Abstract
Objectives. To demonstrate a flexible and practical method to obtain near real-time estimates of the number of at-risk community-dwelling adults with a chronic condition in a defined area potentially affected by a public health emergency.
Methods. We used small area estimation with survey responses from the 2016 Behavioral Risk Factor Surveillance System together with a geographic information system to predict the number of adults with chronic obstructive pulmonary disease who lived in the forecasted path of Hurricane Florence in North and South Carolina in 2018.
Results. We estimated that a range of 32 002 to 676 536 adults with chronic obstructive pulmonary disease resided between 50 and 200 miles of 3 consecutive daily forecasted landfalls. The number of affected counties ranged from 8 to 10 (at 50 miles) to as many as 119 to 127 (at 200 miles).
Conclusions. Community preparedness is critical to anticipating, responding to, and ameliorating these health threats. We demonstrated the feasibility of quickly producing detailed estimates of the number of residents with chronic conditions who may face life-threatening situations because of a natural disaster. These methods are applicable to a range of planning and response scenarios.
Providing life-saving resources and support to vulnerable populations before, during, and after an emergency is essential for effective public health preparedness and response efforts. Natural disasters (e.g., earthquakes, hurricanes, floods, snow and ice storms, heat waves, and wildfires) can result in large-scale public health emergencies disproportionately affecting at-risk populations; this includes individuals with low income, chronic conditions, or disabilities. Human-made disasters, such as terrorist attacks, also require considerations of populations with special health care needs, as do biological threats such as those seen with annual influenza spread and environmental incidents.
More than half of US adults have at least 1 chronic condition, and 42% have more than 1 condition.1 Ensuring that persons with chronic conditions have adequate supplies of medications, medical supplies, and care is critical for effective public health emergency planning and response efforts.2 For example, following a large-scale emergency, individuals with type 1 diabetes can develop life-threatening complications when management of their condition is interrupted.3 Similarly, cancer patients who are treated with chemotherapy are at greater risk for infections4 or may experience interruptions in treatment regimens.5 Individuals with cardiovascular diseases may have difficulty accessing medications and face challenges with adherence.6 Chronic obstructive pulmonary disease (COPD) symptoms may be exacerbated through interruptions in medication schedules or lack of access to stable oxygen supplies.7 Older adults with physical or cognitive impairment such as dementia and Alzheimer’s disease can be adversely affected by the loss of caregiving services.8
The Centers for Disease Control and Prevention (CDC) and the Public Health Emergency Preparedness program play a critical role in preparing for, responding to, and recovering from public health emergencies. The Public Health Emergency Preparedness and Response Capabilities: National Standards for State, Local, Tribal and Territorial Public Health outlines 15 capability national standards for all levels of public health to provide operational support to public health agencies before, during, and after an event.9 The first capability—community preparedness—identifies the role of public health in identifying at-risk individuals who may be disproportionally affected by an emergency to ensure that these populations are accounted for as part of an agency’s emergency planning efforts.
Emergency response and preparedness officials can use a geographic information system (GIS) to identify the unique needs of populations in places affected by a particular event. Yet, these data systems are often inadequate, particularly in local or rural settings. We previously showed that it was possible to combine public health surveillance data with a GIS to obtain estimates of chronic disease and public health response assets for user-defined areas affected by a natural disaster.10
Population health data on chronic disease risk factors and health outcomes are usually obtained from national or nationwide health surveys. However, direct survey estimates for small geographic areas (e.g., counties, cities, or neighborhoods) are typically unavailable because the sample sizes for these areas often are too small to enable reliable estimates with acceptably small standard errors. Strategies to overcome sample size limitations include spatial or temporal aggregation to obtain sufficient sample sizes for reliable direct estimates, with a corresponding lack of geographic or temporal precision.
Furthermore, such approaches do not provide the flexibility and timeliness needed to respond to and, for some events, anticipate urgent requests for up-to-date data for areas smaller than counties and sometimes states. As a result, it is critically important to develop new, innovative methods to produce timely and accurate estimates of populations at risk for adverse effects before, during, or after public health emergencies caused by natural or human-made disasters. In turn these population-level estimates can help preparedness professionals plan for the types, quantities, and staging locations of resources for people with chronic conditions. Using a model-based small area estimation (SAE) approach provides a potentially precise way to estimate chronic disease prevalence in small areas.
