Abstract
Gastrointestinal Kaposi sarcoma (GI-KS) is the most common extra-cutaneous site of KS in HIV/AIDS, and the majority (75%) of affected patients are asymptomatic. GI-KS rarely occurs in the absence of cutaneous lesions. Opportunistic GI infections in HIV/AIDS and GI-KS can present with similar symptoms especially diarrhea, creating a diagnostic challenge. We present a 46-year-old homosexual male with a medical history of HIV/AIDS and neurosyphilis, who presented with 2 weeks of nonbloody diarrhea and abdominal discomfort. He was initially worked up for infectious diarrhea, initiated on highly active anti-retroviral (HAART) and supportively managed with rehydration therapy and analgesia. However, his clinical symptoms did not improve, necessitating abdomen/pelvic CT scan which revealed extensive recto-sigmoid colon thickening and pelvic lymphadenopathy. Due to a high suspicion of malignancy, diagnostic endoscopy and biopsy were done which showed colonic KS. He was treated with intravenous pegylated doxorubicin in addition to HAART which evidently resulted in significant clinical and radiological improvement. The diagnosis of GI-KS could be challenging in the presence of overlapping features with opportunistic GI infections and the absence of cutaneous manifestations of KS because clinicians tend to focus more on infectious etiology. We suggest that clinicians should consider GI-KS in the differential diagnosis of patients with HIV/AIDS that present with diarrhea and other nonspecific abdominal symptoms. Early endoscopic evaluation with biopsy could help to ensure the timely diagnosis and management of GI-KS and ultimately improve outcomes.
Keywords: Early detection, Endoscopic diagnosis, HIV/AIDS, Kaposi sarcoma
Introduction
Kaposi sarcoma (KS) is an angioproliferative malignancy that occurs in about 20% of patients with HIV/AIDS [1]. KS usually affects mucocutaneous sites particularly the skin and sometimes the oropharynx; however, visceral and other extra-cutaneous involvement has been described [2].
Gastrointestinal KS (GI-KS) is the most common extra-cutaneous site of KS in HIV/AIDS, and the majority (75%) of affected patients are asymptomatic [3]. GI-KS rarely occurs in the absence of cutaneous lesions [4]. Symptomatic patients usually present with nonspecific findings such as vague abdominal discomfort, abdominal cramps, nausea, vomiting, diarrhea and sometimes upper and lower GI bleed [5, 6, 7]. GI opportunistic infections in HIV/AIDS frequently present with similar symptoms to GI-KS which can make diagnosis challenging [8].
Case Presentation
A 46-year-old homosexual male with a medical history of HIV/AIDS and neurosyphilis, presented with 2 weeks of non-bloody, mucoid diarrhea and abdominal discomfort. He had no history of recent hospital admission, international travel, and change in diet or sick contacts. He was not on any medications at the time, including highly active anti-retroviral (HAART) medications. He denied fever, chills, loss of appetite, nausea, or vomiting. His physical examination was remarkable for a slightly distended abdomen and hyperactive bowel sounds. No rashes or ulcers were noted on his oral mucosa and skin. Initial laboratory investigations showed an absolute CD4 cell count of 229 cells/μL, HIV-RNA level of 192 copies/mL, and mild anemia (hemoglobin of 12.2 g/dL). Stool microbiology tests were ordered, and he was commenced on HAART and supportive rehydration treatment and analgesics. However, 4 days after initiation of HAART and supportive treatment, his symptoms did not improve and while awaiting results of stool microbiology, an abdomen/pelvic CT scan with intravenous (IV) contrast was obtained which revealed extensive rectosigmoid colon thickening and pelvic lymphadenopathy (Fig. 1a), suggestive of an infiltrative or inflammatory process.
