Abstract
Objectives. To understand changes in behavioral health services utilization and expenditures before and after natural disaster with an adult Medicaid population affected by the Baton Rouge, Louisiana–area flood (August 2016).
Methods. We examined de-identified behavioral health claims data for Medicaid-insured adults in the affected region for 10 months before and after flooding (October 2015–June 2017). This constituted 273 233 provider claims for 22 196 individuals. Claims data included patient gender, behavioral health diagnoses, treatment dates, and costs. We made adjustments for Medicaid expansion by using monthly enrollment data.
Results. Overall, most male patient behavioral health care visits were for substance use disorders (33.6%) and most female patient behavioral health care visits were for depression-related disorders (30%). Both diagnostic categories increased after the flood by 66% and 44%, respectively. Expansion accounted for a 4% increase in claims. Postflood claims reflected 8% to 10% higher costs.
Conclusions. Greater amounts of behavioral health care services were sought in all 10 months of the postflood study period. We observed gender differences in use of services and diagnoses. Behavioral health care services following natural disasters must be extended longer than traditionally expected, with consideration for specific population needs.
In August 2016, a flood in Baton Rouge, the capital city of Louisiana, brought 7-trillion gallons of rain in a period of 36 hours. In addition to $20 billion in property damage, one third of the homes in the region were destroyed.1 Another 6000 businesses were flooded, and more than 278 000 residents were unable to return immediately to work.1 As is common following disasters, high rates of symptoms of depression, anxiety, and posttraumatic stress disorder (PTSD) can persist for months or years, creating a need to expand services and outreach for mental health.2
Before this flood, the Greater Baton Rouge Area (Ascension, East Baton Rouge, East Feliciana, and Livingston Parishes) was already limited in its capacity to provide behavioral health services, because, in part, of the 2013 closure of its local public hospital.3 This hospital had previously delivered care to those living in poverty or without health insurance. In fact, East and West Baton Rouge Parishes were both designated as mental health professional shortage areas for low-income populations.4
Newly elected Governor John Bel Edwards signed Executive Order JBE 16–01 on January 12, 2016. This order formally expanded Medicaid eligibility for Louisiana residents in an effort to facilitate access to care and improve outcomes for mental and physical health.5,6 Enrollment began in June 2016 with coverage beginning July of the same year and 1 month before the Baton Rouge–area flood.5
In January 2017, community and academic partners with more than a decade of history of collaboration created Resilient Baton Rouge (RBR).7–11 With infrastructure support from the Baton Rouge Area Foundation and funding from the Robert Wood Johnson Foundation, the initiative aimed to relieve existing and storm-exacerbated disparities in mental and behavioral health access and outcomes.12 RBR’s goals were to bring evidence-based models to boost local providers’ abilities to address common postdisaster behavioral health issues, focusing first on depression in adults and creating connections locally and nationally that would support community resilience and recovery. It focused on building collaboration among agencies, communities, government, and other stakeholders to bolster resilience in ways that would be meaningful to communities and to strengthen long-term ability to adapt to natural disasters and other hazards. RBR also sought to learn from community residents and service providers what gaps existed in addressing mental health and what the strengths and priorities were for improvements.12
In collaboration with RBR, in this study, we aimed to address a commonly identified community concern regarding how and whether community residents accessed behavioral health services. Specifically, we investigated pre- and postflood Medicaid utilization data to understand impacts on population behavioral health systems after a catastrophic natural disaster.
METHODS
The Louisiana State University School of Public Health, in partnership with the RBR project, requested de-identified Medicaid utilization data. We received a full data set from the Louisiana Department of Health, Office of Behavioral Health in April 2018. This data set contained the behavioral health service (i.e., mental health and substance use treatment) utilization information on more than 22 000 adult Medicaid patients (n = 22 196) from Ascension, East Baton Rouge, East Feliciana, and Livingston Parishes. These patients were documented as receiving services from October 2015 through June 2016 (10 months before the flood), and from September 2016 through June 2017 (10 months after the flood). The flood occurred August 12 through August 22 and affected all of the parishes listed.1 These data included all adult, aged 18 years or older, visits to Medicaid-funded service centers. Medicaid-funded behavioral health treatment service locations included community mental health centers, shelters, inpatient hospitals, inpatient psychiatric facilities, outpatient hospitals, residential treatment facilities, and others.