We applied a validated SAE technique, combined with GIS, to obtain near real-time estimates of the number of community-dwelling persons with chronic conditions who live in the predicted location of a natural disaster. Our goal was to reliably estimate the number of people with chronic conditions with special needs during a public health emergency. We illustrate this capability tool with a case study estimating the number of people with COPD who were potentially affected by Hurricane Florence as it approached a predicted landfall in September 2018. Hurricane Florence, a powerful and long-lived hurricane that caused severe damage in the Carolinas, dropped up to 35.93 inches of rain in some areas of North Carolina and was the wettest tropical cyclone recorded in the Carolinas.11
Hurricanes can cause major property devastation, injury, and death. In addition to the severe, immediate effects, hurricanes cause homelessness and disrupt the daily lives of affected residents—either temporarily because of evacuation or permanently in the case of residential destruction. People who depend on specialized health care, medical devices, and medications may experience life-threatening conditions during disasters. Health threats may be primary, from the stress and conditions brought on by the disaster, or secondary, from loss of access to existing medical resources. Adults aged 65 years and older, people with special assistance and care needs, and adults with chronic health conditions are disparately affected by these events.8 Recommendations for emergency and disaster preparedness of chronically ill patients are available.12
We estimated the number of people with COPD for our example of persons with a special chronic disease–related need. COPD refers to a group of diseases that cause airflow blockage and breathing-related problems, including emphysema and chronic bronchitis. An estimated 16 million Americans have COPD,13 and it is the fourth leading cause of death in the United States.14 Compared with people without COPD, people with COPD are more likely to have activity limitations, including difficulty walking; be unable to work; and need special equipment such as portable oxygen tanks, especially at more progressed stages of the disease.13 They are more likely to have comorbid chronic conditions and more hospitalizations and emergency department visits because of exacerbations.15 Additionally, COPD prevalence is greater among persons with limited resources, including people aged 65 years and older and those of lower socioeconomic position.13 Thus, they are a group with substantial public health needs during a natural disaster or other larger scale emergency.
METHODS
We used the 2016 Behavioral Risk Factor Surveillance System (BRFSS) public use data at the individual level (n = 486 303), along with the respondents’ county of residence from a restricted data set through a data use agreement with the CDC. The BRFSS is a random-digit-dialed telephone (landline and cell phone) health survey conducted by state health departments in all 50 states, the District of Columbia, and some US territories, with assistance from the CDC.16 The BRFSS collects data on sociodemographic characteristics, health-related behaviors, chronic diseases, and other conditions among adults aged 18 years and older. Each state’s sample is weighted to obtain a study population representative of a given state. Among the states and the District of Columbia, sample sizes in 2016 ranged from 2914 in Alaska to 36 995 in Florida. The median combined response rate was 47.1% in 2016,17 using standards set by the American Association for Public Opinion Research.18 The prevalence of COPD was determined by the question, “Has a doctor, nurse, or other health professional ever told you that you have chronic obstructive pulmonary disease (COPD), emphysema or chronic bronchitis?”
Census Tract–Level Estimation Analysis
To predict the number of adults aged 18 years and older with self-reported COPD who lived in the predicted path and actual storm track of Hurricane Florence in 2018, we used multilevel regression and poststratification19 to estimate the prevalence of COPD at each census tract level. We previously applied the multilevel regression and poststratification approach to produce COPD estimates for all the US counties using 2011 BRFSS19 and for the 500 largest US cities and their census tracts from BRFSS.20 Multilevel regression and poststratification has also been applied to several other conditions.21–28 Similarly, in this study we used 2016 BRFSS data to construct a multilevel logistic regression model, which was specified as follows:
where Yijk is the response of having COPD (yes or no) by a respondent k from county i and state j; P(Yijk = 1) is the probability that the respondent reported COPD; Xijk is a vector of fixed effects (predictors), which included individual-level age (13 age groups at 5-year intervals from 18 to ≥ 80 years), sex (male and female), race/ethnicity (non-Hispanic White, Black, American Indian or Alaska Native, Asian, Native Hawaiian/other Pacific Islander, other single race, and 2 or more races, and Hispanic), education level (less than high school, high school, some college, and college and above), and county-level percentage of adult population below 150% of the poverty line obtained from the 2011 to 2016 American Community Survey. b is the vector of parameter estimates, rej represents the state-level random effects, and rei(j) represents the random effect of county nested in the state.
