Hyperparathyroidism is underdiagnosed and undertreated. This article addresses the reasons for these gaps in care.
Keywords: Hyperparathyroidism, Parathyroid hormone, Underdiagnosed, Undertreated
Abstract
Background.
Hyperparathyroidism is both underdiagnosed and undertreated, but the reasons for these deficiencies have not been described. The purpose of this study was to identify reasons for underdiagnosis and undertreatment of hyperparathyroidism that could be addressed by targeted interventions.
Materials and Methods.
We identified 3,200 patients with hypercalcemia (serum calcium >10.5 mg/dL) who had parathyroid hormone (PTH) levels evaluated at our institution from 2011 to 2016. We randomly sampled 60 patients and divided them into three groups based on their PTH levels. Two independent reviewers examined clinical notes and diagnostic data to identify reasons for delayed diagnosis or referral for treatment.
Results.
The mean age of the patients was 61 ± 16.5 years, 68% were women, and 55% were white. Fifty percent of patients had ≥1 elevated calcium that was missed by their primary care provider. Hypercalcemia was frequently attributed to causes other than hyperparathyroidism, including diuretics (12%), calcium supplements (12%), dehydration (5%), and renal dysfunction (3%). Even when calcium and PTH were both elevated, the diagnosis was missed or delayed in 40% of patients. For 7% of patients, a nonsurgeon stated that surgery offered no benefit; 22% of patients were offered medical treatment or observation, and 8% opted not to see a surgeon. Only 20% of patients were referred for surgical evaluation, and they waited a median of 16 months before seeing a surgeon.
Conclusion.
To address common causes for delayed diagnosis and treatment of hyperparathyroidism, we must improve systems for recognizing hypercalcemia and better educate patients and providers about the consequences of untreated disease.
Implications for Practice.
This study identified reasons why patients experience delays in workup, diagnosis, and treatment of primary hyperparathyroidism. These data provide valuable information for developing interventions that increase rates of diagnosis and referral.
Introduction
There is significant room for improvement in the diagnosis and treatment of hyperparathyroidism, but limited information exists on how to improve care for these patients. Hyperparathyroidism is the most common cause of hypercalcemia and affects nearly 2 million Americans [1]. The disease should be suspected when patients present with an elevated serum calcium, and the diagnosis should be confirmed by measuring serum parathyroid hormone (PTH) levels. Hyperparathyroidism is then diagnosed in patients with high (or inadequately suppressed) PTH in the setting of hypercalcemia.
Multiple studies have shown that only about one third of patients with the disease get the appropriate diagnostic workup, and only 20%–30% who are candidates for parathyroidectomy actually get referred to a surgeon to discuss treatment [2], [3]. Untreated hyperparathyroidism increases the risk of adverse events, including nephrolithiasis, osteoporosis or fractures, renal osteodystrophy, cognitive deficits, and cardiovascular disease [4], [5], [6]. Surgical treatment of hyperparathyroidism is more cost‐effective than medical management or observation, even for disease without complications [7].
Although hyperparathyroidism is clearly underdiagnosed and undertreated, the reasons for these gaps in care have not been adequately examined. The purpose of this study was to elucidate why patients with hyperparathyroidism experience delays in diagnosis and have low rates of surgical referrals for treatment. We hypothesized that hypercalcemia might frequently be missed by busy primary care providers and that the diagnosis could be hampered by a low index of suspicion for hyperparathyroidism. We also hypothesized that parathyroidectomy might be underutilized because nonsurgeons overestimated both the risks of surgery and the benefits of medical management for hyperparathyroidism.
Subjects, Materials, and Methods
Data Source and Patient Selection
This retrospective study was approved by the University of Alabama at Birmingham (UAB) Institutional Review Board for Human Use. We used administrative data to identify 3,200 patients at our institution with hypercalcemia from January 2011 to December 2015 who underwent at least one assessment of PTH level at some point following the index calcium. To examine the possibility that the threshold for referral might be related to PTH levels, we divided the cohort into three groups based on the index PTH levels: group 1, >85 pg/mL (elevated); group 2, 66–85 pg/mL (upper limits of normal); and group 3, 21–65 pg/mL (lower limits of normal). We then randomly sampled 20 patients from each group for analysis and verified that they had primary hyperparathyroidism. Hyperparathyroidism was verified by expert review of charts to confirm that each patient had elevated parathyroid hormone in the setting of elevated serum calcium. Additionally, if a patient was found to have secondary hyperparathyroidism, that patient was excluded, and a new patient was randomly selected from the total cohort. The index PTH was defined as the first PTH obtained after the patient's initial elevated calcium level recorded in our system. At UAB, PTH is measured using the ADVIA Centaur Intact PTH assay (Siemens, Tarrytown, NY). The reference range was established on the Automated chemiluminescence immunoassay systems:180 system. Ethylenediaminetetraacetic acid plasma samples were obtained from 142 apparently healthy individuals whose calcium levels ranged from 8.0 to 10.3 mg/dL. Ninety‐five percent of the intact PTH values for these individuals fell in the range of 14–72 pg/mL (1.48–7.63 pmol/L) with an overall range of 11.1–79.5 pg/mL (1.18–8.43 pmol/L).
