MH, Lee YY, Majid NA, Noori NM, Raj SM. Growth reduction among primary school children with light trichuriasis in Malaysia with albendazole. Southeast Asian Journal of Tropical Medicine and Public Health 2013;44(1):19‐24. [PubMed] [Google Scholar]
Watkins 1996 {published data only}
- Watkins WE, Cruz JR, Pollitt E. The effects of deworming on indicators of school performance in Guatemala. Transactions of the Royal Society of Tropical Medicine and Hygiene 1996;90(2):156‐61. [DOI] [PubMed] [Google Scholar]
- Watkins WE, Pollitt E. Effect of removing Ascaris on the growth of Guatemalan schoolchildren. Pediatrics 1996;97(6 Pt 1):871‐6. [PubMed] [Google Scholar]
Willett 1979 {published data only}
- Willett WC, Kilama WL, Kihamia CM. Ascaris and growth rates: a randomized trial of treatment. American Journal of Public Health 1979;69(10):987‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wiria 2013 (Cluster) {published data only}
- Wiria AE, Hamid F, Wammes LJ, Kaisar MM, May L, Prasetyani MA, et al. The effect of three‐monthly albendazole treatment on malarial parasitemia and allergy: a household‐based cluster‐randomized, double‐blind, placebo‐controlled trial. PLOS One 2013;8(3):e57899. [DOI: 10.1371/journal.pone.0057899] [DOI] [PMC free article] [PubMed] [Google Scholar]
Yap 2014 (Screened) {published data only}
- Yap P, Wu FW, Du ZW, Hattendorf J, Chen R, Jiang JY, et al. Effect of deworming on physical fitness of school‐aged children in Yunnan, China: a double‐blind, randomized, placebo‐controlled trial. PLoS Neglected Tropical Diseases 2014;8(7):e2983. [DOI: 10.1371/journal.pntd.0002983] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Araujo 1987 {published data only}
- Araujo RL, Araujo MB, Machado RD, Braga AA, Leite BV, Oliveira JR. Evaluation of a program to overcome vitamin A and iron deficiencies in areas of poverty in Minas Gerais, Brazil. Archivos Latinoamericanos de Nutrición 1987;37(1):9‐22. [PubMed] [Google Scholar]
Assaré 2016a {published data only}
- Assaré RK, Hürlimann E, Ouattara M, N'Guessan NA, Tian‐Bi YN, Yapi A, et al. Sustaining the control of schistosoma mansoni in western Cote d'Ivoire: baseline findings before the implementation of a randomized trial. American Journal of Tropical Medicine and Hygiene 2016;94(2):352‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Assaré 2016b {published data only}
- Assaré RK, Tian‐Bi YN, Yao PK, N'Guessan NA, Ouattara M, Yapi A, et al. Sustaining control of Schistosomiasis mansoni in Western Cote d'Ivoire: results from a SCORE study, one year after initial praziquantel administration. PLOS Neglected Tropical Diseases 2016;10(1):e0004329. [DOI] [PMC free article] [PubMed] [Google Scholar]
Baird 2011 {unpublished data only}
- Baird S, Hicks JH, Kremer M, Miguel E. Worms at Work: Long‐run Impacts of Child Health Gains. http://eml.berkeley.edu//˜emiguel/pdfs/miguel_wormsatwork.pdf (accessed 10 July 2015).
- Baird S, Hicks JH, Kremer M, Miguel E. Worms at work: long‐run impacts of a child health investment. 2016. Available from www.nber.org/papers/w21428 (accessed prior to 20 August 2019). [DOI] [PMC free article] [PubMed]
Baird 2016 {published data only}
- Baird S, Hicks JH, Kremer M, Miguel E. Worms at work: Long‐run impacts of a child health investment. 2016. Available from www.nber.org/papers/w21428 (accessed prior to 20 August 2019). [DOI] [PMC free article] [PubMed]
Beasley 1999 {published data only}
- Beasley NM, Tomkins AM, Hall A, Kihamia CM, Lorri W, Nduma B, et al. The impact of population level deworming on the haemoglobin levels of schoolchildren in Tanga, Tanzania. Tropical Medicine and International Health 1999;4(11):744‐50. [DOI] [PubMed] [Google Scholar]
Bhargava 2003 {published data only}
- Bhargava A, Jukes M, Lambo J, Kihamia CM, Lorri W, Nokes C, et al. Anthelmintic treatment improves the hemoglobin and serum ferritin concentrations of Tanzanian schoolchildren. Food and Nutrition Bulletin 2003;24(4):332‐42. [DOI] [PubMed] [Google Scholar]
Bhutta 2009 {published data only}
- Bhutta Z, Klemm R, Shahid F, Rizvi A, Rah JH, Christian P. Treatment response to iron and folic acid alone is the same as with multivitamins and/or anthelminthics in severely anemic 6‐ to 24‐month‐old children. Journal of Nutrition 2009;139(8):1568‐74. [DOI] [PubMed] [Google Scholar]
Boivin 1993 {published data only}
- Boivin MJ, Giordani B. Improvements in cognitive performance for schoolchildren in Zaire, Africa, following an iron supplement and treatment for intestinal parasites. Journal of Pediatric Psychology 1993;18(2):249‐64. [DOI] [PubMed] [Google Scholar]
Bruckner 2015 {published data only}
- Bruckner S, Agnandji ST, Berberich S, Bache E, Fernandes JF, Schweiger B, et al. Effect of antihelminthic treatment on vaccine immunogenicity to a seasonal influenza vaccine in primary school children in Gabon: a randomized placebo‐controlled trial. PLOS Neglected Tropical Diseases 2015;9(6):e0003768. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bruckner 2016 {published data only}
- Bruckner S, Agnandji ST, Elias J, Berberich S, Bache E, Fernandes J, et al. A single‐dose antihelminthic treatment does not influence immunogenicity of a meningococcal and a cholera vaccine in Gabonese school children. Vaccine 2016;34(44):5384‐90. [DOI] [PubMed] [Google Scholar]
