Abstract
Cross-sectional data reveal that smoking cigarettes is highly prevalent among those who are food insecure. However, there is limited and conflicting evidence concerning whether causal factors may influence associations of food insecurity with smoking behavior. Additionally, temporality is a core feature of food insecurity that should be considered when examining linkages between food insecurity and health behaviors like smoking cessation. In 2019, data were extracted from waves 2012 and 2014 of the Health and Retirement Study—a representative sample of U.S. adults over age 50. Analyses were limited to those who smoked cigarettes in 2012 (n=2,197). Food insecurity was assessed in 2012 and 2014 to indicate food insecurity transitions: (1) initially food insecure (food insecure in 2012 only); (2) became food insecure (food insecure in 2014 only); (3) remained food insecure (food insecure in 2012 and 2014), and; (4) not food insecure (reference group). Multivariable logistic regression examined odds of smoking cessation in 2014 due to food insecurity transition. Becoming food insecure was associated with a 2.0 (95% confidence interval=1.2-3.4) higher odds of smoking cessation. Employment loss or retirement (p=0.020) and diagnosis of a new chronic condition (p=0.026) were also associated with higher odds of smoking cessation. In older U.S. adults, smoking cessation was associated with decreased spending power and new health problems. Future studies should examine whether findings of this study may be similar among younger adults and; whether those who quit smoking due to food insecurity are more susceptible to relapse than those who quit due to other factors.
Keywords: tobacco use, smoking cessation, gerontology, health behavior, coping
INTRODUCTION
Smoking cigarettes is one of the most widely recognized public health problems, associated with numerous chronic conditions from cancer1 to cardiovascular disease2—not to mention the risks due to passive exposure among nonsmokers.3 Campaigns funded by the government and nonprofits in the United States dedicate hundreds of millions dollars annually with the aim of reducing smoking and associated health care costs.4,5 Smoking cessation has health benefits across the life course,6 reducing excess risk of mortality even into old age.7
Smoking cessation is particularly difficult for those with lower socioeconomic standing8,9— contributing to pervasive health disparities.10,11 Evidence suggests community norms, stressful environments and isolation from mainstream smoking perceptions may play a role in lower smoking cessation rates among these populations.12 Food insecurity, which refers to the physical pain of hunger as well as the more common experience of worrying about having enough healthy food to eat,13 could be a contributing factor to poorer smoking cessation among low-income communities.
Cross-sectional data reveal that smoking is highly prevalent among those who are food insecure. For example, among low-income Americans, smoking is 38% more prevalent among households that are food insecure.14 However, there is limited and conflicting evidence concerning the causal nature of this relationship. Longitudinal analysis indicates that those who smoke cigarettes are more likely to become food insecure following economic disruptions, and recovery from food insecurity takes longer among persons who smoke15—likely because the added expense further strains financial resources.16 Additionally, data reveal people use cigarettes to ease psychological distress associated with poor socioeconomic conditions such as food insecurity.17,18 Smoking cigarettes may also provide a coping strategy to aid with appetite suppression during times of austerity.19 In particular, the influence of food insecurity on smoking cessation is poorly understood.
A core feature of food insecurity is that severity can vary over time—whether over the course of a month, as time passes since receiving a pay check or social assistance,20 or; over longer periods, as broader financial circumstances change (e.g. job loss).21 Simply considering the influence of static food insecurity on health and health behaviors overlooks the potential unique role of food insecurity transitions—such as persistent food insecurity or transitioning out of food insecurity. Evidence suggests that prolonged exposure to stressors, such as food insecurity, may diminish the ability to control cravings,22 and; greater stress is associated with higher nicotine dependence.23 Therefore, it is hypothesized that remaining food insecure and becoming food insecure will be associated with smoking more cigarettes and a decreased ability to stop smoking cigarettes than those who do not experience food insecurity. Using longitudinal data from a representative sample of U.S. adults over 50 years, this study examined the association of food insecurity transitions with smoking cessation and change in smoking consumption over two years among older adults.
METHODS
Sample
Data came from the Health and Retirement Study (HRS)—a nationally representative sample of >37,000 individuals over age 50 in 23,000 households in the United States.24 The HRS sample has been built overtime, starting with recruitment of the initial cohort in 1992 of persons born 1931-41. Starting in 1998, HRS made its sample fully representative of the U.S. population over age 50 by enrolling additional age cohorts of persons born 1924-30 and 1942-47. Additionally, HRS uses a steady-state design; meaning, every six years the HRS sample is replenished by recruiting younger age cohorts not previously represented in order to maintain a nationally representative sample. Core questionnaires are mailed every two years to collect information on demographics, socioeconomic status, health and aging-related topics (response rate in 2010 was 88.6%). HRS was approved by the University of Michigan Health Sciences/Behavioral Science Institutional Review Board, and; informed consent is obtained from participants prior to questionnaire administration. HRS is funded by the National Institute on Aging and the Social Security Administration.
Analyses were limited to waves 2012 and 2014—the most recent years of data available so that findings would be most applicable to current economic circumstances and health behavior trends. Those who were not current smokers in 2012 were excluded from the study, no other exclusion criteria were applied. Among the 2,650 current smokers who participated in HRS wave 2012, 2,296 also participated in HRS wave 2014. The analysis sample was limited to 2,197 persons with complete-case data for variables of interest (96% of the eligible sample). All analyses of this study occurred in 2019.
