Abstract
Objectives:
This study aims to investigate the effects of adding whole-body vibration (WBV) exercise to squat training (ST) on the physical function and muscle strength of patients with knee osteoarthritis (KOA).
Methods:
41 participants completed the intervention and measurements (ST group; n=21, age=65.00±4.39 years, BMI=23.01±2.95 kg/m2; WBV+ST group; n=20, age=64.10±4.95 years, BMI=24.79±3.12 kg/m2). The supervised eight-week intervention was performed three times per week with the intensity and duration increased gradually. Visual analog scale, Timed Up and Go test (TUG), 6-min Walk Distance test, and isokinetic measurements were performed at baseline and post-intervention.
Results:
The peak torque (PT) of the extensors at 180°/s increased significantly in the WBV+ST group compared with the ST group (p = 0.046). The peak work of the extensors and the PT of the flexors at 180°/s improved only in the WBV+ST group (p<0.0125). However, no significant changes in these variables were found between groups (p>0.05).
Conclusions:
Adding 8 weeks of WBV training to ST can more effectively improve the muscular strength of knee extensors compared with ST in patients with KOA.
Keywords: Knee Osteoarthritis, Whole-Body Vibration, Muscle Strength, Physical Function, Squat Training
Introduction
Osteoarthritis (OA) is a common musculoskeletal disease that causes pain, disability, and socioeconomic costs in the aging population worldwide[1,2]. The prevalence of OA is rising and will continue to increase within decades because of the longevity and increasing prevalence of obesity[3]. Usually defined as a degenerative, noninfectious knee joint disease, knee osteoarthritis (KOA) is the most common type of OA[4]. Patients with KOA often suffer from knee pain, stiffness, swelling, loss of mobility, and impaired physical functions[5]. Currently, no cure has been known in treatment of KOA. The optimal management offered to patients with mild to moderate KOA involves a combination of pharmacological and non-pharmacological treatments, which aim at pain relief, joint integrity maintenance, and physical function improvement[6]. Recently, several clinical guidelines for KOA, such as the American College of Rheumatology and Osteoarthritis Research Society, have suggested that the core treatment for this disease is education and exercise[6-8].
Exercise has been extensively investigated as an important rehabilitation therapy affecting disease state[3,9]. It has be widely accepted that quadriceps weakness is one of the risk factors for KOA[10,11]. Higher baseline of quadriceps strength might contribute to the decrease in knee pain and narrowing of knee joint space[10,12]. In addition, the movement of knee joint is a compound movement with multiple activity centers. The function of muscles around the knee joint is a key factor contributing to the balance of joint stress. Therefore, as an important element around the knee, quadriceps weakness contributes to knee joint instability, which changes the alignment and stress of the knee and accelerates knee OA progression[13]. Several studies about strength training for the lower limbs has been found to reduce pain and improve physical function in patients with KOA[14,15].
Whole-body vibration (WBV) training is a new modality in muscle strength training[16]. It has also been proposed as a physiotherapy for musculoskeletal system diseases, such as low back pain, osteoporosis, and chronic Achilles tendonitis[17,18]. However, the mechanism underlying the effects of WBV training on muscle strength, physical function, and pain in patients with KOA remains unclear. Several researchers speculated that WBV training improves neuromuscular function to gain physical function and muscle strength. Vibration may activate the muscle spindles, mediate the neural signals via the Ia afferents, and activate muscle fibers via large α-motor neurons called “tonic vibration reflex,” resulting in a reflexive improvement in the recruitment of motor units[19]. During WBV exercise, the force is adjusted by acceleration, but the force in conventional squat training (ST) is simply adjusted by mass, which contributes to muscle strength gain[20]. Therefore, WBV training might change the alignment and stress of the knee and consequently influence knee joint instability and pain.
Recent studies have considered WBV training as an efficient and alternative treatment for patients with KOA[21,22]. However, few clinical trials focused on the effects of WBV training on the pain, functional performance, and knee muscle strength of patients with KOA; moreover, their results showing the superiority of WBV training to other forms of exercise are inconclusive[20,23]. Wang et al. reported improved functional performance but not pain relief or improved self-reported disease state in patients performing WBV training in addition to quadriceps strength training compared with patients performing quadriceps strength training only[24]. Several studies failed to find significant improvements in pain intensity and functional performance[4,25]. Positive results on pain relief and disease state have also been reported[20,26]. The inconsistent results of previous studies hinder the validation of the effects of WBV training on the knee pain, disease state, physical function, and muscle strength of patients with KOA.
Therefore, the present study investigated the effects of adding WBV to ST on the knee pain, physical function, and muscle strength of patients with KOA in comparison with ST alone. We hypothesized that the WBV plus ST program was more effective than ST for relieving pain and improving the disease state, physical function, and muscle strength of patients with KOA.
Materials and methods
This study was a single-center, single-blind randomized controlled trial with blinded outcome assessment. Participants with mild to moderate KOA (Lequesne knee score=1 to 7) were recruited from community centers in Yangpu District, Shanghai, China. This study was conducted at the Sport Medicine and Rehabilitation Center, Shanghai University of Sport. It was approved by the Ethics Committee of the Shanghai University of Sport (Ref. No.: 2016-016). This trial was registered at Chinese Clinical Trial Registry a priori as a clinical trial (ID: ChiCTR-IOR-16009234).
