Abstract
Background/Aims
Few data exist on reference thyroid volumes (Tvols) for Spanish children. The standard tables of the World Health Organization (WHO) are only for children older than 6 years. The present cross-sectional study reports the normal Tvols of 3–14 year-old girls and boys living in Madrid (Spain).
Methods
The study subjects were 217 children aged 3–14 years. Urinary iodine was determined, and, on the same day, cervical ultrasound examinations were performed by a single, experienced paediatric radiologist. The sex-specific, upper normal limits for Tvol were then determined, based on age and body surface area (BSA).
Results
The median urinary iodine concentration was 120 µg/L (interquartile range 80–184); the population was therefore deemed to fall within the optimum range for iodine nutritional status. Eight children with heterogeneous glandular parenchyma were detected, as were 6 with increased vascularity, and 22 with intrathyroid cysts. Tvol increased with age and BSA in both sexes from the age of 3 years. In girls aged 11–12 years, Tvol was significantly larger than that in boys of the same age. When comparing children 6 years old and above, the 97th percentile Tvols with respect to gender/BSA were similar to WHO reference values, but by gender/age they were 30% larger.
Conclusions
This work proposes reference ultrasound-determined Tvols for 3–14-year-old children living in Madrid.
Keywords: Urine iodine, Ultrasound, Childhood, Adolescence, Thyroid volume
Introduction
Iodine is an essential trace element required for the formation of the thyroid hormones, which are crucial for somatic and cognitive development. The recommended iodine intake is 90 µg/day from birth to 8 years of age, 120 µg/day in children 9–13 years old, 150 µg/day in adolescents and adults, and 250–300 µg/day during pregnancy and lactation [1]. According to the World Health Organization (WHO), iodine deficiency affects more than 2 billion people worldwide, most of them children and newborns, and remains the leading nutritionally preventable cause of mental retardation [2]. Although iodine deficiency is prevalent in developing countries, mild or moderate iodine deficiency is not uncommon in industrialized countries. In total, about 20% of the world's population is at risk [3]. To determine the nutritional status of iodine in a population, the WHO and the Iodine Global Network indicate the urinary iodine concentration (UIC, expressed in μg/L) to provide the most practical biochemical estimate of recent iodine intake. The median UIC is used to express the global nutritional level of iodine in a population, although it does not take intra-individual variation into consideration [4, 5]. According to international standards, the normal median UIC value range is 100–199 μg/L, corresponding to a daily oral iodine intake of 150–299 μg [5, 6].
The size of the thyroid gland in school-age children reflects the severity of iodine deficiency in the general population [3]. Historically, 2 methods of thyroid examination have been used: palpation and cervical ultrasound [7]. When available, the latter method is considered better for determining the size of the thyroid gland [8, 9], particularly in areas where goitre rates are low [10]. Although international reference values were proposed by the WHO in 2004 [11], they do not reflect local variation. Local references should therefore be obtained.
In the present work, thyroid volume (Tvol) was determined in children from Madrid (Spain) to establish local values for the first time. The population analyzed had an optimum iodine status [12]. The results obtained were compared with those reported from other parts of the world (Table 1).
Table 1.