Next, we applied the model parameters to the 2010 decennial census population counts at the census tract level to obtain the predicted probability for an individual in a census tract through the following formula:
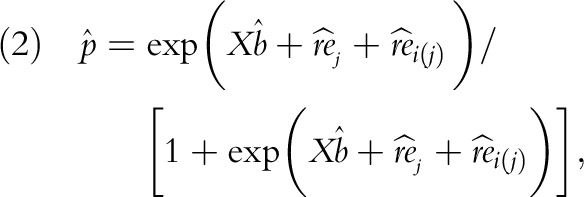 |
where 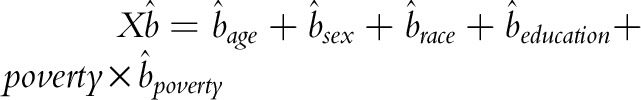
We grouped tract-level population counts by age, sex, and race/ethnicity. The US Census Bureau does not provide census tract–level population data for education level by age, sex, and race; we used bootstrapping to impute it for our formula calculation. The population data by poverty was the tract-level percentage of the adult population living below 150% of the poverty level obtained from the 2011 to 2016 American Community Survey. With the predicted probability, we calculated the point estimate of COPD for any census tract through poststratification. To assess the precision of the estimates, we ran 1000 draws of Monte Carlo simulation and presented the mean estimate and its 95% confidence interval (CI) over 1000 draws. The accuracy of COPD estimates has been evaluated against direct BRFSS survey estimates at state, county, and city levels.19,29–31 All analyses were implemented in SAS version 9.4 (SAS Institute, Cary, NC).
Geographic Information System Analysis
The National Hurricane Center (NHC) produces 5-day storm advisories for each named storm and continues to produce them in near real-time as the storm progresses until it dissipates. These advisories are forecasts with a narrative description of the storm at the time of the forecast; they are accompanied by a map showing (1) the predicted path of the storm over the next 120 hours, (2) 7 points predicting the location of the storm center along the path in 12-hour increments for the first 48 hours and 24-hour increments thereafter (time is measured from the time of the current advisory), (3) the potentially affected coastlines, and (4) the cone of uncertainty, which represents areas most likely to be affected by the storm over the course of the next 5 days. As the storm approaches landfall, the advisories become more frequent. The NHC publishes the 4 geographic files needed to make the map associated with each advisory.32 These files can be read into standard GIS software for cartographic visualization and the type of geographic analysis we performed to produce these COPD estimates in the affected area.
We linked our model-based estimates of COPD at the census tract level to the geographic files of the predicted storm-affected areas in a GIS. We calculated the estimated number of adults with COPD for each census tract by multiplying its model-based estimated prevalence with its 2010 Decennial Census population counts for adults aged 18 years or older.