Power analysis with settings of α=0.05, power (1-β)= 0.80, and effect size=0.25 showed that two groups of 34 participants totally were the required sample size. In addition, a sample size of approximately 20 participants in each group was usually reported in previous related studies. Given the dropouts, we recruited 60 participants for the research. Prior to the initiation of the study, all participants completed a questionnaire to obtain demographic details, including medical history. The participants were diagnosed with KOA by an orthopedic surgeon on the basis of their medical history, X-ray imaging, and physical assessment. Before inclusion in the study, all participants were requested to sign an informed consent.
Participants who met the inclusion criteria and consented to participate were randomly allocated to the intervention groups via computer-generated randomization by the research designer. Allocation was concealed by using sealed, opaque envelopes. The same physical therapist took charge of the interventions for the two groups. Only the research designer and trainers knew the randomized assignments. The assessors were blinded to the randomization and were not involved in the exercise interventions. The assessments were performed at two points: before the intervention and after the 8-week intervention.
Eligibility criteria
Participant selection was based on the classification criteria of the American Rheumatism Association for KOA[27]. Inclusion criteria of participants were as follows: 50-70 years of age, diagnosed as KOA (unilateral or bilateral) according to radiography, pain symptoms for at least 3 months, and mild to moderate KOA based on Lequesne knee score[24,28]. Participants who met the following criteria were excluded: acute symptomatic OA; underwent knee surgery in the past 6 months; diagnosed with other muscular, joint, or neurological conditions that affect the lower limb function; diagnosed with Alzheimer’s disease, Parkinson’s disease, or motor neuron disorders; and currently undertaking a structured exercise program for KOA[24].
Intervention
All interventions were delivered by the same certified physical therapist who had more than 3 years of practical experience in WBV training and ST. Each training session comprised a 5 min warm-up, WBV+ ST or ST, and 5 min cool-down.
WBV+ST group
Participants in the WBV +ST group attended the training program 3 days per week with at least 1 day between each session for 8 weeks. Training was conducted using a vibration device (Sport Platform, i-vib5050, BODYGREEN, China). All sessions were supervised by a physical therapist. TheraBand® resistance bands (The Hygenic Corporation, Akron, OH, USA) were used to prevent participants from falling backwards during training. Without being stretched, one side of the bands was tied to the handle of the platform, and the other side was held by the participants. The participants performed static ST on the vibration platform without shoes. The participants were instructed to flex their knee at 30° and 60° without knee varus. Before each training session, the physical therapist adjusted the angle of knee flexion with a goniometer. The distance between the feet was consistent with the shoulders. The training volume session was increased progressively over the 8-week intervention period by increasing the duration time, number of sets, and total time (Table 1)[29]. The vibration parameters were as follows: frequency of 20 Hz, amplitude of 2 mm, and vertical vibration.
Table 1.
The protocol of ST and WBV+ST intervention.
| Week of intervention | Knee flexion angle | Hold time | Rest time | Number of set | Total time |
|---|---|---|---|---|---|
| 1 | 30° | 30s | 30s | 6 | 12 min |
| 60° | 30s | 30s | 6 | ||
| 2 | 30° | 40s | 40s | 6 | 14 min |
| 60° | 30s | 30s | 6 | ||
| 3 | 30° | 40s | 40s | 7 | 17 min |
| 60° | 40s | 40s | 6 | ||
| 4 | 30° | 50s | 50s | 7 | 21 min |
| 60° | 40s | 40s | 7 | ||
| 5 | 30° | 50s | 50s | 8 | 25 min |
| 60° | 50s | 50s | 7 | ||
| 6 | 30° | 60s | 60s | 8 | 29 min |
| 60° | 50s | 50s | 8 | ||
| 7 | 30° | 60s | 60s | 9 | 34 min |
| 60° | 60s | 60s | 8 | ||
| 8 | 30° | 70s | 70s | 9 | 39 min |
| 60° | 60s | 60s | 9 |
ST, squat training; WBV+ST, whole body vibration + squat training.
ST group
Participants in the ST group attended the training program 3 days per week with at least 1 day between each session for 8 weeks. All sessions were under the supervision of the same physical therapist in the WBV+ST group. Participants performed static ST on flat ground without exposure to vibration. The resistance bands were tied to a fixture differently and used the same as in the WBV+ST group. Duration, set, posture of training, and total training time were the same as those in the WBV group (Table 1).
Outcome measures
All research measures were performed by assessors at baseline and 8 weeks in a blinded manner. Demographic information of the participants was obtained at baseline, which included sex, age, weight, height, body mass index (BMI), and affected side. Each test was conducted by the same assessor. In addition, only the participants who completed intervention sessions were included to perform post measurement.
Self-reported knee pain
A 10-cm visual analog scale (VAS) was used to assess self-reported pain of the affected side over the last week. The number 0 indicated no pain, whereas 10 represented maximal pain.