Upper limits of normal thyroid volume (cm3; p97): a comparison of studies reporting results by age group
| Countrya | Age, years; groups, boys/girls |
Reference | |||||
|---|---|---|---|---|---|---|---|
| 3–4 | 5–6 | 7–8 | 9–10 | 11–12 | 13–14 | ||
| AT BE CZ DE FR HU IT LU NL PL RO SK | 5.4/5.0 | 6.1/6.9 | 7.8/9.2 | 10.4/11.7 | 13.9/14.6 | [36] | |
| MY | 4.5/4.7 | 5.7/6.6 | [26] | ||||
| NL | 5.00/5.20 | 6.50/6.50 | 8.00/9.30 | 10.00/12.00 | 16.00/16.50 | [25] | |
| BR | 3.20/3.20 | 4.50/4.50 | 6.50/6.20 | 7.00/8.10 | 8.00/10.7 | [9] | |
| BH CH JP PE US ZA | 2.91/2.94 | 3.71/3.76 | 4.73/4.96 | 6.03/6.59 | [11] | ||
| ES | 3.30/3.20 | 3.43/4.36 | 4.51/5.81 | [18] | |||
| SE | 4.00/3.80 | 5.10/5.00 | 8.50/7.50 | 7.50/7.50 | [28] | ||
| NG | 2.19/2.37 | 2.46/2.56 | 2.64/2.85 | 3.74/3.89 | 4.66/4.69 | [29] | |
| JP | 2.00/2.10 | 2.5/2.8 | 3.1/3.2 | 4.00/4.40 | 5.90/6.00 | 7.00/6.80 | [24] |
| CN | 5.00/4.80 | 6.00/6.00 | [27] | ||||
| ES | 2.90/3.64 | 3.86/4.10 | 4.40/5.0 | 7.47/6.30 | 7.70/7.89 | 12.50/9.66 | This study |
Abbreviations: AT, Austria; BE, Belgium; BH, Bahrain; BR, Brazil; CH, Switzerland; CN, China; CZ, Czech Republic; DE Germany; ES, Spain; FR, France; HU, Hungary; IT, Italy; JP, Japan; LU, Luxemburg; MY, Malaysia; NG, Nigeria; NL, Netherlands; PE, Peru; PL, Poland; RO, Romania; SK, Slovakia; SE, Sweden; US, United States; ZA, South Africa (Source: https://www.worldatlas.com/aatlas/ ctycodes.htm; accessed April 10, 2018).
Materials and Methods
Subjects
An observational, cross-sectional study was conducted at the Department of Paediatrics at the Puerta de Hierro-Majadahonda Hospital between April 2011 and October 2012. A total of 217 children aged 3–14 years were enrolled. All of them had been referred from primary health care centers in the surrounding area (one of high socioeconomic status) to our outpatient paediatric clinic for reasons other than thyroid problems. Children with a known thyroid disorder or who had received iodine contrast for a radiological examination were excluded.
Variables Assessed
Fasting (overnight) urine samples (10 mL) were taken once from all the children, frozen at −80°C for transport in a portable refrigerator to the Laboratory of Biochemistry at the Hospital La Paz (Madrid, Spain), and the UIC determined using the modified Benotti-Benotti method [13]. Following WHO guidelines, the UIC values were expressed as medians – not means – due to the variability in values between subjects. Height and weight were measured using standard anthropometric techniques, normalized for sex and age, and expressed as mean ± SDs according to standardized published tables [14, 15]. Body surface area (BSA, in m2) was calculated from weight and height measurements using the formula [16]:
BSA = weight (kg)0.425 × height (cm)0.725 × 71.84 × 10–4.
On the same day as blood extraction, the children underwent cervical ultrasonography performed by a single, experienced paediatric radiologist. Tvol was measured using an Acuson Antares Premium apparatus (Siemens, Munich) equipped with a high frequency (13 MHz) linear electronic transducer. Measurements were made with subjects sitting upright and with the neck slightly extended. Tvol was determined as the sum of the volume of both lobes, not including the isthmus, using the formula [11, 17]:
Tvol = width (cm) × length (cm) × thickness (cm) × 0.479.
The echographic variables assessed were total volume of the gland (expressed in cm3), homogeneity of the parenchyma, vascularization of the gland, presence of colloid cysts, and the presence of space-occupying lesions and adjacent tissue abnormalities (lymph nodes, masses and collections). Cervical palpation was not performed, since ultrasound is preferred if an expert radiologist is available [3].
Statistical Analyses
The sample size required for this study was calculated by accepting an alpha risk of 0.05 for an accuracy of ± 6.5%. Data were presented as means ± SD, or medians and interquartile ranges (IQR). The Kolmogorov-Smirnov test was used to determine whether the variables showed a normal distribution. Comparisons of the results for continuous variables between sex/age groups were made using the Student t test. To determine the Tvol percentiles, a statistical correction was made, removing out-of-range values (those that exceeded 3 times the range between p75 and p25) for each group, with the idea of setting a p97 normality limit. All calculations were made using SPSS software version 14. Significance was set at p < 0.05.