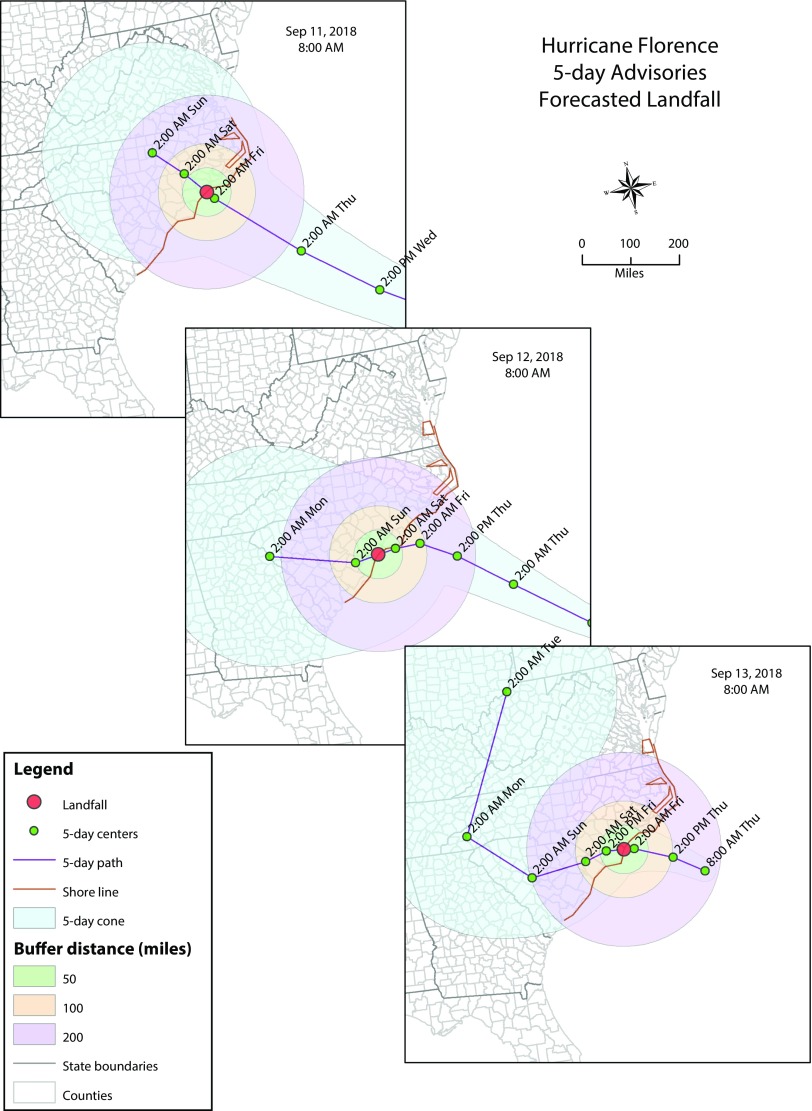
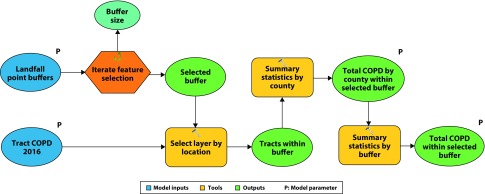
We downloaded the September 11, September 12, and September 13, 2018, 5-day 8 am forecast geographic files from the National Oceanic and Atmospheric Administration’s NHC Web site.32 Through a GIS overlay function, we determined the exact point of landfall of the hurricane for each of the 3 forecasted scenarios. We created 3 spatial buffers on the basis of the forecasted landfall points at 50-, 100- and 200-mile radii (Figure 1). Then we selected census tracts whose geographic centroids were located inside the buffer zones. Finally, we summarized the number of adults with COPD on the basis of the census tracts’ centroid that were inside each buffer. The processes can be built into a geoprocessing model in a GIS to accelerate the calculation in real time and provide the rapid generation of estimates for a large number of alternative forecasts (Figure 2).
FIGURE 1—
Forecasted Storm Tracks, Landfall Locations, and 50-, 100-, and 200-Mile Buffer Zones From Landfall for Hurricane Florence, From 3 Consecutive Days Before Landfall: North Carolina and South Carolina, 2018.
FIGURE 2—
Geoprocessing Model for Estimating the Number of People Within Buffer Zones From Landfall for Hurricane Florence: North Carolina and South Carolina, 2018
Note. COPD = chronic obstructive pulmonary disease.
RESULTS
Target population estimates ranged from 32 002 to 676 536 adults with COPD depending on their residence within 50 miles and 200 miles, respectively, of 3 consecutive daily forecasted points of hurricane landfall (Table 1). The number of affected counties ranged from 8 to 10 (at 50 miles) to as many as 119 to 127 (at 200 miles). Projected points of landfall shifted from Onslow County, North Carolina, on the basis of the September 11, 8 am forecast, to Horry County, South Carolina, on the basis of the September 12, 8 am forecast, and back to North Carolina (New Hanover County), on the basis of the final September 13, 8 am forecast. These shifts in predicted landfall resulted in variations in the expected number of adults with COPD at each of the buffer radii; however, the variations were more pronounced at larger buffer distances: at the 50-mile buffer the range in estimates was 3550 adults; at the 100-mile buffer the range was 30 293 adults; and at the 200-mile buffer the range was 117 508 adults.