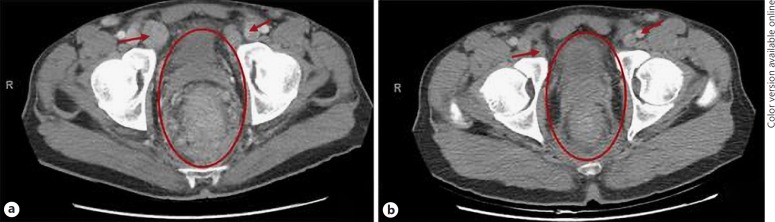
Fig. 1.
Abdomen and pelvic CT scans showing extensive rectosigmoid colon thickening (red circle) and pelvic lymphadenopathy (red arrows) (a) and decrease in the severity of colonic thickening and pelvic lymphadenopathy (while on chemotherapy) (b).
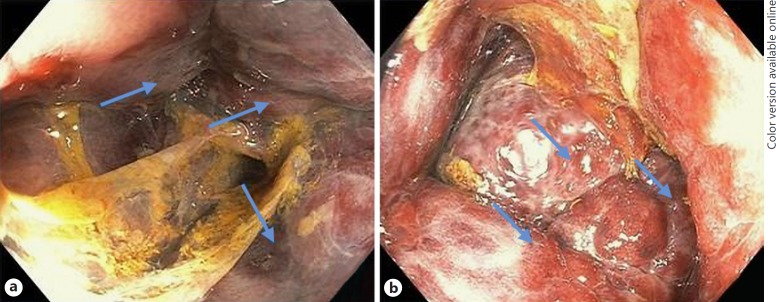
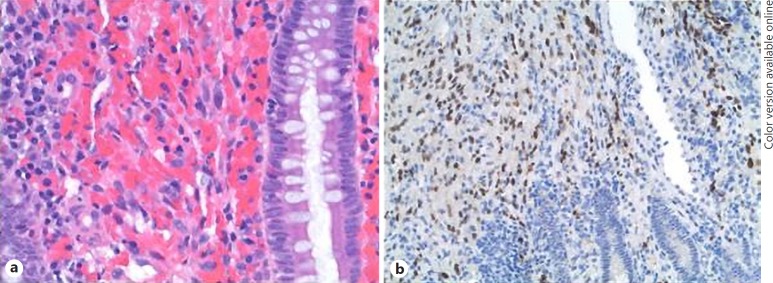
Due to a high suspicion for a malignant process, a colonoscopy was done which showed extensive circumferential edema, violaceous papular lesions and “pseudotumoral” lesions (Fig. 2a, b) in the rectosigmoid colon. Endoscopic biopsy specimens were obtained from the rectosigmoid lesions, and hematoxylin and eosin examination demonstrated vascular proliferation and extravasated blood cells in the lamina propria characterized by slit-like to dilated vessels lined by banal endothelial cells (Fig. 3a). These cells were strongly reactive for HHV-8 by immunohistochemistry, supporting the diagnosis of colonic KS (Fig. 3b). His stool culture tests resulted negative, and he was started on HAART and IV liposomal doxorubicin chemotherapy. The diarrhea and abdominal symptoms resolved and by the fourth cycle of chemotherapy, a repeat pelvic CT scan with IV contrast revealed significant improvement in the rectosigmoid colonic thickening, edema, and pelvic lymphadenopathy (Fig. 1b). Considering the remarkable improvement in his clinical condition, the risks of a repeat endoscopy outweigh its benefits, and we decided to monitor his progress clinically rather than through invasive procedures.
Fig. 2.
Endoscopic image of the rectosigmoid colon showing purplish papular lesions (a) and “pseudotumoral” lesions (blue arrows) strongly suggestive of an infiltrative KS lesion (b).
Fig. 3.
a Hematoxylin and eosin stain of rectosigmoid lesions demonstrating slit-like to dilated vessels with spindle cell vascular proliferation and extravasated red blood cells in the lamina propria. b Immunochemical stain for human herpesvirus 8 showing a positive latent nuclear antigen staining of the spindle cells.
Discussion
KS is a low-grade vascular tumor associated with human herpesvirus 8 infection (HHV-8) [2]. KS usually occurs in immunodeficient states and has 4 clinical and epidemiological variants: classic, iatrogenic or related to immunosuppressive treatment, African or endemic, and epidemic or AIDS-related KS [9]. Endemic and epidemic KS are the two most common clinical forms in the United States and have been linked to GI-KS.