Physical performance measures
The Timed Up and Go test (TUG) was administered to determine the lower-extremity function performance of the patients with KOA. TUG is a simple test that has been proven reliable and valid in the KOA study[30]. The test was conducted as follows: participants stood up from a standard chair (40 cm height), walked 3 m, turned around, walked back, and sat down again. The participants were asked to perform the task as far as possible. The entire walking test was timed using a chronograph (in seconds). The test was performed three times, and the mean of three tests was recorded for analysis.
The 6-min Walk Distance test (6MWD), which is an easy and reliable method used in KOA trials, was used to evaluate the walking ability of the patients with KOA. The distance walked in 6 min was recorded for analysis (in meters).
Knee extensor and flexor strength
The knee extensor and flexor strength of the affected knee joint was measured using an isokinetic dynamometer (Physiomed, CON-TREX, TP 1000, Germany). At first, the assessor secured the participants to the device with Velcro straps at the upper chest, pelvis, and distal femur on the tested side. The participants were asked to perform a 5-min warm-up on treadmills before the formal test. In addition, they were instructed to familiarize with the test procedure through three submaximal contractions before each assessment. In isokinetic muscle test at velocities of 90°/s and 180°/s, the participants performed maximal concentric knee extension-flexion contractions from 80° to 10° of flexion considering 0° the full extension, totaling an active amplitude of 70°. The assessor verbally encouraged the participants to flex and extend the knee joint as forceful as possible. Three maximum concentric contractions for the knee extensors and flexors were performed at an angular velocity of 90°/s. After normalizing by kilogram of body mass, the highest peak torque and peak work (PT and PW, Nm/kg and W/kg, respectively) were used for analysis.
The dynamic endurance of knee extensors and flexors was assessed by using 10 repeated maximum isokinetic contractions at an angular velocity of 180°/s. The Endurance Index of the knee extensor and flexor was defined as the ratio of work performed during the last three contractions over the first three contractions.
The maximum concentric contractions for the knee extensors and flexors at an angular velocity of 180°/s were used for analysis after normalization.
Statistical analysis
SPSS for Windows version 20.0 (IBM Inc. Chicago, IL, USA) was used for statistical analysis. The data were presented as mean±SD. The chi-squared test and student’s t-test were used to determine the difference in demographic characteristics and disease state between the ST and WBV+ST groups. Two-way repeated measures ANOVA was used to determine the difference in outcomes between the two groups. The effect size of between-group effect was calculated by partial eta-square. Significance was set at p<0.05. The paired t-test was performed to test the difference of outcomes within each group. For within-group effect by t-test, the significance was corrected at p<0.0125.
Results
The demographic characteristics of the participants at baseline are shown in [Table 2]. The final sample consisted of 41 participants (n=20 in the WBV+ST group and n=21 in the ST group) (Figure 1). No significant difference in age, sex, height, weight, BMI, VAS, and disease severity was found between the groups. Moreover, no significant difference was found at pre-intervention assessment of all outcomes between groups.
Table 2.
Demographic characteristics of pariticants at baseline.
| Variable | ST (n=21) | WBV+ST (n=20) | P-value |
|---|---|---|---|
| Age (y) | 65.00±4.39 | 64.10±4.95 | 0.541 |
| Sex, M/F, (n) | 1/20 | 4/16 | 0.184 |
| Height (cm) | 157.81±5.59 | 157.79±7.04 | 0.992 |
| Weight (kg) | 57.39±8.59 | 61.72±8.73 | 0.117 |
| BMI (kg/m2) | 23.01±2.95 | 24.79±3.12 | 0.067 |
| VAS | 3.24±2.66 | 3.70±2.34 | 0.560 |
| Lequesne & Mery index # | 12/9/0/0/0 | 12/8/0/0/0 | 0.853 |
ST, squat training; WBV+ST, whole body vibration + squat training; BMI, body mass index; #, Disease severity: mild/ moderate/ severe/very severe/ extremely severe.
Figure 1.
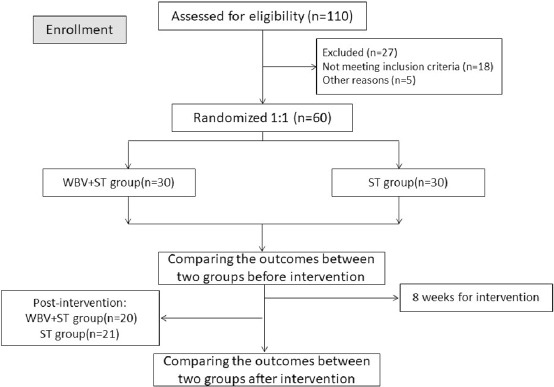
Flowchart of study patients.
Self-reported knee pain
The effects on VAS of the affected side did not differ significantly between groups and within each group (Within-group, F=14.408, p=0.001; Interaction, F=1.814, p=0.186; Between-group, F=0.001, p=0.998).