Measures
Food Insecurity—
In the United States, the standard for assessing household food insecurity is the U.S. Department of Agriculture (USDA) 18-Item Food Security Tool.25 Additionally, there is a 2-item screen that can identify household food insecurity with a sensitivity of 97% and specificity of 83% compared to the USDA 18-Item Food Security Tool, given an affirmative answer to (1) “Within the past 12 months we worried whether our food would run out before we got money to buy more”, or; (2) “Within the past 12 months the food we bought just didn’t last and we didn’t have money to get more”. In HRS, two survey items comparable to the 2-item food insecurity screen, and, previously used to test associations of food insecurity with diabetic morbidity and depression symptomology within HRS,26 were used to identify food insecurity in 2012 and 2014.
HRS participants were asked “Do you have enough money to buy the food you need at all times?” since their last interview, recorded as yes or no. Those who did not respond “no”, were then asked “Do you eat less than you feel you should because of a lack of money?’. Those who did not have enough money to buy food or ate less due to a lack of money were considered food insecure. Binary food insecurity variables in 2012 and 2014 were used to create a 4-category food insecurity transition variable: (1) Not food insecure—not food insecure in 2012 or 2014, which served as the reference group; (2) Initially food insecure—food insecure only in 2012; (3) Became food insecure—food insecure only in 2014, and; (4) Remained food insecure—food insecure in 2012 and 2014.
Smoking behavior—
Both smoking cessation and change in smoking consumption were used as outcome measures for smoking behavior. In 2014, participants were asked “ Do you smoke cigarettes now?”. This was used to create a binary variable for smoking cessation, no longer current smokers vs. current smokers (reference group).
Participants were also asked, “About how many cigarettes or packs do you usually smoke in a day now?” in 2012 and 2014. Packs were considered to have 20 cigarettes. This was used to determine change in cigarette smoking consumption (more, fewer or the same amount [reference]). Those who no longer smoked in 2014 were considered to have smoked fewer cigarettes.
Covariates—
A number of demographic and socioeconomic covariates were included in analyses. Demographic covariates included age (continuous measure), gender (male [reference] vs. female), race/ethnicity (non-Hispanic White [reference] vs. non-Hispanic Black, other) and marital status in 2012 (married [reference] vs. divorced or separated, widowed, single or never married). Socioeconomic covariates included educational attainment at HRS enrollment (≥high school degree [reference] vs. <high school degree), work status in 2012 (work for pay [reference] vs. do not work for pay), retirement status in 2012 (partially or fully retired [reference] vs. not retired) and household income-to-poverty ratio in 2012 (continuous). Household income sources included earnings, unemployment, workers’ compensation, Social Security, public assistance (e.g. welfare/TANF), veterans’ benefits, pension and retirement income, interest, dividends, rents, royalties, income from estates and trusts, educational assistance, alimony, child support and other sources except noncash benefits (i.e. food stamps/Supplemental Nutrition Assistance Program benefits) from all resident family members.
Additionally, analyses adjusted for life transitions that could confound associations of food insecurity transitions with smoking cessation. Indicators for life transitions included change in marital status, change in income and employment transition. Those who no longer work for pay may lose access to social networks that are important for influencing or reinforcing certain health behaviors.27 Those who indicated that they were widowed or divorced in 2014 but were not widowed or divorced in 2012, were considered to have experienced a change in marital status (no change in marital status or unmarried in 2012 [reference]). Among those who worked for pay in 2012, those who indicated that they did not work for pay in 2014 were considered to have experienced an employment transition. Additionally, among those who were not retired in 2012 but did indicate that they were partially or fully retired in 2014 were considered to have experienced an employment transition. Those who did not experience a loss of work for pay or who did not become retired in 2014 served as the reference group for employment transition. Change in income was a continuous measure calculated by the difference in income-to-poverty-ratio between 2012 and 2014. Lastly, analyses accounted for being diagnosed with a new chronic condition, since individuals may be more likely to change their behavior following disease onset,28 and; costs associated with hospitalization could increase risk of food insecurity. In 2012 and 2014, number of chronic conditions was determined based on which of the following 8 diagnoses a respondent reported a history of: psychiatric problems, arthritis, high blood pressure, heart disease, stroke, diabetes, lung disease and cancer. Those with a greater number of chronic conditions in 2014, than in 2012, were considered to have received a new diagnosis. Those without a new diagnosis served as the reference group.
Depressive disorder has been associated with poorer smoking cessation29 and has a bidirectional relationship with food insecurity30, therefore sensitivity analyses accounted for depression status. In 2012, HRS assessed depression over the previous year using the World Health Organization Composite International Diagnostic Interview Short Form (CIDI-SF). The CIDI-SF is designed to identify Major Depression based on the Diagnostic and Statistical Manual of Mental Disorders criteria 31. To be considered depressed, respondents must report symptoms of anhedonia or depressed mood most of the day for over half of a 2-week period or longer to be considered depressed. Those that meet this screening requirement complete an additional seven items which assess symptoms of lost interest, fatigue, weight change, trouble with sleep, trouble concentrating, feeling down and thoughts of death. HRS respondents who scored ≥3 depression symptoms on the 0 to 7 symptom scale were considered to have experienced a major depressive episode in 2012 32.
Statistical Approach
All analyses were conducted using SAS 9.433 and used survey procedures to account for HRS survey design. First, X2 tests compared the distribution of demographic factors; socioeconomic status; change in marital status, income and employment; diagnosis of new chronic conditions and; smoking cessation across levels of food insecurity transitions. Given that analysis of longitudinal data may be sensitive to attrition bias,41 demographic and socioeconomic characteristics for those who participated in the HRS 2012 and 2014 wave (i.e. the analysis sample) were compared.
Next, multivariable logistic regression examined the association of food insecurity transitions with smoking cessation. Model 1 accounted for demographic factors (age, gender, race/ethnicity and marital status). Model 2 accounted for demographic factors and socioeconomic status (all variables in Model 1, plus educational attainment, household income-to-poverty ratio, work and retirement status).