Ethical Statement
This study was approved by the Ethics Research Committee of the Puerta de Hierro-Majadahonda Hospital (Madrid, Spain) in March 2011. Parents provided informed consent for their children to be included after receiving a full explanation of the purpose and nature of all procedures. If the child was over 11 years old, he/she signed the informed consent forms as well. The procedures followed were in accordance with the Helsinki Declaration of 1975, as revised in 2008.
Results
Description of the Population
The children enrolled were 107 girls and 110 boys. These fell into 3 age groups: (a) preschoolers (3–6 years; 38.7% of the total sample); (b) primary school age children (7–10 years; 33.6%), and (c) adolescents (11–14 years; 27.6%). The weight, height, and body mass index of all the participants fell into the normal ranges for Spanish children [14, 15].
Iodine Urinary Concentration and Description of the Ultrasound Thyroid Findings
The overall median UIC was 120.00 μg/L (interquartile range 80–184), that is, within the normal range for children of any age according to the WHO. Seven children had UIC values of > 500 μg/L, probably indicating iodine poisoning (perhaps caused by the use of iodine antiseptics which is common in Spain); 37.8% of the children had values of < 100 μg/L (representing iodine deficiency) and one third of those had values of < 50 μg/L.
Eight children had heterogeneous echogenicity of the thyroid parenchyma (suggesting tiny cystic spaces), 6 showed increased vascularity compatible with thyroiditis as per radiologist and 22 had intrathyroid isolated cysts. One single big cyst was biopsied showing a thyroid adenoma. There were no differences seen in median UIC between these patients and the children with no such problems.
Relationship between Thyroid Gland Volume and Gender/Age and Gender/BSA
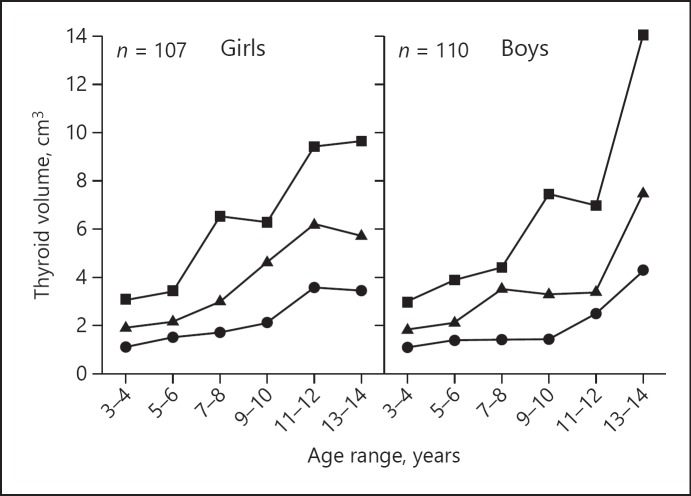
The 11–12 year-old girls had higher Tvol values than did boys of the same age (p = 0.037; Fig. 1). Figure 2 shows the 3rd, 50th and 97th percentiles for gender/BSA.
Fig. 1.
Tvol percentiles in girls and boys by age group in a population with optimum iodine level. Circles, triangles and squares correspond to p3, p50, and p97 values respectively.
Fig. 2.
Thyroid volume (Tvol) percentiles in girls and boys in relation to body surface area (BSA). Circles, triangles and squares correspond to p3, p50 and p97 values respectively.
Thyroid Gland Volumes; Comparison with International Reference Values
Table 1 shows the present age-specific percentile 97 for Tvol compared to the results of other studies undertaken in areas with optimum iodine reference values, including the only other study determined in Spain to date [18]. Compared to WHO standards [11], the present Tvol for children 6 years old and above was 32% higher when adjusted for age and 5% higher when adjusted for BSA.
Discussion
The present results show the iodine status of children in the northwest of the Madrid area to be within the range of normality. The median UIC value (120 μg/L) was similar to those previously reported for other Spanish provinces [18, 19, 20, 21, 22]. Formal international recommendations advise that standard references for thyroid volumes should be determined regionally or nationally. The WHO data for normal thyroid volumes refer only to children over 6 years of age, while 30% of our present population were younger. To the best of our knowledge, only 2 studies have reported Tvol for children between 3 and 6 years of age: one from Brussels [23] – in an area with a median UIC of 68 μg/L – and one from Japan [24] with Tvols smaller than the present study. Only one Spanish study has proposed normal ranges for Tvol, and this refers to children aged 6 years and above [18]. In the present work, Tvol determinations were made by a single paediatric radiologist with more than 28 years of clinical experience. The results are therefore free of interobserver variation, a factor known to have contributed to current disagreements surrounding normal Tvol values for children [9].