Physical performance measures
[Table 3] shows the differences in TUG and 6MWD of the participants at pre-intervention and post-intervention between the ST and WBV+ST groups. No significant difference was found in the TUG results between the ST and WBV+ST groups (Within-group, F=36.791, p<0.001; Interaction, F=3.846, p=0.057; Between-group, F=0.127, p=0.723). As for the 6MWD results, the distance that the participants walked in 6 min in both groups did not increase significantly compared with the baseline (ST, p>0.0125; WBV+ST, p>0.0125), and no significant difference was observed between the ST and WBV+ST groups (Within-group, interaction and between-group effect, p>0.05).
Table 3.
Differences in TUG and 6MWD at pre-intervention and post-intervention.
| ST(n=21) | WBV+ST (n=20) | Within-group | Interaction | Between-group | Effect Size | Power | ||
|---|---|---|---|---|---|---|---|---|
| TUG (second) | Pre-intervention | 7.01±0.61 | 7.14±0.63 | 0.001 | 0.06 | 0.72 | 0.003 | 0.064 |
| Post-intervention | 6.58±0.77 | 6.30±0.84 | ||||||
| 6MWD (meter) | Pre-intervention | 529.10±49.82 | 518.25±57.18 | 0.02 | 0.72 | 0.28 | 0.029 | 0.19 |
| Post-intervention | 576.90±100.70 | 554.25±70.49 |
ST, squat training; WBV+ST, whole body vibration + squat training.
Knee extensor and flexor strength
[Table 4, Figures 2 and 3] show the change in knee extensor and flexor strength at each angular velocity in both groups. The PT and PW values of the knee extensors and flexors at 90°/s did not change significantly between groups (Within-group, interaction and between-group effect of four indexes, p>0.05) (Figure 2). At an angular velocity of 180°/s, only the PT of the knee extensors increased significantly in the WBV+ST group compared with the ST group (Within-group, F=9.432, p=0.004; Interaction, F=17.168, p<0.001; Between-group, F=4.245, p=0.046) (Figure 3). No difference in the PW of the knee extensors, PT of the knee flexors, and PW of the knee flexors was found between the two groups. However, the paired-t test was conducted because of the interaction effect found in these indexes. The PW of the knee extensors and PT of the knee flexors at 180°/s increased significantly in the WBV+ST group (PW of extensors, p=0.005; mean difference= -0.48±0.68; 95% CI, -0.80 to -0.16; PT of flexors, p=0.010; mean difference= 0.13±0.20; 95% CI, 0.03 to 0.22). These outcomes of muscle strength in the ST group did not change significantly within and between groups.
Table 4.
Differences in knee extensors and flexors strength at pre-intervention and post-intervention.
| ST(n=21) | WBV+ST (n=20) | Within-group | Interaction | Between-group | Effect Size | Power | ||
|---|---|---|---|---|---|---|---|---|
| PT(Nm/kg), Extensor, 90°/s | Pre-intervention | 0.68±0.26 | 0.77±0.30 | 0.762 | 0.684 | 0.145 | 0.055 | 0.305 |
| Post-intervention | 0.67±0.24 | 0.79±0.20 | ||||||
| PT(Nm/kg), Extensor, 180°/s | Pre-intervention | 0.50±0.15 | 0.48±0.21 | 0.004 | 0.001 | 0.046 | 0.100 | 0.519 |
| Post-intervention | 0.47±0.17 | 0.72±0.27* | ||||||
| PT(Nm/kg), Flexors, 90°/s | Pre-intervention | -0.39±0.15 | -0.41±0.14 | 0.917 | 0.300 | 0.187 | 0.045 | 0.258 |
| Post-intervention | -0.36±0.23 | -0.45±0.18 | ||||||
| PT(Nm/kg), Flexors, 180°/s | Pre-intervention | -0.29±0.11 | -0.30±0.16 | 0.007 | 0.021 | 0.119 | 0.063 | 0.344 |
| Post-intervention | -0.30±0.11 | -0.43±0.19* | ||||||
| PW(J/kg), Extensor, 90°/s | Pre-intervention | 1.06±0.42 | 1.21±0.48 | 0.201 | 0.187 | 0.057 | 0.109 | 0.557 |
| Post-intervention | 1.06±0.38 | 1.45±0.65 | ||||||
| PW(J/kg), Extensor, 180°/s | Pre-intervention | 1.54±0.52 | 1.50±0.67 | 0.034 | 0.002 | 0.164 | 0.050 | 0.282 |
| Post-intervention | 1.45±0.54 | 1.98±0.76* | ||||||
| PW(J/kg), Flexors, 90°/s | Pre-intervention | 0.61±0.24 | 0.65±0.22 | 0.057 | 0.122 | 0.080 | 0.079 | 0.419 |
| Post-intervention | 0.64±0.20 | 0.86±0.45 | ||||||
| PW(J/kg), Flexors, 180°/s | Pre-intervention | 0.90±0.35 | 0.92±0.49 | 0.014 | 0.061 | 0.240 | 0.036 | 0.214 |
| Post-intervention | 0.94±0.36 | 1.21±0.50 | ||||||
| EI, Extensor, 180°/s | Pre-intervention | 0.84±0.39 | 0.89±0.36 | 0.841 | 0.298 | 0.062 | 0.089 | 0.466 |
| Post-intervention | 0.77±0.16 | 0.98±0.32 | ||||||
| EI, Flexors, 180°/s | Pre-intervention | 0.80±0.62 | 0.88±0.50 | 0.613 | 0.857 | 0.238 | 0.025 | 0.162 |
| Post-intervention | 0.73±0.15 | 0.85±0.32 |
ST, squat training; WBV+ST, whole body vibration + squat training; PT, peak torque; PW, peak power; EI, endurance index;
p < 0.0125, changed diffenertly compared with pre-intervention.
