Abstract
We present a female patient, 13 years old, with diagnosis of hepatocellular carcinoma of fibrolamellar type, which was rapidly evolving. The fibrolamellar hepatocellular carcinoma invaded more than 80% of the hepatic parenchyma without surgical possibility or liver transplantation. Measures applied corresponded to chemotherapy of 1 cycle of cisplatin 40 mg/s/5 days + vincristine 1.5 mg/m<sup>2</sup>/day, 5-fluorouracil, doxorubicin, and dexrazoxane. The case presented aggressive evolution of hepatocellular carcinoma, which led to acute liver failure, with hyperammonemia, sepsis, pulmonary focus plus septic shock, grade III-IV encephalopathy, portal hypertension, and ascites with intra-abdominal hypertension. Death occurred due to multiple organ failure, which involved respiratory failure type KDIGO 1 and 2, acute liver failure, severe pneumonia, pericardial effusion, AKIN 2 acute kidney injury, carcinoma, and pulmonary metastasis. This type of ailment is infrequent in children and adolescents, and the first symptoms are crucial to achieve treatment possibilities.
Keywords: Hepatocellular carcinoma, Encephalopathy, Hyperammonemia, Mexican children
Introduction
Hepatocellular carcinoma (HCC) is a rare tumor, and when it occurs in children, it has a low incidence of 1.6 cases per million, compared with hepatoblastomas, which are more frequent and reach up to 80% of cancer cases in the liver and affect children in the age range of 6 months to 3 years. HCC increases its incidence with greater age [1], but only 0.5–1% of all tumors in children are HCC. In children, when the diagnosis of HCC is early, treatment by chemotherapy shows that about 50% of cases are sensitive and respond to the treatment of cisplatin and doxorubicin, with a significant reduction in α-fetoprotein (AFP) and tumor size [2].
Although there is still a long way to know about the origin of HCC in children and the pathogenesis, more related factors to HCC are attributed to the incidence of infection with the hepatitis B virus (HBV) with an estimated risk of 10% to 25%, a situation that has been demonstrated in several areas of Taiwan, Hong Kong, and other Asian regions, where children with HCC have a history of having presented HBV [3], this being the difference with respect to adults, where the observed risk factors are cirrhosis, chronic diseases such as alteration of the type III glycogen store, type I tyrosinemia, and Wilson's disease or biliary atresia. Other risk factors in different areas of Asia that add up for HCC include Alagille syndrome, maternal HBV infection, progressive familial intrahepatic disease, and tyrosinemia; for the last two factors, when being detected in time, liver transplant before the appearance of symptoms and signs of cancer shows good results [4, 5, 6].
In Japan during the years 2012 and 2013 in a multicenter study, they evaluated children with HCC and the relationship with HBV was positive, in addition to AFP as an indicator in the diagnosis of HCC-HBV, where the records had such high values as 1,225 and up to 2,240,000 ng/mL of AFP [7], when the AFP reference in healthy individuals is less than 20 to 100 ng/mL. In different cases reported in children and adolescents who associated HBV with HCC, they found that the route of greatest coincidence in viral transmission is maternal, followed by blood transfusion; the cases of advanced-stage HCC progress to liver cirrhosis and pulmonary metastasis, where most cases die, with few surviving [8, 9, 10].
Total or partial liver transplantation is another possibility to treat HCC in children; however, it has been reported that there is a low survival rate in advanced stages of the disease compared with other cancers of the liver such as hepatoblastoma, embryonic cancer, biliary atresia, and bile duct cancer. The registry of preexisting diseases with involvement in liver function included cirrhosis due to cholestasis of the liver, hepatitis B, and metabolic disorder [4, 5, 11]. The success of liver transplantation includes factors such as male sex, cirrhosis, bilobal location, multiple carcinogenic sites, vascular invasion, presence of metastases, positive margins to the disease, and stages III and IV of HCC. Thus, liver transplantation can be functional in children when HCC is detected in initial stages I and II and hase low vascularization or invasion of tissue [12].