Patient Demographics and Characteristics
We obtained patient demographic information such as age, sex, race, body mass index (BMI), and insurance type from the electronic medical records. Complications of hyperparathyroidism (kidney stones, osteoporosis, or bone fractures) were recorded based on International Classification of Disease (ICD) revision 9 or 10 codes. The setting (inpatient, outpatient, or emergency room) for the index high calcium was also recorded. We identified the presence of comorbidities using the methods of Elixhauser [8].
Assessing Reasons for Delay in Diagnosis or Treatment of Hyperparathyroidism
Using a preestablished coding guide, two independent reviewers scrutinized clinical documentation and diagnostic data to identify reasons for missed or delayed diagnosis of hypercalcemia and hyperparathyroidism. Reasons given in the chart for not checking a PTH (i.e., attributing hypercalcemia to another cause) were also recorded. A delay in diagnosis was defined as not acknowledging hypercalcemia at the first index high calcium or not checking a PTH after noting hypercalcemia, and not making a diagnosis of hyperparathyroidism when the patient had both elevated calcium and PTH. To increase accuracy and reproducibility of the findings, a consensus was required between the two reviewers for every patient.
Study endpoints were defined as follows:
Elevated calcium not acknowledged: Clinical notes and provider communications were reviewed to determine if the index elevated calcium was acknowledged by health care providers by commenting on the result, discussing plans for further evaluation, discussing the differential, or documenting communication with other providers or the patient.
Appropriate workup of index hypercalcemia (PTH evaluated): If the index episode of hypercalcemia was acknowledged, we documented whether patients subsequently underwent the appropriate workup with evaluation of serum PTH. If no PTH was ordered for the index high calcium, possible reasons for this were gleaned from the chart.
Elevated calcium or PTH attributed to other causes: If PTH was obtained as a part of the hypercalcemia workup, we investigated whether an elevated result was addressed by the health care provider. Furthermore, we recorded whether alternate diagnoses other than hyperparathyroidism were entertained.
Discussion of treatment options and referral for parathyroidectomy: When the diagnosis of hyperparathyroidism was established, we examined the clinical notes to determine which treatment options were documented as discussed with the patient. We then documented the reasons for referral (or nonreferral) for surgical evaluation. Among patients who were referred to a surgeon, we evaluated indications for and rates of parathyroidectomy.
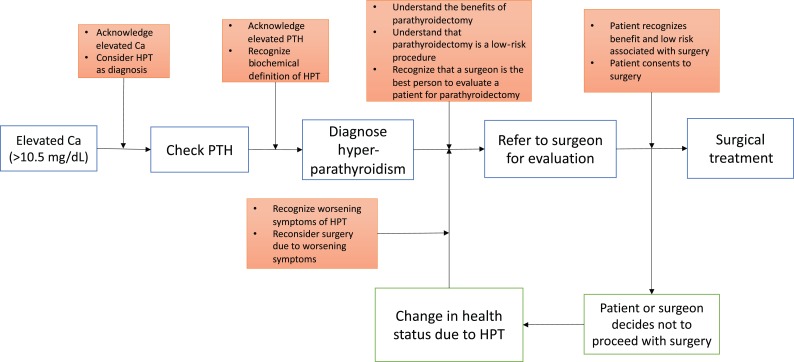
Additionally, we created a flowchart that demonstrates the sequence of events and key decision elements in a chronological order from the index calcium to surgical referral and parathyroidectomy (Fig. 1).
Figure 1.
Flowchart that demonstrates the sequence of events and key decision elements from the index calcium to surgical referral and parathyroidectomy.