Figure 2.
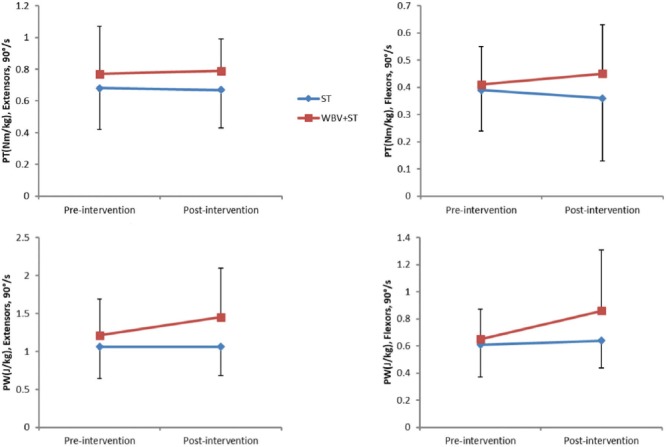
Changes in PT and PW of the knee extensor and flexor at 90°/s over time in each group. WBV+ST, whole body vibration + squat training group; ST, squat training group; PT, peak torque; PW, peak work.
Figure 3.
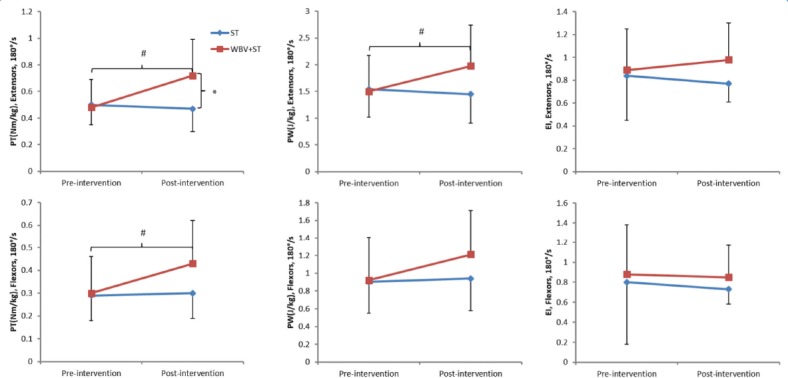
Changes in PT, PW, and EI of the knee extensor and flexor at 180°/s over time in each group. WBV+ST, whole body vibration + squat training group; ST, squat training group; PT, peak torque; PW, peak work; EI, endurance index; #, p < 0.0125 compared with baseline; *, p < 0.05 between groups.
Discussion
This study determined the effects of adding WBV training to ST on the knee pain, physical function, and muscle strength of patients with KOA and compared these effects with those of ST. Results showed that 8-week additional WBV training was more effective in improving knee extensor muscular performance in terms of PT at an angular velocity of 180°/s compared with ST.
Given its feasibility and safety, WBV training is recommended by physiotherapists as an alternative treatment to improve the physical function and self-reported disease status of individuals with KOA. However, previous randomized controlled studies found that the treatment effects of WBV training on KOA are limited and inconclusive compared with other modes of training. Wang et al.[31] found that 24-week WBV offers additional effects on knee pain, self-reported disease state, range of motion, and muscle strength in patients with KOA compared with quadriceps resistance exercise. Tsuji et al. found that WBV training improves self-reported knee function and knee physical function in KOA[20]. However, several studies failed to find significant improvements in pain intensity, self-reported disease state, and functional performance in KOA[4,32]. Considering the lack of guidelines for optimal protocol of WBV training for knee OA, previous studies employed different parameters, such as frequency, amplitude, duration, posture of WBV training, and vibration device. The different outcome measurements also affected the results of previous studies. For example, in the study by Trans et al., the participants trained on different vibration devices gained different physical functions. Muscle strength increased in the stable platform group, whereas proprioception improved in the balance platform group[29]. The frequency of WBV training also influences the physical function. Tseng et al. found that WBV training in low frequency (20 Hz) significantly improves balance performance compared with no vibration and high frequency (40 Hz)[33].
In the current study, the 8-week WBV+ST exercise was not superior to ST in providing pain relief. Consistent with the present study, several meta-analyses[21,25] found that WBV training is not superior to other forms of exercise in decreasing pain intensity or improving self-reported disease status. The relatively short duration (8 weeks) of the intervention program used in our study might have not affected the self-reported pain state of the patients with KOA.