This analysis controlled for the effect of Louisiana Medicaid expansion to ascertain actual change in services utilization attributable to the flood. We identified a 4% increase in Medicaid participants by examining the difference between pre-expansion and postexpansion enrollment. Specifically, before expansion, or 10 months before the flood, 34.3% (1 602 954) of Louisiana residents were enrolled in Medicaid.13 The breakdown for the Baton Rouge area was 31% as a whole (33% East Baton Rouge, 25% Ascension, 38% East Feliciana, 30% Livingston).13 After Medicaid expansion, fiscal year 2016–2017, 38.3% (1 790 956) of Louisiana residents were enrolled in Medicaid.14 For the Baton Rouge area, this was 35% enrolled (37% East Baton Rouge, 28% Ascension, 44% East Feliciana, 33% Livingston).14 Subtracting the area’s Medicaid enrollment before expansion from the enrollment after expansion suggests a −4% adjustment is needed to compare utilization before and after the flood to account for Medicaid expansion 10 months before the flood in the years 2015 to 2016 and 10 months after the flood in 2016 to 2017. For clarity, nonadjusted numbers are also included in the findings.
RESULTS
Most patient visits were documented in East Baton Rouge Parish (73%), which also had the highest population of Medicaid-insured adults of parishes in the Baton Rouge area. The average number of visits over the 21 months reviewed was 10.0 visits per patient (range was 1 visit to 221; these data include both outpatient and inpatient or residential visit days).
Claims made were for patients who ranged in age from 18 to 90 years, with a mean pre- and postflood age of 37.3 and 36.4 years old, respectively. Claims were predominately for women in both study periods: 64.7% (n = 45 519) women before the flood and 59.8% (n = 117 538) women after the flood. Treatment service delivery locations also remained similar before and after the flood, the most common being residential treatment (37.7% of preflood claims; 40.4% of postflood claims), followed by outpatient treatment (34.2% of preflood claims; 32.1% of postflood claims) and hospital or inpatient treatment (14.9% of preflood claims; 16.8% of postflood claims).
Behavioral Health Services Utilization
During the 10 months before the flood in 2015 to 2016, there were 76 597 behavioral health claims (i.e., visits to providers for which Medicaid reimbursement was sought). These claims were made for the 58 810 Medicaid-insured adults in the 4 parishes studied. This constitutes an average claim rate of 1.302 per Medicaid-insured adult. All 4 parishes had higher average visit rates in the 10 months after the flood in 2016 to 2017, with 196 636 total claims for 107 367 individuals. This represents a claims rate of 1.831, an increase of 0.529 visits per individual from the previous year. All 4 parishes followed this overall trend of higher rates of claims per individual in 2016 to 2017 as compared with 2015 to 2016.
The average number of patient visits in the 4 parishes was 8702 per month before the flood (October 2015–July 2016) and 16 677 visits per month after the flood (September 2016–July 2017). This is almost double the utilization of behavioral health services, even when we adjusted for the 4% increase in the Baton Rouge area enrollment attributable to Medicaid expansion. The highest rates of utilization occurred 5 months after the flood when from January 2017 through June 2017 the average visits per month were 18 287. This is greater than 9500 more documented visits per month than the 4 months (September 2016–December 2016) immediately following the flood—or, with adjustment for Medicaid expansion, just less than 9000 more documented visits (Table 1).