Model 3 accounted for demographic factors, socioeconomic status and life transitions (all variables in Model 2, plus becoming divorced or widowed, change in household income, employment transition and being diagnosed with a new chronic condition). Interaction terms of food insecurity with demographic (age, marital status, gender) and socioeconomic (work status, retirement status, educational attainment) factors were tested in Model 3 using separate models.
Multinomial logistic regression was used to determine the association of food insecurity transitions with change in smoking behavior, using no change in cigarette consumption as the reference. Analyses accounted for demographic factors, socioeconomic status and life transitions. Interaction terms of food insecurity by demographic and socioeconomic factors were tested using separate models. Finally, sensitivity analyses included 2012 depression status as a covariate in fully adjusted models for both smoking cessation and change in smoking consumption.
RESULTS
Table 1 describes the analysis sample (n=2,197). Among those who smoked cigarettes in 2012, 384 persons no longer smoked in 2014 (17%), 185 persons were initially food insecure (8%), 174 persons became food insecure in 2014 (8%), 279 persons remained food insecure (13%), while a majority did not report food insecurity (n=1,559; 71%). Overall, social and economic disadvantage were less common among those who were food secure. When looking across food insecurity transitions, those who remained food insecure represented the lowest income group (1.5 household income-to-poverty ratio (IPR); 95% confidence interval (CI)=1.3, 1.7) compared to those who were initially food insecure or became food insecure (average IPR~=2.0). Not earning income; being separated, divorced or widowed; being female and; being non-Hispanic Black was also more common among those who remained food insecure in 2014 compared to initially being food insecure or becoming food insecure.
Table 1.
Characteristics by food insecurity (FI) transition among older adults who smoked in 2012, 2012 to 2014a,b
| FI Transition 2012 to 2014 | |||||
|---|---|---|---|---|---|
| Characteristics | Not FI n = 1,559 |
Initially FI in 2012 n = 185 |
Became FI in 2014 n = 174 |
Remained FI in 2014 n = 279 |
Pc |
| Age, mean (95% CI) | 62.1 (61.5, 62.8) | 60.0 (59.1, 60.9) | 59.4 (58.1, 60.7) | 59.5 (58.6, 60.5) | <0.001 |
| Gender | 0.002 | ||||
| Male | 733 (76.5) | 95 (9.1) | 72 (6.6) | 99 (7.8) | |
| Female | 826 (71.2) | 90 (7.7) | 102 (7.3) | 180 (13.7) | |
| Race/ethnicity | <0.001 | ||||
| Non-Hispanic White | 965 (78.8) | 77 (7.4) | 66 (5.4) | 107 (8.4) | |
| Non-Hispanic Black | 377 (60.5) | 75 (12.1) | 65 (9.9) | 125 (17.5) | |
| Other | 217 (61.8) | 33 (9.2) | 43 (12.7) | 47 (16.4) | |
| Marital status | <0.001 | ||||
| Married | 747 (81.3) | 58 (6.5) | 23 (7.4) | 71 (5.8) | |
| Separated or divorced | 347 (66.2) | 51 (9.6) | 51 (8.4) | 93 (15.8) | |
| Widowed | 205 (70.3) | 21 (7.6) | 69 (6.4) | 40 (14.7) | |
| Single or never married | 260 (68.4) | 55 (11.5) | 31 (6.1) | 75 (14.0) | |
| Educational attainmentd | 0.003 | ||||
| < High school | 1,719 (77.0) | 187 (7.1) | 160 (6.8) | 195 (9.1) | |
| High school degree or above | 10,000 (90.7) | 449 (3.6) | 370 (2.8) | 386 (3.0) | |
| Income-to-poverty ratio (IPR), mean (95% CI) | 4.6 (4.2, 5.1) | 2.1 (1.6, 2.7) | 1.9 (1.5, 2.3) | 1.5 (1.3, 1.7) | <0.001 |
| Work status | <0.001 | ||||
| Do not work for income | 892 (68.9) | 125 (9.3) | 118 (7.9) | 205 (13.8) | |
| Work for income | 667 (80.0) | 60 (7.2) | 56 (5.8) | 74 (7.0) | |
| Retirement status | 0.42 | ||||
| Not retired | 703 (75.2) | 84 (8.7) | 77 (6.3) | 128 (9.7) | |
| Partially or fully retired | 856 (72.5) | 101 (8.1) | 97 (7.6) | 151 (11.9) | |
| Divorced or widowed in 2014 | 0.002 | ||||
| No | 74 (67.2) | 11 (10.1) | 15 (16.9) | 10 (5.8) | |
| Yes | 1,485 (74.2) | 174 (8.3) | 159 (6.4) | 269 (11.1) | |
| IPR change in 2014, mean (95% CI) | −0.5 (−0.8, −0.1) | 0.1 (−0.1, 0.4) | 0.0 (−0.2, 0.3) | 0.1 (−0.1, 0.3) | 0.041 |
| Employment transition in 2014 | 0.22 | ||||
| No | 1,320 (74.8) | 152 (7.8) | 140 (6.8) | 222 (10.5) | |
| Yes | 239 (68.6) | 33 (11.2) | 34 (7.8) | 57 (12.4) | |
| New health diagnosis in 2014e | 0.24 | ||||
| No | 1,204 (75.0) | 138 (8.4) | 125 (6.4) | 200 (10.1) | |
| Yes | 355 (70.0) | 47 (8.2) | 49 (8.7) | 79 (13.1) | |
| Smoking cessation in 2014 | 0.023 | ||||
| No | 1,297 (74.4) | 156 (8.7) | 133 (6.0) | 227 (10.9) | |
| Yes | 262 (71.0) | 29 (7.0) | 41 (11.7) | 52 (10.3) | |
| Change in smoking consumptionf | 0.22 | ||||
| Same | 541 (77.4) | 65 (8.9) | 49 (4.9) | 76 (8.8) | |
| More | 333 (72.5) | 32 (6.9) | 35 (7.5) | 66 (13.2) | |
| Fewer | 685 (71.6) | 88 (8.7) | 90 (8.4) | 137 (11.3) | |
Data come from the U.S. Health and Retirement Study (HRS) and cell values represent column percentages unless otherwise indicated
All variables assessed in 2012 unless otherwise indicated
X2 or F test
Assessed during initial HRS enrollment wave
Additional number of chronic conditions in 2014 vs. 2012
Number of cigarettes per day in 2014 vs. 2012
When considering smoking behavior, proportions of smoking cessation were similar across food insecurity transitions—except for those who became food insecure. Among those who quit smoking, 12% became food insecure, whereas only 6% of those who did not quit smoking became food insecure. For change in smoking consumption, proportions did not appear to vary by food insecurity transition.