Campbell 2015 {published data only}
- Campbell SJ, Nery S, D'Este C, Llewellyn S, Andrews R, Gray DJ, et al. Analysis of risk factors for soil‐transmitted helminth infections and impact on child development in Timor‐Leste. Tropical Medicine and International Health 2015;20:308. [Google Scholar]
Campbell 2016 {published data only}
- Campbell SJ, Nery SV, D'Este CA, Gray DJ, McCarthy JS, Traub RJ, et al. Water, sanitation and hygiene related risk factors for soil‐transmitted helminth and Giardia duodenalis infections in rural communities in Timor‐Leste. International Journal for Parasitology 2016;46(12):771‐9. [DOI] [PubMed] [Google Scholar]
Campbell 2017 {published data only}
- Campbell SJ, Nery SV, D'Este CA, Gray DJ, McCarthy JS, Traub RJ, et al. Investigations into the association between soil‐transmitted helminth infections, haemoglobin and child development indices in Manufahi District, Timor‐Leste. Parasites and Vectors 2017;10(1):192. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chen 2016 {published data only}
- Chen K, Xie HM, Tian W, Zheng X, Jiang AC. Effect of single‐dose albendazole and vitamin A supplementation on the iron status of pre‐school children in Sichuan, China. British Journal of Nutrition 2016;115(8):1415‐23. [DOI] [PubMed] [Google Scholar]
Cooper 2006 {published data only}
- Cooper PJ, Chico ME, Vaca MG, Moncayo AL, Bland JM, Mafla E, et al. Effect of albendazole treatments on the prevalence of atopy in children living in communities endemic for geohelminth parasites: a cluster‐randomised trial. Lancet 2006;367(9522):1598‐603. [DOI] [PubMed] [Google Scholar]
Cowden 2000 {published data only}
- Cowden J, Hotez P. Mebendazole and albendazole treatment of geohelminth infections in children and pregnant women. Pediatric Infectious Disease Journal 2000;19(7):659‐60. [DOI] [PubMed] [Google Scholar]
Croke 2014 {published data only}
- Croke K. The long run effects of early childhood deworming on literacy and numeracy: Evidence from Uganda. http://scholar.harvard.edu/files/kcroke/files/ug_lr_deworming_071714.pdf (accessed 10 July 2015). [DOI] [PMC free article] [PubMed]
de Ruiter 2017 {published data only}
- Ruiter K, Tahapary DL, Wammes LJ, Wiria AE, Hamid F, Lieshout L, et al. The effect of three‐monthly albendazole treatment on Th2 responses: Differential effects on IgE and IL‐5. Parasite Immunology 2017;39(6):e12428. [DOI] [PubMed] [Google Scholar]
Diouf 2002 {published data only}
- Diouf S, Diagne I, Moreira C, Signate SY, Faye O, Ndiaye O, et al. Integrated treatment of iron deficiency, vitamin A deficiency and intestinal parasitic diseases: impact on Senegalese children's growth [Traitement integre de la carence en fer, de l'avitaminose A et des parasitoses intestinales: impact sur la croissance des enfants senegalais]. Archives de Pédiatrie 2002;9(1):102‐3. [DOI] [PubMed] [Google Scholar]
Evans 1986 {unpublished data only}
- Evans J, Martin J, Mascie‐Taylor CG. The Effect of Periodic Deworming with Pyrantel Pamoate on the Growth and Nutritional Status of Pre‐school Children in Northern Bangladesh [Monograph No. 3]. London: Save the Children Fund, 1986. [Google Scholar]
Fernando 1983 {published and unpublished data}
- Fernando MA, Balasuriya, Somaratne. Effect of Ascaris lumbricoides infestation on growth of children. Indian Pediatrics 1983;20(10):721‐31. [PubMed] [Google Scholar]
Forrester 1998 {published data only}
- Forrester JE, Bailar JC 3rd, Esrey SA, José MV, Castillejos BT, Ocampo G. Randomised trial of albendazole and pyrantel in symptomless trichuriasis in children. Lancet 1998;352(9134):1103‐8. [DOI] [PubMed] [Google Scholar]
Friis 2003 {published data only}
- Friis H, Mwaniki D, Omondi B, Muniu E, Thiong'o F, Ouma J, et al. Effects on haemoglobin of multi‐micronutrient supplementation and multi‐helminth chemotherapy: a randomized, controlled trial in Kenyan school children. European Journal of Clinical Nutrition 2003;57(4):573‐9. [DOI] [PubMed] [Google Scholar]
Gilgen 2001 {published data only}
- Gilgen D, Mascie‐Taylor CG. The effect of anthelmintic treatment on helminth infection and anaemia. Parasitology 2001;122(Pt 1):105‐10. [DOI] [PubMed] [Google Scholar]
- Gilgen DD, Mascie‐Taylor CG, Rosetta L. Intestinal helminth infections, anaemia and labour productivity of female tea pluckers in Bangladesh. Tropical Medicine and International Health 2001;6(6):449‐57. [DOI] [PubMed] [Google Scholar]
Hadidjaja 1998 {published data only}
- Hadidjaja P, Bonang E, Suyardi MA, Abidin SA, Ismid IS, Margono SS. The effect of intervention methods on nutritional status and cognitive function of primary school children infected with Ascaris lumbricoides. American Journal of Tropical Medicine and Hygiene 1998;59(5):791‐5. [DOI] [PubMed] [Google Scholar]
Hamidu 2014 {published data only}