TABLE 1—
Total Patient Visit Counts (Claims) by Month Before and After Flood: Baton Rouge Area, LA, October 2015–June 2017
| Parish |
|||||
| Date | Total Counts | Asc | EBR | EF | Liv |
| 2015 | |||||
| Oct | 9 446 | 895 | 7 097 | 203 | 1 251 |
| Nov | 7 891 | 633 | 5 947 | 188 | 1 123 |
| Dec | 7 095 | 607 | 5 174 | 172 | 1 142 |
| 2016 | |||||
| Jan | 7 532 | 713 | 5 404 | 195 | 1 219 |
| Feb | 8 229 | 790 | 11 417 | 248 | 1 179 |
| Mar | 8 820 | 929 | 6 424 | 287 | 1 180 |
| Apr | 8 977 | 792 | 6 667 | 276 | 1 242 |
| May | 9 203 | 812 | 6 972 | 271 | 1 148 |
| Jun | 9 404 | 850 | 7 061 | 223 | 1 270 |
| Jul | 12 660 | 1 217 | 9 316 | 382 | 1 745 |
| Total—Aug | 12 765 | 1 156 | 9 429 | 339 | 1 841 |
| Aug 1–11 | 5 606 | 523 | 4 122 | 158 | 803 |
| Aug 12–22a | 3 036 | 254 | 2 284 | 75 | 423 |
| Aug 23–31 | 4 123 | 379 | 3 023 | 106 | 615 |
| Sep | 13 370 | 1 339 | 9 623 | 354 | 2 054 |
| Oct | 14 849 | 1 490 | 10 558 | 393 | 2 408 |
| Nov | 14 817 | 1 308 | 10 938 | 335 | 2 236 |
| Dec | 15 473 | 1 554 | 11 240 | 341 | 2 338 |
| 2017 | |||||
| Jan | 18 211 | 1 811 | 13 241 | 380 | 2 779 |
| Feb | 16 282 | 1 660 | 11 854 | 387 | 2 381 |
| Mar | 19 832 | 2 229 | 14 059 | 452 | 3 092 |
| Apr | 18 072 | 1 992 | 12 724 | 438 | 2 918 |
| May | 19 872 | 1 992 | 14 238 | 458 | 3 184 |
| Jun | 20 433 | 2 191 | 14 530 | 509 | 3 203 |
Note. Asc = Ascension Parish; EBR = East Baton Rouge Parish; EF = East Feliciana Parish; Liv = Livingston Parish. Claims categorized according to the “service from” date. The maximum total service duration for any given claim was 97 days (for 1 claim), followed by 32 days. All claims except for 1 spanned no more than 32 days over 2 month.
Flood.
With the exception of community mental health centers, all of the Medicaid-funded behavioral health treatment service locations saw an increase in service utilization greater than what would otherwise be expected by Medicaid expansion alone (a 4% increase would be the typical expectation). The largest increase in service utilization occurred for residential placement services (from 7722 to 26 950 patients, a 249.0% increase), followed by hospital or inpatient services (from 13 821 to 27 312 patients, a 97.6% increase), and outpatient services (from 56 487 to 95 713 patients, a 69.4% increase).
Behavioral Health Diagnoses
Patients were seen for a range of diagnoses during these visits. The highest number of visits were documented as addressing depression-related issues (23.8%) and substance use–related issues (23.8%). The reasons for visits differed by gender. More than a third (33.6%) of all male visits were for substance use–related disorders (the most frequent reason given for a visit) as compared with female visits that were most often reported as addressing depression-related disorders (30.0%). Overall, women were reported more frequently accessing care, as compared with men, in every category accept substance-related disorders (Table 2).
TABLE 2—
Visits by Diagnoses and Gender Before and After Flood: Baton Rouge Area, LA, October 2015–June 2017
| Diagnosis | Total Visits, No. (%) | Men, No. (%) | Women, No. (%) |
| Schizophrenic and psychotic disorders | 50 342 (18.4) | 28 393 (26.7) | 21 949 (13.1) |
| Bipolar disorders | 32 049 (11.7) | 7 360 (6.9) | 24 689 (14.8) |
| Depressive disorders | 65 009 (23.8) | 14 858 (14.0) | 50 151 (30.0) |
| Anxiety disorders | 18 987 (6.9) | 4 188 (3.9) | 14 799 (8.9) |
| Trauma and stress disorders | 10 176 (3.7) | 2 161 (2.0) | 8 015 (4.8) |
| Substance and addictive disorders | 64 981 (23.8) | 35 632 (33.6) | 29 349 (17.6) |
| All others | 31 689 (11.6) | 13 584 (12.8) | 18 105 (10.8) |
| Total | 273 233 | 106 176 | 167 057 |
Note. The following classification scheme was used for patient diagnoses, based on the International Classification of Diseases, Tenth Revision (ICD-10; Geneva, Switzerland: World Health Organization; 1992) system: schizophrenia and psychotic–related disorders: ICD F20-29; bipolar disorders: ICD F30-31; depressive disorders: ICD F32-33; anxiety disorders: ICD F40-419; trauma and stress-related disorders: ICD F43-439; substance use and addictive disorders: ICD F10-19.