Supplemental Table 1 compares the distribution of characteristics for HRS respondents who smoke among those who participated in 2012 wave to the analysis sample (i.e. those who participated in 2012 and 2014). Proportions across characteristics differed by no more than 1%, and, age and household income-to-poverty ratio were comparable. This indicates that attrition bias was not a concern.
Table 2 shows the odds of smoking cessation by food insecurity transition. In fully adjusted models, those who became food insecure had a 2.0 (95% CI= 1.1, 3.4) times higher odds of smoking cessation than those who did not report food insecurity. However, other food insecurity transitions were not associated with smoking cessation. Additionally, both employment transition and being diagnosed with a new chronic condition were associated with cessation. Those who stopped earning income or became retired had a 1.6 (95% CI=1.1, 2.4) times higher odds of smoking cessation than those who did not experience a change in employment status. Those with a new health diagnosis had a 1.4 (95% CI= 1.0, 2.0) times higher odds of smoking cessation than those without a new health diagnosis. Findings were not moderated by demographic or socioeconomic factors (data not shown). Additionally, results remained unchanged when accounting for 2012 depression status in sensitivity analyses (n=2,167). Meeting criteria for major depression in 2012 was not associated with smoking cessation (odds ratio (OR) = 0.8; 95% CI = 0.5, 1.2).
Table 2.
| Crude | Model 1 | Model 2 | Model 3 | |||||
|---|---|---|---|---|---|---|---|---|
| Demographics | Demographics and Socioeconomic Status |
Demographics, Socioeconomic Status and Life Transitions |
||||||
| OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | |
| FI Transition | 0.033 | 0.024 | 0.032 | 0.048 | ||||
| Not FI | Ref. | Ref. | Ref. | Ref. | ||||
| Initially FI in 2012 | 0.8 (0.5, 1.4) | 0.9 (0.5, 1.5) | 0.9 (0.5, 1.4) | 0.8 (0.5, 1.4) | ||||
| Became FI in 2014 | 2.0 (1.2, 3.4) | 2.1 (1.3, 3.5) | 2.1 (1.2, 3.5) | 2.0 (1.1, 3.4) | ||||
| Remained FI in 2014 | 1.0 (0.6, 1.7) | 1.0 (0.6, 1.8) | 1.0 (0.6, 1.7) | 1.0 (0.6, 1.6) | ||||
| Age, mean (95% CI) | -- | 1.0 (1.0, 1.0) | 0.12 | 1.0 (1.0, 1.0) | 0.14 | 1.0 (1.0, 1.0) | 0.25 | |
| Gender | 0.25 | 0.24 | 0.19 | |||||
| Male | Ref. | Ref. | Ref. | |||||
| Female | -- | 1.2 (0.9, 1.7) | 1.2 (0.9, 1.7) | 1.2 (0.9, 1.7) | ||||
| Race/ethnicity | 0.45 | 0.28 | 0.23 | |||||
| Non-Hispanic White | Ref. | Ref. | Ref. | |||||
| Non-Hispanic Black | -- | 1.0 (0.7, 1.6) | 1.1 (0.7, 1.7) | 1.0 (0.7, 1.7) | ||||
| Other | -- | 1.3 (0.8, 2.1) | 1.4 (0.9, 2.3) | 1.5 (0.9, 2.4) | ||||
| Marital status | 0.18 | 0.9 (0.5, 1.5) | 0.13 | 0.11 | ||||
| Married | Ref. | Ref. | ||||||
| Separated or divorced | -- | 0.7 (0.4, 1.0) | 0.6 (0.4, 1.0) | 0.6 (0.4, 0.9) | ||||
| Widowed | -- | 0.7 (0.4, 1.2) | 0.7 (0.4, 1.2) | 0.7 (0.4, 1.2) | ||||
| Single or never married | -- | 0.9 (0.5, 1.5) | 0.9 (0.5, 1.5) | 0.9 (0.5, 1.5) | ||||
| Educational attainmentc | 0.09 | 0.07 | ||||||
| < High school | Ref. | Ref. | ||||||
| High school degree or above | -- | -- | 1.4 (0.9, 2.1) | 1.5 (1.0, 2.2) | ||||
| Income-to-poverty ratio (IPR) | -- | -- | 1.0 (0.9, 1.0) | 0.20 | 1.0 (0.9, 1.0) | 0.18 | ||
| Work status | 0.62 | 0.76 | ||||||
| Do not work for income | Ref. | Ref. | ||||||
| Work for income | -- | -- | 1.1 (0.8, 1.4) | 1.0 (0.8, 1.4) | ||||
| Retirement status | 0.92 | 0.46 | ||||||
| Not retired | Ref. | Ref. | ||||||
| Partially or fully retired | -- | -- | 1.0 (0.7, 1.5) | 1.2 (0.8, 1.7) | ||||
| Divorced or widowed in 2014 | 0.73 | |||||||
| No | Ref. | |||||||
| Yes | -- | -- | -- | 0.9 (0.5, 1.7) | ||||
| IPR change in 2014 | -- | -- | -- | 1.0 (0.9, 1.0) | 0.44 | |||
| Employment transition in 2014 | 0.020 | |||||||