We found radiological abnormalities as heterogeneous glands and cysts in some patients, these patients have been followed by a paediatric endocrinologist, not showing further complications.
Table 1 provides a summary of the age-adjusted p97 Tvol from different countries and the results for the present study. Although no statistical analysis was performed, it can be seen that the present results are similar to those reported from the Netherlands, Malaysia, China, Sweden and Brazil [9, 25, 26, 27, 28]. However, the Tvol values are higher than those reported by the WHO [11], and from Japan and Nigeria [24, 29], probably due to genetic or environmental factors.
In the present work, significant sex differences in Tvol were found for the 11–12 year-old group (with girls showing higher values). These data agree with the results of previous reports from other countries, which suggest that between 8 and 12 years of age, girls have a higher Tvol than boys [11, 24, 25, 26, 27, 28, 29, 30, 31]. This might be related to the earlier onset of puberty in girls, or to possible differences in iodine status due to differences in consumption of iodine-rich food. However, no such gender differences were found in other studies [18, 32, 33, 34, 35]. The present Tvol values are higher than those reported in the one other study performed in Spain [18]. Madrid lies at the center of the country, whereas this other study was performed in a coastal area where the consumption of iodine-rich foods such as fish and seafood are historically higher; this might explain the difference. The present Tvol values are, however, smaller than those reported by Delange in several European countries in 1997 [2]. This may signal that good progress has been made Spain over the last 2 decades with respect to achieving adequate iodine status.
Linear correlations between BSA and Tvol have been detected in different countries [9, 24, 31, 32, 33, 34]. BSA/gender Tvol tables are important in countries with a high poverty rate, where there can be mismatches between age and the expected BSA [10, 31, 35]. However, in countries like Spain, in which people's nutritional status is usually appropriate, it is more convenient to use tables based on age/sex, especially since the radiologist taking the required ultrasound images will commonly not know the BSA of the patient [23, 36]. In the Netherlands, Wiersinga et al. [25] observed that, until the age of 14, differences in Tvol with respect to sex were greater than those with respect to BSA.
The present Tvol values are similar to those recorded in other regions and countries. However, the small sample size forced the present use of 2-year ranges instead of single years, perhaps reducing the reliability of the results. Further, since goitres may take years to return to normal after restoring the patient's iodine status, the WHO recommends carrying out Tvol studies in populations that have long (though without specifying how long) been in a situation of iodine sufficiency. Spain was iodine-deficient until 2003, so the 9 years that elapsed until the time of the present research may not have been enough to normalize the Tvols in the general population. Another limitation of this study is that it was performed at single hospital with a specific population from a medium-high socioeconomic background; the results may not, therefore, be representative of the entire Madrid province. Multicentre studies should be undertaken to address this issue.
In conclusion, the iodine status of children in this part of Madrid lies in the optimal range. The Tvols recorded are comparable to those noted for other countries; however, they are around 30% higher than WHO values for children aged 6 years and above. Larger, multicenter studies are needed to gather more data. To our knowledge, this is only the third published report to provide Tvol data for children aged 3–6 years.
Statement of Ethics
This study was approved by the Ethics Research Committee of the Puerta de Hierro-Majadahonda Hospital (Madrid, Spain) in March 2011. Parents provided informed consent for their children to be included after receiving a full explanation of the purpose and nature of all procedures. If the child was over 11 years old, he/she signed the informed consent forms as well. The procedures followed were in accordance with the Helsinki Declaration of 1975, as revised in 2008.
Disclosure Statement
The authors declare that they have no conflicts of interest to disclose.
Funding Sources
This research received no grant funding.
Author Contributions
All authors contributed to the study design, recruited the subjects, and discussed the results. M.T.G.-A., S.A.S., and P.R.P. conceived the study. M.T.G.-A. and R.P.P. analyzed the results. M.M.M. performed all the ultrasound examinations. M.T.G.-A. wrote the first draft of the manuscript. All authors revised and approved the final version.
