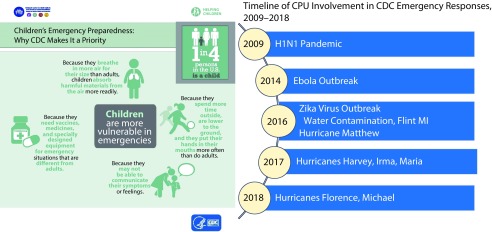
This issue of AJPH highlights the importance of community preparedness for public health emergencies. An essential component of community preparedness is the capacity to address the needs of children, who comprise nearly one quarter of the US population and are particularly vulnerable to disaster-related morbidity and mortality (Figure 1).1 However, communities may not be well equipped to address children’s needs.
FIGURE 1—
Children’s Preparedness at the Centers for Disease Control and Prevention (CDC) and Children’s Preparedness Unit Involvement in CDC Emergency Responses: United States, 2009–2018
THE CHILDREN’S PREPAREDNESS UNIT
The Children’s Preparedness Unit (CPU; https://www.cdc.gov/childrenindisasters) at the Centers for Disease Control and Prevention (CDC) works to create resilient communities through cultivating partnerships, building technical expertise within and outside of CDC, integrating children’s needs into medical countermeasures, and increasing partners’ and communities’ awareness about the unique physical, developmental, and social-emotional needs of children in preparedness and response. Through the lens of successive public health emergency responses, we describe CPU’s evolution from a small workgroup convened to support CDC’s 2009 pandemic influenza response to an integral part of CDC’s emergency planning and response for all hazard types, as well as a reliable resource and committed stakeholder for community pediatric preparedness planning.
PEDIATRIC NEEDS IN EMERGENCY RESPONSE
In May 2009, CDC mobilized a team of children’s health experts to address the disproportionate impact of pandemic influenza A (H1N1) on pediatric populations2,3 and to field questions and concerns from the public and health care providers about the needs of children. The team’s expertise focused on pediatric medical care and countermeasures, epidemiology, and surveillance. It developed education materials and resources for community members, health care providers, and other professionals who serve children. Establishing partnerships with key stakeholders was central to the early development of CPU. Relationships with national organizations (e.g., American Academy of Pediatrics), state health departments, and local groups (e.g., faith-based organizations) provided important means to disseminate and amplify key prevention messages. The work of these children’s health experts during the H1N1 response laid the groundwork for establishing a CPU outside the CDC emergency response structure. Relationships developed between the nascent CPU and its partners formed the foundation for collaboration to improve pediatric emergency preparedness planning with sectors already focused on children’s health and well-being that continues today.
From 2014 to 2017, CPU provided pediatric expertise in CDC’s responses for two infectious disease outbreaks: Ebola in West Africa (2014–2016) and Zika virus in the Americas (2015–2017). The Ebola response built upon CPU’s experience in the H1N1 response; close collaboration between pediatric and epidemiology experts resulted in optimal surveillance of pediatric risk factors and outcomes. Furthermore, CPU solidified and expanded domestic and international partnerships and built both internal and external infrastructure that would allow faster, more coordinated responses for future public health emergencies resulting in better protection for children.
The Zika response also highlighted the need for strong cross-sector partnerships and collaboration to facilitate adherence to clinical guidance for the diagnosis, evaluation, and treatment of infants and children with congenital Zika virus exposure. During the response, CPU augmented partnerships with the American Academy of Pediatrics and other pediatric organizations and included new maternal and obstetric health partners such as the American College of Obstetricians and Gynecologists to support the coordination of care for maternal–infant dyads affected by Zika.
During its involvement in the 2016 Flint, Michigan, response to lead contamination in drinking water, CPU again demonstrated the value of pediatric partnerships and community collaboration. In partnership with the US Department of Education, CPU disseminated appropriate and timely information to Flint schools, including educational materials (e.g., https://tinyurl.com/y7o65czp) to address community concerns. CPU also fostered positive relationships with schoolteachers, recognizing them as trusted voices in the Flint community. This further facilitated the distribution of accurate health information to children and their families.
Between October 2016 and October 2018, six major hurricanes hit the continental United States and US Territories. The 2017 hurricane response by CDC was the first to include an At-Risk Task Force, within which CPU operated, specifically dedicated to addressing the needs of children and other vulnerable populations as part of the CDC response structure. The At-Risk Task Force functioned as an independent task force, making CPU more agile and better able to provide technical assistance and consultation to affected state, local, and tribal health departments and federal partners.
The hurricane responses highlighted the need to understand and address children’s mental health from a public health perspective and provide public health materials designed specifically for children, families, and communities about postdisaster coping. In response, CPU collaborated to develop a resource (https://tinyurl.com/rwc0p3) for families and communities to talk to children about how to cope after a disaster. Being positioned within the At-Risk Task Force meant that the CPU team was better able to provide resources for families and communities about children’s coping after a disaster.