TABLE 1—
Estimated Number of Adults Aged 18 Y and Older With COPD Living Within Selected Distances of 3 Consecutive Daily Forecasts of Landfall for Hurricane Florence: North Carolina and South Carolina, 2018
| No. Adults With COPDa (No. Counties in Buffer) |
|||||
| Forecast Numberb | Date and Time of Forecast | Forecasted Landfall | 50-Mile Buffer Radius | 100-Mile Buffer Radius | 200-Mile Buffer Radius |
| al062018048A | 9/11/2018 8:00 AM | 9/14/2018 | 35 552c (10) | 122 932 (28) | 559 028 (127) |
| al062018052A | 9/12/2018 8:00 AM | 9/15/2018 | 35 289 (8) | 153 225 (29) | 676 536 (122) |
| al062018056A | 9/13/2018 8:00 AM | 9/14/2018 | 32 002 (9) | 138 913 (28) | 588 460 (119) |
Note. COPD = chronic obstructive pulmonary disease; GIS = geographic information system; SAE = small area estimation.
Estimates were obtained from the SAE model and may not necessarily equal the actual numbers.
Source. National Oceanic and Atmospheric Administration. National Hurricane Center GIS archive—tropical cyclone advisory forecast. Available at: https://www.nhc.noaa.gov/gis/archive_forecast_results.php?id=al06&year=2018&name=Hurricane. Accessed November 9, 2018.
Estimates of the number of people with COPD were aggregated from census tracts; confidence intervals were not produced at the buffer level. Table A (available as a supplement to the online version of this article at http://www.ajph.org) provides estimates and confidence intervals by individual census tract at the 50-mile buffer for the September 11, 2018 predicted path.
For any given forecast, the number of estimated adults with COPD at each distance buffer depended on where the storm made landfall. The largest number of adults with COPD within 50 miles of landfall was predicted on the basis of the September 11 forecast, for landfall in Onslow County, North Carolina. However, using this same September 11 forecast, the estimated number of adults with COPD living within a 100-mile buffer of predicted landfall in Onslow County was actually the lowest of the 3 forecasts. The highest estimated number of adults with COPD living within 100- and 200-mile buffers of landfall was determined by the September 12 forecast for landfall in Horry County, South Carolina. The actual landfall near Wrightsville Beach in New Hanover County, North Carolina, which was consistent with the September 13, 8 am forecast, resulted in the lowest predicted number of adults with COPD (32 002) living within 50 miles of landfall. Yet, the number of adults with COPD increased more than 18-fold from the 50-mile buffer to the 200-mile buffer (588 460).
Because we aggregated estimates from the census tracts and did not model them at the buffer level, we did not estimate CIs. However, Table A (available as a supplement to the online version of this article at http://www.ajph.org) shows the census tract estimates within the 50-mile buffer zone for the September 11 forecast, along with 95% CIs for those specific tracts.
DISCUSSION
A previous report10 demonstrated the feasibility of combining health survey data with the functionality of a GIS to enable researchers and public health officials to obtain estimates of chronic conditions and selected public health response assets (e.g., number of hospitals, hospital beds, and hospital workers) for user-defined areas potentially affected by natural disasters. In that report, it was only possible to predict chronic conditions at the county level by aggregating 4 years of direct survey estimates from the BRFSS. Because producing estimates for more local levels was not possible at that time (e.g., through SAE), it was not feasible to create precise models of the potential impact of a public health emergency at the community level. Moreover, producing ad hoc county-level estimates was time and resource intensive (making it impossible to model impact on a near real-time basis) and was not flexible enough to account for changes in weather projections, largely rendering the method inefficient for emergency preparedness efforts.
Another report demonstrated the combined use of GIS and dynamic simulation to model surges in demand for trauma care as a result of mass casualty disasters.33 Other researchers reported on the development of a tool to estimate the number of individuals with preexisting medical conditions who might need postdisaster medical care,34 specifically the number of daily hospitalizations, hospital bed demand, nursing home bed demand, demand for clinical visits, and demand for special medical care for 7 delineated chronic conditions. Model inputs relied on estimated national prevalence rates for the 7 chronic conditions, applied to local populations estimated to be at risk for a disaster.