In addition, the 8-week additional WBV training did not lead to a superior effect to ST in TUG and 6MWD. One possible reason for the negative result on physical function may be that the duration of WBV training used in our study was not enough to cause a significant difference between the two groups. Moreover, the parameters of WBV training used in our study were as follows: frequency of 20 Hz and amplitude of 2 mm displacement. In previous studies, the frequencies of 20-35 Hz and amplitudes of 2-4 mm were applied[4,20,29,31]. Another possibility may be that the parameters of WBV intervention were insufficient to improve the physical function significantly. WBV training at higher intensity or longer duration might provide significant effects in patients with KOA.
The effects of WBV exercise over other forms of exercise on muscular strength are inconsistent. Wang et al. found that after 12-week intervention, the WBV exercise offers superior improvement in knee extensor strength tested by a hand-held dynamometer compared with other exercises[31]. Previous studies that assessed muscle strength using isokinetic dynamometry concluded that WBV exercise offers a positive effect on knee extensor strength, which is consistent with our study[29,34]. By contrast, Tsuji et al. indicated that the isokinetic knee extension/flexion PT and average power at a velocity of 60°/s in patients with KOA do not significantly increase after 8 weeks of WBV compared with the control group without vibration exposure[20]. However, the participants in Tsuji et al.’s study were not allocated randomly and not limited based on disease state, which might have affected the results. In addition, the treatment dosage and participant age differed in previous studies[4,24,26]. The authors concluded that the difference in muscle strength measurements, treatment dosage, participant age, and disease severity may have caused the inconsistent conclusions.
Currently, the mechanism of muscle strength gain in the WBV group is not clear. Vibration may activate the muscle spindles, mediate the neural signals via the Ia afferents, and activate muscle fibers via large α-motor neurons called “tonic vibration reflex,” resulting in a reflexive improvement in the recruitment of motor units[19]. Another explanation may be the acceleration caused by the vibration platform. During the WBV exercise, the force is adjusted by acceleration, but the force in conventional ST is simply adjusted by mass[20]. Pamukoff et al.[35] reported that one session of vibration stimulation acutely improves quadriceps strength, voluntary activation, and corticomotor excitability in patients who underwent anterior cruciate ligament reconstruction. They speculated that the effects of WBV exercise on quadriceps function might be derived from enhanced corticomotor excitability.
Limitations
Generalization of the present results has several limitations. First, the parameters of the vibration program differed among previous studies in terms of duration, total time of vibration exposure, and frequency. The program is limited to compare the effects of WBV exercise with other previous studies. Comparing the treatment effect from either intervention is difficult without a true control group. In addition, about 30% of the participants did not complete the intervention. Nine participants in the ST group and ten participants in the WBV group dropped out, which reduced the sample size of this study. After analysis, the withdrawal of subjects was mainly due to personal or family reasons (such as babysitting or other housework). In addition, the intervention of WBV training and ST was supervised by physiotherapists independently, which failed to increase the enthusiasm of the participants. In future studies, the researchers should pay attention to the diversity and attractiveness of the intervention to avoid the high dropout rate. In this study, the disease state of the participants with KOA was not evaluated by the researchers after the intervention. Thus, the effect of WBV on KOA incidence or progression was not explored.
Conclusion
The current study showed the superiority of the 8-week additional WBV exercise over ST on muscle strength gain in patients with KOA. Our findings show the potential benefits of adding WBV exercise to ST on pain relief and knee extensor strength gain for KOA. Therefore, adding WBV exercise to ST may be an effective intervention to improve muscle strength around the knee for individuals with KOA.
Acknowledgements
The authors certify that they have no affiliations with or financial involvement in any organization or entity with a direct financial interest in the subject matter or materials discussed in the article. This work was supported by the Shanghai Committee of Science and Technology (No. 14490503800) and the National Natural Science Fund of China (No. 11572202).
Footnotes
The authors have no conflict of interest.
Edited by: G. Lyritis
Author contributions
ZL and LW contributed to the conception and design of the trial and drafted the manuscript. ZL and SL participated in trial registration, communication, and monitoring. LW, ZL and XY participated in the statistical analysis design. All authors read and approved the final version of the manuscript.