Metabolic deficiencies related to HCC in children are alterations in the pentose phosphate pathway involved with the production of NADPH used in various metabolic pathways of biosynthesis and reduction of glutathione. It has been demonstrated that the deficiency in transaldolase occurs as a mutation in pR192C in the TALDO 1 gene reported in the population of the Arab Emirates; clinically, in hepatosplenomegaly with progression to cirrhosis, nephropathies, connective tissue abnormalities, coagulopathies, cytopenia, heart disease, and high risk of HCC, in most cases, death occurs in childhood due to metabolic complications, the indicators being the coagulation alterations with prothrombin time >15 s, which does not correct with the administration of vitamin K, high bilirubin for more than a week, and the international normalized index >1.5 (TP >26 or INR >2), similar to the presence of neuropsychiatric signs with alterations in ALT levels, acid-base, and electrolyte imbalance [cited in 13]. The increase in AFP is associated with the development of HCC tested in a mouse model [14] and in children who presented HCC [7].
Few cases of HCC have been reported in children in Mexico, considering that there is a vaccination scheme from birth that is protective in the first years of life and includes the hepatitis B vaccine. Functional deficiencies of the liver in the case of the study are described in a 13-year-old female adolescent with a short time (4 months) between the first symptoms and the evolution of HCC until death occurred.
Case Report/Case Presentation
A female, 13 years of age, presented with abdominal distension, generalized pain, and a weight loss of approximately 5 kg within a 2-month period. The TAC revealed hypodense tumoration, heterogeneous with the involvement of segments II, IVa, and IVb (Fig. 1 and 2). Extension included nearly the whole right hemiabdomen and part of the left (80% of the hepatic parenchyma), without data of peritoneal irritation. Initial biopsy by TRUCUT and the histopathology reported fibrolamellar-type HCC (Fig. 3). Extension studies revealed metastasis to the lung, high serum markers in serum AFP, and negative detection of the hepatitis B and C viruses. There was a paternal antecedent of cancer of the pancreas. She had complete immunizations for BCG (hepatitis B), pentavalent, DPT (rotavirus, pneumococcus, influenza), and serine/arginine-rich human papilloma virus (SR-HPV).
Fig. 1.

Computed tomography revealed hypodense, heterogeneous tumor with involvement of segments II, IVa, and IVb.
Fig. 2.

Computed tomography revealed extension of almost all of the right hemiabdomen and part of the left one (80% of the liver parenchyma), without data of peritoneal irritation.
Fig. 3.
Histopathology reported fibrolamellar-type hepatocellular carcinoma.
HCC imaging and the surgical assessment indicated little probability of resection, the reason for which management was established with neoadjuvant chemotherapy with cisplatin 40 mg/s/5 days plus vincristine 1.5 mg/m2 on day 1, 5-fluorouracil, doxorubicin, and dexrazoxane with the purpose of tumor cytoreduction. At 2 weeks of diagnosis and follow-up, TAC revealed abdomen with carcinomatosis and renal and pulmonary tumor activity. At the same time, acute kidney failure presented with ammonemia, with response to conventional measures, reaching levels of ammonemia of 416 mg/dL and a high possibility of cerebral edema. The application of renal PRISMA only achieved reduction to levels of 150 and 290 mg/dL, with evident nonreversible acute kidney failure and no candidacy for liver transplantation. In week 3 of follow-up with encephalopathy, liver failure, and hyperammonemia, kidney failure was considered without response to the application of PRISMA and MARS with time limit-of-function. The patient's decease was registered with a follow-up of 27 days under hospitalization and a previous antecedent of 45 days to symptomatology. The patient had acute kidney failure, hyperammonemia, sepsis without isolated focus, fibrolamellar hepatocarcinoma, hepatic encephalopathy grade III-IV, portal hypertension, ascites with probable intrabdominal hypertension, sepsis with pulmonary shock plus Kidney Disease Improving Global Outcomes (KDIGO) types 1 and 2 respiratory insufficiency, acute kidney failure, severe pneumonia, hemorrhage in pericardium, Acute Kidney Injury Network (AKIN) 2, carcinoma, and pulmonary metastasis.
