Abstract
Abstract
Background: Childhood undernutrition causes significant morbidity and mortality in low- and middle-income countries (LMICs). In Tanzania, the in-hospital prevalence of undernutrition in children under five years of age is approximated to be 30% with a case fatality rate of 8.8%. In Tanzania, the burden of undernourished children under five years of age presenting to emergency departments (EDs) and their outcomes are unknown. This study describes the clinical profiles and outcomes of this population presenting to the emergency department of Muhimbili National Hospital (ED-MNH), a large, urban hospital in Dar es Salaam, Tanzania.
Methods
This was a prospective descriptive study of children aged 1–59 months presenting to the ED-MNH over eight weeks in July and August 2016. Enrolment occurred through consecutive sampling. Children less than minus one standard deviation below World Health Organization mean values for Weight for Height/Length, Height for Age, or Weight for Age were recruited. Structured questionnaires were used to document primary outcomes of patient demographics and clinical presentations, and secondary outcomes of 24-h and 30-day mortality. Data was summarised using descriptive statistics and relative risks (RR).
Results
A total of 449 children were screened, of whom 34.1% (n = 153) met criteria for undernutrition and 95.4% (n = 146) of those children were enrolled. The majority of these children, 56.2% (n = 82), were male and the median age was 19 months (IQR 10–31 months). They presented most frequently with fever 24.7% (n = 36) and cough 24.0% (n = 35). Only 6.7% (n = 9) were diagnosed with acute undernutrition by ED-MNH physicians. Mortality at 24 h and 30 days were 2.9% (n = 4) and 12.3% (n = 18) respectively. A decreased level of consciousness with Glasgow Coma Scale below fifteen on arrival to the ED and tachycardia from initial vital signs were found to be associated with a statistically significant increased risk of death in undernourished children, with mortality rates of 16.1% (n = 23), and 24.6% (n = 35), respectively.
Conclusions
In an urban ED of a tertiary referral hospital in Tanzania, undernutrition remains under-recognized and is associated with a high rate of in-hospital mortality.
Keywords: Emergency department, Malnutrition, Paediatrics, Sub-Saharan Africa
Background
Childhood undernutrition is a common and serious health problem affecting children under the age of 5 years [1, 2]. Undernutrition is a devastating condition which affects the entire body; this predisposes children to opportunistic infections and severe illness. Acute undernutrition is known to be complicated by life-threatening medical conditions such as dehydration and shock, hypoglycaemia, hypothermia, electrolyte abnormalities, and micronutrient deficiencies [3–5].
In low- and middle-income countries (LMICs), children have high rates of undernutrition, and there are several identified risk factors for undernutrition: unemployment, living in a rural area, poor hygiene, low levels of maternal education, long distances to health care, poor socio-economic status, a large number of siblings in the family, cessation of breastfeeding before six months, poor immunization history, unrepaired or undiagnosed congenital disease, and disease conditions such as HIV/AIDS [6, 7–9]. Most healthcare facilities in LMICs use the World Health Organization (WHO) recommended 10 step protocol [3] in the management of undernourished children [1, 4, 10, 11]. This protocol calls for prompt management of dehydration and/or shock, hypoglycaemia, and hypothermia, the treatment of infection, the correction of micronutrient deficiencies and electrolyte abnormalities, and the careful reintroduction of feeding, along with rehabilitation, emotional support, time for recovery, and a follow-up plan [3]. This WHO protocol has been shown to improve mortality rates of undernourished children under five years of age in LMICs [1, 11]. However, these guidelines focus on longitudinal hospital management, and the initial management of acutely ill undernourished children in EDs in LMICs remains variable in terms of care, resources, and local protocols [4, 11, 12].
In Tanzania, emergency medicine is a relatively new specialty and Muhimbili National Hospital (MNH) is the only public hospital with a full-capacity ED. In the ED-MNH, physicians have the resources for early recognition, stabilisation, treatment, and proper disposition of acutely ill undernourished children [13–15].
Prior to this study, the burden and outcomes of acutely ill undernourished children at the ED-MNH were unknown. We aimed to describe the clinical profiles and outcomes of these acutely ill, undernourished children under five years of age who presented to the ED-MNH. Our results provide an opportunity to begin to define the role of emergency medicine providers in the initial recognition and management of acutely ill, undernourished children.
Methods
Study design
This was a prospective descriptive study conducted from July 4, 2016 to August 31, 2016. Undernourished children aged 1–59 months presenting to the ED-MNH were included in our study after obtaining parental consent.