Abbreviations: Ca, calcium; HPT, hyperparathyroidism; PTH, parathyroid hormone.
Statistical Analysis
We used the likelihood ratio chi‐square test to compare proportions across groups based on the index PTH and the Kruskal‐Wallis test for continuous variables. Differences were considered significant at α < .05, and all analysis was performed using Stata software (version 14.0, 2015; StataCorp, College Station, TX).
Results
Patient Demographics and Clinical Characteristics
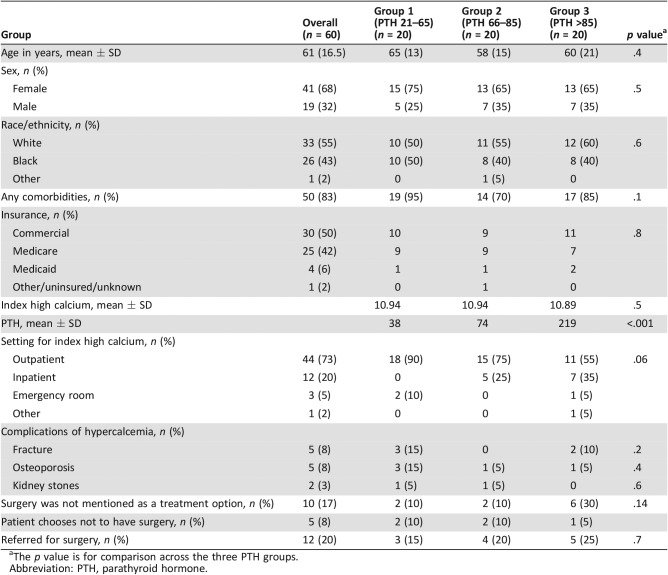
The mean age of our cohort was 61 ± 16.5 years. Forty‐one patients (68%) were women, and 33 (55%) were white. The mean BMI of the cohort was 27 ± 6.4 kg/m2. The majority of patients (73.3%) had their index high calcium evaluated in an outpatient setting, and 20% were seen as inpatients. Most patients had commercial insurance (50%), followed by Medicare (41%) and Medicaid (7%). Fifty patients (83%) had at least one comorbidity (Table 1). Complications of hyperparathyroidism included osteoporosis in five patients (8%), fractures in five patients (8%), and nephrolithiasis in two patients (3%). There was no difference in the mean index serum calcium between the three PTH groups (p = .5; Table 1).
Table 1. Comparison of demographics and reasons for delayed diagnosis or treatment across groups based on PTH levels.
The p value is for comparison across the three PTH groups.
Abbreviation: PTH, parathyroid hormone.
Reasons for Delayed Diagnosis of Hyperparathyroidism
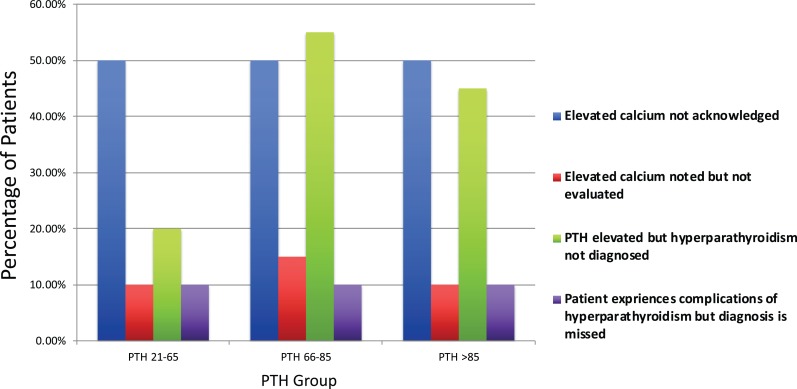
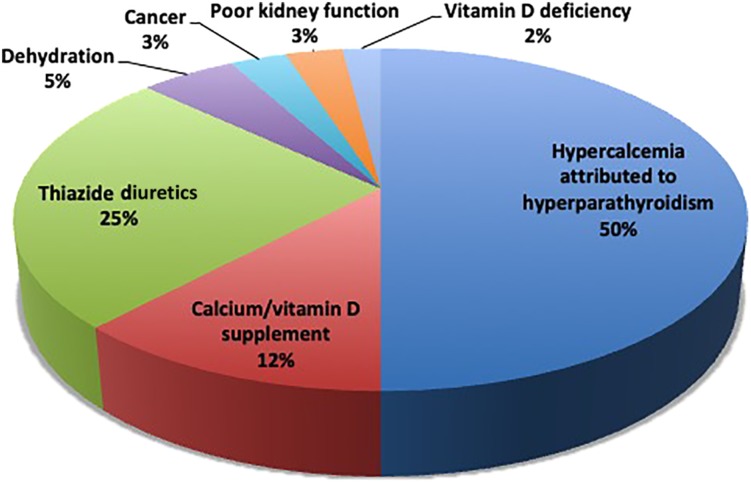
Fifty percent of patients had at least one high calcium that was not acknowledged by their provider (either in clinic notes or provider communications or by ordering additional evaluation), and 12% (7 of 60) of patients did not have PTH checked as part of the initial hypercalcemia workup for their index high calcium (Fig. 2). The remaining patients had PTH levels evaluated following another high calcium after the index lab value. The rates of missed hypercalcemia were similar across the three PTH groups (Fig. 2). Additionally, when patients were divided into two groups based on calcium levels (10.6–11 mg/dL and >11 mg/dL), hypercalcemia was missed in 53% of patients in the former and 38% of the latter group. The most common reasons for failure to work up a high calcium included a proposed plan to recheck calcium that was never completed (two patients), attributing hypercalcemia to laboratory error (two patients), and no clear reason that we could identify (three patients; Table 1). Hypercalcemia was attributed to causes other than hyperparathyroidism in 19 (32%) patients. Common