Patient Visits by Diagnosis Counts
Diagnoses seen in behavioral health settings supported by Medicaid also fluctuated before and after the flood. Specifically, the average monthly visits for diagnosed behavioral health conditions seen after the flood all showed increases. The largest average increases were in visits for substance-related and addictive disorders (+70%), trauma and stress-related disorders (+66%), anxiety disorders (+49%), and depressive disorders (+48%; with adjustment for Medicaid expansion—66%, 62%, 45%, and 44%, respectively). In terms of total numbers of visits, substance-related and addictive disorders and depressive disorders placed the most demand on settings (Table 3).
TABLE 3—
Behavioral Health Diagnostic Categories Before and After Flood: Baton Rouge–Area, LA, October 2015–June 2017
| Diagnostic Category |
|||||||
| Date | Schizophrenic and Psychotic | Bipolar | Trauma and Stress | Depressive | Anxiety | Substance and Addictive | Other |
| 2015 | |||||||
| Oct | 2 683 | 1 181 | 249 | 1 940 | 577 | 1 430 | 1 092 |
| Nov | 2 189 | 915 | 206 | 1 546 | 474 | 1 431 | 907 |
| Dec | 1 679 | 927 | 238 | 1 789 | 500 | 977 | 790 |
| 2016 | |||||||
| Jan | 1 675 | 991 | 196 | 2 054 | 493 | 992 | 946 |
| Feb | 1 957 | 1 100 | 212 | 2 188 | 471 | 1 110 | 985 |
| Mar | 2 081 | 1 193 | 236 | 2 370 | 620 | 1 160 | 953 |
| Apr | 2 150 | 1 148 | 244 | 2 411 | 555 | 1 163 | 1 084 |
| May | 2 183 | 1 248 | 268 | 2 459 | 586 | 1 261 | 993 |
| Jun | 2 123 | 1 293 | 255 | 2 494 | 662 | 1 334 | 1 053 |
| July | 2 434 | 1 462 | 335 | 3 144 | 838 | 3 016 | 1 122 |
| Before flood, mean | 2 115 | 1 146 | 244 | 2 240 | 578 | 1 387 | 993 |
| Total Aug | 2 397 | 1 356 | 411 | 3 184 | 881 | 2 939 | 1 202 |
| Aug 1–11 | 1 034 | 587 | 158 | 1 418 | 401 | 1 311 | 526 |
| Aug 12–22a | 513 | 309 | 104 | 705 | 186 | 817 | 291 |
| Aug 23–31 | 850 | 460 | 149 | 1 061 | 294 | 811 | 385 |
| Sep | 2 251 | 1 500 | 526 | 3 321 | 928 | 3 153 | 1 338 |
| Oct | 2 401 | 1 722 | 575 | 3 631 | 931 | 3 853 | 1 374 |
| Nov | 2 390 | 1 692 | 595 | 3 727 | 952 | 3 691 | 1 383 |
| Dec | 2 259 | 1 741 | 578 | 3 939 | 991 | 4 205 | 1 397 |
| 2017 | |||||||
| Jan | 2 807 | 2 002 | 701 | 4 452 | 1 214 | 5 017 | 1 586 |
| Feb | 2 535 | 1 684 | 663 | 3 973 | 1 098 | 4 611 | 1 354 |
| Mar | 2 893 | 2 123 | 834 | 4 834 | 1 327 | 5 490 | 1 790 |
| Apr | 2 575 | 1 955 | 711 | 4 527 | 1 240 | 4 928 | 1 595 |
| May | 2 734 | 2 115 | 911 | 5 102 | 1 355 | 5 323 | 1 763 |
| Jun | 2 650 | 2 140 | 986 | 5 337 | 1 360 | 5 663 | 1 765 |
| After flood, mean | 2 550 | 1 867 | 708 | 4 284 | 1 140 | 4 593 | 1 535 |
| Increase | 435 | 721 | 464 | 2 044 | 562 | 3 206 | 542 |
| Total | 49 046 | 31 488 | 9 930 | 68 422 | 18 053 | 62 747 | 26 472 |
Note. The following classification scheme was used for patient diagnoses, based on the International Classification of Diseases, Tenth Revision (ICD-10; Geneva, Switzerland: World Health Organization; 1992) system: schizophrenia and psychotic–related disorders: ICD F20-29; bipolar disorders: ICD F30-31; depressive disorders: ICD F32-33; anxiety disorders: ICD F40-419; trauma and stress-related disorders: ICD F43-439; substance use and addictive disorders: ICD F10-19.