- Hamidu BB, Tettevi EJ, Larbi JA, Osei‐Atweneboana MY. The efficacy of albendazole and levamisole drug combination in individuals with reduced efficacy for single‐dose albendazole treatment against hookworm infections. American Journal of Tropical Medicine and Hygiene 2014;Conference: 63rd Annual Meeting of the American Society of Tropical Medicine and Hygiene, ASTMH 2013 New Orleans, LA United States. Conference Start: 20141102 Conference End: 20141106. Conference Publication: (var.pagings). 91 (5 SUPPL. 1):152. [Google Scholar]
Hathirat 1992 {published data only}
- Hathirat P, Valyasevi A, Kotchabhakdi NJ, Rojroongwasinkul N, Pollitt E. Effects of an iron supplementation trial on the Fe status of Thai schoolchildren. British Journal of Nutrition 1992;68(1):245‐52. [DOI] [PubMed] [Google Scholar]
Hosseini 2017 {published data only}
- Hosseini M, Shalchiantabrizi P, Dadgarmoghaddam M, Ahmady‐Simab S, Behjati A, Salari M. The effect of oral levamisole co‐administration on the level of immune response to hepatitis b vaccine in healthy individuals: a randomized clinical trial. Iranian Journal of Allergy, Asthma, and Immunology 2017;16(3):219‐27. [PubMed] [Google Scholar]
Jalal 1998 {published data only}
- Jalal F, Nesheim MC, Agus Z, Sanjur D, Habicht JP. Serum retinol concentrations in children are affected by food sources of beta‐carotene, fat intake, and anthelmintic drug treatment. American Journal of Clinical Nutrition 1998;68(3):623‐9. [DOI] [PubMed] [Google Scholar]
Jinabhai 2001a {published data only}
- Jinabhai CC, Taylor M, Coutsoudis A, Coovadia HM, Tomkins AM, Sullivan KR. Epidemiology of helminth infections: implications for parasite control programmes, a South African perspective. Public Health Nutrition 2001;4(6):1211‐9. [DOI] [PubMed] [Google Scholar]
Jinabhai 2001b {published data only}
- Jinabhai CC, Taylor M, Coutsoudis A, Coovadia HM, Tomkins AM, Sullivan KR. A randomized controlled trial of the effect of antihelminthic treatment and micronutrient fortification on health status and school performance of rural primary school children. Annals of Tropical Paediatrics 2001;21(4):319‐33. [DOI] [PubMed] [Google Scholar]
Karyadi 1996 {published data only}
- Karyadi E, Gross R, Sastroamidjojo S, Dillon D, Richards AL, Sutanto I. Anthelminithic treatment raises plasma iron levels but dose not decrease the acute‐phase response in Jakarta School children. Southeast Asian Journal of Tropical Medicine and Public Health 1996;27(4):742‐53. [PubMed] [Google Scholar]
Klarmann‐Schulz 2017 {published data only}
- Klarmann‐Schulz U, Specht S, Debrah AY, Batsa L, Ayisi‐Boateng NK, Osei‐Mensah J, et al. Comparison of doxycycline, minocycline, doxycycline plus albendazole and albendazole alone in their efficacy against onchocerciasis in a randomized, open‐label, pilot trial. PLOS Neglected Tropical Diseases 2017;11(1):e0005156. [DOI] [PMC free article] [PubMed] [Google Scholar]
Krubwa 1974 {published data only}
- Krubwa F, Gatti F, Lontie M, Nguete M, Vandepitte J, Thienpont D. Quarterly administration of mebendazole to suburban school children [Administration trimestrielle de mebendazole en milieu scolaire suburbain]. Médecine Tropicale 1974;34(5):679‐87. [Google Scholar]
Kvalsvig 1991b {published data only}
- Kvalsvig JD, Cooppan RM, Connolly KJ. The effects of parasite infections on cognitive processes in children. Annals of Tropical Medicine and Parasitology 1991;85(5):551‐68. [DOI] [PubMed] [Google Scholar]
Latham 1990 {published data only}
- Latham MC, Stephenson LS, Kurz KM, Kinoti SN. Metrifonate or praziquantel treatment improves physical fitness and appetite of Kenyan schoolboys with Schistosoma haematobium and hookworm infections. American Journal of Tropical Medicine and Hygiene 1990;43(2):170‐9. [DOI] [PubMed] [Google Scholar]
Marinho 1991 {published data only}
- Marinho HA, Shrimpton R, Giugliano R, Burini RC. Influence of enteral parasites on the blood vitamin A levels in preschool children orally supplemented with retinol and/or zinc. European Journal of Clinical Nutrition 1991;45(11):539‐44. [PubMed] [Google Scholar]
Mofid 2015 {published data only}
- Mofid LS, Casapia M, Montresor A, Rahme E, Fraser WD, Marquis GS, et al. Maternal Deworming Research Study (MADRES) protocol: A double‐blind, placebo‐controlled randomised trial to determine the effectiveness of deworming in the immediate postpartum period. BMJ Open 2015;5(6):e008560. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moser 2016 {published data only}
- Moser W, Ali SM, Ame SM, Speich B, Puchkov M, Huwyler J, et al. Efficacy and safety of oxantel pamoate in school‐aged children infected with Trichuris trichiura on Pemba Island, Tanzania: a parallel, randomised, controlled, dose‐ranging study. Lancet Infectious Diseases 2016;16(1):53‐60. [DOI] [PubMed] [Google Scholar]
Mwaniki 2002 {published data only}
- Mwaniki D, Omondi B, Muniu E, Thiong'o F, Ouma J, Magnussen P, et al. Effects on serum retinol of multi‐micronutrient supplementation and multi‐helminth chemotherapy: a randomised, controlled trial in Kenyan school children. European Journal of Clinial Nutrition 2002;56(7):666‐73. [DOI] [PubMed] [Google Scholar]
Ozier 2011 {unpublished data only}
- Ozier O. Exploiting externalities to estimate the long‐term effects of early childhood deworming. http://files.givewell.org/files/DWDA%202009/Interventions/Deworming/Ozier%20Yale.pdf (accessed 10 July 2015).