Acknowledgements
We are grateful to all the children and families who participated in this study. We thank Dr. Soledad Santacruz, Department of Biochemistry, Hospital Universitario La Paz Madrid, for analysing the urine samples.
References
- 1.World Health Organization United Nations Children's Fund, International Council for Control of IDD Council for Control of Iodine Deficiency Disorders [Internet] Geneva: Assessment of iodine deficiency disorders and monitoring their elimination. A guide for programme managers. (3rd edn) 2007 [cited 2018 March 13]. Available from: http://apps.who.int/iris/bitstream/10665/43781/1/9789241595827_eng.pdf. [Google Scholar]
- 2.Delange F. Iodine deficiency as a cause of brain damage. Postgrad Med J. 2001 Apr;77((906)):217–20. doi: 10.1136/pmj.77.906.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization United Nations Children's Fund [Internet] Geneva: Iodine deficiency in Europe: a continuing public health problem. 2007 [cited 2018 April 10]. Available from: http://apps.who.int/iris/bitstream/10665/43398/1/9789241593960_eng.pdf. [Google Scholar]
- 4.Ristic-Medic D, Piskackova Z, Hooper L, Ruprich J, Casgrain A, Ashton K, et al. Methods of assessment of iodine status in humans: a systematic review. Am J Clin Nutr. 2009 Jun;89((6)):2052S–69S. doi: 10.3945/ajcn.2009.27230H. [DOI] [PubMed] [Google Scholar]
- 5.König F, Andersson M, Hotz K, Aeberli I, Zimmermann MB. Ten repeat collections for urinary iodine from spot samples or 24-hour samples are needed to reliably estimate individual iodine status in women. J Nutr. 2011 Nov;141((11)):2049–54. doi: 10.3945/jn.111.144071. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization [Internet]. Geneva: Urinary iodine concentrations for determining iodine status in populations. 2013 [cited 2018 March 18]. Available from: http://apps.who.int/iris/bitstream/10665/85972/1/WHO_NMH_NHD_EPG_13.1_eng.pdf
- 7.Zimmermann M, Saad A, Hess S, Torresani T, Chaouki N. Thyroid ultrasound compared with World Health Organization 1960 and 1994 palpation criteria for determination of goiter prevalence in regions of mild and severe iodine deficiency. Eur J Endocrinol. 2000 Dec;143((6)):727–31. doi: 10.1530/eje.0.1430727. [DOI] [PubMed] [Google Scholar]
- 8.Peterson S, Sanga A, Eklöf H, Bunga B, Taube A, Gebre-Medhin M, et al. Classification of thyroid size by palpation and ultrasonography in field surveys. Lancet. 2000 Jan;355((9198)):106–10. doi: 10.1016/S0140-6736(99)07221-9. [DOI] [PubMed] [Google Scholar]
- 9.Rossi A, Tomimori E, Camargo R, Medeiros-Neto G. Determination of thyroid volume by Sonography in healthy Brazilian schoolchildren. J Clin Ultrasound. 2002 May;30((4)):226–31. doi: 10.1002/jcu.10060. [DOI] [PubMed] [Google Scholar]
- 10.Kim BK, Choi YS, Oak CH, Park YH, Kim JH, Park DJ, et al. Determination of thyroid volume by ultrasonography among schoolchildren in Philippines. Int J Endocrinol. 2012;2012:387971. doi: 10.1155/2012/387971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zimmermann MB, Hess SY, Molinari L, De Benoist B, Delange F, Braverman LE, et al. New reference values for thyroid volume by ultrasound in iodine-sufficient schoolchildren: a World Health Organization/Nutrition for Health and Development Iodine Deficiency Study Group Report. Am J Clin Nutr. 2004 Feb;79((2)):231–7. doi: 10.1093/ajcn/79.2.231. [DOI] [PubMed] [Google Scholar]