alternate explanations for hypercalcemia included calcium supplementation (12%), thiazide diuretics (25%), dehydration (5%), cancer (3%), impaired renal function (3%), and vitamin D deficiency (2%) (Fig. 3). In patients with lower PTH levels (group 1), clinicians were significantly more likely to attribute hypercalcemia to either calcium supplements or thiazide use than in patients with higher PTH levels (groups 2 and 3; Fig. 3).
Figure 2.
The reasons for delayed diagnosis of hyperparathyroidism are similar regardless of index parathyroid hormone level.
Abbreviation: PTH, parathyroid hormone.
Figure 3.
Hypercalcemia is frequently misattributed to causes other than hyperparathyroidism.
Even when there was at least one clearly elevated PTH in the setting of hypercalcemia, hyperparathyroidism was not considered as the likely cause in 40% of patients (4 of 20), including in ∼50% of patients in the two highest PTH groups (Fig. 3).
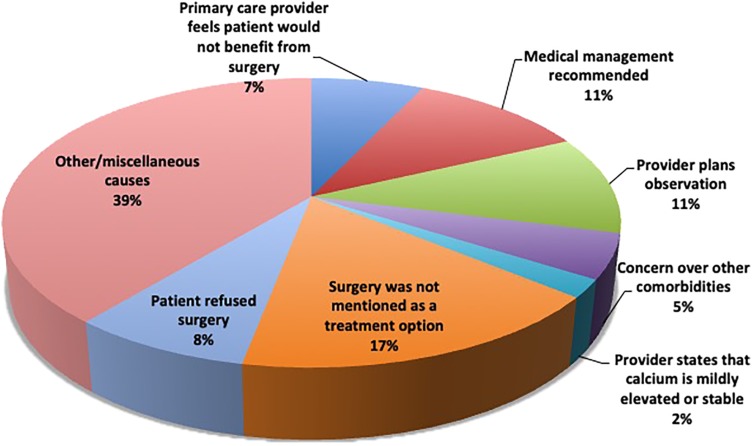
Reasons for Delayed Surgical Referral
The diagnosis of hyperparathyroidism was missed in 10% of patients with clear complications of hyperparathyroidism (kidney stones, osteoporosis, or fractures) with elevated calcium and/or PTH who met the NIH consensus criteria for treatment [9]. Of the 60 patients with hyperparathyroidism in our cohort, 22 patients were diagnosed by their primary care providers with hyperparathyroidism (either by ICD codes or in their clinic notes), and only 20% (12 of 60) were referred for surgery. Interestingly, there were no differences in the rates of surgical referral based on the index PTH levels. Surgery was not even mentioned as a treatment option for 17% of the total cohort, including one third of patients in the highest PTH group (Table 1). Additionally, the likelihood that a patient's primary care physician discussed surgical management did not differ across the three PTH groups. Among patients who were not offered surgical referral, 7% were counseled by a nonsurgeon that surgery offered no benefit, and 22% were offered medical treatment (calcimimetics, bisphosphonates, vitamin D supplementation, and calcium) or observation as an alternative to parathyroidectomy (Fig. 4). The likelihood of patients being offered medical management for hyperparathyroidism was highest in the group with the highest index PTH levels. When the diagnosis of hyperparathyroidism was established and surgery was offered as a treatment option, only 8% (5 of 60) chose not to have an operation. Among the 12 patients (20%) who saw a surgeon, 100% were deemed eligible for parathyroidectomy. The median wait time from the index high calcium until surgery was 16 months.