Flood.
Medicaid Costs
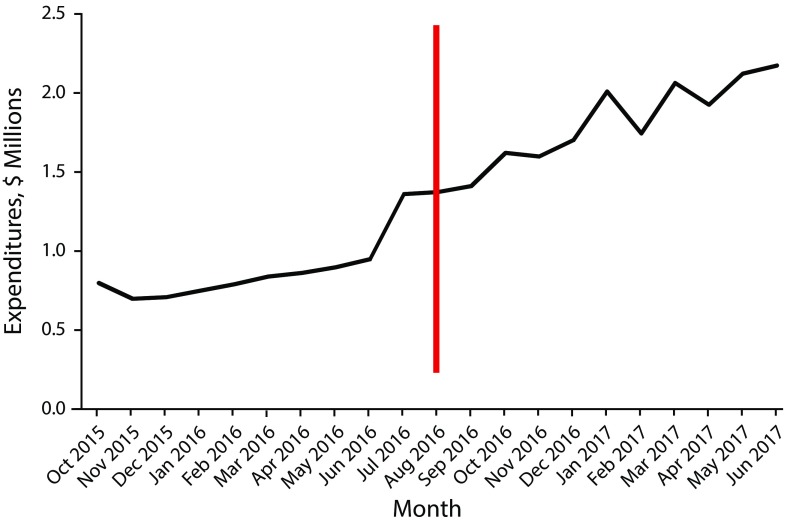
The total Medicaid paid for services during the study period was $28 334 973 with an average cost of $104 per visit. These costs are different before and after the flood. Before the flood, the total costs for visits was $7 260 059, with an average visit costing $95. After the flood, Medicaid paid $21 074 914, with an average service visit costing $107. This represents a 14% increase in payments after the flood (an 8–10% increase when we adjusted for Medicaid expansion). Figure 1 shows the average monthly cost of mental health treatment reimbursements throughout the entire study, before and after the flood.
FIGURE 1—
Monthly Medicaid Behavioral Health Expenditure Before and After Flood: Baton Rouge Area, LA, 2015–2017
DISCUSSION
This case study of Medicaid-funded behavioral health service utilization 10 months before the flood and 10 months after the flood supports the need for increased behavioral health services, particularly after a disaster. Previous work has demonstrated that one third of individuals with significant exposure to a natural disaster develop behavioral health disorders.15 A theoretical description of how individuals come to terms with such events and work through grief is described in phases of disaster by DeWolfe. DeWolfe’s framework describes 4 phases of a disaster: mitigation, preparedness, response, and recovery.16,17 During the response stage, communities can see an increase in bonding, often referred to as the “honeymoon phase.” This newfound cohesion can provide initial improvement in coping but is often not sustained. Thus, behavioral health conditions may not emerge until after this honeymoon phase is complete. De Ville de Goyet et al. expand DeWolfe’s framework, particularly the recovery stage of disaster, stating the need for psychosocial aftercare services to be explicitly expanded for at least 6 months after a disaster.18 To mitigate barriers to care, previous literature has suggested that such expanded services should be accessible regardless of health insurance status.19 The present study, however, provides insight to the unique situation of a disaster event when insurance access is expanded in addition to behavioral health services.