Study setting
MNH is located in the Ilala municipality in the city of Dar es Salaam and serves as the national tertiary referral hospital in Tanzania. It is the only public hospital with a full-capacity ED in the country. The ED-MNH opened in 2010 and is currently the only training site in Tanzania for the degree of Master of Medicine in Emergency Medicine. The ED-MNH sees 150 to 200 acutely ill patients (adults and children) each day, one fourth of whom are children under 18 years of age. There are dedicated paediatric treatment and resuscitation rooms where nurses, general practitioners, and resident physicians provide care that is overseen by emergency medicine physician specialists.
Sample size calculation
We calculated that a sample size of 135 subjects would allow us to characterize the mortality rate among our study population with a 95% confidence interval (CI). Our assumptions for this calculation were extrapolated from published data from Mwanza, Tanzania by Ngallaba et al. [1] that showed a case fatality rate of 8.8% amongst undernourished children. We further adjusted the sample size to account for up to a 10% loss to follow-up.
Study procedure
A consecutive sampling technique was used for enrolment. Paediatric patients aged between 4 weeks and 59 months presenting to the ED-MNH during pre-selected research shifts for 8 weeks were screened for undernutrition using the WHO Z-score criteria for undernutrition, which are Weight for Height/Length (WFH/WFL), Height for Age (HFA), or Weight for Age (WFA) less than one standard deviation (< −1SD) below established mean values. The most significant Z-score for each patient was used to classify the severity of their undernutrition [6]. The principal investigator or a trained research assistant initially obtained verbal consent from each parent/caregiver to screen children for eligibility. For those who were eligible, written consent was obtained. Patient demographics (age in months, sex, residences, and referral status), clinical presentation, physical exam findings, initial interventions, and outcomes were documented both from the caretaker interviews and the electronic medical record for all enrolled patients. The children’s body weights were measured using a standardised digital scale, heights were measured using a measurement height/length board in conscious children above two years, and length was measured in children less than two years and all unconscious children using a length board. Z-scores for WFH/WFL, HFA, and WFA were calculated and compared to the WHO standardised growth chart to interpret the severity of undernutrition. For each patient, their most significant Z-score was used to classify their undernutrition. They were classified as severe for a Z-score < − 3 SD, moderate for a Z-score between − 3 SD and < − 2 SD, and mild for a Z-score between − 2 SD and < − 1 SD. ED final diagnoses were recorded for all children enrolled in the study and all children were followed up through their hospital stay by evaluation of their medical records, and through direct cell phone calls to their caregivers at 24 h, 48 h, and 30 days after their ED visits to determine their outcome. ED providers were blinded to the study investigator’s findings.
Study outcomes
The primary outcomes included identifying the proportion of acutely ill children under five years of age presenting to the ED-MNH that were undernourished, establishing whether or not undernutrition was being documented as an ED physician diagnosis, and determining the in-ED mortality of undernourished children. Secondary outcomes included determining the 24-h, 48-h, 30-day, and overall hospital mortality of acutely ill children with undernutrition.
Data analysis
Data were analysed with StatsDirect version 3.0.133 (Stats Direct Ltd., Cheshire, UK). Descriptive statistics (counts, median, interquartile ranges and percentages) were generated for demographic characteristics, clinical features, and outcomes of patients in our study. Inter-group comparisons were made using the Chi Square or Fisher’s exact tests, relative risks, and 95% confidence intervals (CIs) [16]. Two-sided p-values < 0.05 were considered significant.