Histopathological Analysis
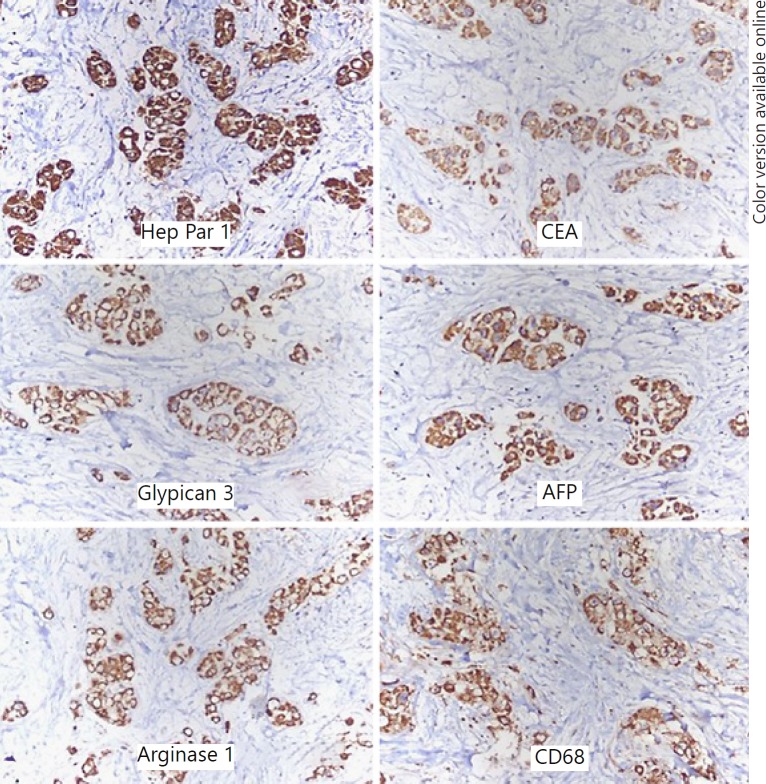
Evaluation of the slides of the initial biopsy showed the following: immunohistochemistry with Hep Par 1-positive carcinoembryonic antigen, positive arginase, positive CD68, and positive serum AFP, resulting in cellular and morphological elements that were consistent with stage IV fibrolamellar HCC, with moderate necrotic changes associated with slight inflammation and slight desmoplasia, vascular permeation, or absent neural. There was residual hepatic tissue with chronic slight portal inflammation (Fig. 3 and 4).
Fig. 4.
Immunohistochemistry with Hep Par 1-positive carcinoembryonic antigen, positive arginase, positive CD68, and positive serum α-fetoprotein (AFP). Stage IV fibrolamellar hepatocellular carcinoma.
Clinical Analysis
The clinical follow-up approached the assessment of hepatic enzymes, coagulation times, ionic control, chemotherapy, and hematological and neurological follow-up, with the most important data observed in Table 1. There was hemodynamic follow-up, cardiorespiratory follow-up, and uresis.
Table 1.
Follow-up hemodynamic, cardiorespiratory, and uresis values
| Week 1 |
Week 2 |
Week 3 |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| BP | 103/68 | 91/70 | 112/75 | 103/68 | 93/69 | 115/76 | 130/90 | 138/64 | 110/56 | 73/39 |
| HR | 86 | 93 | 100 | 123 | 120 | 120 | 113 | 68 | 88 | 140 |
| BF | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 | 20 |
| °T | 36 | 35.7 | 36.2 | 36 | 35.9 | 37 | 36 | 35.2 | 36.3 | 38.3 |
| SAT | 96 | 96 | 94 | 97 | 97 | 98 | 98 | 99 | 100 | |
| UI | 940 | 900 | 840 | 80 | 123 | 80 | 23 | 28 | 5 | 0 |
BP, blood pressure; HR, heart rate; BF, breathing frequency; °T, temperature; SAT, saturation; UI, urinary index.