| No | Ref. | |||||||
| Yes | -- | -- | -- | 1.6 (1.1, 2.4) | ||||
| New health diagnosis in 2014 | 0.026 | |||||||
| No | Ref. | |||||||
| Yes | -- | -- | -- | 1.4 (1.0, 2.0) | ||||
U.S. Health and Retirement Study
n = 2,197
Assessed during HRS enrollment wave
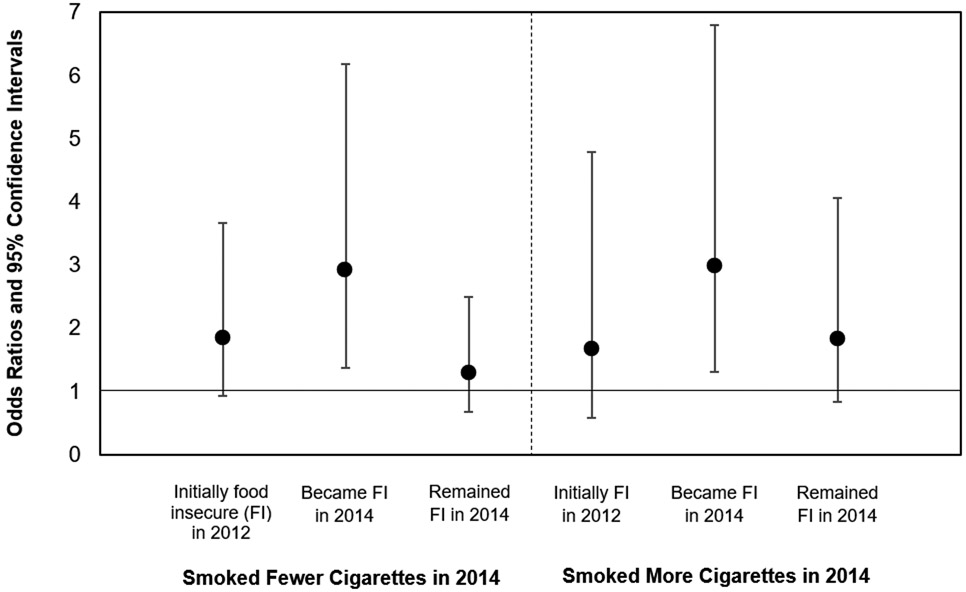
When using multinomial regression to examine changes in smoking consumption, testing main effects indicated that food insecurity transition was not associated with smoking more or fewer cigarettes (Table 3). However, interactions were present for gender (interaction p-value = 0.025) and marital status (interaction p-value < 0.001)—which were subsequently explored using stratified analyses. Among women, becoming food insecure was associated with a 2.9 (1.4, 6.2) times higher odds of smoking fewer cigarettes and a 3.0 (1.3, 6.8) times higher odds of smoking more cigarettes (Figure 1). Food insecurity transition was not associated with change in smoking behavior among men (data not shown). Among those who were widowed; being initially food insecure in 2012 was associated with smoking more cigarettes in 2014 (OR=8.0; 95% CI=1.8, 35.9). Food insecurity transition was not associated with change in smoking consumption for those who were married; separated or divorced or; single or never married (data not shown). Adjusting for 2012 depression status in sensitivity analyses did not change findings for associations between food insecurity transition with change in smoking consumption.
Table 3.
Multinomial logistic regression for the association of food insecurity (FI) transition with smoking more or fewer cigarettesa, HRSb 2012-2014c
| Change in Number of Cigarettes Smoked Per Day |
|||
|---|---|---|---|
| More | Fewer | ||
| OR (95% CI) | OR (95% CI) | P | |
| FI Transition | 0.65 | ||
| Not FI | Ref. | Ref. | |
| Initially FI in 2012 | 0.8 (0.4, 1.5) | 1.0 (0.6, 1.5) | |
| Became FI in 2014 | 1.4 (0.7, 2.8) | 1.6 (0.9, 2.9) | |
| Remained FI in 2014 | 1.5 (0.8, 2.8) | 1.2 (0.7, 2.0) | |
| Age, mean (95% CI) | 1.0 (1.0, 1.0) | 1.0 (1.0, 1.0) | 0.48 |
| Gender | 1.0 (1.0, 1.0) | 1.0 (1.0, 1.0) | 0.67 |
| Male | Ref. | Ref. | |
| Female | 1.0 (0.8, 1.3) | 1.1 (0.9, 1.5) | |
| Race/ethnicity | 0.023 | ||
| Non-Hispanic White | Ref. | Ref. | |
| Non-Hispanic Black | 1.4 (1.0, 2.0) | 1.3 (0.9, 1.9) | |
| Other | 2.1 (1.3, 3.5) | 1.5 (1.0, 2.3) | |
| Marital status | 0.39 | ||
| Married | Ref. | Ref. | |
| Separated or divorced | 0.8 (0.6, 1.1) | 1.0 (0.7, 1.4) | |
| Widowed | 0.8 (0.5, 1.4) | 0.7 (0.5, 1.1) | |
| Single or never married | 0.9 (0.6, 1.4) | 1.1 (0.7, 1.6) | |
| Educational attainmentd | 0.39 | ||
| < High school | Ref. | Ref. | |
| High school degree or above | 1.1 (0.8, 1.5) | 1.3 (0.9, 1.8) | |
| Income-to-poverty ratio (IPR) | 1.0 (1.0, 1.0) | 1.0 (1.0, 1.0) | 0.96 |
| Work status | 0.24 | ||
| Do not work for income | Ref. | Ref. | |
| Work for income | 0.9 (0.5, 1.4) | 0.7 (0.5, 1.1) | |
| Retirement status | 0.76 | ||
| Not retired | Ref. | Ref. | |
| Partially or fully retired | 1.2 (0.7, 1.8) | 1.1 (0.8, 1.5) | |
| Divorced or widowed in 2014 | 0.39 | ||
| No | Ref. | Ref. | |
| Yes | 1.4 (0.6, 2.9) | 1.4 (0.8, 2.3) | |
| IPR change in 2014 | 1.0 (1.0, 1.1) | 1.1 (1.0, 1.1) | 0.11 |
| Employment transition in 2014 | 0.21 | ||
| No | Ref. | Ref. | |
| Yes | 0.9 (0.6, 1.4) | 1.3 (0.9, 1.9) | |
| New health diagnosis in 2014 | 0.015 | ||
| No | Ref. | Ref. | |
| Yes | 1.0 (0.7, 1.4) | 1.5 (1.1, 2.0) | |
Number of cigarettes per day in 2014 vs. 2012; reference=same number/no change
U.S. Health and Retirement Study
n=2,197
Assessed during HRS enrollment wave
Figure 1. Multinomial logistic regression for the association of food insecurity transitions with change in smoking behaviora among women, HRSb 2012-2014c-e.