Results
Demographic characteristics and classification of undernourished children under five years of age
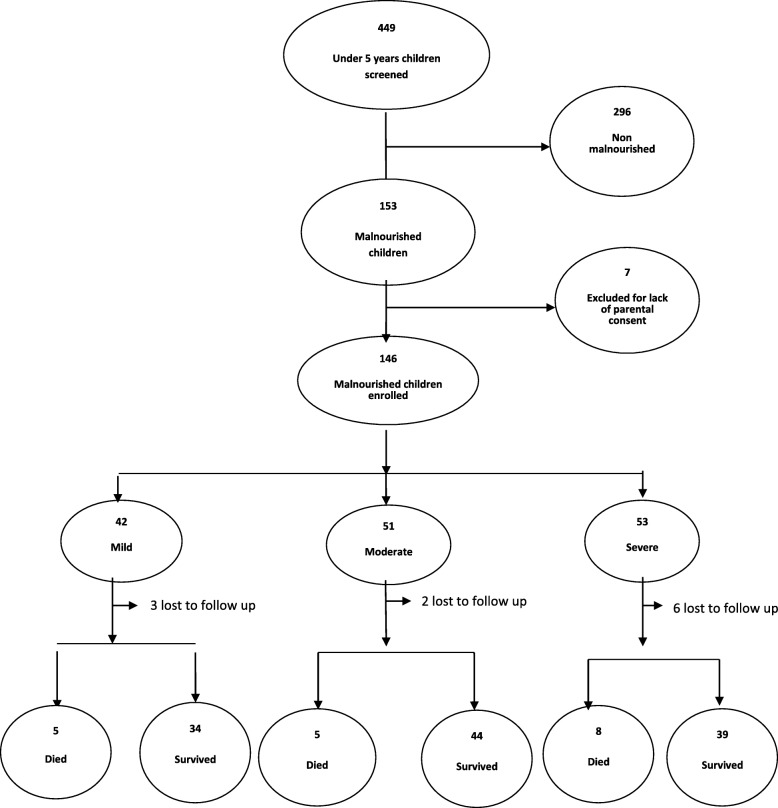
A total of 449 children under five years of age were screened throughout the eight-week study period; 34.1% (n = 153) were identified as undernourished. Among those children, parents of 95.4% (n = 146) consented to be in the study and were enrolled (Fig. 1). Among those enrolled, 28.8% (n = 42) had mild, 34.9% (n = 51) had moderate, and 36.3% (n = 53) had severe undernutrition.
Fig. 1.
The study flow chart showing the enrolment of children under five years of age, malnutrition classification, and their outcomes
The majority of children were male 56.2% (n = 85) with a median age of 19 months (IQR = 10–31 months). Almost one third, 31.5% (n = 46), were between one and twelve months of age. Most caretakers were biological mothers (90.4%, n = 132) and had at least primary school education (89%, n = 130). Low socioeconomic status (as evidenced by self-identification as peasants and/or housewives) was identified in 66.5% (n = 97) of caretakers. Most patients, 68.5% (n = 99), were referred from peripheral health facilities and 44.5% (n = 65) were ill for more than two weeks before presenting to the ED-MNH. The majority of patients, 65.1% (n = 95), resided in the city of Dar es Salaam (Table 1).
Table 1.
Demographic characteristics and classification of undernourished childrena
| Characteristics | Overall (N = 146) n (%) |
Mild (N = 42) n (%) |
Moderate(N = 51) n (%) |
Severe (N = 53) n (%) |
|---|---|---|---|---|
| Age in groups | ||||
| 1–12 month | 46 (31.5) | 8 (19.0) | 13 (25.5) | 25 (47.2) |
| 13–24 month | 39 (26.7) | 16 (38.1) | 16 (31.4) | 7 (13.2) |
| 25–36 month | 29 (19.9) | 6 (14.3) | 13 (25.5) | 10 (18.9) |
| 37–48 month | 20 (13.7) | 5 (11.9) | 7 (13.7) | 8 (15.1) |
| 49–59 month | 12 (8.2) | 7 (16.7) | 2 (3.9) | 3 (5.7) |
| Child’s sex | ||||
| Male | 82 (56.2) | 22 (52.4) | 31 (60.8) | 29 (54.7) |
| Duration of illness | ||||
| More than 2 weeks | 65 (44.5) | 18 (42.9) | 16 (31.4) | 31 (58.5) |
| Referred status | ||||
| Referred | 100 (68.5) | 31 (73.8) | 26 (51.0) | 43 (81.1) |
| Self referral | 46 (31.5) | 11 (26.2) | 25 (49.0) | 10 (18.9) |
| Residence | ||||
| Dar es Salaam | 95 (65.1) | 29 (69.0) | 36 (70.6) | 30 (56.6) |
| Other | 51 (34.9) | 13 (31.0) | 15 (29.4) | 23 (43.4) |
aZ-scores for WFH/WFL, HFA, and WFA were calculated and for each patient. The most severe Z-score for each child was used and interpreted as severe for a Z-score < −3 SD, moderate for a Z-score between − 3 SD and < − 2 SD, and mild for a Z-score between − 2 SD and < − 1 SD
Clinical characteristics associated with undernutrition in children under five years of age
Fever was the most common chief complaint among patients in our study and was present in 24.7% (n = 36) of cases. On examination, 19.9% (n = 29) of the children had fever (> 38.3 °C), 24.6% (n = 35) had tachycardia for their respective age, and 16.1% (n = 23) had a decreased level of consciousness (GCS < 15). Among children who had laboratory tests performed, hyponatremia (sodium < 132 mmol/L for children below 12 months, < 136 mmol/L for children 12 months and above) was found in 74.4% (n/N = 29/39) and anaemia (haemoglobin < 10.9 g/dl) was detected in 77.1% (n/N = 37/48) of patients. Fifty-eight children (39.7%) had pre-existing chronic disease, 29 had congenital heart disease and 19 had cerebral palsy (Table 2).