The GIS and SAE approach described here has several contributions and strengths. First, it is an application of a validated SAE methodology for the purpose of public health preparedness and response, which directly addresses the first capability outlined in CDC’s Public Health Emergency Preparedness and Response Capabilities: community preparedness.9 This example illustrates an effective strategy to determine “risks to the health of the jurisdiction,” including identifying populations who have medical and public health needs that may make them disproportionately at risk during an emergency. This approach provides the data necessary to help public health and emergency response professionals plan for needed resources and services for at-risk populations. Second, it demonstrates the ability to forecast the number of people potentially affected by a disaster using a validated SAE method coupled with the flexibility of using GIS data for projected paths of severe weather events or the course of a natural disaster.
Because the SAEs can be precomputed, stored in a file for rapid access, and updated frequently, the method that we described is near real time. This is important because the estimate of at-risk populations needed to be rapidly updated owing to rapidly changing forecasts and frequently limited advance notice about an impending event. Using this methodology, targeted emergency preparedness efforts can be initiated more quickly, which could mean savings in terms of efficient allocation of resources and preventing loss of life.
Our approach can take other mitigating factors into account. For example, we were able to produce estimates by census tract, as noted in Table A. Planners can take into account, for example, that particular areas in a predicted storm path might be differentially affected on the basis of expected storm damage, community infrastructure, past experience with communities, or other factors that planners and responders might consider important. Other relevant data, such as transportation routes, topography, and expected storm damage, could be included as available.
In addition, this approach can be extended to other chronic conditions for which data are available. The BRFSS collects annual data for additional chronic conditions (coronary heart disease, stroke, asthma, cancer, depressive disorder, kidney disease, diabetes) for which this methodology can be used. Depending on the disaster, there may be a need to identify different subpopulations, for example, estimating the number of adults with current asthma during a wildfire emergency (e.g., the 2017 or 2018 California wildfire seasons). The SAE methodology and GIS analysis could be used to identify subpopulations such as older adults and adults with chronic conditions at higher risk of severe complications from infectious diseases (e.g., influenza).
Lastly, the ability to model the number and characteristics of populations who may be affected by a public health emergency is a strength of this approach and can aid officials in predicting service needs and resources in advance of an event, regardless of chronic disease status. Resources for which detailed planning estimates are needed include general and specialized medical care from first responders and health care professionals; medical treatment facilities, such as clinics and hospital beds; specialized medical equipment, such as oxygen, continuous positive airway pressure devices, asthma rescue inhalers, and epinephrine autoinjectors; and prescription medications for conditions such as diabetes, high blood pressure, angina, and COPD. The detailed planning estimates can help preparedness professionals in detailed planning activities to ensure that once a disaster occurs, adequate resources are available and staged to most effectively respond.
Directly measured data should be used whenever they are available and of sufficient quality. However, this modeling approach can be a useful tool when direct data are absent, which is frequently the case at the local level. In this context, these results are subject to some limitations. First, our model-derived estimates from the state-based BRFSS can be affected by biases from both the survey itself (e.g., recall) and the modeling process (e.g., choice of covariables).29,30 Second, the estimates of the number of people with COPD here refers to noninstitutionalized adults who may have urgent needs related to treatment of their COPD. These estimates do not include those in nursing homes, for example, who must be accounted for by other means in planning for urgent events. Third, estimates of at-risk individuals will depend on the availability, quality, and level of detail of data in various data sets.
Horn and Kirsch summarized the current state of the public health community to meet the essential needs for noncommunicable diseases in disasters.35 Despite having learned many lessons as a result of Hurricane Katrina, and having made progress since 2005, there are still many opportunities to plan for and respond to the needs of persons with a chronic disease during an emergency. By combining an innovative, validated, and flexible SAE methodology with an ongoing nationwide health survey in a GIS, we have demonstrated the feasibility of quickly producing detailed estimates of the potential numbers of residents with chronic conditions who may be affected by a natural disaster for a range of planning and response scenarios.
CONFLICTS OF INTEREST
The authors have no conflicts of interest.
HUMAN PARTICIPANT PROTECTION
Protocol approval was not necessary because no human participants were involved in this study.
REFERENCES
- 1.Buttorff C, Ruder T, Bauman M. Multiple chronic conditions in the United States. Santa Monica, CA: RAND Corporation; 2017. Available at: https://www.rand.org/pubs/tools/TL221.html. Accessed January 9, 2019.