aNumber of cigarettes per day in 2014 vs. 2012; reference=same number/no change
bU.S. Health and Retirement Study
cn (men and women)=2,197; n (women subsample in stratified analyses)=1,197
dAccounting for age, race/ethnicity, marital status, educational attainment, household income-to-poverty ratio, work status, retirement status, change in household income-to-poverty ratio, employment transition and being diagnosed with a new health condition
eFood insecurity transition and gender interaction p-value = 0.025
DISCUSSION
Findings of this study clarify the association of food insecurity with smoking behavior among older adults. In a representative sample of adults over age 50 in the U.S., becoming food insecure was associated with a greater odds of smoking cessation. Additionally, employment loss or retirement and being diagnosed with a new chronic condition were associated with smoking cessation. Being diagnosed with a new chronic conditions was also associated with smoking fewer cigarettes. Findings suggest that decreased spending power and the onset of health problems is associated with smoking reduction among older Americans. Future studies should examine whether smoking cessation in response to food insecurity makes individuals more susceptible to relapse than if they had decided to quit smoking for other reasons.
While it was initially hypothesized that persistent food insecurity or onset of food insecurity would make smoking cessation less likely—evidence of this study indicated otherwise. Instead, smoking cessation appears to be a coping mechanism by which older adults deal with the onset of food insecurity. This task-oriented response to becoming food insecure is consistent with prior research on coping over the life course.34 Lazarus (1996) posits that once the reality of a situation has been accepted, people tend to respond to life stressors in constructive ways, regardless of age. Given that cigarette smoking increases risk of food insecurity,15 no longer having the need to purchase cigarettes due to smoking cessation frees up financial resources that can be used to obtain food.
While not the main focus of this study, findings also indicate that leaving the work force and being diagnosed with a new chronic condition are associated with smoking cessation and smoking fewer cigarettes among older adults. Prior research has examined similar associations. In HRS waves 1992-2010, Quiñones and colleagues also observed that a new health diagnosis is associated with greater smoking cessation.35 However, analyses within the HRS 1994 wave revealed that involuntary job loss was associated with smoking relapse among those who previously quit smoking and, smoking more cigarettes among current smokers.36 This earlier study by Falba and colleagues (2005) is contradictory with current findings. Additional research is needed to determine whether associations of food insecurity and employment transitions with smoking cessation could be moderated by macro-level factors across time periods, such as the Great Recession or cigarette taxation.
Among European adults ≥50 years who smoked at baseline, becoming widowed or divorced was associated with a lower probability of smoking cessation, whereas; transitions to unemployment and retirement were not associated with smoking cessation.37 Further research is needed to determine why trends among U.S. older adults concerning associations of marriage and employment transitions with smoking cessation appear to be incongruent from those in Europe. The finding that depression was not associated with smoking cessation or change is smoking consumption also contrasts with prior work, which observed that older adults with depressive disorders were less likely to have quit smoking in the 12-months prior.29
Interestingly, when examining moderation of the association between food insecurity transition and change in smoking consumption, interactions were observed for gender and marital status. Future studies should seek to replicate these findings since they were not part of initial hypotheses. Among women, becoming food insecure was associated with a higher odds of smoking fewer cigarettes and a higher odds of smoking more cigarettes—as opposed to smoking the same amount. Future research is needed to examine what additional factors contribute to smoking consumption decisions among women who become food insecure. While the association of becoming food insecure with smoking more cigarettes is consistent with initial hypotheses, it is not clear why this was only observed for women and requires further study. Additionally, more work is needed to determine why transitioning out of food insecurity could be associated with smoking more cigarettes among those who are widowed.
Limitations
HRS provides a nationally representative sample of older adults who smoke in the United States from 2012-2014. The relatively high initial-response and re-interview rates within HRS, and, the use of survey weights in analyses, which account for differential non-response, help mitigate selection bias.40 Additionally, findings indicated that attrition bias was not a concern, given that the distribution of characteristics for HRS respondents in 2012 was similar for those who also participated in 2014.