Table 2.
Clinical characteristics with classification of undernutritiona in children
| Abnormal clinical findings | Overall (Nb = 146) n/N (%) | Mild (N = 42) n/N (%) | Moderate (N = 51) n/N (%) | Severe(N = 53) n/N (%) |
|---|---|---|---|---|
| Chief complaints | ||||
| Fever | 36/146 (24.7) | 14/42 (33.3) | 13/51 (25.5) | 9/53 (17.0) |
| Coughing | 35/146 (24.0) | 9/42 (21.4) | 12/51 (23.5) | 14/53 (26.4) |
| Difficulty in breathing | 26/146 (17.8) | 7/42 (16.7) | 7/51 (13.7) | 13/53 (24.5) |
| Failure to thrive | 15/146 (10.3) | 2/42 (4.8) | 7/51 (13.7) | 6/53 (11.3) |
| Lower limb swelling | 9/146 (6.2) | 2/42 (4.8) | 4/51 (7.8) | 3/53 (5.7) |
| Vital signs | ||||
| Hypoxia (SPO2 < 90%) | 9/144 (6.3) | 1/41 (2.4) | 2/50 (4.0) | 6/53 (11.3) |
| Bradypnea | 8/143 (5.6) | 5/41 (12.2) | 2/50 (4.0) | 1/52 (1.9) |
| Tachycardia | 35/142 (24.6) | 11/41 (26.8) | 14/49 (28.6) | 10/52 (19.2) |
| Temperature > 37.5 °C | 29/146 (19.9) | 8/42 (19.0) | 9/51 (17.6) | 12/53 (22.6) |
| Low AVPU score (GCS < 15) | 23/143 (16.1) | 8/42 (19.0) | 8/48 (16.7) | 7/51 (13.7) |
| Point of care tests (POCs) | ||||
| Hypoglycaemia < 3.5 mmol/dl | 3/58 (5.2) | 1/16 (6.3) | 1/15 (6.7) | 1/27 (3.7) |
| Hypokalaemia | 12/39 (30.8) | 2/11 (18.2) | 5/12 (41.7) | 5/15 (33.3) |
| Hyponatremia | 29/39 (74.4) | 8/11 (72.7) | 9/12 (75.0) | 12/16 (75.0) |
| Haemoglobin (< 10.9 g/dl) | 37/48 (77.1) | 13/15 (86.7) | 11/13 (84.6) | 13/20 (65.0) |
| Child’s chronic disease | ||||
| Congenital heart diseases | 29/146 (19.9%) | 4/42 (9.5%) | 8/5 1 (15.7%) | 17/53 (32.1%) |
| Cerebral palsy | 19/146 (13.0%) | 4/42 (9.5%) | 7/51 (13.7%) | 8/53 (15.1%) |
| Hydrocephalus | 5/146 (3.4%) | 0 | 4/51 (7.8%) | 1/53 (1.9%) |
aZ-scores for WFH/WFL, HFA, and WFA were calculated and for each patient. The most severe Z-score for each child was used and interpreted as severe for a Z-score < −3 SD, moderate for a Z-score between −3 SD and < −2 SD, and mild for a Z-score between −2 SD and < −1 SD
bN represents the total number of children in each column that had the test/variable recorded
Disposition and mortality of undernourished children under five years
Most of undernourished children, 71.2% (n = 104), were admitted to the hospital wards from the ED-MNH, 26.7% (n = 39) were discharged home directly from the ED-MNH, and 2.1% (n = 3) died in the ED-MNH. Four undernourished children (2.9%) died in the first 24 h of hospitalization. A total of 13.3% (n = 18) died at the end of the 30-day follow-up (Table 3). At 24 h and at 30 days, nine (6.2%) and eleven (7.5%) patients respectively were lost to follow-up.
Table 3.