References
- 1.Bijlsma JW, Berenbaum F, Lafeber FP. Osteoarthritis:an update with relevance for clinical practice. Lancet. 2011;377(9783):2115–26. doi: 10.1016/S0140-6736(11)60243-2. [DOI] [PubMed] [Google Scholar]
- 2.Glyn-Jones S, Palmer AJ, Agricola R, Price AJ, Vincent TL, et al. Osteoarthritis. Lancet. 2015;386(9991):376–87. doi: 10.1016/S0140-6736(14)60802-3. [DOI] [PubMed] [Google Scholar]
- 3.Schiphof D, van den Driest JJ, and Runhaar J. Osteoarthritis year in review 2017:rehabilitation and outcomes. Osteoarthritis Cartilage. 2018;26(3):326–340. doi: 10.1016/j.joca.2018.01.006. [DOI] [PubMed] [Google Scholar]
- 4.Park YG, Kwon BS, Park JW, Cha DY, Nam KY, et al. Therapeutic effect of whole body vibration on chronic knee osteoarthritis. Ann Rehabil Med. 2013;37(4):505–15. doi: 10.5535/arm.2013.37.4.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heidari B. Knee osteoarthritis prevalence, risk factors, pathogenesis and features:Part I. Caspian J Intern Med. 2011;2(2):205–12. [PMC free article] [PubMed] [Google Scholar]
- 6.Hochberg MC, Altman RD, April KT, Benkhalti M, Guyatt G, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res. 2012;64(4) doi: 10.1002/acr.21596. [DOI] [PubMed] [Google Scholar]
- 7.McAlindon TE, Bannuru RR, Sullivan MC, Arden NK, Berenbaum F, et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage. 2014;22(3):363–88. doi: 10.1016/j.joca.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 8.Fernandes L, Hagen KB, Bijlsma JW, Andreassen O, Christensen P, et al. EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis. Ann Rheum Dis. 2013;72(7):1125–35. doi: 10.1136/annrheumdis-2012-202745. [DOI] [PubMed] [Google Scholar]
- 9.Nguyen C, Lefevre-Colau MM, Poiraudeau S, and Rannou F. Rehabilitation (exercise and strength training) and osteoarthritis:A critical narrative review. Ann Phys Rehabil Med. 2016;59(3):190–5. doi: 10.1016/j.rehab.2016.02.010. [DOI] [PubMed] [Google Scholar]
- 10.Segal NA, Glass NA, Torner J, Yang M, Felson DT, et al. Quadriceps weakness predicts risk for knee joint space narrowing in women in the MOST cohort. Osteoarthritis Cartilage. 2010;18(6):769–75. doi: 10.1016/j.joca.2010.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Takagi S, Omori G, Koga H, Endo K, Koga Y, et al. Quadriceps muscle weakness is related to increased risk of radiographic knee OA but not its progression in both women and men:the Matsudai Knee Osteoarthritis Survey. Knee Surg Sports Traumatol Arthrosc 2017. doi: 10.1007/s00167-017-4551-5. [DOI] [PubMed] [Google Scholar]
- 12.Amin S, Baker K, Niu J, Clancy M, Goggins J, et al. Quadriceps strength and the risk of cartilage loss and symptom progression in knee osteoarthritis. Arthritis Rheum. 2009;60(1):189–98. doi: 10.1002/art.24182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van der Esch M, Holla JF, van der Leeden M, Knol DL, Lems WF, et al. Decrease of muscle strength is associated with increase of activity limitations in early knee osteoarthritis:3-year results from the cohort hip and cohort knee study. Arch Phys Med Rehabil. 2014;95(10):1962–8. doi: 10.1016/j.apmr.2014.06.007. [DOI] [PubMed] [Google Scholar]
- 14.Imoto AM, Peccin MS, Trevisani VF. Quadriceps strengthening exercises are effective in improving pain, function and quality of life in patients with osteoarthritis of the knee. Acta Ortop Bras. 2012;20(3):174–9. doi: 10.1590/S1413-78522012000300008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Knoop J, Steultjens MP, Roorda LD, Lems WF, van der Esch M, et al. Improvement in upper leg muscle strength underlies beneficial effects of exercise therapy in knee osteoarthritis:secondary analysis from a randomised controlled trial. Physiotherapy. 2015;101(2):171–7. doi: 10.1016/j.physio.2014.06.002. [DOI] [PubMed] [Google Scholar]
- 16.Rees SS, Murphy AJ, Watsford ML. Effects of whole body vibration on postural steadiness in an older population. J Sci Med Sport. 2009;12(4):440–4. doi: 10.1016/j.jsams.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 17.Wysocki A, Butler M, Shamliyan T, and Kane RL. Whole-body vibration therapy for osteoporosis:state of the science. Ann Intern Med. 2011;155(10):680–6. doi: 10.7326/0003-4819-155-10-201111150-00006. W206-13. [DOI] [PubMed] [Google Scholar]
- 18.Horstmann T, Jud HM, Frohlich V, Mundermann A, and Grau S. Whole-body vibration versus eccentric training or a wait-and-see approach for chronic Achilles tendinopathy:a randomized clinical trial. J Orthop Sports Phys Ther, 2013;43(11):794–803. doi: 10.2519/jospt.2013.4762. [DOI] [PubMed] [Google Scholar]