However, a number of limitations should be considered. Data collection in HRS prevents drawing causal conclusions since both food insecurity and smoking behavior are collected at the same time point every two years. When assessing smoking status, HRS asks study participants about cigarette use specifically. Therefore, this study could not examine tobacco use and smoking cessation from other sources (e.g. chew, pipe, cigar, e-cigarettes). Findings should not be generalized to younger adults. Trends in smoking cessation differ across age groups. For example, quit attempts tend to be more common among those in their early to mid-40’s.29 By the time individuals reach 50 years or above, it may take greater pressure from external factors (e.g. financial strain from food insecurity or onset of a chronic illness) to motivate smoking cessation. Thus, further research is needed to determine whether findings of this study may be similar among younger age groups. While analyses adjust for a number of demographic and socioeconomic factors, health status and life transitions; it is possible that there is residual confounding due to other factors such as area-level socioeconomic status. For example, ‘food deserts’—i.e. areas with poor access to a variety of healthy, affordable foods—have a higher density of ‘convenience stores’,38 where 69% of cigarette sales to current adult smokers occur in the U.S.39
Conclusions
Among older adults in the U.S., smoking cessation and smoking fewer cigarettes were associated with decreased spending power and the onset of new health problems. Unexpectedly, becoming food insecure was associated with a higher odds of smoking cessation. Future studies should examine whether smoking cessation due to food insecurity makes older adults more susceptible to relapse than if they had decided to quit smoking for other reasons. Determining whether associations of food insecurity with smoking behavior vary in response to macro-level factors across time periods (e.g. economic recession, cigarette taxation) could be of particular benefit to policy makers. Additionally, qualitative data could reveal decision making processes for smoking behavior in response to food insecurity transitions—which could help identify underlying pathways when considering moderation by gender and marital status.
Supplementary Material
HIGHLIGHTS.
Becoming food insecure (FI) was associated with smoking cessation in older U.S. adults.
However, in women, becoming FI was also associated with smoking more per day.
Job transition and new health problems were also related with smoking less and cessation.
ACKNOWLEDGEMENTS
The research presented in this paper is that of the author and does not reflect the official policy of the NIH. RSB is supported by the National Institute of Mental Health (NIMH T32-MH73553). The NIMH did not have any role in study design; collection, analysis or interpretation of data; writing the report; or the decision to submit the report for publication. RSB designed this study, analyzed and interpreted the data, and wrote the manuscript. Article contents have not been previously presented elsewhere. No financial disclosures were reported by the author of this paper.
FINANCIAL DISCLOSURE: No financial disclosures were reported by the author of this paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONFLICT OF INTEREST STATEMENT: RSB is supported by the National Institute of Mental Health (NIMH T32-MH73553). The NIMH did not have any role in study design; collection, analysis or interpretation of data; writing the report; or the decision to submit the report for publication.
REFERENCES
- 1.Alberg AJ, Brock MV, Ford JG, Samet JM, Spivack SD. Epidemiology of Lung Cancer: Diagnosis and Management of Lung Cancer, 3rd ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2013; 143(5, Supplemental):e1S–e29S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Campbell SC, Moffatt RJ, Stamford BA. Smoking and smoking cessation—The relationship between cardiovascular disease and lipoprotein metabolism: A review. Atherosclerosis. 2008;201 (2):225–235. [DOI] [PubMed] [Google Scholar]
- 3.Vardavas CI, Panagiotakos DB. The causal relationship between passive smoking and inflammation on the development of cardiovascular disease: a review of the evidence. Inflamm Allergy Drug Targets. 2009;8(5):328–333. [DOI] [PubMed] [Google Scholar]
- 4.Holtgrave DR, Wunderink KA, Vallone DM, Healton CG. Cost-Utility Analysis of the National truth® Campaign to Prevent Youth Smoking. Am J Prev Med 2009;36(5):385–388. [DOI] [PubMed] [Google Scholar]
- 5.King BA, Pechacek TF, Mariolis P. Best practices for comprehensive tobacco control programs, 2014. 2014. [Google Scholar]
- 6.Girard D, Delgado-Eckert E, Schaffner E, et al. Long-term smoking cessation and heart rate dynamics in an aging healthy cohort: Is it possible to fully recover? Environ Res. 2015;143:39–48. [DOI] [PubMed] [Google Scholar]
- 7.Mons U, Müezzinler A, Gellert C, et al. Impact of smoking and smoking cessation on cardiovascular events and mortality among older adults: meta-analysis of individual participant data from prospective cohort studies of the CHANCES consortium. BMJ. 2015;350:h1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Flint AJ, Novotny TE. Poverty status and cigarette smoking prevalence and cessation in the United States, 1983-1993: the independent risk of being poor. Tob Control. 1997;6(1): 14–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gilman S, Abrams D, Buka S. Socioeconomic status over the life course and stages of cigarette use: initiation, regular use, and cessation. J Epidemiol Community Health. 2003;57(10):802–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vidrine JI, Reitzel LR, Wetter DW. Smoking and health disparities. Curr Cardiovasc Risk Rep. 2009;3(6):403. [Google Scholar]
- 11.Vidrine JI, Reitzel LR, Wetter DW. The role of tobacco in cancer health disparities. Curr Oncol Rep. 2009; 11 (6):475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stead M, MacAskill S, MacKintosh A-M, Reece J, Eadie D. “It’s as if you’re locked in”: qualitative explanations for area effects on smoking in disadvantaged communities. Health Place. 2001. ;7(4):333–343. [DOI] [PubMed] [Google Scholar]