Discussion
Liver failure has been described as rare in children, as has the incidence of HCC. However, when it presents, it is lethal. The alternatives that are suggested in other groups include liver transplantation within a very short time and under poorly stable conditions of the patients [2, 11]. The etiology of cases of HCC assume the infectious origin due to the viruses of hepatitis A, B, not A, not B, D, and E, Epstein-Barr and cytomegalovirus, being most frequent in zones with poorly active or null programs with respect to vaccination, as occurs in various Asian countries [8, 9, 10, 14, 15, 16]. Other causes that lead to liver failure are associated with hepatotoxic drugs (acetaminophen, paracetamol, nitrofurantoin, ciprofloxacin, amoxillin, clavulanic acid, valproic acid, sulfas, and diclofenac), toxins (fungi, organic solvents, medicinal herbs, bacteria), and metabolic diseases, such as fatty liver, hemolysis, elevated liver enzyme levels, and low platelet levels (HELPP syndrome), leukemia, lymphoma, tuberculosis, tumors, and Reye syndrome [4, 5, 17].
Hepatitis is a high-risk factor for the manifestation of HCC in child population, verified in diverse regions of Asia, where it was not until the 80s and 90s that vaccination systems were implemented, observing an important diminution in cases of HCC [18].
The case study described herein can be classified as a case of acute liver failure of tumor origin with an evolution of approximately 4 months in the manifestation of the symptomatology of carcinoma identified as fibrolamellar-type HCC, which is, in the child population in Mexico, registered at a low percentage of incidence of 0.5% in hepatic tumors in children and adolescents. The case was identified as stage IV HCC due to pulmonary and peritoneal cavity metastases, with an extension greater than 80% in hepatic parenchyma and being unresectable (Fig. 1 and 2). Thus, the treatment option comprised chemotherapy as unique cycle in that the advance of the disease was rapid (at 1 week of diagnosis) and led to acute liver failure with grade 4 hyperammonemia, with ammonia greater than 200 mg/dL, and even higher than 400 mg/dL. It is noteworthy that patients with hyperammonemia do not achieve purification of high levels of ammonium [19], in addition to the provision of kidney support with PRISMA and MARS, with a partial response in the decrease of plasma ammonium of around 150 mg/dL without reaching normality.
The hyperammonemia of the patient that led to hepatic encephalopathy did not only imply hepatic injury, but also metabolic disorders and alterations in the concentration of ammonia, urea, glutaminase, alteration of glucose, and an excess of toxins in the central nervous system, a situation that caused disorientation and cognitive disorders in their primary manifestations [6, 20]. In the treatment of the case and the following of the guidelines, we ran out of options while, in addition to the non-resection of the HCC [21], liver transplantation was not an option due to the rapid evolution of the HCC, and even less so in the face of the evolution of a poor prognosis that existed from the moment of diagnosis.
As may be observed in Tables 2 and 3, the case presented various criteria of poor prognosis, such as alteration in the coagulation times of >15 s and higher bilirubin levels for more than 1 week of evolution. Additionally, the normalized international index of >1.5, rather than the TP, was not corrected with the administration of vitamin K (TP >26 s or INR >2). Also, neuropsychiatric signs, alteration in alanine aminotransferase (ALT) levels, and acid-base and electrolyte disequilibrium were present (Table 3). Unfortunately, the etiological origin of the HCC was unable to be identified, in that the antecedents complied with the complete vaccination scheme and with good health until the manifestation of the HCC.
Table 2.
Metabolic monitoring of coagulation times and liver enzymes
| Parameters | Diagnosis | Week 1 | Week 2 | Week 3 |
|---|---|---|---|---|
| Procalcitonin (<0.5 ng/mL) | 87 | 106 and 1,232 | 172 | 200 |
| PCR (0–3 mg/L) | 70 | 186 and 446 | 233 | 160 |
| Total bilirubin (0.3–1.3 ng/dL) | 0.6 | 1.3 | ||
| FA (33–96 U/L) | 141 | |||
| TGO (12–38 U/L) | 184 | |||
| TGP (7–41 U/L) | 182 | |||
| GGT (9.58 U/L) | 124 | |||
| Albumin (3.5–5.5 g/dL) | 3.1 | |||
| TP (12.7–15.4 s) | 21 | 22.3 and 30 | 20 | 18 |
| TPT (25–35 s) | 26 | 44 and 120 | 44 | 45 |
Table 3.