Ozier 2016 {published data only}
- Ozier O. Exploiting externalities to estimate the long‐term effects of early childhood deworming. 2016. http://economics.ozier.com/owen/papers/ozier_early_deworming_20160727.pdf (accessed prior to 20 August 2019).
Pollitt 1991 {published data only}
- Pollitt E, Wayne W, Perez‐Escamilla R, Latham M, Stephenson LS. Double blind clinical trial on the effects of helminth infection on cognition. FASEB Journal 1991;5:A1081. [Google Scholar]
Rohner 2010 {published data only}
- Rohner F, Zimmermann MB, Amon RJ, Vounatsou P, Tschannen AB, N'goran EK, et al. In a randomized controlled trial of iron fortification, anthelmintic treatment and intermittent preventive treatment of malaria for anemia control in Ivorian children, only anthelmintic treatment shows modest benefit. Journal of Nutrition 2010;140(3):635‐41. [DOI] [PubMed] [Google Scholar]
Srichaikul 2016 {published data only}
- Srichaikul B, Samappito S, Wongyai S, Bakker G. The comparative double‐blind clinical study in antihelmintic efficacy between Thai traditional herbal formulae and mebendazole. American Journal of Therapeutics 2016;23(4):e1025‐31. [DOI] [PubMed] [Google Scholar]
Steinmann 2008 {published data only}
- Steinmann P, Zhou XN, Du ZW, Jiang JY, Xiao SH, Wu ZX, et al. Tribendimidine and albendazole for treating soil‐transmitted helminths, Strongyloides stercoralis and Taenia spp.: open‐label randomized trial. PLOS Neglected Tropical Diseases 2008;2(10):e322. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stephenson 1980 {published data only}
- Stephenson LS, Crompton DW, Latham MC, Schulpen TW, Nesheim MC, Jansen AA. Relationships betweenAscaris infection and growth of malnourished preschool children in Kenya. American Journal of Clinical Nutrition 1980;33(5):1165‐72. [DOI] [PubMed] [Google Scholar]
Stephenson 1985 {published data only}
- Stephenson LS, Latham MC, Kurz KM, Kinoti SN, Oduori ML, Crompton DW. Relationships of Schistosoma hematobium, hookworm and malarial infections and metrifonate treatment to hemoglobin level in Kenyan school children. American Journal of Tropical Medicine and Hygiene 1985;34(3):519‐28. [DOI] [PubMed] [Google Scholar]
Stobaugh 2017 {published data only}
- Stobaugh HC, Bollinger LB, Adams SE, Crocker A H, Grise JB, Kennedy JA, et al. Effect of a package of health and nutrition services on sustained recovery in children after moderate acute malnutrition and factors related to sustaining recovery: a cluster‐randomized trial. American Journal of Clinical Nutrition 2017;106(2):657‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tahapary 2015 {published data only}
- Tahapary DL, Ruiter K, Martin I, Lieshout L, Guigas B, Soewondo P, et al. Helminth infections and type 2 diabetes: A cluster‐randomized placebo controlled SUGARSPIN trial in Nangapanda, Flores, Indonesia. BMC Infectious Diseases 2015;15(1):133. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tahapary 2017 {published data only}
- Tahapary DL, Ruiter K, Martin I, Brienen EAT, Lieshout L, Cobbaert CM, et al. Effect of anthelmintic treatment on insulin resistance: a cluster‐randomized placebo‐controlled trial in Indonesia. Clinical Infectious Diseases 2017;65(5):764‐71. [DOI] [PubMed] [Google Scholar]
Tanumihardjo 1996 {published data only}
- Tanumihardjo SA, Permaesih D, Muherdiyantiningsih, Rustan E, Rusmil K, Fatah AC, et al. Vitamin A status of Indonesian children infected with Ascaris lumbricoides after dosing with vitamin A supplements and albendazole. Journal of Nutrition 1996;126(2):451‐7. [DOI] [PubMed] [Google Scholar]
Tanumihardjo 2004 {published data only}
- Tanumihardjo SA, Permaesih D, Muhilal. Vitamin A status and hemoglobin concentrations are improved in Indonesian children with vitamin A and deworming interventions. European Journal of Clinical Nutrition 2004;58(9):1223‐30. [DOI] [PubMed] [Google Scholar]
Taylor 2001 {published data only}
- Taylor M, Jinabhai CC, Couper I, Kleinschmidt I, Jogessar VB. The effect of different anthelmintic treatment regimens combined with iron supplementation on the nutritional status of schoolchildren in KwaZulu‐Natal, South Africa: a randomized controlled trial. Transactions of the Royal Society of Tropical Medicine and Hygiene 2001;95(2):211‐6. [DOI] [PubMed] [Google Scholar]