There is also a critical need for accurate, fiscally prudent, and timely surveillance data on children’s needs including mental health and resilience. Currently no single syndromic surveillance system provides comprehensive and timely information about children’s disaster mental health needs. Such surveillance could allow public health professionals to assess and recommend appropriate, evidence-based interventions to support children’s mental health needs at the community level.
The involvement of CPU in each public health emergency described highlights—in different ways—the importance of addressing the physical, emotional, developmental, and mental health needs of children in disasters. The implications of, and lessons learned from, CPU’s ongoing involvement in CDC’s emergency responses is increasing attention to a population that is often disproportionately impacted by disasters.
LOOKING TO THE FUTURE
Lessons learned in emergency response inform CPU’s day-to-day activities to improve pediatric emergency preparedness and attenuate the public health impact of disasters before disasters occur. The CPU continues to build partnerships and facilitate linkages between clinicians and public health subject matter experts. These types of partnerships ensure that threat-specific pediatric needs are assessed and guidance for clinicians and public health practitioners on the use of life-saving therapeutics, vaccines, and other medical material in the event of a mass-casualty incident is relevant and meaningful.4,5 Although better surveillance of children’s disaster-related needs in general is still needed, such threat-specific guidance materials can augment community preparedness resources available online and be quickly disseminated through established partners to promote uptake during a crisis.
In addition, CPU collaborates with partners to improve pediatric preparedness capacity at the state and local level by developing, implementing, and evaluating pediatric-focused preparedness exercises (https://tinyurl.com/AAP-TTX). These exercises are designed for state and local health departments to engage in multisector planning and partnership building to improve clinical and public health preparedness for pediatric populations. Exercises can familiarize partners with enhanced preparedness strategies, strengthen stakeholder communications, identify gaps in critical response capabilities, and provide education to improve capacity.6
The result of the CPU’s evolution during and outside of emergency response is a public health preparedness infrastructure at CDC that is stronger, more inclusive of children’s needs, and positioned to meet challenges as they arise. The Enactment of Public Law No. 116-22, the Pandemic and All-Hazards Preparedness and Advancing Innovation Act of 2019, codifies CPU within CDC for the first time, reflecting the important function a children’s preparedness unit plays in CDC’s emergency preparedness for children.7
Going forward, CPU will continue to leverage its expertise to champion the unique needs of children in preparedness and response activities. The CPU will expand partnerships with pediatric organizations, provide technical assistance and clinical information, and deliver communication resources to federal, state, and local agencies to help strengthen pediatric preparedness at the community level.
ACKNOWLEDGMENTS
This article is based on “Caring for Children in Disaster Response: Building the Link Between Developmental Pediatrics and Infectious Disease One Event at a Time” presented by Georgina Peacock, for the Cheng T. Cho, MD, PhD, Pediatric Infectious Diseases Lectureship at the University of Kansas, Kansas City, KS, May 26, 2016.
The authors would like to recognize the outstanding work of the following people: Karen Cobham-Owens, whose efforts as a member of the Children’s Preparedness Unit (CPU) have been integral to the success of CPU and invaluable to the integration of children’s needs into emergency preparedness and response at CDC—we are grateful for her ongoing commitment to this work—and Stephanie Griese, whose early leadership provided the strong foundation on which CPU operates today.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
REFERENCES
- 1.Bartenfeld MT, Peacock G, Griese SE. Public health emergency planning for children in chemical, biological, radiological, and nuclear (CBRN) disasters. Biosecur Bioterror. 2014;12(4):201–207. doi: 10.1089/bsp.2014.0036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Louie JK, Gavali S, Acosta M et al. Children hospitalized with 2009 novel influenza A (H1N1) in California. Arch Pediatr Adolesc Med. 2010;164(11):1023–1031. doi: 10.1001/archpediatrics.2010.203. [DOI] [PubMed] [Google Scholar]
- 3.Cox CM, Blanton L, Dhara R, Brammer L, Finelli L. 2009 pandemic influenza A (H1N1) deaths among children—United States, 2009–2010. Clin Infect Dis. 2011;52(suppl 1):S69–S74. doi: 10.1093/cid/ciq011. [DOI] [PubMed] [Google Scholar]
- 4.Bradley JS, Peacock G, Krug SE et al. Pediatric anthrax clinical management. Pediatrics. 2014;133(5):e1411–e1436. doi: 10.1542/peds.2014-0563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Griese SE, Kisselburgh HM, Bartenfeld MT et al. Pediatric botulism and use of equine botulinum antitoxin in children: a systematic review. Clin Infect Dis. 2017;66(suppl 1):S17–S29. doi: 10.1093/cid/cix812. [DOI] [PubMed] [Google Scholar]
- 6.Chung S, Gardner AH, Schonfeld DJ et al. Addressing children’s needs in disasters: a regional pediatric tabletop exercise. Disaster Med Public Health Prep. 2018;12(5):582–586. doi: 10.1017/dmp.2017.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pandemic and All-Hazards Preparedness and Advancing Innovations Act of 2019. HR 269. Available at: https://www.congress.gov/bill/116th-congress/senate-bill/1379. Accessed July 30, 2019.