Metabolic data and ionic balance
| Parameters/reference | Diagnostic | Week 1 | Week 2 | Week 3 | ||
|---|---|---|---|---|---|---|
| Na+ (137–145 mmol/L) | 144 | 145 | 149 | 145 | 144 | 145 |
| K+ (3.6–5 mmol/L) | 4.2 | 3.4 | 4.1 | 3.6 | 4.5 | 3.4 |
| Cl (99–105 mmol/L) | 103 | 107 | 111 | 107 | 106 | 106 |
| Ca+2 (8.5–10.2 mg) | 9.2 | 8.6 | 9.0 | 9.0 | 9.0 | 8.7 |
| P (2.5–4.5 mg) | 3.9 | 5 | 5 | 3.7 | 1.7 | 2.7 |
| Mg+2 (1.7–1.2 mg) | 1.7 | 1.7 | 2 | 2.7 | 2.1 | 1.7 |
| Creatinine (3.3±0.3 mg/dL) | 0.6 | 0.7 | 0.7 | 0.7 | 0.5 | 0.5 |
| BUN (0.7–1.2 mg/dL) | 7 | 16 | 18 | 14 | 14 | |
| Urea (6–20 mg/dL) | 15 | 27 | 34 | 30 | 30 | |
| Glucose (70–100 mg) | 125 | 122 | 131 | 134 | 110 | 134 |
| Lactate (2 mmol/L) | 20.2 | 20 | 21 | 24 | ||
| Ammonium (15–45 µg/dL or 11–32 µmol/L) | 290 | 416 | 368 | 290 | 165 | 228 and 153 |
The hematological follow-up was also assessed (Table 4), the latter including surveillance of the case, which exhibited sepsis and chemotherapy-associated medullary aplasia. The HCC evolved with repercussions on the liver failure, the clinical treatment did not function, and the poor prognosis reached 27 days of the treatment approach. From the beginning, the case was approached by palliative care by means of whoever was administering comfort care and sedation analgesia. In terms of the control of convulsions and abnormal movements, from the time of hepatic failure, the pupils were isochoric, and hemodynamically, the status was hypotension, tachycardia, capillary filling greater than 3 s, low pulses, and with not-reported or null uresis. Ventilator phase was III A/C. Additionally, the patient exhibited systemic inflammatory response. The prognosis always indicated an elevated risk of complications, such as cardiac failure, septic shock, disseminated intravascular coagulation, liver failure, multiple organ dysfunction, and death.
Table 4.
Hematological parameters
| Parameters | Diagnostic | Week 1 | Week 2 | Week 3 | |||
|---|---|---|---|---|---|---|---|
| Hemoglobin (12–18 mg/dL) | 14.3 | 14.1 | 12.0 | 11.4 | - | 10.1 | 10.8 |
| Hematocrit (37–54%) | 47.0 | 47.4 | 42.0 | 34.2 | - | 29.7 | 33.4 |
| Leukocytes (5–10 thousand/µL) | 19,910 | 19,910 | 16,000 | - | 1,680 | 630 | 700 |
| Neutrophils (1.5–7.4 millon/µL) | 17,600 | 17,650 | 17,000 | 1,080 | 160 | 10 | |
| Lymphocytes (0.94–4.8 millon/µL) | 1,500 | 1,570 | - | - | 550 | 460 | 680 |
| Monocytes (0–0.8 millon/µL) | 610 | 610 | - | - | - | - | - |
| Platelets (l50–500 thousand) | 480 | 480 | 415 | 190 | 49 | 42 | 17 |
Conclusion
In sum, this rare case in a child population in Mexico corresponded to one of stage IV fibrolamellar HCC (of 3 months of evolution) that led to multiple organ failure and sepsis with 3 weeks of evolution in hospital. In cases such as this and with high cellular aggression, treatment alternatives are few.
Statement of Ethics
This work was carried out in compliance with the ethical regulations and informed consent in the handling of information and the safeguarding of personal data. The authors have no ethical conflicts to disclose.
Disclosure Statement
The authors have no conflicts of interest to declare.