Thein‐Hlaing 1991 {published data only}
- Thein‐Hlaing, Thane‐Toe, Than‐Saw, Myat‐Lay‐Kyin, Myint‐Lwin. A controlled chemotherapeutic intervention trial on the relationship between Ascaris lumbricoides infection and malnutrition in children. Transactions of the Royal Society of Tropical Medicine and Hygiene 1991;85(4):523‐8. [DOI] [PubMed] [Google Scholar]
Trehan 2016 {published data only}
- Trehan I. A combined package of micronutrients and albendazole does not improve environmental enteric dysfunction or stunting in rural Malawian children. Journal of Pediatric Gastroenterology and Nutrition 2016;63:S37‐8. [Google Scholar]
Uscátegui 2009 {published data only}
- Uscátegui RM, Correa AM, Carmona‐Fonseca J. Changes in retinol, hemoglobin and ferritin concentrations in Colombian children with malaria [Spanish]. Biomédica: revista del Instituto Nacional de Salud 2009;29(2):270‐81. [PubMed] [Google Scholar]
Van der Zalm 2016 {published data only}
- Zalm MM, Soelen N, Mandalakas AM, Jacobsen M, Detjen AK, Marx FM, et al. The effect of deworming on tests of tuberculosis infection in children with recent tuberculosis exposure: a randomized controlled trial. Pediatric Infectious Disease Journal 2016;35(6):622‐7. [DOI] [PubMed] [Google Scholar]
Wammes 2016 {published data only}
- Wammes LJ, Hamid F, Wiria AE, May L, Kaisar MM, Prasetyani‐Gieseler MA, et al. Community deworming alleviates geohelminth‐induced immune hyporesponsiveness. Proceedings of the National Academy of Sciences of the United States of America 2016;113(44):12526‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2017 {published data only}
- Wang AZ, Shulman RJ, Crocker AH, Thakwalakwa C, Maleta KM, Devaraj S, et al. A combined intervention of zinc, multiple micronutrients, and albendazole does not ameliorate environmental enteric dysfunction or stunting in rural Malawian children in a double‐blind randomized controlled trial. Journal of Nutrition 2017;147(1):97‐103. [DOI] [PubMed] [Google Scholar]
Wright 2009 {published data only}
- Wright VJ, Ame SM, Haji HS, Weir RE, Goodman D, Pritchard DI, et al. Early exposure of infants to GI nematodes induces Th2 dominant immune responses which are unaffected by periodic anthelminthic treatment. PLOS Neglected Tropical Diseases 2009;3(5):e433. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yang 2003 {published data only}
- Yang WP, Shao JO, Chen YJ. Effect of chemotherapeutic regimens on soil‐transmitted nematode infections in areas with low endemicity [Chinese]. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi [Chinese Journal of Parasitology and Parasitic Diseases] 2003;21(2):128. [PubMed] [Google Scholar]
References to studies awaiting assessment
Carmona‐Fonseca 2015 {published data only}
- Carmona‐Fonseca J, Correa‐Botero A. Effect of periodic albendazole and vitamin A treatment on intestinal helminths and anaemia in children from Uraba (Antioquia, Colombia) [Efecto del albendazol y la vitamina A periódicos sobre helmintos intestinales y anemia en niños del Urabá Antioqueño]. Biosalud 2015;14(1):9‐25. [Google Scholar]
References to ongoing studies
NCT00367627 {unpublished data only}
- NCT00367627. Relative efficacy of two regimens of ante‐helminthic treatment. clinicaltrials.gov/ct2/show/NCT00367627 first posted 23 August 2006.
NCT02725255 {published data only}
- NCT02725255. Design and clinical evaluation of a school meal with deworming properties. clinicaltrials.gov/ct2/show/NCT02725255 first posted 31 March 2016.
NCT02754583 {published data only}
- NCT02754583. Sanitation, Water, and Instruction in Face‐washing for Trachoma (SWIFT). clinicaltrials.gov/ct2/show/NCT02754583 first posted 28 April 2016.
Additional references
Aiken 2014
- Aiken AM, Davey C, Hargreaves JR, Hayes RJ. Reanalysis of health and educational impacts of a school‐based deworming program in western Kenya: Part 1, pure replication, 3ie Replication Paper 3, Part 1. Washington, DC: International Initiative for Impact Evaluation (3ie). www.3ieimpact.org/evidence‐hub/replication‐studies‐status/worms‐identifying‐impacts‐education‐and‐health‐presence (accessed 21 June 2019).