Palinkas et al. found that high rates of symptoms of depression, anxiety, and PTSD persisted in the months, and even years, after disasters, creating a need to expand services and outreach for mental health.2 Higher utilization of services was found in this study as well, consistent with this literature. The current study also expands research by Palinkas et al. via inclusion of substance-related disorders, which rose 70%, as compared with trauma, anxiety, and depression-related issues that increased approximately 48%.2
Previous studies have shown gender differences in use of behavioral health services and diagnoses.20–22 Specifically, earlier data on treatment patterns have shown higher rates of visits and treatment with women.20 Gender gaps have also been observed in diagnoses, with men having higher rates of substance use disorders and women having higher rates of both depression and anxiety-related conditions.21,22 The current study parallels these data and expands upon the research by showing an accentuation of needs in these treatment areas after a disaster. The practice implication of these data suggests a need for increased clinical focus on substance use and depression and anxiety disorders and gender considerations for each in the aftermath of a disaster. Further study of the gendered differences in the acute and long-term psychosocial effects of a natural disaster would contribute to the growing body of research examining gender and disasters.23,24
Claims data reflect higher utilization and costs immediately following Medicaid expansion, with a slight plateau in the brief period between expansion and the flood. However, we observed greater utilization of behavioral health services in all 10 study months after the flood even when we adjusted for the increase in the number of Medicaid enrollees during that same period. Thus, the traditional recommendation of psychosocial services expanding for at least 6 months after a disaster, as argued by De Ville de Goyet et al., may not be adequate to address needs during the recovery phase of a disaster.18 Other natural disaster studies have found persistence of treatment needs up to 2 years after an event.25
Previous research on natural disasters in Louisiana has found significant prevalence of PTSD and other mood disorders in affected populations.26 Galea et al. found that natural disasters in Louisiana affected behavioral health outcomes in association with disaster exposure and independently of socioeconomic status, which suggests that the findings of this study are likely generalizable to the entire affected population of Baton Rouge rather than only Medicaid-insured individuals.26 It is reasonable to conclude that all health care networks (private and public) should plan to expand and facilitate access to behavioral health services following natural disasters, in particular for the treatment of depression-related disorders and substance use–related disorders. Service capacity–building efforts focused on expanding behavioral health outreach and training for providers in evidence-based therapies may be particularly effective in postdisaster contexts.10–12
Behavioral health care access in response to natural disasters is of particular importance in Louisiana. In a previous study of behavioral health care and primary care integration, 76% of individuals who screened positive for PTSD had a history of natural disaster exposure. The majority of patients in that study were female, consistent with the present findings.27
Limitations
Following Hurricane Katrina in 2005, the majority of individuals who received treatment of behavioral health conditions did not receive psychotherapy, and the majority were not treated by a behavioral health specialist.28 Instead, most received treatment by a general health care practitioner.28 Our study of the Baton Rouge–area flood did not differentiate among types of treatment or providers, though this is recommended as an area of future examination. Furthermore, we did not specifically survey the effect of the flood upon individuals who were receiving behavioral health services before disaster exposure. Individuals with predisaster behavioral health disorders may have increased risk for poor health outcomes,29 and the effect of the flood on this subpopulation merits additional, future study.
This retrospective study did not exclude new Medicaid enrollees in its analyses because the database utilized did not include this information; rather, the information was de-identified. This limitation did not allow for isolated analyses of individuals who were Medicaid beneficiaries before the flood. This study posits that if the flood had not occurred, there would have been an expected increase of 4% in behavioral health visits or claims for this region. However, following the flood, there were significantly more claims than what would typically be expected to be attributable to Medicaid expansion alone, thus arguing a disaster effect regardless of expansion. Finally, this study was limited to the effect of the flood on Medicaid insurance claims related to behavioral health services.
Conclusions
Following the Baton Rouge–area flood, increased amounts of behavioral health services were sought in all 10 months of the postflood study period. In addition to utilization increases, there were differences in treatment patterns and diagnoses between genders. In particular, women had higher rates of visits and treatment and greater diagnoses of depression and anxiety disorders while men had higher rates of substance use–disorder diagnosis. The findings of this study argue the need for the extension of behavioral health care services following a disaster and considerations for the gendered differences in need within the population. Disasters are known to have an impact on service utilization in other medical fields,30 and the impact of the flood and Louisiana Medicaid utilization in other health categories (e.g., chronic disease management, infectious disease incidence) remains to be determined.