Funding Sources
This work was carried out under the medical care scheme called “Popular Insurance,” which is an economic support that covers the costs of medical care and medicines and clinical analysis for patients seen from the Third Level and High Hospital system and Medical Speciality. Due to the above, the economic credit for this work is supported in the administration of the High Specialty Regional Hospital of Bajío for the Department of Education and Research.
Author Contributions
Javier Santiago-Reynoso, Karina Senyase Zamaripa-Martínez, Juan Manuel Dorantes-Loya, Guillermo J. Gaytán-Fernández: medical care team of patients in different days of work during the week and weekend, specialists in oncopediatrics, hematology, and internal medicine. Evelia Apolinar-Jiménez: specialist in nutrition with participation in patient program during hospitalization. Francisco Paz-Gómez: histopathologist specialist, with work in handling of biopsies, immunohistological stains of study case. Felipe Farias-Serratos: subspecialty in neurosurgery, considered in the opinion of the case due to neurological failures. María Maldonado-Vega: toxicology specialist and participant in the follow-up of the case study during her hospital stay.
Acknowledgement
Nursing staff and clinician staff who tried to handle sample, and services of the Regional Hospital of High Specialty Bajío. The authors thank Carlos Tena Tamayo Principal of High Specialty Regional Hospital for the financial support to carry out the study from the Department of Education, Planning and Research.
References
- 1.Goh GB, Li JW, Chang PE, Chow KY, Tan CK. Deciphering the epidemiology of hepatocellular carcinoma through the passage of time: A study of 1,401 patients across 3 decades. Hepatol Commun. 2017 Jun;1((6)):564–71. doi: 10.1002/hep4.1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schmid I, von Schweinitz D. Pediatric hepatocellular carcinoma: challenges and solutions. J Hepatocell Carcinoma. 2017 Jan;4:15–21. doi: 10.2147/JHC.S94008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pronocitro C, Mulyani NS, Ghufron AA, Hazazi YH, Ardianto B, Heriyanto DS. Efficacy of Hepatitis B Vaccination among Children in Special Region of Yogyakarta, Indonesia: Evaluation of Humoral and Cellular Immunity. Kobe J Med Sci. 2018 Jan;63((3)):E92–8. [PMC free article] [PubMed] [Google Scholar]
- 4.Jiménez Gómez JM, Begoña PM, Donat Aliaga E. Hepatología y Nutrición SEGHNP-AEP. 2009. Fallo hepático agudo. Protocolos diagnóstico-terapéuticos de Gastroenterología; pp. pp. 197–204. [Google Scholar]
- 5.Sotelo Cruz N. Diagnóstico y tratamiento de niños con falla hepática aguda. Revista Mexicana de Pediatria. 2010;77((2)):72–7. [Google Scholar]
- 6.Reyes-Cerecedo A, Flores-calderón J, Villasis-Keever MA, Ortiz-Galván RC, et al. Consenso para el manejo de la falla hepática aguda en pediatría. Rev Mex Pediatr. 2017;84((3)):120–6. [Google Scholar]
- 7.Tajiri H, Takano T, Tanaka H, Ushijima K, Inui A, Miyoshi Y, et al. Hepatocellular carcinoma in children and young patients with chronic HBV infection and the usefulness of alpha-fetoprotein assessment. Cancer Med. 2016 Nov;5((11)):3102–10. doi: 10.1002/cam4.917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Poovorawan Y, Sripattanawat R, Theamboonlers A, Chongsrisawat V, Nuchprayoon I. Hepatocellular carcinoma: significance of HBV vertical transmission. Asian Pac J Allergy Immunol. 1998 Jun-Sep;16((2-3)):93–103. [PubMed] [Google Scholar]
- 9.Tanaka T, Miyamoto H, Hino O, Kitagawa T, Koike M, Iizuka T, et al. Primary hepatocellular carcinoma with hepatitis B virus-DNA integration in a 4-year-old boy. Hum Pathol. 1986 Feb;17((2)):202–4. doi: 10.1016/s0046-8177(86)80296-9. [DOI] [PubMed] [Google Scholar]