- 2.Ford ES, Mokdad AH, Link MW et al. Chronic disease in health emergencies: in the eye of the hurricane. Prev Chronic Dis. 2006;3(2):A46. [PMC free article] [PubMed] [Google Scholar]
- 3.Fonseca VA, Smith H, Kuhadiya N et al. Impact of a natural disaster on diabetes: exacerbation of disparities and long-term consequences. Diabetes Care. 2009;32(9):1632–1638. doi: 10.2337/dc09-0670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Preventing infections in cancer patients: information for patients and caregivers. Available at: https://www.cdc.gov/cancer/preventinfections/patients.htm. Accessed January 7, 2019.
- 5.Ullman K. Cancer care during natural disasters. J Natl Cancer Inst. 2011;103(24):1819–1820. doi: 10.1093/jnci/djr527. [DOI] [PubMed] [Google Scholar]
- 6.Krousel-Wood MA, Islam T, Muntner P et al. Medication adherence in older clinic patients with hypertension after Hurricane Katrina: implications for clinical practice and disaster management. Am J Med Sci. 2008;336(2):99–104. doi: 10.1097/MAJ.0b013e318180f14f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kobayashi S, Hanagama M, Yamanda S et al. Impact of a large-scale natural disaster on patients with chronic obstructive pulmonary disease: the aftermath of the 2011 Great East Japan Earthquake. Respir Investig. 2013;51(1):17–23. doi: 10.1016/j.resinv.2012.10.004. [DOI] [PubMed] [Google Scholar]
- 8.Aldrich N, Benson WF. Disaster preparedness and the chronic disease needs of vulnerable older adults. Prev Chronic Dis. 2008;5(1):A27. [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention, Center for Preparedness and Response. Public health emergency preparedness and response capability standards: national standards for state, local, tribal, and territorial public health. 2018. Available at: https://www.cdc.gov/cpr/readiness/capability standards.htm. Accessed January 28, 2019.
- 10.Holt JB, Mokdad AH, Ford ES, Simoes EJ, Bartoli WP, Mensah GA. Use of BRFSS data and GIS technology for rapid public health response during natural disasters. Prev Chronic Dis. 2008;5(3):A97. [PMC free article] [PubMed] [Google Scholar]
- 11.US Census. Emergency preparedness: 2018 Hurricane Florence. Available at: https://www.census.gov/topics/preparedness/events/hurricanes/florence.html. Accessed January 7, 2019.
- 12.Tomio J, Sato H. Emergency and disaster preparedness for chronically ill patients: a review of recommendations. Open Access Emerg Med. 2014;6:69–79. doi: 10.2147/OAEM.S48532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. Employment and activity limitations among adults with chronic obstructive pulmonary disease—United States, 2013. MMWR Morb Mortal Wkly Rep. 2015;64(11):290–295. [PMC free article] [PubMed] [Google Scholar]
- 14.National Center for Health Statistics. Health, United States, 2017: With Special Feature on Mortality. Hyattsville, MD: 2018. Available at: https://www.cdc.gov/nchs/hus/index.htm. Accessed November 1, 2018. [PubMed] [Google Scholar]
- 15.Wheaton AG, Ford ES, Cunningham TJ, Croft JB. Chronic obstructive pulmonary disease, hospital visits, and comorbidities—National Survey of Residential Care Facilities, 2010. J Aging Health. 2015;27(3):480–499. doi: 10.1177/0898264314552419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Overview: BRFSS 2016. Available at: https://www.cdc.gov/brfss/annual_data/2016/pdf/overview_2016.pdf. Accessed November 6, 2018.
- 17.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System: 2016 Summary Data Quality Report. Available at: https://www.cdc.gov/brfss/annual_data/2016/pdf/2016-sdqr.pdf. Accessed November 6, 2018.
- 18.American Association for Public Opinion Research. Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys. 9th ed. Ann Arbor, MI: 2016. [Google Scholar]
- 19.Zhang X, Holt JB, Lu H et al. Multilevel Regression and Poststratification for Small-Area Estimation of Population Health Outcomes: A Case Study of Chronic Obstructive Pulmonary Disease Prevalence Using the Behavioral Risk Factor Surveillance System. Am J Epidemiol. 2014;179(8):1025–1033. doi: 10.1093/aje/kwu018. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention. 500 Cities project data. 2016. Available at: https://www.cdc.gov/500cities. Accessed October 30, 2018.