Aiken 2015
- Aiken A, Davey C, Hargreaves J, Hayes R. Re‐analysis of health and educational impacts of a school‐based deworming program in western Kenya: a pure replication. International Journal of Epidemiology 2015;44(5):1572‐80. [DOI: 10.1093/ije/dyv127] [DOI] [PMC free article] [PubMed] [Google Scholar]
Albonico 2008
- Albonico M, Allen H, Chitsulo L, Engels D, Gabrielli AF, Savioli L. Controlling soil‐transmitted helminthiasis in pre‐school‐age children through preventive chemotherapy. PLOS Neglected Tropical Diseases 2008;2(3):e126. [DOI] [PMC free article] [PubMed] [Google Scholar]
Anderson 1991
- Anderson RM, May RM. Infectious Diseases of Humans: Dynamics and Control. Oxford: Oxford University Press, 1991. [Google Scholar]
Andrews 2017
- Andrews JR, Bogoch II, Utzinger J. The benefits of mass deworming on health outcomes: new evidence synthesis, the debate persists. Lancet Global Health 2017 Jan 1;5(1):e4‐5. [DOI] [PubMed] [Google Scholar]
Bleakely 2004
- Bleakley H. Disease and development: evidence from hookworm eradication in the American South. Quarterly Journal of Economics 2007;122(1):73‐117. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bundy 2009
- Bundy DA, Kremer M, Bleakley H, Jukes MC, Miguel E. Deworming and development: asking the right questions, asking the questions right. PLOS Neglected Tropical Diseases 2009;3(1):e362. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bundy 2017
- Bundy DA, Silva N, Horton S, Jamison DT, Patton GC. Disease Control Priorities, Third Edition: Volume 8. Child and Adolescent Health and Development. 3rd Edition. Vol. 8, Washington, DC: World Bank, 2017. [Google Scholar]
Carrasco‐Labra 2015
- Carrasco‐Labra A, Brignardello‐Peetersen R, Santesso N, Neumann I, Mustafa RA, Mbuagbaw L, et al. Comparison between the standard and a new alternative format of the Summary‐of Findings tables in Cochrane review users: study protocol for a randomized controlled trial. Trials 2015;16:164. [DOI 10.1186/s13063‐015‐0649‐6] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cooper 2000
- Cooper E. Treatment for intestinal helminth infection. Message does not follow from systematic review's findings. BMJ 2000;321(7270):1225‐6. [PubMed] [Google Scholar]
Copenhagen Consensus Center 2012
- Copenhagen Consensus Center. Copenhagen Consensus 2012. www.copenhagenconsensus.com/Default.aspx?ID=1626 (accessed 22 May 2012).
Croke 2016
- Croke K, Hicks JH, Hsu E, Kremer M, Miguel E. Does mass deworming affect child nutrition? Meta‐analysis, cost‐effectiveness, and statistical power. NBER Working Paper No. 22382. July 2016. www.nber.org/papers/w22382 (accessed prior to 20 August 2019).
Davey 2015
- Davey C, Aiken A, Hayes R. Re‐analysis of health and educational impacts of a school based deworming program in Western Kenya: a statistical replication of a cluster quasi‐randomised stepped‐wedge trial. International Journal of Epidemiology 2015; DOI 10.1093/ije/dyv128. [DOI] [PMC free article] [PubMed]
Evidence Action 2015
- Evidence Action. World's largest deworming program in India to start with support from Evidence Action. www.evidenceaction.org/blog‐full/largest‐deworming‐program‐in‐india‐to‐start‐with‐support‐from‐evidence‐action (accessed 16 April 2015).
Evidence Action 2018
- Evidence Action. The evidence for deworming. www.evidenceaction.org/dewormtheworld/#the‐evidence‐for‐deworming (accessed 18 September 2018).
Garner 2013
- Garner P, Taylor‐Robinson D, Sachdev HS. DEVTA: results from the biggest clinical trial ever. Lancet 2013;381(9876):1439‐41. [DOI] [PubMed] [Google Scholar]
GiveWell 2011
- GiveWell. Errors in DCP2 cost‐effectiveness estimate for deworming. http://blog.givewell.org/2011/09/29/errors‐in‐dcp2‐cost‐effectiveness‐estimate‐for‐deworming/ (accessed 22 May 2012).
GRADEpro 2014 [Computer program]
- McMaster University. GRADEpro. Version [used January 2015]. McMaster University, 2014.