GI-KS affecting the colon usually presents with abdominal cramps and diarrhea as seen in our patient. The etiology of diarrhea in HIV or AIDS is mostly infectious and common pathogens include cytomegalovirus, protozoans, microsporidium, cryptosporidium, and giardia lamblia; and bacterial agents such as salmonella, campylobacter, and mycobacterium avium-intracellulare [8]. GI-KS presenting with diarrhea in a patient with HIV/AIDS without cutaneous manifestations could create a diagnostic dilemma because clinicians tend to focus more on the infectious differential etiologies.
Though the incidence of KS has declined since the advent of HAART, it is still associated with significant morbidity and poor prognosis in AIDS patients [10]. Early diagnosis and treatment of GI-KS is important for survival, and diagnosis is made mainly through endoscopy and biopsy [11]. According to the guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents presenting with diarrhea, endoscopic evaluation is only indicated when medical tests for infectious causes (stool culture, microscopy, Clostridium difficiletoxin assay, and blood culture) fail to reveal an etiology or treatment for an established diagnosis fails [8]. Sometimes, the results of these tests take considerable time to become available which could delay the diagnosis of visceral KS, and negatively impact management and outcomes. However, there is a high probability that colonic KS and an infectious cause of diarrhea may co-occur in HIV/AIDS [12], and clinicians may be inclined to stop any further medical investigations when the infectious etiology is detected.
A retrospective study by Nagata et al. [5], highlighted clinical factors that predict an endoscopic diagnosis of GI-KS in the absence of cutaneous lesions. Men who have sex with men (MSM), low CD4 count (<100 cells/mL), high HIV RNA viral load, and no HAART treatment were strong predictors of GI-KS. Interestingly, our patient had a serum CD4 count of 224 cells/µL at diagnosis, suggesting that GI-KS can also occur with a relatively higher level of CD4 count. Clinicians should maintain a low threshold to perform screening and diagnostic endoscopy to detect GI-KS in high risk asymptomatic and symptomatic HIV/AIDS patients, respectively.
HAART is recommended for patients with AIDS-related KS. GI involvement is an indication for additional systemic chemotherapy and the first-line treatment is with IV liposomal doxorubicin [13]. Early diagnosis and initiation of HAART and systemic chemotherapy have been shown to improve the overall 5-year survival rate to about 90% [14]. Our patient was treated with IV pegylated doxorubicin and HAART which evidently resulted in improvement in his KS-related clinical symptoms and abdominal imaging features (Fig. 1b).
Conclusion
Delay in the diagnosis and treatment of GI-KS is associated with a poor prognosis. The diagnosis of GI-KS could be challenging in the presence of overlapping features with opportunistic GI infections and absence of cutaneous manifestations of KS. Early endoscopic evaluation with biopsy could help in timely diagnosis and management of GI-KS and ultimately improve outcomes. We suggest that clinicians should consider early endoscopy in the primary diagnostic workup of diarrhea and other nonspecific abdominal symptoms in patients with HIV/AIDS that are at high risk for GI-KS.
Statement of Ethics
Written and informed consent was obtained from the patient to publish this case including the images.
Disclosure Statement
The authors do not have any conflicts of interest to disclose or any financial disclosures.
Funding Sources
No funding was used for this study.
Author Contributions
All the authors contributed to the preparation and writing of the manuscript.
Acknowledgement
We would like to acknowledge the Pathology residency department, Emory University, Atlanta, GA, USA, for their assistance with obtaining and interpreting the pathology slides used in this study.