- 12.García Ascaso MT. Situación nutricional de yodo en niños de entre 3 y 14 años: variables individuales, familiares, dietéticas, analíticas y ecográficas. PhD thesis. Madrid: Facultad de Medicina, Universidad Autónoma de Madrid. 2013 https://repositorio.uam.es/bitstream/handle/10486/662030/garcia_%20ascaso_marta_taida.pdf?sequence=1. [Google Scholar]
- 13.Benotti J, Benotti N, Pino S, Gardyna H. Determination of total iodine in urine, stool, diets, and tissue. Clin Chem. 1965 Oct;11((10)):932–6. [PubMed] [Google Scholar]
- 14.Hernández M, Castellet J, Narvaíza JL, Rincón JM, Ruios I, Sánchez E, et al. Curvas y tablas de crecimiento. Madrid: Ed. Garsi; 1988. [Google Scholar]
- 15.Carrascosa Lezcano A, Fernández García JM, Fernández Ramos C, Ferrández Longás A, López-Siguero JP, Sánchez González E, et al. Grupo Colaborador Español Estudio transversal español de crecimiento 2008. Parte II: valores de talla, peso e índice de masa corporal desde el nacimiento a la talla adulta. An Pediatr (Barc) 2008 Jun;68((6)):552–69. doi: 10.1157/13123287. [DOI] [PubMed] [Google Scholar]
- 16.Du Bois D, Du Bois EF. A formula to estimate the approximate surface area if height and weight be known. Arch Intern Med (Chic) 1916;17:863–71. [PubMed] [Google Scholar]
- 17.Brunn J, Block U, Ruf G, Kunze WP, Scriba PC. Volumetrie der schilddrüsenlappen mittels real-time-sonographie. Dtsch Med Wochenschr. 1981;106((41)):1338–40. doi: 10.1055/s-2008-1070506. [DOI] [PubMed] [Google Scholar]
- 18.Zubiaur Cantalapiedra A, Zapico Álvarez-Cascos MD, Ruiz Pérez L, Sanguino López L, Sánchez Serrano FJ, Alfayate Guerra R, et al. Situación nutricional de yodo en la población escolar de Alicante. An Pediatr (Barc) 2007 Mar;66((3)):260–6. doi: 10.1157/13099688. [DOI] [PubMed] [Google Scholar]
- 19.Serra-Prat M, Díaz E, Verde Y, Gost J, Serra E, Puig Domingo M. Prevalencia del déficit de yodo y factores asociados en escolares de 4 años. Med Clin (Barc) 2003 Mar;120((7)):246–9. doi: 10.1016/s0025-7753(03)73667-7. [DOI] [PubMed] [Google Scholar]
- 20.Delgado E, Díaz-Cadórniga FJ, Tartón T, Bobis ML, Valdés MM, Méndez A. Erradicación de los trastornos por deficiencia de yodo en Asturias (España): 18 años de yodoprofilaxis con sal. Endocrinol Nutr. 2004;51((9)):492–6. [Google Scholar]
- 21.Olmedo Carrillo P, García Fuentes E, Gutiérrez Alcántara C, Serrano Quero M, Moreno Martínez M, Ureña Fernández T, et al. T. UF, Santiago Fernández P: evaluación del estado de nutrición yódica en población general en la provincia de Jaén. Endocrinol Nutr. 2015;62((8)):373–9. doi: 10.1016/j.endonu.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 22.Vila L, Donnay S, Arena J, Arrizabalaga JJ, Pineda J, Garcia-Fuentes E, et al. Iodine status and thyroid function among Spanish schoolchildren aged 6-7 years: the Tirokid study. Br J Nutr. 2016 May;115((9)):1623–31. doi: 10.1017/S0007114516000660. [DOI] [PubMed] [Google Scholar]
- 23.Chanoine JP, Toppet V, Lagasse R, Spehl M, Delange F. Determination of thyroid volume by ultrasound from the neonatal period to late adolescence. Eur J Pediatr. 1991 Apr;150((6)):395–9. doi: 10.1007/BF02093716. [DOI] [PubMed] [Google Scholar]
- 24.Suzuki S, Midorikawa S, Fukushima T, Shimura H, Ohira T, Ohtsuru A, et al. Thyroid Examination Unit of the Radiation Medical Science Center for the Fukushima Health Management Survey Systematic determination of thyroid volume by ultrasound examination from infancy to adolescence in Japan: the Fukushima Health Management Survey. Endocr J. 2015;62((3)):261–8. doi: 10.1507/endocrj.EJ14-0478. [DOI] [PubMed] [Google Scholar]