Gulani 2007
- Gulani A, Nagpal J, Osmond C, Sachdev HP. Effect of administration of intestinal anthelmintic drugs on haemoglobin: systematic review of randomised controlled trials. BMJ 2007;334(7603):1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hall 2008
- Hall A, Hewitt G, Tuffrey V, Silva N. A review and meta‐analysis of the impact of intestinal worms on child growth and nutrition. Maternal and Child Nutrition 2008;4(Suppl 1):118‐236. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hawkes 2013
- Hawkes N. Deworming debunked. BMJ 2013;346:e8558. [DOI] [PubMed] [Google Scholar]
Hawkes 2017
- Hawkes N. WHO advises blanket anti‐worming treatment for children despite lack of benefit. BMJ 2017 Oct 4;359:j4589. [DOI] [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JPT, Deeks JJ (editors). Chapter 7: Selecting studies and collecting data. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Higgins 2011b
- Higgins JP, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Higgins 2011c
- Higgins JP, Altman DG, Gotzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011; Vol. 343:d5928. [DOI] [PMC free article] [PubMed]
Hotez 2009
- Hotez PJ, Fenwick A, Savioli L, Molyneux DH. Rescuing the bottom billion through control of neglected tropical diseases. Lancet 2009;373(9674):1570‐5. [DOI] [PubMed] [Google Scholar]
Hotez 2011a
- Hotez PJ. New antipoverty drugs, vaccines, and diagnostics: a research agenda for the US President's Global Health Initiative (GHI). PLOS Neglected Tropical Diseases 2011;5(5):e1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hotez 2011b
- Hotez PJ. Unleashing "civilian power": a New Americandiplomacy through neglected tropical disease control, elimination, research, and development. PLOS Neglected Tropical Diseases 2011;5(6):e1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jamison 2006
- Jamison DT, Breman JG, Measham AR, Alleyne G, Claeson M. Evans DB, et al (editors). Disease Control Priorities in Developing Countries. 2nd Edition. New York: Oxford University Press and the World Bank, 2006. [PubMed] [Google Scholar]
Jourdan 2018
- Jourdan PM, Lamberton PH, Fenwick A, Addiss DG. Soil‐transmitted helminth infections. Lancet 2018;391(10117):252–65. [DOI] [PubMed] [Google Scholar]
Jullien 2016
- Jullien S, Sinclair D, Garner P. The impact of mass deworming programmes on schooling and economic development: an appraisal of long‐term studies. International Journal of Epidemiology 2016;45(6):21402153. [DOI: 10.1093/ije/dyw283] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kramer 2014
- Kramer CV, Zhang F, Sinclair D, Olliaro PL. Drugs for treating urinary schistosomiasis. Cochrane Database of Systematic Reviews 2014, Issue 8. [DOI: 10.1002/14651858.CD000053.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JP, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Lo 2017
- Lo NC, Addiss DG, Hotez PJ, King CH, Stothard JR, Evans DS, et al. A call to strengthen the global strategy against schistosomiasis and soil‐transmitted helminthiasis: the time is now. Lancet. Infectious Diseases 2017;17(2):e64‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Molyneux 2005
- Molyneux DH, Hotez PJ, Fenwick A. "Rapid‐impact interventions": how a policy of integrated control for Africa's neglected tropical diseases could benefit the poor. PLOS Medicine 2005;2(11):e336. [DOI] [PMC free article] [PubMed] [Google Scholar]
Montresor 2002
- Montresor A, Crompton DW, Gyorkos TW, Savioli L. Helminth Control in School‐age Children: a Guide for Managers of Control Programmes. Geneva: World Health Organization, 2002. [Google Scholar]
Mudur 2015
- Mudur G. Deworming programme in India sparks controversy. BMJ 2015;350:h720. [DOI: 10.1136/bmj.h720] [DOI] [PubMed] [Google Scholar]
Pabalan 2018
- Pabalan N, Singian E, Tabangay L, Jarjanazi H, Boivin MJ, Ezeamama AE. Soil‐transmitted helminth infection, loss of education and cognitive impairment in school‐aged children: A systematic review and meta‐analysis. PLOS Neglected Tropical Diseases 2018;12(1):e0005523. [DOI] [PMC free article] [PubMed] [Google Scholar]
Patel 2014
- Patel A, Bagree S. School‐based deworming: a clear role for the European Commission. www.schoolsandhealth.org/News/Pages/School‐Based‐Deworming‐‐A‐Clear‐Role‐for‐the‐European‐Commission.aspx (accessed 18 September 2018).
Review Manager 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Salam 2015
- Salam RA, Haider BA, Humayun Q, Bhutta ZA. Effect of administration of antihelminthics for soil‐transmitted helminths during pregnancy. Cochrane Database of Systematic Reviews 2015, Issue 6. [DOI: 10.1002/14651858.CD005547.pub2] [DOI] [PubMed] [Google Scholar]
Savioli 2000
- Savioli L, Neira M, Albonico M, Beach MJ, Chwaya HM, Crompton DW, et al. Treatment for intestinal helminth infection. Review needed to take account of all relevant evidence, not only effects on growth and cognitive performance. BMJ 2000;321(7270):1226‐7. [PubMed] [Google Scholar]
Strunz 2014
- Strunz EC, Addiss DG, Stocks ME, Ogden S, Utzinger J, Freeman MC. Water, sanitation, hygiene, and soil‐transmitted helminth infection: a systematic review and meta‐analysis. PLoS Medicine 2014;11(3):e1001620. [DOI] [PMC free article] [PubMed] [Google Scholar]
Taylor‐Robinson 2017
- Taylor‐Robinson D, Garner P. Campbell replication confirms little or no effect of community deworming (comment). Lancet Global Health 2017;5(1):PE2‐e3. [DOI: 10.1016/S2214-109X(16)30289-3] [DOI] [PubMed] [Google Scholar]
Vos 2015
- Vos T, Barber RM, Bell B, Bertozzi‐Villa A, Biryukov S, Bolliger I, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015 Aug 22;386(9995):743–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
Welch 2016
- Welch VA, Awasthi S, Cumberbatch C, Fletcher R, McGowan J, Merritt K, et al. Deworming and adjuvant interventions for improving the developmental health and well‐being of children in low‐ and middle‐income countries. Campbell Review (https://campbellcollaboration.org/library/mass‐deworming‐interventions‐child‐health.html) 2016.