CONFLICTS OF INTEREST
The authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or nonfinancial interest in the subject matter or materials discussed in this article.
HUMAN PARTICIPANT PROTECTION
All work was completed under institutional review board approval from the Louisiana State University Health Sciences Center New Orleans (approval no. 9852).
REFERENCES
- 1.Gallo A, Russell G. Sobering stats: 110,000 homes worth $20B in flood-affected areas in Baton Rouge region, analysis says. The Advocate. August 2016. Available at: http://www.theadvocate.com/louisiana_flood_2016/article_62b54a48-662a-11e6-aade-afd357ccc11f.html. Accessed October 12, 2018.
- 2.Palinkas LA, Petterson JS, Russell J, Downs MA. Community patterns of psychiatric disorders after the Exxon Valdez oil spill. Am J Psychiatry. 1993;150(10):1517–1523. doi: 10.1176/ajp.150.10.1517. [DOI] [PubMed] [Google Scholar]
- 3.Kaliba A., Earl K. Long Hospital closure community inputs on potential uses of the property and economic profiles of residents living within the vicinity of the property. 2015. Available at: https://www.researchgate.net/publication/297759100_Earl_K_Long_Hospital_Closure_Community_Inputs_on_Potential_Uses_of_the_Property_and_Economic_Profiles_of_Residents_Living_within_the_Vicinity_of_the_Property. Accessed October 12, 2018.
- 4.Louisiana Department of Health and Hospitals. Mental health professional shortage areas. 2018. Available at: http://ldh.la.gov/assets/oph/pcrh/HPSAMaps/HPSA_Mental_Shortages_woLabels.jpg. Accessed October 12, 2018.
- 5.Edwards JB, Gee R. Medicaid Expansion 2016/2017. Baton Rouge, Louisiana. 2017. Available at: http://ldh.la.gov/assets/HealthyLa/Resources/MdcdExpnAnnlRprt_2017_WEB.pdf. Accessed October 12, 2018.
- 6.Louisiana Executive Order No. JBE 16-01. Medicaid Expansion. 2016. Available at: http://gov.louisiana.gov/assets/ExecutiveOrders/JBE1601.pdf. Accessed October 12, 2018.
- 7.Arevian AC, Castillo E, Chung B et al. The Community and Patient Partnered Research Network (CPPRN): application of patient-centered outcomes research to promote behavioral health equity. Ethn Dis. 2018;28(2 suppl):295–302. doi: 10.18865/ed.28.S2.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ngo VK, Centanni A, Wong E, Wennerstrom A, Miranda J. Building capacity for cognitive behavioral therapy delivery for depression in disaster-impacted contexts. Ethn Dis. 2011;21(3 suppl 1):S1–S44. [PMC free article] [PubMed] [Google Scholar]
- 9.Bentham W, Badger K, Vannoy S, Wennerstrom A, Springgate B. Opportunities and challenges of implementing collaborative mental health care in post-Katrina New Orleans. Ethn Dis. 2011;21(3 suppl 1):30–37. [PMC free article] [PubMed] [Google Scholar]
- 10.Springgate BF, Wennerstrom A, Meyers D et al. Building community resilience through mental health infrastructure and training in post-Katrina New Orleans. Ethn Dis. 2011;21(3 suppl 1):20–29. [PMC free article] [PubMed] [Google Scholar]
- 11.Wennerstrom A, Vannoy S, Allen C et al. Community-based participatory development of community health worker mental health outreach role to extend collaborative care in post Katrina New Orleans. Ethn Dis. 2011;21(3 suppl 1):45–51. [PMC free article] [PubMed] [Google Scholar]
- 12.Keegan R, Grover LT, Patron D et al. Case study of resilient Baton Rouge: applying depression collaborative care and community planning to disaster recovery. Int J Environ Res Public Health. 2018;15(6):E1208. doi: 10.3390/ijerph15061208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Louisiana Department of Health. 2016. Louisiana Medicaid 2016 Annual Report. Available at: http://ldh.la.gov/assets/medicaid/AnnualReports/2016AnnualReport.pdf. Accessed October 12, 2018.