Disposition and mortality of undernourished of children under five years
| Clinical variables | Undernourished children n/N a (%) |
|---|---|
| Admitted to the ward | 104/146 (71.2) |
| Discharge from ED | 39/146 (26.7) |
| Died in ED | 3/146 (2.1) |
| 24-h hospital mortality | 4/137 (2.9) |
| 48-h hospital mortality | 6/137 (4.4) |
| 30-day hospital mortality | 18/135 (13.3) |
aN = total patients with followup at each given time period. N was 146 on day of enrolment and N = 137 at 24- and 48-h, and N = 135 at 30 day followup
In undernourished children, the most common diagnoses made by emergency physicians were congenital heart disease 20.7% (n = 28), pneumonia 11.1% (n = 15), and cerebral palsy 8.9% (n = 12). Undernutrition (of any severity) was formally diagnosed by the emergency physician in 6.7% (n = 9) of the undernourished children. Diagnoses of congenital heart disease, pneumonia, and/or cerebral palsy did not have a statistically significant association with mortality in our sample. A reduced level of consciousness on arrival to the ED, with a Glasgow Coma Scale of less than fifteen, and tachycardia were statistically significant risk factors for death, with mortality rates of 16.1% (n = 23), and 24.6% (n = 35), respectively. (Table 4). There was no significant association between the severity of undernutrition and mortality.
Table 4.
Final diagnosis and risk of death of undernourished children under 5 years
| Clinical variables | Overall n/N (%) |
Died n/N (%) |
Survived n/N (%) |
RR(95% CI) | P value |
|---|---|---|---|---|---|
| Provider’s diagnosis | |||||
| Congenital heart diseases | 28/135 (20.7%) | 2/18 (11.1%) | 26/117 (22.2%) | 0.5 (0.1–1.7) | 0.44 |
| Pneumonia | 15/135 (11.1%) | 3/18 (16.7%) | 12/117 (10.3%) | 1.6 (0.5–4.2) | 0.69 |
| Cerebral palsy | 12/135 (8.9%) | 1/18 (5.6%) | 11/117 (9.4%) | 0.6 (0.1–2.8) | 0.93 |
| Acute malnutrition | 9/135 (6.7%) | 3/18 (16.7%) | 6/117 (5.1%) | 2.8 (1.0–6.6) | 0.19 |
| Tumours | 9/135 (6.7%) | 2/18 (11.1%) | 7/117 (6.0%) | 1.8 (0.5–5.0) | 0.76 |
| Vital signs, point of care test | |||||
| Bradypnea | 8/133 (6.0%) | 1/18 (5.6%) | 7/115 (6.1%) | 0.9 (0.2–3.9) | > 0.99 |
| Tachycardia | 34/134 (25.3%) | 10/18 (55.5%) | 24/116 (21.6%) | 3.7 (1.6–8.3) | < 0.01 |
| Hypotension | 8/21 (38.1%) | 3/8 (37.5%) | 5/13 (38.5%) | 1.0 (0.3–2.8) | > 0.99 |
| Low AVPU score (GCS < 15) | 21/132 (15.6%) | 8/18 (44.4%) | 13/114 (11.4%) | 4.2 (1.9–9.1) | < 0.01 |
| Fever (T > 37.5 °C) | 28/135 (20.7%) | 5/18 (27.8%) | 23/117 (19.7%) | 1.5 (0.6–3.5) | 0.63 |
| Hypoglycaemia (RBG < 3.5) | 3/55 (5.5%) | 1/16 (6.3%) | 2/39 (5.1%) | 1.2 (0.2–3.3) | > 0.99 |
| Hypokalaemia | 10/35 (28.6%) | 3/10 (30.0%) | 7/25 (28.0%) | 1.1 (0.3–3.0) | 0.90 |
| Undernutrition classification | |||||
| Mild type | 39/135 (28.9%) | 5/18 (27.8%) | 34/117 (29.1%) | 1.0 (0.4–2.3) | > 0.99 |
| Moderate type | 49/135 (36.3%) | 5/18 (27.8%) | 44/117 (37.6%) | 0.7 (0.3–1.7) | 0.59 |
| Severe type | 47/135 (34.8%) | 8/18 (44.4%) | 39/117 (33.3%) | 1.5 (0.6–3.4) | 0.51 |
Discussion
This study showed that a large proportion (34.1%) of acutely ill children presenting to the ED-MNH suffer from undernutrition. As has been observed in previous in-hospital patient studies, in our study most undernourished children were males under 2 years of age [1, 17, 18] and most caretakers were biological mothers with low socioeconomic status [11, 19–21]. Interestingly, we found an overwhelming number of primary caretakers had at least primary school education, which is in contrast with previous studies, as education has been shown to be protective in the development of childhood undernutrition [9, 19]. However, we did not have a control group of non-undernourished children to compare the relative rates of caretaker education. We also observed high numbers of children with congenital heart diseases and cerebral palsy as the most common chronic diseases, which have been reported to be associated with poor feeding practises leading to undernutrition [22, 23]. As MNH is a tertiary referral centre that specifically takes care of children with congenital heart disease and cerebral palsy, the high number of children with undernutrition with these chronic diseases in our study is unlikely to reflect the burden of undernourished children in most acute care settings in Tanzania.