Welch 2017
- Welch VA, Ghogomu E, Hossain A, Awasthi S, Bhutta ZA, Cumberbatch C, et al. Mass deworming to improve developmental health and wellbeing of children in low‐income and middle‐income countries: a systematic review and network meta‐analysis. Lancet Global Health 2017;5(1):e40‐e50. [DOI: 10.1016/S2214-109X(16)30242-X] [DOI] [PubMed] [Google Scholar]
WHO 2002
- WHO Expert Committee on the Control of Schistosomiasis (2001: Geneva, Switzerland). Prevention and Control of Schistosomiasis and Soil‐transmitted Helminthiasis: Report of a WHO Expert Committee. WHO Technical Report Series no. 912. Geneva: World Health Organization, 2002. [PubMed] [Google Scholar]
WHO 2005
- World Health Organization. Strategy Development and Monitoring for Parasitic Diseases and Vector Control Team. Deworming: The Millennium Development Goals. The Evidence is in: Deworming Helps Meet the Millennium Development Goals [WHO/CDS/CPE/PVC/2005.12]. Geneva: World Health Organization, 2005. [Google Scholar]
WHO 2006a
- World Health Organization. WHO Essential Medicines Library. 2006. mednet3.who.int/emlib/ (accessed 13 June 2007).
WHO 2006b
- World Health Organization. Preventive chemotherapy in human helminthiasis. Coordinated use of anthelminthic drugs in control interventions: a manual for health professionals and programme managers. http://whqlibdoc.who.int/publications/2006/9241547103_eng.pdf. WHO, (accessed 11 July 2015).
WHO 2011
- World Health Organization. Helminth control in school‐age children. A guide for managers of control programmes. Second edition. http://whqlibdoc.who.int/publications/2011/9789241548267_eng.pdf (accessed 10 July 2015).
WHO 2015
- World Health Organization. e‐Library of Evidence for Nutrition Actions (eLENA). Deworming to combat the health and nutritional impact of helminth infections. www.who.int/elena/titles/deworming/en/ (accessed 18 May 2015).
WHO 2017a
- World Health Organization. Guideline: preventive chemotherapy to control soil‐transmitted helminth infections in at‐risk population groups. Geneva: World Health Organization; 2017. Licence: CC BY‐NC‐SA 3.0 IGO. www.who.int/nutrition/publications/guidelines/deworming/en/ (accessed prior to 20 August 2019). [PubMed]
WHO 2018a
- World Health Organization. Investing to overcome the global impact of neglected tropical diseases [Internet]. Available from www.who.int/neglected_diseases/9789241564861/en/ (accessed 12 September 2018).
WHO 2018b
- World Health Organization. London declaration on neglected tropical diseases [Internet]. www.who.int/neglected_diseases/London_Declaration_NTDs.pdf (accessed 18 September 2018).
World Bank 2003
- World Bank. School deworming. Public Health at a Glance; HNP notes. Washington, DC: World Bank. http://documents.worldbank.org/curated/en/902481468324576662/School‐deworming (accessed 10 July 2015).
References to other published versions of this review
Dickson 2000a
- Dickson RC, Awasthi S, Demellweek C, Williamson PR. Anthelmintic drugs for treating worms in children: effects on growth and cognitive performance. Cochrane Database of Systematic Reviews 2000, Issue 2. [DOI: 10.1002/14651858.CD000371] [DOI] [PubMed] [Google Scholar]
Dickson 2000b
- Dickson R, Awasthi S, Williamson P, Demellweek C, Garner P. Effects of treatment for intestinal helminth infection on growth and cognitive performance in children: systematic review of randomised trials. BMJ 2000;320(7251):1697‐701. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dickson 2007
- Dickson RC, Awasthi S, Demellweek C, Williamson PR. Anthelmintic drugs for treating worms in children: effects on growth and cognitive performance. Cochrane Database of Systematic Reviews 2007, Issue 4. [DOI: 10.1002/14651858.CD000371.pub2] [DOI] [PubMed] [Google Scholar]
Taylor‐Robinson 2007
- Taylor‐Robinson DC, Jones AP, Garner P. Deworming drugs for treating soil‐transmitted intestinal worms in children: effects on growth and school performance. Cochrane Database of Systematic Reviews 2007, Issue 4. [DOI: 10.1002/14651858.CD000371.pub3] [DOI] [PubMed] [Google Scholar]
Taylor‐Robinson 2012a
- Taylor‐Robinson DC, Maayan N, Soares‐Weiser K, Donegan S, Garner P. Deworming drugs for soil‐transmitted intestinal worms in children: effects on nutritional indicators, haemoglobin and school performance. Cochrane Database of Systematic Reviews 2012, Issue 7. [DOI: 10.1002/14651858.CD000371.pub4] [DOI] [PubMed] [Google Scholar]
Taylor‐Robinson 2012b
- Taylor‐Robinson DC, Maayan N, Soares‐Weiser K, Donegan S, Garner P. Deworming drugs for soil‐transmitted intestinal worms in children: effects on nutritional indicators, haemoglobin and school performance. Cochrane Database of Systematic Reviews 2012, Issue 11. [DOI: 10.1002/14651858.CD000371.pub5] [DOI] [PubMed] [Google Scholar]
Taylor‐Robinson 2015
- Taylor‐Robinson DC, Maayan N, Soares‐Weiser K, Donegan S, Garner P. Deworming drugs for soil‐transmitted intestinal worms in children: effects on nutritional indicators, haemoglobin, and school performance. Cochrane Database of Systematic Reviews 2015, Issue 7. [DOI: 10.1002/14651858.CD000371.pub6] [DOI] [PMC free article] [PubMed] [Google Scholar]