References
- 1.International Collaboration on HIV and Cancer Highly active antiretroviral therapy and incidence of cancer in human immunodeficiency virus-infected adults. J Natl Cancer Inst. 2000 Nov;92((22)):1823–30. doi: 10.1093/jnci/92.22.1823. [DOI] [PubMed] [Google Scholar]
- 2.Chang Y, Cesarman E, Pessin MS, et al. Identification of herpes-like DNA sequences in AIDS-associated kaposi's sarcoma. Science (80-) 1994;266((5192)):1865–1869. doi: 10.1126/science.7997879. doi:. [DOI] [PubMed] [Google Scholar]
- 3.Arora M, Goldberg EM. Kaposi sarcoma involving the gastrointestinal tract. Gastroenterol Hepatol (N Y) 2010 Jul;6((7)):459–62. [PMC free article] [PubMed] [Google Scholar]
- 4.Lee AJ, Brenner L, Mourad B, Monteiro C, Vega KJ, Munoz JC. Gastrointestinal Kaposi's sarcoma: case report and review of the literature. World J Gastrointest Pharmacol Ther. 2015 Aug;6((3)):89–95. doi: 10.4292/wjgpt.v6.i3.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nagata N, Shimbo T, Yazaki H, Asayama N, Akiyama J, Teruya K, et al. Predictive clinical factors in the diagnosis of gastrointestinal Kaposi's sarcoma and its endoscopic severity. PLoS One. 2012;7((11)):e46967. doi: 10.1371/journal.pone.0046967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mansfield SA, Stawicki SP, Forbes RC, Papadimos TJ, Lindsey DE. Acute upper gastrointestinal bleeding secondary to Kaposi sarcoma as initial presentation of HIV infection. J Gastrointestin Liver Dis. 2013 Dec;22((4)):441–5. [PMC free article] [PubMed] [Google Scholar]
- 7.W. R P. S, S. S. Kaposi sarcoma presenting as massive gastrointestinal bleeding. Am J Gastroenterol. 2012;107:S272–3. [Google Scholar]
- 8.Rezende RE, Kahwage RL, da Costa TV, Machado AA, Brunaldi MO, Kemp R, et al. Upper gastrointestinal Kaposi's sarcoma in HIV-infected patients: ten years of endoscopy observation at a single Brazilian center. Int J Infect Dis. 2015 Oct;39:110–5. doi: 10.1016/j.ijid.2015.09.006. [DOI] [PubMed] [Google Scholar]
- 9.AIDSinfo . Guidel Prev Treat Opportunistic Infect HIV-Infected Adults Adolesc. 2017. Guidelines for Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents. [Google Scholar]
- 10.La Ferla L, Pinzone MR, Nunnari G, Martellotta F, Lleshi A, Tirelli U, et al. Kaposi' s sarcoma in HIV-positive patients: the state of art in the HAART-era. Eur Rev Med Pharmacol Sci. 2013 Sep;17((17)):2354–65. [PubMed] [Google Scholar]
- 11.Lodi S, Guiguet M, Costagliola D, Fisher M, de Luca A, Porter K, CASCADE Collaboration Kaposi sarcoma incidence and survival among HIV-infected homosexual men after HIV seroconversion. J Natl Cancer Inst. 2010 Jun;102((11)):784–92. doi: 10.1093/jnci/djq134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mönkemüller KE, Wilcox CM. Diagnosis and treatment of colonic disease in AIDS. Gastrointest Endosc Clin N Am. 1998 Oct;8((4)):889–911. doi: 10.1016/S1052-5157(18)30238-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bower M, Collins S, Cottrill C, Cwynarski K, Montoto S, Nelson M, et al. AIDS Malignancy Subcommittee British HIV Association guidelines for HIV-associated malignancies 2008. HIV Med. 2008 Jul;9((6)):336–88. doi: 10.1111/j.1468-1293.2008.00608.x. 10.1111/hiv.12136. [DOI] [PubMed] [Google Scholar]
- 14.Bower M, Dalla Pria A, Coyle C, Andrews E, Tittle V, Dhoot S, et al. Prospective stage-stratified approach to AIDS-related Kaposi's sarcoma. J Clin Oncol. 2014 Feb;32((5)):409–14. doi: 10.1200/JCO.2013.51.6757. [DOI] [PubMed] [Google Scholar]