The high frequency of symptoms of fever and cough found in our study is similar to what is reported in previous studies among undernourished children presenting to acute intake areas and EDs in sub-Saharan Africa [1, 9, 24, 25]. These symptoms could be the result of acute illness due to sepsis, pneumonia, upper respiratory infections, and malaria, all of which are believed to be associated with acute undernutrition [1, 9]. Furthermore, the findings of hypoxia, tachycardia, tachypnoea, and hypotension are similar to observations made in previous studies in Kenya, which also found such variables to be risk factors for mortality among undernourished children [19, 26, 27]. The abnormal routine investigation findings we observed, such as low blood glucose, hypokalaemia, hyponatremia, and low haemoglobin are also similar to what has been observed in previous studies of undernourished children in Kenya [19, 28, 29].
Our study found that although the true percentage of acute undernourished patients was 34.1%, emergency physicians only wrote down a diagnosis related to acute undernutrition in 6.7% of children. This low recognition rate is concerning since the care rendered to undernourished children should differ from their non-undernourished counterparts [4, 12, 30]. In order to optimise patient outcomes, providers need to give special consideration to the possibility of undernutrition with the use of a screening tool at EDs [1, 3]. We also found that undernourished children are likely to be hospitalised. This may be attributed to the fact that the majority of these children presented with fever and cough, which might signify sepsis and pneumonia, making these children less likely to be discharged from the ED.
We found a 30-day mortality of 13.3% in undernourished children in our study, similar to previous studies in LMICs, which report mortality ranges from 3.4 to 40.1% of undernourished children under five years of age [1, 10, 27, 31]. Of these, 2.9% of deaths occurred within the first 24 h of hospitalisation, a time period that is often associated with initial management in the ED. The observed overall mortality is unacceptably high compared to the WHO accepted rate of less than 5%, and this might result from late recognition, variability in treatment, and late arrival to care [1, 4, 12, 30, 32]. In our study we did find that reduced levels of consciousness (GCS < 15) and tachycardia were associated with a statistically significant increase in mortality among undernourished children, similar to observations made in the Maitland et al. study [18]. However, our study was not powered to evaluate for clinical features that increased the risk of mortality. An additional consideration for future analysis includes the relative hospital length of stay and resource utilization among children who are undernourished and those who are not. Finally, future studies should focus on the impact of interventions aimed at increasing identification and early treatment of undernutrition in the ED on patient disposition and outcomes.
Limitations
In this study, the primary goal was to describe the cohort of undernourished children presenting to the ED-MNH. As we did not recruit a control group, we are unable to compare between groups. Furthermore, this study was a single centre study at an urban tertiary referral ED. Therefore, the results may not be generalizable to other hospitals. Most undernourished children in Tanzania are treated at health centres and district hospitals, so those that arrive at MNH may be more complex by the nature of the referral system.
There was low recognition of undernutrition by ED physicians in our study, and low recording of the presence or absence of oedema that would have helped up to define the severity of the undernutrition. We used what was recorded in the chart to measure recognition of undernutrition. ED physicians might have recognised undernutrition without documenting it as an ED diagnosis. Finally, while we report univariate analysis of the clinical factors associated with mortality among the undernourished children, the sample size did not allow for multivariate analysis.
Conclusion
More than one third of acutely ill children below the age of five years who presented to the national hospital’s ED in Tanzania were undernourished and this group had a high admission and mortality rate. Although the rate of undernutrition was high, emergency medicine physicians rarely made the diagnosis of undernutrition formally, as evidenced by documentation in the chart. Emergency physicians need to consider the diagnosis of undernutrition to ensure proper patient management and disposition of these patients. Future studies should focus on the impact of interventions aimed at improving the identification of undernutrition in the ED and the effects of ED management on these children, their dispositions and outcomes.
Acknowledgements
The principal investigator would like to thank Dr. Ellen Weber, Donald Cyprian Kabilondo, MNH-ED staff, and study participants for making this study successful.
Abbreviations
- AVPU Scale
Alert, Voice, Pain and Unresponsive
- CI
Confidence Interval
- ED
Emergency Department
- GCS
Glasgow Coma Scale.
- LMIC
Low- and Middle-Income Countries
- MNH
Muhimbili National Hospital
- RR
Relative Risk
- SD
Standard Deviation
- USA
United States of America
- WHO
World Health Organization
Author’s contributions
Conceptualization: PB HS JM BM. Data curation: PB HS JM BM. Formal analysis: PB HS BM. Methodology: PB HS MS BM VM. Project administration: PB. Supervision: HS JM VM BM. Validation: PB JM HS MS BM VM. Writing-original draft: PB. Writing review & editing: PB JM VM BM MS HS. All authors read and approved the final manuscript.