Figure 4.
Common reasons why patients with hyperparathyroidism are not referred for curative parathyroidectomy.
Discussion
In this study, we identified common reasons for delays in diagnosis and treatment of hyperparathyroidism. Our results showed that the most common reasons for delayed diagnosis include failure to note hypercalcemia, inadequate workup for hypercalcemia, or not considering a diagnosis of hyperparathyroidism. We also found that health care providers appear to overestimate the benefits of medical therapy and/or observation and underestimate the potential benefits of parathyroidectomy, as indicated by low rates of surgical referral relative to medical management.
There are several potential explanations for why providers may miss an elevated calcium on laboratory testing or attribute hypercalcemia to other causes. First, busy primary care physicians process hundreds of laboratory values in any given week, making it relatively easy to miss any single abnormality in the flood of clinical information. Because high calcium may be considered of lesser importance than laboratory values related to diabetes or to kidney or liver dysfunction, providers may not experience a sense of urgency related to diagnosis or further workup. Furthermore, we noticed a tendency to evaluate hypercalcemia by repeating the calcium measurement without checking a PTH level. Continuing to repeat calcium levels without checking PTH does not provide enough information to diagnose the cause of hypercalcemia because a seemingly normal calcium is indicative of hyperparathyroidism if the PTH is inadequately suppressed (normo‐calcemic hyperparathyroidism). Second, a significant proportion of patients had their index hypercalcemia occur in the inpatient or emergency room settings. When patients are admitted for other medical problems, it is relatively easy to miss an additional laboratory abnormality, and the hypercalcemia may never be referred to the patient's primary care provider for further evaluation. Of note, 73% of our cohort were seen in an outpatient setting; therefore, the percentage of each reason that hypercalcemia was attributed to causes other than hyperparathyroidism might have been different if there had been an equal representation of outpatient and inpatient settings. However, this difference likely reflects what is seen in clinical practice, as outpatient visits with primary care physicians are more common than inpatient visits.
When it comes to referring patients for surgery, the majority of patients (61%) who did not see a surgeon were either told that they would not benefit from an operation or never had surgery discussed as a treatment option (Fig. 4). This can be explained with several reasons. First, providers may be confused by the various guidelines related to treatment recommendations for “asymptomatic” hyperparathyroidism. There may also be a mistaken sense that hyperparathyroidism does not have a substantial impact on health in the absence of significant bone disease or development of kidney stones. There also appears to be a belief among primary care physicians that either medical management or just observing patients with hyperparathyroidism is preferable to surgery. However, in their recently published cost‐effectiveness study that compared parathyroidectomy with observation for patients with asymptomatic hyperparathyroidism, Zanocco et al. found that parathyroidectomy is a less costly and more effective treatment strategy that leads to a significantly greater quality‐adjusted life expectancy [7]. There is currently no medical management that actually treats the underlying parathyroid dysfunction that causes hyperparathyroidism, and it is entirely unclear whether “medical management” does more than expose patients to the side effects and costs of medication. Second, physicians who do not perform parathyroidectomy likely have little sense of what the operation entails or the ratio of risks and benefits. This may lead them to overestimate the potential risks of surgery and to underappreciate the benefits for patients with hyperparathyroidism. Minimally invasive parathyroidectomy has been shown to reduce operative time, decrease morbidity, and have a higher cure rate [10], [11]. Third, patients may not have been informed about the extreme low risk of minimally invasive parathyroidectomy, even among those with significant comorbidities (5% of our cohort), in order to consider seeing a surgeon [12]. Although not all patients with hyperparathyroidism will be candidates for surgery, the optimal person to have a conversation about the risks and benefits of parathyroidectomy is a surgeon who frequently performs the operation. Recognition of this fact has prompted the American Association of Endocrine Surgeons to recommend that patients with hyperparathyroidism at least have the opportunity to discuss treatment options with a surgeon, regardless of whether they ultimately undergo surgery [5]. This would enable all patients with hyperparathyroidism to make informed decisions about their care.