- 10.Shimoda T, Uchida T, Miyata H, Abe K, Ariga H, Shikata T, et al. A 6-year-old boy having hepatocellular carcinoma associated with hepatitis B surface antigenemia. Am J Clin Pathol. 1980 Dec;74((6)):827–31. doi: 10.1093/ajcp/74.6.827. [DOI] [PubMed] [Google Scholar]
- 11.Vinayak R, Cruz RJ, Jr, Ranganathan S, Mohanka R, Mazariegos G, Soltys K, et al. Pediatric liver transplantation for hepatocellular cancer and rare liver malignancies: US multicenter and single-center experience (1981-2015) Liver Transpl. 2017 Dec;23((12)):1577–88. doi: 10.1002/lt.24847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shen JY, Li C., Wen TF., Yan LN., Li B., Wang WT., Yang JY., Xu MQ., Highness TN. Liver transplantation versus surgical resection for HCC meeting the Milan criteria. Medicine. 2016;95((52)):e5756. doi: 10.1097/MD.0000000000005756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rodan LH, Berry GT. N-Acetylcysteine Therapy in an Infant with Transaldolase Deficiency Is Well Tolerated and Associated with Normalization of Alpha Fetoprotein Levels. JIMD Rep. 2017;31:73–7. doi: 10.1007/8904_2016_555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hanczko R, Fernandez DR, Doherty E, Qian Y, Vas G, Niland B, et al. Prevention of hepatocarcinogenesis and increased susceptibility to acetaminophen-induced liver failure in transaldolase-deficient mice by N-acetylcysteine. J Clin Invest. 2009 Jun;119((6)):1546–57. doi: 10.1172/JCI35722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tajiri H, Takano T, Tanaka H, Ushijima K, Inui A, Miyoshi Y, et al. Hepatocellular carcinoma in children and young patients with chronic HBV infection and the usefulness of alpha-fetoprotein assessment. Cancer Med. 2016 Nov;5((11)):3102–10. doi: 10.1002/cam4.917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shen JY, Li C, Wen TF, Yan LN, Li B, Wang WT, et al. Lv-Nan Yan, Bo Li, Wen-Tao Wang, Jia-Yin Yang, Ming-Qing Xu, Tholakkara Nazar Highness. Liver transplantation versus surgical resection for HCC meeting the Milan criteria. A propensity score analysis. Medicine (Baltimore) 2016;95((52)):52. doi: 10.1097/MD.0000000000005756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roque JE, Rios GM, Pinochet VC, Vignolo AP, Humeres AR, Rios RH, Quiroga GM, Rodríguez MG, Mora X, rius AM, Hepp KJ. Falla Hepática fulminante en Niños. Rev Chil Pediatr. 2009;80((2)):144–9. [Google Scholar]
- 18.Goh GBB., Li JW., Chang PE., Chow KY, Tan CK. Deciphering the epidemiology of hepatocellular carcinoma through the passage of time: a study of 1,401 patients across 3 decades. Hepatology communications. 2017;1((6)):564–571. doi: 10.1002/hep4.1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sethi S, Tageja N, Singh J, Arabi H, Dave M, Badheka A, et al. Hyperammonemic encephalopathy: a rare presentation of fibrolamellar hepatocellular carcinoma. Am J Med Sci. 2009 Dec;338((6)):522–4. doi: 10.1097/MAJ.0b013e3181bccfb4. [DOI] [PubMed] [Google Scholar]
- 20.Tong MJ, Rosinski AA, Huynh CT, Raman SS, Lu DS. Long-term survival after surveillance and treatment in patients with chronic viral hepatitis and hepatocellular carcinoma. Hepatol Commun. 2017 Jun;1((7)):595–608. doi: 10.1002/hep4.1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hae WL., Jeong ML., Jung-Hwan Y., Yoon JK., Joong-Won P., Sang-Jae P., Seong HK., Nam-Joon Y., Kyung-Suk S. A prospective randomized study comparing radiofrecuency ablation and hepatic resection for hepatocellular carcinoma. Annals of Surgical Treatment and Research. 2018;94:2–74. doi: 10.4174/astr.2018.94.2.74. https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]