- 21.Eberth JM, Zhang X, Hossain M, Tiro JA, Holt JB, Vernon SW. County-level estimates of human papillomavirus vaccine coverage among young adult women in Texas, 2008. Tex Public Health J. 2013;65(1):37–40. [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang X, Onufrak S, Holt JB, Croft JB. Estimating small area (census block group) childhood obesity prevalence in the United States: a multilevel approach. Prev Chronic Dis. 2013;10:120252. doi: 10.5888/pcd10.120252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eke P, Zhang X, Hu L et al. Predicting periodontitis at state and local levels in the United States. J Dent Res. 2016;95(5):515–522. doi: 10.1177/0022034516629112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. Prevalence of doctor-diagnosed arthritis at state and county levels—United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65(19):489–494. doi: 10.15585/mmwr.mm6519a2. [DOI] [PubMed] [Google Scholar]
- 25.Berkowitz Z, Zhang X, Richards TB, Peipins L, Henley SJ, Holt JB. Multilevel small-area estimation of multiple cigarette smoking status categories using the 2012 behavioral risk factor surveillance system. Cancer Epidemiol Biomarkers Prev. 2016;25(10):1402–1410. doi: 10.1158/1055-9965.EPI-16-0244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Berkowitz Z, Zhang X, Richards T, Nadel M, Peipins L, Holt J. Multilevel small-area estimation of colorectal cancer screening in the United States. Cancer Epidemiol Biomarkers Prev. 2017;27(3):245–253. doi: 10.1158/1055-9965.EPI-17-0488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lin M, Zhang X, Holt JB, Robison V, Li C-H, Griffin SO. Multilevel model to estimate county-level untreated dental caries among US children aged 6–9 years using the National Health and Nutrition Examination Survey. Prev Med. 2018;111:291–298. doi: 10.1016/j.ypmed.2017.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Berkowitz Z, Zhang X, Richard TB et al. Multilevel regression for small-area estimation of mammography use in the United States, 2014. Cancer Epidemiol Biomarkers Prev. 2019;28(1):32–40. doi: 10.1158/1055-9965.EPI-18-0367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang X, Holt JB, Yun S, Lu H, Greenlund K, Croft JB. Validation of multilevel regression and poststratification methodology for small area estimation of health indicators from the Behavioral Risk Factor Surveillance System. Am J Epidemiol. 2015;182(2):127–137. doi: 10.1093/aje/kwv002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang Y, Holt JB, Zhang X et al. Comparison of methods for estimating prevalence of chronic diseases and health behaviors for small geographic areas: Boston validation study, 2013. Prev Chronic Dis. 2017;14:E99. doi: 10.5888/pcd14.170281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang Y, Holt JB, Xu F et al. Using 3 health surveys to compare multilevel models for small area estimation for chronic diseases and health behaviors. Prev Chronic Dis. 2018;15:E133. doi: 10.5888/pcd15.180313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.National Oceanic and Atmospheric Administration. NHC GIS Archive—Tropical Cyclone Advisory Forecast. Available at: https://www.nhc.noaa.gov/gis/archive_forecast_results.php?id=al06&year=2018&name=Hurricane. Accessed November 6, 2018.
- 33.Carr B, Walsh L, Williams J, Pryor J, Branas C. A geographic simulation model for the treatment of trauma patients in disasters. Prehosp Disaster Med. 2016;31(4):413–421. doi: 10.1017/S1049023X16000510. [DOI] [PubMed] [Google Scholar]
- 34.Shrestha SS, Sosin DM, Meltzer MI. Planning for baseline medical care needs of a displaced population after a disaster. Disaster Med Public Health Prep. 2012;6(4):335–341. doi: 10.1001/dmp.2012.58. [DOI] [PubMed] [Google Scholar]
- 35.Horn RB, Kirsch TD. Disaster Response 2.0: noncommunicable disease essential needs still unmet. APJH. 2018;108(S3):S202–S203. doi: 10.2105/AJPH.2018.304604. [DOI] [PMC free article] [PubMed] [Google Scholar]