Funding
This was a non-funded project; the principal investigators used their own funds to support the data collection and logistics.
Availability of data and materials
The structured questionnaire and full dataset supporting the conclusions of this article are available from the authors on request.
Ethics approval and consent to participate
The study protocol was reviewed and approved by the Institutional Review Board of the Muhimbili University of Health and Allied Sciences’ Institutional Review Board (MUHAS-IRB) and permission to collect data was obtained from relevant authorities at MNH. Verbal consent was obtained first from the parent or caretaker to screen children for eligibility, followed by written consent for patients who met the criteria for malnutrition, prior to enrolment in the study.
Consent for publication
Not applicable
Competing interests
The authors declare no conflicts of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Prosper J. Bashaka, Phone: +255-765-670-125, Email: prosperbashaka@gmail.com
Hendry R. Sawe, Email: hendry_sawe@yahoo.com
Victor Mwafongo, Email: vmwafongo@muhas.ac.tz.
Juma A. Mfinanga, Email: jumamfinanga@gmail.com
Michael S. Runyon, Email: mikerunyon@yahoo.com
Brittany L. Murray, Email: brittany.murray@emory.edu
References
- 1.Ngallaba SE, Makerere DJ, Kapesa A, Mongela S, Namanya B. Outcome and effectiveness of inpatient Care of Malnourished Underfive Children in district hospitals of Mwanza region, North Western Tanzania. Open J Prev Med. 2014;04(05):293–298. doi: 10.4236/ojpm.2014.45036. [DOI] [Google Scholar]
- 2.United Nations (UN), Millennium Development Goals (MDGs) report, 2015. Available from:http://www.un.org/millenniumgoals/2015_MDG_Report/pdf/MDG%202015%20rev%20(July%201).
- 3.World Health Organization (WHO). Management of Severe Malnutrition: a manual for physicians and other senior health workers, vol. 1999. Geneva.
- 4.Wallis L, Reynolds TA. African Federation for Emergency Medicine (AFEM) Cape Town: Oxford University Press Southern Africa; 2013. [Google Scholar]
- 5.Cloete J. Management of severe acute malnutrition. S Afr Med J. 2015;105(7):605. doi: 10.7196/SAMJnew.7782. [DOI] [PubMed] [Google Scholar]
- 6.Improving child nutrition;the achievable imperative for global Progress. In: United Nations children’s funds (UNICEF). Available from: http://www.unicef.org/publications/files/Nutrition_Report_final_lo_res_8_April.
- 7.Egata G, Berhane Y, Worku A. Predictors of acute undernutrition among children aged 6 to 36 months in east rural Ethiopia: a community based nested case - control study. BMC Pediatr 14. 2014(1):91. [DOI] [PMC free article] [PubMed]
- 8.Ministry of Health and Social Welfare (MoHSW). Tanzania National Nutrition Strategy July 2011/12- June 2015/2016. Available from: http://scalingupnutrition.org/wp-content/uploads/2013/04/Tanzania_National-Nutrition-Strategy.
- 9.Ocheke I, Thandi P. Malnutrition in acutely ill children at the Paediatric emergency unit in a tertiary Hospital in Nigeria. Niger Med J. 2015;56(2):111. doi: 10.4103/0300-1652.150695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Benyera O, FLM H. Outcomes in Malnourished Children at a Tertiary Hospital in Swaziland after Implementation of the World Health Organization Treatment Guidelines. South Afr J Child Health. 2013;7(4):135. doi: 10.7196/sajch.626. [DOI] [Google Scholar]
- 11.Nagar R, Nagar T, Gupta B. Treatment outcome in patients with severe acute malnutrition managed with Protocolised Care at Malnutrition Treatment corner in Rajasthan, India: a prospective observational study (quasi-experimental). Int J Res Med Sci. 2016:238–45.
- 12.Health, Department-Republic of South Africa. Severe acute malnutrition, emergency treatment in South Africa. Available from: http://www.up.ac.za/media/shared/Legacy/sitefiles/file/45/1335/877/samwallchartemergencytreatment_severe_malnutritionfinal_2.
- 13.Muhimbili National Hospital (MNH). Emergency Medicine Department - Muhimbili National Hospital. [cited Mar 29, 2016]. Available from: http://www.mnh.or.tz/index.php/emergency.