- 19.De Gail P, Lance JW, and Neilson PD. Differential effects on tonic and phasic reflex mechanisms produced by vibration of muscles in man. J Neurol Neurosurg Psychiatry. 1966;29(1):1–11. doi: 10.1136/jnnp.29.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tsuji T, Yoon J, Aiba T, Kanamori A, Okura T, et al. Effects of whole-body vibration exercise on muscular strength and power, functional mobility and self-reported knee function in middle-aged and older Japanese women with knee pain. Knee. 2014;21(6):1088–95. doi: 10.1016/j.knee.2014.07.015. [DOI] [PubMed] [Google Scholar]
- 21.Wang P, Yang X, Yang Y, Yang L, Zhou Y, et al. Effects of whole body vibration on pain, stiffness and physical functions in patients with knee osteoarthritis:a systematic review and meta-analysis. Clin Rehabil. 2015;29(10):939–51. doi: 10.1177/0269215514564895. [DOI] [PubMed] [Google Scholar]
- 22.Zafar H, Alghadir A, Anwer S, and Al-Eisa E. Therapeutic effects of whole-body vibration training in knee osteoarthritis:a systematic review and meta-analysis. Arch Phys Med Rehabil. 2015;96(8):1525–32. doi: 10.1016/j.apmr.2015.03.010. [DOI] [PubMed] [Google Scholar]
- 23.Segal NA, Glass NA, Shakoor N, Wallace R. Vibration platform training in women at risk for symptomatic knee osteoarthritis. PM R. 2013;5(3):201–9. doi: 10.1016/j.pmrj.2012.07.011. quiz 209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang P, Yang L, Li H, Lei Z, Yang X, et al. Effects of whole-body vibration training with quadriceps strengthening exercise on functioning and gait parameters in patients with medial compartment knee osteoarthritis:a randomised controlled preliminary study. Physiotherapy. 2016;102(1):86–92. doi: 10.1016/j.physio.2015.03.3720. [DOI] [PubMed] [Google Scholar]
- 25.Li X, Wang XQ, Chen BL, Huang LY, and Liu Y. Whole-Body Vibration Exercise for Knee Osteoarthritis:A Systematic Review and Meta-Analysis. Evid Based Complement Alternat Med. 2015;2015:758147. doi: 10.1155/2015/758147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Simao AP, Avelar NC, Tossige-Gomes R, Neves CD, Mendonca VA, et al. Functional performance and inflammatory cytokines after squat exercises and whole-body vibration in elderly individuals with knee osteoarthritis. Arch Phys Med Rehabil. 2012;93(10):1692–700. doi: 10.1016/j.apmr.2012.04.017. [DOI] [PubMed] [Google Scholar]
- 27.Altman R, Asch E, Bloch D, Bole G, Borenstein D, et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum. 1986;29(8):1039–49. doi: 10.1002/art.1780290816. [DOI] [PubMed] [Google Scholar]
- 28.Lin DH, Lin CH, Lin YF, Jan MH. Efficacy of 2 non-weight-bearing interventions, proprioception training versus strength training, for patients with knee osteoarthritis:a randomized clinical trial. J Orthop Sports Phys Ther. 2009;39(6):450–7. doi: 10.2519/jospt.2009.2923. [DOI] [PubMed] [Google Scholar]
- 29.Trans T, Aaboe J, Henriksen M, Christensen R, Bliddal H, et al. Effect of whole body vibration exercise on muscle strength and proprioception in females with knee osteoarthritis. Knee. 2009;16(4):256–61. doi: 10.1016/j.knee.2008.11.014. [DOI] [PubMed] [Google Scholar]
- 30.Steffen TM, Hacker TA, Mollinger L. Age- and gender-related test performance in community-dwelling elderly people:Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds. Phys Ther. 2002;82(2):128–37. doi: 10.1093/ptj/82.2.128. [DOI] [PubMed] [Google Scholar]
- 31.Wang P, Yang L, Liu C, Wei X, Yang X, et al. Effects of Whole Body Vibration Exercise associated with Quadriceps Resistance Exercise on functioning and quality of life in patients with knee osteoarthritis:a randomized controlled trial. Clin Rehabil. 2016;30(11):1074–1087. doi: 10.1177/0269215515607970. [DOI] [PubMed] [Google Scholar]
- 32.Avelar NC, Simao AP, Tossige-Gomes R, Neves CD, Rocha-Vieira E, et al. The effect of adding whole-body vibration to squat training on the functional performance and self-report of disease status in elderly patients with knee osteoarthritis:a randomized, controlled clinical study. J Altern Complement Med. 2011;17(12):1149–55. doi: 10.1089/acm.2010.0782. [DOI] [PubMed] [Google Scholar]
- 33.Tseng SY, Hsu PS, Lai CL, Liao WC, Lee MC, et al. Effect of Two Frequencies of Whole-Body Vibration Training on Balance and Flexibility of the Elderly:A Randomized Controlled Trial. Am J Phys Med Rehabil. 2016;95(10):730–7. doi: 10.1097/PHM.0000000000000477. [DOI] [PubMed] [Google Scholar]
- 34.Bokaeian HR, Bakhtiary AH, Mirmohammadkhani M, Moghimi J. The effect of adding whole body vibration training to strengthening training in the treatment of knee osteoarthritis:A randomized clinical trial. J Bodyw Mov Ther. 2016;20(2):334–40. doi: 10.1016/j.jbmt.2015.08.005. [DOI] [PubMed] [Google Scholar]
- 35.Pamukoff DN, Pietrosimone B, Lewek MD, Ryan ED, Weinhold PS, et al. Whole-Body and Local Muscle Vibration Immediately Improve Quadriceps Function in Individuals With Anterior Cruciate Ligament Reconstruction. Archives Of Physical Medicine And Rehabilitation. 2016;97(7):1121–1129. doi: 10.1016/j.apmr.2016.01.021. [DOI] [PubMed] [Google Scholar]