Our study adds to the existing literature by exploring the mechanisms behind the significant underdiagnosis and undertreatment of hyperparathyroidism. Prior work demonstrated the extent of the problem but did not explore why the disease is underdiagnosed or undertreated. Our group evaluated 10,432 patients with hypercalcemia (>10.5 mg/d) over a 5‐year period and found that only 28% had a documented diagnosis of hypercalcemia and 31% had PTH levels measured. In this study, only 22% of eligible patients were referred for surgical evaluation [2]. Similarly, Yeh et al. found that 39%–51% of eligible patients underwent parathyroidectomy in the Kaiser Permanente health system, and Kuo et al. showed that only 30% of eligible patients in California underwent treatment [13], [14].
Several limitations of this study should be acknowledged. First, the sample size is relatively small and may not be broadly representative of outcomes at other institutions. However, our findings have considerable face validity and appear to explain the consistently low rates of diagnosis and treatment for hyperparathyroidism observed at our institution and others. Our findings also reflect the consensus of our team and conversations with several experienced endocrine surgeons on factors likely related to diagnosis and treatment. Additionally, rather than providing a definitive explanation for delays in the diagnosis and treatment of hyperparathyroidism, this study was meant to be exploratory and to establish a framework for future qualitative evaluation of this complex problem. Our preliminary list of barriers to diagnosis and treatment can be further explored through semistructured interviews or focus groups with primary care providers and patients to more fully understand patient, provider, and system factors that should be targeted for intervention. Second, our analysis is limited to what is documented in patients’ charts, and it is possible that clinicians made decisions or plans that were not documented. We were careful, however, to search for evidence of treatment plans in notes, provider‐patient communications, and laboratory orders to minimize the risk of missing action plans. Additionally, we plan to conduct future qualitative work to explore how primary care providers approach the diagnosis and treatment of hyperparathyroidism. Our current work is useful to help design an appropriate interview guide and coding scheme for that analysis. Regarding the decision to refer patients for surgery, we know that untreated hyperparathyroidism increases the risk of fractures by 75%, cardiovascular disease by 250%, kidney stones by 500%, and dementia by 41%. Hyperparathyroidism also leads to a 14‐fold increase in renal failure and a 40% increase in mortality [15], [16]. Advancements in surgical techniques have also made the operation safer and well tolerated by patients, so that the majority of parathyroidectomies can be done on an outpatient basis. Consequently, professional society guidelines have begun to reflect a growing consensus that any patient who is a reasonable candidate for surgery should at least be offered the opportunity to decide whether they want to have a parathyroidectomy [5], [17].
Conclusion
Our study provides insight into why hyperparathyroidism is underdiagnosed and undertreated. We identified common problems that could delay diagnosis and treatment of hyperparathyroidism. Importantly, many of these factors can be addressed by a clinical intervention. The number of patients with missed hypercalcemia could be reduced by machine learning algorithms that scour the medical record and prompt providers to further evaluate high calcium [18]. We could also educate providers and patients about the importance of early diagnosis and about the more subtle complications of hyperparathyroidism to create a sense of urgency for treatment. Regardless of the intervention components that are selected, our study provides a useful starting point for anyone interested in improving rates of diagnosis and treatment of hyperparathyroidism.
Author Contributions
Conception/design: Ammar Asban, Courtney J. Balentine
Provision of study material or patients: Rongbing Xie, James K. Kirklin
Collection and/or assembly of data: Ammar Asban, Alex Dombrowsky, Reema Mallick
Data analysis and interpretation: Ammar Asban, Courtney J. Balentine
Manuscript writing: Ammar Asban, James K. Kirklin, Raymon H. Grogan, David F. Schneider, Herbert Chen, Courtney J. Balentine
Final approval of manuscript: Ammar Asban, Alex Dombrowsky, Reema Mallick, Rongbing Xie, James K. Kirklin, Raymon H. Grogan, David F. Schneider, Herbert Chen, Courtney J. Balentine
Disclosures
James K. Kirklin: Xeltis (C/A). The other authors indicated no financial relationships.