- 25.Wiersinga WM, Podoba J, Srbecky M, van Vessem M, van Beeren HC, Platvoet-Ter Schiphorst MC. A survey of iodine intake and thyroid volume in Dutch schoolchildren: reference values in an iodine-sufficient area and the effect of puberty. Eur J Endocrinol. 2001 Jun;144((6)):595–603. doi: 10.1530/eje.0.1440595. [DOI] [PubMed] [Google Scholar]
- 26.Foo LC, Zulfiqar A, Nafikudin M, Fadzil MT, Asmah AS. Local versus WHO/International Council for Control of Iodine Deficiency Disorders-recommended thyroid volume reference in the assessment of iodine deficiency disorders. Eur J Endocrinol. 1999 Jun;140((6)):491–7. doi: 10.1530/eje.0.1400491. [DOI] [PubMed] [Google Scholar]
- 27.Mo Z, Lou X, Mao G, Wang Z, Zhu W, Chen Z, et al. Larger thyroid volume and adequate iodine nutrition in Chinese schoolchildren: local normative reference values compared with WHO/IGN. Int J Endocrinol. 2016;2016:8079704. doi: 10.1155/2016/8079704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Filipsson Nyström H, Andersson M, Berg G, Eggertsen R, Gramatkowski E, Hansson M, et al. Thyroid volume in Swedish school children: a national, stratified, population-based survey. Eur J Clin Nutr. 2010 Nov;64((11)):1289–95. doi: 10.1038/ejcn.2010.162. [DOI] [PubMed] [Google Scholar]
- 29.Marchie TT, Oyobere O, Eze KC. Comparative ultrasound measurement of normal thyroid gland dimensions in school aged children in our local environment. Niger J Clin Pract. 2012 Jul-Sep;15((3)):285–92. doi: 10.4103/1119-3077.100622. [DOI] [PubMed] [Google Scholar]
- 30.de Benoist B, Andersson M, Takkouche B, Egli I. Prevalence of iodine deficiency worldwide. Lancet. 2003 Nov;362((9398)):1859–60. doi: 10.1016/S0140-6736(03)14920-3. [DOI] [PubMed] [Google Scholar]
- 31.Brahmbhatt S, Brahmbhatt RM, Boyages SC. Thyroid ultrasound is the best prevalence indicator for assessment of iodine deficiency disorders: a study in rural/tribal schoolchildren from Gujarat (Western India) Eur J Endocrinol. 2000 Jul;143((1)):37–46. doi: 10.1530/eje.0.1430037. [DOI] [PubMed] [Google Scholar]
- 32.Zou Y, Ding G, Lou X, Zhu W, Mao G, Zhou J, et al. Factors influencing thyroid volume in Chinese children. Eur J Clin Nutr. 2013 Nov;67((11)):1138–41. doi: 10.1038/ejcn.2013.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.González M, González CP, Sanabria A. Determinación ecográfica del volumen normal de la glándula tiroides en una población pediátrica de Bogotá, Colombia. Biomedica. 2006 Mar;26((1)):95–100. [PubMed] [Google Scholar]
- 34.Kaloumenou I, Alevizaki M, Ladopoulos C, Antoniou A, Duntas LH, Mastorakos G, et al. Thyroid volume and echostructure in schoolchildren living in an iodine-replete area: relation to age, pubertal stage, and body mass index. Thyroid. 2007 Sep;17((9)):875–81. doi: 10.1089/thy.2006.0327. [DOI] [PubMed] [Google Scholar]
- 35.Xu F, Sullivan K, Houston R, Zhao J, May W, Maberly G. Thyroid volumes in US and Bangladeshi schoolchildren: comparison with European schoolchildren. Eur J Endocrinol. 1999 Jun;140((6)):498–504. doi: 10.1530/eje.0.1400498. [DOI] [PubMed] [Google Scholar]
- 36.Delange F, Benker G, Caron P, Eber O, Ott W, Peter F, et al. Thyroid volume and urinary iodine in European schoolchildren: standardization of values for assessment of iodine deficiency. Eur J Endocrinol. 1997 Feb;136((2)):180–7. doi: 10.1530/eje.0.1360180. [DOI] [PubMed] [Google Scholar]