- 13.Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household Food Security in the United States in 2017. U.S. Department of Agriculture, Economic Research Service; 2018. [Google Scholar]
- 14.Armour BS, Pitts MM, Lee C. Cigarette smoking and food insecurity among low-income families in the United States, 2001. Am J Health Promot. 2008;22(6):386–390. [DOI] [PubMed] [Google Scholar]
- 15.Farrelly MC, Shafer PR. Comparing Trends Between Food Insecurity and Cigarette Smoking Among Adults in the United States, 1998 to 2011. Am J Health Promot. 2017;31(5):413–416. [DOI] [PubMed] [Google Scholar]
- 16.Hernandez DC, Reesor L, Reitzel LR, Businelle MS, Wetter DW, Kendzor DE. Smoking, financial strain, and food insecurity. Health Behav Policy Rev. 2017;4(2): 182–188. [Google Scholar]
- 17.Peretti-Watel P, Constance J. “It’s All We Got Left”. Why Poor Smokers are Less Sensitive to Cigarette Price Increases. Int J Environ Res Public Health. 2009;6(2):608–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Twyman L, Bonevski B, Paul C, Bryant J. Perceived barriers to smoking cessation in selected vulnerable groups: a systematic review of the qualitative and quantitative literature. BMJ Open. 2014;4(12):e006414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jo Y-H, Talmage DA, Role LW. Nicotinic receptor-mediated effects on appetite and food intake. J Neurobiol. 2002;53(4):618–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Seligman HK, Bolger AF, Guzman D, López A, Bibbins-Domingo K. Exhaustion Of Food Budgets At Month’s End And Hospital Admissions For Hypoglycemia. Health Aff (Millwood). 2014;33(1):116–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Loopstra R, Reeves A, McKee M, Stuckler D. Food insecurity and social protection in Europe: Quasi-natural experiment of Europe’s great recessions 2004–2012. Prev Med. 2016;89:44–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carim-Todd L, Mitchell SH, Oken BS. Impulsivity and Stress Response in Nondependent Smokers (Tobacco Chippers) in Comparison to Heavy Smokers and Nonsmokers. Nicotine Tob Res. 2016; 18(5):547–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hobkirk AL, Krebs NM, Muscat JE. Income as a moderator of psychological stress and nicotine dependence among adult smokers. Addict Behav. 2018;84:215–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sonnega A, Faul JD, Ofstedal MB, Langa KM, Phillips JW, Weir DR. Cohort Profile: the Health and Retirement Study (HRS). Int J Epidemiol. 2014;43(2):576–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Radimer KL, Kathy L. Measurement of household food security in the USA and other industrialised countries. Public Health Nutr. 2002;5(6A):859–864. [DOI] [PubMed] [Google Scholar]
- 26.Bergmans RS, Zivin K, Mezuk B. Depression, food insecurity and diabetic morbidity: Evidence from the Health and Retirement Study. J Psychosom Res. 2019;117:22–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cornwell EY, Waite LJ. Social Disconnectedness, Perceived Isolation, and Health among Older Adults. J Health Soc Behav. 2009;50(1):31–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Keenan PS. Smoking and Weight Change After New Health Diagnoses in Older Adults. Arch Intern Med. 2009;169(3):237–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Agrawal A, Sartor C, Pergadia ML, Huizink AC, Lynskey MT. Correlates of smoking cessation in a nationally representative sample of U.S. adults. Addict Behav. 2008;33(9):1223–1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Huddleston-Casas C, Charnigo R, Simmons LA. Food insecurity and maternal depression in rural, low-income families: a longitudinal investigation. Public Health Nutr. 2009;12(8):1133–1140. [DOI] [PubMed] [Google Scholar]
- 31.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition: DSM-5. Washington, D.C: American Psychiatric Publishing; 2013. [Google Scholar]
- 32.Documentation of Affective Functioning Measures in the Health and Retirement Study. Ann Arbor, MI: University of Michigan Survey Research Center; 2000. [Google Scholar]
- 33.SAS Institute Inc. SAS Software Verrsion 9.4. Cary, NC, USA: SAS Institute Inc.; 2013. [Google Scholar]
- 34.Lazarus RS. Chapter 16 - The Role of Coping in the Emotions and How Coping Changes over the Life Course In: Magai C, McFadden SH, eds. Handbook of Emotion, Adult Development, and Aging. San Diego: Academic Press; 1996:289–306. [Google Scholar]
- 35.Quiñones AR, Nagel CL, Newsom JT, Huguet N, Sheridan P, Thielke SM. Racial and ethnic differences in smoking changes after chronic disease diagnosis among middle-aged and older adults in the United States. BMC Geriatr. 2017; 17(1):48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Falba T, Teng H-M, Sindelar JL, Gallo WT. The effect of involuntary job loss on smoking intensity and relapse. Addiction. 2005; 100(9): 1330–1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Trias-Llimós S, Muszyńska MM, Cámara AD, Janssen F. Smoking cessation among European older adults: the contributions of marital and employment transitions by gender. Eur J Ageing. 2017; 14(2): 189–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Alviola PA, Nayga RM, Thomsen MR, Wang Z. Determinants of Food Deserts. Am J Agric Econ. 2013;95(5): 1259–1265. [Google Scholar]
- 39.Kruger J, Jama A, Lee JGL, et al. Point-of-sale cigarette purchase patterns among U.S. adult smokers—National Adult Tobacco Survey, 2012–2014. Prev Med. 2017;101:38–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sonnega A, Weir D. The Health and Retirement Study: A Public Data Resource for Research on Aging. Open Health Data. 2014;2(1):e7. [Google Scholar]
- 41.Weir DR, Faul JD, Langa KM. Proxy interviews and bias in cognition measures due to non-response in longitudinal studies: a comparison of HRS and ELSA. Longitud Life Course Stud. 2011;2(2): 170–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.