(C/A) Consulting/advisory relationship; (RF) Research funding; (E) Employment; (ET) Expert testimony; (H) Honoraria received; (OI) Ownership interests; (IP) Intellectual property rights/inventor/patent holder; (SAB) Scientific advisory board
References
- 1.Yeh MW, Ituarte PH, Zhou HC et al. Incidence and prevalence of primary hyperparathyroidism in a racially mixed population. J Clin Endocrinol Metab 2013;98:1122–1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Balentine CJ, Xie R, Kirklin JK et al. Failure to diagnose hyperparathyroidism in 10,432 patients with hypercalcemia: Opportunities for system‐level intervention to increase surgical referrals and cure. Ann Surg 2017;266:632–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Press DM, Siperstein AE, Berber E et al. The prevalence of undiagnosed and unrecognized primary hyperparathyroidism: A population‐based analysis from the electronic medical record. Surgery 2013;154:1232–1238. [DOI] [PubMed] [Google Scholar]
- 4.Weber T, Eberle J, Messelhauser U et al. Parathyroidectomy, elevated depression scores, and suicidal ideation in patients with primary hyperparathyroidism: Results of a prospective multicenter study. JAMA Surg 2013;148:109–115. [DOI] [PubMed] [Google Scholar]
- 5.Wilhelm SM, Wang TS, Ruan DT et al. The American Association of Endocrine Surgeons Guidelines for definitive management of primary hyperparathyroidism. JAMA Surg 2016;151:959–968. [DOI] [PubMed] [Google Scholar]
- 6.Brito K, Edirimanne S, Eslick GD. The extent of improvement of health‐related quality of life as assessed by the SF36 and Paseika scales after parathyroidectomy in patients with primary hyperparathyroidism‐‐a systematic review and meta‐analysis. Int J Surg 2015;13:245–249. [DOI] [PubMed] [Google Scholar]
- 7.Zanocco KA, Wu JX, Yeh MW. Parathyroidectomy for asymptomatic primary hyperparathyroidism: A revised cost‐effectiveness analysis incorporating fracture risk reduction. Surgery 2017;161:16–24. [DOI] [PubMed] [Google Scholar]
- 8.Elixhauser A, Steiner C, Harris DR et al. Comorbidity measures for use with administrative data. Med Care 1998;36:8–27. [DOI] [PubMed] [Google Scholar]
- 9.conference NIH. Diagnosis and management of asymptomatic primary hyperparathyroidism: Consensus development conference statement. Ann Intern Med 1991;114:593–597. [DOI] [PubMed] [Google Scholar]
- 10.Bergenfelz A, Lindblom P, Tibblin S et al. Unilateral versus bilateral neck exploration for primary hyperparathyroidism: A prospective randomized controlled trial. Ann Surg 2002;236:543–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adler JT, Sippel RS, Chen H. The influence of surgical approach on quality of life after parathyroid surgery. Ann Surg Oncol 2008;15:1559–1565. [DOI] [PubMed] [Google Scholar]
- 12.Reema Mallick HC. Diagnosis and management of hyperparathyroidism. Adv Surg 2018;52:137–153. [DOI] [PubMed] [Google Scholar]
- 13.Yeh MW, Wiseman JE, Ituarte PH et al. Surgery for primary hyperparathyroidism: Are the consensus guidelines being followed? Ann Surg 2012;255:1179–1183. [DOI] [PubMed] [Google Scholar]
- 14.Kuo EJ, Al‐Alusi MA, Du L et al. Surgery for primary hyperparathyroidism: Adherence to consensus guidelines in an academic health system. Ann Surg 2019;269:158–162. [DOI] [PubMed] [Google Scholar]
- 15.Yu N, Donnan PT, Leese GP. A record linkage study of outcomes in patients with mild primary hyperparathyroidism: The Parathyroid Epidemiology and Audit Research Study (PEARS). Clin Endocrinol 2011;75:169–176. [DOI] [PubMed] [Google Scholar]
- 16.Hagstrom E, Kilander L, Nylander R et al. Plasma parathyroid hormone is associated with vascular dementia and cerebral hyperintensities in two community‐based cohorts. J Clin Endocrinol Metab 2014;99:4181–4189. [DOI] [PubMed] [Google Scholar]
- 17.Bilezikian JP, Bandeira L, Khan A et al. Hyperparathyroidism. Lancet 2018;391:168–178. [DOI] [PubMed] [Google Scholar]
- 18.Somnay YR, Craven M, McCoy KL et al. Improving diagnostic recognition of primary hyperparathyroidism with machine learning. Surgery 2017;161:1113–1121. [DOI] [PMC free article] [PubMed] [Google Scholar]