- 14.Razzak JA, Kellermann AL. Emergency medical Care in Developing Countries: is it worthwhile? 2002. [PMC free article] [PubMed] [Google Scholar]
- 15.Anderson P, Petrino R, Halpern P, Tintinalli J. The globalization of emergency medicine and its importance for public health: Pinchas Halpern, & Judith Tintinalli a b c d; 2006. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2627492/pdf/17128364 [DOI] [PMC free article] [PubMed]
- 16.MedCalc . Free statistical calculator. 1993. [Google Scholar]
- 17.Ubesie AC, Ibeziako NS, Ndiokwelu CI, Uzoka CM, Nwafor CA. Under-five protein energy malnutrition admitted at the University of in Nigeria Teaching Hospital, Enugu: a 10-year retrospective review. Nutr J. 2012;11(1):43. doi: 10.1186/1475-2891-11-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Munthali T, Jacobs C, Sitali L, Dambe R, Michelo C. Mortality and Morbidity Patterns in Under-Five Children with Severe Acute Malnutrition in Zambia: A Five-year Retrospective Review of Hospital-Based Records (2009–2013). Arch Public Health. 2015 [cited Feb 29, 2016];73(1). Available from: http://www.archpublichealth.com/content/73/1/23. [DOI] [PMC free article] [PubMed]
- 19.Maitland K, Newton C. Children with severe malnutrition: can those at highest risk of death be identified with the WHO protocol? 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Habaasa G. An investigation on factors associated with malnutrition among Underfive children in Nakaseke and Nakasongola districts. Uganda BMC Pediatr. 2015 [cited Mar 8, 2016;15(1) Available from: http://www.biomedcentral.com/1471-2431/15/134. [DOI] [PMC free article] [PubMed]
- 21.Ogunlesi T., Dedeke IO., Kuponiyi O. Socio-Economic Classification of Children Attending Specialist Pediatric Centres in Ogun State, Nigeria, 2008.
- 22.Okoromah CAN, Ekure EN, Lesi FEA, Okunowo WO, Tijani BO, Prevalence OJC. Profile and predictors of malnutrition in children with congenital heart defects: a case control observational study. Arch Dis Child. 2011;96(4):354–360. doi: 10.1136/adc.2009.176644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sissya H, Fataki M. Prevalence of malnutrition and associated feeding problems among children with cerebral palsy attending Muhimbili National Hospital-Dar es Salaam. Tanzania; 2010.
- 24.Belaynew WBG. Assessment of factors associated with malnutrition among Underfive years age children at Machakel Woreda, Northwest Ethiopia: a case control study. J Nutr Food Sci. 2014; cited Oct 29, 2015];04(01). Available from: http://www.omicsonline.org/assessment-of-factors-associated-with-malnutrition-among-under-five-years-age-children-at-machakel-woreda-northwest-ethiopia-a-case-control-study-2155-9600.1000256.php?aid=22387.
- 25.Mamidi Raja Sriswan, Kulkarni Bharati, Radhakrishna Kv, Shatrugna Veena. Hospital based nutrition rehabilitation of severely undernourished children using energy dense local foods. Indian Pediatrics. 2010;47(8):687–693. doi: 10.1007/s13312-010-0101-7. [DOI] [PubMed] [Google Scholar]
- 26.Heikens GT. How can we improve the Care of Severely Malnourished Children in Africa? PLoS Med. 2007;4(2):e45. doi: 10.1371/journal.pmed.0040045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Maimuna MA. Prevalence of undernutrition, risk factors and outcomes of severe malnutrition among undernourished children admitted to Bugando medical Centre in Mwanza. Tanzania; 2013. Available from: http://www.bugando.ac.tz/theses/M.Sc.DissertationMaimunaAhmed
- 28.Ocheke IE, Puoane T. Factors influencing the pattern of malnutrition among acutely ill children presenting in a tertiary Hospital in Nigeria. May. 2014; Available from: http://www.ajol.info/index.php/njp/article/view/107287/97174.
- 29.World Health Organization (WHO). Haemoglobin Concentrations for Diagnosis of Anemia and Assement of Severity.
- 30.Antwi S. Malnutrition: missed opportunities for diagnosis. 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lenters LM, Wazny K, Webb P, Ahmed T, Bhutta ZA. Treatment of severe and moderate acute malnutrition in low- and middle-income settings: a systematic review, meta-analysis and Delphi process. BMC Public Health. 2013;13(Suppl 3):S23. doi: 10.1186/1471-2458-13-S3-S23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.World Health Organization (WHO) United Nations Children’s funds. UNICEF: World Bank. Levels and Trends in Child Malnutrition; 2015. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The structured questionnaire and full dataset supporting the conclusions of this article are available from the authors on request.