- 14.Louisiana Department of Health. Louisiana Medicaid 2017 Annual Report. Available at: http://ldh.la.gov/assets/medicaid/AnnualReports/MedicaidAnnualReport2017.pdf. Accessed October 12, 2018.
- 15.North CS, Pfefferbaum B. Mental health response to community disasters: a systematic review. JAMA. 2013;310(5):507–518. doi: 10.1001/jama.2013.107799. [DOI] [PubMed] [Google Scholar]
- 16.DeWolfe DJ. Training manual for mental health and human service workers in major disasters. 2nd ed. HHS Publication No. ADM 90-538. Rockville, MD: Substance Abuse and Mental Health Services Administration, Center for Mental Health Services; 2000.
- 17.RestoreYourEconomy. Phases of disaster. Available at: http://restoreyoureconomy.org/disasteroverview/phases-of-disaster. Accessed October 12, 2018.
- 18.de Ville de Goyet C, Marti RZ, Osorio C. Natural disaster mitigation and relief. In: Jamison DT, Breman JG, Measham AR, editors. Disease Control Priorities in Developing Countries. New York, NY: Oxford University Press; 2006. pp. 1147–1161. [Google Scholar]
- 19.Lowe SR, Norris FH, Galea S. Mental health service utilization among natural disaster survivors with perceived need for services. Psychiatr Serv. 2016;67(3):354–357. doi: 10.1176/appi.ps.201500027. [DOI] [PubMed] [Google Scholar]
- 20.Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve month use of mental health services in the United States. Arch Gen Psychiatry. 2005;62(6):629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- 21.McHugh RK, Votaw VR, Sugarman DE, Greenfield SF. Sex and gender differences in substance use disorders. Clin Psychol Rev. 2018;66:12–23. doi: 10.1016/j.cpr.2017.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Altemus M, Sarvaiya N, Neill-Epperson C. Sex differences in anxiety and depression clinical perspectives. Front Neuroendocrinol. 2014;35(3):320–330. doi: 10.1016/j.yfrne.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fordham M. Gender, sexuality and disaster. In: Wisner B, Gaillard JC, Kelman I, editors. Handbook of Natural Hazards and Disaster Risk Reduction. Abingdon, UK: Routledge; 2012. pp. 424–434. [Google Scholar]
- 24.Gaillard JC, Sanz K, Balgos BC et al. Beyond men and women: a critical perspective on gender and disaster. Disasters. 2017;41(3):429–447. doi: 10.1111/disa.12209. [DOI] [PubMed] [Google Scholar]
- 25.Isaranuwatchai W, Coyte PC, McKenzie K, Noh S. The 2004 tsunami and mental health in Thailand: a longitudinal analysis of one and two-year post-disaster data. Disasters. 2017;41(1):150–170. doi: 10.1111/disa.12188. [DOI] [PubMed] [Google Scholar]
- 26.Galea S, Brewin CR, Gruber M et al. Exposure to hurricane-related stressors and mental illness after Hurricane Katrina. Arch Gen Psychiatry. 2007;64(12):1427–1434. doi: 10.1001/archpsyc.64.12.1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Osofsky HJ, Osofsky JD, Hansel TC et al. The Louisiana mental and behavioral health capacity project trauma-informed integrated care model and improved posttraumatic stress outcomes. J Public Health Manag Pract. 2017;23(6):S25–S31. doi: 10.1097/PHH.0000000000000652. [DOI] [PubMed] [Google Scholar]
- 28.Wang PS, Gruber MJ, Powers RE et al. Disruption of existing mental health treatments and failure to initiate new treatment after Hurricane Katrina. Am J Psychiatry. 2008;165(1):34–41. doi: 10.1176/appi.ajp.2007.07030502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tharp AT, Constans JI, Yin R et al. Service provision in disaster preparation, response, and recovery for individuals with predisaster mental illness. Am J Disaster Med. 2012;7(3):171–174. doi: 10.5055/ajdm.2012.0092. [DOI] [PubMed] [Google Scholar]
- 30.Gruebner O, Lowe SR, Sykora M et al. A novel surveillance approach for disaster mental health. PLoS One. 2017;12(7):e0181233. doi: 10.1371/journal.pone.0181233. [DOI] [PMC free article] [PubMed] [Google Scholar]